Abstract
Introduction
Appendicitis in the developing world is a cause of significant preventable morbidity. This prospective study from a regional hospital in South Africa constructs a robust cost model that demonstrates the cost effectiveness of an efficient curative surgical service in a primary healthcare-orientated system.
Methods
A prospective audit of all patients with acute appendicitis admitted to Edendale Hospital was undertaken from September 2010 to September 2011. A microcosting approach was used to construct a cost model based on the estimated cost of operative and perioperative interventions together with the associated hospital stay. For cost analysis, patients were divided into the following cohorts: uncomplicated appendicitis, complicated appendicitis with localised intra-abdominal sepsis, complicated appendicitis with generalised intra-abdominal sepsis, with and without intensive care unit admission.
Results
Two hundred patients were operated on for acute appendicitis. Of these, 36% (71/200) had uncomplicated appendicitis and 57% (114/200) had perforation. Pathologies other than appendicitis were present in 8% (15/200) and these patients were excluded. Of the perforated appendices, 45% (51/114) had intra-abdominal contamination that was localised while 55% (63/114) generalised sepsis. The mean cost for each patient was: 6,578 ZAR (£566) for uncomplicated appendicitis; 14,791 ZAR (£1,272) for perforation with localised intra-abdominal sepsis and 34,773 ZAR (£2,990) for perforation with generalised intra-abdominal sepsis without intensive care admission. With intensive care admission it was 77,816 ZAR (£6,692). The total cost of managing acute appendicitis was 4,272,871 ZAR (£367,467). Almost 90% of this total cost was owing to advanced disease with abdominal sepsis and therefore potentially preventable.
Conclusions
Early uncomplicated appendicitis treated appropriately carries little morbidity and is relatively inexpensive to treat. As the pathology progresses, the cost rises exponentially. An efficient curative surgical service must be regarded as a cost effective component of a primary healthcare orientated system.
Keywords: Appendicitis, Complications, Cost, Model
Previously, it was reported that acute appendicitis was relatively uncommon in Southern Africa. More recent studies have suggested that the incidence of the disease in the region is increasing. 1–5 These studies also suggest that in Southern Africa, acute appendicitis presents late and is associated with significant morbidity. 1 In Southern Africa, the reported perforation rate of acute appendicitis ranges from 22% to 54%. 1–5 This is much higher than that reported in the developed world, which ranges from 14% to 22%. 1–5 This translates into considerable morbidity due to abdominal sepsis, which places a major burden on already limited resources. 6 . The primary healthcare approach that has been advocated in the developing world emphasises preventative strategies rather than curative services. 7–10 However, acute appendicitis is not amenable to primary preventative strategies. Secondary prevention aims at limiting the complications of the disease process, and this depends on early recognition and early surgery. 11
Traditionally, the public health approach has not focused on surgical services, which have been perceived as expensive curative services that benefit individuals rather than communities. 12 Despite this, there is a growing realisation that basic curative surgical care is an integral part of a comprehensive and efficient primary healthcare system. 7–9,13 The provision of appropriate curative surgical services should be an extremely cost-effective healthcare intervention in the management of acute appendicitis. 7,10 It would limit the morbidity associated with the disease in the region currently. 7 There is a paucity of published research focusing on the cost of acute appendicitis in developing countries. Our study from a regional hospital in South Africa attempts to construct a robust cost model of acute appendicitis with the intention of demonstrating the cost effectiveness of early surgical intervention in this disease compared with the cost of managing delayed advanced disease.
Methods
From September 2010 to September 2011, a prospective audit of acute appendicitis was undertaken at Edendale Hospital in Pietermaritzburg, South Africa. Patients were divided into two broad groups for analysis: uncomplicated non-perforated acute appendicitis and complicated acute appendicitis. Furthermore, the complicated appendicitis cohort was subdivided into those patients in whom perforation was associated with localised intra-abdominal contamination and those in whom it was associated with generalised four-quadrant soiling. Patients requiring intensive care unit (ICU) admission were analysed separately.
Four cost drivers were considered: cost of operative time, cost of analgesia, cost of antimicrobials and cost of hospital stay. A cost formula was constructed for each individual cost driver. Costs of consumables (antibiotics and analgesia) were obtained from the pharmacy manager, and cost of operating room and ward costs were obtained from the hospital financial manager. The sum of each individual cost drives was used to generate a total cost. The individual cost formulas are depicted in Table 1. The total cost was calculated by summation of all the individual costs.
Table 1.
Cost formulas
| Cost of operation | Cost per minute (108 ZAR) × time (mins) × number of patients |
| Cost of analgesia | Cost per day (50 ZAR) × number of days × number of patients |
| Cost of antibiotics | |
| Amoxicillin/clavulanic acid | 100 ZAR per day × number of days × number of patients |
| Gentamicin | 60 ZAR per day × number of days × number of patients |
| Piperacillin/tazobactam | 650 ZAR per day × number of days × number of patients |
| Fluconazole | 750 ZAR per day × number of days × number of patients |
| Cost of hospital stay | |
| Cost of ICU stay | 8,000 ZAR per day × mean number of days × number of patients |
| Cost of ward stay | 1,245 ZAR per day × mean number of days × number of patients |
| Cost of hospital stay (ICU cases) | Cost of ICU stay + cost of ward stay |
ICU = intensive care unit
Results
A total of 200 patients (128 male [64%], 72 female [36%]) were operated on for suspected acute appendicitis. The mean age was 22.8 years (median: 19.5 years). Of this group, 15 patients (8%) had pathologies other than appendicitis. These were excluded from our costing. Macroscopic inflammation of the appendix without perforation was found in 36% (71/200) and perforation in 57% (114/200). Of the perforated appendices, 45% (51/114) were associated with localised intra-abdominal contamination and 55% (63/114) had generalised four-quadrant soiling. The patients were divided into four groups for analysis: macroscopic inflammation without perforation (n=71), perforation with local contamination (n=51), perforation with four-quadrant contamination not requiring ICU admission (n=43), and perforation and four-quadrant contamination requiring ICU admission (n=20).
Strict antibiotic guidelines are enforced at our institution and these were used as a basis for our cost estimations. Patients with an inflamed appendix receive 24 hours of amoxicillin/clavulanic acid, a total of 3 doses of 1.2g each. Patients with perforated appendicitis receive 5 days of amoxicillin/clavulanic acid (1.2g 3 times per day for 5 days) together with gentamicin (240mg once daily for 5 days). Patients with four-quadrant sepsis who do not respond to the above regimen are converted to extended spectrum antibiotics (piperacillin/tazobactam) and an antifungal agent (fluconazole).
The cost of operating theatre time was 108 ZAR per minute. The cost of analgesia for an average patient was approximately 50 ZAR per day. For the uncomplicated group, the mean operating time was 30 minutes. All these patients received a mean of 24 hours of antibiotics and had a mean length of hospital stay of 2.5 days.
A total of 51 patients had perforation associated with localised intra-abdominal contamination. The mean operating time in this cohort was 60 minutes. All these patients received a mean of 5 days of antibiotics and the mean length of hospital stay was 5.8 days.
There were 63 patients with perforation associated with four-quadrant contamination. Twenty required ICU admission while forty-three were admitted to the general ward. The mean operating time required for each case was 90 minutes. Of the 43 patients who did not require ICU admission, the mean length of hospital stay was 9.5 days. In the cohort of 20 patients who required ICU admission, the mean length of stay in the ICU was 4.8 days. Following discharge from the ICU, the mean length of stay in the general ward was 12.9 days.
The total cost of antimicrobial therapy for the ICU was calculated based on the combination of agents used, with the mean duration of therapy derived from all patients in the group. The cost to stay in the ward was 1,245 ZAR per day and in the ICU it was 8,000 ZAR per day. The ICU daily cost included the use of the ventilator, oxygen therapy and sedation.
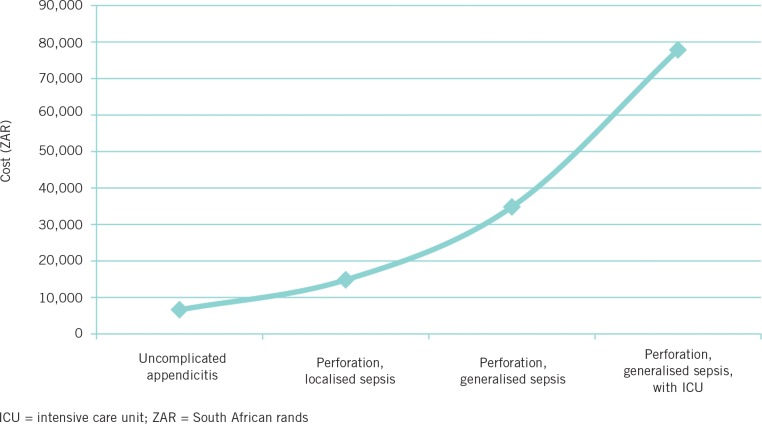
Table 2 summarises all the costs. The total cost for all 185 patients with acute appendicitis over the 12-month period was 4,272,871 ZAR. As severity of the illness increased, so costs increased exponentially (Fig 1).
Table 2.
Summary of costs
| Cost driver | Uncomplicated appendicitis (n=71) | Perforation, localised sepsis (n=51) | Perforation, generalised sepsis (n=43) | Perforation, generalised sepsis, with ICU (n=20) | Total cost |
|---|---|---|---|---|---|
| Operating time | 230,040 | 330,480 | 417,960 | 194,400 | 1,172,880 |
| Analgesia | 8,875 | 14,790 | 20,425 | 17,700 | 61,790 |
| Antibiotics | 7,100 | 40,800 | 548,250 | 255,000 | 851,150 |
| Hospital stay | 220,988 | 368,271 | 508,583 | 1,089,210 | 2,187,051 |
| Total cost | 467,003 | 754,341 | 1,495,218 | 1,556,310 | 4,272,871 |
| Mean cost for each patient (ZAR) | 6,578 | 14,791 | 34,773 | 77,816 | |
| Mean cost for each patient (GBP)* | 566 | 1,272 | 2,990 | 6,692 | |
| Mean cost for each patient (USD)* | 908 | 2,041 | 4,799 | 10,739 |
Based on yearly average exchange rate in 2011: 1 ZAR = 0.086 GBP
Based on yearly average exchange rate in 2011: 1 ZAR = 0.138 USD
Figure 1.
Cost per patient in South African rands for different patient cohorts
Discussion
Acute appendicitis represents a significant workload for the surgical services in our environment. 1,2,14,15 As in other developing countries, a multitude of factors (eg health seeking behaviour, inadequate access to healthcare facilities, failure to recognise and refer acute appendicitis and logistical difficulties) conspire to cause delay, resulting in significant morbidity. 1,16–18 Preventable morbidity translates into significant consumption of already limited resources. 7–9 While the primary prevention of acute appendicitis is not possible, the secondary prevention of morbidity is potentially achievable. Public health measures must focus on ensuring adequate access to facilities capable of recognising and treating acute appendicitis and early operative intervention. 19,20 It is important that secondary prevention of the complications of acute appendicitis is prioritised.
Accurate costing is important for administrators and policy makers. 21 The methods of estimating the direct cost of healthcare have traditionally been classified into two broad groups: 22–24 the bottom-up approach (microcosting) and the top-down approach (macrocosting). The bottom-up approach identifies and assesses the cost of each individual factor that contributes to the total cost to the healthcare system. The top-down approach uses global measures such as overall hospital stay to assign the total costs of a pathology to the healthcare system. This overall cost is then divided by the total number of patients treated to derive an estimate of average individual cost per patient. There are variations in the estimated cost using these different approaches. 25 In general, the bottom-up approach usually results in a higher but more accurate estimate. 26
A study on the cost of orthopaedic trauma in KwaZulu Natal province compared the two methods and showed a difference of approximately 10%. 23 Other studies have demonstrated that the difference can be as high as 20%. 27 The bottom-up approach is more accurate because it allocates costs based on the actual consumption of specific resources, especially those relating to administrative and other services that support patient care. These represent a significant proportion of total direct costs. 27 In general, three types of costs need to be considered: direct costs, which include hospitalisation costs, physicians costs and medication costs; indirect costs, which are those borne by the patient (eg as time off work, time of travel and productivity losses); and opportunity costs. 28,29 An opportunity cost is the cost incurred because a limited resource is being used to treat a preventable pathology. 30,31 This resource cannot therefore be used to treat another deserving pathology.
Our study confined itself to assessing the direct costs of acute appendicitis and demonstrated that the total direct cost to the service was over four million ZAR. For a patient presenting with uncomplicated appendicitis, the total direct cost was 6,578 ZAR. In other words, for less than £600 the disease is cured, morbidity is negligible and the patients (who are usually young) experience minimal disruption and loss of income. 12
Once the patient develops a perforation associated with localised intra-abdominal contamination, the direct cost doubles to 14,791 ZAR. Perforation with four-quadrant contamination that does not require ICU support sees a further doubling of direct costs to 34,773 ZAR. Once ICU support is required, the direct cost doubles again to 77,816 ZAR. This is over ten times that of an uncomplicated case. The treatment of advanced and complicated acute appendicitis accounted for 90% of the total expenditure. This implies that earlier recognition and treatment would have resulted in significant savings.
What was not considered in this study was the opportunity costs incurred in treating advanced disease, and the indirect costs borne by the patient and society in terms of lost economic activity. Consuming operating time and ICU resources for this preventable disease means that these resources cannot be used for the treatment of other pathologies. This costing is important as it shows the centrality of providing appropriate curative surgical services to a developing world health system. If secondary prevention fails, costs and morbidity rise exponentially.
Failure of secondary prevention of the complications of acute appendicitis results in major preventable cost and morbidity. In order to reduce cost and morbidity, the efforts of public health planners must be directed towards the secondary prevention of advanced abdominal sepsis. This involves a multifaceted approach that includes patient education programmes as well as efforts to increase access to healthcare facilities in rural areas and to improve the capacity of primary healthcare facilities in recognising acute appendicitis and to refer accordingly. There must be an improvement in the logistics to transfer these patients to surgical facilities.
An efficient and robust healthcare system is of the utmost importance if savings are to be achieved and morbidity is to be avoided. This costing provides convincing evidence to support the contention that efficient surgical services are a vital component of an integrated, comprehensive and cost-effective developing world healthcare service. Neglected benign surgical disease results in preventable morbidity as well as dramatically increased direct costs and opportunity costs.
Conclusions
Acute appendicitis is a common surgical pathology in our environment. If treated appropriately, early uncomplicated appendicitis has little morbidity and is relatively inexpensive to treat. As the pathology progresses from localised perforation to generalised perforation with sepsis, the cost of treating the disease rises exponentially. Improvements in so-called secondary prevention of this disease process will reduce morbidity and provide major cost savings. This study shows the importance and potential cost effectiveness of appropriate surgical services in a primary healthcare system. Without appropriate efficient surgical services, actual costs and preventable morbidity from this common disease escalate exponentially.
References
- 1.Kong VY, Bulajic B, Allorto NLet al Acute appendicitis in a developing country. World J Surg 2012; 36: 2,068–2,073 [DOI] [PubMed] [Google Scholar]
- 2.Rogers AD, Hampton MI, Bunting M, Atherstone AK. Audit of appendicectomies at Frere Hospital, Eastern Cape. S Afr J Surg 2008; 46: 74–77 [PubMed] [Google Scholar]
- 3.Madiba TE, Haffejee AA, Mbete DLet al Appendicitis among African patients at King Edward VIII Hospital, Durban, South Africa: a review. East Afr Med J 1998; 75: 81–84 [PubMed] [Google Scholar]
- 4.Levy RD, Degiannis E, Kantarovsky Aet al Audit of acute appendicitis in a black South African population. S Afr J Surg 1997; 35: 198–202 [PubMed] [Google Scholar]
- 5.Walker AR, Shipton E, Walker BFet al Appendicectomy incidence in black and white children aged 0 to 14 years with a discussion on the disease’s causation. Trop Gastroenterol 1989; 10: 96–101 [PubMed] [Google Scholar]
- 6.Salati S, Rather A, Wani S. Perforated appendicitis – an experience from a tertiary care center in Kashmir. Internet J Surg 2009; 21 [Google Scholar]
- 7.Nordberg EM, Mwobobia I, Muniu E. Major and minor surgery output at district level in Kenya: review and issues in need of further research. Afr J Health Sci 2002; 9: 17–25 [DOI] [PubMed] [Google Scholar]
- 8.Nordberg EM. Incidence and estimated need of caesarean section, inguinal hernia repair, and operation for strangulated hernia in rural Africa. BMJ 1984; 289: 92–93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nordberg E. Surgical operations in eastern Africa: a review with conclusions regarding the need for further research. East Afr Med J 1990; 67(3 Suppl): 1–28 [PubMed] [Google Scholar]
- 10.Kingsnorth AN, Oppong C, Akoh Jet al Operation Hernia to Ghana. Hernia 2006; 10: 376–379 [DOI] [PubMed] [Google Scholar]
- 11.Bickell NA, Aufses AH, Rojas M, Bodian C. How time affects the risk of rupture in appendicitis. J Am Coll Surg 2006; 202: 401–406 [DOI] [PubMed] [Google Scholar]
- 12.Neoptolemos JP, Raraty M, Finch M, Sutton R. Acute pancreatitis: the substantial human and financial costs. Gut 1998; 42: 886–891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Goosen J, Veller M. Trauma and emergency surgery: South African model. World J Surg 2008; 32: 1,622–1,625 [DOI] [PubMed] [Google Scholar]
- 14.Mason RJ. Surgery for appendicitis: is it necessary? Surg Infect 2008; 9: 481–488 [DOI] [PubMed] [Google Scholar]
- 15.Heaton KW. Aetiology of acute appendicitis. BMJ 1987; 294: 1,632–1,633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Adi AJ. Clinical presentation of appendicitis in Nigeria adults. J Med Med Sci 2011; 2: 1,147–1,151 [Google Scholar]
- 17.Farthouat P, Fall O, Ogougbemy Met al Appendicectomy in the tropics: prospective study at Hôpital Principal in Dakar. Med Trop 2005; 65: 549–553 [PubMed] [Google Scholar]
- 18.Daniel E, Marsha D. Childhood appendicitis: factors associated with its incidence and perforation in Ethiopian children. Ethiop Med J 1991; 29: 15–19 [PubMed] [Google Scholar]
- 19.Johnson AP, Ashley M, Alexander JL. The prevention of perforated appendicitis. A challenge for health education. J Natl Med Assoc 1975; 67: 46–47 [PMC free article] [PubMed] [Google Scholar]
- 20.Ball CG, Sutherland FR, Dixon Eet al Surgical trauma referrals from rural level III hospitals: should our community colleagues be doing more, or less? J Trauma 2009; 67: 180–184 [DOI] [PubMed] [Google Scholar]
- 21.Sculpher MJ, Pang FS, Manca Aet al Generalisability in economic evaluation studies in healthcare: a review and case studies. Health Technol Assess 2004; 8: 1–192 [DOI] [PubMed] [Google Scholar]
- 22.Lipscomb J, Yabroff KR, Brown MLet al Health care costing: data, methods, current applications. Med Care 2009; 47(7 Suppl 1): S1–S6 [DOI] [PubMed] [Google Scholar]
- 23.Lutge EE, Muirhead D. The epidemiology and cost of trauma to the orthopaedic department at a secondary-level hospital. S Afr J Surg 2005; 43: 74–77 [PubMed] [Google Scholar]
- 24.Allorto NL, Clarke DL, Thomson SR. A cost model case comparison of current versus modern management of burns at a regional hospital in South Africa. Burns 2011; 37: 1,033–1,037 [DOI] [PubMed] [Google Scholar]
- 25.Negrini D, Kettle A, Sheppard Let al The cost of a hospital ward in Europe: is there a methodology available to accurately measure the costs? J Health Organ Manag 2004; 18: 195–206 [DOI] [PubMed] [Google Scholar]
- 26.Clement FM, Ghali WA, Donaldson C, Manns BJ. The impact of using different costing methods on the results of an economic evaluation of cardiac care: microcosting vs gross-costing approaches. Health Econ 2009; 18: 377–388 [DOI] [PubMed] [Google Scholar]
- 27.Chapko MK, Lui CF, Perkins Met al Equivalence of two healthcare costing methods: bottom-up and top-down. Health Econ 2009; 18: 1,188–1,201 [DOI] [PubMed] [Google Scholar]
- 28.Baker JJ. Activity-based costing for integrated delivery systems. J Health Care Finance 1995; 22: 57–61 [PubMed] [Google Scholar]
- 29.Berlin MF, Smith TH. Evaluation of activity-based costing versus resource-based relative value costing. J Med Pract Manage 2004; 19: 219–227 [PubMed] [Google Scholar]
- 30.Russell LB. Opportunity costs in modern medicine. Health Aff 1992; 11: 162–169 [DOI] [PubMed] [Google Scholar]
- 31.Palmer S, Raftery J. Opportunity cost. BMJ 1999; 318: 1,551–1,552 [DOI] [PMC free article] [PubMed] [Google Scholar]