Abstract
Background
Although running is a popular leisure-time physical activity, little is known about the long-term effects of running on mortality. The dose-response relations between running, as well as the change in running behaviors over time and mortality remain uncertain.
Objectives
We examined the associations of running with all-cause and cardiovascular mortality risks in 55,137 adults, aged 18 to 100 years (mean age, 44).
Methods
Running was assessed on the medical history questionnaire by leisure-time activity.
Results
During a mean follow-up of 15 years, 3,413 all-cause and 1,217 cardiovascular deaths occurred. Approximately, 24% of adults participated in running in this population. Compared with non-runners, runners had 30% and 45% lower adjusted risks of all-cause and cardiovascular mortality, respectively, with a 3-year life expectancy benefit. In dose-response analyses, the mortality benefits in runners were similar across quintiles of running time, distance, frequency, amount, and speed, compared with non-runners. Weekly running even <51 minutes, <6 miles, 1-2 times, <506 metabolic equivalent-minutes, or <6 mph was sufficient to reduce risk of mortality, compared with not running. In the analyses of change in running behaviors and mortality, persistent runners had the most significant benefits with 29% and 50% lower risks of all-cause and cardiovascular mortality, respectively, compared with never-runners.
Conclusions
Running, even 5-10 minutes per day and slow speeds <6 mph, is associated with markedly reduced risks of death from all causes and cardiovascular disease. This study may motivate healthy but sedentary individuals to begin and continue running for substantial and attainable mortality benefits.
Keywords: running pattern, all-cause mortality, cardiovascular mortality, dose-response, epidemiology, physical exercise
Running is a popular and convenient leisure-time physical activity with a consistent growth, despite some public concerns about the possible harmful effects of running (1,2). It is well-established that physical activity has substantial health benefits. The World Health Organization and the U.S. government have recently released evidence-based Physical Activity Guidelines, recommending at least 150 minutes of moderate-intensity or 75 minutes of vigorous-intensity aerobic activity per week, or an equivalent combination of both (3,4). However, compared with the compelling evidence on moderate-intensity activity and health (5), it is unclear whether there are health benefits to vigorous-intensity activity, such as running, for <75 minutes per week.
This study sought to investigate whether leisure-time running is associated with all-cause and cardiovascular disease (CVD) mortality risks, whether there is a dose-response relation between running and mortality, and whether different patterns of change in running behaviors are associated with mortality.
Methods
Study Population
The Aerobics Center Longitudinal Study is a prospective, observational cohort study designed to examine the effects of physical activity and fitness on various health outcomes. Participants are self-referred or are referred by their employers or physicians for periodic preventive medical examinations at the Cooper Clinic in Dallas, Texas. This cohort is primarily non-Hispanic whites, college-educated, and from middle-to-upper socioeconomic strata (6). The current study participants were men and women aged 18 to 100 years (mean age, 44) at baseline who received at least 1 extensive medical examination between 1974 and 2002. Among 60,603 participants, we excluded 3,294 individuals reporting myocardial infarction (MI), stroke, or cancer at baseline, and 2,172 individuals with <1 year of mortality follow-up to minimize potential bias due to serious undetected underlying diseases on mortality. The final sample included 55,137 individuals (26% women) for analyses of all-cause mortality, and 52,941 individuals for analyses of CVD mortality, after excluding 2,196 individuals who died from causes other than CVD. The Cooper Institute Institutional Review Board reviewed and approved the study annually. All participants gave written informed consent for the examinations and follow-up study.
Assessment of Running
Running or jogging activity during the past 3 months was assessed at baseline by the physical activity questionnaire including 4 questions about duration, distance, frequency, and speed as part of the medical examination. To calculate total weekly running time, the average duration of running was multiplied by the frequency. To calculate total amount of running, the metabolic equivalent (MET) value for a given speed was multiplied by the weekly running time (7). Participants were classified into 6 groups: non-runners and 5 quintiles of weekly running time (minutes), distance (miles), frequency (times), amount (MET-minutes), and speed (mph) in runners. For complete analyses of running characteristics and mortality, we defined runners as those who reported all 4 detailed running questions, and non-runners as those who did not report any running question. We also examined the associations between change in running behaviors and mortality in a subgroup of 20,647 participants from the overall 60,603 sample who received at least 2 medical examinations between 1974 and 2002 and were free from MI, stroke, or cancer at both examinations. We defined 4 categories of change in running behaviors using the baseline and last follow-up examination: “remained non-runners” as non-runners at both examinations, “became non-runners” as runners only at the baseline examination, “became runners” as runners only at the last examination, and “remained runners” as runners at both examinations. Total amount of other physical activities except running (cycling, swimming, walking, basketball, racquet sports, aerobic dance, and other sports-related activities) was classified into 3 groups: 0, 1-499, and ≥500 MET-minutes per week based on the physical activity guidelines (5). To reduce confounding bias in the association between running and mortality, total amount of other physical activities except running was adjusted in all multivariable regression models. Our physical activity assessment has been described elsewhere (8), and formerly validated and shown to correlate to measured cardiorespiratory fitness and physiological variables (6,9).
Clinical Examination
Physicians conducted comprehensive examinations. Resting blood pressure was recorded using the standard auscultation method. Blood glucose and cholesterol were analyzed using automated bioassays after ≥12 hours of overnight fast. Body mass index (BMI) was calculated from measured weight and height (kg/m2). Cardiorespiratory fitness was assessed using a maximal treadmill exercise test (10). Standardized medical questionnaires were used to assess health behaviors (smoking, alcohol consumption, and leisure-time physical activity), physician-diagnosed medical conditions, and parental history of CVD.
Mortality Surveillance
Participants were followed for mortality from the baseline examination through the date of death for decedents or December 31, 2003, for survivors using the National Death Index. For the analysis of change in running behaviors and mortality, we followed for mortality from the last follow-up examination through the date of death or 2003. Death from CVD was defined by the ICD-9 codes 390-449.9 and ICD-10 Revision codes I00-I78.
Statistical Analysis
Multivariable Cox proportional hazard models were used to estimate hazard ratios (HRs) and 95% confidence intervals (CIs) of mortality across running categories. Population attributable fractions (PAFs) and survival differences for running and other mortality predictors determined by the baseline assessment were estimated, as described by Bruzzi et al. (11), and using the risk advancement period approach (12). We tested effect modification by sex on the associations between running and mortality using interaction terms in the regressions and by comparing risk estimates in the sex-stratified analyses. Based on no significant interactions observed, the pooled analyses were performed. The proportional hazard assumptions were satisfied by comparing the log-log survival plots. SAS software (SAS Institute, Inc., Cary, NC) was used for all analyses and 2-sided p values <0.05 were deemed significant.
Results
There were 3,413 all-cause deaths and 1,217 CVD deaths during the mean (interquartile range) follow-up of 14.7 (6.5-21.7) years and 14.6 (6.3-21.8) years, respectively. At baseline, runners were more likely to be men, younger, leaner, less smoking, less participation in other types of physical activities, and had lower prevalence of chronic diseases and higher cardiorespiratory fitness levels (Table 1).
Table 1.
Population Characteristics by Quintile of Weekly Running Time
| Characteristic | Quintile of Running Time (minutes/week) |
|||||
|---|---|---|---|---|---|---|
| Non-runners (0) | 1 (<51) | 2 (51-80) | 3 (81-119) | 4 (120-175) | 5 (≥176) | |
| Female | 29.1 | 12.4 | 15.5 | 14.4 | 15.9 | 17.9 |
| Age (yr) | 45 (11) | 40 (9) | 41 (9) | 42 (9) | 42 (9) | 43 (9) |
| Body mass index (kg/m2)* | 26.3 (4.7) | 25.2 (3.2) | 25.0 (3.2) | 24.8 (3.0) | 24.6 (3.1) | 23.9 (2.9) |
| <25.0 | 42.3 | 49.9 | 53.1 | 55.4 | 58.1 | 67.9 |
| 25.0-29.9 | 40.6 | 42.6 | 40.3 | 39.2 | 36.4 | 28.8 |
| ≥30.0 | 17.1 | 7.5 | 6.6 | 5.4 | 5.5 | 3.3 |
| Smoking status | ||||||
| Never | 53.9 | 58.1 | 54.8 | 54.1 | 55.5 | 54.5 |
| Former | 27.3 | 29.0 | 32.8 | 35.4 | 36.1 | 38.5 |
| Current | 18.8 | 12.9 | 12.4 | 10.5 | 8.4 | 7.0 |
| Heavy alcohol drinking† | 17.2 | 19.3 | 18.2 | 19.2 | 18.4 | 17.9 |
| Total amount of other physical activities except running (MET-minutes/week)‡ | ||||||
| 0 | 59.0 | 61.6 | 69.1 | 72.4 | 71.8 | 72.1 |
| 1-499 | 16.6 | 11.2 | 9.9 | 8.6 | 8.3 | 6.6 |
| ≥500 | 24.4 | 27.2 | 21.0 | 19.0 | 19.9 | 21.3 |
| Systolic blood pressure (mm Hg) | 120 (15) | 118 (13) | 119 (14) | 119 (14) | 120 (14) | 120 (14) |
| Diastolic blood pressure (mm Hg) | 81 (10) | 79 (9) | 79 (10) | 79 (9) | 79 (9) | 79 (9) |
| Hypertension§ | 31.6 | 22.1 | 22.9 | 24.0 | 24.2 | 23.9 |
| Fasting glucose (mg/dl) | 99.7 (19.1) | 97.1 (11.8) | 97.5 (13.0) | 97.3 (11.8) | 97.2 (11.6) | 97.0 (10.6) |
| Diabetesl | 6.2 | 3.4 | 3.3 | 2.8 | 3.0 | 2.9 |
| Total cholesterol (mg/dl) | 208.5 (40.8) | 200.3 (38.4) | 201.3 (38.9) | 201.7 (38.1) | 200.3 (38.4) | 199.2 (37.8) |
| Hypercholesterolemia¶ | 29.3 | 20.8 | 21.1 | 21.5 | 21.5 | 19.6 |
| Abnormal electrocardiogram# | 8.7 | 4.9 | 4.8 | 5.1 | 4.5 | 5.8 |
| Parental cardiovascular disease | 27.6 | 23.0 | 23.5 | 26.2 | 27.5 | 27.4 |
| Cardiorespiratory fitness (maximal METs)†† | 10.2 (2.2) | 12.5 (1.9) | 12.8 (2.0) | 13.2 (2.1) | 13.6 (2.2) | 14.6 (2.6) |
Data are mean (SD) or %.
Calculated as the weight in kilograms divided by the square of the height in meters.
Defined as alcohol drinks >14 and >7 per week for men and women, respectively.
Total physical activity levels from other leisure-time activities except running.
Defined as systolic or diastolic blood pressure ≥140/90 mmHg or history of physician diagnosis.
Defined as fasting glucose ≥126 mg/dl, current therapy with insulin, or history of physician diagnosis.
Defined as total cholesterol ≥240 mg/dl or history of physician diagnosis.
Defined as abnormal resting or exercise electrocardiogram including rhythm and conduction disturbances and ischemic ST-T wave abnormalities.
Estimated from the final treadmill speed and grade during the maximal exercise test in a subsample of 50,995 participants. MET denotes metabolic equivalent.
Compared with non-runners, runners had 30% and 45% lower risks of all-cause and cardiovascular mortality, respectively, after adjusting for potential confounders (Figure 1). These associations were consistent regardless of sex, age, BMI, health conditions, smoking status, and alcohol consumption. We estimated PAFs for running and other mortality predictors, such as smoking, overweight/obesity, and chronic diseases. Not running was almost as important as hypertension, accounting for 16% of all-cause and 25% of cardiovascular mortality (Table 2). Also, non-runners had 3 years lower life-expectancy compared with runners after adjusting for other mortality predictors.
Figure 1. Hazard Ratios of All-Cause and Cardiovascular Mortality by Subgroup.
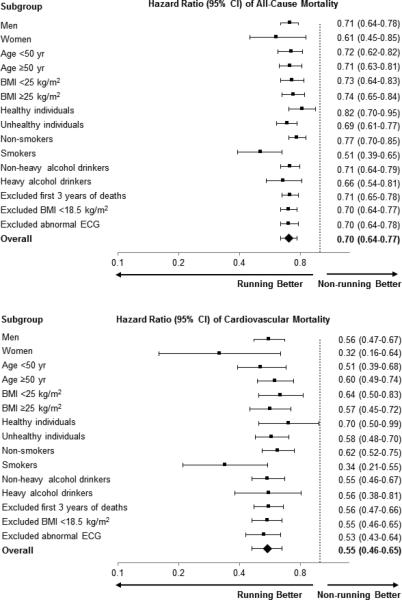
The reference group for all analyses includes non-runners. All hazard ratios were adjusted for baseline age (years), sex (not in sex-stratified analyses), examination year, smoking status (never, former, or current [not in smoking-stratified analyses]), alcohol consumption (heavy drinker or not [not in alcohol drinking-stratified analyses]), other physical activities except running (0, 1-499, or ≥500 MET-minutes per week), and parental cardiovascular disease (yes or no). Unhealthy was defined as the presence of one or more of the following health conditions: abnormal ECG, hypertension, diabetes, or hypercholesterolemia. Heavy alcohol drinking was defined as >14 and >7 drinks per week for men and women, respectively.
BMI=body mass index, CI=confidence interval, ECG=electrocardiogram.
Table 2.
Hazard Ratios, Population Attributable Fractions, and Estimated Decreased Life Expectancy by Running and Other Mortality Predictors
| All-Cause Mortality* | Cardiovascular Mortality* | |||||
|---|---|---|---|---|---|---|
| Mortality Predictor | HR (95% CI) | PAF (%)† | Decreased Life Expectancy (years)‡ | HR (95% CI) | PAF (%)† | Decreased Life Expectancy (years)‡ |
| Non-runner | 1.24 (1.13-1.37) | 16 | 3.0 | 1.40 (1.18-1.66) | 25 | 4.1 |
| Current smoker | 1.67 (1.54-1.80) | 11 | 7.0 | 1.69 (1.49-1.92) | 12 | 6.3 |
| Overweight or obesity | 1.16 (1.08-1.25) | 8 | 2.0 | 1.43 (1.26-1.63) | 20 | 4.4 |
| Parental CVD | 1.20 (1.12-1.29) | 7 | 2.5 | 1.38 (1.23-1.54) | 13 | 3.9 |
| Abnormal ECG | 1.55 (1.42-1.70) | 7 | 6.0 | 2.43 (2.14-2.77) | 17 | 10.7 |
| Hypertension | 1.46 (1.36-1.57) | 15 | 5.2 | 1.94 (1.72-2.18) | 28 | 8.0 |
| Diabetes | 1.36 (1.23-1.51) | 3 | 4.2 | 1.53 (1.31-1.79) | 6 | 5.1 |
| Hypercholesterolemia | 1.06 (0.98-1.13) | 2 | 0.7 | 1.32 (1.18-1.48) | 10 | 3.4 |
HR, PAF, and decreased life expectancy were adjusted for baseline age (years), sex, examination year, and all other mortality predictors in the table. The reference category for each HR and PAF analysis includes individuals who did not have the particular mortality predictor.
PAF was computed as Pc(1-1/HRadj), where Pc is the prevalence of the mortality predictor among mortality cases, and HRadj is the multivariable HR for mortality associated with the specified mortality predictor. Pc (ordered as listed in the table) was 83.7, 28.4, 59.6, 40.9, 19.0, 47.4, 12.6, and 33.9 for all-cause mortality and 86.7, 28.4, 66.7, 46.2, 29.2, 58.0, 16.6, and 41.6 for cardiovascular mortality.
Decreased life expectancy was compared β coefficients for mortality associated with each year of age with the β coefficients difference in mortality for each mortality predictor using the multivariable Cox proportional hazards model.
CI=confidence interval, HR=hazard ratios, PAF=population attributable fraction.
In the dose-response analyses (Table 3), runners across all 5 quintiles of weekly running time, even the lowest quintile of <51 minutes per week had lower risks of all-cause and CVD mortality compared with non-runners. However, these mortality benefits were similar between lower and higher doses of weekly running time. In fact, among runners (after excluding non-runners in the analyses), there were no significant differences in hazard ratios of all-cause and CVD mortality across quintiles of weekly running time (all p-values >0.10). In additional analyses using weekly running time of <60, 60-119, 120-179, and ≥180 minutes, we found similar trends with the corresponding HRs (95% CIs) of 0.73 (0.61-0.86), 0.65 (0.56-0.75), 0.71 (0.59-0.86), and 0.76 (0.63-0.92) for all-cause mortality, and 0.46 (0.33-0.65), 0.56 (0.43-0.73), 0.54 (0.38-0.77), and 0.65 (0.46-0.92) for CVD mortality, respectively, compared with non-runners after adjusting for confounders included in model 2. All analyses were adjusted for total physical activity levels achieved by other leisure-time activities besides running (Model 2). When we excluded individuals who reported participating in other activities besides running (39%), similar associations between weekly running time and mortality were found (all p-values <0.05). Furthermore, we adjusted for possible intermediate variables, such as BMI and medical conditions, on the causal pathway between running and mortality (Model 3). The associations were attenuated, but remained significant at the lower levels of running time. However, to avoid overadjustment for intermediate variables, we did not adjust for those intermediate variables in the models for other analyses.
Table 3.
Hazard Ratios of All-Cause and Cardiovascular Mortality by Quintiles of Weekly Running Time
| Quintile of Running Time (minutes/week) |
||||||
|---|---|---|---|---|---|---|
| Group | Non-runners (0) | 1 (<51) | 2 (51-80) | 3 (81-119) | 4 (120-175) | 5 (≥176) |
| All-Cause Mortality | ||||||
| No. of participants | 42,121 | 2,710 | 2,584 | 2,505 | 2,647 | 2,570 |
| No. of deaths | 2,857 | 110 | 116 | 103 | 112 | 115 |
| Person-years of follow-up | 602,752 | 41,653 | 42,197 | 41,082 | 40,473 | 40,426 |
| Death rate* | 45.9 | 31.7 | 29.7 | 29.8 | 31.5 | 33.8 |
| Adjusted HR (95% CI) | ||||||
| Model 1† | 1.00 | 0.69 (0.57-0.83) | 0.65 (0.54-0.78) | 0.65 (0.53-0.79) | 0.69 (0.57-0.83) | 0.74 (0.61-0.89) |
| Model 2‡ | 1.00 | 0.70 (0.58-0.85) | 0.67 (0.55-0.80) | 0.67 (0.55-0.82) | 0.71 (0.58-0.86) | 0.77 (0.63-0.92) |
| Model 3§ | 1.00 | 0.80 (0.66-0.97) | 0.76 (0.63-0.91) | 0.78 (0.64-0.95) | 0.84 (0.69-1.02) | 0.89 (0.74-1.07) |
| Cardiovascular Mortality | ||||||
| No. of participants | 40,319 | 2,628 | 2,501 | 2,435 | 2,567 | 2,491 |
| No. of deaths | 1,055 | 28 | 33 | 33 | 32 | 36 |
| Person-years of follow-up | 575,352 | 40,497 | 40,766 | 39,983 | 39,275 | 39,233 |
| Death rate* | 17.8 | 8.0 | 9.0 | 10.3 | 9.1 | 11.6 |
| Adjusted HR (95% CI) | ||||||
| Model 1† | 1.00 | 0.45 (0.31-0.66) | 0.50 (0.36-0.71) | 0.58 (0.41-0.82) | 0.51 (0.36-0.72) | 0.65 (0.46-0.91) |
| Model 2‡ | 1.00 | 0.45 (0.31-0.66) | 0.52 (0.37-0.73) | 0.60 (0.42-0.84) | 0.53 (0.37-0.75) | 0.67 (0.48-0.93) |
| Model 3§ | 1.00 | 0.59 (0.40-0.86) | 0.67 (0.47-0.95) | 0.82 (0.58-1.16) | 0.78 (0.54-1.11) | 0.86 (0.62-1.21) |
Death rate per 10,000 person-years adjusted for baseline age, sex, and examination year.
Model 1 was adjusted for baseline age (years), sex, and examination year.
Model 2 was adjusted for model 1 plus smoking status (never, former, or current), alcohol consumption (heavy drinker or not), other physical activities except running (0, 1-499, or ≥500 MET-minutes per week), and parental CVD (yes or no).
Model 3 was adjusted for Model 2 plus body mass index (kg/m2) and presence or absence of abnormal electrocardiogram, hypertension, diabetes, and hypercholesterolemia.
CI=confidence interval, CVD=cardiovascular disease, HR=hazard ratio.
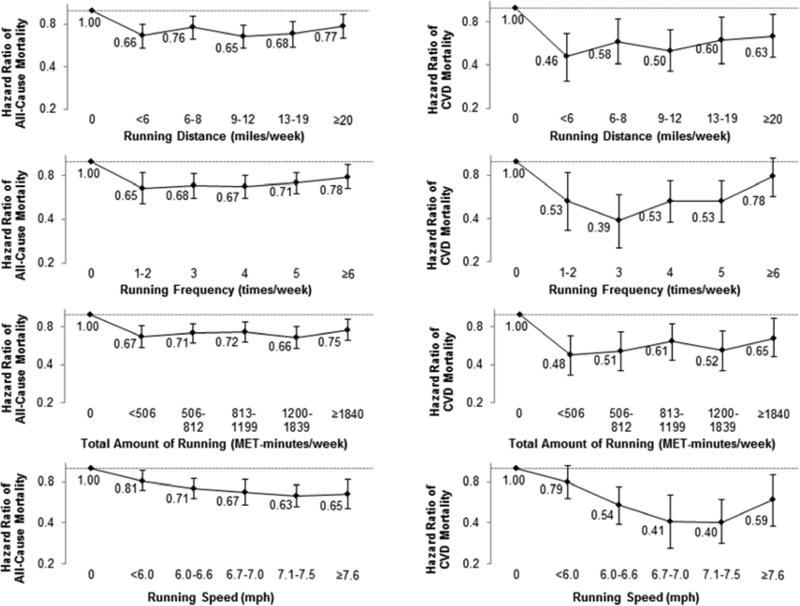
Runners across all quintiles of other running characteristics had lower risks of all-cause mortality compared with non-runners (Figure 2). Even the lowest quintiles of weekly running distance (<6 miles), frequency (1-2 times), amount (<506 MET-minutes), and speed (<6 mph) had significantly lower risks of all-cause mortality compared with not running. Similar trends were observed with the risk of CVD mortality.
Figure 2. Hazard Ratios of All-Cause and Cardiovascular Mortality by Running Distance, Frequency, Total Amount, and Speed.
Participants were classified into six groups: non-runners and five quintiles of each running distance, frequency, total amount, and speed. All hazard ratios were adjusted for baseline age (years), sex, examination year, smoking status (never, former, or current), alcohol consumption (heavy drinker or not), other physical activities except running (0, 1-499, or ≥500 MET-minutes per week), and parental cardiovascular disease (yes or no). The bars indicate 95% confidence intervals and hazard ratios are shown next to the bars.
CVD=cardiovascular disease, MET=metabolic equivalent.
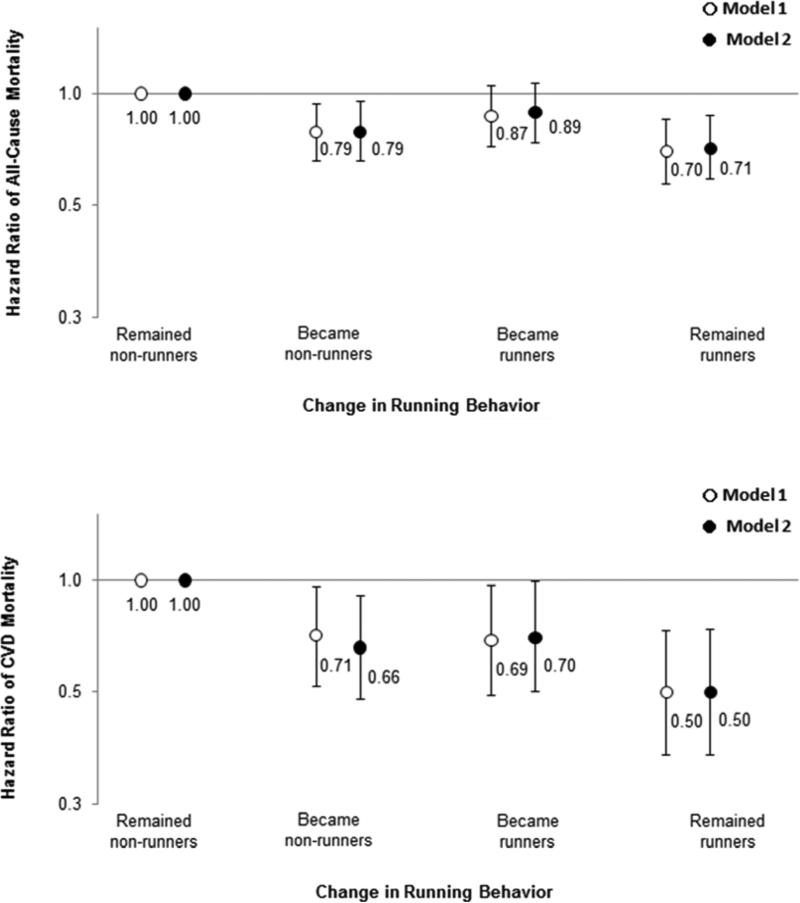
Among 20,647 individuals who received 2 medical examinations over a mean (interquartile range) interval of 5.9 years (1.5-8.5), 65% participants remained non-runners, 14% stopped running, 8% started running, and 13% continued running, indicating that the more consistent group is the inactive non-runners. Compared with never-runners (non-runners at both examinations), runners at one or both examinations were more likely to have lower mortality risks (Figure 3). Persistent runners over an average of 5.9 years, however, indicated the most significant mortality benefit, with 29% and 50% lower risks of all-cause and CVD mortality, respectively.
Figure 3. Hazard Ratios of All-Cause and Cardiovascular Mortality by Change in Running Behaviors.
Model 1 was adjusted for baseline age (years), sex, examination year, and interval between the baseline and last examinations (years). Model 2 was adjusted for Model 1 plus baseline smoking status (never, former, or current), alcohol consumption (heavy drinker or not), other physical activities except running (0, 1-499, or ≥500 MET-minutes per week), and parental CVD (yes or no). The number of participants (deaths) in remained non-runners, became non-runners, became runners, and remained runners were 13,522 (1,013), 2,847 (141), 1,578 (131), and 2,700 (113) for all-cause mortality, and 12,885 (376), 2,753 (47), 1,485 (38), and 2,616 (29) for cardiovascular mortality, respectively. The bars indicate 95% confidence intervals and hazard ratios are shown next to the bars.
CVD=cardiovascular disease.
Discussion
There were 3 major findings from this study (Central Illustration). First, runners had consistently lower risks of all-cause and CVD mortality compared with non-runners. Second, running even at lower doses or slower speeds was associated with significant mortality benefits. Third, persistent running over time was more strongly associated with mortality reduction.
An earlier study found a 39% lower risk of all-cause mortality in 538 runners who were ≥50 years from the Runners Association database compared with 423 matched non-runners from the Lipid Research Clinics database after adjusting for baseline age, sex, and functional ability (13). In our subsample of runners aged ≥50, we found 29% lower mortality risk, compared with non-runners. The somewhat greater mortality benefits of running in the earlier study may be because runners from a running club were more likely to be health conscious, and physical activities other than running were not adjusted for in the analyses.
Recently, the Copenhagen City Heart Study found similar mortality benefits in 1,878 joggers, compared with non-joggers after adjusting for a similar set of confounders used in our analyses (14). In their dose-response analysis, they observed a U-shaped relation between jogging time and mortality. Compared with no jogging, weekly jogging <150 minutes was associated with mortality reduction, however, ≥150 minutes of weekly jogging did not show significant mortality benefits, due to the small numbers of deaths and wide confidence intervals in that category. In our current study of more than 13,000 runners, we used quintiles of weekly running time to have an equal number of participants across different doses of running. We found a lower mortality risk in running more than 150 minutes per week. However, mortality benefits were slightly smaller at the highest quintile of weekly running time of ≥176 minutes per week. Several studies have suggested slightly lower or no mortality benefits at higher doses of vigorous-intensity activities. The Harvard Alumni study reported a slightly higher death rate in vigorous sports participation ≥180 minutes compared with <180 minutes per week (15). A large study of 416,175 adults found no additional mortality benefits >50 minutes per day of vigorous-intensity activities (16). Recent studies propose that excessive endurance sports may potentially induce adverse cardiovascular effects, such as arrhythmias and myocardial damage (17-20). In contrast, there are studies showing a linear dose-response relation between running and CVD risk with more benefits at higher doses of running (2,21). Thus, future studies are needed on this dose-response issue about whether there is an optimum upper-limit of vigorous-intensity activities, beyond which additional activity provides no further mortality benefits.
Another short report from the Copenhagen City Heart Study suggested a reduced mortality risk in 96 persistent male joggers (22). Our study now suggests that even less persistent runners (runners at 1 of the 2 examinations over 5.9 years of interval) appeared to have some mortality benefits compared with never-runners. However, persistent runners had the most mortality benefit.
Current physical activity guidelines recommend a minimum of 75 minutes per week of vigorous-intensity aerobic activity such as running for health benefits (3,4). However, we found mortality benefits even <75 minutes per week of running. In additional analyses, we found that a minimum of 30-59 minutes per week of running (5-10 minutes per day) was associated with lower risks of all-cause (HR, 0.72; 95% CI, 0.59-0.88) and CVD mortality (HR, 0.42; 95% CI, 0.28-0.63), compared with no running. Several large studies have also suggested mortality benefits <75 minutes per week of vigorous-intensity aerobic activities (15,21,23, 24). This finding has clinical and public health importance. Since time is one of the strongest barriers to participate in physical activity, this study may motivate more people to start running and continue to run as an attainable health goal for mortality benefits. Compared with moderate-intensity activity, vigorous-intensity activity, such as running, may be a better option for time efficiency, producing similar, if not greater, mortality benefits in 5-10 minutes per day in many healthy but sedentary individuals who may find 15-20 minutes per day of moderate-intensity activity too time consuming. However, for the majority of the population who are inactive and may not want to participate in running as a daily routine, a progressive transitional phase (for example, starting with walking) may be useful to reduce injury risk. In the context of population-mortality burden, we found that if all non-runners became runners in this population, 16% of all-cause deaths and 25% of CVD deaths would be prevented, based on the estimation of PAFs. Since several studies reported acute MI or sudden cardiac death during running races, we examined the long-term effects of running on coronary heart disease mortality and sudden cardiac death. Compared with non-runners, runners had 45% lower risk of coronary heart disease mortality (HR, 0.55; 95% CI, 0.44-0.69), after adjusting for potential confounders. In addition, the sudden cardiac death rate was approximately half in runners compared with non-runners (1.5 vs 0.7 per 10,000 person-years). Furthermore, runners also had 40% lower risk of stroke mortality (HR, 0.60; 95% CI, 0.39-0.92), compared with non-runners after adjusting for confounders.
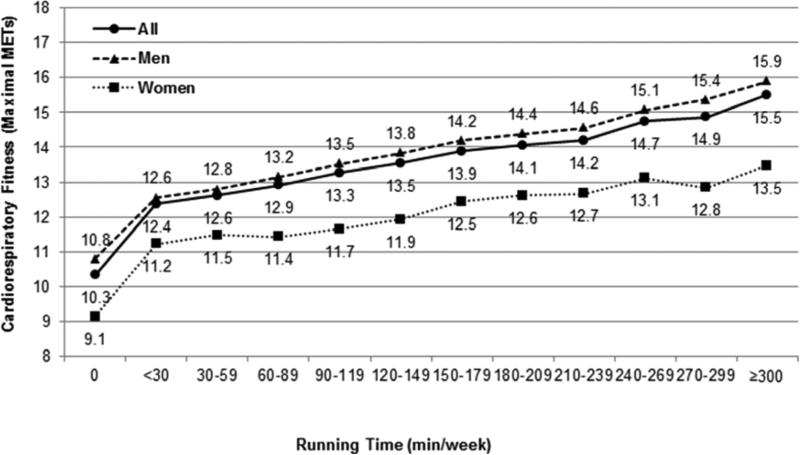
Several randomized controlled trials reported that vigorous-intensity aerobic activities improved blood pressure, insulin sensitivity, and blood lipid profile (25-27). There is also convincing observational evidence of the benefits of running in preventing chronic diseases including coronary heart disease, stroke, hypertension, diabetes, and hypercholesterolemia (2,21,28). Cardiorespiratory fitness is a strong morbidity and mortality predictor (10,29,30), as a possible link between running and mortality (13). We found that runners had approximately 30% higher cardiorespiratory fitness than non-runners, and there was a linear increase of cardiorespiratory fitness with increasing running time (p-value <0.001) at baseline (Figure 4). Every 30 minutes of additional weekly running time was associated with 0.5 METs higher cardiorespiratory fitness after accounting for age and sex (p-value <0.001). We found no mortality benefits of running after further adjustment for cardiorespiratory fitness, as we have previously observed in total leisure-time physical activity and mortality (8). Therefore, it is possible that the mortality benefits of running may be explained by improved cardiorespiratory fitness. However, running is a behavior and cardiorespiratory fitness is a physiologic attribute, which also is affected by other factors such as genotype. Thus, the current findings of no additional mortality benefits at the higher doses of running compared with lower doses of running may be related to other factors besides cardiorespiratory fitness.
Figure 4. Baseline Cardiorespiratory Fitness by Weekly Running Time.
Cardiorespiratory fitness was estimated from the final treadmill speed and grade during the maximal exercise test in a subsample of 50,995 participants. All p-values for linear trend across weekly running time were <0.001 after adjusting for age and sex (not in sex-stratified analyses). MET=metabolic equivalent.
Strengths of this study include the very large sample size across a wide age-range, extensive mortality follow-up, and comprehensive analyses and control of potential confounding factors including other non-running activities. In addition, we used various running characteristics to investigate the associations of both baseline and change in running with mortality.
Limitations
There are, however, several potential limitations. Our cohort consisted primarily of well-educated whites from middle-to-upper socioeconomic strata, which may limit the generalizability of the findings. However, the potential for confounding by race/ethnicity, education, and income may be reduced in this population. Physiological characteristics of our cohort are similar to other representative population samples (6). Another limitation is the use of self-reported running during the past 3 months, which is longer than conventional physical activity questionnaires, which include the previous 1 week or 1 month. Although running during the past 3 months could be more representative than running during the previous week or month, it may also increase the inaccuracy of self-report of running due to recall bias. People tend to over-report their leisure-time physical activities, because it is a socially desirable behavior (31). However, this over-reporting bias would likely induce an underestimation of the true mortality benefits of running toward the null hypothesis. Runners are healthier than non-runners in this population with lower prevalence of chronic diseases at baseline (Table 1). It is possible that healthy people may run more, which could lead to reverse causality. However, we found consistent mortality benefits in runners in both healthy and unhealthy individuals (Figure 1). Also, we observed mortality benefits after additional adjustment for medical conditions (Table 3). Another potential limitation is the lack of adequate dietary information.
Conclusions
We found consistent long-term mortality benefits of leisure-time running. This study underlines that running even at relatively low doses (5-10 minutes per day), below the current minimum guidelines of vigorous-intensity aerobic activity, is sufficient for substantial mortality benefits.
Perspectives.
COMPETENCY IN MEDICAL KNOWLEDGE 1: Leisure-time running, even at low intensity or pace, reduces all-cause and cardiovascular mortality independent of sex, age, body mass index, health behavior, and medical conditions. Reduction in mortality is related to continued running activity over time, and running is as important as such other prognostic variables as smoking, obesity or hypertension.
COMPETENCY IN INTERPERSONAL & COMMUNICATION SKILLS: Health care providers should explain to patients the significant mortality benefits of running even as little as 5-10 minutes daily. Try to motivate patients to start running and to continue running as an attainable health goal.
TRANSLATIONAL OUTLOOK 1: Further research is needed to determine whether there is an upper limit to the amount of vigorous physical activity, beyond which additional exercise provides no further mortality reduction.
Figure. Central Illustration: Leisure-Time Running Reduces All-Cause and Cardiovascular Mortality Risk.
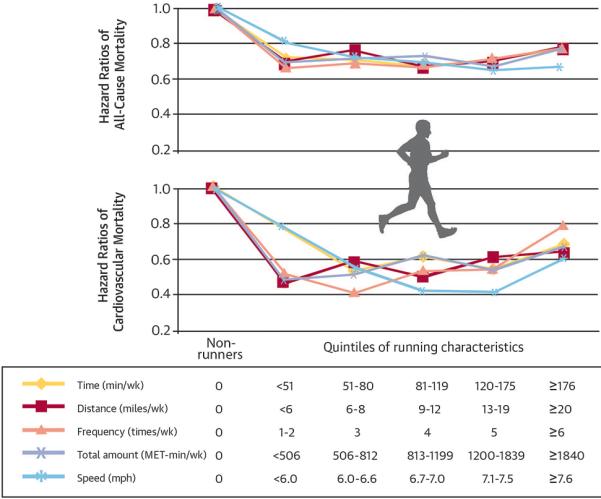
Legend: Hazard ratios of all-cause and cardiovascular mortality by running characteristics (weekly running time, distance, frequency, total amount, and speed). Participants were classified into six groups: non-runners (reference group) and five quintiles of each running characteristic. All hazard ratios were adjusted for baseline age (years), sex, examination year, smoking status (never, former, or current), alcohol consumption (heavy drinker or not), other physical activities except running (0, 1-499, or ≥500 MET-minutes/week), and parental history of cardiovascular disease (yes or no). All p values for hazard ratios across running characteristics were <0.05 for all-cause and cardiovascular mortality except for running frequency of ≥6 times/week (p=0.11) and speed of <6.0 mph (p=0.10) for cardiovascular mortality. MET=metabolic equivalent.
Acknowledgments
We thank the Cooper Clinic physicians and technicians for collecting the baseline data and staff at the Cooper Institute for data entry and data management.
This study was supported by the National Institutes of Health grants (AG06945, HL62508, and DK088195), and an unrestricted research grant from The Coca-Cola Company.
Abbreviations and Acronyms
- BMI
body mass index
- CI
confidence interval
- CVD
cardiovascular disease
- ECG
electrocardiogram
- HR
hazard ratio
- MET
metabolic equivalent
- PAF
population attributable fraction
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors have reported that they have no relationships to disclose.
References
- 1.Lamppa R. 2011 Marathon, half-marathon and state of the sport reports. 2011 http://www.runningusa.org/statistics. Accessed December 1, 2013.
- 2.Williams PT. Reductions in incident coronary heart disease risk above guideline physical activity levels in men. Atherosclerosis. 2010;209:524–7. doi: 10.1016/j.atherosclerosis.2009.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization Global Recommendations on Physical Activity for Health. 2010 http://www.who.int/dietphysicalactivity/factsheet_recommendations/en/index.html. Accessed December 1, 2013. [PubMed]
- 4.US Department of Health and Human Services 2008 Physical Activity Guidelines for Americans. 2008 http://health.gov/PAGuidelines. Accessed December 1, 2013.
- 5.Physical Activity Guidelines Advisory Committee Physical Activity Guidelines Advisory Committee Report. 2008 http://health.gov/PAGuidelines. Accessed December 1, 2013.
- 6.Blair SN, Kannel WB, Kohl HW, et al. Surrogate measures of physical activity and physical fitness. Evidence for sedentary traits of resting tachycardia, obesity, and low vital capacity. Am J Epidemiol. 1989;129:1145–56. doi: 10.1093/oxfordjournals.aje.a115236. [DOI] [PubMed] [Google Scholar]
- 7.Ainsworth BE, Haskell WL, Herrmann SD, et al. 2011 Compendium of Physical Activities: a second update of codes and MET values. Med Sci Sports Exerc. 2011;43:1575–81. doi: 10.1249/MSS.0b013e31821ece12. [DOI] [PubMed] [Google Scholar]
- 8.Lee DC, Sui X, Ortega FB, et al. Comparisons of leisure-time physical activity and cardiorespiratory fitness as predictors of all-cause mortality in men and women. Br J Sports Med. 2011;45:504–10. doi: 10.1136/bjsm.2009.066209. [DOI] [PubMed] [Google Scholar]
- 9.Stofan JR, DiPietro L, Davis D, et al. Physical activity patterns associated with cardiorespiratory fitness and reduced mortality: the Aerobics Center Longitudinal Study. Am J Public Health. 1998;88:1807–13. doi: 10.2105/ajph.88.12.1807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee DC, Sui X, Artero EG, et al. Long-term effects of changes in cardiorespiratory fitness and body mass index on all-cause and cardiovascular disease mortality in men: the Aerobics Center Longitudinal Study. Circulation. 2011;124:2483–90. doi: 10.1161/CIRCULATIONAHA.111.038422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bruzzi P, Green SB, Byar DP, et al. Estimating the population attributable risk for multiple risk factors using case-control data. Am J Epidemiol. 1985;122:904–14. doi: 10.1093/oxfordjournals.aje.a114174. [DOI] [PubMed] [Google Scholar]
- 12.Brenner H, Gefeller O, Greenland S. Risk and rate advancement periods as measures of exposure impact on the occurrence of chronic diseases. Epidemiology. 1993;4:229–36. doi: 10.1097/00001648-199305000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Chakravarty EF, Hubert HB, Lingala VB, et al. Reduced disability and mortality among aging runners: a 21-year longitudinal study. Arch Intern Med. 2008;168:1638–46. doi: 10.1001/archinte.168.15.1638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schnohr P, Marott JL, Lange P, et al. Longevity in male and female joggers: the Copenhagen City Heart Study. Am J Epidemiol. 2013;177:683–9. doi: 10.1093/aje/kws301. [DOI] [PubMed] [Google Scholar]
- 15.Paffenbarger RS, Jr., Hyde RT, Wing AL, et al. Physical activity, all-cause mortality, and longevity of college alumni. N Engl J Med. 1986;314:605–13. doi: 10.1056/NEJM198603063141003. [DOI] [PubMed] [Google Scholar]
- 16.Wen CP, Wai JP, Tsai MK, et al. Minimum amount of physical activity for reduced mortality and extended life expectancy: a prospective cohort study. Lancet. 2011;378:1244–53. doi: 10.1016/S0140-6736(11)60749-6. [DOI] [PubMed] [Google Scholar]
- 17.Andersen K, Farahmand B, Ahlbom A, et al. Risk of arrhythmias in 52 755 long-distance cross-country skiers: a cohort study. Eur Heart J. 2013;34(47):3624–31. doi: 10.1093/eurheartj/eht188. [DOI] [PubMed] [Google Scholar]
- 18.Claessen G, Colyn E, La GA, et al. Long-term endurance sport is a risk factor for development of lone atrial flutter. Heart. 2011;97:918–22. doi: 10.1136/hrt.2010.216150. [DOI] [PubMed] [Google Scholar]
- 19.Neilan TG, Januzzi JL, Lee-Lewandrowski E, et al. Myocardial injury and ventricular dysfunction related to training levels among nonelite participants in the Boston marathon. Circulation. 2006;114:2325–33. doi: 10.1161/CIRCULATIONAHA.106.647461. [DOI] [PubMed] [Google Scholar]
- 20.O'Keefe JH, Patil HR, Lavie CJ, et al. Potential adverse cardiovascular effects from excessive endurance exercise. Mayo Clin Proc. 2012;87:587–95. doi: 10.1016/j.mayocp.2012.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chomistek AK, Cook NR, Flint AJ, et al. Vigorous-intensity leisure-time physical activity and risk of major chronic disease in men. Med Sci Sports Exerc. 2012;44:1898–905. doi: 10.1249/MSS.0b013e31825a68f3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schnohr P, Parner J, Lange P. Mortality in joggers: population based study of 4,658 men. BMJ. 2000;321:602–3. doi: 10.1136/bmj.321.7261.602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Leitzmann MF, Park Y, Blair A, et al. Physical activity recommendations and decreased risk of mortality. Arch Intern Med. 2007;167:2453–60. doi: 10.1001/archinte.167.22.2453. [DOI] [PubMed] [Google Scholar]
- 24.Yu S, Yarnell JW, Sweetnam PM, et al. What level of physical activity protects against premature cardiovascular death? The Caerphilly study. Heart. 2003;89:502–6. doi: 10.1136/heart.89.5.502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Houmard JA, Tanner CJ, Slentz CA, Duscha BD, McCartney JS, Kraus WE. Effect of the volume and intensity of exercise training on insulin sensitivity. J Appl Physiol. 2004;96:101–6. doi: 10.1152/japplphysiol.00707.2003. [DOI] [PubMed] [Google Scholar]
- 26.Kraus WE, Houmard JA, Duscha BD, et al. Effects of the amount and intensity of exercise on plasma lipoproteins. N Engl J Med. 2002;347:1483–92. doi: 10.1056/NEJMoa020194. [DOI] [PubMed] [Google Scholar]
- 27.Whelton SP, Chin A, Xin X, et al. Effect of aerobic exercise on blood pressure: a meta-analysis of randomized, controlled trials. Ann Intern Med. 2002;136:493–503. doi: 10.7326/0003-4819-136-7-200204020-00006. [DOI] [PubMed] [Google Scholar]
- 28.Williams PT. Vigorous exercise, fitness and incident hypertension, high cholesterol, and diabetes. Med Sci Sports Exerc. 2008;40:998–1006. doi: 10.1249/MSS.0b013e31816722a9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kodama S, Saito K, Tanaka S, et al. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: a meta-analysis. JAMA. 2009;301:2024–35. doi: 10.1001/jama.2009.681. [DOI] [PubMed] [Google Scholar]
- 30.Lee DC, Sui X, Church TS, et al. Changes in fitness and fatness on the development of cardiovascular disease risk factors hypertension, metabolic syndrome, and hypercholesterolemia. J Am Coll Cardiol. 2012;59:665–72. doi: 10.1016/j.jacc.2011.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Adams SA, Matthews CE, Ebbeling CB, et al. The effect of social desirability and social approval on self-reports of physical activity. Am J Epidemiol. 2005;161:389–98. doi: 10.1093/aje/kwi054. [DOI] [PMC free article] [PubMed] [Google Scholar]