Abstract
Introduction
Soft tissue reactions following metal-on-metal (MoM) arthroplasty of the hip have been under considerable discussion. These reactions are seen following both hip resurfacing and MoM total hip arthroplasty (THA). The phenomenon may arise owing to shedding of metal particles in high wear states, hypersensitivity with normal metal wear rates or a combination of the two.
Methods
Three patients were identified who had developed a soft tissue reaction (pseudotumour) following MoM hip resurfacing procedures. The prostheses were revised to ceramic-on-ceramic (CoC) THA with only minimal debridement of the pseudotumour. Pre and postoperative magnetic resonance imaging was performed to assess the size of the lesions.
Results
Progressive and satisfactory resolution of the associated pseudotumours was identified following revision of the prostheses to CoC THA.
Conclusions
In the early stages of pseudotumour formation following MoM hip resurfacing, this potentially devastating condition can be managed adequately with revision to a CoC bearing THA with minimal soft tissue excision.
Keywords: Pseudotumour, Metal-on-metal, Revision, Hip arthroplasty, Ceramic-on-ceramic
Metal-on-metal (MoM) arthroplasty of the hip was initiated in 1938, and there are some reports that the prostheses pioneered by McKee and Watson-Farrar produced an occasional atypical and unusual response involving surrounding soft tissues. 1–3 Particulate wear debris from polyethylene acetabular components are well known to potentially produce large cystic or solid swellings but these reactions appear to be of a more benign nature than those generated by metal. 4,5
Over the last two decades there has been a marked increase in the number of MoM devices inserted, particularly hip resurfacing implants. 6 In a small percentage of cases, extensive muscle necrosis, nerve damage, bursa formation and muscle swellings (pseudotumours) have been observed. 7
Clinicians are sometimes uncertain about the extent of surgical debridement and excision required in the event of a pseudotumour identified on magnetic resonance imaging (MRI). We present three cases in which revision of MoM resurfacing to a ceramic-on-ceramic (CoC) total hip arthroplasty (THA) resulted in resolution of the associated soft tissue reaction, both clinically and on subsequent MRI. Patient consent was obtained for inclusion in this paper and for the use of MRI.
The patients described presented within a few years of MoM resurfacing. The diagnosis of pseudotumour was based on MRI findings after presentation with either a palpable lump and/or symptoms. In all cases, the diagnosis was confirmed histologically to be an aseptic lymphocytic vasculitis associated lesion (ALVAL). Limited debridement was performed during revision surgery. The patients were all converted to CoC hybrid THA and were followed up regularly, which included postoperative MRI.
Results
Case 1
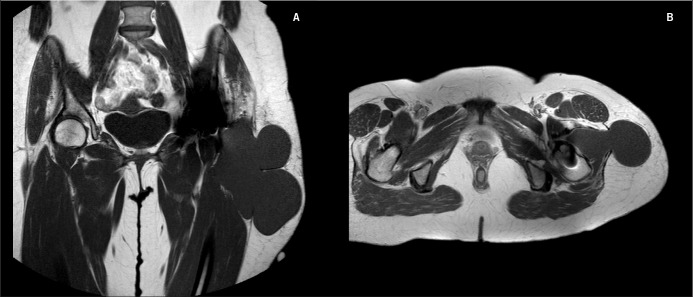
A 49-year-old woman underwent a left Cormet™ (Corin, Cirencester, UK) hip resurfacing in April 2002. Initial recovery was uncomplicated until two years following surgery, when she presented with a painless cystic swelling over the lateral aspect of her left thigh. By July 2008 she was noted to have a 20cm × 8cm soft tissue mass in the superficial tissues of the thigh. Ultrasonography showed a subcutaneous heterogeneous swelling, predominantly solid but with cystic areas. MRI showed a lobulated mass lying laterally to the left hip with an inner component lying around the greater trochanter and an outer component in the subcutaneous soft tissues, involving both the flexor and extensor compartments of the thigh (Fig 1). A decision was made in January 2009 to explore the swelling and revise the components.
Figure 1.
T1 weighted magnetic resonance imaging of Patient 1 on coronal (A) and axial (B) sections
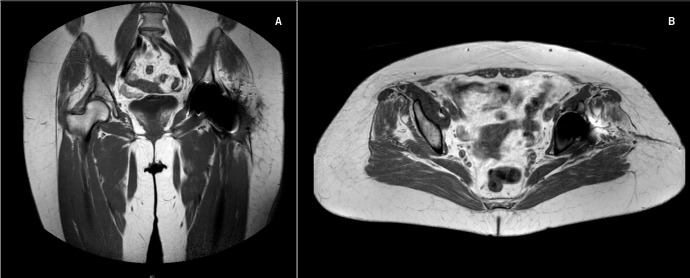
Intraoperative findings on revision in June 2009, 86 months after initial surgery, included an enlarged bursa, a thickened psoas tendon and a loose femoral component. Samples were sent for histological analysis and the components revised to a conventional THR using a Trident® uncemented acetabular component (Stryker, Newbury, UK) and cemented Exeter™ stem (Stryker) with CoC bearings. Extensive debridement of the lesion was not undertaken. Histology showed particulate metal wear debris and a diffuse inflammatory infiltrate consistent with ALVAL. Two months following her procedure, the visible swelling had resolved completely and repeat MRI seven months after revision showed significant reduction in pseudotumour size (Fig 2).
Figure 2.
T1 weighted coronal magnetic resonance imaging of Patient 1 taken two months postoperatively: coronal (A) and axial sections (B)
Case 2
A 52-year-old woman underwent a right Cormet™ hip resurfacing for osteoarthritis in December 2004. She developed pain in the right groin, buttock and greater trochanter region at six months, progressing to signs of psoas impingement by 18 months. Hip aspiration was performed at 17 months, which yielded a small amount of blood stained fluid with no growth on culture. Ultrasonography at 20 months showed a mass in the right psoas muscle with radiological signs of possible loosening of the femoral component. MRI at 21 months showed expansion of the right iliacus muscle. A diagnosis of pseudotumour plus possible loosening of the femoral component was made and she was therefore listed for revision.
At the time of surgery, 28 months following the initial procedure, the femoral component was indeed found to be loose, and a large pseudotumour was identified involving the iliopsoas muscle and extending into the pelvis. Limited resection of the soft tissue mass was performed with the decision being made not to explore the mass into the pelvis. Tissue samples were sent for histology, which confirmed ALVAL, and the components were revised to a Trident® uncemented acetabular component and cemented Exeter™ stem with ceramic bearings. She was completely asymptomatic at four months. Repeat MRI six months later showed no identifiable lesion (including no sign of the intrapelvic extension) with atrophy of the gluteal muscles only (Fig 3).
Figure 3.
T1 weighted magnetic resonance imaging of Patient 2 taken ten months postoperatively: coronal (A) and axial sections (B)
Case 3
A 58-year-old woman underwent a left Cormet™ hip resurfacing in June 2003. She developed a lump in her left groin early in the postoperative period, which recurred despite multiple aspirations. Computed tomography at 24 months confirmed a 3cm × 4cm mass anterior to the prosthesis extending into the groin relating to the inguinal canal. It was thought to be putting pressure on the femoral vein as there was an associated femoral deep vein thrombosis (DVT). The DVT was treated and she had ultrasonography in February 2006, which showed that the mass, still present, had now solidified. Aspiration at 39 months showed an inflammatory infiltrate and she went on to have an open exploration of the left groin lesion the following month, where no abnormality was identified. Her symptoms improved temporarily following this but recurred within three months, prompting MRI, which identified a swelling of the iliopsoas muscle.
The patient was coping with her symptoms at this time and therefore further intervention was deferred but the lump in her groin continued to enlarge. By 63 months postoperatively, she was experiencing severe left hip pain with a large swelling palpable in the groin. Repeat MRI showed an 8cm × 5.5cm thin walled cystic structure lying anterior to the left hip and medial to the iliopsoas insertion (Fig 4).
Figure 4.
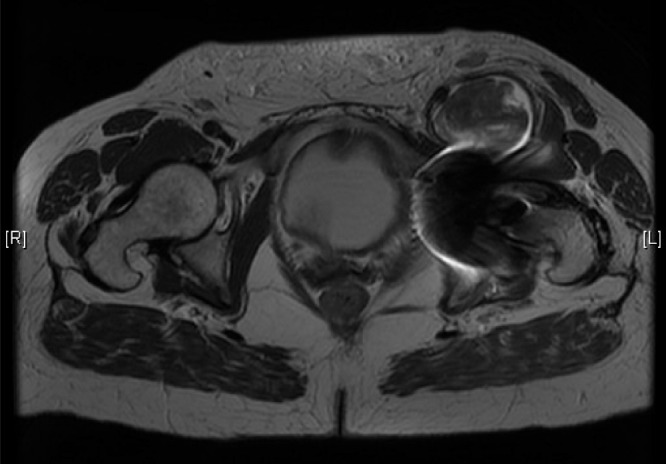
Gadolinium enhanced T1 weighted axial magnetic resonance imaging of Patient 3
The patient underwent surgery in December 2008 (66 months after the initial procedure), where a fluid filled necrotic mass was found anterior to the hip, extending under the femoral nerve into the medial aspect of the thigh. The lesion was debulked and the bursa drained but a decision was made not to explore medially into the thigh. Samples were sent for histology, which demonstrated prominent metal pigment deposition with an inflammatory infiltrate consistent with ALVAL. The components were revised to a Trident® uncemented acetabular component and cemented Exeter™ stem with ceramic bearings. Five weeks postoperatively, the patient was mobilising well and the groin swelling had resolved, with repeat MRI at 11 months showing a marked reduction in the size of the lesion (Fig 5).
Figure 5.
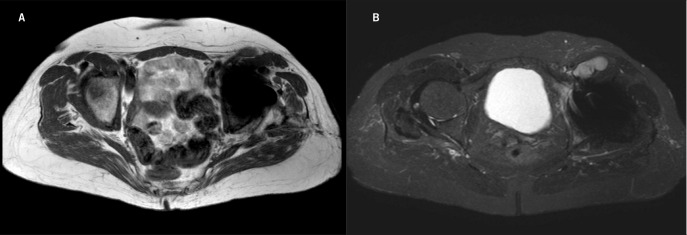
Axial sections of T1 (A) and T2 (B) weighted magnetic resonance imaging of Patient 3 taken 11 months postoperatively
Discussion
Revision of a MoM hip resurfacing with associated pseudotumour formation can be a procedure potentially requiring extensive soft tissue resection. 8 Some such cases have been associated with nerve palsy, 9 which has a poor prognosis. 8
Much concern has been generated by these recent observations while at the same time there is an increasing awareness of the problems relating to high wear states, particularly following MoM resurfacing. These problems appear to arise predominantly in women, and have been postulated to be associated with anterior prominence of the acetabular component, impingement with edge wear and excessive abduction of the cup. 7 High wear states and particle shedding are thought to generate a local sensitivity reaction but whether this is related to the well-described type IV hypersensitivity reactions is not certain. 10 Moreover, skin patch sensitivity may not be a reliable indicator since skin sensitivity is thought to be a distinct immunological process and has not been found to be representative of a deep immune response. 11
The cases we present were addressed by insertion of a hybrid THA with large diameter CoC articulation. There was rapid clinical resolution of swelling, and in the patient with the large pseudotumour extending into the pelvis (case 2), there was progressive resolution and disappearance of this lesion, the only residual findings at MRI two years later being atrophy of the surrounding muscles.
There is clearly a gradation in the severity of these lesions ranging from relatively benign cystic swellings to osteolysis 12 and extensive tissue necrosis. 13 Campbell et al have shown a distinction between the histological findings of pseudotumour secondary to high metal wear and pseudotumour forming in patients suspected of metal hypersensitivity. 14 They found less disruption of the synovial surface and greater preservation of the normal tissue architecture in the high wear group whereas the most extensive tissue damage and the densest lymphocyte aggregates were found to occur in patients suspected of metal hypersensitivity, which occurred typically in the absence of high wear.
It could be hypothesised from this that muscle biopsy could be a preliminary investigation that may be indicative of the severity of the lesion and guide the necessity for widespread tissue excision. However, the efficacy of this has not been evaluated and the degree of excision in these cases is still uncertain. Referral to specialist centres for these revision procedures is therefore recommended.
Conversion of the MoM to a CoC bearing with a conservative approach to soft tissue excision reduces patient recovery time owing to the less extensive tissue loss and is likely to have an associated improved longer term functional outcome.
Conclusions
Pseudotumour formation has become a well-known complication following MoM THA. If associated with widespread muscle involvement or symptoms of nerve compression are present then referral to a specialist centre may be appropriate. However, in the early stages simple conversion to CoC THA using a conservative approach to soft tissue debridement appears to be an adequate option.
References
- 1.August AC, Aldam CH, Pynsent PB. The McKee–Farrar hip arthroplasty. J Bone Joint Surg Br 1986; 68: 520–527 [DOI] [PubMed] [Google Scholar]
- 2.Dandy DJ, Theodorou BC. The management of local complications of total hip replacement by the McKee–Farrar technique. J Bone Joint Surg Br 1975; 57: 30–35 [PubMed] [Google Scholar]
- 3.Mckee GK, Watson-Farrar J. Replacement of arthritic hips by the McKee–Farrar prosthesis. J Bone Joint Surg Br 1966; 48: 245–259 [PubMed] [Google Scholar]
- 4.Heath JC, Freeman MA, Swanson SA. Carcinogenic properties of wear particles from prostheses made in cobalt-chromium alloy. Lancet 1971; 1: 564–566 [DOI] [PubMed] [Google Scholar]
- 5.Heath JC, Webb M. Content and intracellular distribution of the inducing metal in the primary rhabdomyosarcomata induced in the rat by cobalt, nickel and cadmium. Br J Cancer 1967; 21: 768–779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Graves SE, Davidson D, Ingerson Let al.The Australian Orthopaedic Association National Joint Replacement Registry. Med J Aust 2004; 180: S31–S34 [DOI] [PubMed] [Google Scholar]
- 7.Pandit H, Glyn-Jones S, McLardy-Smith Pet al.Pseudotumours associated with metal-on-metal hip resurfacings. J Bone Joint Surg Br 2008; 90: 847–851 [DOI] [PubMed] [Google Scholar]
- 8.Grammatopoulos G, Pandit H, Kwon YMet al.Hip resurfacings revised for inflammatory pseudotumour have a poor outcome. J Bone Joint Surg Br 2009; 91: 1,019–1,024 [DOI] [PubMed] [Google Scholar]
- 9.Harvie P, Giele H, Fang Cet al.The treatment of femoral neuropathy due to pseudotumour caused by metal-on-metal resurfacing arthroplasty. Hip Int 2008; 18: 313–320 [DOI] [PubMed] [Google Scholar]
- 10.Goodman SB. Wear particles, periprosthetic osteolysis and the immune system. Biomaterials 2007; 28: 5,044–5,048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Swiontkowski MF, Agel J, Schwappach Jet al.Cutaneous metal sensitivity in patients with orthopaedic injuries. J Orthop Trauma 2001; 15: 86–89 [DOI] [PubMed] [Google Scholar]
- 12.De Haan R, Campbell PA, Su EP, De Smet KA. Revision of metal-on-metal resurfacing arthroplasty of the hip: the influence of malpositioning of the components. J Bone Joint Surg Br 2008; 90: 1,158–1,163 [DOI] [PubMed] [Google Scholar]
- 13.Ollivere B, Darrah C, Barker Tet al.Early clinical failure of the Birmingham metal-on-metal hip resurfacing is associated with metallosis and soft-tissue necrosis. J Bone Joint Surg Br 2009; 91: 1,025–1,030 [DOI] [PubMed] [Google Scholar]
- 14.Campbell PA, Ebramzadeh E, Nelson Set al.Histological features of pseudotumor-like tissues from metal-on-metal hips. Clin Orthop Relat Res 2010; 468: 2,321–2,327 [DOI] [PMC free article] [PubMed] [Google Scholar]