Abstract
About one third of adolescents in the USA are overweight and/or obese. Obesity during the adolescent years is associated with many adverse health consequences, including type 2 diabetes, hypertension, hyperlipidemia, and psychosocial problems. Because of substantial advances in technologies and wide acceptance by adolescents, it is now possible to use technology for healthy weight management and prevention of obesity. This systematic review used Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines and aimed to evaluate the existing literature reported on the effectiveness of technology-based intervention (web-based, e-learning, and active video games) in preventing obesity in adolescents. The primary aim of this review was to explore if components of specific interventions were associated with a reduction in body mass index. Research articles obtained from CINAHL, Embase, PubMed, PsycInfo, and the Cochrane database from1990 to 2014 were reviewed. A total of 131 published articles were identified, and 14 met the inclusion criteria of a randomized or nonrandomized clinical study with body mass index as primary outcome and/or secondary outcomes of diet/physical activity and/or psychosocial function, tested lifestyle interventions to prevent obesity, used technology, and studied adolescents (aged 12–18 years). The results indicated that six of 14 studies found body mass index and/or body fat decreased at short-term (less than 12 months) follow-up. Six of eleven studies that examined physical activity or physical activity-related outcomes found an improved physical activity outcome (time playing active video games and increase in physical activity time), while five of seven studies which assessed dietary outcomes indicated improvement in dietary behaviors. Five of seven studies suggested an improvement in psychosocial function (reduced depression, improved self-esteem and efficacy, improvement on Behavior Assessment Scale) in adolescents involved in the technology-based intervention. All effective interventions utilized dietary and physical activity strategies as part of intervention components. Because of the variation in duration of intervention (range 10 weeks to 2 years), it is not clear what length of intervention is most effective. Future research should assess the long-term impact of technology-based interventions and evaluate mediators and moderators for weight change in adolescents.
Keywords: technology intervention, obesity, adolescents, web-based, exer-gaming
Introduction
Obesity among adolescents has reached epidemic proportions worldwide.1 Approximately one third of adolescents in the USA are currently overweight or at risk for becoming overweight.2 Obesity in adolescence predisposes this age group to obesity in adulthood and is a major risk factor for a number of serious health conditions, including diabetes, hypertension, heart disease, stroke, osteoarthritis, and certain types of cancer.3–5 Because 80% of obese adolescents will become obese adults,6 with increased susceptibility to type 2 diabetes mellitus and cardiovascular disease,7–9 management of obesity in adolescents is critical. Many intervention studies have been conducted to address this epidemic health concern.10–12 As technology has become such an important part of daily life, especially among adolescents, technology-based interventions, including Internet-based weight management tools, social media, apps for smartphones, and active video games, have been developed as methods to prevent obesity in this age group.13–15
The most recent research suggests that 78% of adolescents in the USA have cell phones (47% smartphones), 23% have a tablet computer, and 93% have access to a computer and use one at home.12 Due to the high use of technology among adolescents, there are health promotion opportunities that include tapping into the new media channels integral to youth culture.13 The use of mobile technologies may offer a practical and reliable means of managing obesity in busy primary care clinics. In the last decade, several interventions using technology to prevent obesity have been tested in schools, in after school programs, and in the clinic setting. Few systematic reviews have been conducted to examine the impact of technology-based interventions on childhood obesity.16,17 An et al examined the effect of web-based weight management on children and adolescents,16 and Lu et al explored the effect of health video games on prevention of childhood obesity.17 The review by An et al explored multiple types of intervention, including home Internet interventions, interventions with parents, and interactive websites.16 Although their review included weight-related variables (body mass index [BMI], BMI percentile, physical activity, and diet) it included studies testing for multiple other outcomes and included various targeted populations (children, parents) which made comparison of studies difficult. In contrast, Lu et al reviewed studies that focused only on health video games in overweight or obese children.17 There is a dearth of knowledge on the impact of technology-based interventions, including both web-based and active video games, on weight management and weight-related health behaviors (physical activity, sedentary activity, and diet) in adolescents.
The purpose of this review is to assist health care providers and researchers in making more informed decisions about which types of technology-based interventions for adolescent obesity prevention are most suitable and achieve sustainable weight reduction, impact on amount of physical activity, a reduction in sedentary activity, improved dietary behaviors, and/or positive psychosocial outcomes. With the advancement of technology and the opportunity to explore the use of technology as an approach to adolescent obesity, it is important to systematically review the methodological rigor of technology-based interventions and their impact on BMI, and to identify types of interventions that work best for prevention of obesity in adolescents. The two specific objectives of this review were to evaluate the existing literature reported on the effectiveness of technology-based interventions in preventing obesity in adolescents and to explore components of these interventions that are associated with significant BMI outcomes.
Methods
Data sources
This systematic review was conducted and reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines that have been used for other obesity-related systematic reviews.18 Our search covered all available years from January 1990 to January 2014 in CINAHL, Embase, PubMed, PsycINFO, and the Cochrane Library. The bibliographies of included articles were hand-searched, and promising titles were reviewed in order to locate articles not catalogued in the major databases. If the reviewer was unable to determine if an article pertained to the study by title, then the abstract was reviewed. The search terms used were (Adiposity[mh] OR Body Mass Index[mh] OR Body Weight[mh:noexp] OR Body Weight Changes[mh] OR Obesity[mh] OR Overweight[mh] OR Weight Gain[mh] OR Weight Loss[mh] OR Weight Reduction Program[mh] OR “abdominal fat”[tiab] OR adiposity[tiab] OR bmi[tiab] OR “body mass index”[tiab] OR “body weight”[tiab] OR obese[tiab] OR obesity[tiab] OR overweight[tiab] OR “visceral fat”[tiab] OR “weight loss”[tiab] OR “weight management”[tiab] OR “weight reduction”[tiab]) AND Blogging[mh] OR Cellular Phone[mh] OR Computer-Assisted Instruction[mh] OR Computer Graphics[mh] OR Computer Systems[majr] OR Computers[majr] OR Computers, Handheld[mh] OR Educational Technology[mh] OR Electronic Mail[mh] OR Interactive Tutorial[pt] OR Internet[mh] OR Multimedia[mh] OR Software[mh:noexp] OR Technology[majr:noexp] OR Telecommunications [majr:noexp] O R Telemedicine[mh:noexp] OR Text Messaging[mh] OR User-Computer Interface[mh] OR Videoconferencing[mh] OR Video Games[mh] OR Webcasts as Topic[mh] OR Wireless Technology[mh].
To assure the quality of the study findings reported, we selected papers that used either a randomized controlled trial approach or a quasi-experimental study design. Inclusion criteria consisted of: randomized clinical trials or clinical trials without randomization or a control group; a primary outcome including BMI or BMI z-score (both self-report and measurement collected using the World Health Organization classification) and one of the health behaviors (diet and physical activity); trials that tested lifestyle/weight management interventions (through physical activity or diet modification using Internet or active video games) intended to prevent obesity or excessive weight gain; trials that tested lifestyle interventions using at least one of the eHealth/mHealth (term used for the practice of medicine and public health supported by mobile devices) intervention components including web (Internet)-based, social media, and mobile communication technology; and participants included adolescents aged from 12–18 years. Papers were excluded if they described primary prevention interventions or if the majority of participants were over 18 years of age and if the articles were published in a language other than English.
Data extraction
This systematic review compares randomized controlled trials and pre-post test (quasi-experimental) studies that utilized technology-based interventions including active video games and the Internet as interventions to decrease BMI or percent body fat. The studies focused primarily on increasing physical activity, decreasing sedentary activity, improving dietary outcomes, and/or improving diet skills (increased fruit and vegetables, decreased sugary drinks and high fat foods) as well as improving psychosocial well-being (weight concerns, self-efficacy, self-esteem, and peer support). This review involves assessing educational, behavioral, and health promotion interventions delivered through technology including web/Internet-based, social media, and mobile communication technology aimed to prevent obesity in adolescents.
Outcome variables
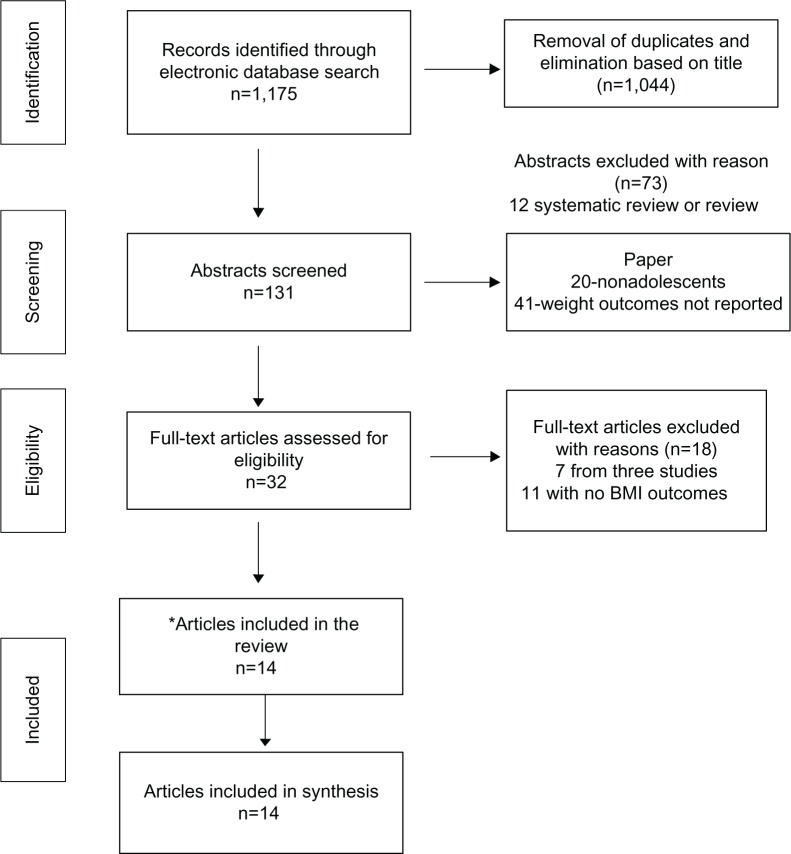
The initial search generated a total of 1,175 papers from all the search databases. To obtain rigorous scientific evidence, only randomized controlled trials and pre-post test studies were selected for this systematic review in terms of key outcomes and interventions used. One reviewer screened the study title and abstract as the first screening stage and narrowed the articles to 131 papers. Two reviewers then reviewed the abstract and narrowed the search from 131 articles to 32 articles by eliminating duplicate papers based on the same research. Articles that were nonintervention studies, such as review papers, and cross-sectional studies were also excluded. The primary outcome was reduction of BMI in adolescents with the use of technology. Studies that did not target obesity, were not technology-based, and not conducted in adolescents were excluded. Based on the inclusion criteria, two reviewers examined the full papers and identified 14 studies that met the inclusion criteria13,21–33 (see Figure 1).
Figure 1.
Preferred reporting items for systematic reviews and meta-analyses flow diagram for articles identified, screened eligible, and included in this paper.
Note: *Systematic reviews.
Abbreviation: BMI, body mass index.
The 14 studies reviewed used a variety of outcome measures, including weight-related measures (ie, BMI, BMI z-score) which were the primary outcomes reviewed in this paper, as well as several secondary outcomes including percentage of body fat, physical activity level, physical fitness, dietary intake, and psychosocial variables (ie, self-esteem, self-competence). In this review, the effects of the interventions were evaluated in terms of weight-related measurements, specifically BMI and BMI z-score, as they were used in the studies included in the review.
Intervention components
Detailed examination of the following components of effective interventions was conducted: behavior change targets, method used to effect weight changes, frequency of contact, and duration of the intervention. The effectiveness of the intervention was determined by reviewing the results of the study and reporting the study findings.
Assessment of methodological rigor
We adapted the methodological rigor assessment for the included articles from those in use by the Cochrane Effective Practice and Organization of Care Review Group and recent systematic reviews.19,20 The nine criteria were scored objectively using published data and reflect potential bias (see Table 1). Studies were rated independently by two reviewers. Disagreements were discussed until consensus was reached. Disagreement between reviewers was due to confusion in meaning of “intent to treat”, and once clarified, consensus was reached. Each item was rated as “yes” (1), “no” (0), or “not applicable”. A total methodological quality score (ranging from 0 to 9) was calculated by summing up all “yes” items. Studies were rated as having good methodological quality if they met at least 80% of the criteria (seven of nine items or five of six items).
Table 1.
Methodological rigor of included studies
| Reference | Randomization | Blinding | Inclusion/exclusion criteria clearly described | Intent-to-treat analysis used | Adequate sample size calculations shown | Adequate control group* | Standard measures described | Comparison of baseline parameters of completers versus noncompleters | 80% retention rate** | MR score |
|---|---|---|---|---|---|---|---|---|---|---|
| Adamo et al21 | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 7/9 |
| Chen et al22 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8/9 |
| Christison and Khan13 | N/A | N/A | 1 | 0 | 0 | N/A | 1 | 1 | 1 | 4/6 |
| Doyle et al23 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8/9 |
| Ezendam et al24 | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 7/9 |
| Hung et al25 | N/A | N/A | 1 | 0 | 0 | N/A | 1 | 1 | 1 | 4/6 |
| Jago et al26 | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 6/9 |
| Jones et al27 | 1 | 1 assessor | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 8/9 |
| Maddison et al28 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8/9 |
| Nguyen et al29 | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 6/9 |
| Owens et al30 | N/A | N/A | 1 | 1 | 0 | N/A | 1 | 0 | 0 | 3/6 |
| Staiano et al31 | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 6/9 |
| Wagener et al32 | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 6/9 |
| Williamson et al33 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 7/9 |
Notes:
Control group was reflective of study group in number, age, sex, ethnicity
80% of participants completed the intervention.
Abbreviations: N/A, not available; MR, methodological rigor.
Results
Effectiveness of technology-based intervention in preventing adolescent obesity
BMI/percentage body fat
Six studies (42.8%) found a significant decrease in BMI or percentage body fat after the intervention.13,23,25,27,28,33 Four Internet-based intervention studies23,25,27,33 and two active video game-based interventions13,34 reported that adolescents in the intervention group had significantly reduced BMI and/or percentage body fat immediately after the intervention or up to 9 months post intervention. Short-term effects of technology-based interventions were found (less than 12 months of follow-up) in all six studies, while one study (by Williamson et al)33 found no beneficial effect on BMI at assessment 2 years post baseline (see Table 2 for study description).
Table 2.
Study description
| Reference | Study design | Sample characteristics | Intervention/control/components | Intervention duration/follow-up | Retention rate (%)* | Outcomes | Results |
|---|---|---|---|---|---|---|---|
| Adamo et al21 | RCT | Overweight and/or obese, aged 12–17 years Total n=30 Canada |
Interactive video game cycling versus stationary cycling to music PA |
Twice weekly (60 minutes) for 10 weeks Follow-up right after the intervention |
86.1% | Body composition Metabolic profile PA and diet behavior |
No difference in all outcomes between groups, except for some exercise behaviors Minutes spent at vigorous intensity and distance pedaled were higher in the music group |
| Chen et al22 | RCT | Normal weight, overweight or obese Chinese-American 12–15 years n=54 USA |
Tailored web-based versus general health web-based information Diet/PA/SB |
Once a week for 8 weeks Follow-up at 6 months post intervention |
93% | Body composition BP PA and diet behavior Knowledge/self-efficacy |
1. No difference in body composition 2. Intervention group significantly decreased waist-to-hip ratio and DBP, increased PA vegetable/fruit intake and knowledge |
| Christison and Khan13 | Prospective Observational |
Overweight or obese 8–16 years n=48 USA |
10 weekly 2-hour sessions. Nutrition and behavior education Active video game (one hour ×10 weeks Diet/PA |
Once weekly for 10 weeks Follow-up assessment done immediately after the intervention |
83% | Body composition PA and diet behavior Psychological |
Significantly reduced BMI and BMI z-score Significantly reduced television time and soda consumption while increased PA time and eating at the table Significantly improved global self-worth and behavioral conduct |
| Reference | Study design | Sample characteristics | Intervention/control | Intervention duration/follow-up | Retention rate (%) | Outcomes | Results |
|
| |||||||
| Doyle et al23 | RCT | Overweight or obese 12–18 years n=80 USA |
16-week Internet program versus usual care handouts Diet/PA |
16-week program Follow-up at 4 months post intervention |
82.5% | Body composition PA and diet behavior |
BMI z-score was reduced significantly in the intervention compared with the control from baseline to post intervention but not at 4-month follow-up Intervention group reported using more eating and PA-related skills more often post intervention and at follow-up |
| Reference | Study design | Sample characteristics | Intervention/control | Intervention duration/follow-up | Study completion rate (%) | Outcomes | Results |
|
| |||||||
| Hung et al25 | Quasi-experimental (pre and post) | BMI >25 12–14 years n=37 Taiwan |
WEP was integrated with a weight-loss student group held at school for 14 weeks Diet/PA |
Regular classes (weekly), exercise course (weekly) and individual counseling (2–3/6 months) After intervention |
97.3% | Body composition Physical fitness Self-esteem and self-efficacy |
BMI, waist circumference, and triceps skinfold was reduced Improve fitness Improved self-esteem and self-efficacy |
| Jago et al26 | RCT | Boys: no weight criteria 10–14 years n=473 USA |
Boy scouts fit for life (20 minutes weekly contact + Internet) versus mirro image F/V PA |
9-week troop and Internet program log onto the study website at least twice a week after intervention and 6 month after | 90.4% | Body composition PA Self-efficacy and preference |
No difference in body composition between groups Spring intervention group had increased light PA by 12 minutes |
| Jones et al27 | RCT By school |
n=l05 Mean age 15.1 (SD = 1) years USA |
SB2-BED versus wait list control 16 week Internet-based healthy weight maintenance program with mentor program Diet/PA/SB |
SB2-BED 16-week Internet-facilitated, semistructured program versus wait list control 9-month follow-up for height, weight, completion of self-report questionnaire and semistructured interview | 83% (17% had no ending data) |
BMI Binge eating behaviors Dietary fat and sugar intake Depression Adherence |
Reduction in BMI for intervention ↓ binge eating behaviors and weight and shape concerns No change in dietary fat and sugar intake No change in depression Those that did not complete were more likely white, reported depressed, had more weight and shape concerns |
| Maddison et al28 | RCT | n=322 Age 10–14 years |
Active video game upgrade package info on PA healthy eating, and weight loss/inactive video game Diet/PA |
Assigned to active video game or no change (sedentary) video games Assessments at baseline, 12, and 24 weeks |
100% | BMI Body composition PA Cardiorespiratory fitness Video game play |
BMI intervention no change, BMI in control ↑ ↓ body fat in intervention Time playing active video games ↑ with ↓ in time playing no active video games |
| Nguyen et al25 | RCT Blinded |
11=151 13–16 years |
Loozit group program, a two-phase behavioral lifestyle intervention with or without additional therapeutic contact Diet/PA/SB |
7-week group session (parents and adolescent separately) on diet and PA (phase 1) followed by quarterly adolescent only sessions (phase 2) with telephone or email coaching for intervention group | 88% | Food snacking BMI Self-reported psychosocial and lifestyle changes |
Additional therapeutic contact had no impact on outcomes |
| Owens et al30 | Pre and post | 8 families n=2l subjects 10± 1.6 years |
4 families loaned Wii Fit™ exercise modules without instruction or suggestions for use (intervention) and 4 families not Control group loaned device after 3 months PA |
Randomized family given Wii Fit to use in home for 3 months then control families given Wii Fit for 3 months | 100% No mention of withdrawals |
Body composition Daily PA Balance Muscular fitness Aerobic fitness Flexibility Wii Fit use |
No significant change in daily physical activity, muscular fitness, flexibility, balance, or body composition |
| Staiano et al3 | RCT | Overweight and obese African-American adolescents 15–19 years n=54 |
20-week exercise game (video game that requires gross motor activity) three groups: competitive exergame, cooperative exer game, or control PA |
20-week exer game (video game that requires gross motor activity) Baseline, 10-week and 20-week data collection |
72% | BMI Peer support Self-efficacy Self esteem |
Cooperative lost the most weight, ↑ self-efficacy No difference in weight gain with competitive and control Both competitive and cooperative had increased peer support |
| Wagener et al32 | RCT | n=40 12–18 years |
Supervised 10-week group dance-based exer game exercise or waitlist control group PA |
Exer gaming in group setting (dance game). Adolescents came to 10-week group-based exer game exercise program | 97.5% | BMI Perceived competence scale Behavior Assessment Scale Parent Rating Scale for Adolescents |
No difference in pre/post-test BMI Improved self-perceived psychological adjustment and competence to exercise |
| Williamson et al33 | RCT | n=57 (40 parent and adolescent dyads) 11–15 years 13.2 years average age |
Interactive behavioral Internet program/control condition Diet/PA |
Counselors were educated on culturally relevant dietary and physical activity issues, and they incorporated this information into the face-to-face and Internet counseling sessions Two-year intervention |
70% | BMI, body weight, body composition Weight loss behaviors |
Adolescents in the behavioral treatment lost more body fat immediately after the intervention but no difference was found at 2 years follow up |
Note: Wii Fit™; Nintendo, Kyoto, Japan.
Abbreviations: BD2, Student Bodies 2; BMI, body mass index; WEP, weight loss E-learning program; PA, physical activity; RCT, randomized controlled trial; SD, standard deviation; F/V, fruit and vegetable; SB, sedentary behavior; BP, blood pressure; SBP, systolic blood pressure; DBP, diastolic blood pressure.
Physical activity, sedentary activity time, and dietary behavior
Six of the eleven studies that examined physical activity or physical activity-related outcomes found improved physical activity outcomes (four Internet-based interventions and two active video gaming interventions).13,21,23,26,28,35 Two of three studies that assessed the impact of technology-based interventions on reducing sedentary activity time found a significant decrease in sedentary behaviors (all active video game interventions).13,28 For dietary behavior, five of eleven studies assessed dietary outcomes indicating improvement in dietary behaviors (ie, increased fruit/vegetable intake, decreased sugary drinks and snacking) in adolescents in the intervention groups (four Internet-based interventions and one active video game intervention).13,22–24,33 For instance, a study by Chen et al22 on tailored web-based interventions for Chinese-American adolescents (aged 12–15 years) found a significant decrease in sedentary activity associated with improved physical activity and fruit/vegetable intake at 6 months post intervention. Maddison et al28 examined an active video game upgrade package in adolescents aged 10–14 years and found that youth in the intervention group increased the time playing active video games while decreasing the time in nonactive video games (see Table 3).
Table 3.
Outcome measured by study: arrows indicate significant increase or decrease on the outcomes
| Reference | BMI | Other metabolic index | Physical activity | Sedentary behavior | Diet | Self-efficacy | Knowledge | Psychosocial |
|---|---|---|---|---|---|---|---|---|
| Adamo et al21 | No difference | No effect | ↑ vigorous PA time in control group | N/A | No effect | N/A | N/A | |
| Chen et al22 | No difference | ↓ waist-hip ratio and DBP | ↑ PA | N/A | ↑ F/V | No effect | ↑ | |
| Christison and Khan13 | ↓ BMI and BMI z-score | N/A | ↑ PA time | ↓ television time | ↓ soda ↑ eat at table |
N/A | N/A | ↑ global self-worth |
| Doyle et al23 | ↓ BMI z-score | N/A | ↑ PA skill | N/A | ↑ diet skill | N/A | N/A | N/A |
| Ezendam et al24 | No difference | N/A | ↓ step counts at 4 months follow-up but not at 2 years | N/A | ↓ sugary drink and snack ↑ F/V |
N/A | N/A | N/A |
| Hung et al25 | ↓ BMI and triceps skinfold | N/A | ↑ fitness | ↑ S-E | ↑ self-esteem | |||
| Jago et al26 | No difference | N/A | ↑ light PA time | N/A | N/A | No effect | N/A | N/A |
| Jones et al27 | ↓ BMI | N/A | N/A | N/A | No effect | N/A | N/A | ↓ weight concern No change in depression |
| Maddison et al28 | ↓ no change in BMI body fat | N/A | ↑ time in active video game | ↑ time in inactive game | No effect | N/A | N/A | N/A |
| Nguyen et al29 | No difference | N/A | No effect | No effect | No effect | N/A | N/A | No effect |
| Owens et al30 | No difference | N/A | No effect | N/A | N/A | N/A | N/A | N/A |
| Staiano et al31 | No difference | N/A | N/A | N/A | N/A | N/A | N/A | ↑ peer support and self-efficacy |
| Wagener et al32 | No difference | N/A | N/A | N/A | N/A | N/A | N/A | ↑ psychosocial adjustment and competence |
| Williamson et al33 | ↓ body fat at 6 months post intervention No difference after 2 years |
N/A | No difference | N/A | ↓ fatty foods | N/A | N/A | N/A |
Note: ↑↓ indicate significant increase and decrease, respectively.
Abbreviations: BMI, body mass index; PA, physical activity; N/A, not available; DBP, diastolic blood pressure; F/V, fruit and vegetable; S-E, self-efficacy.
Other psychosocial outcomes
Seven studies assessed the impact of technology-based interventions on psychosocial outcomes (ie, self-efficacy, weight concern, peer support, and self-competence).13,22,25–27,29,31,32 Five of the seven studies suggested improvement in psychosocial function in adolescents using the technology-based interventions.13,22,25,27,31,32 For example, Wagener et al32 found that adolescents in an exer-gaming program had improved self-perceived psychological adjustment and competence to exercise after the intervention, and Jones et al27 found that adolescents in their intervention group reported fewer weight and body shape concerns (see Table 3).
Components of effective interventions
Seven Internet-based interventions and seven active video game-based interventions were included in this systematic review. Six of 14 studies (four Internet-based and two active video game-based interventions) found that BMI and/or body fat decreased.13,23,25,27,28,33 All effective interventions utilized dietary and physical activity strategies as part of the intervention components. Six Internet-based interventions required weekly logins whereas active video game interventions recommended daily use. Based on the results, it is recommended that the intervention intensity that was based weekly has the potential to decrease obesity (see Table 4 for significant BMI outcomes with intervention components).
Table 4.
Significant BMI outcome (decreased BMI or percent body fat)
| Reference | Intervention type | Intervention components | Intervention duration | Intervention intensity | Follow-up time | Study type |
|---|---|---|---|---|---|---|
| Christison and Khan13 | Active video game | Diet and PA | 10 weeks | Weekly | 10 weeks after baseline | Pre-post |
| Doyle et al23 | Internet | Diet and PA | 16 weeks | Weekly | 4 months post intervention | RCT |
| Jones et al27 | Internet | Diet, PA, and SB | 16 weeks | Weekly | 9 months | RCT |
| Hung et al25 | Internet | Diet and PA | 14 weeks | Weekly | 14 weeks | Pre-post |
| Madison et al28 | Active video game | Diet and PA | 12 weeks | 60 minutes most days of the week | 24 weeks | RCT |
| Williamson et al33 | Internet | Diet and PA | 1 year | 52 sessions, weekly | 6 months (decreased BMI) and 2 years (no difference) | RCT |
Abbreviations: BMI, body mass index; PA, physical activity; RCT, randomized controlled trial; SB, sedentary behavior.
Discussion
The present systematic review investigates the potential impact of recent technological innovations (such as the Internet or active video games) for adolescents and the effect of these technology-based interventions on weight-related outcomes. Based on our review of 14 clinical intervention studies, there is no clear evidence that technology-based interventions decrease obesity in adolescents. We found that slightly less than half of the studies reviewed in this paper supported the use of technology in reducing unhealthy weight in adolescents. All effective interventions included improving physical activity and healthy eating habit as key components. However, each of these interventions only had a short-term impact on weight management. This is consistent with other obesity prevention interventions in children that are either home-based or school-based.36–38 Because of the variation in duration of intervention (ranging from 10 weeks to 2 years) and dose (daily to weekly), the literature to date does not provide enough evidence on the optimal dose or duration of the most effective intervention for prevention of obesity in adolescents, although the trend pointed toward dosing a minimum of one hour/weekly for 10–16 weeks for best results. This is consistent with a systematic review done for obesity prevention in a primary care setting.39
In comparing the various modalities of technology and their delivery (Internet versus active video games), there is no clear evidence that one format is more effective than another. Depending on the age of the participants, different modalities might be more attractive than others. For example, a younger adolescent might prefer exer-games and interacting with peers, while an older adolescent might prefer a smartphone app or Internet-based program for weight management that could be used privately.
The literature currently available is also insufficient to examine the impact of technology-based obesity prevention interventions on weight-health related outcomes such as physical activity, sedentary activity, dietary behaviors, or psychosocial outcomes. In eleven studies that examined the impact of technology-based obesity prevention on physical activity and dietary behaviors, only six reported positive improvement in these outcomes. Even fewer studies examined the impact of interventions on sedentary behaviors and psychosocial outcomes. Therefore, it is challenging to determine the effect of technology-based intervention on weight-related health behaviors, and we do not know whether improvement of these behaviors led to decreased weight among adolescents. One plausible reason for this lack of evidence might be the wide range of ages encompassed by these studies. Participants in the various studies ranged in age from 10–19 years. These years encompass later childhood (9–12 years), early adolescence (13–14 years), and late adolescence (15–17 years) as well as young adulthood (18–19 years). The developmental differences and the prevalence of using technology among these age groups may impact any potential trend seen in the data. Depending on the age group being investigated, interest in technology and use may vary.
This review suggests that both active video games and Internet-based interventions including diet and physical components have the potential to decrease obesity in adolescence, especially Internet-based interventions. Because of the variation in duration of intervention (10 weeks to 2 years), it is not clear what length of intervention is most effective. Only one study included long-term follow-up data (more than 12 months after the intervention), and the intervention did not support long-term efficacy with regard to healthy weight management.33
Our review indicates that several interventions provide short-term improvements in BMI but none that seem to be sustainable. Sustained weight loss is an ongoing struggle, regardless of the sample being studied or the interventions used, and is no different in this population. Very few interventions seem to specifically focus on lifelong lifestyle modifications. Many of the interventions that were investigated either provided the participants with the necessary equipment (ie, loaning Wii Fit, allowing temporary upgrades to active video games) or were activities that were set up for a limited time period at school (GameBike or Dance-Dance Revolution). After the intervention, participants no longer had access to these exercise opportunities, so likely reverted back to the prestudy lifestyle habits that lead to their overweight or obesity. Technology-based intervention for weight management needs to be developed in such a way that it incorporates resources that will continue to be available in order to see sustainability.
The goal of this review was to determine ways in which health care providers and researchers can make more informed decisions about which types of technology-based interventions for adolescent obesity are most suitable and achieve sustainable weight reduction, impact the amount of physical activity, reduce sedentary activity, improve dietary behaviors, and/or positive psychosocial outcomes. Although we found no clear evidence of an effect of technology-based intervention for prevention of obesity in adolescents, the use of developmentally appropriate technology has the potential to assist health care providers in dealing with the obesity epidemic, especially when interventions focus on both physical activity and healthy dietary behaviors. Future research should include rigorous evaluation of cost- effectiveness as well as the mediating and moderating factors associated with effective technology-based interventions, and should also include more long-term follow-up. In addition, assessment of weight-related health outcomes, such as physical activity, sedentary activity, dietary behaviors, self-efficacy, and quality of life, should be included in future research.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Wang Y, Lobstein T. Worldwide trends in childhood overweight and obesity. Int J Pediatr Obes. 2006;1(1):11–25. doi: 10.1080/17477160600586747. [DOI] [PubMed] [Google Scholar]
- 2.Iannotti RJ, Wang J. Trends in physical activity, sedentary behavior, diet, and BMI among US adolescents, 2001–2009. Pediatrics. 2013;132(4):606–614. doi: 10.1542/peds.2013-1488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bjorge T, Engeland A, Tverdal A, Smith GD. Body mass index in adolescence in relation to cause-specific mortality: a follow-up of 230,000 Norwegian adolescents. Am J Epidemiol. 2008;168(1):30–37. doi: 10.1093/aje/kwn096. [DOI] [PubMed] [Google Scholar]
- 4.Levi Z, Kark JD, Barchana M, et al. Measured BMI in adolescence and the incidence of colorectal cancer in a cohort of 1.1 million males. Cancer Epidemiol Biomarkers Prev. 2011;20(12):2524–2531. doi: 10.1158/1055-9965.EPI-11-0531. [DOI] [PubMed] [Google Scholar]
- 5.Reilly JJ, Kelly J. Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: systematic review. Int J Obes (Lond) 2011;35(7):891–898. doi: 10.1038/ijo.2010.222. [DOI] [PubMed] [Google Scholar]
- 6.Rademacher ER, Jacobs DR, Jr, Moran A, Steinberger J, Prineas RJ, Sinaiko A. Relation of blood pressure and body mass index during childhood to cardiovascular risk factor levels in young adults. J Hypertens. 2009;27(9):1766–1774. doi: 10.1097/HJH.0b013e32832e8cfa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lloyd LJ, Langley-Evans SC, McMullen S. Childhood obesity and adult cardiovascular disease risk: a systematic review. Int J Obes (Lond) 2010;34(1):18–28. doi: 10.1038/ijo.2009.61. [DOI] [PubMed] [Google Scholar]
- 8.Lloyd LJ, Langley-Evans SC, McMullen S. Childhood obesity and risk of the adult metabolic syndrome: a systematic review. Int J Obes (Lond) 2012;36(1):1–11. doi: 10.1038/ijo.2011.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Weiss R, Cali AM, Dziura J, Burgert TS, Tamborlane WV, Caprio S. Degree of obesity and glucose allostasis are major effectors of glucose tolerance dynamics in obese youth. Diabetes Care. 2007;30(7):1845–1850. doi: 10.2337/dc07-0325. [DOI] [PubMed] [Google Scholar]
- 10.Feliu Rovira A, Paris Miro N, Zaragoza-Jordana M, et al. Clinical and metabolic effectiveness of a new motivational therapy for the treatment of obesity in adolescents (OBEMAT) An Pediatr (Barc) 2013;78(3):157–166. doi: 10.1016/j.anpedi.2012.06.006. Spanish. [DOI] [PubMed] [Google Scholar]
- 11.Gourlan M, Sarrazin P, Trouilloud D. Motivational interviewing as a way to promote physical activity in obese adolescents: a randomised-controlled trial using self-determination theory as an explanatory framework. Psychol Health. 2013;28(11):1265–1286. doi: 10.1080/08870446.2013.800518. [DOI] [PubMed] [Google Scholar]
- 12.Madden M, Lenhart A, Duggan M, Cortesi S, Gasser U. Teens and Technology. 2013. [Accessed March 9, 2014]. Available from: http://www.pewinternet.org/Reports/2013/Teens-and-Tech.aspx.
- 13.Christison A, Khan HA. Exergaming for health: a community-based pediatric weight management program using active video gaming. Clin Pediatr (Phila) 2012;51(4):382–388. doi: 10.1177/0009922811429480. [DOI] [PubMed] [Google Scholar]
- 14.Pellegrini CA, Duncan JM, Moller AC, et al. A smartphone-supported weight loss program: design of the ENGAGED randomized controlled trial. BMC Public Health. 2012;12:1041. doi: 10.1186/1471-2458-12-1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Woolford SJ, Clark SJ, Strecher VJ, Resnicow K. Tailored mobile phone text messages as an adjunct to obesity treatment for adolescents. J Telemed Telecare. 2010;16(8):458–461. doi: 10.1258/jtt.2010.100207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.An J, Hayman L, Park Y, Dusaj T, Ayres C. Web-based weight management programs for children and adolescents a systematic review of randomized controlled trial studies. Adv Nurs Sci. 2009;32(3):222–240. doi: 10.1097/ANS.0b013e3181b0d6ef. [DOI] [PubMed] [Google Scholar]
- 17.Lu AS, Kharrazi H, Gharghabi F, Thompson D. A systematic review of health videogames on childhood obesity prevention and intervention. Games Health J. 2013;2(3):131–141. doi: 10.1089/g4h.2013.0025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lavelle HV, Mackay DF, Pell JP. Systematic review and meta-analysis of school-based interventions to reduce body mass index. J Public Health (Oxf) 2012;34(3):360–369. doi: 10.1093/pubmed/fdr116. [DOI] [PubMed] [Google Scholar]
- 19.Sargent GM, Pilotto LS, Baur LA. Components of primary care interventions to treat childhood overweight and obesity: a systematic review of effect. Obes Rev. 2011;12(5):e219–e235. doi: 10.1111/j.1467-789X.2010.00777.x. [DOI] [PubMed] [Google Scholar]
- 20.Tobias DK, Zhang C, van Dam RM, Bowers K, Hu FB. Physical activity before and during pregnancy and risk of gestational diabetes mellitus: a meta-analysis. Diabetes Care. 2011;34(1):223–229. doi: 10.2337/dc10-1368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Adamo KB, Rutherford JA, Goldfield GS. Effects of interactive video game cycling on overweight and obese adolescent health. Appl Physiol Nutr Metab. 2010;35(6):805–815. doi: 10.1139/H10-078. [DOI] [PubMed] [Google Scholar]
- 22.Chen JL, Weiss S, Heyman MB, Cooper B, Lustig RH. The efficacy of the web-based childhood obesity prevention program in Chinese-American adolescents (qeb ABC study) J Adolesc Health. 2011;49(2):148–154. doi: 10.1016/j.jadohealth.2010.11.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Doyle AC, Goldschmidt A, Huang C, Winzelberg AJ, Taylor CB, Wilfley DE. Reduction of overweight and eating disorder symptoms via the Internet in adolescents: a randomized controlled trial. J Adolesc Health. 2008;43(2):172–179. doi: 10.1016/j.jadohealth.2008.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ezendam NP, Brug J, Oenema A. Evaluation of the Web-based computer-tailored FATaintPHAT intervention to promote energy balance among adolescents: results from a school cluster randomized trial. Arch Pediatr Adolesc Med. 2012;166(3):248–255. doi: 10.1001/archpediatrics.2011.204. [DOI] [PubMed] [Google Scholar]
- 25.Hung SH, Hwang SL, Su MJ, et al. An evaluation of a weight-loss program incorporating E-learning for obese junior high school students. Telemed J E Health. 2008;14(8):783–792. doi: 10.1089/tmj.2007.0121. [DOI] [PubMed] [Google Scholar]
- 26.Jago R, Baranowski T, Baranowski JC, et al. Fit for Life Boy Scout badge: outcome evaluation of a troop and Internet intervention. Prev Med. 2006;42(3):181–187. doi: 10.1016/j.ypmed.2005.12.010. [DOI] [PubMed] [Google Scholar]
- 27.Jones M, Luce KH, Osborne MI, et al. Randomized, controlled trial of an internet-facilitated intervention for reducing binge eating and overweight in adolescents. Pediatrics. 2008;121(3):453–462. doi: 10.1542/peds.2007-1173. [DOI] [PubMed] [Google Scholar]
- 28.Maddison R, Foley L, Ni Mhurchu C, et al. Effects of active video games on body composition: a randomized controlled trial. Am J Clin Nutr. 2011;94(1):156–163. doi: 10.3945/ajcn.110.009142. [DOI] [PubMed] [Google Scholar]
- 29.Nguyen B, Shrewsbury VA, O’Connor J, et al. Two-year outcomes of an adjunctive telephone coaching and electronic contact intervention for adolescent weight-loss maintenance: the Loozit randomized controlled trial. Int J Obes (Lond) 2013;37(3):468–472. doi: 10.1038/ijo.2012.74. [DOI] [PubMed] [Google Scholar]
- 30.Owens SG, Garner JC, 3rd, Loftin JM, van Blerk N, Ermin K. Changes in physical activity and fitness after 3 months of home Wii Fit use. J Strength Cond Res. 2011;25(11):3191–3197. doi: 10.1519/JSC.0b013e3182132d55. [DOI] [PubMed] [Google Scholar]
- 31.Staiano AE, Abraham AA, Calvert SL. Adolescent exergame play for weight loss and psychosocial improvement: a controlled physical activity intervention. Obesity (Silver Spring) 2013;21(3):598–601. doi: 10.1038/oby.2012.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wagener TL, Fedele DA, Mignogna MR, Hester CN, Gillaspy SR. Psychological effects of dance-based group exergaming in obese adolescents. Pediatr Obes. 2012;7(5):e68–e74. doi: 10.1111/j.2047-6310.2012.00065.x. [DOI] [PubMed] [Google Scholar]
- 33.Williamson DA, Walden HM, White MA, et al. Two-year internet-based randomized controlled trial for weight loss in African-American girls. Obesity (Silver Spring) 2006;14(7):1231–1243. doi: 10.1038/oby.2006.140. [DOI] [PubMed] [Google Scholar]
- 34.Maddison R, Mhurchu CN, Jull A, Prapavessis H, Foley LS, Jiang Y. Active video games: the mediating effect of aerobic fitness on body composition. Int J Behav Nutr Phys Act. 2012;9:54. doi: 10.1186/1479-5868-9-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Berenson GS, Agirbasli M, Nguyen QM, Chen W, Srinivasan SR. Glycemic status, metabolic syndrome, and cardiovascular risk in children. Med Clin North Am. 2011;95(2):409–417. doi: 10.1016/j.mcna.2010.11.011. ix. [DOI] [PubMed] [Google Scholar]
- 36.Barnett A, Cerin E, Baranowski T. Active video games for youth: a systematic review. J Phys Act Health. 2011;8(5):724–737. doi: 10.1123/jpah.8.5.724. [DOI] [PubMed] [Google Scholar]
- 37.O’Brien A. “Web-based weight management programs for children and adolescents: a systematic review of randomized controlled trial studies” by An, Hayman, Park, Dusaj, and Ayres (Jul–Sep 2009, Vol 32, No 3, pp 222–240) ANS Adv Nurs Sci. 2010;33(1):2. doi: 10.1097/ANS.0b013e3181d1ec00. [DOI] [PubMed] [Google Scholar]
- 38.Katz DL. School-based interventions for health promotion and weight control: not just waiting on the world to change. Annu Rev Public Health. 2009;30:253–272. doi: 10.1146/annurev.publhealth.031308.100307. [DOI] [PubMed] [Google Scholar]
- 39.Jacobson D, Gance-Cleveland B. A systematic review of primary healthcare provider education and training using the Chronic Care Model for childhood obesity. Obes Rev. 2011;12(5):e244–e256. doi: 10.1111/j.1467-789X.2010.00789.x. [DOI] [PubMed] [Google Scholar]