Abstract
Aim:
The aim of the following study is to evaluate the retinal nerve fiber layer (RNFL) and ganglion cell complex (GCC) thickness in patients with type 2 diabetes mellitus (DM).
Materials and Methods:
Average, inferior, and superior values of RNFL and GCC thickness were measured in 123 patients using spectral domain optical coherence tomography. The values of participants with DM were compared to controls. Diabetic patients were collected in Groups 1, 2 and 3. Group 1 = 33 participants who had no diabetic retinopathy (DR); Group 2 = 30 participants who had mild nonproliferative DR and Group 3 = 30 participants who had moderate non-proliferative DR. The 30 healthy participants collected in Group 4. Analysis of variance test and a multiple linear regression analysis were used for statistical analysis.
Results:
The values of RNFL and GCC in the type 2 diabetes were thinner than controls, but this difference was not statistically significant.
Conclusions:
This study showed that there is a nonsignificant loss of RNFL and GCC in patients with type 2 diabetes.
Keywords: Ganglion cell complex, optical coherence tomography, retinal nerve fiber layer, type 2 diabetes
Diabetic retinopathy (DR) is one of the most frequent causes of blindness in the working age population. As the prevalence of diabetes mellitus (DM) increases globally and patients live longer, the development of DR as a microvascular complication of DM also rises.[1] DR classified non-proliferative (NPDR) and proliferative (PDR). The optical coherence tomography (OCT) has been used for evaluation the thickness of retinal nerve fiber layer (RNFL) and ganglion cell complex (GCC) in some diseases.[2,3,4,5,6,7,8] The purpose of this study was to compare the RNFL and GCC thickness between diabetic patients and healthy subjects.
Materials and Methods
Two hundred and forty-six eyes of 123 patients were evaluated prospectively.
Inclusion criteria for diabetic patients were type 2 DM. Group 1 (n = 33) included patients who had no DR, Group 2 included 30 patients who had mild NPDR (n = 30 patients) and Group 3 (n = 30) included patients who had moderate NPDR. The control Group 4, included 30 healthy patients who have no systemic or ophthalmologic problems.
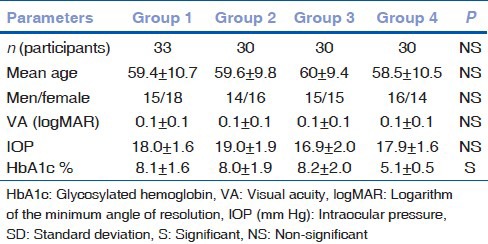
All patients in the control group were evaluated for undiagnosed DM [Table 1]. All participants evaluated by retinal specialists through indirect fundoscopy, slit-lamp stereo biomicroscopy and fundus fluorescein angiography. Mild NPDR was defined as microaneurysms only, moderate NPDR was defined more than just microaneurysms, but less than severe NPDR by international clinical DR disease severity scale.[9]
Table 1.
The characteristic features of participants in four groups
Exclusion criteria were refractive error (spheric Equivalent) >±3.00 diopters, visual acuity below 0.1 logarithm of the minimum angle of resolution, had significant media opacity, a history of glaucoma, uveitis, retinal disease, grade of DR >moderate DR and history of intraocular surgery in the last 6 months. All subjects underwent pupillary dilation (Tropicamide 1%, Alcon Lab, Inc., USA) and an ophthalmologic examination, including slit-lamp biomicroscopy (SL, Tokyo, Japan) with a +78 diopters handheld lens and OCT. Fundus fluorescein angiography (Kowa VX-10i, Kowa Company, Ltd., Tokyo, Japan) was performed in diabetic patients for excluded severe or proliferative retinopathy. The mean glycosylated hemoglobin (HbA1c) was calculated from all available HbA1c measurements in the last 6 months preceding the study visit in the diabetic patients. RNFL and GCC thickness were measured using spectral domain OCT (RTVue-100, Optovue Inc., Fremont, CA, USA).
The study adhered to the tenets of the Declaration of Helsinki. All participants gave written informed consent. This study was approved by local Ethics Committee. Statistical analyses were performed with SPSS 18.00 for Windows (SPSS, Chicago, IL, USA). Analysis of variance was used to assess differences in average age between diabetic patients with no DR, mild and moderate NPDR and controls. Average HbA1c and duration of diabetes were compared using the unpaired t-test between patients with no DR, mild and moderate NPDR.
Results
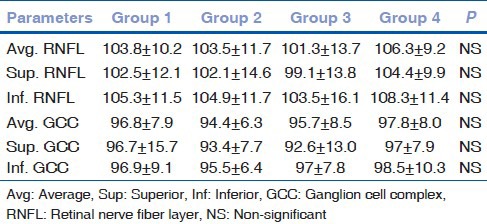
One hundred and twenty-three patients (246 eyes) were analyzed. The characteristic features of participants in four groups were summarized in Table 1. HbA1c level significantly higher in the patients with DM compared to the controls. The ratio of HbA1c was similar in diabetic patients. The values of RNFL and GCC are given in Table 2. GCC and RNFL were thinner in patients with DM compared to control but this difference was not statistically significant [Table 2].
Table 2.
The values of GCC and RNFL inf., sup., avg. in four groups
Discussion
The previous studies no showed absolutely agreement for status of RNFL and GCC in patients with type 2 DM. A study found that at early stage of DR, the macula and RNFL thickness were altered.[10] A study showed that only inferior RNFL thinning associated with peripheral neuropathy but age, duration of disease and retinopathy levels did not significantly influence RNFL thickness.[7]
An another study showed that only superior quadrant peripapillary RNFL thickness was slightly less in diabetic patients than normal subjects.[11]
This study was aimed to inspect the thickness of RNFL and GCC thickness in patients with type 2 DM.
The present study had some limitations. The sample size was small and study was not included patients severe NPDR or PDR. The grading of the severity of DR was done through ophthalmologic examination, including indirect fundoscopy and slit-lamp stereo biomicroscopy, instead of the gold standard, namely, seven-field stereoscopic fundus photography assessment by independent trained graders.
Conclusions
The RNFL and GCC thickness were thinner in patients with type 2 diabetes than controls, but this thinning was not statistically significant.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
References
- 1.King H, Aubert RE, Herman WH. Global burden of diabetes, 1995-2025: Prevalence, numerical estimates, and projections. Diabetes Care. 1998;21:1414–31. doi: 10.2337/diacare.21.9.1414. [DOI] [PubMed] [Google Scholar]
- 2.Firat PG, Doganay S, Demirel EE, Colak C. Comparison of ganglion cell and retinal nerve fiber layer thickness in primary open-angle glaucoma and normal tension glaucoma with spectral-domain OCT. Graefes Arch Clin Exp Ophthalmol. 2013;251:831–8. doi: 10.1007/s00417-012-2114-5. [DOI] [PubMed] [Google Scholar]
- 3.Davydovskaia MV, Tsysar’ MA, Boĭko AN, Akopian VS, Semenova NS, Filonenko IV, et al. Damage of macular ganglion cell complex and peripapillary retinal nerve fiber layer in multiple sclerosis. Zh Nevrol Psikhiatr Im S S Korsakova. 2012;112:47–51. [PubMed] [Google Scholar]
- 4.DeBuc Cabrera D, Somfai GM. Early detection of retinal thickness changes in diabetes using Optical Coherence Tomography. Med Sci Monit. 2010;16:MT15–21. [PubMed] [Google Scholar]
- 5.Rao HL, Babu JG, Addepalli UK, Senthil S, Garudadri CS. Retinal nerve fiber layer and macular inner retina measurements by spectral domain optical coherence tomograph in Indian eyes with early glaucoma. Eye (Lond) 2012;26:133–9. doi: 10.1038/eye.2011.277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kim NR, Lee ES, Seong GJ, Kang SY, Kim JH, Hong S, et al. Comparing the ganglion cell complex and retinal nerve fibre layer measurements by Fourier domain OCT to detect glaucoma in high myopia. Br J Ophthalmol. 2011;95:1115–21. doi: 10.1136/bjo.2010.182493. [DOI] [PubMed] [Google Scholar]
- 7.Shahidi AM, Sampson GP, Pritchard N, Edwards K, Vagenas D, Russell AW, et al. Retinal nerve fibre layer thinning associated with diabetic peripheral neuropathy. Diabet Med. 2012;29:e106–11. doi: 10.1111/j.1464-5491.2012.03588.x. [DOI] [PubMed] [Google Scholar]
- 8.Kim NR, Hong S, Kim JH, Rho SS, Seong GJ, Kim CY. Comparison of macular ganglion cell complex thickness by Fourier-domain OCT in normal tension glaucoma and primary open-angle glaucoma. J Glaucoma. 2013;22:133–9. doi: 10.1097/IJG.0b013e3182254cde. [DOI] [PubMed] [Google Scholar]
- 9.The Eye M.D association. International Clinical Diabetic Retinopathy Disease Severity Scale. American Academy of Ophthalmology. AAO. 05.01.2002. online for download: http://bit.ly/zqlw9e .
- 10.Oshitari T, Hanawa K, Adachi-Usami E. Changes of macular and RNFL thicknesses measured by Stratus OCT in patients with early stage diabetes. Eye (Lond) 2009;23:884–9. doi: 10.1038/eye.2008.119. [DOI] [PubMed] [Google Scholar]
- 11.Sugimoto M, Sasoh M, Ido M, Wakitani Y, Takahashi C, Uji Y. Detection of early diabetic change with optical coherence tomography in type 2 diabetes mellitus patients without retinopathy. Ophthalmologica. 2005;219:379–85. doi: 10.1159/000088382. [DOI] [PubMed] [Google Scholar]


