Abstract
Infundibulocystic basal cell carcinoma is a rare variant. It was first described in 1987 and proposed as a new basal cell carcinoma (BCC) subtype by Ackerman and Walsh in 1990. Dermoscopy is a noninvasive diagnostic technique that allows prompt identification of many types of BCC. However, dermoscopic findings for the infundibulocystic variant have not been reported. In our patient the dermoscopic findings were maple leaf-like areas in the periphery of the tumor, multiple scattered blue-gray dots and globules, short, fine telangiectasia and chrysalis or white-shiny streaks. All these structures had an underlying anatomopathological correlation.
Conclusion:
According to our case report, dermoscopy findings may aid to clearly diagnose this unusual BCC variant with proper histopathological correlation.
Keywords: infundibulocystic, basal cell carcinoma, dermoscopy, histopathology
Introduction
Infundibulocystic basal cell carcinoma is a rare subtype of the most frequent form of human skin cancer (basal cell carcinoma). It was first described in 1987 and proposed as a new basal cell carcinoma (BCC) variant by Ackerman and Walsh in 1990 [1,2]. This unusual variant has been described to occur as a solitary entity or as part of nevoid basal cell carcinoma syndrome [3].
Histopathologically it is a well circumscribed, superficially located, basaloid cell tumor with hyperchromatic, pleomorphic nuclei and rare mitoses, multiple tiny cysts containing cornified cells lined by infundibular epithelium. It typically lacks follicular bulbs and papillae or papillary mesenchymal bodies. The stroma usually has abundant connective tissue mucin [4].
Dermoscopy is a non-invasive diagnostic technique that has become an integrative part of the clinical approach of skin tumors since it significantly improves the early diagnosis of melanoma and non-melanoma skin cancer (NMSC) compared to the naked eye examination [5]. Dermoscopy has also been used to improve pre-operative margin evaluation and monitoring treatment response to topical therapy [6,7]. Dermoscopic criteria for BCC have been clearly established and its value in discriminating superficial BCC from other subtypes was recently reported [8].
However, there is no previous dermoscopic description of the infundibulocystic variant.
Case presentation
A 49-year-old, female patient, skin phototype V, presented to the outpatient dermatology clinic for evaluation. The dermatological examination revealed a 4 mm, well-circumscribed, pigmented skin tumor affecting the medial aspect of her anterior right thigh. The neoplasm had a pale center with a peripheral pigmented rim with superficial scale, and it was firm to palpation. Clinically, the lesion resembled a dermatofibroma (Figure 1). Dermoscopic evaluation revealed the presence of maple leaf-like areas on the periphery, multiple scattered blue-gray dots and globules, short, fine telangiectasia and chrysalis or white-shiny streaks (Figure 2).
Figure 1.

Clinical examination revealed a 4 mm, well-circumscribed, pigmented skin tumor affecting the medial aspect of her anterior right thigh. The neoplasm had a pale center with a peripheral pigmented rim with superficial scale, and it was firm to palpation. [Copyright: ©2014 Roldán-Marín et al.]
Figure 2.

Dermoscopy revealed the presence of maple leaf-like areas on the periphery, multiple scattered blue-gray dots and globules, short, fine telangiectasia and chrysalis or white-shiny streaks. [Copyright: ©2014 Roldán-Marín et al.]
Due to the inconsistency between the clinical appearance and the dermoscopic findings, an excisional biopsy was performed. The histopathological examination at low magnification showed a well circumscribed, superficially located tumor, formed by anastomosing cords of basaloid keratinocytes with several tiny cornifying cysts (Figure 3). At higher magnification, tumor cells had scant cytoplasm with hyperchromatic, pleomorphic nuclei with rare mitoses and few necrotic cells. Some keratinocytes had granular melanin in their cytoplasm. There was a lymphocytic peritumoral inflammatory infiltrate. At the upper reticular dermis there was an increased number of collagen bundles horizontally arranged and aligned parallel to the epidermis. Lateral and deep margins were tumor free.
Figure 3.
At low magnification histopathological showed a well circumscribed, superficially located tumor, formed by anastomosing cords of basaloid keratinocytes with several tiny cornifying cysts. [Copyright: ©2014 Roldán-Marín et al.]
Discussion
We present a case of infundibulocystic basal cell carcinoma, meaning a BCC with upper follicular differentiation. Basal cell carcinoma rarely shows differentiation toward epithelial structures of adnexa including follicular, sebaceous, eccrine and apocrine. BCC was originally considered a neoplasm derived from the basal cells of the epidermis. Later, it was proposed that it could derive from primary epithelial germ cells or from any part of the equipotential ectoderm of the skin in combination with organized mesodermal stroma [9]. Thus basaloid cells in BCC have the potential for differentiation toward various epidermal appendages. A combination of different kinds of follicular differentiation toward infundibula and follicular germ cells is unique in the infundibulocystic variant of BCC.
Histopathologically, differential diagnosis includes basaloid follicular hamartoma and trichoepithelioma [2].
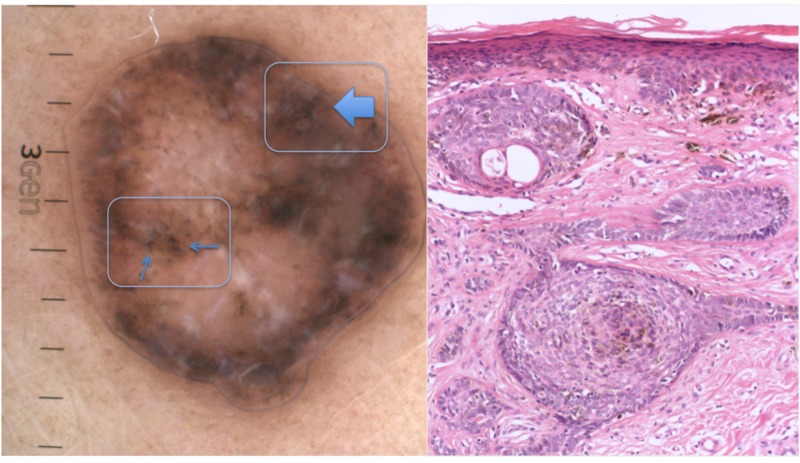
Dermoscopy is a powerful, non-invasive, diagnostic tool, which greatly increases diagnostic accuracy. It has demonstrated to help diagnose BCC and its various subtypes with high sensitivity and specificity [5,7]. In our patient, dermoscopy clearly showed criteria compatible with basal cell carcinoma. The maple leaf-like areas in the periphery as well as the scattered blue-gray dots and globules were due to the presence of pigmented epithelial nests in the papillary dermis (Figures 4 and 5). Short, fine telangiectasia was consistent with the presence of dilated blood vessels in the superficial dermis (Figure 6). The presence of chrysalis or white shiny structures was in agreement with the presence of an increased number of collagen bundles horizontally disposed and aligned parallel to the epidermis [10] (Figure 7).
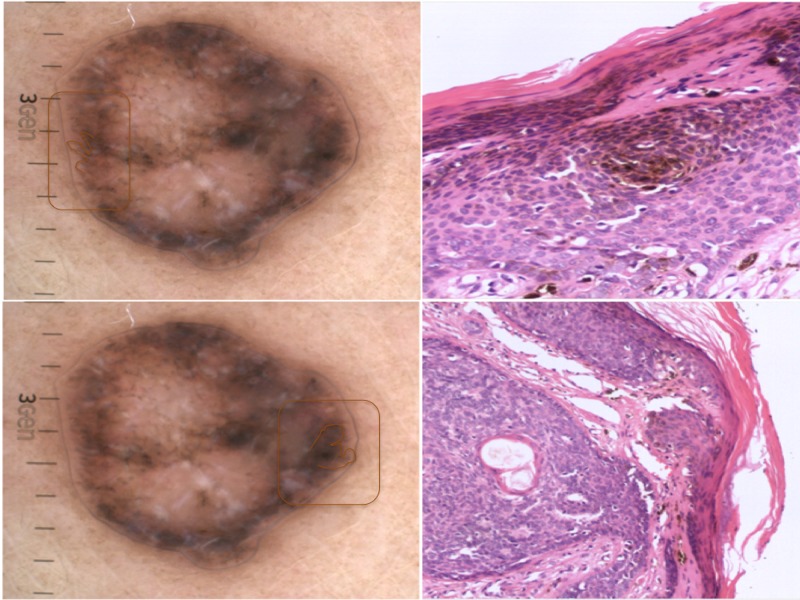
Figures 4 and 5.
Maple leaf-like areas in the periphery as well as the scattered blue-gray dots and globules linked to the presence of pigmented epithelial nests in the papillary dermis. [Copyright: ©2014 Roldán-Marín et al.]
Figure 6.
Short, fine telangiectasia due to the presence of dilated blood vessels in the superficial dermis. [Copyright: ©2014 Roldán-Marín et al.]
Figure 7.
White shiny structures related to the presence of an increased number of collagen bundles horizontally arranged and aligned parallel to the epidermis. [Copyright: ©2014 Roldán-Marín et al.]
This case illustrates the benefit of dermoscopy in establishing the diagnosis of basal cell carcinoma, even in this rare subtype. It also serves to exemplify how dermoscopy clearly aids the approach in the differential diagnosis between trichoepithelioma and BCC, which histologically can sometimes only be determined with immunohistochemistry staining. However, the most prominent dermoscopic findings in trichoepithelioma are arborizing telangiectasia and in desmoplastic lesions, an ivory-white background throughout [11,12].
Conclusion
This case report clearly exemplifies the usefulness of dermoscopy in the detection of BCC, even in this unusual subtype. It also serves to demonstrate once more how dermoscopy may bridge the gap between clinical and histopathological correlation, since each dermoscopic structure is related to a specific underlying anatomopathological correlate.
Footnotes
Funding: None.
References
- 1.Tozawa T, Ackerman AB. Basal cell carcinoma with follicular differentiation. Am J Dermatopathol. 1987;9:474–82. doi: 10.1097/00000372-198712000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Walsh N, Ackerman AB. Infundibulocystic basal cell carcinoma: a newly described variant. Mod Pathol. 1990;3:599–608. [PubMed] [Google Scholar]
- 3.Requena L, Fariña MC, Robledo M, et al. Multiple hereditary infundibulocystic basal cell carcinomas: a genodermatosis different from nevoid basal cell carcinoma syndrome. Arch Dermatol. 1999;135:1227–35. doi: 10.1001/archderm.135.10.1227. [DOI] [PubMed] [Google Scholar]
- 4.Kato N, Ueno H. Infundibulocystic basal cell carcinoma. Am J Dermatopathol. 1993;15:265–7. doi: 10.1097/00000372-199306000-00013. [DOI] [PubMed] [Google Scholar]
- 5.Lallas A, Argenziano G, Zendri E, et al. Update on non-melanoma skin cancer and the value of dermoscopy in its diagnosis and treatment monitoring. Expert Rev Anticancer Ther. 2013;13:541–58. doi: 10.1586/era.13.38. [DOI] [PubMed] [Google Scholar]
- 6.Caresana G, Giardini R. Dermoscopy-guided surgery in basal cell carcinoma. J Eur Acad Dermatol Venereol. 2010;24:1395–9. doi: 10.1111/j.1468-3083.2010.03652.x. [DOI] [PubMed] [Google Scholar]
- 7.Fargnoli MC, Kostaki D, Piccioni A, Micantonio T, Peris K. Dermoscopy in the diagnosis and management of non-melanoma skin cancers. Eur J Dermatol. 2012;22:456–63. doi: 10.1684/ejd.2012.1727. [DOI] [PubMed] [Google Scholar]
- 8.Lallas A, Tzellos T, Kyrgidis A, et al. Accuracy of dermoscopic criteria for discriminating superficial from other subtypes of basal cell carcinoma. J Am Acad Dermatol. 2014;70:303–11. doi: 10.1016/j.jaad.2013.10.003. [DOI] [PubMed] [Google Scholar]
- 9.Lever WF, Schaumburg-Lever G. Lever WF, Schaumburg-Lever G. Lever's Histopathology of the Skin. 7th ed. Philadelphia: JB Lippincott; 1990. Basal cell epithelioma; pp. 622–34. [Google Scholar]
- 10.Liebman TN, Rabinovitz HS, Balagula Y, Jaimes-Lopez N, Marghoob AA. White shiny structures in melanoma and BCC. Arch Dermatol. 2012:148–146. doi: 10.1001/archdermatol.2011.618. [DOI] [PubMed] [Google Scholar]
- 11.Ardigo M, Zieff J, Scope A, et al. Dermoscopic and reflectance confocal microscope findings of trichoepithelioma. Dermatology. 2007;215:354–8. doi: 10.1159/000107631. [DOI] [PubMed] [Google Scholar]
- 12.Khelifa E, Masouyé I, Kaya G, Le Gal FA. Dermoscopy of desmoplastic trichoepithelioma reveals other criteria to distinguish it from basal cell carcinoma. Dermatology. 2013;226:101–4. doi: 10.1159/000346246. [DOI] [PubMed] [Google Scholar]