Abstract
Objective:
The objective of our study was to evaluate the effect of the STOP STEMI© medical application on door-to-balloon (D2B) time in patients arriving to our emergency department with an acute ST Elevation Myocardial Infarction (STEMI). STOP STEMI© is a novel medical application developed by physicians to improve the coordination and communication tasks essential to rapid assessment and care of the patients suffering from a STEMI.
Methods:
We conducted a retrospective before and after review of the Good Shepherd Health System STEMI quality assurance/improvement dashboard for a 10-month period between November, 2012 and September, 2013 (4 months before STOP STEMI© and 6 months after). Data was collected using a standard data collection form and entered on the dashboard by a STEMI coordinator blinded to study objectives. We calculated the average D2B times before and after initiation of STOP STEMI© along with the improvement in the benchmarks of D2B less than 90 min and D2B less than 60 minutes. A subgroup analysis of Center for Medicare and Medicaid services (CMS) reportable cases was conducted to evaluate these benchmarks in the subset of patients meeting the criteria for CMS reporting by our facility.
Results:
During the study period, we received 155 STEMI patients, average 0.5 patients per day. One hundred twelve of the patients underwent percutaneous coronary intervention (PCI), 37 preSTOP STEMI©, and 75 postSTOP STEMI©. Of the 112 PCI cases, 7 were excluded leaving 105 cases for analysis, 36 preapplication and 69 postapplication. We found a 22% reduction in the average door-to-balloon time after implementing the STOP STEMI© application (91–71 minutes) respectively, the average difference of 20 minutes P = 0.05 (95% CI, -1–40minutes). In the analysis of CMS reportable cases (n = 64 cases), we observed a decrease in the average D2B of 15 minutes (68–53 minutes), a 22% reduction P = 0.03 (95% CI 1–29min). In the CMS reportable cases, we saw an improvement in the D2B time less than 90 minutes from 78–95% and less than 60 minutes D2B improvement from 56–80%. We also observed an appropriate absolute reduction in PCI resource utilization by 11%.
Conclusions:
In this cohort of patients, the utilization of STOP STEMI© decreased the average door-to-balloon times by 22% in the patients with acute STEMI arriving at our emergency department. This effect was maintained when looking at the subset of all STEMI cases reportable to CMS. We also observed modest improvements in meeting the less than 60-minute, less than 90-minute benchmarks, and improvements in the resource utilization.
Keywords: STEMI, STOP STEMI©, percutaneous coronary intervention, door-to balloon-time
We sought to determine if implementation of the STOP STEMI© medical application would improve door-to-balloon (DTB) times in the patients presenting with a STEMI to our level II emergency department (ED) (Figure 1). Our ED is part of a community medical center with an annual volume of 90,000.
FIGURE 1.
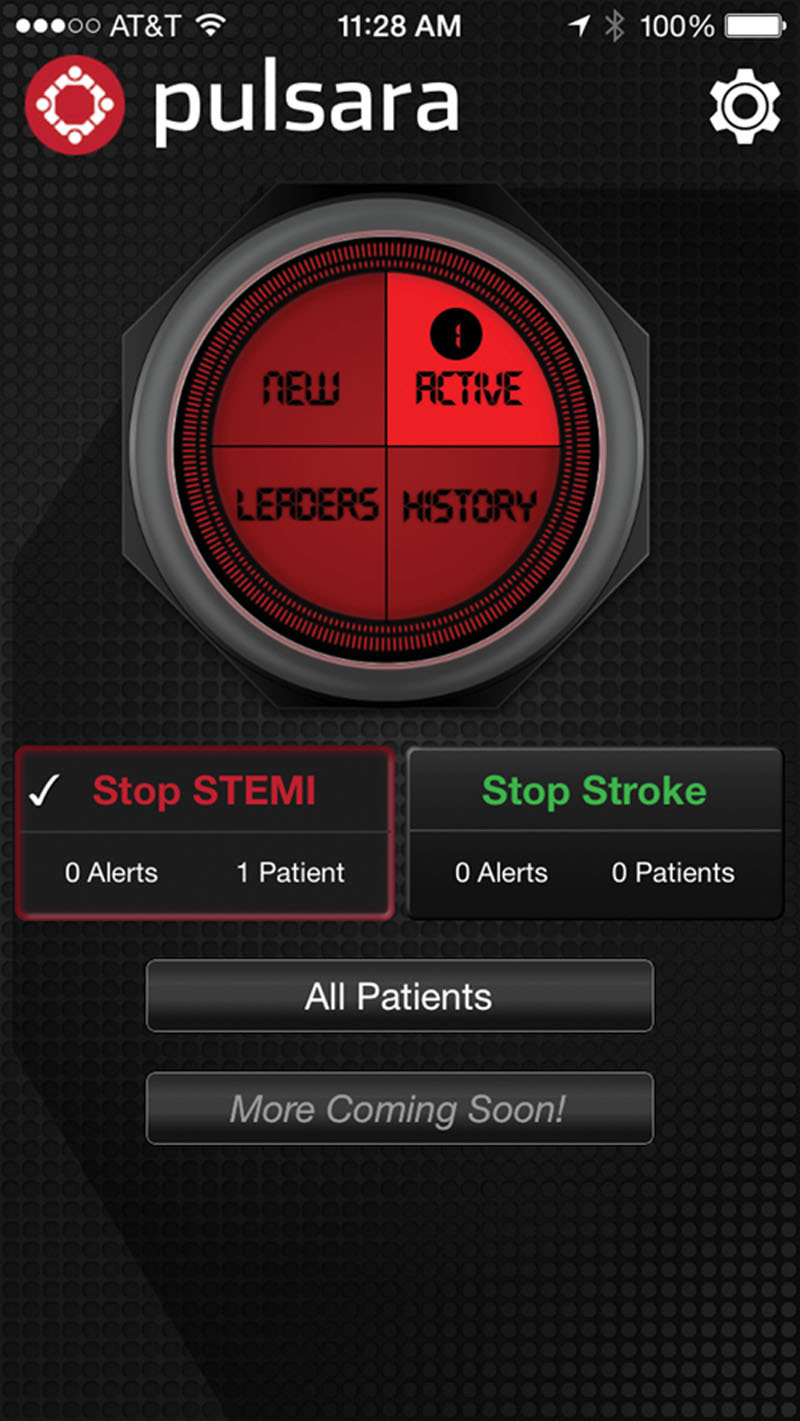
STOP STEMI© home screen.
STOP STEMI© is a novel medical application developed by physicians to enhance the coordination and communication tasks essential to the rapid assessment and care of the patients suffering from a STEMI. Medical personnel activate the application when a STEMI identified (Figure 2). An image is taken of the electrocardiogram (ECG) and, along with the patient details, transmitted to all pertinent members of the STEMI care team (Emergency Medical Services [EMS], ED, catheterization laboratory personnel, cardiologist on call, etc.). These members are immediately alerted by a siren tone on the application and have immediate access to the ECG and relevant patient information in real time (Figure 3).
FIGURE 2.
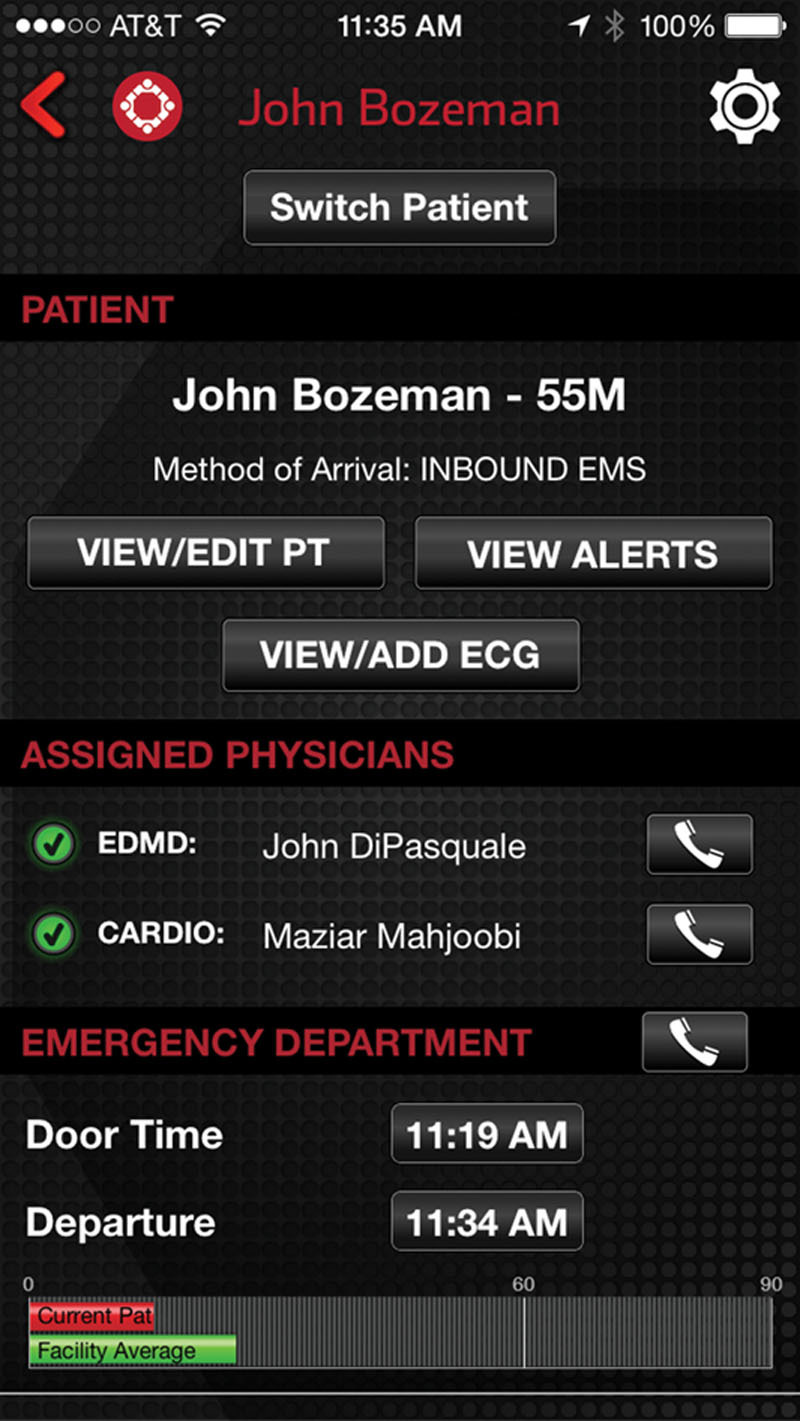
STOP STEMI© patient screen.
FIGURE 3.
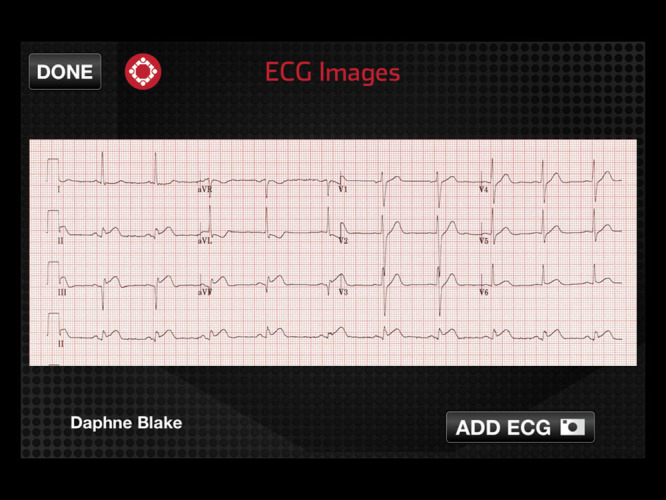
STOP STEMI© ECG.
When each link in the care team is ready to receive the patient, they can update their readiness status on the application to facilitate coordination of care (Figure 4). The application has a universal clock that promotes a sense of urgency among all stakeholders. No specialized hardware is required as the application is compatible with smartphones and tablets. (see supplemental digital content 1, STOP STEMI© introduction video)
FIGURE 4.
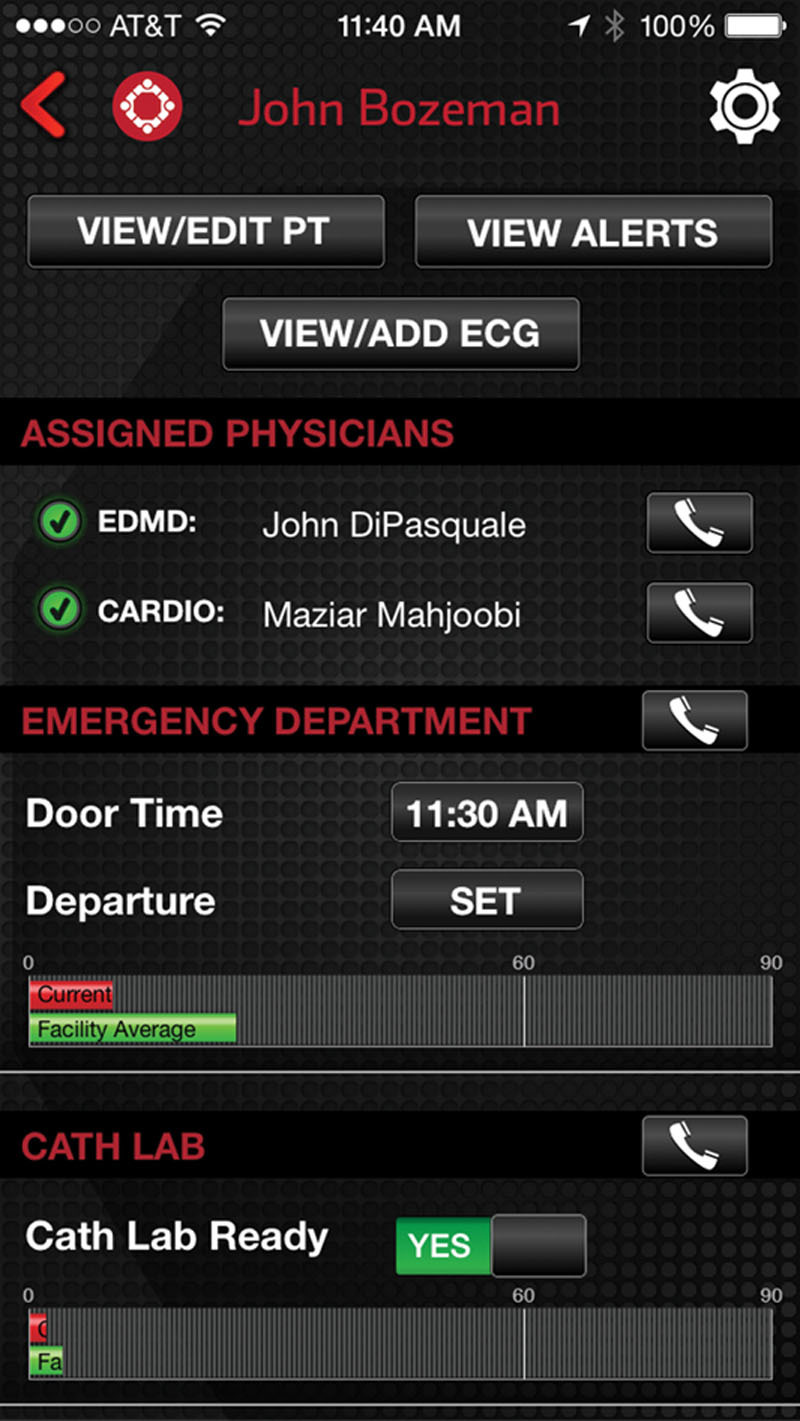
STOP STEMI© cath lab ready.
STOP STEMI has several additional benefits. This application tracks the healthcare provider performance compared to the standard benchmarks for quality improvement monitoring. There are also significant resource utilization advantages. Because physicians can rapidly review ECG findings, appropriate modifications to EMS and inhospital STEMI activations can be made rapidly. STOP STEMI© also provides immediate feedback on elapsed time inasmuch as activation by utilizing a universal clock comparing the current case against national benchmarks.
Methods
The data was abstracted by the Good Shepherd Health System STEMI coordinator from the medical records using a standardized abstraction form and entered into a quality improvement database (Good Shepherd STEMI portal). We included any patient arriving by EMS or private vehicle to the emergency department with an acute STEMI who received PCI therapy between November 04, 2012 to September 29, 2013. The STEMI coordinator used a standard abstraction form and was blinded to study the objectives. The study includes all available data from the STEMI dashboard 4 months before the initiation of STOP STEMI© (November 04, 2012–March 4, 2013) and 6 months after the application was introduced (March 5, 2013–9/29/2013). Investigators used the recorded door and device times on the STEMI dashboard. Data was analyzed using Excel software statistics package (paired 2 tailed student’s t test). All eligible PCI cases were analyzed for this report and subgroup analysis was done on all the cases that met the criteria for Centers for Medicare Services (CMS) reporting. The subgroup contained patients who arrived with STEMI and received PCI that met CMS criteria for reporting. These requirements exclude complicated cases requiring interval resuscitation, pacemaker placement during STEMI, and other confounders that exclude them from being reported to CMS for benchmarking purposes. This study received Institutional Review Board approval from the University of Texas Health Science Center Tyler.
Results
During our study period, 155 cases arrived with STEMI and 112 patients received PCI (72% of the total cases). Seven cases were not included in the analysis: 4 of these were inpatients and 3 (1 preapp and 2 postapp) and had insufficient data to determine D2B time, leaving 105 cases for analysis. In the 4 months before the STOP STEMI (November, 2012–March, 2013) there were 48 cases, 36 received PCI with a mean D2B time of 91 minutes. In the postapplication period (March, 2013–September, 2013) there were 107 cases, 69 with PCI. The mean D2B time postapplication was 71 minutes, representing a 20 minute (22% improvement) in D2B time from preapplication P = 0.05 (95% CI, -1–40 minutes). When analyzing the PCI cases that were reported to CMS (N 64), 23 preapplication and 41 postapplication, we observed a 22% reduction in D2B time of 15 minutes (68–53 minutes after the app) P < 0.05 (95% CI 1–29minutes). The percentage of PCI with D2B<90 minutes and D2B<60 minutes improved from 78–95% and 56–80%, respectively. The utilization was improved with a reduction in the rate of PCI on activated cases from 75–64%, representing 11% absolute reduction in PCI utilization after initiating the application.
Conclusions
In this cohort of patients, STOP STEMI© decreased average D2B times by 22% in the patients with acute STEMI arriving at our ED. This effect was maintained when looking at the subset of all STEMI cases reportable to CMS. We also observed modest improvements in meeting the less than 60-minute and less than 90-minute benchmarks along with improved resource utilization.
Discussion
It is clear from the existing literature that outcomes for STEMI patients are optimized when D2B times are less than 90 minutes. (AHA class one recommendation, 1–4) Multiple studies also correlate improved mortality rates by decreasing D2B times.1–5 A compelling review of a large cardiovascular registry (10,965 patients) found that the median D2B time was 96 minutes with only 44% of the patients meeting the <90-minute national benchmark goal.6 Several other trials have also demonstrated that a high percentage of STEMIs do not meet the 90-minute D2B benchmark.1,3,6–9
In a 2000 study published in JAMA (27,080 patients), mortality increased by 41% for patients with D2B times over 120 minutes. After adjustments for baseline patient demographic data, hospital mortality significantly increased as D2B times increased.9 These results have been consistently replicated in other clinical trials, demonstrating an inverse relationship between D2B time and survival independent of symptom onset and the presence or absence of cardiovascular risk factors.1,3 Furthermore, it has been recommended that because catheterization laboratory activation time is critical component to decreasing door-to-balloon time, institutions should adopt and customize tools to optimize this metric.10
Shoholz et al in 2008 investigated the effect of formalized systems of STEMI care education and data feedback on D2B times. During the 3 study periods with formalized feedback, D2B times showed a modest decrease, demonstrating the impact of staff education and feedback on streamlining this process.11 A similar study in 2012, looked at the effect of a streamlined referral protocol for patients requiring transfer from an outside facility for STEMI. This protocol reduced the D2B time from 122 minutes to 101 minutes. The authors concluded that coordinated systems of STEMI care improve patient outcomes.12
STOP STEMI© enhances coordination and communication among providers beginning at the point of care. In this series of patients, the application had a significant impact on D2B times for patients suffering an acute STEMI. Our institution’s processes for coordinating STEMI care before the initiation of the application yielded an average D2B times of 91 minutes and 78% of CMS reportable cases meeting the national standard of <90 minutes. Our former process was based on emergency physician activation of cardiac catheterization laboratory resources. Once STEMI is identified; the ED, cardiology on call, house supervisor and cardiac catheterization laboratory team members are activated by pager from the unit clerk on duty. We utilize prehospital EMS ECG technology as well for more efficient EMS activated STEMI. Our system has a dedicated STEMI coordinator (RN) who conducts a quarterly catheterization laboratory meeting. This meeting provides detailed feedback on benchmarks, fall out cases and feedback to representatives from EMS, cardiology and the ED for a system of ongoing quality performance and improvement. STOP STEMI© significantly improved our already successful operational model. It is quite possible that the positive effect of STOP STEMI© may have greater impact in systems with less developed acute STEMI care processes. Our data include all PCIs regardless of their eligibility for reporting to CMS. Some of the cases excluded from CMS reporting include those with interval cardiac arrest before PCI, pacemaker placements or transfer from an outside facility. All of these confounders should greatly increase the D2B times. The application seems to perform well even when applied to this difficult mix of cases with a 22% improvement in D2B times. When isolating the subset of cases reported to CMS, STOP STEMI© improved D2B times by 22% and improved the percentage of cases meeting the <90 minute guideline from 78% to 95%. Additionally the goal of D2B <60 minutes in CMS reportable cases improved from 56% to 80% after initiating the STOP STEMI© application.
McCabe et al studied 411 cardiac catheterization laboratory activations for STEMI and found 36% false positive rate of activation.13 Our findings suggest decreased utilization of PCI resources after implementation of STOP STEMI©. The reported facility costs for cardiac PCI is $3067 per case.14 Using STOP STEMI© during this study period could potentially result in utilization savings of approximately $171,138 during the study period [(155 activations) (0.36 false positive activation rate) ($3067/case)].
We recognize that there are some limitations to the findings reported in this investigation. We utilized a retrospective design, which has inherent biases. The data, however, are compelling given the low cost and safety of this intervention. We do plan on prospectively evaluating the performance of STOP STEMI© in our patient population. Our trial is also limited by a small sample size resulting in a lack of statistical significance in the main study group. Despite this limitation, our results for CMS reportable cases are statistically significant, most likely due to the magnitude of the differences found. Finally, our conclusions are based on the data collected at a high volume community based ED that may not be generalizable to other centers. Prospective multicenter investigations are needed to fully evaluate the impact of this medical application on D2B times and patient outcomes for STEMI.
DISCLOSURES
Nothing to declare.
References
- 1.Saif SR, Jeptha PC, Jersey C, et al. Association of door-to-balloon time and mortality in patients admitted to hospital with ST elevation myocardial infarction: national cohort study. BMJ. 2009;338:b180. doi: 10.1136/bmj.b1807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hiroki S, Yoshihisa N, Takeshi M, et al. Association of onset to balloon and door to balloon time with long -term clinical outcome in patients with ST elevation acute myocardial infarction having primary percutaneous coronary intervention: observational study. BMJ. 2012;344:e3257–e3257. doi: 10.1136/bmj.e3257. [DOI] [PubMed] [Google Scholar]
- 3.Robert LM, Yongfei W, Jeph H, et al. Effect of door-to-balloon time on mortality in patients with ST-segment elevation myocardial infarction. J Am Coll Cardiol. 2006;47:2180–2186. doi: 10.1016/j.jacc.2005.12.072. [DOI] [PubMed] [Google Scholar]
- 4.Frederick GK. 2009 focused updates: ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction (updating the 2004 guideline and 2007 focused update) and ACC/AHA/SCAI guidelines on percutaneous coronary intervention (updating the2005 guideline and 2007 focused update) a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. JACC. 2009;54(:2205–2241. doi: 10.1016/j.jacc.2009.10.015. [DOI] [PubMed] [Google Scholar]
- 5.Giuseppe DL, Harry S, Jan PO, et al. Time delay to treatment and mortality in primary angioplasty for acute myocardial infarction: every minute of delay counts. Circulation. 2004;109:1223–1225. doi: 10.1161/01.CIR.0000121424.76486.20. [DOI] [PubMed] [Google Scholar]
- 6.Rajendra HM, Vincent JB, Wenqin P, et al. Achieving rapid reperfusion with primary percutaneous coronary intervention remains a challenge: insights from American Heart Association’s get with the guidelines program. AM Heart J. 2008;155:1059–1067. doi: 10.1016/j.ahj.2008.01.010. [DOI] [PubMed] [Google Scholar]
- 7.Roberto JC, Igor FP, James CB, et al. Outcome of patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention during on- versus off-hours. Am J Cardiol. 2013;111(7):946–954. doi: 10.1016/j.amjcard.2012.11.062. [DOI] [PubMed] [Google Scholar]
- 8.Andrew PR, Fredric MH, Damon K. Decreasing door-to-balloon times via a streamlined referral protocol for patients requiring transport. Am J Emerg Med. 2013(3):499–503. doi: 10.1016/j.ajem.2012.09.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Christopher PC, Gibson CM, Costas TL, et al. Relationship of symptom-onset-to-balloon time and door-to-balloon time with mortality in patients undergoing angioplasty for acute myocardial infarction. JAMA. 2000;283:2941–2947. doi: 10.1001/jama.283.22.2941. [DOI] [PubMed] [Google Scholar]
- 10.James MM, Ehrin JA, Kurt S, et al. Impact of door-to-activation time on door-to-balloon time in primary percutaneous coronary intervention for ST-segment elevation myocardial infarctions a report from the Activate-SF Registry. Circ Cardiovasc Qual Outcomes. 2012;5:672–679. doi: 10.1161/CIRCOUTCOMES.112.966382. [DOI] [PubMed] [Google Scholar]
- 11.Karl HS, Reinhard H, Dorothe A, et al. Contact-to-balloon time and door-to-balloon time after initiation of a formalized data feedback in patients with acute ST-elevation myocardial infarction. Am J Cardiol. 2008;101:46–52. doi: 10.1016/j.amjcard.2007.07.078. [DOI] [PubMed] [Google Scholar]
- 12.Michel RL, George AW, Derek YS, et al. Reduction in mortality as a result of direct transport from the field to a receiving center for primary percutaneous coronary intervention. J Am Coll Cardiol. 2012;60:1223–1230. doi: 10.1016/j.jacc.2012.07.008. [DOI] [PubMed] [Google Scholar]
- 13.McCabe JM, Armstrong EJ, Kulkarni A, et al. Prevalence and factors associated with false-positive ST-segment elevation myocardial infarction diagnoses at primary percutaneous coronary intervention–capable centers: a report from the Activate-SF registry. Arch Intern Med. 2012;172:864–871. doi: 10.1001/archinternmed.2012.945. [DOI] [PubMed] [Google Scholar]
- 14.Weintraub WS, Mahoney EM, Zhang Z, et al. One year comparison of costs of coronary surgery versus percutaneous coronary intervention in the stent or surgery trial. Heart. 2004;90:782–788. doi: 10.1136/hrt.2003.015057. [DOI] [PMC free article] [PubMed] [Google Scholar]


