Abstract
Sedentary behavior is emerging as an independent risk factor for pediatric obesity. Some evidence suggests that limiting sedentary behavior alone could be effective in reducing body mass index (BMI) in children. However, whether adding physical activity and diet-focused components to sedentary behavior reduction interventions could lead to an additive effect is unclear. This meta-analysis aims to assess the overall effect size of sedentary behavior interventions on BMI reduction, and to compare whether interventions that have multiple components (sedentary behavior, physical activity, and diet) have a higher mean effect size than interventions with single (sedentary behavior) component. Included studies (N=25) were randomized controlled trails of children (<18 years) with intervention components aimed to reduce sedentary behavior and measured BMI at pre- and post-intervention. Effect size was calculated as the mean difference in BMI change between children in an intervention and a control group. Results indicated that sedentary behavior interventions had a significant effect on BMI reduction. The pooled effect sizes of multi-components interventions (g=−.060~−.089) did not differ from the single-component interventions (g=−.154), and neither of them had a significant effect size on its own. Future pediatric obesity interventions may consider focusing on developing strategies to decrease multiple screen-related sedentary behaviors.
Keywords: Sedentary behavior, Children, Body mass index, Obesity
Introduction
Overweight and obesity in childhood are known to have detrimental effects on both physical and psychosocial health. Problems in cardiovascular (e.g., hypercholesterolemia, hypertension) and endocrine functioning (e.g., hyperinsulinism, impaired glucose tolerance, type 2 diabetes mellitus) as well as and mental health concerns (e.g., depression, low self-esteem) are common in obese children and adolescents.1 These comorbidities will likely persist into adulthood.2 Moreover, obesity in childhood is known to be an independent risk factor for adult obesity. Being obese in childhood is also believed to be an important early risk factor for adult morbidity and mortality.3,4 Unfortunately, successful treatments for obesity have been elusive. In addition, only about 10% of obese children seek weight loss treatment.5 Therefore, much effort has been devoted to developing obesity prevention programs, in the hope that this strategy will be more effective to solve obesity as a public health problem. In fact, prevention in children is viewed as the best approach to reverse the rising global prevalence of obesity.6
Interactions between genetic, biological, psychological, sociocultural, and environmental factors are evident in childhood obesity.1,7 The rapid increase of overweight and obese children during the past two decades suggests that environmental factors may play a greater role than genetic factors.8 The increasing prevalence of obesity is believed to be a result of an increase in the energy content of dietary intake, decrease in level of physical activity, and increase in sedentary behavior.9–11 Behavioral methods have been the predominant approach to preventing obesity and often involve dietary modification and efforts to promote physical activity.12 However, some researchers argue that reducing sedentary behavior alone should lead to a reduction in obesity.6 A study by Epstein and collegues13 found that a consistent reduction of daily sedentary time may be as or more important than short periods of vigorous activity for maintaining a long-term energy balance. A recent systematic review on 232 studies done by Tremblay and colleagues14 revealed a dose-response relation between increased sedentary behavior and negative physical and psychosocial health outcomes. Specifically, more than 2 hours per day of sedentary behavior (assessed primarily as TV viewing) was associated with unfavorable body composition, decreased fitness, lowered self-esteem and decreased academic achievement in children aged 5–17 years. Another systematic review of prospective studies also suggests a moderate evidence (i.e., consisting findings across multiple high- and low-quality studies) for a longitudinal inverse relationship between sedentary time and aerobic fitness during childhood.15
In the past years, it was generally believed that the links between sedentary behavior and childhood obesity include displacement of physical activity, increased energy intake due to unhealthy food choices during TV watching, effects of food advertising, and decreased metabolic rate while watching TV.16–18 However, it is now recognized that one’s level of sedentary behavior may be relatively independent of physical activity level. A cross-national study showed that spending more than 2 hours daily in screen-based sedentary behaviors was not consistently associated with lower level of physical activity among children.19 Findings from a study by Wong and Leatherdale20 also support the notion that being highly sedentary is not equivalent to a lack of physical activity among children. These results suggest that there is time for both sedentary and active behaviors through the day for children, and sedentary activity is not simply the lack of physical activity. Moreover, elevated likelihood of being overweight or obese was found in those who were sufficiently active but who had high levels of sedentary behaviors.21 Therefore, sedentary behavior is emerging as an important risk factor for obesity independent of physical activity.22
In recent years, there has been increased interest in understanding the effectiveness of obesity interventions aiming to reduce sedentary time among children. A number of narrative reviews conducted in the past few years concluded that interventions with an emphasis on decreasing sedentary behavior have resulted in positive health behavior change (i.e., decreased sedentary time) and were associated with improvement of weight parameters.23–25 More recently, several meta-analytic reviews have also been conducted to evaluate the effectiveness of sedentary behavior interventions among children in a more systematic way.26–29 These studies all found a small but statistically significant effect size for a reduction in sedentary time among the intervention groups, although Wahi et al., found such effect existed only among preschool children. Only two of these meta-analytic reviews 28,29 examined the intervention effects on children’s weight parameters (i.e., body mass index [BMI]), which is a more direct indicator of intervention success in terms of obesity prevention. van Grieken et al., found a significant difference in mean BMI change at post-intervention in favor of the intervention groups among the 14 studies reviewed. However, this meta-analysis excluded interventions for overweight and obese children. On the other hand, Wahi et al., failed to find a significant difference in mean BMI change at post-intervention between the intervention and control groups among the 6 studies reviewed. Moreover, this review combined multifaceted interventions aiming to modify several behaviors including dietary habits, physical activity, and sedentary behaviors with interventions that solely focusing on a single behavior, reducing sedentary time. Therefore, it is not clear which behavior change contributed the most to weight improvement, or whether it was additive effect of change in all three behaviors that led to the BMI change. The inconsistent finding in BMI may partly due to the different inclusion/exclusion criteria that the van Grienken et al. and Wahi et al. meta-analytic reviews applied. Meanwhile, since the last literature search cut-off date for the two meta-analyses (April, 2011), results from at least 10 new sedentary intervention studies for children have been published. Inclusion of these new studies may help us to better elucidate the effects of sedentary interventions on BMI change among children.
The primary aim of the present meta-analysis was to summarize and compare the effects of three different types of sedentary behavior interventions to reduce body fat in children: (1) interventions solely aiming to reduce sedentary behaviors (SB), (2) interventions aiming to reduce sedentary behaviors in combination with the promotion of physical activity (SB+PA), and (3) interventions aiming to reduce sedentary behaviors, in combination with promoting physical activity and improving dietary habits (SB+PA+diet). Since body mass index (BMI=Kg/m2) was used most consistently as the primary indicator of body fat in these studies, BMI reduction served as the primary outcome in this meta-analysis. It was hypothesized that interventions targeting multiple behavioral factors (SB+PA+diet) would have a greater effect on reducing BMI than interventions that only target one behavioral factor (SB), given that sedentary behavior, physical activity, and diet are thought to have independent and possibly additive effects on childhood obesity risk.6,10 The secondary aim of this study was to explore the effects of variables that may potentially moderate the intervention outcomes including (a) demographic characteristics of study participants (e.g., age, weight status); (b) intervention features and design (e.g., type of sedentary behaviors targeted, intervention delivery setting, intervention intensity, intervention duration, retention rate) and (c) outcome reporting features (e.g., format of BMI reported, whether standard deviation of the BMI change was reported). It is anticipated that results from this study will provide promising directions for future childhood obesity prevention research.
Methods
Literature Search Strategy
A literature search was conducted following the recommendations of Lipsey and Wilson.30 First, a computer search was conducted in Ovid Medline, PsycINFO, Web of Science, and Google Scholar from the first available year to July 2012 and restricted to articles published in the English language only. The following keyword combinations were used: Sedentary Behavior, Sedentary Lifestyle, Physical Inactivity, Television, or Screen Time, and Obesity or Overweight, and Children, Youth, Teens or Adolescence (see Table S1 for sample full search strategy used for OVID Medline). Titles and abstracts identified through the search process were reviewed to identify relevant articles. A related records search was performed through Web of Science for identified articles. Second, the table of contents for journals that commonly publish articles in the area were reviewed (e.g., Obesity, American Journal of Preventive Medicine, Journal of Pediatrics). Finally, bibliographies of narrative reviews and all identified articles were examined to achieve any additional studies.
Inclusion and Exclusion Criteria
Inclusion criteria for this meta-analysis were: (1) all study participants must be children age 18 or younger; (2) the study must be a randomized controlled intervention with a no-treatment control; and (3) the intervention must have components to reduce sedentary behaviors such as watching TV/DVD/VCR, playing sedentary video/computer games, and sitting time in general. Studies were included if children were randomly assigned to an intervention and to either an active control group that received some non-obesity prevention related information (e.g., a general parenting skill training, or a fire drill training), or a control group with usual-programming (e.g., standard physical education classes or any standard school curriculum classes), or an assessment-only control group. Random assignment to condition is crucial because it is the best way to generate a comparison group that is equal on any potential confounding variables at baseline, especially when intervention effects were accessed based on significant differences in change over time across conditions. Studies were excluded if: (1) the intervention used physical activity promotion as a method to reduce sedentary behaviors rather than specifically designed to limit time spent in sedentary behaviors, (2) the study did not report measurement of BMI before and after the intervention separately for the intervention and control groups, and (3) if the study only reported adjusted (for covariates such as baseline BMI, ethnicity, and household income) BMI at post-intervention.
The outcome variable for this meta-analysis was defined as the intervention vs. control group difference in BMI change scores before and after the intervention period. The predictor variable was the sedentary behavior intervention type: SB only intervention, SB+PA intervention, or SB+PA+diet intervention.
Data Extraction
A coding form was developed for data extraction and analysis purposes. The following information was extracted from each study by two reviewers independently: (a) study identification information (e.g., authors, year of publication, publication form); (b) sample characteristics (e.g., mean and range of age, country participants live in, gender composition of the sample, percent overweight at baseline of the sample); (c) study characteristics (e.g., type of intervention, intervention delivery setting, type of sedentary behaviors targeted, duration of intervention, frequency of intervention sessions, type of control group, attrition rate, presence of study follow-up) and (d) effect size information (e.g., format of reported BMI, mean BMI and standard deviation for each group at each time point). Agreement among reviewers for each item ranged from 90% to 100%, and all discrepancies were resolved through discussions that led to a consensus.
Risk of Bias Assessment
The Quality Assessment Tool for Quantitative Studies was used to assess study quality.31 For each study, six domains were scored with high, moderate, or low for risk of bias: selection bias, study design, confounders, blinding, data collection methods, and withdrawals and drop-outs. An overall rating of the study quality was then assigned based on scores from these six domains. The quality assessment was performed independently by two reviewers and the findings were compared and discussed until consensus was achieved.
Effect Size Calculation
Effect sizes were computed as d indices and expressed the difference in mean of the BMI change between children in an intervention and a control group, with negative values indicating a better outcome (a greater BMI decrease) for the intervention group. The d indices were calculated from the means and standard deviation of the BMI change scores (the difference between pre-intervention and post-intervention). When the standard deviation of the change score was not reported, the pooled standard deviation of the pre- and post-intervention was estimated by assuming the correlation between the two was equal to .90. When BMI change scores and standard deviation were only reported by subgroups (e.g., by gender), a combined effect across subgroups was computed.32 Effect sizes were corrected for small-sample bias by transforming the standardized mean difference, d, to Hedge’s g before analysis.30 Each effect size was weighed by the inverse of its variance to provide a more efficient estimation of true population effects by giving greater weight to studies with larger samples.
Summary of Meta-Analytic Data Analyses
The data analyses included (a) calculation of weighted effect sizes and 95% confidence intervals; (b) use of homogeneity analysis to test effect sizes variation; and if significant heterogeneity exists, an exploration of potential moderators; and (c) examination of potential publication bias. All meta-analytic tests were analyzed using a random-effects model, which assumes an underlying distribution of true effect sizes from which the included studies are drawn, and accounts for variability in effect sizes caused by both sampling error and true differences in effect sizes between studies.33
The homogeneity of mean corrected effect sizes was examined to determine if the variability in outcomes was greater than expected from sampling error and measurement artifacts. Q-statistics and I-squared were used to determine heterogeneity among studies. A significant Q-statistic (within-group) indicates heterogeneity of effects. I-square reports the extent of such heterogeneity. Potential moderators were determined a priori and included participants’ mean age, population (general population vs. overweight/obese children only), type of sedentary behaviors targeted (TV viewing only vs. multiple sedentary behaviors), intervention delivery setting (school-, home-, clinic-based, vs. mixed), intervention intensity (average sessions per week), intervention duration (in weeks), retention rate, format of BMI reported (raw scores vs. standardized z-score) and whether standard deviation of the BMI change score was reported or estimated. Moderators were examined using an omnibus test of between-group difference in mean effects (Qb). In addition, to explore the relationship among moderators (e.g., what type of intervention features might co-exist), bivariate correlation test was also performed.
Publication bias was examined using Egger’s test of the regression intercept and funnel plots. If either a small-study effect or an asymmetric shape of funnel plot was present, possible publication bias was suspected and trim and fill method was used to adjust the estimates.32 Effect size calculation and publication bias tests were conducted using Stata (Version 12), and meta-regression was run using SPSS (Version 17.0).
Results
Sample Characteristics
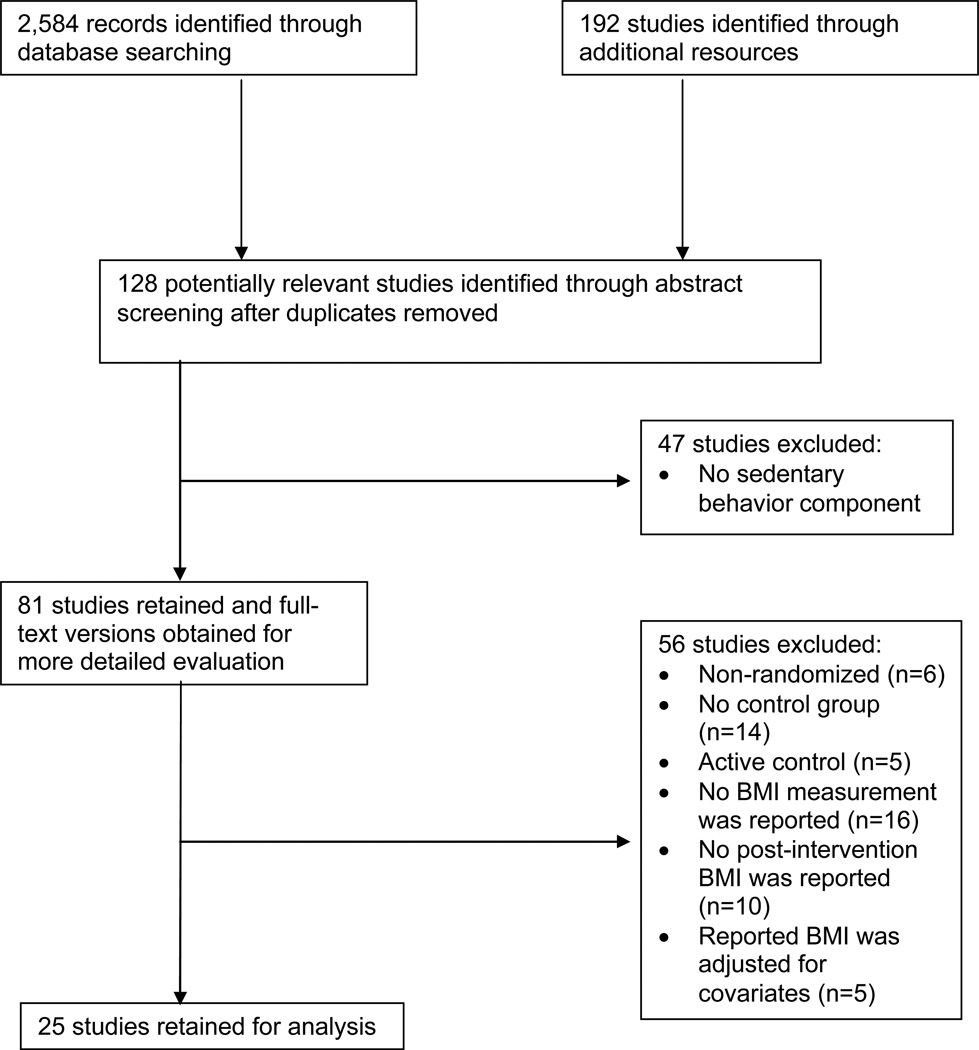
A total of 25 unique studies were included in this meta-analysis: five were SB only interventions,34–38 ten were SB+PA interventions,39–48 and ten were SB+PA+diet interventions.49–58 Figure 1 shows the flowchart for retrieving the articles. Table 1 summarizes the general characteristics of the final 25 studies. All studies were published in peer-reviewed journals, and five were results from pilot studies. Most of the studies were published fairly recently (16 were published between year 2008 and year 2012). Table 2 provides more details for each intervention study.
Figure 1.
Flowchart for literature search.
Table 1.
General Characteristics of Included Studies
| Characteristics | Number of Studies |
|---|---|
| Publication Year | |
| Prior to 2000 | 1 |
| 2001–2005 | 4 |
| 2006–2010 | 14 |
| 2011–2012 | 6 |
| Country of Study | |
| North America (U.S. or Canada) | 14 |
| Europe | 6 |
| Australia and New Zealand | 4 |
| Asia | 1 |
| Mean Age of Study Sample | |
| < 6 years | 5 |
| 6–12 years | 15 |
| > 12 years | 5 |
| Targeted Sample | |
| General population | 16 |
| Overweight or obese children only | 9 |
| Setting of Intervention | |
| School-based | 5 |
| Home-based | 9 |
| Clinic-based | 5 |
| Mixeda | 6 |
| Sedentary Behaviors Targeted | |
| TV viewing only | 10 |
| TV viewing and other screen-related activities | 15 |
| Duration of Intervention | |
| < 3 months | 8 |
| 3 months – 6 months | 9 |
| > 6 months | 8 |
| Intervention Follow-upb | |
| Has follow-up | 9 |
| No follow-up | 16 |
| Format of BMI Reported | |
| Raw BMI score | 14 |
| Age/gender standardized z-BMI score | 11 |
Note:
Interventions that had both school/clinic component and home component.
Studies that had follow-up measurements of height and weight after the end of intervention.
Table 2.
Characteristics of the Interventions
| Study | Intervention Type |
Participants | Intervention | Control | Duration (weeks) |
Follow-up Measurementa |
Effects on BMI |
|---|---|---|---|---|---|---|---|
| Dennison et al., 2004 | SB | N=222 Age range: 2.5–5.5 Mean age (year): 4 Sex: 49% male Race: mostly white General population |
School and home-based. No behavior change theories specified; intervention aimed to show preschool staff and parents the positive alternative activities to TV viewing, such as improved literacy skills and enhanced social skills. Children attended a 7-session program to be educated to reduce TV-viewing time. After each class, materials and activities were sent home to foster discussion between parents and children. | No treatment | 39 | None | No significant difference in BMI raw score and BMI z-score change between intervention and control groups. |
| Robinson et al., 1999 | SB | N=198 Age range: 8–10 Mean age (year): 9.9 Sex: 53% male Race: mostly white General population |
School and home-based. Based on social cognitive theory, children were educated to budget TV watching time (self-monitoring and self-reporting strategies), newsletters were sent to parents to help children stay within budget. Each household also received an electronic television time manager to help with budgeting. | No treatment | 25 | None | Children in the intervention group had a significant decrease in raw BMI as compared with the control group. |
| Todd et al., 2008 | SB | N=22 Age range: 8–11 Mean age (year): 9.9 Sex: all male Race: mostly (>80%) white General population |
Home-based. No behavior change theories specified; intervention aimed to enhance awareness of electronic media use and to set goals to minimize use. Children and parents attended family-centered interactive session designed to reduce TV-viewing time and increase awareness to minimize electronic media use. TV and computer-locking devices were installed to help monitoring and limiting children’s TV and computer use. Follow-up newsletters were sent to home. | No treatment | 20 | None | No significant change in BMI raw score between intervention and control groups. |
| Epstein et al., 2008 | SB | N=70 Age range: 4–7 Mean age (year): 6 Sex: 53% male Race: mostly white Children BMI at or above 75th BMI percentile |
Home-based. No behavior change theories specified; a reward system was set up based on children’s TV-viewing time. TV allowance was set up to budget children’s TV-viewing time. Children earned $0.25 for each half hour under budget, up to $2.00 per week. Parents praised children for reduced TV-viewing time and for engaging in alternative behaviors. Monthly newsletters were sent to parents with information about how to rearrange home environment. | No treatment | 104 | None | Children in the intervention group had a significant decrease in BMI z-score as compared with the control group. |
| Mhurchu et al, 2009 | SB | N=29 Age range: 9–12 Mean age: 10.4 Sex: 62% male Race: 65% European Obese population |
Home-based. No behavior change theories specified; TV time monitor was provided to limit children’s access to TV. Parents had the control of the time budget, and were encouraged to restrict TV watching to 1 hour per day or less for their children. | Only receive verbal advice on general strategies to decrease TV watching; no TV time monitor was provided | 6 | None | No significant difference in BMI raw score and BMI z-score change between intervention and control groups. |
| Reilly et al., 2006 | SB+PA | N=545 Age range: 4–5 Mean age (year): 4.2 Sex: 50% male Race: mostly white General population |
School and home based. No behavior change theories specified; intervention components included enhanced physical activity program in nursery (three 30-min sessions a week over 24 weeks) plus home-based health education aimed at increasing physical activity through play and reducing TV viewing time. | No treatment | 24 | Week 28 | No significant difference in BMI raw score change between intervention and control groups. |
| Maloney et al., 2008 | SB+PA | N=60 Age range: 7–8 Mean age (year): 7.5 Sex: 50% male Race: mostly white General population |
Home-based. No behavior change theories specified; written physician prescription was given to children to play 120 minutes per week of Dance Dance Revolution and daily minutes of Dance Dance Revolution play was recorded, supervised by parents. | No treatment | 10 | Week 18 | Children in the intervention group had a significant decrease in BMI raw score as compared with the control group. |
| Graves et al., 2010 | SB+PA | N=58, Age range: 8–10 Mean age: 9.2 Sex: 67% male Race: mostly white General population |
Home-based. No behavior change theories specified; a peripheral device (jOG), a step-powered video game, was given to children to encourage light-to-moderate intensity activity and reduce sedentary time. | No treatment | 12 | None | No significant difference in BMI raw score change between control and intervention groups. |
| Goran et al., 2005 | SB+PA | N=209 Age range: 8.8–11.1 Mean age (year): 9.4 Sex: 40% male Race: mostly Hispanic General population |
School-based. Based on social cognitive theory, eight CD-ROM interactive animated lessons, four classroom lessons, and four family-based assignments were delivered over 8 weeks. Each lesson incorporated elements of social cognitive theory including outcome expectancies, behavioral capability and modeling, goal setting, self-monitoring, reinforcement, self-efficacy, and environmental aspects aiming to increase levels of physical activity, decrease sedentary behavior, and alter psychosocial variables related to physical activity. | No treatment | 8 | None | No significant difference in BMI raw score and BMI z-score change between intervention and control groups. Female students in the intervention group had a significantly larger decrease in BMI z-score as compared with the control group. |
| Harrison et al., 2006 | SB+PA | N=312 Age range: 9–11 Mean age (year): 10.2 Sex: 57% male Race: mostly white General population |
School-based. Based on social cognitive theory, the 10-lesson, teacher-led intervention emphasized on self-control, self-monitoring, and goal setting skills. | No treatment | 16 | None | No significant difference in BMI raw score change between control and intervention groups. |
| Simon et al., 2008 | SB+PA | N=954 Age range: 9.9–13.8 Mean age (year): 11.6 Sex: 46.7% male Race: mostly white General population |
School-based. A multilevel program aimed to affect the intrapersonal, social and certain environmental determinants of physical activity with three principal targets: (1) knowledge, attitudes, beliefs and motivation towards physical activity; (2) social support; and (3) environmental conditions. The intervention included an educational components focusing on physical activity and sedentary behavior and opportunities for physical activity were provided at lunchtime and after school hours. | No treatment | 208 | None | Children in the intervention group had a significant smaller increase in BMI z-score as compared with the control group. |
| Spruijt-Metz et al., 2008 | SB+PA | N=459 Age range: 12–13 Mean age (year): 12.5 Sex: all female Race: mostly Hispanic General population |
School-based. Based on the self determination theory and the theory of meanings of behavior, the intervention aimed to increase positive meanings and promote intrinsic motivation for physical activity. Students received information about media-based physical activity and TV-viewing and other sedentary behaviors classroom education and participated in learning activities that supported engagement in physical activity and TV-viewing time. | No treatment | 1 | Week 13 | No significant difference of BMI z-score change between intervention and control groups. |
| Faith et al., 2001 | SB+PA | N=10 Age range: 8–12 Mean age (year): 10 Sex: 70% male Race: no info Obese population |
Home-based. Intervention was based on the behavioral theory of reinforcement. Children pedaled on the electronically braked cycle ergometer to activate power of TV. | No treatment | 10 | None | Children in the intervention group had a decrease in raw BMI whereas children in the control group had an increase in raw BMI. |
| Goldfield et al., 2006 | SB+PA | N=30 Age range: 8–12 Mean age (year): 10.5 Sex: 43% male Race: mostly white Overweight and obese population |
Home-based. Intervention was based on the behavioral theory of reinforcement, with an open-loop feedback system. Children accumulated 400 counts of physical activity on pedometers earned 1 hour of TV/VCR/DVD time. Parents reviewed the physical activity amount and implemented the contingencies (the open-loop feedback feature). | No treatment | 8 | None | Children in the intervention group had a significant decrease in BMI raw score as compared with the control group. |
| Maddison et al., 2011 | SB+PA | N=322, Age range: 10–14 Mean age (year): 11.6 Sex: 73% male; Race: 57% European Overweight or obese population |
Home-based. No behavior change theories specified; active video games were given to children to encourage them to increase physical activity and decrease screening time. | No treatment | 24 | None | Children in the control group had a significant increase in BMI z-score as compared with the intervention group. |
| Gentile et al., 2009 | SB+PA+diet | N=1323; Age range: 6.1–12.7 Mean age (year): 9.6 Sex: 47% Race: 90% white General population |
School and home-based. Based on the social ecological framework, the intervention targeted families as the primary leverage point, and school-based reinforcement and incentives as well as community support as the secondary leverage points. Children were encouraged to adapt to healthy lifestyle by using self-rewards, school education, family-planned meals, and creating short-term and long-term goals of healthy active lifestyle. | No treatment | 30 | Week 26 | No significant difference in BMI raw score change between intervention and control groups. |
| Fitzgibbon et al., 2012 | SB+PA+diet | N=128; Age range: 3–5 Mean age (year): 4.5 Sex: 50% male Race: Hispanic General population |
School and home-based. Based on social cognitive theory, and relevant components of the health belief model and self-determination theory were also incorporated. Intervention curriculum included nutrition instruction and physical activity session, both supplemented by a Spanish language CD. Child component targeted specific child behaviors to increase consumption of fruits, vegetables, and fiber; decrease fat intake; reduce television viewing; and increase the duration and level of daily physical activity. | Weekly general health education | 14 | Week 52 | Both the intervention and control groups decreased BMI raw score and BMI z-score. No significant difference in BMI raw score and BMI z-score change between intervention and control groups. |
| Lubans et al., 2012 | SB+PA+diet | N=357, Age range: 12–14 Mean age (year): 13.2 Sex: all female Race: mostly Australian General population |
School and home-based. Based on social cognitive theory, the intervention targeted psychological, behavioral, and environmental influences on physical activity and nutrition behavior change, and focused on promoting lifetime physical activities, reducing sedentary behaviors, and encouraging low-cost healthy eating. Intervention components included enhanced school sport sessions, interactive seminars, nutrition workshops, lunch-time physical activity sessions, handbooks and pedometers, parent newsletters, and text messaging for social support. | No treatment | 52 | None | No significant difference in BMI raw score and BMI z-score change between intervention and control groups. |
| Singh et al., 2009 | SB+PA+diet | N=1108 Age range: 12–14 Mean age (year): 12.7 Sex: 49.5% male Race: mostly Western/Dutch General population |
School-based. Using an intervention mapping approach, intervention selected multiple theoretical strategies for behavioral change, including self monitoring, self-evaluation, reward, increasing skills, goal setting, environmental changes, social encouragement, social support, information regarding behavior and personalized messages. The intervention consisted of an educational program (individual component), and an environmental component (i.e., changes in and around school cafeterias). | No treatment | 35 | Week 17 and week 52 | No significant difference of BMI raw score change between intervention and control groups. |
| French et al., 2011 | SB+PA+diet | N=90 Age range: 12–17 Mean age (year): 14.7 Sex: 61% male Race: 58% white General population |
Home-based. Based on the social ecology framework, the intervention included both household environment and individual-level behavioral components such as placement of TV time-limiting devices, provision of guidelines about food availability, face-to-face group sessions, and monthly newsletters. | No treatment | 52 | None | No significant difference in BMI z-score change between intervention and control groups. |
| Taveras et al., 2011 | SB+PA+diet | N=475, Age range: 2–6.9 Mean age (years): 4.9 Sex: 52% male; Race: no info; Overweight population |
Clinic-based. Based on the chronic care model, the major components of the intervention involved changes to the health care system. Intervention includes primary care restructuring, and families received motivational interviewing by pediatric nurse practitioners regarding TV viewing and fast food and sugar intake. | Usual care which included well-child care visits and follow-up appointments for weight checks with their pediatrician or subspecialist | 52 | None | No significant difference in raw BMI score and BMI z-score change between intervention and control groups. |
| McCallum et al., 2007 | SB+PA+diet | N=163 Age range: 5–9 Mean age (year): 7.4 Sex: 48% male Race: no info Obese population |
Clinic-based. Using an intervention mapping approach, modifiable behavioral determinants of obesity were identified. General practitioners used a brief solution-focused approach to set and record appropriate, healthy lifestyle goals with the family, assisted by a personalized 20-page family folder, which aimed to help improve children’s physical activity, TV viewing and other sedentary behaviors and diet. | No treatment | 12 | Week 39 and week 65 | No significant difference in BMI raw score change between intervention and control groups. |
| Hughes et al., 2008 | SB+PA+diet | N=134 Age range: 5–11 Mean age (year): 8.7 Sex: 44% male Race: no info Overweight population |
Clinic-based. A best-practice, family-centered, behavior change counseling delivered by pediatric dietitians. Used multiple behavioral strategies including exploring motivation to change, exploring pros and cons of change, identifying barriers to change, problem-solving barriers, goal-setting, rewards, self-monitoring, social support, and preventing relapse to modify diet, physical activity, TV viewing and other sedentary behaviors. | No treatment | 26 | Week 25 and week 52 | No significant difference of BMI z-score change between intervention and control groups from baseline to 6 and 12 months. |
| Wafa et al., 2011 | SB+PA+diet | N=107 Age range: 7–11 Mean age (year): 9.8 Sex: 50% male; Race: no info; Obese population |
Clinic-based. A parent-centered, dietician-led program based on trans-theoretical model and social cognitive theory. The program included 8 group sessions focused on changing diet, physical activity, and sedentary behavior. Parents also received treatment materials. | No treatment | 24 | None | No significant difference in BMI z-score change between intervention and control groups. |
| Saelens et al., 2002 | SB+PA+diet | N=44 Age range: 12–16 Mean age (year): 14.2 Sex: 59.1% male Race: 70.5% white Overweight population |
Clinic-based. No behavior change theories specified; intervention aimed to address behavioral skills including self-monitoring, goal setting, problem solving, stimulus control, self-reward, and preplanning. Children engaged in a computer-based program on physical activity, diet, and sedentary behavior education. Children also received weekly phone counseling. Parents received information sheets including recommended parental skills. | A single session of physician weight counseling | 17 | Week 23 | Children in the intervention group had a slight decrease in BMI z-score as compared with the control group. |
Note:
Indicates the follow-up measurement occurred at post-intervention, if any.
Risk of Bias Assessment
Table 3 shows the results of the quality assessment for each study. Selection bias was low (rating of strong) for studies where participants were randomly selected from a comprehensive list of individuals and participation rate was high (>80%). Selection bias was high (rating of weak) for studies where participants were self-referred or the selection of participants was not described adequately. Since our search criteria only included randomized control trails, all of the included studies were strong in study design. However, only 11 of the 25 studies reported sequence generation of the randomization. Most of the studies (88%) had comparable intervention and control groups on key demographic variables and study outcomes at baseline (rating of strong on confounders). Seven studies reported that the outcome assessors were not aware of the group assignment, four studies reported the opposite, and the rest of the studies did not describe the blinding of the outcome assessor. Only one study reported that the study participants were not aware of the primary research question, two studies reported the opposite, and the rest of the study did not describe such information. All studies used valid and reliable data collection methods. Furthermore, most studies (92%) had good retention rate (at least 80%) post-intervention. Overall, ten studies were rated strong for study quality, four studies were rated weak, and the others were rated moderate.
Table 3.
Assessment of Risk of Bias of Included Studies
| Study | Selection Bias |
Study Design |
Confounders | Blinding | Data Collection Methods |
Withdrawals and Drop-outs |
Global Rating |
|---|---|---|---|---|---|---|---|
| Dennison et al., 2004 | Strong | Strong | Strong | Moderate | Strong | Strong | Strong |
| Robinson et al., 1999 | Moderate | Strong | Strong | Strong | Strong | Strong | Strong |
| Todd et al., 2008 | Weak | Strong | Strong | Moderate | Strong | Strong | Moderate |
| Epstein et al., 2008 | Weak | Strong | Strong | Weak | Strong | Strong | Weak |
| Mhurchu et al., 2009 | Weak | Strong | Strong | Moderate | Strong | Strong | Moderate |
| Reilly et al., 2006 | Strong | Strong | Strong | Moderate | Strong | Strong | Strong |
| Maloney et al., 2008 | Weak | Strong | Strong | Moderate | Strong | Strong | Moderate |
| Graves et al., 2010 | Moderate | Strong | Strong | Weak | Strong | Moderate | Moderate |
| Goran et al., 2005 | Moderate | Strong | Strong | Moderate | Strong | Strong | Strong |
| Harrison et al., 2006 | Moderate | Strong | Strong | Moderate | Strong | Strong | Strong |
| Simon et al., 2008 | Strong | Strong | Strong | Moderate | Strong | Strong | Strong |
| Spruijt-Metz et al., 2008 | Strong | Strong | Strong | Moderate | Strong | Strong | Strong |
| Faith et al., 2001 | Weak | Strong | Weak | Moderate | Weak | Strong | Weak |
| Goldfield et al., 2006 | Moderate | Strong | Strong | Moderate | Weak | Strong | Moderate |
| Maddison et al., 2011 | Weak | Strong | Strong | Weak | Strong | Strong | Weak |
| Gentile et al., 2009 | Moderate | Strong | Strong | Moderate | Strong | Strong | Strong |
| Fitzgibbon et al., 2012 | Strong | Strong | Strong | Weak | Strong | Strong | Moderate |
| Lubans et al., 2012 | Moderate | Strong | Strong | Moderate | Strong | Strong | Strong |
| Singh et al., 2009 | Moderate | Strong | Moderate | Weak | Strong | Strong | Moderate |
| French et al., 2011 | Weak | Strong | Weak | Moderate | Strong | Strong | Weak |
| Taveras et al., 2011 | Weak | Strong | Strong | Moderate | Strong | Strong | Moderate |
| McCallum et al., 2007 | Weak | Strong | Strong | Moderate | Strong | Strong | Moderate |
| Hughes et al., 2008 | Moderate | Strong | Strong | Moderate | Strong | Moderate | Moderate |
| Wafa et al., 2011 | Weak | Strong | Strong | Moderate | Strong | Strong | Moderate |
| Saelens et al., 2002 | Moderate | Strong | Strong | Moderate | Strong | Strong | Strong |
Mean Effect Sizes for SB only vs. SB+PA vs. SB+PA+diet Interventions
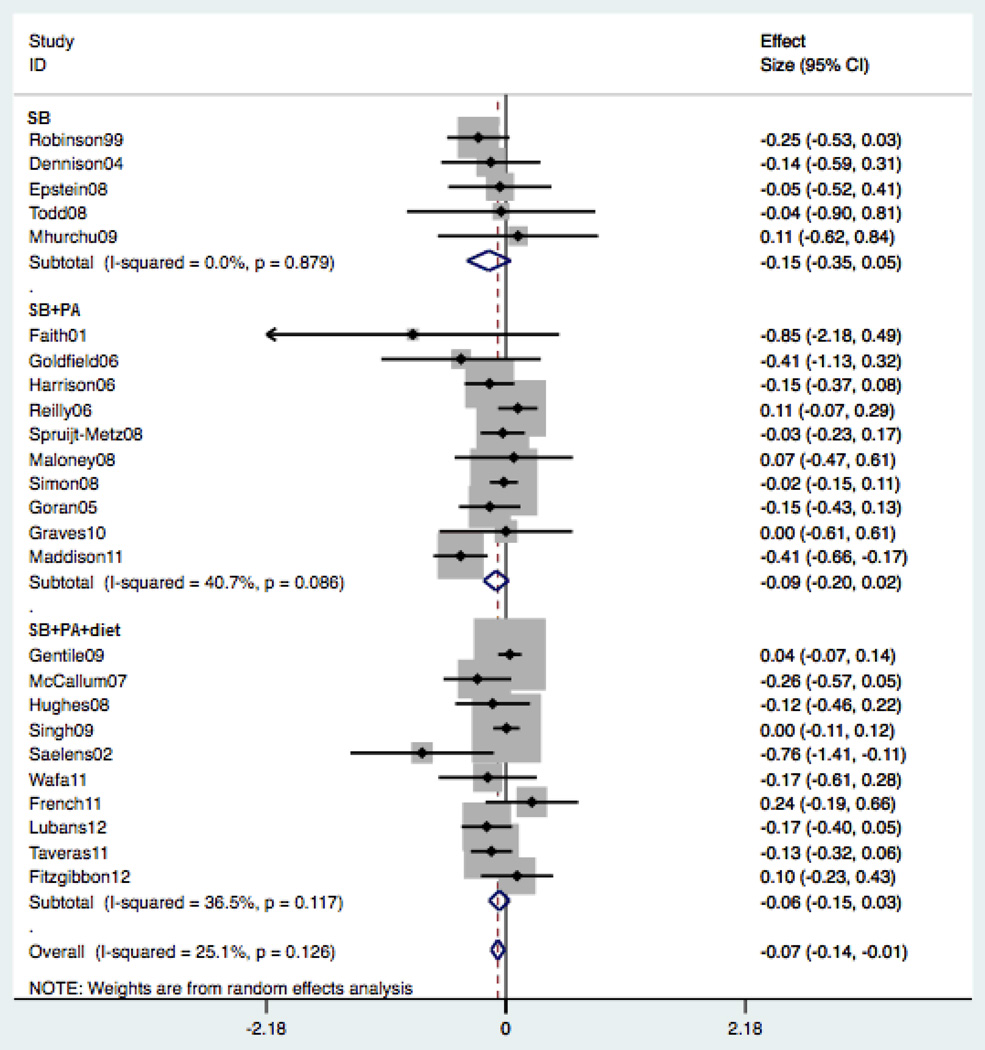
Across all studies, the total number of participants (intervention + control group) with complete data was 389 for SB only interventions, 2,805 for SB+PA interventions, and 3,851 for SB+PA+diet interventions. When the three types of intervention studies were combined together, the pooled effect size from all 25 studies was significant (g = −.073, p = .021), indicating an overall effect of sedentary behavior intervention on BMI reduction among children (see Table 3). This effect size indicates that the mean BMI reduction for the intervention groups was .10 (kg/m2) greater compared to the control groups. However, when examined separately, the effect sizes were not significantly different from zero for SB only interventions (g = −.154, p = .129), SB+PA interventions (g = −.089, p = .125), and SB+PA+diet interventions (g = −.060, p = .214). No significant difference was found for mean effect size among SB interventions, SB+PA interventions, and SB+PA+diet interventions (Qb = 32.05, p = .126). Figure 2 shows the adjusted effect size for each study by intervention type.
Figure 2.
Effect size on BMI reduction by intervention type.
Note: I-square – the variation in pooled effect size attributable to heterogeneity within that group.
Heterogeneity and Moderator Analyses
Table 3 shows that the effects of studies were homogeneous within SB interventions (Q = 1.19, p = .879), SB+PA interventions (Q = 15.18, p = .086), and SB+PA+diet interventions (Q = 14.17, p = .117) in the random-effects model. The heterogeneity observed in the pooled estimate was low (I2 = 25%, p = .126; see Figure 2). Since insignificant heterogeneity was observed, the moderator analyses set a priori to explain heterogeneity were not explored. Bivariate correlations showed that only intervention delivery setting was significantly associated with intervention type (Spearman’s Rho = .565, p = .003). All of the clinic-based intervention studies had multiple components (SB+PA+diet). Most (80%) of the school-based interventions were SB+PA type. Among the moderators, participants’ age was associated with type of sedentary behaviors targeted (r = .568, p = .004). Interventions with older participants were more likely to target multiple sedentary behaviors. Intervention delivery setting was associated with intervention intensity (r = −.809, p < .001). The clinic-based interventions had the lowest intensity (i.e., less than one session per week).
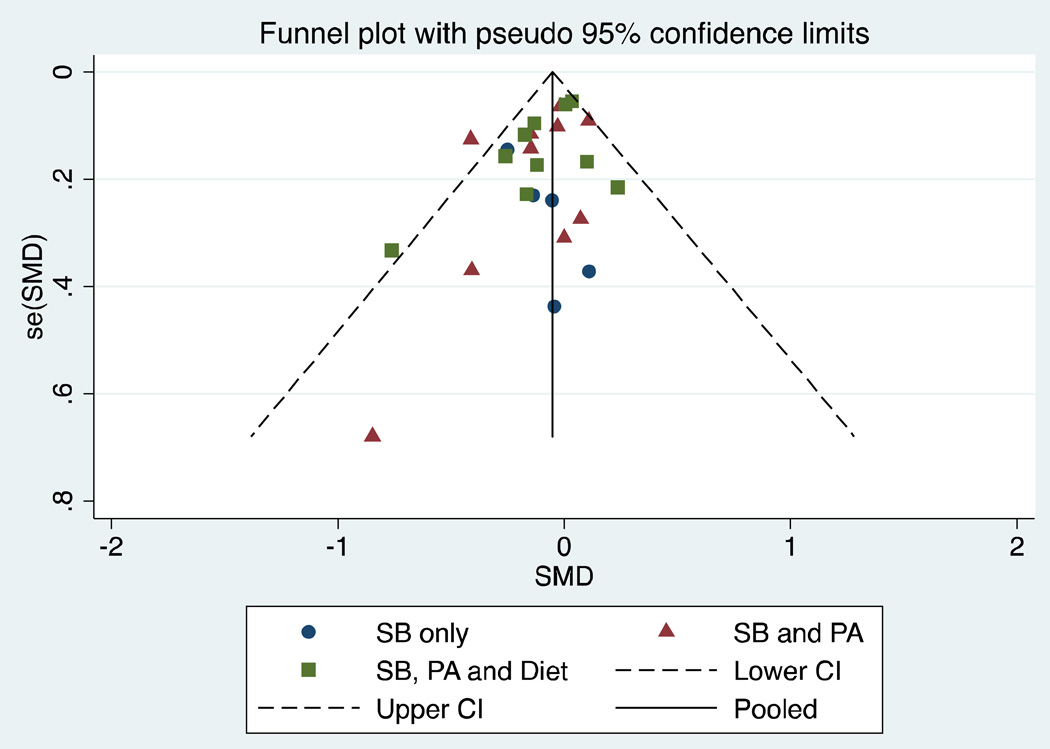
Publication Bias
The Egger’s regression test showed small-study effects (i.e., small studies produce larger effect size) for the 25 studies (b0 = −.887, p = .037). The funnel plot of effect size from each study is in general symmetrical (see Figure 3), suggests the absence of publication bias. A further trimmed-and-filled analysis also confirmed that there was no publication bias.
Figure 3.
Funnel plot for BMI reduction, by intervention type.
Discussion
Results from this meta-analysis of 25 studies suggest that interventions seeking to decrease sedentary behaviors among children significantly reduced BMI when compared to children in control groups. Although the observed magnitude of BMI mean differences (g = −.073, p = .021) between intervention and control groups at post-intervention may not achieve a level considered to be clinically significant (a minimum of .25 standardized BMI unit reduction) for the treatment of obese children,59 it may be approaching the magnitude of change required to achieve population-level public health significance in obesity prevention interventions among non-obese children, which is not entirely known.
When looking at each type of intervention studies (SB, SB+PA, and SB+PA+diet) separately, none had a significant effect in BMI reduction. Further, contrary to our hypothesis, multi-components interventions (SB+PA or SB+PA+diet) were not more effective in BMI reduction than SB only interventions in this sample of studies. This result is consistent with van Grieken’s28 findings. However, another meta-analytic study of the obesity interventions for children showed that the mean effect sizes for three- or four-component intervention were much greater than the one- or two-component interventions.60 In this review, there was only one study with four intervention components (physical activity, nutrition, counseling, and medication) among the 40 studies under examination, and the difference between one- and two-component interventions was not significant. Our results also showed that the SB only interventions had a larger mean effect size (g = −.154) than the SB+PA (g = −.089) and SB+PA+diet (g = −.060) interventions, although none of the subgroup effect sizes was statistically significant. This finding is similar to a narrative review article examining obesity prevention programs in children, which suggested that intervention studies focusing on single behavior change had a stronger impact on BMI than those focused on multiple behavior changes.10 It is possible that for children, altering one behavior is easier to accomplish than altering two or more behaviors at the same time. In fact, most multiple health behavior change interventions in children failed to achieve significant changes, and the successful ones were all found among adults.61 Thus, multi-component obesity interventions might not be more effective than a single-component intervention among children. However, it is important to note that in the present meta-analysis, the effect of the interventions on targeted behavior change (i.e., sedentary behavior, physical activity, dietary intake) was not evaluated. Therefore, it is not clear whether the BMI reduction in multi-component interventions was a result of a decrease in sedentary behaviors, an increase in physical activity, an improvement in diet, or any combination thereof. Furthermore, it is also possible that we were not able to detect a significant difference between the three types of interventions due to limited power.
We did not observe a significant heterogeneity among the studies in this analysis. Only 25% of the variation in the overall effect size was attributable to between-studies heterogeneity (p-value n.s.). Nevertheless, the studies included in our analysis encompass interventions of different characteristics and purposes. For example, we included both prevention studies (interventions that targeted the general population) and treatment studies (interventions that were exclusively for overweight and obese children). Inclusion of both prevention and treatment studies could attenuate the observed effect of BMI reduction since the effect size is generally higher in treatment studies.60 Indeed, the two studies that had a significant effect size in BMI reduction in our sample were both treatment programs targeting overweight and obese children.48,49 However, the primary focus of our meta analysis was to assess the overall effect of sedentary behavior interventions (regardless of prevention or treatment orientation) on BMI reduction, and how such effect sizes may differ between single- versus multi-component interventions.
A particularly interesting finding from our analysis was that all of the clinic-based interventions included three components (SB+PA+diet). It is possible that given the short contact period (total intervention sessions raged from 4 to 11 times, with an average of meeting once every three weeks) with children, practitioners tried to give out as much helpful information as they could during each encounter. It is also possible that medical practice emphasizes the provision of all available evidence-based strategies for BMI reduction to patients. However, since results from the current meta-analysis suggest that the multi-component interventions did not exceed (and the mean effect size was even lower than) the single-component interventions on BMI reduction, and given the limited contact time, clinical health practitioners might want to consider focusing solely on limiting sedentary behaviors to reduce BMI for their pediatric patients.
Several limitations of the current study need to be noted. BMI reduction was the only parameter used to evaluate the effectiveness of interventions in this study. It is possible that an intervention may successfully reduce children’s time spent in sedentary behaviors in the absence of significant BMI change. Also, the intervention effect on BMI reduction was assessed by comparing the BMI change scores between the intervention and control group. It is possible that children in both intervention and control groups have increased BMI, but the intervention group has a smaller increase than the control group. In this case, the intervention is effective in slowing down the increase of BMI (rather than reducing BMI in children), and attenuating the rate of BMI increase in children also has health benefits.62 Children in this sample of studies were relatively young (participants for most studies aged from 4–12 years). Therefore, findings from this study may not be applied to children in older age groups. Moreover, demographic features of study participants, such as ethnicity and socioeconomic status, were often not reported in the primary studies; make it difficult to know how results generalize to other populations. Almost all of the studies included in the present meta-analysis were interventions carried out in developed countries within North America and Europe. Childhood obesity is a global problem, and the prevalence rate has been increasing steadily in some developing countries.63,64 Children’s lifestyles may be quite different across countries and cultures. Therefore, lifestyle interventions to prevent childhood obesity, such as sedentary behavior interventions, may not be universally effective. Lastly, we used the unadjusted mean BMI scores to calculate effect size, and excluded studies that only reported adjusted post-intervention outcomes. Although adjusting for covariates (e.g., demographic variables, baseline BMI) is a preferred way to present intervention results since it controls for potential cofounders, these adjusted results would not be comparable to the other majority studies that reported unadjusted results.
In summary, interventions that target to reduce sedentary behaviors among children are effective in reducing BMI. However, adding a physical activity promotion and diet improvement component to the intervention program did not appear to have an additive effect. A comprehensive sedentary behavior intervention that targets to reduce multiple sedentary activities may be as effective as multi-component programs in BMI reduction, and could be a promising way to prevent obesity in children.
Supplementary Material
Table 4.
Effect Size (ES) Summary (Random-Effects Model)
| Intervention Type |
k | Total N |
Adjusted ES range |
Mean ES (g) |
95% CI | z | p | Heterogeneity Q | p |
|---|---|---|---|---|---|---|---|---|---|
| SB | 5 | 389 | −.251 – .110 | −.154 | −.354 – .045 | 1.52 | .129 | 1.19 | .879 |
| SB+PA | 10 | 2,805 | −.846 – .108 | −.089 | −.202 – .025 | 1.53 | .125 | 15.18 | .086 |
| SB+PA+diet | 10 | 3,851 | −.762 – .236 | −.060 | −.154 – .034 | 1.24 | .214 | 14.17 | .117 |
| Overall | 25 | 7.045 | −.846 – .236 | −.073 | −.135 – −.011 | 2.31 | .021 | 32.05 | .126 |
Acknowledgements
CPD is supported by a post-doctoral fellowship, University of Texas School of Public Health Cancer Education and Career Development Program-National Cancer Institute/National Institutes of Health grant R25 CA57712. He was previously supported by National Cancer Institute grant 5 T32 CA 009492-25 (University of Southern California, Mary Ann Pentz, PI). The content is solely the responsibility of the author and does not necessarily represent the official views of the National Cancer Institute or the National Institutes of Health.
The authors would like to thank Dr. Wendy Wood from Department of Psychology University of Southern California for her comments on the preliminary version of this manuscript, and Dr. Chih-Ping Chou from Department of Preventive Medicine for his advice on statistical methods. This study was partially supported by American Cancer Society 118283-MRSGT-10-012-01-CPPB (Dunton, P. I).
Footnotes
The authors declare that there are no conflicts of interest.
REFERENCE
- 1.Krebs NF, Jacobson MS. Prevention of pediatric overweight and obesity. Pediatrics. 2003;112:424–430. doi: 10.1542/peds.112.2.424. [DOI] [PubMed] [Google Scholar]
- 2.Guo SS, Chumlea WC. Tracking of body mass index in children in relation to overweight in adulthood. Am J Clin Nutr. 1999;70:145S–148S. doi: 10.1093/ajcn/70.1.145s. [DOI] [PubMed] [Google Scholar]
- 3.Freedman DS, Dietz WH, Srinivasan SR, Berenson GS. The relation of overweight to cardiovascular risk factors among children and adolescents: the Bogalusa Heart Study. Pediatrics. 1999;103:1175–1182. doi: 10.1542/peds.103.6.1175. [DOI] [PubMed] [Google Scholar]
- 4.Must A, Strauss RS. Risks and consequences of childhood and adolescent obesity. Int J Obes Relat Metab Disord. 1999;23:S2–S11. doi: 10.1038/sj.ijo.0800852. [DOI] [PubMed] [Google Scholar]
- 5.Stice E, Shaw H, Marti CN. A meta-analytic review of obesity prevention programs for children and adolescents: the skinny on interventions that work. Psychol Bull. 2006;132:667–691. doi: 10.1037/0033-2909.132.5.667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Caballero B. Obesity prevention in children: opportunities and challenges. Int J Obes Relat Metab Disord. 2004;28:S90–S95. doi: 10.1038/sj.ijo.0802797. [DOI] [PubMed] [Google Scholar]
- 7.Han JC, Lawlor DA, Kimm SY. Childhood obesity. Lancet. 2010;375:1737–1748. doi: 10.1016/S0140-6736(10)60171-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Marti A, Moreno-Aliaga MJ, Hebebrand J, Martínez JA. Genes, lifestyles and obesity. Int J Obes Relat Metab Disord. 2004;28:S29–S36. doi: 10.1038/sj.ijo.0802808. [DOI] [PubMed] [Google Scholar]
- 9.Utter J, Neumark-Sztainer D, Jeffery R, Story M. Couch potatoes or french fries: are sedentary behaviors associated with body mass index, physical activity, and dietary behaviors among adolescents? J Am Diet Assoc. 2003;103:1298–1305. doi: 10.1016/s0002-8223(03)01079-4. [DOI] [PubMed] [Google Scholar]
- 10.Waters E, de Silva-Sanigorski A, Hall BJ, et al. Interventions for preventing obesity in children. Cochrane Database Syst Rev. 2011;12:001871. doi: 10.1002/14651858.CD001871.pub3. [DOI] [PubMed] [Google Scholar]
- 11.Rey-López JP, Vicente-Rodríguez G, Biosca M, Moreno LA. Sedentary behaviour and obesity development in children and adolescents. Nutr Metab Cardiovasc Dis. 2008;18:242–251. doi: 10.1016/j.numecd.2007.07.008. [DOI] [PubMed] [Google Scholar]
- 12.Bautista-Castaño I, Doreste J, Serra-Majem L. Effectiveness of interventions in the prevention of childhood obesity. Eur J Epidemiol. 2004;19:617–622. doi: 10.1023/b:ejep.0000036890.72029.7c. [DOI] [PubMed] [Google Scholar]
- 13.Epstein LH, Paluch RA, Gordy CC, Dorn J. Decreasing sedentary behaviors in treating pediatric obesity. Arch Pediatr Adolesc Med. 2000;154:220–226. doi: 10.1001/archpedi.154.3.220. [DOI] [PubMed] [Google Scholar]
- 14.Tremblay MS, LeBlanc AG, Kho ME, et al. Systematic review of sedentary behaviour and health indicators in school-aged children and youth. Int J Behav Nutr Phys Act. 2011;8:98. doi: 10.1186/1479-5868-8-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chinapaw MJ, Proper KI, Brug J, van Mechelen W, Singh AS. Relationship between young peoples' sedentary behaviour and biomedical health indicators: a systematic review of prospective studies. Obes Rev. 2011;12:e621–e632. doi: 10.1111/j.1467-789X.2011.00865.x. [DOI] [PubMed] [Google Scholar]
- 16.Robinson TN. Television viewing and childhood obesity. Pediatr Clin North Am. 2001;48:1017–1025. doi: 10.1016/s0031-3955(05)70354-0. [DOI] [PubMed] [Google Scholar]
- 17.Matheson DM, Killen JD, Wang Y, Varady A, Robinson TN. Children's food consumption during television viewing. Am J Clin Nutr. 2004;79:1088–1094. doi: 10.1093/ajcn/79.6.1088. [DOI] [PubMed] [Google Scholar]
- 18.Vandewater EA, Shim MS, Caplovitz AG. Linking obesity and activity level with children's television and video game use. J Adolesc. 2004;27:71–85. doi: 10.1016/j.adolescence.2003.10.003. [DOI] [PubMed] [Google Scholar]
- 19.Melkevik O, Torsheim T, Iannotti RJ, Wold B. Is spending time in screen-based sedentary behaviors associated with less physical activity: a cross national investigation. Int J Behav Nutr Phys Act. 2010;7:46. doi: 10.1186/1479-5868-7-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wong SL, Leatherdale ST. Association between sedentary behavior, physical activity, and obesity: inactivity among active kids. Prev Chronic Dis. 2009;6:A26. [PMC free article] [PubMed] [Google Scholar]
- 21.Sugiyama T, Healy G, Dunstan D, Salmon J, Owen N. Joint associations of multiple leisure-time sedentary behaviours and physical activity with obesity in Australian adults. Int J Behav Nutr Phys Act. 2008;5:35. doi: 10.1186/1479-5868-5-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Spanier PA, Marshall SJ, Faulkner GE. Tackling the obesity pandemic: a call for sedentary behaviour research. Can J Public Health. 2006;97:255–257. doi: 10.1007/BF03405599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.DeMattia L, Lemont L, Meurer L. Do interventions to limit sedentary behaviours change behaviour and reduce childhood obesity? A critical review of the literature. Obes Rev. 2007;8:69–81. doi: 10.1111/j.1467-789X.2006.00259.x. [DOI] [PubMed] [Google Scholar]
- 24.Leung MM, Agaronov A, Grytsenko K, Yeh MC. Intervening to reduce sedentary behaviors and childhood obesity among school-age youth: A systematic review of randomized trials. J Obes. 2012;2012:685430. doi: 10.1155/2012/685430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schmidt ME, Haines J, O'Brien A, et al. Systematic review of effective strategies for reducing screen time among young children. Obesity. 2012;20:1338–1354. doi: 10.1038/oby.2011.348. [DOI] [PubMed] [Google Scholar]
- 26.Biddle SJH, O'Connell S, Braithwaite RE. Sedentary behaviour interventions in young people: a meta-analysis. Br J Sports Med. 2011;45:937–942. doi: 10.1136/bjsports-2011-090205. [DOI] [PubMed] [Google Scholar]
- 27.Maniccia DM, Davison KK, Marshall SJ, Manganello JA, Dennison BA. A meta-analysis of interventions that target children's screen time for reduction. Pediatrics. 2011;128:e193–e210. doi: 10.1542/peds.2010-2353. [DOI] [PubMed] [Google Scholar]
- 28.van Grieken A, Ezendam NPM, Paulis WD, van der Wouden JC, Raat H. Primary prevention of overweight in children and adolescents: a meta-analysis of the effectiveness of interventions aiming to decrease sedentary behaviour. Int J Behav Nutr Phys Act. 2012;9:61. doi: 10.1186/1479-5868-9-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wahi G, Parkin PC, Beyene J, Uleryk EM, Birken CS. Effectiveness of interventions aimed at reducing screen time in children: a systematic review and meta-analysis of randomized controlled trials. Arch Pediatr Adolesc Med. 2011;165:979–986. doi: 10.1001/archpediatrics.2011.122. [DOI] [PubMed] [Google Scholar]
- 30.Lipsey MW, Wilson DB. Practical Meta-Analysis. California: Sage; 2001. [Google Scholar]
- 31.National Collaborating Centre for Methods and Tools. Quality Assessment Tool for Quantitative Studies. Hamilton, ON: McMaster University; 2008. (Updated April, 2010). Retrieved from http://www.nccmt.ca/registry/view/eng/14.html. [Google Scholar]
- 32.Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to meta-analysis. United Kingdom: Wiley; 2009. [Google Scholar]
- 33.Cooper HM, Hedges LV, Valentine JC. The handbook of research synthesis and meta-analysis. Second ed. New York: Russell Sage Foundation Publications; 2009. [Google Scholar]
- 34.Robinson TN. Reducing children's television viewing to prevent obesity: a randomized controlled trial. JAMA. 1999;282:1561–1567. doi: 10.1001/jama.282.16.1561. [DOI] [PubMed] [Google Scholar]
- 35.Dennison BA, Russo TJ, Burdick PA, Jenkins PL. An intervention to reduce television viewing by preschool children. Arch Pediatr Adolesc Med. 2004;158:170–176. doi: 10.1001/archpedi.158.2.170. [DOI] [PubMed] [Google Scholar]
- 36.Epstein LH, Roemmich JN, Robinson JL, et al. A randomized trial of the effects of reducing television viewing and computer use on body mass index in young children. Arch Pediatr Adolesc Med. 2008;162:239–245. doi: 10.1001/archpediatrics.2007.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Todd MK, Reis-Bergan MJ, Sidman CL, et al. Effect of a family-based intervention on electronic media use and body composition among boys aged 8–11 years: a pilot study. J Child Health Care. 2008;12:344–358. doi: 10.1177/1367493508097404. [DOI] [PubMed] [Google Scholar]
- 38.Ni Mhurchu C, Roberts V, Maddison R, et al. Effect of electronic time monitors on children's television watching: pilot trial of a home-based intervention. Prev Med. 2009;49:413–417. doi: 10.1016/j.ypmed.2009.09.003. [DOI] [PubMed] [Google Scholar]
- 39.Faith MS, Berman N, Heo M, et al. Effects of contingent television on physical activity and television viewing in obese children. Pediatrics. 2001;107:1043–1048. doi: 10.1542/peds.107.5.1043. [DOI] [PubMed] [Google Scholar]
- 40.Goran MI, Reynolds K. Interactive multimedia for promoting physical activity (IMPACT) in children. Obes Res. 2005;13:762–771. doi: 10.1038/oby.2005.86. [DOI] [PubMed] [Google Scholar]
- 41.Goldfield GS, Mallory R, Parker T, et al. Effects of open-loop feedback on physical activity and television viewing in overweight and obese children: a randomized, controlled trial. Pediatrics. 2006;118:e157–e166. doi: 10.1542/peds.2005-3052. [DOI] [PubMed] [Google Scholar]
- 42.Harrison M, Burns CF, McGuinness M, Heslin J, Murphy NM. Influence of a health education intervention on physical activity and screen time in primary school children: 'Switch Off--Get Active'. J Sci Med Sport. 2006;9:388–394. doi: 10.1016/j.jsams.2006.06.012. [DOI] [PubMed] [Google Scholar]
- 43.Reilly JJ, Kelly L, Montgomery C, et al. Physical activity to prevent obesity in young children: cluster randomised controlled trial. BMJ. 2006;333:1041. doi: 10.1136/bmj.38979.623773.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Spruijt-Metz D, Nguyen-Michel ST, Goran MI, Chou CP, Huang TT. Reducing sedentary behavior in minority girls via a theory-based, tailored classroom media intervention. Int J Pediatr Obes. 2008;3:240–248. doi: 10.1080/17477160802113415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Maloney A, Bethea T, Kelsey K, et al. A pilot of a video game (DDR) to promote physical activity and decrease sedentary screen time. Obesity. 2008;16:2074–2080. doi: 10.1038/oby.2008.295. [DOI] [PubMed] [Google Scholar]
- 46.Simon C, Schweitzer B, Oujaa M, et al. Successful overweight prevention in adolescents by increasing physical activity: a 4-year randomized controlled intervention. Int J Obes. 2008;32:1489–1498. doi: 10.1038/ijo.2008.99. [DOI] [PubMed] [Google Scholar]
- 47.Graves LE, Ridgers ND, Atkinson G, Stratton G. The effect of active video gaming on children's physical activity, behavior preferences and body composition. Pediatr Exerc Sci. 2010;22:535–546. doi: 10.1123/pes.22.4.535. [DOI] [PubMed] [Google Scholar]
- 48.Maddison R, Foley L, Mhurchu CN, et al. Effects of active video games on body composition: a randomized controlled trial. Am J Clin Nutr. 2011;94:156–163. doi: 10.3945/ajcn.110.009142. [DOI] [PubMed] [Google Scholar]
- 49.Saelens BE, Sallis JF, Wilfley DE, Patrick K, Cella JA, Buchta R. Behavioral weight control for overweight adolescents initiated in primary care. Obesity. 2002;10:22–32. doi: 10.1038/oby.2002.4. [DOI] [PubMed] [Google Scholar]
- 50.McCallum Z, Wake M, Gerner B, et al. Outcome data from the LEAP (Live, Eat and Play) trial: a randomized controlled trial of a primary care intervention for childhood overweight/mild obesity. Int J Obes. 2006;31:630–636. doi: 10.1038/sj.ijo.0803509. [DOI] [PubMed] [Google Scholar]
- 51.Hughes AR, Stewart L, Chapple J, et al. Randomized, controlled trial of a best-practice individualized behavioral program for treatment of childhood overweight: Scottish Childhood Overweight Treatment Trial (SCOTT) Pediatrics. 2008;121:e539–e546. doi: 10.1542/peds.2007-1786. [DOI] [PubMed] [Google Scholar]
- 52.Gentile DA, Welk G, Eisenmann JC, et al. Evaluation of a multiple ecological level child obesity prevention program: Switch® what you Do View, and Chew. BMC Med. 2009;7:49. doi: 10.1186/1741-7015-7-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Singh AS, Chin A, Paw MJ, Marijke J, Brug J, van Mechelen W. Dutch obesity intervention in teenagers: effectiveness of a school-based program on body composition and behavior. Arch Pediatr Adolesc Med. 2009;163:309–317. doi: 10.1001/archpediatrics.2009.2. [DOI] [PubMed] [Google Scholar]
- 54.French SA, Gerlach AF, Mitchell NR, Hannan PJ, Welsh EM. Household Obesity Prevention: Take Action—a Group-Randomized Trial. Obesity. 2011;19:2082–2088. doi: 10.1038/oby.2010.328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Taveras EM, Gortmaker SL, Hohman KH, et al. Randomized controlled trial to improve primary care to prevent and manage childhood obesity: the High Five for Kids study. Arch Pediatr Adolesc Med. 2011;165:714–722. doi: 10.1001/archpediatrics.2011.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wafa SW, Talib RA, Hamzaid NH, et al. Randomized controlled trial of a good practice approach to treatment of childhood obesity in Malaysia: Malaysian Childhood Obesity Treatment Trial (MASCOT) Int J Pediatr Obes. 2011;6:e62–e69. doi: 10.3109/17477166.2011.566340. [DOI] [PubMed] [Google Scholar]
- 57.Lubans DR, Morgan PJ, Okely AD, et al. Preventing obesity among adolescent girls: One-year outcomes of the nutrition and enjoyable activity for teen girls (NEAT Girls) Cluster Randomized Controlled Trial. Arch Pediatr Adolesc Med. 2012;166:821–827. doi: 10.1001/archpediatrics.2012.41. [DOI] [PubMed] [Google Scholar]
- 58.Fitzgibbon ML, Stolley MR, Schiffer L, et al. Family-based Hip-Hop to Health: outcome results. Obesity. 2012:136. doi: 10.1038/oby.2012.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ford AL, Hunt LP, Cooper A, Shield JP. What reduction in BMI SDS is required in obese adolescents to improve body composition and cardiometabolic health? Arch Dis Child. 2010;95:256–261. doi: 10.1136/adc.2009.165340. [DOI] [PubMed] [Google Scholar]
- 60.Seo DC, Sa J. A meta-analysis of obesity interventions among U.S. minority children. J Adolesc Health. 2010;46:309–323. doi: 10.1016/j.jadohealth.2009.11.202. [DOI] [PubMed] [Google Scholar]
- 61.Prochaska JJ, Spring B, Nigg CR. Multiple health behavior change research: An introduction and overview. Prev Med. 2008;46:181–188. doi: 10.1016/j.ypmed.2008.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Daniels SR, Arnett DK, Eckel RH, et al. Overweight in children and adolescents: pathophysiology, consequences, prevention, and treatment. Circulation. 2005;111:1999–2012. doi: 10.1161/01.CIR.0000161369.71722.10. [DOI] [PubMed] [Google Scholar]
- 63.James PT, Leach R, Kalamara E, Shayeghi M. The worldwide obesity epidemic. Obes Res. 2012:2001.123. doi: 10.1038/oby.2001.123. [DOI] [PubMed] [Google Scholar]
- 64.Gupta N, Goel K, Shah P, Misra A. Childhood obesity in developing countries: epidemiology, determinants, and prevention. Endocr Rev. 2012;33:48–70. doi: 10.1210/er.2010-0028. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.