Abstract
Primary malignant melanoma of the lung is a very rare disease with about 40 cases reported in English literature. We report a 49-year-old female with history of 2 month chest pain who was revealed to have a peripheral lung mass in left upper lobe by chest CT scan. Left upper lobectomy was performed and post-operative pathology revealed to be primary malignant melanoma of the lung. 4 months after operation, a node in right breast was found by patient herself and needle aspiration biopsy revealed to be breast cancer. The patient refused any diagnostic and therapeutic procedure and died of extensive metastasis 3 months later. Primary malignant melanoma of the lung is highly malignant disease with poor prognosis in most patients.
Keywords: Primary malignant melanoma of the lung (PMML), lobectomy, pathology, metastasis
Case report
A 49-year-old female was admitted to our department with complaints of mild chest pain, no any other respiratory symptoms. The symptom started 2 months ago, and CT scan of chest revealed a peripheral lung mass in left upper lobe and severe spinal deformity of coronal curve (Figure 1). No positive signs besides obvious coronal spinal curve deformity were found on physical examination. Enhanced CT scan of head, chest, upper abdomen and 99mTc HDP bone scan were performed and distant metastasis was excluded. Routine pre-operative evaluation revealed that the patient was good surgical candidate without major co-morbidities. Thoracotomy and left upper lobectomy was performed. The patient recovered well after operation and was discharged home on 10th post-operative day. Pathological study proved to be primary malignant melanoma of the lung (PMML), with immunohistochemistry revealing the tumor to be positive for melanocyte makers HMB-45, MELAN-A and S-100 (Figure 2), while negative for E1/AE3 (PCK), CK20, CK5/6/7 and TTF-1. Careful thorough skin examination was repeated to exclude skin malignant melanoma.
Figure 1.

CT scan of the chest demonstrates a lobulated mass in the left upper lobe.
Figure 2.
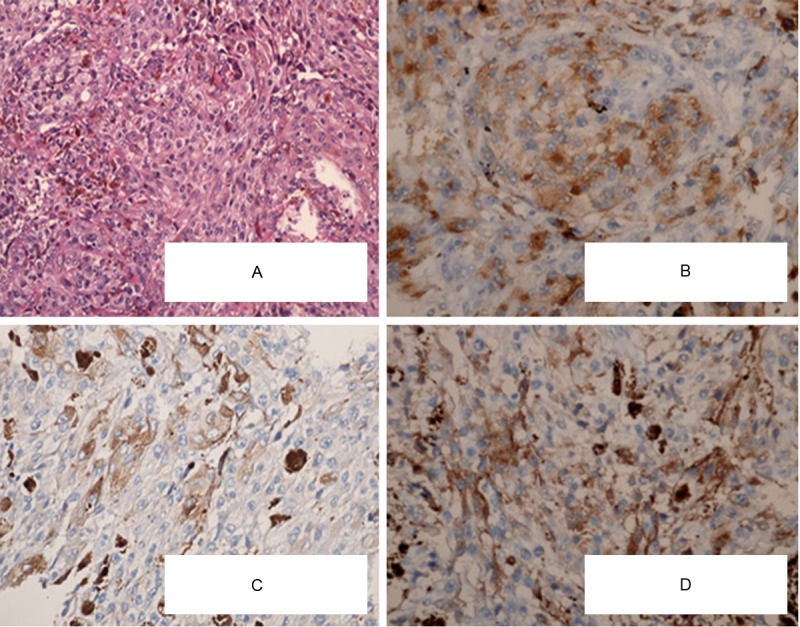
Histopathological findings. A: Tumor consisted of malignant epithelial tumor cells and spindle cells with large amounts of acidophilic cytoplasm and prominent nucleoli (HE, original magnification ×200). B: Immunohistochemical staining for HMB-45 is positive (Original magnification ×200). C: Immunohistochemical staining for M-A is positive (Original magnification ×200). D: Immunohistochemical staining for S-100 is positive (Original magnification ×200).
The patient was closely followed-up after surgical treatment, receiving no chemo-therapy or radio-therapy. 4 months after operation, the patient came to hospital because of a node in right breast, needle aspiration biopsy of breast node revealed to be breast cancer (Figure 3). A whole body 18F-FDG PET-CT and surgical resection was strongly suggested but the patient refused any kinds of diagnostic and therapeutic procedures. 3 months later, the patient died of extensive metastasis of PMML.
Figure 3.
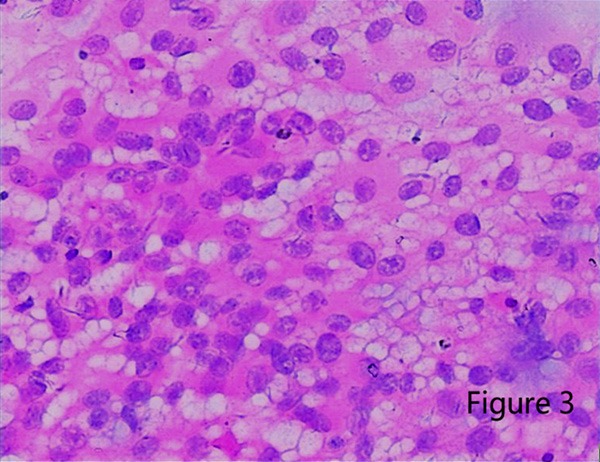
4 months after operation, a node in right breast was found and needle aspiration biopsy revealed to be breast cancer (Original magnification ×200).
Discussion
Most malignant melanomas originate from melanocytes in skin, while occasionally begin in some other pigmented tissues, such as in choroid of the eye, oral cavity, vagina or in digestive tract [1-3]. Primary malignant melanoma of the lung is very rare. To date, only about 40 cases have been reported in English literature [4-6]. The accurate mechanism of PMML is not clear yet, although it is speculated that PMML arises from some epithelial cells of squamous metaplasia that have undergone differentiation towards melanocytes.
Usually, PMML manifests with symptoms of chest pain, cough, hemoptysis, obstructive pneumonia, or atelectasis and so on. However, none of theses manifestations is specific. They are shared with many other respiratory diseases. Furthermore, some PMML are incidentally found just on routine chest radiography without any symptoms and signs. Most PMML cases are diagnosed by pathological studies after operation. Jensen proposed that diagnostic criteria for PMML should include the following: 1) Junctional changes like “dropping off” or “nesting” of melanoma cells just beneath the bronchial epithelium; 2) Invasion of the bronchial epithelium by melanoma cells; 3) Malignant melanoma associated with these epithelial changes; 4) A solitary lung tumor; 5) No history of a cutaneous, mucous membrane or ocular melanoma; 6) Absence of any other detectable tumor at the time of diagnosis [7]. The presented case met all the aforementioned diagnostic criteria when originally diagnosed. The breast node that was found 4 months after operation was more likely to be metastatic tumor from PMML, although needle aspiration biopsy revealed to be breast cancer. HE stain revealed that cells in breast node were morphologically similar to those in lung mass.
Evidence shows only underwent surgical resection cases with PMML had chances of long term survival, although some surgically treated patients died of metastasis and relapse within 1 years after operation [8], including our patient. So, for PMML patients without detectable distant metastasis, surgical resection provides the optimal choice of treatment. No convincing evidence showed benefits of postoperatively chemotherapy or radiotherapy yet, because of inadequate cases of this disease.
References
- 1.Jovanovic P, Mihajlovic M, Djordjevic-Jocic J, Vlajkovic S, Cekic S, Stefanovic V. Ocular melanoma: an overview of the current status. Int J Clin Exp Pathol. 2013;6:1230–1244. [PMC free article] [PubMed] [Google Scholar]
- 2.Kumar A, Bindal R, Shetty DC, Singh HP. Primary oral malignant melanoma: Clinico- pathological series of four cases. Dent Res J (Isfahan) 2012;9:338–344. [PMC free article] [PubMed] [Google Scholar]
- 3.Szumilo J, Dabrowsk A. Primary esophageal malignant melanoma. Pol J Pathol. 2011;62:148–151. [PubMed] [Google Scholar]
- 4.Testin M, Trabucco S, Di Venere B, Piscitelli D. Ileal intussusception due to intestinal metastases from primary malignant melanoma of the lung. Am Surg. 2002;68:377–379. [PubMed] [Google Scholar]
- 5.Wilson RW, Moran CA. Primary melanoma of the lung: a clinicopathologic and immunohistochemical study of eight cases. Am J Surg Pathol. 1997;21:1196–1202. doi: 10.1097/00000478-199710000-00010. [DOI] [PubMed] [Google Scholar]
- 6.Gong L, Liu XY, Zhang WD, Zhu SJ, Yao L, Han XJ, Lan M, Li YH, Zhang W. Primary pulmonary malignant melanoma: a clinicopathologic study of two cases. Diagn Pathol. 2012;7:123. doi: 10.1186/1746-1596-7-123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jensen OA, Egedorf J. Primary malignant melanoma of the lung. Scand J Respir Dis. 1967;48:127–135. [PubMed] [Google Scholar]
- 8.Pan XD, Zhang B, Guo LC, Gu DM, Mao YQ, Li J, Xie Y, Wang L. Primary malignant melanoma of the lung in the elderly: case report and literature review. Chin Med J (Engl) 2010;123:1815–1817. [PubMed] [Google Scholar]


