Abstract
Background/Aims:
There are many similarities and overlaps in clinical, radiological, endoscopic, and histological features among intestinal tuberculosis (ITB), Crohn's disease (CD), and primary intestinal lymphoma (PIL), and the differential diagnosis of ITB can be very challenging for clinicians.
Patients and Methods:
The clinical, radiologic, endoscopic, and pathological data of 213 patients were analyzed retrospectively. According to the diagnostic criteria and exclusive criteria of ITB, CD, and PIL, 83 patients were recruited and divided into three groups, including 30 cases in the ITB group, 38 cases in the CD group, and 15 cases in the PIL group, and the medical data and statistical analysis were recorded.
Results:
Rural patients with abdominal pain as the first symptom and with transverse ulcer and caseating granulomas were more common in the ITB group than the CD group, whereas urban patients with stool change as the first symptom, moderate or severe anemia, thickening of intestinal wall, rectal involvement, skipping distribution, prominent lymphoid aggregates, and irregular glands were more common in CD group than ITB group (P < 0.05). Young patients (age < 30 years) with fever, weakness, fatigue, abdominal mass, intestinal perforation, and emergent operation were more common in ITB group than PIL group, whereas thickening of intestinal wall, malignant lymphocytes, limited distribution, and involvement of small intestine occurred more in PIL group than ITB group (P < 0.05).
Conclusion:
The differential diagnosis of ITB from CD and PIL can be made by a combination of clinical manifestation, endoscopy, and pathological examinations.
Keywords: Crohn's disease, clinic, differential, diagnosis, intestinal tuberculosis, primary intestinal lymphoma
Intestinal tuberculosis (ITB) is a specific chronic intestinal disease caused by Mycobacterium tuberculosis infection. Nowadays there is still no sensitive, accurate, convenient, and specific marker to diagnose ITB. In recent decades, with the improvement of economy, life quality and sanitary conditions, the incidence of tuberculosis (TB) has declined and the prevalence of ITB has gradually reduced. According to the fifth national TB epidemiological sample report in China, TB epidemic status is still serious and unbalanced. Therefore, clinicians still need to pay considerate attention to ITB.
Crohn's disease (CD) is a chronic gastrointestinal inflammatory granulomatous disease whose etiology is not clear yet. CD is a common disease in the United States and European countries. In China, the incidence of CD is lower but not uncommon, and with industrialization and urbanization, the incidence of CD in China and other developing countries is gradually increasing.[1,2]
The clinical manifestations of primary intestinal lymphoma (PIL) are nonspecific, such as abdominal pain, vomiting, weight loss, and intestinal perforation.[3] Although the incidence is not high, it is similar to ITB in clinical manifestations and still needs to be distinguished.
A large number of clinical case reports and analysis show that they are frequently difficult to distinguish and are misdirected at one another.[4,5] In China, ITB is more common than CD and PIL, however, the pathogenesis and treatment of the three diseases are quite distinct, and misdiagnosis and inappropriate management will dramatically interfere with the life quality and increase the medical expenditure. Furthermore, a misdiagnosis will lead to a delay in initiating effective therapy, which may aggravate the illness and even threaten life. Hence making an accurate diagnosis at the earliest possible stage is very important.[6] Through this study, we hope to find some meaningful clinical indicators to identify the three diseases and provide a reference for the diagnosis of ITB.
PATIENTS AND METHODS
Subjects
According to the medical record system, we reviewed 213 hospitalized cases (82 cases of ITB, 109 cases of CD, and 22 cases of PIL) from May 2007 to October 2012 in Renmin Hospital and Zhongnan Hospital of Wuhan University. The data of endoscopy, surgery, and histological examination and clinical effects were collected. According to the inclusion criteria and exclusion criteria enrolled in the study group, a total of 83 patients were ultimately enrolled.
Methods
The diagnosis of ITB will comply with any of the following: (1) presence of caseating granulomas on histology of disease tissue (intestine, peritoneum, or lymph nodes); (2) demonstration of acid-fast bacilli (AFB) on smear or on histological section; (3) positive culture for acid-fast bacilli; (4) histological or microbiological confirmed TB at extraintestinal site; (5) positive result of TB-PCR; (6) highly suspected cases considered by the combination of clinical, endoscopic, and histological features and sensitive response to anti-TB drugs.[7] The diagnosis of CD is based on the standard specification of inflammatory bowel disease diagnosis and treatment.[8] The diagnosis of PIL coincides with the 1961 Dawson proposed standards.[9] Cases of ulcerative colitis, repeated cases and cases that lost vital information were excluded.
Statistical analysis
We designed a scale to analyze patients' clinical, laboratory, imaging, and endoscopy information. And the collected data were divided into three groups (ITB group, CD group, and PIL group). Comparative statistical methods were applied to analyze the differences among the groups. Univariate measurement data were used in the analysis of variance. If the collected data did not comply with the normal distribution, KW nonparametric test method would be used for analysis. Univariate count data were analyzed by the Chi-square test, and if the data did not comply with the conditions of the Chi-square test, Fisher's exact method was applied. A probability (P) value of less than 0.05 was considered statistically significant.
RESULTS
Demographic features
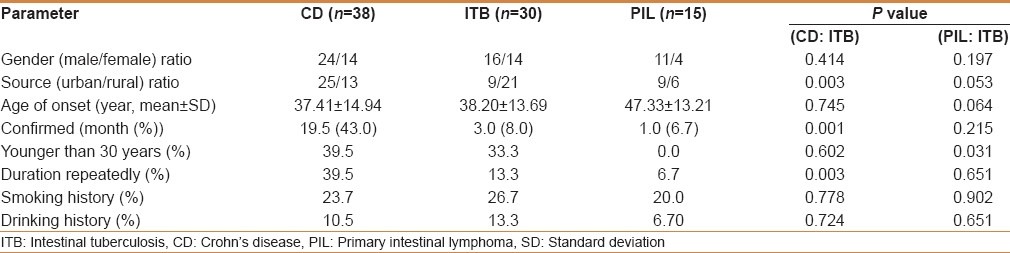
There were no significant differences in patients' gender ratio and average age among the three groups. However, there were fewer patients younger than 30 years in the PIL group compared to the ITB group (P < 0.05). The geographical ratio of ITB (urban: Rural) was 1:2.33, whereas the ratio of CD was 1.92:1 (P < 0.05). The median time from onset to diagnosis in the CD group was 19.5 months, whereas in the ITB group it was 3.0 months [Table 1].
Table 1.
Differences of demographic features
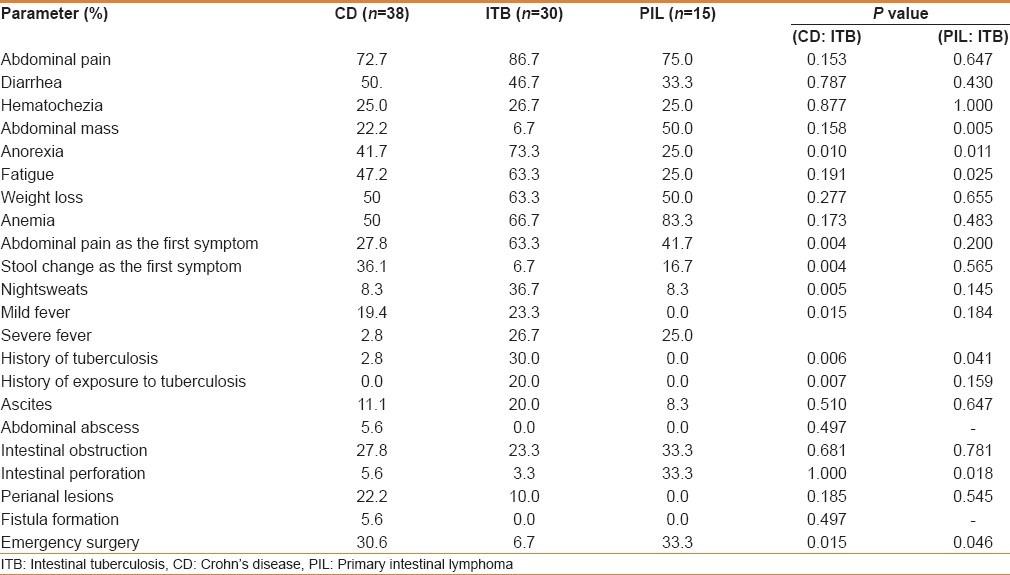
Comparisons of clinical manifestations and complications
Abdominal pain was the initial symptom of ITB more frequently, whereas the change in stool was more common in CD (P < 0.05). Additionally, the incidences of anorexia, night sweats, and fever were higher than those in the CD group (P < 0.05). PIL patients frequently had palpable abdominal mass, and the incidence of abdominal mass was significantly higher than that in the ITB group (P < 0.05). Besides, PIL patients who needed emergency surgical treatments due to complications were more common than those in the ITB group [Table 2].
Table 2.
Differences of clinical manifestations
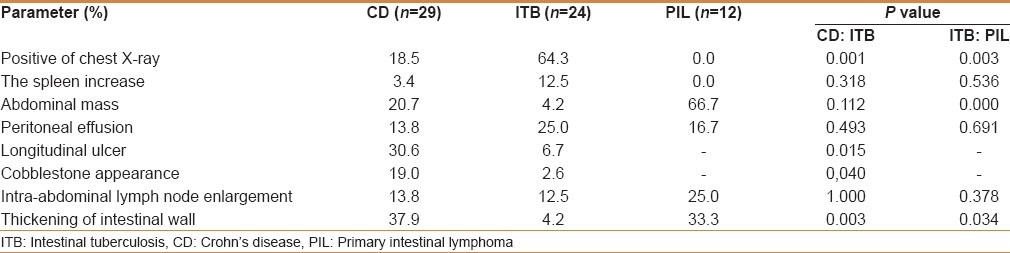
Imaging examinations
Chest X-ray examinations showed that 18.5% patients of the CD group and 64.3% of ITB patients had active pulmonary TB (P < 0.05). Longitudinal ulcer and cobblestone appearance occurred more in the CD group when compared to the ITB group no barium examinations [Figure 1]. In the PIL group, 66.7% of patients had palpable abdominal masses, whereas in the ITB group these occurred in only 4.2% [Table 3].
Figure 1.
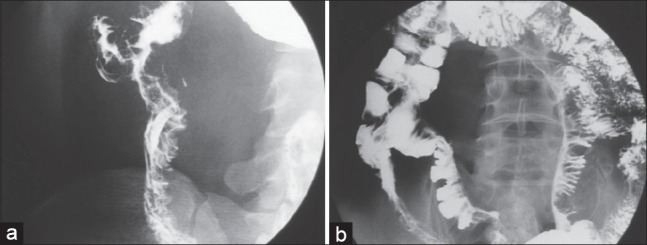
Barium findings. (a) Narrowing deformation and ulcers of varying sizes of ascending colon were found in ITB group. (b) Longitudinal ulcers and stiff bowel of mesenteric edge, and cobblestone-some appearance were found in the CD group
Table 3.
Differences of imaging examinations
Lesions and morphological comparisons
The predilection sites of three the three diseases were the ileocecal valve and terminal ileum. But lesions that involved the right colon only occurred more frequently in the ITB group compared to the CD group (P < 0.05). While the incidence of rectal lesions in CD was higher compared to ITB (26.5% vs. 3.3%, P < 0.05). Segmental distribution of lesions was more common in CD than ITB (P < 0.05). Longitudinal ulcers were more common in the CD group, whereas transverse ulcers were more common in the ITB group (61.9% vs. 40.9%, P < 0.05). Ulcers in the PIL group were rare, but when present, the lesion would be irregularly large and deep. Lumps occurred more frequently in the PIL group compared to the ITB group (91.7% vs 26.7%, P < 0.05) [Table 4 and Figure 2].
Table 4.
Locations of lesions and morphology
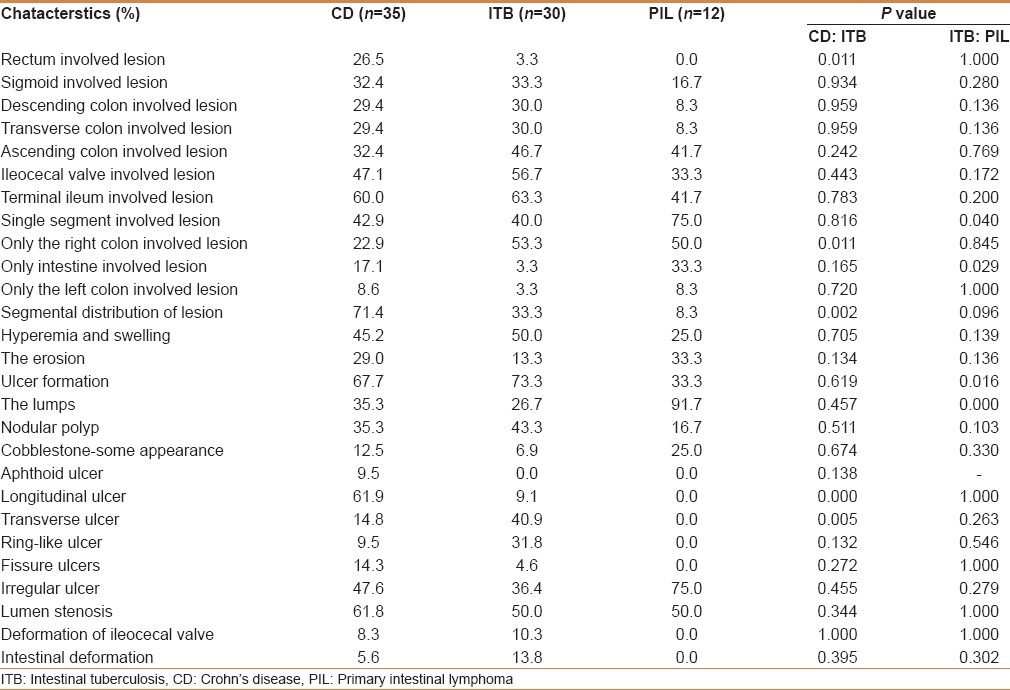
Figure 2.
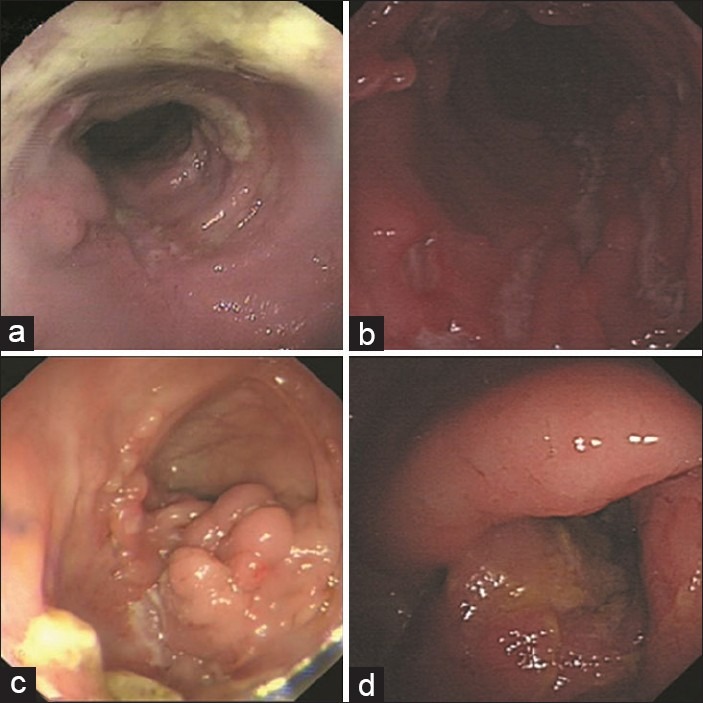
(a) Ring-like ulcer in ITB. (b) Longitudinal ulcer in CD. (c) Nodule mass-like hyperplasia in ITB. (d) Large lump in PIL
Results of mucosal biopsies
The incidences of granulomas in CD and ITB were 31.0% and 42.1% respectively, whereas noncaseating granulomas were 31.0% and 18.4% respectively. However, caseous granulomas occurred only in ITB when compared to CD (23.7% vs 0.0%, P < 0.05). The incidences of submucosal lymphoid aggregates and irregular glandular structures were 19.0% and 15.5% in the CD group, whereas these changes were not seen in the cases with ITB (P < 0.05). The detection rate of atypical lymphocytes in the PIL group was 71.4%, which was not seen in the ITB group (0.0%, P < 0.05). There were no granulomas in the PIL group, whereas the incidence of granulomas in the ITB group was 42.1% (P < 0.05) [Table 5 and Figure 3].
Table 5.
Comparisons of mucosal biopsy
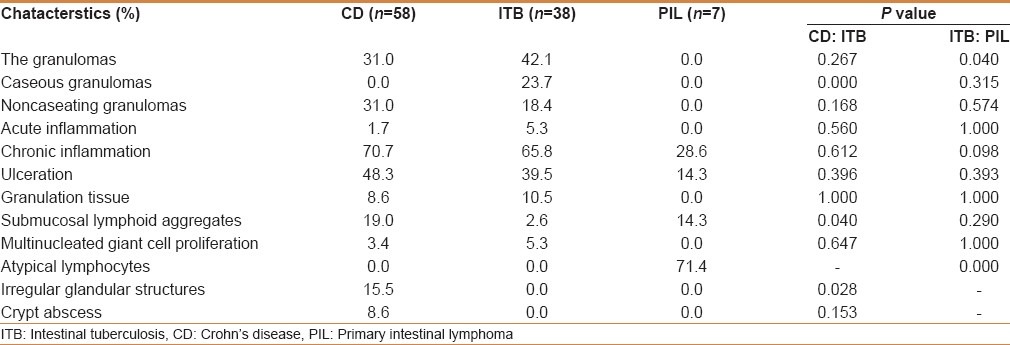
Figure 3.
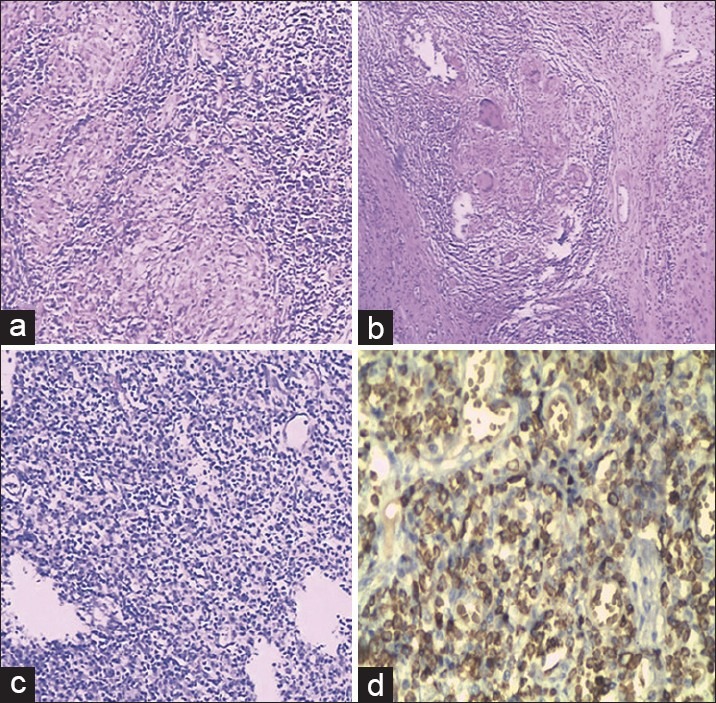
Pathological features. (a) Caseating granulomas from the mucosa of a patient with ITB [HE, ×100] (b) Large granulomas in the ulcerated mucosa of a patient with CD [HE, ×100]. (c) Atypical lymphoid from the mucosa of a patient with PIL [HE, ×100]. (d) Atypical lymphoid from the mucosa of a patient with PIL [IHC, ×100]
DISCUSSION
The diagnosis and identification of ITB is still a difficult challenge due to the lack of an economical, simple, and reliable diagnostic method. In China, TB is still endemic in some areas.[1] In recent decades, the TB incidence has declined in developed countries, but the incidence remains high in countries that have high rates of HIV infection, high rates of diabetes, high prevalence of malnutrition, and crowded living conditions.[10] A report showed that, in 2005, there were less than 25 TB patients in North America, 25-49 patients in Brazil, and more than 100 patients in South Africa per 100,000 people.[11] Along with the high incidence of TB, ITB has also elevated in incidence. At the same time, the number of patients with CD multiplied in the same region.[2] Although the incidence rate of PIL is not high, its clinical presentation is similar to ITB. Therefore, it is particularly important to discriminate ITB from CD and PIL in China.
Differentiations between ITB and CD
In this study, ITB patients were still mostly from rural areas whereas the majority of patients in the CD group were from urban areas. ITB is more common in rural areas and the reasons may be as follows: (1) People are vulnerable to TB due to poor living conditions, poor nutritional status, and weak resistance to disease; (2) Poor sanitation and poor hygiene habits provide routes of transmission for TB, and (3) Therapy of ITB is not desirable owing to lack of health awareness, timely attendance, and treatment compliance. The specific impact of the mechanism needs to be studied, but the geographical differences of patients for the differential diagnosis have certain reference significances. We also found that the first symptom of ITB patients was abdominal discomfort or abdominal pain, whereas that in the CD group tended to be diarrhea or hematochezia. We speculated that ITB lesions were not only inflammatory ulcers, but also proliferative lesions, whereas in CD the full-thickness of the intestinal wall was involved with inflammation as well as ulcers ITB lesions were confined to the right colon, whereas CD lesions were broader and rectal lesions were common. Therefore, when symptoms in patients were complex and lack specificity, the first symptom played a role in differentiating ITB and CD.
In Western countries, CD patients tend to present with intestinal fistulas, perianal disease, and extraintestinal manifestations,[12,13] but according to an epidemiologic study in China, intestinal fistulas and perianal diseases were rare in CD patients.[14] Extraintestinal manifestations of CD patients in our study group were rare to see. Therefore, the above clinical manifestations in differentiating CD and ITB were not sensitive. These differences may be due to mild progression of CD in China, but the exact cause needs to be further studied. Additionally, there were also reports that suggested fistulas from TB do occur.[15,16,17] These phenomena reduced the value of intestinal fistulas, perianal lesions, and extraintestinal manifestations for the differential diagnosis of ITB. Furthermore, there was more frequent need of emergency surgeries in the CD group when compared to ITB which might indicate that CD tended to develope more serious complications when compared to ITB.
Abdominal B ultrasound and computed tomography (CT) examinations had a certain value for the diagnosis of CD and ITB. The use of barium meals systematically can delineate the extent of the disease but the use of CT scans, abdominal ultrasound, and endoscopic ultrasound can image the layers of the intestinal wall and degree of involvement.
This study suggested that CD lesion distribution was wider than ITB and ITB tended to be limited to the ileocecum and its surrounding bowel. CD often involved the rectum. rectal involvement has been reported to occur in up to 39% of cases which might aid in differentiating ITB from CD.[18] Recent studies have shown that the incidence of CD associates with an abnormal immune response to normal intestinal flora that could colonize in any part of the intestine, which can explain the reason why the CD lesions distributed more widely than ITB with lymphocytes tendency.[19] When endoscopic examination reveals extensive intestinal lesions or lesions involving the rectum with a segmental distribution, we should consider the possibility of CD.
Both ITB and CD are chronic granulomatous conditions and show an overlap in their histological features.[20] This study revealed the significance of repeated biopsies to increase the diagnosis rate of ITB. ITB lesions were located in the ileocecum and more limited than CD lesions. ITB endoscopic mucosal biopsies were chiefly taken from a single lesion, whereas the number of CDs biopsy sites was more than ITB group due to the wide distribution of lesions. These may have an impact on the efficiency of endoscopic biopsy. However, one of the limitations of mucosal biopsies is that granulomas are found in only 50%-80% of intestinal mucosal biopsies from patients with clinically confirmed TB and in 15%-65% of mucosal biopsies from patients with CD.[4]
In this study, granuloma detection rate in the ITB group and the CD group were 42.1% and 31.0% respectively. Among these lesions, the incidence of confluent granulomas with caseous necrosis in the ITB group was 23.7%, whereas none were found in the CD group. Caseous granulomas remain to be a specific marker of ITB. Therefore, if the pathological examination only finds noncaseating granulomas, it is not an instant evidence of CD, which requires a combination of other pathological changes. And if pathological examinations find both noncaseating granulomas and lymphocyte aggregations in the submucosa, the patient was more likely to have a diagnosis of CD. In addition, the irregular mucosal glandular structure plays a definite role in the differentiation between ITB and CD, especially on the basis of noncaseating granulomas, which tends to contribute to the diagnosis of CD. The reason why CD appeared as an unclear and irregular structure of mucous gland is not clear yet, the reason maybe its association with the degree of CD lesions.
Differentiations between ITB and PIL
It is reported that there were more people older than 40 years with PIL[21] and more people younger than 40 years with ITB.[22] But in this study, there were 33.3% patients with ITB under the age of 30 years, whereas not even one in the PIL group. According to our results, the age of onset in the PIL group was younger than that in past reports, but occurrence below 30 years was rare. Therefore, there was no difference in the possibility of patients older than 30 years between ITB and PIL while it is more likely to be ITB when the patient was younger than 30 years.
In three PIL cases with high fever, two cases had intestinal perforation and acute peritonitis. This revealed that it is rare to find fever in PIL patients, which is caused by the original disease. It was reported that the fever of PIL would definitely contribute to the diagnosis in the past; however, this was not the case in our study and when fever is present a look for a complication as a cause of fever is warranted. Low-grade fever symptoms were more likely to be diagnosed as ITB. In this study, 63.3% patients with PIL had abdominal masses, which was higher than that in previous reports (28.6%).[21] Thus, careful and repeated abdominal examinations on patients were very important to the differential diagnosis. The lesion progression of PIL developed rapidly and lesions invasion was forcing, so patients often went to hospital for acute perforation and severe abdominal pain. Thus, when the patient has acute abdominal pain, we should consider the possibility of PIL.
Similar to the ITB group, the lesions occurred more often in the ileocecum and right colon in the PIL group. Another research showed that the sigmoid colon and rectum were the second most common site usually involved.[21] In this study, there was no case of rectal involvement in the PIL group, which suggested that the frequency of PIL rectal involvement had geographical difference.[21] In China, PIL and ITB lesions rarely involved the rectum, was somewhat helpful in the differential diagnosis. Additionally, PIL lesions were more likely to be limited than ITB. Therefore, the diagnosis tended to be ITB when multiple parts of the the intestinal tract was involved. Ten patients of the PIL group had a huge mass, whereas two patients of ITB showed multiple segments of nodular hyperplasia. The typical ulcers of PIL were diffuse or had irregular shapes.
Pathology examinations revealed that the typical heterotypic lymphocyte, is a gold standard for the diagnosis of PIL. The detection rate of granuloma was 42.1% in the ITB group, none were seen in the PIL group (P < 0.05). Still, misdiagnosis based on the presence of a few atypical lymphocytes has been reported.[22] It would be beneficial to increase the biopsy yield by taking multiple samples or receiving anti-TB treatment or even laparotomy if necessary.
Quantiferon-TB Gold test (QFT) is a blood interferon-γ release test that measures the release of IFN-γ after stimulation in vitro by MTB.[23] This test was approved by the US Food and Drug Administration as an aid in diagnosing MTB infection, including both latent TB infection and TB disease.[23] The advantage of this test can exclude the interference of Bacillus Calmette Guerin vaccine and non-TB mycobacterium, thus it has a high specificity. However, the practical value of QFT has not yet been confirmed by a large scale study. The advent of QFT provides an important new indirect tool for the clinician to assist in the diagnosis of ITB. But a positive QFT result is not a diagnostic standard for ITB and the QFT has a supplementary role in the differential diagnosis of ITB.[24]
Footnotes
Source of Support: This work was supported by National Natural Science Foundation of China (Key Grant No. 81170350) and Hubei Province Natural Science Fund of China (Key Grant No.2009CDB283)
Conflict of Interest: None declared.
REFERENCES
- 1.Dye C. Global epidemiology of tuberculosis. Lancet. 2006;367:938–40. doi: 10.1016/S0140-6736(06)68384-0. [DOI] [PubMed] [Google Scholar]
- 2.Almadi MA, Ghosh S, Aljebreen AM. Differentiating intestinal tuberculosis from Crohn's disease: A diagnostic challenge. Am J Gastroenterol. 2009;104:1003–12. doi: 10.1038/ajg.2008.162. [DOI] [PubMed] [Google Scholar]
- 3.Ghimire P, Wu GY, Zhu L. Primary gastrointestinal lymphoma. World J Gastroenterol. 2011;17:697–707. doi: 10.3748/wjg.v17.i6.697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Makharia GK, Srivastava S, Das P, Goswami P, Singh U, Tripathi M, et al. Clinical, endoscopic, and histological differentiations between Crohn's disease and intestinal tuberculosis. Am J Gastroenterol. 2010;105:642–51. doi: 10.1038/ajg.2009.585. [DOI] [PubMed] [Google Scholar]
- 5.Zhou ZY, Luo HS. Differential diagnosis between Crohn's disease and intestinal tuberculosis in China. Int J Clin Pract. 2006;60:212–4. doi: 10.1111/j.1742-1241.2006.00702.x. [DOI] [PubMed] [Google Scholar]
- 6.Pulimood AB, Amarapurkar DN, Ghoshal U, Phillip M, Pai CG, Reddy DN, et al. Differentiation of Crohn's disease from intestinal tuberculosis in India in 2010. World J Gastroenterol. 2011;17:433–43. doi: 10.3748/wjg.v17.i4.433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Patel N, Amarapurkar D, Agal S, Baijal R, Kulshrestha P, Pramanik S, et al. Gastrointestinal luminal tuberculosis: Establishing the diagnosis. J Gastroenterol Hepatol. 2004;19:1240–6. doi: 10.1111/j.1440-1746.2004.03485.x. [DOI] [PubMed] [Google Scholar]
- 8.Cooperative Group of Inflammatory Bowel Disease of Chinese Medical Association. Chinese consensus on standard management of inflammatory bowel disease. Chin J Digest. 2007;27:545–50. [Google Scholar]
- 9.Dawson IM, Cornes JS, Morson BC. Primary malignant lymphoid tumours of the intestinal tract. Report of 37 cases with a study of factors influencing prognosis. Br J Surg. 1961;49:80–9. doi: 10.1002/bjs.18004921319. [DOI] [PubMed] [Google Scholar]
- 10.Dooley KE, Chaisson RE. Tuberculosis and diabetes mellitus: Convergence of two epidemics. Lancet Infect Dis. 2009;9:737–46. doi: 10.1016/S1473-3099(09)70282-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Epstein D, Watermeyer G, Kirsch R. Review article: The diagnosis and management of Crohn's disease in populations with high-risk rates for tuberculosis. Aliment Pharmacol Ther. 2007;25:1373–88. doi: 10.1111/j.1365-2036.2007.03332.x. [DOI] [PubMed] [Google Scholar]
- 12.Michelassi F, Stella M, Balestracci T, Giuliante F, Marogna P, Block GE. Incidence, diagnosis, and treatment of enteric and colorectal fistulae in patients with Crohn's disease. Ann Surg. 1993;218:660–6. doi: 10.1097/00000658-199321850-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cohen Z, McLeod RS. Perianal Crohn's disease. Gastroenterol Clin North Am. 1987;16:175–89. [PubMed] [Google Scholar]
- 14.Liu QS, Li L, Luo CH, Yang YS. Clinical features and of Crohn's disease: Comparison between 85 Chinese patients and 68 American patients comparison. Med J Chin PLA. 2006;31:863–5. [Google Scholar]
- 15.Molloy D, Sayana MK, Keane J, Mehigan B. Anal fistula: An unusual presentation of tuberculosis in a migrant health care professional. Ir J Med Sci. 2009;178:527–9. doi: 10.1007/s11845-008-0229-9. [DOI] [PubMed] [Google Scholar]
- 16.Wong WM, Lai KC, Yiu WC, Wong BC, Chan FL, Lai CL. Intestinal tuberculosis mimicking fistulizing Crohn's disease. J Gastroenterol Hepatol. 2007;22:137–9. doi: 10.1111/j.1440-1746.2006.03311.x. [DOI] [PubMed] [Google Scholar]
- 17.Penchev R, Karageorgiev A, Hristov P, Iordanov D, Abdominal TB. Peritonitis due to perforated intestinal TB and upper intestinal fistulas. Surgical treatment. Khirurgiia (Sofiia) 2010;6:65–8. [PubMed] [Google Scholar]
- 18.Liu XW, Li XF, Zou YY, Zhou MH, Ouyang CH, Wu XP, et al. Screening of clinical and endoscopic parameters for differentiating Crohn's disease and intestinal tuberculosis by logistic regression analysis. World Chin J Digestol. 2010;18:621–7. [Google Scholar]
- 19.Barnich N, Darfeuille-Michaud A. Role of bacteria in the etiopathogenesis of inflammatory bowel disease. World J Gastroenterol. 2007;13:5571–6. doi: 10.3748/wjg.v13.i42.5571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kirsch R, Pentecost M, Hall Pde M, Epstein DP, Watermeyer G, Friederich PW. Role of colonoscopic biopsy in distinguishing between Crohn's disease and intestinal tuberculosis. J Clin Pathol. 2006;59:840–4. doi: 10.1136/jcp.2005.032383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wong MT, Eu KW. Primary colorectal lymphomas. Colorectal Dis. 2006;8:586–91. doi: 10.1111/j.1463-1318.2006.01021.x. [DOI] [PubMed] [Google Scholar]
- 22.Liu H, Hu NZ, Wang LM. 55 cases of intestinal tuberculosis clinical features and misdiagnosis analysis. Chin J Digest. 2008;28:275–7. [Google Scholar]
- 23.Mazurek GH, Jereb J, Lobue P, Iademarco MF, Metchock B, Vernon A. Division of Tuberculosis Elimination, National Center for HIV, STD, and TB Prevention, Centers for Disease Control and Prevention (CDC). Guidelines for using the QuantiFERON-TB Gold test for detecting Mycobacterium tuberculosis infection, United States. MMWR Recomm Rep. 2005;54:49–55. [PubMed] [Google Scholar]
- 24.Kim BJ, Choi YS, Jang BI, Park YS, Kim WH, Kim YS, et al. Prospective evaluation of the clinical utility of interferon-gamma assay in the differential diagnosis of intestinal tuberculosis and Crohn's disease. Inflamm Bowel Dis. 2011;17:1308–13. doi: 10.1002/ibd.21490. [DOI] [PubMed] [Google Scholar]


