Abstract
Mammographic breast density is an established risk factor for breast cancer. However, results are inconclusive regarding its use in risk prediction models. The current study evaluated 13,409 postmenopausal participants in the NSABP Study of Tamoxifen and Raloxifene. A measure of breast density as reported on the entry mammogram report was extracted and categorized according to The American College of Radiology Breast Imaging Reporting and Data System (BI-RADS) classifications. An increased risk of invasive breast cancer was associated with higher mammographic breast density (P<0.001). The association remained significant after adjusting for age, treatment, and smoking history (HR 1.35, 95%CI 1.16-1.58), as well as when added to a model including the Gail score (HR 1.33, 95%CI 1.14-1.55). At five years after random assignment, time-dependent AUC improved from 0.63 for a model with Gail score alone to 0.64 when considering breast density and Gail score. Breast density was also significant when added to an abbreviated model tailored for estrogen receptor-positive breast cancers (P=0.02). In this study, high BI-RADS breast density was significantly associated with increased breast cancer risk when considered in conjunction with Gail score but provided only slight improvement to the Gail score for predicting the incidence of invasive breast cancer. The BI-RADS breast composition classification system is a quick and readily available method for assessing breast density for risk prediction evaluations; however, its addition to the Gail model does not appear to provide substantial predictability improvements in this population of postmenopausal healthy women at increased risk for breast cancer.
Keywords: Breast cancer risk, breast density, tamoxifen, raloxifene, Gail model
Introduction
Breast cancer is the most frequently diagnosed cancer among women worldwide (1). Therefore, accurately identifying women who have an increased risk for developing breast cancer so they may be targeted for increased screening or preventive interventions remains a high priority. The primary method for assessing non-genetic breast cancer risk is currently based on the Gail model (2-7). It is a validated statistical model that has been widely accepted for breast cancer prediction. The Gail model does not currently include a measure of breast density, which has been associated with a three- to five-fold increased risk of breast cancer for women with dense tissue occupying more than half of their breast (8-10). Some studies have suggested that adding a measure of breast density to the Gail model may improve its predictive capabilities (8, 11-13); however, it is not clear whether this is true in all populations or if the gain in predictability is of sufficient magnitude to warrant the addition of breast density to the model.
Breast density is most commonly measured through mammography. On a mammogram, fat appears dark since it is radiologically lucent; but connective and epithelial tissue are radiologically dense. Thus, mammographic breast density is a measure of the area of the breast that appears white on a mammogram. There are various methods for classifying mammographic breast density. Due to convenience and cost, the most widely used is based on The American College of Radiology Breast Imaging Reporting and Data System (BI-RADS), which is a comprehensive guide designed to standardize breast imaging reporting and terminology (14). According to BI-RADS, radiologists are instructed to include a separate rating category for both the mammographic findings and the breast composition or density in each mammogram report. The rating system for mammographic findings consists of seven categories of breast cancer risk and corresponding recommendations for the appropriate follow-up care. The classification system for breast density has four categories: almost entirely fat (<25% glandular), scattered fibroglandular densities (25-50% glandular), heterogeneously dense (51-75% glandular), or extremely dense (>75% glandular). The BI-RADS density classifications have been found to have only moderate inter-observer agreement. However, these guidelines are routinely followed in clinical practice in the United States for reporting mammographic breast density, making them readily available for possible use in risk prediction tools (15, 16).
The Gail model predicts a woman’s five-year and lifetime risk for developing breast cancer based on her reproductive, medical, and family history. The individual risk factors that are currently included in the model are age at assessment, race, the number of previous breast biopsies, history of atypical hyperplasia in the breast, age of menarche, parity, age at the first live birth of a child, and history of breast cancer in a first degree female relative (i.e., mother, sister, daughter). Any woman with a five-year risk of invasive breast cancer of 1.66% or greater is considered to be at high risk and should be evaluated further. Although some simple lifestyle modifications can help to reduce risk, other more complex prophylactic techniques may be considered. One’s risk for breast cancer can be reduced by bilateral mastectomy (90%), or chemopreventive therapies such as tamoxifen or raloxifene (50%). However, these interventions are not without risk for other complications or side effects (17-19). The Gail model has good calibration, which indicates accuracy in predicting incidence of breast cancer in subgroups of women. However, as is common with most risk prediction models for relatively rare diseases (20), the Gail model has low discrimination (c-statistics ranging from 0.58-0.62) and therefore only modestly distinguishes at the individual level who will and will not develop breast cancer.
Researchers have suggested that different risk prediction models might perform better for different subgroups of women (i.e., premenopausal vs. postmenopausal) or for different types of breast cancer (i.e., estrogen receptor [ER]-positive vs. ER-negative) (21). Using data from the Women’s Health Initiative (WHI), Chlebowski and colleagues attempted to find improved risk prediction models when considering ER-status among postmenopausal women (21, 22). They determined that adding additional risk factors to the Gail model did not provide significant improvement. However, they also found that for ER-positive breast cancer in postmenopausal women, a more parsimonious model performed nearly as well as the Gail model with similar discriminatory accuracy. The simpler model included age, family history of breast cancer, and a history of a previous breast biopsy. Chlebowski and colleagues assessed a number of personal characteristics but did not have the ability to assess breast density. Improving risk prediction models by including mammographic breast density has been supported in existing literature (8, 11-13); however, this needs to be studied in multiple independent populations before being put into clinical use.
In this report, we used data collected through the National Surgical Adjuvant Breast and Bowel Project (NSABP) Study of Tamoxifen and Raloxifene (STAR) to investigate the relationship between baseline mammographic breast density and the risk of invasive breast cancer. STAR was a randomized clinical trial that compared the relative effects of raloxifene to tamoxifen on breast cancer risk. We used data from this large breast cancer prevention trial to investigate whether a routine assessment of mammographic breast density improves the predictability of the Gail model.
Methods
Description of STAR
Between July 1, 1999, and November 4, 2004, 19,747 participants at nearly 200 clinical centers throughout North America were enrolled and randomly assigned to receive either tamoxifen or raloxifene. Each clinical center obtained approval from institutional review boards, and all participants provided written informed consent. In April 2006, initial trial results showed that raloxifene was as effective as tamoxifen in preventing invasive breast cancer and was less toxic (19). An update of the findings in 2010 indicated that raloxifene continued to have fewer side effects and maintained 76% of the effectiveness of tamoxifen in preventing invasive breast cancer (23).
STAR participants were postmenopausal with no previous history of invasive breast cancer. Upon entry, each participant was assessed for all risk factors included in the Gail model, and only those considered to be at high risk for developing breast cancer, defined by a Gail score ≥1.66% or having a history of lobular carcinoma in situ, were eligible for the study. Participants were also required to have had a baseline mammogram indicating absence of disease within one year prior to random assignment and were required to submit documentation of this mammogram to the NSABP Biostatistical Center. Women were excluded from STAR if they had a previous bilateral or unilateral prophylactic mastectomy, a history of invasive breast cancer, or invasive cancer of any other type less than five years before random assignment, with the exception of basal or squamous cell carcinoma of the skin. Other inclusion and exclusion criteria, along with additional details regarding the design and recruitment of STAR have been previously published (19).
Follow-up for STAR participants occurred every six months for the first five years of the study and annually thereafter. Each participant received an annual bilateral mammogram and a physical breast examination at each follow-up appointment. Participants were also assessed at each follow-up visit for information regarding all other events of interest including the diagnosis of other invasive cancers, cardiovascular disease, thromboembolic disease, and fractures. Staff members at each clinical center collected documentation for all reported events and submitted the documentation to the NSABP. Diagnosis of each event was then centrally reviewed and confirmed by trained medical professionals.
Study Design
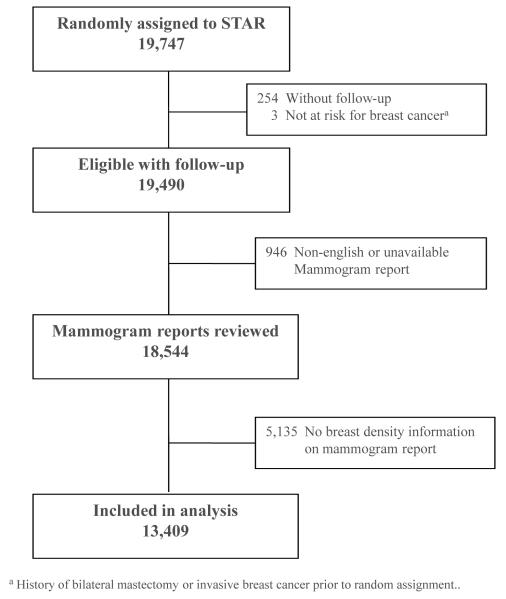
The current study included all STAR participants with follow-up for whom breast density information could be abstracted from the baseline mammogram report. Follow-up was based on data used in the most recent update of the trial (March 31, 2009), representing an average of 6.3 years. The flow of participants included in the current study is shown in Figure 1. Three women were excluded from the analyses because they were not at risk for invasive breast cancer because of a previous bilateral mastectomy or diagnosis of breast cancer.
Figure 1.
CONSORT diagram of the NSABP Study of Tamoxifen and Raloxifene (STAR) breast density analysis.
We used the entry mammogram reports to determine each woman’s BI-RADS category of breast density. Of the 19,490 eligible STAR participants with follow-up data, entry mammogram reports were reviewed for 18,544 women (95%). We did not include women with non-English mammogram reports (mostly from French-Canadian clinical sites) or those for whom we did not have an entry mammogram report available. An independent reviewer trained in radiology examined each available mammogram report and completed a breast density form based on the reported findings. Specifically, the reviewer searched each report for a qualitative description similar to the BI-RADS recommended terminology and/or a quantitative percentage of breast density. A derived BI-RADS breast density classification was then imputed from this information. At least one measure of breast density was described in the report for 13,409 participants, with most reporting only a qualitative description (99%). There were four mammogram reports that contained only percent breast density, and these were categorized into one of the four BI-RADS categories based on the coinciding recommended percentage ranges by the American College of Radiology. There were also 100 reports that included both measures, and of those, 93 contained a percent breast density that agreed with those recommended in the BI-RADS density classifications. For the remaining seven that did not agree, the derived BI-RADS breast density category was assigned based on the percent density information since it has been shown to be more accurate than the qualitative categories (15, 24).
The Gail scores were centrally calculated at the NSABP Biostatistical Center using information about all risk factors included in the Gail model collected from participants during eligibility assessments for STAR. Each participant’s height and weight were measured at entry by clinical staff members at each participating clinical center, and these measurements were used to calculate body mass index (BMI). Other variables, including smoking history and history of diabetes, were assessed via questionnaires that had been administered upon entry.
Statistical Analysis
We used the chi-square test to compare the distributions of participant characteristics at entry according to the derived BI-RADS categories of breast density. Cox proportional hazards regression was used to determine whether mammographic breast density at entry was associated with invasive breast cancer. Breast density was first explored as a 4-class variable; however, based on the appearance of an approximately linear increase in the hazards of invasive breast cancer, we decided to include breast density as a single ordinal term (with values 0, 1, 2, and 3 representing the four BI-RADS categories) in the model. We adjusted for possible explanatory variables including age, treatment group, BMI, years of cigarette smoking, and history of diabetes upon entry by including them in the model with breast density. The majority of the participants were white (93%), and there were only 19 cases of breast cancer diagnosed among non-white participants, so we did not include race/ethnicity as a potential factor. We used backward elimination to drop out all the potential variables that did not reach a statistically significant level of P<0.05. Because treatment with tamoxifen or raloxifene may differentially affect breast density, we tested for an interaction between breast density and treatment. We then added breast density to a model with the Gail score and subsequently to a model including Gail score and the significant explanatory variables. We calculated the time to invasive breast cancer as the time from random assignment to the date of diagnosis of invasive breast cancer. If the participant did not develop invasive breast cancer, her time was censored on the first of three possible occurrences including bilateral mastectomy, date of death, or date of last follow-up.
A secondary analysis investigated an abbreviated model developed by Chlebowski and colleagues (21) that was tailored for ER-positive breast cancer. Chlebowski’s abbreviated model included only age, number of first-degree relatives with breast cancer, and number of previous breast biopsies. Our measure of breast density was added to this model to determine whether it significantly improved the predictability for this specific type of breast cancer. The variables for number of relatives and biopsies were coded in the same way that was reported by Chlebowski et al. (0 or ≥1 for number of relatives and 0, 1, or >1 for number of biopsies) and time to diagnosis was censored for ER-negative invasive breast cancers and those for whom ER status was unknown. P values used to assess the statistical significance of variables in all modeling were determined using the likelihood ratio test, and all tests were evaluated using a 2-sided P value of 0.05. Analyses were performed using SAS version 9.2 software (SAS Institute, Inc.).
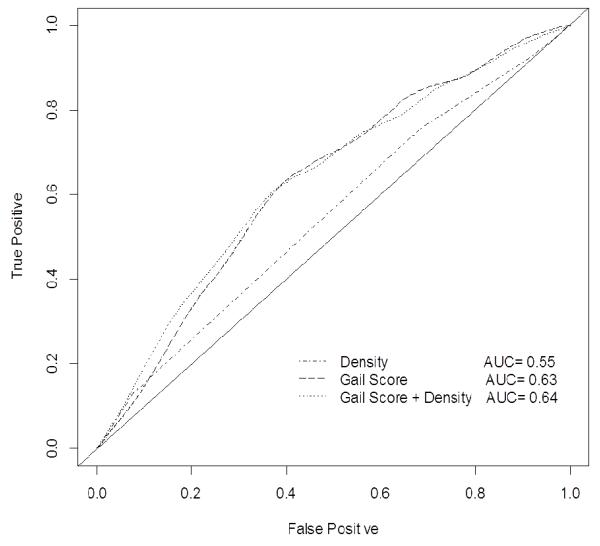
We assessed the discriminatory accuracy of the models through the use of time-dependent receiver operator characteristic (ROC) curves and the corresponding area under the curve (AUC) (25). ROC curves plot the true-positive rate (sensitivity) versus the false-positive rate (1-specificity) for all possible threshold values for the probability of an outcome at a specific time, t. The corresponding AUC(t) represents the probability that a person with onset of disease by time t has a higher risk score than a person with no event by time t. An ROC curve representing a non-predictive model would connect the coordinates (0,0) and (0,1) and have a corresponding AUC(t) of 0.50, indicating that the model predicts no better than chance. Conversely, an AUC(t) of 1.0 would indicate perfect discrimination between women who develop breast cancer by time t and those who do not. The c-statistic, which is a measure of the AUC, provides a global assessment of model performance over a given time frame. In addition to time-specific ROC curves and AUCs, modified overall c-statistics were calculated for each model as estimates of concordance measures that are free of censoring and to provide inference regarding the difference between the models (26). ROC analyses and the global c-statistics were computed using R (version 2.13.2) packages written specifically for time-dependent outcomes with censored data (25-27).
Results
The distributions of participant characteristics at entry by the derived BI-RADS levels of breast density are presented in Table 1. Women with high breast density were younger than those with less dense breasts. The mean age in the highest breast density category was 57.0 years compared to 59.5 years in the lowest density category. Women with more dense breasts had a higher five-year predicted breast cancer risk (Gail score), but had a lower BMI. The mean BMI decreased from 33.0 in the lowest breast density category to 25.7 in the highest breast density category. Women with dense breasts were also less likely to have a history of diabetes than those with less dense breasts.
Table 1.
Participant characteristics upon entry to the NSABP STAR trial for women included in the analyses
| Participant Characteristic | BI-RADS Breast Density |
P value | |||
|---|---|---|---|---|---|
|
Fatty No. (%) |
Scattered No. (%) |
Heterogeneously No. (%) |
Extremely No. (%) |
||
|
| |||||
| Age, y | |||||
| < 50 | 106 (9.9) | 263 (8.2) | 801 (9.9) | 123 (11.7) | <.001 |
| 50-59 | 439 (41.1) | 1,507 (47.2) | 4,194 (51.8) | 607 (57.9) | |
| ≥ 60 | 522 (48.9) | 1,421 (44.5) | 3,108 (38.4) | 318 (30.3) | |
| Treatment | |||||
| Tamoxifen | 534 (50.0) | 1,630 (51.1) | 4,001 (49.4) | 510 (48.7) | 0.36 |
| Raloxifene | 533 (50.0) | 1,561 (48.9) | 4,102 (50.6) | 538 (51.3) | |
| No. 1° relatives with BC | |||||
| 0 | 222 (20.8) | 827 (25.9) | 2,447 (30.2) | 379 (36.2) | <.001 |
| ≥ 1 | 845 (79.2) | 2,364 (74.1) | 5,656 (69.8) | 669 (63.8) | |
| No. previous breast biopsies | |||||
| 0 | 566 (53.0) | 1,315 (41.2) | 2,662 (32.9) | 244 (23.3) | <.001 |
| 1 | 284 (26.6) | 958 (30.0) | 2,547 (31.4) | 311 (29.7) | |
| > 1 | 203 (19.0) | 879 (27.5) | 2,811 (34.7) | 476 (45.4) | |
| Unknown | 14 (1.3) | 39 (1.2) | 83 (1.0) | 17 (1.6) | |
| 5-year predicted BC risk (%)a | |||||
| ≤ 2.00 | 153 (14.3) | 382 (12.0) | 891 (11.0) | 102 (9.7) | <.001 |
| 2.01-3.00 | 375 (35.1) | 992 (31.1) | 2,431 (30.0) | 277 (26.4) | |
| 3.01-5.00 | 298 (27.9) | 1,031 (32.3) | 2,546 (31.4) | 359 (34.3) | |
| ≥ 5.01 | 241 (22.6) | 786 (24.6) | 2,235 (27.6) | 310 (29.6) | |
| Body Mass Index (kg/m2)b | |||||
| < 25.0 | 109 (10.2) | 687 (21.5) | 2,784 (34.4) | 559 (53.4) | <.001 |
| 25.0–29.9 | 305 (28.6) | 1,087 (34.1) | 2,866 (35.4) | 303 (28.9) | |
| ≥ 30.0 | 653 (61.2) | 1,417 (44.4) | 2,453 (30.3) | 185 (17.7) | |
| History of diabetes | |||||
| No | 965 (90.4) | 2,972 (93.1) | 7,670 (94.7) | 1,014 (96.8) | <.001 |
| Yes | 102 (9.6) | 219 (6.9) | 433 (5.3) | 34 (3.2) | |
| History of smoking (years) | |||||
| None | 601 (56.3) | 1,740 (54.5) | 4,565 (56.3) | 596 (56.9) | 0.002 |
| < 15 | 103 (9.7) | 417 (13.1) | 1,060 (13.1) | 133 (12.7) | |
| 15-34 | 217 (20.3) | 680 (21.3) | 1,663 (20.5) | 226 (21.6) | |
| ≥ 35 | 138 (12.9) | 330 (10.3) | 759 (9.4) | 88 (8.4) | |
| Unknown | 8 (0.7) | 24 (0.8) | 56 (0.7) | 5 (0.5) | |
|
| |||||
| Total | 1,067 | 3,191 | 8,103 | 1,048 | |
Determined by the Gail model.
There was one participant for whom BMI was unknown.
Abbreviations: BI-RADS, The American College of Radiology Breast Imaging Reporting and Data System; BC, breast cancer.
A total of 349 cases of invasive breast were cancer diagnosed. Table 2 presents the distribution of cases by the derived BI-RADS categories of breast density and ER-status. The results of univariable and multivariable analyses are shown in Table 3. Baseline breast density was significantly associated with risk of invasive breast cancer. When assessed univariably (Model 1), the hazard ratio (HR) per increase of BI-RADS breast density category was 1.30 with a 95% confidence interval (CI) of 1.12 to 1.51 (P<0.001). Of all the possible explanatory variables assessed, only age, treatment, and years of smoking remained significant. The HR for breast density after adjustment for the significant explanatory variables (Table 3, Model 2) was 1.35 with a 95% CI of 1.16 to 1.58 (P<0.001). The interaction between breast density and treatment was not significant (P=0.33).
Table 2.
Distribution of invasive breast cancer cases by breast density category and ER-status: NSABP STAR
| BI-RADS Breast Density | Number at Risk |
Number of Cases |
|||
|---|---|---|---|---|---|
| ER-Negative N (%) |
ER-Positive N (%) |
ER-Unknown N (%) |
Total N (%) |
||
|
| |||||
| Almost entirely fatty | 1,067 | 5 (0.5) | 14 (1.3) | 0 (0) | 19 (1.8) |
| Scattered fibroglandular densities | 3,191 | 16 (0.5) | 47 (1.5) | 4 (0.1) | 67 (2.1) |
| Heterogeneously dense | 8,103 | 51 (0.6) | 169 (2.1) | 4 (<0.1) | 224 (2.8) |
| Extremely dense | 1,048 | 11 (1.0) | 25 (2.4) | 3 (0.3) | 39 (3.7) |
|
| |||||
| Total | 13,409 | 83 (0.6) | 255 (1.9) | 11 (0.1) | 349 (2.6) |
Abbreviations: BI-RADS, The American College of Radiology Breast Imaging Reporting and Data System; ER, estrogen receptor.
Table 3.
Breast density and incidence of invasive breast cancer: NSABP STAR
| Variable | Model 1 | Model 2 | Model 3 | Model 4 | ||||
|---|---|---|---|---|---|---|---|---|
| HRa (95% CI) | P | HRa (95% CI) | P | HRa (95% CI) | P | HRa (95% CI) | P | |
|
| ||||||||
| Breast density | 1.30 (1.12 – 1.51) | <.001 | 1.35(1.16 – 1.58) | <.001 | 1.29 (1.11 – 1.50) | <.001 | 1.33 (1.14 – 1.55) | <.001 |
| Gail Score | ------- | --- | ------- | --- | 1.13 (1.09 – 1.17) | <.001 | 1.11 (1.07 – 1.15) | <.001 |
| Age | ------- | --- | 1.04 (1.02 – 1.05) | <.001 | ------- | --- | 1.03 (1.01 – 1.04) | <.001 |
| Treatment | ------- | --- | 1.25 (1.01 – 1.55) | 0.04 | ------- | --- | 1.25 (1.01 – 1.55) | 0.04 |
| Cigarette Smokingb | ------- | --- | 1.11 (1.01 – 1.22) | <.001 | ------- | --- | 1.10 (1.00 – 1.21) | <.001 |
HR for breast density is per increase of BI-RADS density category; HR for Gail score is per 1 percent increment in Gail score; HR for age is per one year increase; reference group for treatment was tamoxifen; reference group for years of cigarette smoking (none, <15, 15-34, 35+ yrs) was none.
Those with unknown smoking status were excluded from analyses.
Abbreviations: HR, hazard ratio; CI, confidence interval; BI-RADS, The American College of Radiology Breast Imaging Reporting and Data System.
When breast density was added to a model with Gail score, both Gail score and breast density were significant (Table 3, Model 3). As the Gail score increased in increments of one percent, the HR was 1.13 (95% CI, 1.09-1.17; P<0.001). The HR for breast density was 1.29 (95% CI, 1.11-1.50; P<0.001) per increase of BI-RADS density category. Adjustment for the significant explanatory variables had negligible effects on the results for Gail score and breast density (Table 3, Model 4). The resulting HR for Gail score was 1.11 (P<0.001) and the HR for breast density was 1.33 (P<0.001). Figure 2 shows the time-specific ROC curves at year five for the models with breast density only, Gail score only, and Gail score and breast density. The AUC for the model with breast density only was 0.55, indicating low discriminatory accuracy not much better than chance. When considering the other two models, the AUC improved from 0.63 for the model with Gail score only to 0.64 when considering Gail score and breast density. The overall c-statistic throughout the first five years of follow-up was 0.627 for the model with Gail score only and 0.633 when breast density was added. The difference of 0.005 was not statistically significant (95% CI, −0.016-0.027).
Figure 2.
Estimated ROC curves and corresponding AUC at year 5 for models with BI-RADS breast density only, Gail score only, and Gail score and BI-RADS breast density: NSABP STAR.
There were 255 cases of ER-positive breast cancer. Based on Chlebowski’s abbreviated model, we ran a proportional hazards model for ER-positive invasive breast cancer with the variables of age, number of relatives, and number of breast biopsies (Table 4). Breast density significantly added to this abbreviated model (P=0.02). The HR for breast density was 1.24 with a 95% CI of 1.03 to 1.49. Among our data, the number of relatives was not significant in this model. We therefore ran a model excluding this variable, but the effects on breast density were negligible (HR, 1.24; 95% CI, 1.04-1.49; P=0.02). Breast density had very little effect on the discriminatory accuracy of the Chlebowski model, with a time-specific AUC at year five of 0.60 for both the original model and the Chlebowski model plus breast density (data not shown).
Table 4.
Breast density and Chlebowski’s abbreviated model for ER-positive invasive breast cancer: NSABP STAR
| Variables | HRa | 95% CI | P-value |
|---|---|---|---|
| Age | 1.03 | 1.02 – 1.05 | <.001 |
| No. 1° relatives with breast cancer | 0.82 | 0.62 – 1.08 | 0.17 |
| No. previous breast biopsiesb | 1.27 | 1.08 – 1.50 | 0.004 |
| Breast density | 1.24 | 1.03 – 1.49 | 0.02 |
HR for age is per one year increase; reference groups for number of relatives and breast biopsies were “0”; HR for breast density is per increase of BI-RADS density category.
Those with unknown biopsy data were excluded from analyses.
Abbreviations: HR, hazard ratio; CI, confidence interval; ER, estrogen receptor; BI-RADS, The American College of Radiology Breast Imaging Reporting and Data System.
Discussion
In this study of postmenopausal participants of a chemoprevention clinical trial with an increased risk for developing breast cancer, we found that the derived BI-RADS classification of breast density at entry was directly and significantly associated with the risk of invasive breast cancer. This association persisted when adjusting for important explanatory variables and when accounting for the calculated probability of developing breast cancer in the next five years based on the Gail model. Despite this significance, we found that the derived BI-RADS classification of breast density did not appear to predict breast cancer risk much better than chance, and considering breast density in conjunction with the Gail score only slightly improved model discrimination.
The Gail model has been validated and performs well in predicting the incidence of breast cancer in the population as a whole. However, its modest discrimination indicates that it is not as good at predicting whether any given individual will develop breast cancer and should not be considered as a tool of diagnostic screening. Thus the Gail model is limited to the extent to which it identifies a meaningfully frequent category of high risk women who might uniquely benefit from one of the preventive interventions currently available. Identifying new risk factors and improving risk prediction models remains a high priority in breast cancer prevention and risk reduction. Previous research has found promising results regarding the inclusion of breast density in risk prediction models. Using data from the Breast Cancer Detection Demonstration Project, Chen and colleagues (11) added a continuous measure of breast density to a model with weight, age of first live birth, number of affected relatives, and number of breast biopsies. They reported improved risk discrimination with this new model when compared to the Gail model, with increases in concordance ranging from 0.01 to 0.09 across the seven 5-year age groups that they studied. Three other studies (8, 12, 13) used data from more than one million women from seven mammography registries of the Breast Cancer Surveillance Consortium (BCSC). All three reported modest improvement in predictive accuracy after adding breast density to the models with increases in c-statistics ranging from 0.01 to 0.03. These studies were based on large samples of a general screening population of pre- and postmenopausal women and therefore have good generalizability. However, they did not include all factors of the Gail model in their assessments (i.e., information regarding history of atypical hyperplasia was not available), and breast cancer diagnoses were ascertained through linkage with cancer registries. Furthermore, the study by Barlow et al. (12) focused only on one-year risk for breast cancer and used cases of breast cancer diagnosed by the index mammogram, which could potentially overestimate risk.
Although breast density was significantly related to breast cancer risk, the HRs in our study were smaller than in previous studies. When comparing the highest breast density group to the lowest group, the HR was 2.46 compared to a three to five-fold increased risk of breast cancer previously reported (8-10). One reason for our findings may be that our population consists only of high-risk women. It could be that the relationship between breast density and breast cancer is not as strong for those already at an increased risk based on other risk factors. Also, our population received chemopreventive therapy for five years, which substantially reduced the risk of breast cancer and may also have affected breast density. Previous studies have reported a decrease in breast density over time with the use of tamoxifen (28-31). We did not have the ability to assess breast density over time because submitted copies of the mammogram reports were not required for all participants during follow-up. Nevertheless, underlying changes in breast density due to treatment could have changed individual risk over time in a way that we could not measure. The current study found only a slight increase in predictive accuracy when considering breast density in conjunction with the Gail score. The modest improvements, however, are not surprising. Although a two-fold increased risk with breast density is substantial, modeling has shown that risk factors with relative risks of at least 20 may be needed to show significant improvements in predictive accuracy (13, 32, 33).
The current study has some limitations. First, the only measure of breast density available was the derived BI-RADS category based on terminology included in mammogram reports by radiologists at each clinical site, and therefore was not standardized. The breast density categories may have been more accurate if we were able to collect the actual mammographic films and have an independent radiologist evaluate each film. Furthermore, computer aids that quantitatively calculate the percent of dense breast tissue in relation to the whole area of the breast or those that take the thickness of the breast into account to calculate volumetric breast density are believed to be more precise and reproducible methods for measuring breast density (10, 34, 35). However, these methods can be costly and perhaps not appropriate for widespread use. Another criticism may involve the relationship between breast density and BMI. Since BMI is positively related to total breast area, which is the denominator for percent breast density, women with high BMI are more likely to have a low percent breast density (36). Therefore, since a high BMI may increase breast cancer risk, it is believed that the effect of percent breast density on risk will tend to be underestimated when not adjusted for BMI (37). However, in our study, BMI was not associated with an increased risk for breast cancer, and furthermore, adjusting for BMI had negligible effects on our HR estimate for breast density. Another concern when studying breast density is the possibility of masking bias because prevalent cancers at the time of an initial mammogram could remain undetected in women with very dense breasts. However, earlier studies have shown that the bias effect is only small and short-lived (10, 34). Particularly, one study looked at the site of dense tissue compared to the site of subsequent breast cancer and found that density in the cancer region of the breast was not a significant risk factor, thereby providing suggestive evidence that masking bias is not responsible for the density/breast cancer relationship (38).
This study provides further evidence that mammographic breast density is significantly associated with invasive breast cancer by evaluating the relationship among high-risk postmenopausal participants in a clinical trial with clearly defined and accurately measured exposures and endpoints. Our derived BI-RADS breast density classification was significant when considered in conjunction with the Gail score, and it also added significantly to Chlebowski’s abbreviated model for predicting ER-positive breast cancer. However, it provided only slight improvement in discrimination for predicting the incidence of invasive breast cancer. The BI-RADS breast composition classification system is a quick and readily available method for assessing breast density for risk prediction evaluations, but it does not appear to provide a clinically useful improvement in the ability to predict breast cancer risk using the Gail model. Future studies should focus on more accurate techniques for measuring breast density that may provide greater magnitudes of model improvement that could justify the inclusion of breast density in existing breast cancer risk prediction models.
Acknowledgments
This study was supported by: Public Health Service grants (U10-CA-12027, U10-CA-69651, U10-CA-37377, and U10-CA-69974) from the National Cancer Institute, Department of Health and Human Services; Zeneca Pharmaceuticals, a business unit of ZENECA Inc.; and Eli Lilly and Company
Footnotes
The following authors report the following potential conflicts of interest:
Dr. Cauley: Commercial Research Grant: Horizon-Novartis; Consultant/Advisory Board: Novartis
Dr. Wickerham: Honoraria from Speakers’ Bureau: Eli Lilly & Co.
References
- 1.American Cancer Society . Global cancer facts & figures. 2nd edition American Cancer Society; Atlanta: 2011. [Google Scholar]
- 2. [Accessed: 2/7/12];Breast cancer risk assessment tool [Internet] 2008 [updated 5/16/2011]. Available at: http://www.cancer.gov/bcrisktool.
- 3.Gail MH, Brinton LA, Byar DP, Corle DK, Green SB, Schairer C, et al. Projecting individualized probabilities of developing breast cancer for white females who are being examined annually. J Natl Cancer Inst. 1989;81:1879–86. doi: 10.1093/jnci/81.24.1879. [DOI] [PubMed] [Google Scholar]
- 4.Costantino JP, Gail MH, Pee D, Anderson S, Redmond CK, Benichou J, et al. Validation studies for models projecting the risk of invasive and total breast cancer incidence. J Natl Cancer Inst. 1999;91:1541–8. doi: 10.1093/jnci/91.18.1541. [DOI] [PubMed] [Google Scholar]
- 5.Rockhill B, Spiegelman D, Byrne C, Hunter DJ, Colditz GA. Validation of the Gail et al. model of breast cancer risk prediction and implications for chemoprevention. J Natl Cancer Inst. 2001;93:358–66. doi: 10.1093/jnci/93.5.358. [DOI] [PubMed] [Google Scholar]
- 6.Gail MH, Costantino JP, Pee D, Bondy M, Newman L, Selvan M, et al. Projecting individualized absolute invasive breast cancer risk in African American women. J Natl Cancer Inst. 2007;99:1782–92. doi: 10.1093/jnci/djm223. [DOI] [PubMed] [Google Scholar]
- 7.Matsuno RK, Costantino JP, Ziegler RG, Anderson GL, Li H, Pee D, et al. Projecting individualized absolute invasive breast cancer risk in Asian and Pacific Islander American women. J Natl Cancer Inst. 2011;1032:951–61. doi: 10.1093/jnci/djr154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tice JA, Cummings SR, Smith-Bindman R, Ichikawa L, Barlow WE, Kerlikowske K. Using clinical factors and mammographic breast density to estimate breast cancer risk: Development and validation of a new predictive model. Ann Intern Med. 2008;148:337–47. doi: 10.7326/0003-4819-148-5-200803040-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kerlikowske K, Ichikawa L, Miglioretti DL, Buist DS, Vacek PM, Smith-Bindman R, et al. Longitudinal measurement of clinical mammographic breast density to improve estimation of breast cancer risk. J Natl Cancer Inst. 2007;99:386–95. doi: 10.1093/jnci/djk066. [DOI] [PubMed] [Google Scholar]
- 10.Boyd NF, Martin LJ, Bronskill M, Yaffe MJ, Duric N, Minkin S. Breast tissue composition and susceptibility to breast cancer. J Natl Cancer Inst. 2010;102:1224–37. doi: 10.1093/jnci/djq239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chen J, Pee D, Ayyagari R, Graubard B, Schairer C, Byrne C, et al. Projecting absolute invasive breast cancer risk in white women with a model that includes mammographic density. J Natl Cancer Inst. 2006;98:1215–26. doi: 10.1093/jnci/djj332. [DOI] [PubMed] [Google Scholar]
- 12.Barlow WE, White E, Ballard-Barbash R, Vacek PM, Titus-Ernstoff L, Carney PA, et al. Prospective breast cancer risk prediction model for women undergoing screening mammography. J Natl Cancer Inst. 2006;98:1204–14. doi: 10.1093/jnci/djj331. [DOI] [PubMed] [Google Scholar]
- 13.Tice JA, Cummings SR, Ziv E, Kerlikowske K. Mammographic breast density and the Gail model for breast cancer risk prediction in a screening population. Breast Cancer Res Treat. 2005;94:115–22. doi: 10.1007/s10549-005-5152-4. [DOI] [PubMed] [Google Scholar]
- 14.D’Orsi CJ, Bassett LW, Berg WA, et al. BI-RADS: Mammography. In: D’Orsi CJ, Mendelson EB, Ikeda DM, et al., editors. Breast Imaging Reporting and Data System: ACR BI-RADS - breast imaging atlas. 4th edition American College of Radiology; Reston, VA: 2003. [Google Scholar]
- 15.Nicholson BT, LoRusso AP, Smolkin M, Bovbjerg VE, Petroni GR, Harvey JA. Accuracy of assigned BI-RADS breast density category definitions. Acad Radiol. 2006;13:1143–9. doi: 10.1016/j.acra.2006.06.005. [DOI] [PubMed] [Google Scholar]
- 16.Boyd NF, Martin LJ, Yaffe MJ, Minkin S. Mammographic density and breast cancer risk: current understanding and future prospects. Breast Cancer Res. 2011;13:223. doi: 10.1186/bcr2942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Anderson BO. Prophylactic surgery to reduce breast cancer risk: a brief literature review. Breast J. 2001;7:321–30. doi: 10.1046/j.1524-4741.2001.21059.x. [DOI] [PubMed] [Google Scholar]
- 18.Fisher B, Costantino JP, Wickerham DL, Redmond CK, Kavanah M, Cronin WM, et al. Tamoxifen for prevention of breast cancer: report of the National Surgical Adjuvant Breast and Bowel Project P-1 study. J Natl Cancer Inst. 1998;90:1371–88. doi: 10.1093/jnci/90.18.1371. [DOI] [PubMed] [Google Scholar]
- 19.Vogel VG, Costantino JP, Wickerham DL, Cronin WM, Cecchini RS, Atkins JN, et al. Effects of tamoxifen vs raloxifene on the risk of developing invasive breast cancer and other disease outcomes: The NSABP Study of Tamoxifen and Raloxifene (STAR) P-2 trial. JAMA. 2006 Jun 21;295(23):2727–41. doi: 10.1001/jama.295.23.joc60074. [DOI] [PubMed] [Google Scholar]
- 20.Cummings SR, Tice JA, Bauer S, Browner WS, Cuzick J, Ziv E, et al. Prevention of breast cancer in postmenopausal women: Approaches to estimating and reducing risk. J Natl Cancer Inst. 2009;101:384–98. doi: 10.1093/jnci/djp018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chlebowski RT, Anderson GL, Lane DS, Aragaki AK, Rohan T, Yasmeen S, et al. Predicting risk of breast cancer in postmenopausal women by hormone receptor status. J Natl Cancer Inst. 2007;99:1695–705. doi: 10.1093/jnci/djm224. [DOI] [PubMed] [Google Scholar]
- 22.Gail MH, Anderson WF, Garcia-Closas M, Sherman ME. Absolute risk models for subtypes of breast cancer. J Natl Cancer Inst. 2007;99:1657–9. doi: 10.1093/jnci/djm228. [DOI] [PubMed] [Google Scholar]
- 23.Vogel VG, Costantino JP, Wickerham DL, Cronin WM, Cecchini RS, Atkins JN, et al. Update of the National Surgical Adjuvant Breast and Bowel Project Study of Tamoxifen and Raloxifene (STAR) P-2 trial: Preventing breast cancer. Cancer Prev Res (Phila) 2010;3:696–706. doi: 10.1158/1940-6207.CAPR-10-0076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Martin KE, Helvie MA, Zhou C, Roubidoux MA, Bailey JE, Paramagul C, et al. Mammographic density measured with quantitative computer-aided method: comparison with radiologists’ estimates and BI-RADS categories. Radiology. 2006;240:656–65. doi: 10.1148/radiol.2402041947. [DOI] [PubMed] [Google Scholar]
- 25.Heagerty PJ, Lumley T, Pepe MS. Time-dependent ROC curves for censored survival data and a diagnostic marker. Biometrics. 2000;56:337–44. doi: 10.1111/j.0006-341x.2000.00337.x. [DOI] [PubMed] [Google Scholar]
- 26.Uno H, Cai T, Pencina MJ, D’Agostino RB, Wei LJ. On the C-statistics for evaluating overall adequacy of risk prediction procedures with censored survival data. Stat Med. 2011;30:1105–17. doi: 10.1002/sim.4154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Heagerty PJ, Zheng Y. Survival model predictive accuracy and ROC curves. Biometrics. 2005;61:92–105. doi: 10.1111/j.0006-341X.2005.030814.x. [DOI] [PubMed] [Google Scholar]
- 28.Cuzick J, Warwick J, Pinney E, Warren RM, Duffy SW. Tamoxifen and breast density in women at increased risk of breast cancer. J Natl Cancer Inst. 2004;96:621–8. doi: 10.1093/jnci/djh106. [DOI] [PubMed] [Google Scholar]
- 29.Cuzick J, Warwick J, Pinney E, Duffy SW, Cawthorn S, Howell A, et al. Tamoxifen-induced reduction in mammographic density and breast cancer risk reduction: a nested case-control study. J Natl Cancer Inst. 2011;103:744–52. doi: 10.1093/jnci/djr079. [DOI] [PubMed] [Google Scholar]
- 30.Brisson J, Brisson B, Coté G, Maunsell E, Bérubé S, Robert J. Tamoxifen and mammographic breast densities. Cancer Epidemiol Biomarkers Prev. 2000;9:911–5. [PubMed] [Google Scholar]
- 31.Atkinson C, Warren R, Bingham SA, Day NE. Mammographic patterns as a predictive biomarker of breast cancer risk: effect of tamoxifen. Cancer Epidemiol Biomarkers Prev. 1999;8:863–6. [PubMed] [Google Scholar]
- 32.Pepe MS, Janes H, Longton G, Leisenring W, Newcomb P, Limitations of. the odds ratio in gauging the performance of a diagnostic, prognostic, or screening marker. Am J Epidemiol. 2004;159:882–90. doi: 10.1093/aje/kwh101. [DOI] [PubMed] [Google Scholar]
- 33.Wald NJ, Hackshaw AK, Frost CD. When can a risk factor be used as a worthwhile screening test? BMJ. 1999;319:1562–5. doi: 10.1136/bmj.319.7224.1562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Harvey JA, Bovbjerg VE. Quantitative assessment of mammographic breast density: Relationship with breast cancer risk. Radiology. 2004;230:29–41. doi: 10.1148/radiol.2301020870. [DOI] [PubMed] [Google Scholar]
- 35.Lokate M, Kallenberg MG, Karssemeijer N, Van den Bosch MA, Peeters PH, Van Gils CH. Volumetric breast density from full-field digital mammograms and its association with breast cancer risk factors: a comparison with a threshold method. Cancer Epidemiol Biomarkers Prev. 2010;19:3096–105. doi: 10.1158/1055-9965.EPI-10-0703. [DOI] [PubMed] [Google Scholar]
- 36.Stone J, Warren RM, Pinney E, Warwick J, Cuzick J. Determinants of percentage and area measures of mammographic density. Am J Epidemiol. 2009;170:1571–8. doi: 10.1093/aje/kwp313. [DOI] [PubMed] [Google Scholar]
- 37.Boyd NF, Martin LJ, Sun L, Guo H, Chiarelli A, Hislop G, et al. Body size, mammographic density, and breast cancer risk. Cancer Epidemiol Biomarkers Prev. 2006;15:2086–92. doi: 10.1158/1055-9965.EPI-06-0345. [DOI] [PubMed] [Google Scholar]
- 38.Vachon CM, Brandt KR, Ghosh K, Scott CG, Maloney SD, Carston MJ, et al. Mammographic breast density as a general marker of breast cancer risk. Cancer Epidemiol Biomarkers Prev. 2007;16:43–9. doi: 10.1158/1055-9965.EPI-06-0738. [DOI] [PubMed] [Google Scholar]