Abstract
This is a case study of a female patient diagnosed with superficial spreading melanoma who decided to treat the lesion by the application of a preparation known as black salve. Persistence of the melanoma was documented five years later with subsequent evidence of metastatic spread to the regional lymph nodes, lungs, liver, subcutaneous tissues and musculature. A literature search has revealed one other case study of the use of black salve for the treatment of melanoma.
Keywords: black salve, melanoma, metastatic
Case report
In 2006 an otherwise healthy 76-year-old woman presented to her general practitioner (GP) with a pigmented skin lesion on her right calf below the popliteal fossa. The GP took a 5 mm biopsy of this lesion, which was reported as a superficial spreading melanoma with a Breslow thickness of 0.6 mm. There was a family history of a brother age 80 and a son aged 23 both succumbing to melanoma with cerebral metastases.
The patient was referred to a surgeon and wide margin excision was discussed, but she declined to undergo surgery and subsequently purchased black salve via the Internet, applying it to the melanoma under a closed dressing for 24 hours. This caused localized inflammation and ulceration, and the ulcer reportedly healed over a period of six to eight weeks. In 2011, five years later, when the patient presented for a routine skin check, a small dark blue firm nodule with surrounding skin discoloration was noticed on her right calf at the site of the biopsied melanoma (Figure 1A). Arrangements were made for an excisional biopsy, but the patient did not attend.
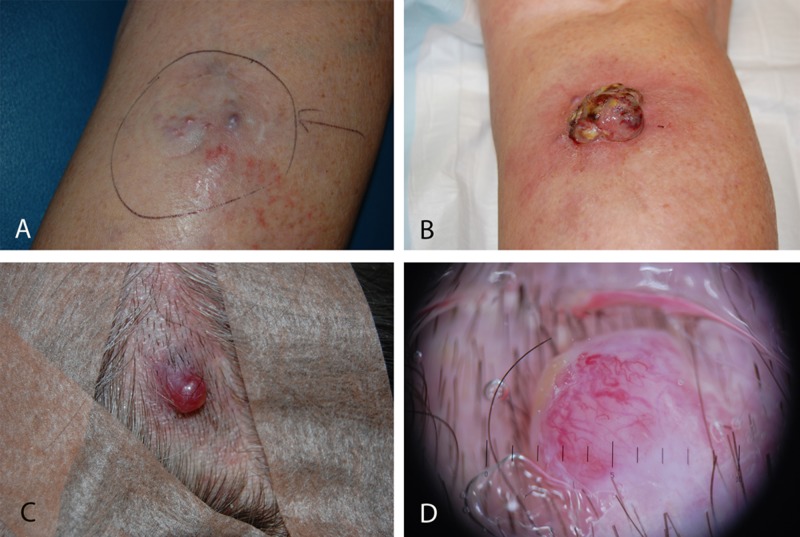
Figure 1.
(A) A nodule on the right calf where a biopsy five years earlier discovered thin invasive melanoma; (B) Image of the site shown in Figure 1A five months later; (C) Metastatic melanoma skin deposit on the scalp; (D) Dermatoscopy image of the lesion shown in Figure 1C. [Copyright: ©2014 Sivyer et al.]
Five months later the patient re-presented with a fungating nodular lesion in the right calf (Figure 1B). A provisional diagnosis was made of melanoma with a nodular component and after discussion with the patient she was referred to a surgeon for excision of the lesion and consideration of sentinel node biopsy. The patient did not attend these appointments but purchased black salve via the Internet and applied it to the lesion. Three weeks later the patient re-presented to her GP with a large eschar on her right calf that was removed to reveal an ulcer and a pink nodule with surrounding erythema.
In February 2013 (i.e., seven years after her original presentation with melanoma) the patient developed edema of her right lower leg and consulted with a different GP who referred her to a different surgeon. This surgeon found a hard craggy mass in her right inguinal region and was of the opinion that the mass was responsible for the lower leg edema by virtue of pressure on the inguinal veins and lymphatics. The patient agreed to surgical removal of the 60 × 50 mm fungating lesion on her right calf with a split skin graft to cover the defect. She also agreed to a fine needle aspiration (FNA) of the mass in her right groin.
Histopathology of the mass removed from the right calf revealed ulcerated nodules of metastatic or in-transit malignant melanoma with apparent complete local excision.
The FNA of her right groin revealed histological appearances consistent with a melanoma deposit in a lymph node.
Four months later a nodular lesion on the scalp, which the patient regarded as a cyst (Figures 1C and 1D), was removed surgically and histology revealed melanocytic proliferation with numerous dermal mitoses consistent with a metastatic deposit.
The patient agreed to radiotherapy in an attempt to shrink the right inguinal mass to relieve the peripheral edema of her right leg and underwent a course of 10 treatments with subsequent partial resolution of the edema.
In August 2013 the patient agreed to further investigations and a CT PET scan was performed. This revealed lesions consistent with metastatic melanoma “…involving the lungs, liver, right groin, subcutaneous tissues and musculature…” (Figure 2).
Figure 2.
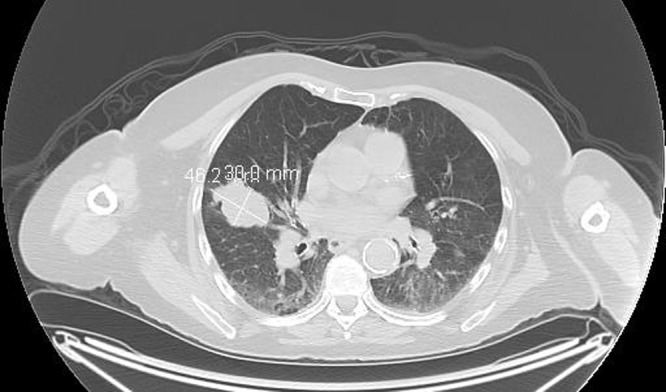
PET CT scan of the chest showing lesions consistent with metastatic melanoma in the right lung. [Copyright: ©2014 Sivyer et al.]
Evidence of persistent disease has continued with a large mass arising adjacent to the site of the original tumor on the right calf, photographed in November 2013 (Figure 3).
Figure 3.

A photograph taken in November 2013, seven years after a thin melanoma on the patient’s right calf was treated with black salve, shows a large ulcerated mass adjacent to a skin graft marking the site of local excision performed in February 2013. [Copyright: ©2014 Sivyer et al.]
Conclusions
One other case of black salve being used to treat melanoma has been reported in the literature. The male patient in that case treated a nodule on the right chest wall with the application of black salve. Because the lesion continued to grow and ulcerate, he presented to a hospital emergency department eight months following the initial black salve application. Biopsy of the lesion at that time confirmed melanoma. A CT scan showed a nodule in the lung, but metastatic melanoma was not confirmed histologically in that case study [1].
The exact composition of black salve varies but common ingredients are zinc chloride and powdered bloodroot from the bloodroot plant, Sanguinaria canadensis [2]. During the 1930’s to 1950’s a similar compound was used by Dr. Fred Mohs to fix tissue prior to surgical excision but this method has subsequently been replaced by fresh tissue excision [2]. Mohs’ original formula included zinc chloride, bloodroot and antimony sulphide [3]. The ingredient zinc chloride is a strong escharotic and has been used for the debridement of chronic leg ulcers and for chemo-surgical debridement of osteolytic bone [4]. The other major ingredient Sanguinaria canadensis is a perennial flowering plant native to North Eastern America and the ingredient is known colloquially as bloodroot, Indian Paint and redroot [2]. When the root is harvested and cut, a red liquid drains which thickens to a paste. This paste is also a strong escharotic and has been used by indigenous Americans to treat warts, polyps and moles [2]. The active ingredient in the bloodroot rhizome is a benzyl isoquinolone alkaloid [BIA]. BIA’s are a diverse group of specialized plant metabolites that includes approximately 2,500 known structures including the narcotic analgesics morphine and codeine. Sanguinarine contains antimicrobial properties [5], and invitro studies show that it also contains potent anti-cancer properties [6]. A recently published research article has shown that sanguinariine is a rapid inducer of melanoma caspase-dependent cell death that is mediated by oxidative stress [7]
Despite arguable molecular rationale for the topical application of these natural compounds, preclinical and clinical data in this field are still scant and no controlled clinical trial has yet been published demonstrating any relevant clinical efficacy.
One brand of black salve, Cansema (manufacturer Omega Alpha Labs), is marketed on the Internet as “…a miraculous product with a miraculous history with roots that go back to the late 19th century.” The advertisement goes on to state: “Only suppression and greed have prevented its enormous benefits from being made available to the mainstream” [8]. Many testimonials praising the results of Cansema are also listed on the Internet [9]. It is likely that some patients researching cancer treatments on the Internet might not be aware that testimonials are not valid scientific proof. It has been argued by one author that “When they read that the Mohs technique offers the highest known cure rate for skin cancer and that the salve for sale is identical to Dr. Mohs’ original formula it is fair to assume that some will infer that the salve available for sale produces the stated cure rates” [3].
The Australian Government has issued warnings to consumers about the use of black and red salves in treating cancer and, in an authoritative warning, states, “The TGA is not aware of any credible, scientific evidence which shows that any black or red salve preparation is effective in treating cancer” [10].
The case presented here involves a patient who, having had an initial diagnosis of thin invasive melanoma, decided to follow the option of an alternative cancer treatment rather than conventional evidence based treatment.
The reason the patient gave for seeking alternative treatment in 2006 was the cost of immediate surgical management in the Australian private health system. When she failed to attend this private appointment, her GP contacted her. The GP then arranged for her to be seen in the local public hospital at no cost, though there was going to be a delay of a couple of weeks for the appointment. Once again the patient did not attend this appointment. At that time the patient was reportedly also encouraged by an acquaintance to use black salve.
It is speculation, but perhaps having witnessed the death of her brother at age 80 and her own son at age 23 from cerebral metastatic melanoma, the patient was in denial of her own disease. As it turned out, there was a time delay of seven years before she agreed to conventional management of her melanoma.
During this time there were consultations with three GPs, three surgeons, one dermatologist, one radiologist and an oncologist. The patient exercised the undisputed right to follow the treatment regimen of personal choice. Over a period of seven years the disease progressed both locally and systemically. It is not known whether distant metastases were already present at the time of original diagnosis, but based on the staging of the tumor (Stage 1), the prognosis for 10-year disease-free survival was 87.9% [11]. Ten-year survival prognosis for Stage 4 melanoma (lung metastases) is 2.5% [11].
We believe it is essential that patients are adequately informed about evidence-based treatment and warned about the potential adverse consequences associated with an alternative treatment regimen but we also believe that support should continue to be provided regardless of choices made.
Footnotes
Funding: None.
References
- 1.Cienki JJ, Zaret L. An Internet misadventure: bloodroot salve toxicity. J Altern Complement Med. 2010;16(10):1125–7. doi: 10.1089/acm.2010.0140. [DOI] [PubMed] [Google Scholar]
- 2.Mohs FE. Mikhail GR. Mohs Micrographic Surgery. Philadelphia: WB Saunders; 1991. Origins and progress of Mohs micrographic surgery; pp. 1–3. [Google Scholar]
- 3.Elston DM. Escharotic agents, Fred Mohs, and Harry Hoxsey. J Am Acad Dermatol. 2005;53:523–5. doi: 10.1016/j.jaad.2005.04.091. [DOI] [PubMed] [Google Scholar]
- 4.Jellinek N. Escharotic and other botanical agents for the treatment of skin cancer: A review. J Am Acad Dermatol. 2005;53:487–95. doi: 10.1016/j.jaad.2005.04.090. [DOI] [PubMed] [Google Scholar]
- 5.Mitscher LA, Park YH, Clark D, et al. Antimicrobial agents from higher plants. An investigation of Hunnemannia fumariaefolia. Pseudoalcoholates of sanguinarine and chelerythrine. Lloydia. 1978;41:145–50. [PubMed] [Google Scholar]
- 6.Han MH, Park C, Clark D. Apoptosis induction of human bladder cancer cells by Sanguinarine through reactive oxygen species-mediated up-regulation of early growth response Gene-1. PLOS ONE. 8(5):e63425. doi: 10.1371/journal.pone.0063425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Burgeiro A, Bento A, Gajate C, et al. Rapid human melanoma cell death induced by sanguinarine through oxidative stress. Eur J Pharmacol. 2013;705(1–3):109–18. doi: 10.1016/j.ejphar.2013.02.035. [DOI] [PubMed] [Google Scholar]
- 8.Cansema www.altcancer.com/cansema.htmAccessed October 20, 2013.
- 9.Cansema www.altcancer.com. Accessed October 20, 2013.
- 10.Australian Government Department of Health and Ageing Therapeutic Goods Administration. Black and red salves in treating cancer. www.tga.gov.au/safety/alerts-medicine-black-salve-120203.htm. Accessed October 20, 2013.
- 11.Aitken JF, Barbour A, Burmeister B, et al. Clinical Practice Guidelines for the Management of Melanoma in Australia and New Zealand. Sydney, Australia: Cancer Council Australia; Australian Cancer Network; Ministry of Health, New Zealand; 2008. p. 159. [Google Scholar]