Abstract
Aims
The optimal platelet inhibition strategy for ACS patients managed without revascularization is unknown.
We aimed to evaluate efficacy and safety of ticagrelor vs. clopidogrel in the non-ST-elevation acute coronary syndrome (NSTE-ACS) subgroup of the PLATO trial, in the total cohort, and in the subgroups managed with and without revascularization within 10 days of randomization.
Methods and results
We performed a retrospective analysis of the primary endpoint of cardiovascular death/myocardial infarction/stroke. Among 18 624 PLATO patients, 11 080 (59%) were categorized as NSTE-ACS at randomization. During the initial 10 days, 74% had angiography, 46% PCI, and 5% CABG. In NSTE-ACS patients, the primary endpoint was reduced with ticagrelor vs. clopidogrel [10.0 vs. 12.3%; hazard ratio (HR) 0.83; 95% confidence interval (CI) = 0.74–0.93], as was myocardial infarction (6.6 vs. 7.7%; HR 0.86; 95% CI = 0.74–0.99), cardiovascular death (3.7 vs. 4.9%; HR 0.77; 95% CI = 0.64–0.93), and all-cause death (4.3 vs. 5.8%; HR 0.76; 95% CI = 0.64–0.90). Major bleeding rate was similar between treatment groups (13.4 vs. 12.6%; HR 1.07; 95% CI = 0.95–1.19), but ticagrelor was associated with an increase in non-CABG major bleeding (4.8 vs. 3.8%; HR 1.28; 95% CI = 1.05–1.56). Within the first 10 days, 5366 (48.4%) patients were managed without revascularization. Regardless of revascularization or not, ticagrelor consistently reduced the primary outcome (HR 0.86 vs. 0.85, interaction P = 0.93), and all-cause death (HR 0.75 vs. 0.73, interaction P = 0.89) with no significant increase in overall major bleeding.
Conclusion
In patients with NSTE-ACS, benefit of ticagrelor over clopidogrel in reducing ischaemic events and total mortality was consistent with the overall PLATO trial, independent of actually performed revascularization during the initial 10 days.
Keywords: Platelet inhibition, Acute coronary syndrome
See page 2055 for the editorial comment on this article (doi:10.1093/eurheartj/ehu202)
Introduction
Dual antiplatelet therapy with aspirin and a P2Y12 inhibitor is standard of care in acute coronary syndromes (ACS).1,2 Ticagrelor is the first reversibly binding direct P2Y12 inhibitor. As opposed to clopidogrel and prasugrel, it does not require enzymatic activation, and causes faster, greater, and more consistent platelet inhibition compared with clopidogrel.3,4 The Platelet Inhibition and Patient Outcomes (PLATO) trial compared ticagrelor with clopidogrel in patients with ACS. Ticagrelor was superior in preventing ischaemic events (the composite of death from vascular causes, myocardial infarction, and stroke), as well as death from any cause, without a significant increase in all-cause major bleeding. PLATO included both invasively and non-invasively managed patients. The decision on which management strategy to pursue was made by the investigator.5
The third-generation thienopyridine prasugrel is, like clopidogrel, an irreversible P2Y12 inhibitor, but with faster and more consistent platelet inhibition.6 Prasugrel, when compared with clopidogrel, reduced ischaemic events in patients with ACS planned for PCI in the Trial to Assess Improvement in Therapeutic Outcomes by Optimizing Platelet Inhibition with Prasugrel (TRITON),7 but in non-ST-elevation acute coronary syndrome (NSTE-ACS) patients planned for management without revascularization, prasugrel showed no benefit over clopidogrel in the Targeted Platelet Inhibition to Clarify the Optimal Strategy to Medically Manage Acute Coronary Syndromes (TRILOGY-ACS) trial.8
The aim of the present study was to explore the effect of ticagrelor vs. clopidogrel in the total NSTE-ACS subgroup of the PLATO trial and also stratified by initial management with or without revascularization.
Methods
Study design
The PLATO trial (ClinicalTrials.gov No. NCT00391872) was an international randomized double-blind, double-dummy phase III study comparing ticagrelor with clopidogrel in ACS. Details of the study design and overall results have been published previously.5,9 Briefly, a total of 18 624 patients were randomized to receive either ticagrelor or clopidogrel on background treatment with aspirin. The study included patients with ST-elevation MI intended for primary PCI, as well as patients with non-ST-elevation ACS, regardless if aimed for an initial invasive or non-invasive treatment strategy. It adhered to the Declaration of Helsinki, to the specifications of the International Conference of Harmonization, and to Good Clinical Practice; and was approved by national and institutional regulatory authorities and ethics committees. All participants provided written informed consent.
Patients
Two or more of the following inclusion criteria were required for patients enrolled without ST-elevation ACS at admission: (1) ST-segment changes on ECG indicating ischaemia [ST-segment depression or transient elevation (≥1 mm) in at least two contiguous leads]; (2) positive biomarker indicating myocardial necrosis (troponin I or T or CK-MB above the upper limit of normal); (3) one of the following: ≥60 years of age, previous myocardial infarction or coronary artery bypass surgery, coronary artery disease with ≥50% stenosis in ≥2 vessels, previous ischaemic stroke, transient ischaemic attack (TIA), carotid stenosis, cerebral revascularization, diabetes mellitus, peripheral artery disease, or chronic renal dysfunction.
In the current analysis, NSTE-ACS was in the data-base defined as absence of either persistent ST-segment elevation of 1 mV for 20 min in two contiguous leads or new (or presumed new) left bundle branch block in entry ECG. In addition to the overall NSTE-ACS population, we also analysed outcomes in the subgroups of NSTE-ACS patients who initially underwent revascularization and those who were treated without early revascularization. Both cohorts required endpoint-free survival for 10 days post-randomization to determine revascularization status. The no-revascularization subgroup was defined as NSTE-ACS patients who did not undergo any revascularization procedure (PCI or CABG) with or without angiography during the first 10 days.
Endpoints
The primary efficacy endpoint of the present study was the composite of cardiovascular death, myocardial infarction, (excluding silent infarctions) and stroke. Each component alone and all-cause death were secondary efficacy endpoints. Major bleeding by PLATO criteria9 and life-threatening/fatal bleeding were the primary safety endpoints. Secondary safety endpoints were CABG-related major bleeding, non-CABG-related major bleeding, minor bleeding, intracranial bleeding, and fatal bleeding. Additional secondary safety outcomes were bleeding events as defined by TIMI (major, minor, and non-CABG related major) and GUSTO (severe and moderate). An independent central adjudication committee, unaware of treatment assignments, assessed all endpoints. Major bleeding as defined by TIMI was recorded from the electronic case report form, where a drop of 50 g/L in haemoglobin was used as a cut-off, but this did not necessarily require clinical evidence of bleeding.
Statistical analyses
Patient characteristics and medical history, in-hospital procedures and medications, discharge ACS status, and post-discharge medications are presented by treatment in the NSTE-ACS patient cohort as well as by revascularization status subgroup. Continuous variables are presented as median and 25th–75th percentiles; categorical variables are presented as number and percentage. The treatment effect of ticagrelor vs. clopidogrel on the primary and secondary endpoints was compared within the subgroup of NSTE-ACS patients. Kaplan–Meier estimated event rates at 360 days and total number of observed events during the study were presented for each endpoint. Hazard ratios (HR), confidence intervals (CI), and P-values from unadjusted Cox proportional hazards regression models were presented. Kaplan–Meier estimated event rates were plotted by treatment for the primary efficacy endpoint, all-cause death, major bleeding, and non-CABG related major bleeding.
To examine whether the effect of ticagrelor in patients with NSTE-ACS differed based on early revascularization, Cox proportional hazards models were fitted for each endpoint using a treatment-by-revascularization interaction term. In these models, we adjusted for region of the world to account for differences in revascularization practice and the time-to-event was measured from a landmark at 10 days post-randomization. Kaplan–Meier rates 350 days post-landmark are presented for each treatment/revascularization category along with HR for ticagrelor vs. clopidogrel in the revascularization and medical management subgroups. Interaction P-values assess whether the treatment effect is different depending on revascularization status. Kaplan–Meier event rates adjusted for region are plotted by the four treatment/revascularization categories for the primary efficacy endpoint, all-cause death, major bleeding, and non-CABG related major bleeding. For consistency with the PLATO design paper,9 we also performed a 30-day landmark analysis; and as a sensitivity analysis, we also performed a 10-day landmark analysis of the full study population. Finally, the association of treatment with the primary efficacy endpoint was evaluated within several patient cohorts using Cox proportional hazards models, separately within the revascularization and non-revascularization subgroups. Forest plots present the HR for ticagrelor vs. clopidogrel in each subgroup cohort. Endpoints are defined using intent to treat and a P-value of 0.05 is used to denote statistical significance. Data were analysed using SAS version 9.2 for all analyses.
Results
Patient characteristics
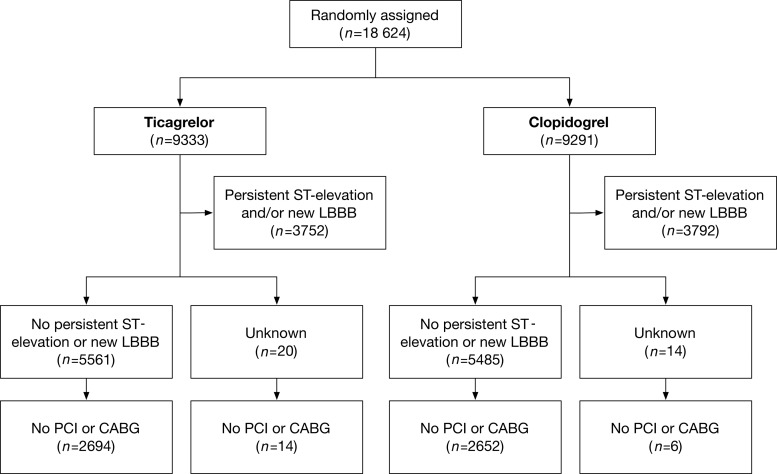
The PLATO trial included 18 624 patients with ACS, of which 11 080 patients were classified as NSTE-ACS at randomization. Of these, 5581 were randomized to ticagrelor and 5499 to clopidogrel (Figure 1). The baseline and in-hospital characteristics were similar between groups in the overall NSTE-ACS population (Table 1). In the overall NSTE-ACS group, 74% of patients had a coronary angiography performed, 46% underwent PCI, and 5% CABG. The discharge diagnosis (in this population categorized as NSTE-ACS at admission) was NSTEMI in 65%, STEMI in 8%, and unstable angina/other in 27%.
Figure 1.
Trial profile—patients classified by entry ECG and by treatment during the first 10 days after randomization.
Table 1.
Baseline characteristics and invasive procedures by randomized treatment in the overall NSTE-ACS population, and by initial treatment strategy (within the first 10 days after randomization)
| Overall NSTE-ACS |
NSTE-ACS with revascularization |
NSTE-ACS without revascularization |
||||
|---|---|---|---|---|---|---|
| Ticagrelor (N = 5581) | Clopidogrel (N = 5499) | Ticagrelor (N = 2873) | Clopidogrel (N = 2841) | Ticagrelor (N = 2708) | Clopidogrel (N = 2658) | |
| Demographics | ||||||
| Age, median (25th–75th percentile), years | 64 (56–72) | 64 (56–72) | 63 (55–71) | 63 (55–71) | 65 (57–73) | 65 (57–73) |
| Age ≥ 75 years, n (%) | 955 (17.1) | 1024 (18.6) | 420 (14.6) | 460 (16.2) | 535 (19.8) | 564 (21.2) |
| Female gender, n (%) | 1746 (31.3) | 1746 (31.8) | 706 (24.6) | 716 (25.2) | 1040 (38.4) | 1030 (38.8) |
| Body weight <60 kg, n (%) | 398 (7.2) | 389 (7.1) | 165 (5.8) | 172 (6.1) | 233 (8.6) | 217 (8.2) |
| Body mass index, median (25th–75th percentile), kg/m2 | 27.5 (24.8–30.8) | 27.4 (24.8–30.5) | 27.5 (24.9–30.8) | 27.5 (24.9–30.5) | 27.5 (24.7–30.6) | 27.3 (24.6–30.5) |
| GRACE risk score nomogram | 130 (112–150) | 130 (112–149) | 128 (110–145) | 127 (110–145) | 133 (114–154) | 134 (116–153) |
| Cardiovascular risk factors, n (%) | ||||||
| Current smoking | 1636 (29.4) | 1640 (29.9) | 1000 (34.8) | 960 (33.8) | 636 (23.6) | 680 (25.6) |
| Hypertension | 3915 (70.2) | 3835 (69.8) | 1881 (65.5) | 1886 (66.4) | 2034 (75.3) | 1949 (73.4) |
| Dyslipidaemia | 2885 (51.8) | 2852 (51.9) | 1515 (52.8) | 1569 (55.2) | 1370 (50.7) | 1283 (48.3) |
| Diabetes mellitus | 1608 (28.9) | 1520 (27.7) | 756 (26.3) | 747 (26.3) | 852 (31.6) | 773 (29.1) |
| Medical history, n (%) | ||||||
| Angina pectoris | 2932 (52.6) | 2890 (52.6) | 1337 (46.5) | 1356 (47.7) | 1595 (59.1) | 1534 (57.8) |
| Myocardial infarction | 1400 (25.1) | 1410 (25.7) | 609 (21.2) | 608 (21.4) | 791 (29.3) | 802 (30.2) |
| Congestive heart failure | 397 (7.1) | 429 (7.8) | 99 (3.4) | 103 (3.6) | 298 (11.0) | 326 (12.3) |
| Percutaneous coronary intervention (PCI) | 944 (16.9) | 918 (16.7) | 537 (18.7) | 517 (18.2) | 407 (15.1) | 401 (15.1) |
| Coronary artery bypass graft (CABG) | 434 (7.8) | 474 (8.6) | 214 (7.4) | 218 (7.7) | 220 (8.1) | 256 (9.6) |
| Transient ischaemic attack | 185 (3.3) | 189 (3.4) | 82 (2.9) | 74 (2.6) | 103 (3.8) | 115 (4.3) |
| Non-hemorrhagic stroke | 246 (4.4) | 243 (4.4) | 81 (2.8) | 98 (3.5) | 165 (6.1) | 145 (5.5) |
| Peripheral arterial disease | 400 (7.2) | 413 (7.5) | 174 (6.1) | 204 (7.2) | 226 (8.4) | 209 (7.9) |
| Chronic renal disease | 273 (4.9) | 279 (5.1) | 117 (4.1) | 108 (3.8) | 156 (5.8) | 171 (6.4) |
| Physical findings, median (25th–75th percentile) | ||||||
| Heart rate (bpm) | 72 (64–80) | 72 (64–81) | 71 (62–80) | 72 (63–80) | 72 (64–82) | 72 (64–82) |
| Systolic blood pressure (mmHg) | 135 (120–150) | 134 (120–150) | 135 (120–150) | 135 (120–150) | 134 (120–150) | 132 (120–150) |
| Diastolic blood pressure (mmHg) | 80 (70–89) | 80 (70–87) | 80 (70–89) | 80 (70–87) | 80 (70–89) | 80 (70–87) |
| Risk indicators, n (%) | ||||||
| Troponin positive, n (%) | 4356 (80.8) | 4323 (81.3) | 2522 (89.6) | 2486 (89.3) | 1834 (71.3) | 1837 (72.4) |
| ST depression (≥1 mm) | 3158 (56.8) | 3201 (58.4) | 1547 (54.0) | 1535 (54.2) | 1611 (59.8) | 1666 (62.8) |
| TIMI risk score > 2 | 4838 (89.7) | 4785 (89.8) | 2584 (91.3) | 2566 (91.8) | 2254 (88.0) | 2219 (87.7) |
| Type of ACS at discharge, n (%) | ||||||
| STEMI | 449 (8.1) | 437 (8.0) | 330 (11.5) | 305 (10.7) | 119 (4.4) | 132 (5.0) |
| NSTEMI | 3605 (64.8) | 3525 (64.3) | 2045 (71.2) | 2025 (71.3) | 1560 (58.0) | 1500 (56.7) |
| UA/other | 1509 (27.1) | 1524 (27.8) | 497 (17.3) | 510 (18.0) | 1012 (37.6) | 1014 (38.3) |
| Antithrombotic treatment during index hospitalization, n (%) | ||||||
| Aspirin | 5386 (96.6) | 5316 (96.8) | 2797 (97.4) | 2779 (97.8) | 2589 (95.9) | 2537 (95.8) |
| Unfractionated heparin | 2910 (52.1) | 2856 (51.9) | 1845 (64.2) | 1845 (64.9) | 1065 (39.3) | 1011 (38.0) |
| Low molecular weight heparin | 3181 (57.0) | 3084 (56.1) | 1568 (54.6) | 1501 (52.8) | 1613 (59.6) | 1583 (59.6) |
| Fondaparinux | 194 (3.5) | 191 (3.5) | 87 (3.0) | 76 (2.7) | 107 (4.0) | 115 (4.3) |
| Bivalirudin | 140 (2.5) | 133 (2.4) | 135 (4.7) | 122 (4.3) | 5 (0.2) | 11 (0.4) |
| GP IIb/IIIa inhibitor | 1170 (21.0) | 1117 (20.3) | 982 (34.2) | 963 (33.9) | 188 (6.9) | 154 (5.8) |
| Other drug from randomization to end of study, n (%) | ||||||
| Beta-blocker | 4768 (85.4) | 4685 (85.2) | 2536 (88.3) | 2512 (88.4) | 2232 (82.4) | 2173 (81.8) |
| ACE-inhibitor and/or ARB | 4693 (84.2) | 4602 (83.8) | 2447 (85.2) | 2433 (85.6) | 2246 (83.2) | 2169 (81.9) |
| Statin | 5196 (93.1) | 5109 (92.9) | 2777 (96.7) | 2745 (96.6) | 2419 (89.3) | 2364 (88.9) |
| Proton-pump inhibitor | 2776 (49.7) | 2613 (47.5) | 1618 (56.3) | 1536 (54.1) | 1158 (42.8) | 1077 (40.5) |
| Calcium channel inhibitor | 1553 (27.8) | 1515 (27.6) | 720 (25.1) | 723 (25.4) | 833 (30.8) | 792 (29.8) |
| Diuretic | 2393 (42.9) | 2280 (41.5) | 1073 (37.3) | 1037 (36.5) | 1320 (48.9) | 1243 (46.9) |
| Invasive procedures | ||||||
| Coronary angiography | ||||||
| During first 10 days, n (%) | 4143 (74.5) | 4072 (74.2) | 2873 (100.0) | 2841 (100.0) | 1270 (47.2) | 1231 (46.6) |
| After first 10 days, n (%) | 357 (6.4) | 335 (6.1) | 0 (0) | 0 (0) | 357 (13.3) | 335 (12.7) |
| PCI | ||||||
| During first 10 days, n (%) | 2590 (46.4) | 2550 (46.4) | 2590 (90.1) | 2550 (89.8) | 0 (0) | 0 (0) |
| After first 10 days, n (%) | 279 (5.0) | 291 (5.3) | 11 (0.4) | 3 (0.1) | 268 (9.9) | 288 (10.8) |
| CABG | ||||||
| During first 10 days, n (%) | 296 (5.3) | 305 (5.5) | 296 (10.3) | 305 (10.7) | 0 (0) | 0 (0) |
| After first 10 days, n (%) | 382 (6.8) | 375 (6.8) | 55 (1.9) | 55 (1.9) | 327 (12.1) | 320 (12.0) |
At 10 days post-randomization, 5366 patients were alive and had not undergone revascularization. There were regional differences in the proportion of patients undergoing revascularization during the initial 10 days (Asia/Australia 44%, Central/South America 40.3%, Europe/Middle East/Africa 49.8%, North America 71.6%). Non-revascularized and revascularized patients were of similar age (63 vs. 65), but patients who did not undergo revascularization were more likely to be of female gender (39 vs. 25%), and more likely to have comorbidities (e.g. previous myocardial infarction, heart failure, renal disease). Although non-revascularized patients had more comorbidities, they were less likely to be troponin I positive (Table 1). The proportion of patients with TIMI risk score >2 was slightly higher in the revascularization group (92 vs. 88%). During the first 10 days, 47% of non-revascularized patients underwent coronary angiography. When including only those who had angiography during the initial 10 days, female gender was more common in the non-revascularized (36%) than revascularized (25%). No significant coronary artery disease at angiography was noted in 32 and 0.7% of the non-revascularized and revascularized, respectively.
Efficacy in the overall non-ST-elevation acute coronary syndrome population
Efficacy and safety outcomes of the overall NSTE-ACS population are summarized in Table 2, and Kaplan–Meier curves are shown in Supplementary material online. The incidence of the primary composite endpoint was reduced with ticagrelor vs. clopidogrel (10.0 vs. 12.3%; HR 0.83; 95% CI = 0.74–0.93; P = 0.0013) (see Supplementary material online, Figure S1A). Cardiovascular death occurred less often in the ticagrelor group than in the clopidogrel group (3.7 vs. 4.9%; HR 0.77; 95% CI = 0.64–0.93; P = 0.0070), and myocardial infarction was also less common with ticagrelor vs. clopidogrel (6.6 vs. 7.7%; HR 0.86; 95% CI = 0.74–0.99; P = 0.0419), whereas stroke incidence did not differ significantly between treatment arms (1.3 vs. 1.4%; HR 0.95; 95% CI 0.69–1.33; P = 0.79). All-cause death was reduced in those treated with ticagrelor vs. clopidogrel (4.3 vs. 5.8%; HR 0.76; 95% CI = 0.64–0.90; P = 0.0020) (see Supplementary material online, Figure S1B).
Table 2.
Efficacy and safety outcomes in patients with NSTE-ACS
| Ticagrelor % (n) | Clopidogrel % (n) | HR (95% CI) | P-value | |
|---|---|---|---|---|
| Efficacy endpoints | ||||
| CV death/MI (excluding silent)/stroke | 10.0 (533) | 12.3 (630) | 0.83 (0.74, 0.93) | 0.0013 |
| All-cause death/MI(excl. silent)/stroke | 10.5 (557) | 13.0 (664) | 0.82 (0.73, 0.92) | 0.0006 |
| CV death/MI(all)/stroke/severe recurrent ischaemia/recurrent ischaemia/TIA/arterial thrombotic event | 15.5 (824) | 17.8 (918) | 0.88 (0.80, 0.96) | 0.0058 |
| Myocardial infarction (excluding silent) | 6.6 (345) | 7.7 (392) | 0.86 (0.74, 0.99) | 0.0419 |
| Cardiovascular death (includes vascular and unknown deaths) | 3.7 (194) | 4.9 (247) | 0.77 (0.64, 0.93) | 0.0070 |
| Stroke | 1.3 (69) | 1.4 (71) | 0.95 (0.69, 1.33) | 0.79 |
| All-cause death | 4.3 (224) | 5.8 (290) | 0.76 (0.64, 0.90) | 0.0020 |
| Safety endpoints | ||||
| Major bleeding (study criteria) | 13.4 (660) | 12.6 (618) | 1.07 (0.95, 1.19) | 0.26 |
| Major or minor bleeding (study criteria) | 18.2 (900) | 16.3 (794) | 1.14 (1.03, 1.25) | 0.0078 |
| Non-CABG related major bleeding (study criteria) | 4.8 (225) | 3.8 (176) | 1.28 (1.05, 1.56) | 0.0139 |
| Fatal bleeding | 0.3 (13) | 0.4 (18) | 0.72 (0.35, 1.47) | 0.37 |
| Life threatening or fatal bleeding (study criteria) | 6.6 (331) | 6.5 (315) | 1.05 (0.90, 1.22) | 0.56 |
| Intracranial bleeding | 0.3 (14) | 0.2 (7) | 2.01 (0.81, 4.99) | 0.13 |
| Other major bleeding | 7.2 (344) | 6.6 (318) | 1.08 (0.93, 1.25) | 0.34 |
| Major bleeding (TIMI criteria) | 9.2 (452) | 8.7 (422) | 1.07 (0.94, 1.22) | 0.33 |
| Major or minor bleeding (TIMI criteria) | 13.2 (653) | 12.3 (602) | 1.08 (0.97, 1.21) | 0.16 |
| Non-CABG related major bleeding (TIMI criteria) | 2.9 (137) | 2.2 (99) | 1.39 (1.07, 1.80) | 0.0131 |
| GUSTO severe bleeding | 3.1 (146) | 3.2 (151) | 0.96 (0.77, 1.21) | 0.74 |
| GUSTO moderate or severe bleeding | 8.6 (416) | 7.8 (382) | 1.08 (0.94, 1.25) | 0.25 |
Each treatment group is summarized as Kaplan–Meier rates at 360 days and total number of events during the study. P-values and hazard ratios (95% CI) come from unadjusted Cox models testing ticagrelor vs. clopidogrel.
Safety
With ticagrelor when compared with clopidogrel, there was no significant difference in PLATO major bleeding (13.4 vs. 12.6%; HR 1.07; 95% CI = 0.95–1.19; P = 0.26), but a higher rate of non-CABG-related major bleeding (4.8 vs. 3.8%; HR 1.28; 95% CI = 1.05–1.56; P = 0.0139) (see Supplementary material online, Figure S2A and B). There was no significant difference in the rate of life-threatening or fatal bleeding (6.6 vs. 6.5%; HR 1.05; 95% CI = 0.90–1.22, P = 0.56), nor any significant difference in the rate of intracranial bleeding with ticagrelor compared with clopidogrel (0.3 vs. 0.2%; HR 2.01; 95% CI = 0.81–4.99; P = 0.13). The composite of major or minor bleeding (by PLATO criteria) occurred more often in the ticagrelor group (18.2 vs. 16.3%; HR 1.14; 95% CI = 1.03–1.25, P = 0.0078). When assessed by TIMI criteria, there was no significant difference in major or minor bleeding (13.2 vs. 12.3%; HR 1.08; 95% CI = 0.97–1.21; P = 0.16). TIMI major bleeding, GUSTO severe, and GUSTO moderate or severe bleeding also did not appear to differ significantly between ticagrelor and clopidogrel, whereas TIMI non-CABG-related major bleeding was more common in the ticagrelor group (Table 2).
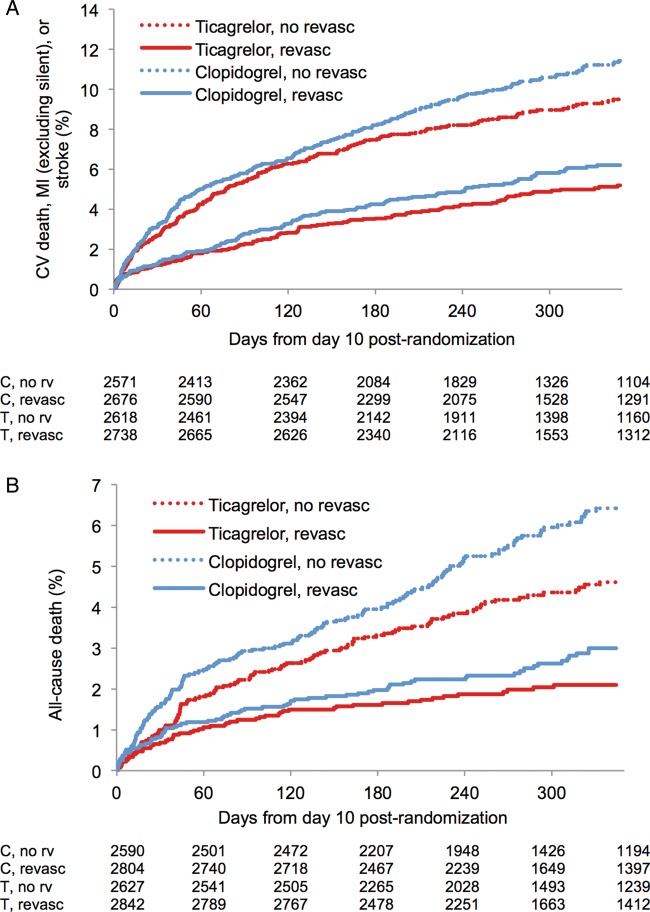
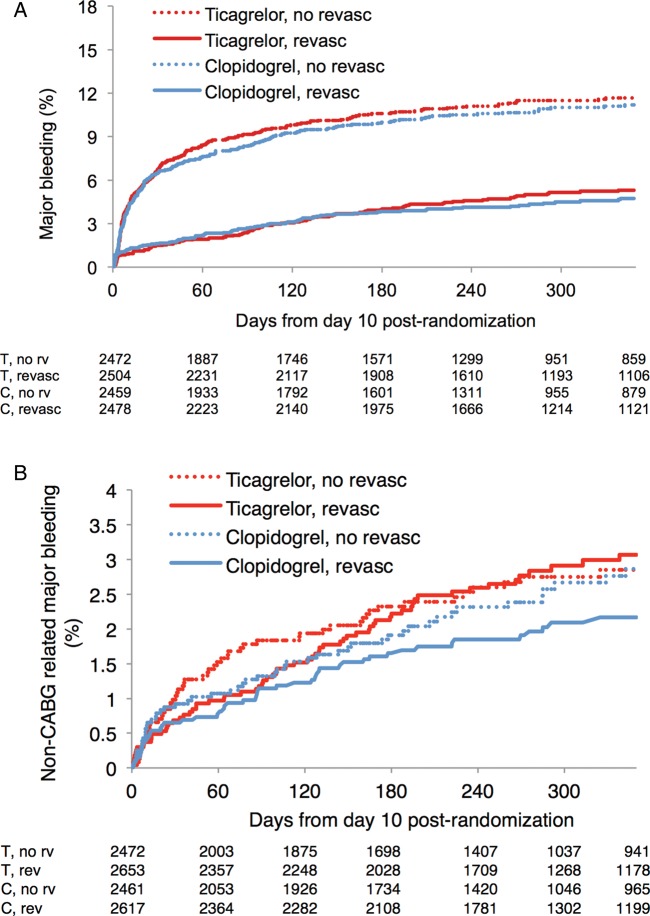
Efficacy and safety according to treatment strategy
Event rates were considerably higher in NSTE-ACS patients treated without revascularization compared with patients undergoing revascularization during the initial 10 days. For both revascularized and non-revascularized patients, there were similar proportional reductions of the primary endpoint with ticagrelor compared with clopidogrel (HR 0.86 vs. 0.85, interaction P = 0.93) (Figure 2A, Table 3) consistent with the overall trial. There was also a consistent reduction in all-cause death (HR 0.75 vs. 0.73; interaction P = 0.89) (Figure 2B). No significant difference in overall major bleeding was seen with ticagrelor vs. clopidogrel within each treatment strategy (revascularization/no revascularization) (Figure 3A). There was a higher incidence of non-CABG-related major bleeding with ticagrelor vs. clopidogrel in patients with NSTE-ACS with no significant interaction by invasive treatment strategy (HR 1.32 vs. 1.07; interaction P = 0.43) (Figure 3B). The primary outcome was reduced in major subgroups in both revascularized and non-revascularized patients (see Supplementary material online, Figures S3 and S4). The results were consistent with a 30-day landmark for revascularization (see Supplementary material online, Table S1), as well as in the full study population (see Supplementary material online, Table S2). In patients who underwent angiography during the initial 10 days with or without significant coronary disease, the effect of ticagrelor vs. clopidogrel was consistent (see Supplementary material online, Table S3).
Figure 2.
Efficacy endpoints stratified by management strategy—Kaplan–Meier estimates of time to first occurrence of: (A) primary endpoint, (B) all-cause death, from 10 days post-randomization onward.
Table 3.
Interaction of ticagrelor treatment and revascularization within 10 days (adjusting for region)
| NSTE-ACS with revascularization |
NSTE-ACS without revascularization |
Interaction P | |||||||
|---|---|---|---|---|---|---|---|---|---|
| N | Ticagrelor KM rate | Clopidogrel KM rate | HR (95% CI) | N | Ticagrelor KM rate | Clopidogrel KM rate | HR (95% CI) | ||
| Efficacy endpoints | |||||||||
| CV death/MI (excluding silent)/stroke | 5416 | 5.11 | 6.10 | 0.86 (0.68, 1.09) | 5189 | 9.63 | 11.60 | 0.85 (0.72, 1.01) | 0.93 |
| All-cause death/MI (excl. silent)/stroke | 5416 | 5.44 | 6.60 | 0.85 (0.67, 1.06) | 5189 | 10.15 | 12.53 | 0.84 (0.71, 0.99) | 0.94 |
| CV death/MI (all)/stroke/severe recurrent ischaemia/recurrent ischaemia/TIA/arterial thrombotic event | 5290 | 8.73 | 10.31 | 0.86 (0.71, 1.03) | 5109 | 14.14 | 15.16 | 0.97 (0.84, 1.13) | 0.29 |
| Myocardial infarction (excluding silent) | 5438 | 3.52 | 3.88 | 0.90 (0.68, 1.21) | 5201 | 6.04 | 6.68 | 0.94 (0.75, 1.17) | 0.85 |
| Cardiovascular death (includes vascular and unknown deaths) | 5648 | 1.64 | 2.33 | 0.76 (0.52, 1.13) | 5217 | 4.07 | 5.44 | 0.75 (0.58, 0.98) | 0.95 |
| Stroke | 5632 | 0.67 | 0.59 | 1.18 (0.60, 2.34) | 5209 | 1.48 | 1.69 | 0.92 (0.58, 1.46) | 0.56 |
| All-cause death | 5648 | 2.03 | 2.88 | 0.75 (0.53, 1.07) | 5217 | 4.77 | 6.65 | 0.73 (0.57, 0.93) | 0.89 |
| Safety endpoints | |||||||||
| Major bleeding (study criteria) | 4983 | 5.25 | 4.68 | 1.10 (0.84, 1.44) | 4931 | 11.83 | 11.43 | 1.05 (0.88, 1.26) | 0.82 |
| Major or minor bleeding (study criteria) | 4842 | 7.76 | 6.35 | 1.22 (0.97, 1.54) | 4847 | 14.59 | 13.96 | 1.07 (0.91, 1.25) | 0.34 |
| Non-CABG major bleeding (study criteria) | 5270 | 3.14 | 2.38 | 1.32 (0.92, 1.90) | 4933 | 2.78 | 2.79 | 1.07 (0.74, 1.56) | 0.43 |
| Fatal or life-threatening major bleeding (study criteria) | 5173 | 2.25 | 2.01 | 1.18 (0.79, 1.76) | 4962 | 5.77 | 6.11 | 0.95 (0.75, 1.22) | 0.37 |
| Other major bleeding (study criteria) | 5178 | 3.10 | 2.85 | 1.02 (0.72, 1.45) | 4945 | 6.50 | 5.68 | 1.16 (0.91, 1.49) | 0.55 |
| Major bleeding (TIMI criteria) | 5102 | 3.42 | 2.79 | 1.21 (0.86, 1.70) | 4952 | 8.04 | 8.39 | 0.97 (0.79, 1.20) | 0.28 |
| Major or minor bleeding (TIMI criteria) | 4990 | 5.24 | 4.56 | 1.12 (0.85, 1.47) | 4933 | 11.78 | 11.16 | 1.08 (0.91, 1.29) | 0.85 |
| Non-CABG major bleeding (TIMI criteria) | 5316 | 1.88 | 1.19 | 1.66 (1.01, 2.72) | 4952 | 2.05 | 1.84 | 1.19 (0.76, 1.87) | 0.34 |
| GUSTO severe bleeding | 5286 | 1.16 | 1.49 | 0.75 (0.45, 1.26) | 4946 | 2.75 | 2.46 | 1.13 (0.77, 1.65) | 0.22 |
| GUSTO moderate or severe bleeding | 5134 | 3.93 | 3.30 | 1.13 (0.82, 1.55) | 4945 | 7.18 | 5.96 | 1.19 (0.95, 1.51) | 0.78 |
Kaplan–Meier (KM) rates 350 days after day 10 post-randomization.
Figure 3.
Bleeding stratified by revascularization—Kaplan–Meier estimate of (A) time to major bleeding according to the PLATO criteria from day 10 post-randomization, and (B) time to non-CABG major bleeding.
Discussion
In this subgroup analysis, ticagrelor compared with clopidogrel reduced the composite endpoint of cardiovascular death, myocardial infarction, and stroke as well as the individual endpoints of cardiovascular death, myocardial infarction, and all-cause death without any significant difference in major bleeding in patients with an entry diagnosis of NSTE-ACS. The event curves for the primary composite endpoint and total mortality separated continuously for the duration of the trial. The benefits with ticagrelor were observed both in patients who underwent and in those who did not undergo early revascularization, regardless whether angiography was performed or not. These results are consistent with the previously reported subgroup analysis of all ACS patients with an intended strategy (prior to randomization) of no revascularization, where about one-fifth still underwent PCI and about 4% had CABG surgery before discharge.10
Although current guidelines advocate early invasive management in NSTE-ACS,1,2 a large proportion of patients are managed non-invasively.11,12 Patients who are managed without revascularization usually have more comorbidities, higher risk of bleeding, and inferior outcome than patients who are revascularized.13 The optimal platelet inhibition strategy in these patients has been uncertain. P2Y12 inhibition has previously been shown to reduce ischaemic events in NSTE-ACS patients managed without revascularization. In the Clopidogrel in Unstable Angina to Prevent Recurrent Events (CURE) trial, which randomized NSTE-ACS patients to receive either clopidogrel or placebo (on background aspirin treatment), 64% of patients did not undergo revascularization after randomization. There were almost identical relative reductions in CV death/MI/stroke with clopidogrel in the non-invasive and invasive subgroups.14 The Clopidogrel for High Atherothrombotic Risk and Ischemic Stabilization, Management and Avoidance (CHARISMA) trial studied the addition of clopidogrel to aspirin in a stable, more heterogeneous population at risk for atherothrombotic events. Overall, the combination was not more effective than aspirin monotherapy, but a trend towards benefit was noted in those with symptomatic atherosclerotic disease, whereas a trend towards harm was seen in those included based only on multiple cardiovascular risk factors.15
This issue was also recently studied in the TRILOGY-ACS trial, in which NSTE-ACS patients intended for management without revascularization were prospectively randomized to receive either prasugrel or clopidogrel (both irreversible P2Y12 inhibitors). The results showed no significant overall benefit of prasugrel over clopidogrel during 24 months, even though the Kaplan–Meier curves for the efficacy endpoints tended to separate after 1 year,8 and with a reduction of the primary outcome in the subgroup who underwent angiography.16 In the no revascularization subgroup of the current PLATO NSTE-ACS substudy, there were consistent benefits with ticagrelor when compared with clopidogrel concerning both mortality and non-fatal ischaemic events. Although the no revascularization subgroup of the present PLATO substudy seems similar to the TRILOGY-ACS population, it is impossible to compare the effect of the respective new P2Y12 inhibitor vs. clopidogrel across the two studies. Patients with intention for treatment without revascularization were prospectively studied in TRILOGY-ACS, while the present PLATO substudy was a post hoc stratification with subgroups of revascularization/no revascularization defined post randomization and post procedures. The TRILOGY-ACS population also was of higher risk with more prevalent comorbidities such as hypertension, dyslipidaemia, and diabetes, and had higher rates of previous myocardial infarction and revascularization procedures.
In ACS patients managed with revascularization, more potent P2Y12 inhibition has been associated with better outcomes, as shown in the intention for invasive management subgroup analysis of PLATO for ticagrelor17 and in TRITON for prasugrel.7 In the Clopidogrel and Aspirin Optimal Dose Usage to Reduce Recurrent Events–Seventh Organization to Assess Strategies in Ischemic Syndromes (CURRENT OASIS-7) trial also, intensified P2Y12 inhibition with double dose clopidogrel for the first 7 days showed no significant difference in outcome in the overall population,18 but a reduction in cardiovascular events, including stent thrombosis in the pre-specified (albeit post-randomization) subgroup undergoing PCI.19
With more potent platelet inhibition, bleeding complications have usually been increasing. In TRITON-TIMI 38, where prasugrel vs. clopidogrel was evaluated in ACS, prasugrel demonstrated a reduction in thrombotic events, but at the cost of significantly increased rates of major bleeding, including fatal bleeding, particularly in patients at high bleeding risk defined as high age and low body weight.7 In TRILOGY-ACS on the other hand, which included a lower maintenance dose, prasugrel did not cause any increased major bleeding rate, including patients >75 years of age. In the present analysis, there was no significant difference in PLATO-defined total major bleeding with ticagrelor compared with clopidogrel. However, the incidence of non-CABG-related major bleeding was significantly higher in the ticagrelor group. There was no significant difference in life-threatening or fatal bleeding or major bleeding as defined by the TIMI criteria, but the composite of PLATO major/minor bleeding was increased with ticagrelor.
Study limitations
There are several limitations to this work. The sample size is large, which gives high power to detect even relatively small differences in effect that may or may not be clinically important. The revascularization/no revascularization analyses were post hoc investigations of subgroups identified post-randomization, which makes the analyses subject to potential bias. Because landmark analyses were used, the risk of time-dependent confounding is acknowledged. As sensitivity analyses, we also performed landmark analyses at 30 days instead of 10 days, with consistent results. Nevertheless, the findings reported with regard to revascularization status should be interpreted strictly as exploratory and hypothesis generating. The present results based on actual revascularization strategy support and complement those of our previous analysis based on pre-randomization intention to treat with invasive or conservative management, and the results based on performed revascularization or not are consistent with the overall NSTE-ACS results, as well as the overall PLATO results.
Conclusions
In this substudy of the PLATO trial, ticagrelor compared with clopidogrel consistently reduced the rates of ischaemic events and mortality without any difference in overall major bleeding in patients with an entry diagnosis of NSTE-ACS, and this effect was independent of whether or not early revascularization was performed. These results harmonize with the European Society of Cardiology (ESC) NSTE-ACS guidelines, which recommend ticagrelor in all patients at moderate-to-high risk of ischaemic events, regardless of initial treatment strategy.1
Supplementary material
Supplementary material is available at European Heart Journal online.
Funding
This work was supported by AstraZeneca, who funded the PLATO trial. Funding to pay the Open Access publication charges for this article was provided by Astra Zeneca.
Conflicts of interest: D.L.: Institutional research grant from AstraZeneca to perform this research; and lecture fees from AstraZeneca. C.V.: research grant from AstraZeneca to perform this research; member of the Speakers’ Bureaus for AstraZeneca, Eli Lilly & Company, and The Medicines Company. C.P.C.: research grants/support from Accumetrics, AstraZeneca, CSL Behring, Essentialis, GlaxoSmithKline, Merck, Regeneron, Sanofi, and Takeda; on advisory boards for Alnylam, Bristol-Myers Squibb, Lipimedix, and Pfizer (funds donated to charity); and holds equity in Automedics Medical Systems. R.A.H.: consulting/advisory board fees from Bristol-Myers Squibb, Sanofi, Portola Pharmaceuticals, Johnson & Johnson and Merck; grant support from Eli Lilly/Daiichi Sankyo., Merck, Portola Pharmaceuticals, Sanofi, Johnson & Johnson, Bristol-Myers Squibb, The Medicines Company, and AstraZeneca. A.H.: reports being an employee of AstraZeneca. J.M.: reports being an employee of AstraZeneca and having equity ownership. S.H.: advisory board member for AstraZeneca, Bristol-Myers Squibb, Pfizer, and Bayer; research support from GlaxoSmithKline, Pfizer, and Sanofi-Aventis. P.G.S.: research grant (to INSERM U698): NYU School of Medicine, Sanofi, Servier. Speaking or consulting: Amarin, AstraZeneca, Bayer, Boehringer-Ingelheim, Bristol-Myers-Squibb, Daiichi-Sankyo, GSK, Lilly, Medtronic, Otsuka, Pfizer, Roche, sanofi, Servier, The Medicines Company, Vivus. Stockholding: Aterovax. J.H.C.: advisory board fees from BMS, AstraZeneca, Eli Lilly/Daiichi Sankyo; consultancy fees from Merck and Servier. R.F.S.: research grants from AstraZeneca, Eli Lilly/Daiichi Sankyo, and Merck; research support from Accumetrics; honoraria from AstraZeneca, Eli Lilly/Daiichi Sankyo, Merck, Iroko, Accumetrics, and Medscape; consultancy fees from AstraZeneca, Merck, Novartis, Accumetrics, Sanofi-Aventis/Regeneron, Bristol-Myers Squibb, Eisai, Roche and Daiichi Sankyo. S.R.S.: reports no conflict of interest. L.W.: research grants from AstraZeneca, Merck & Co, Boehringer-Ingelheim, Bristol-Myers Squibb/Pfizer, GlaxoSmithKline; consultant for Merck & Co, Regado Biosciences, Evolva, Portola, C.S.L. Behring, Athera Biotechnologies, Boehringer-Ingelheim, AstraZeneca, GlaxoSmithKline, and Bristol-Myers Squibb/Pfizer; lecture fees from AstraZeneca, Boehringer-Ingelheim, Bristol-Myers Squibb/Pfizer, GlaxoSmithKline, and Merck & Co.; honoraria from Boehringer Ingelheim, AstraZeneca, Bristol-Myers Squibb/Pfizer, GlaxoSmithKline, and Merck & Co.; travel support from AstraZeneca and Bristol-Myers Squibb/Pfizer. S.K.J.: research grant from AstraZeneca, Eli Lilly, Bristol-Myers Squibb, Terumo Inc, Medtronic, and Vascular Solutions; honoraria from The Medicines Company, AstraZeneca, Eli Lilly, Bristol-Myers Squibb, and IROKO; consultant/advisory board from AstraZeneca, Eli Lilly, Merck, Medtronic, and Sanofi.
Supplementary Material
Acknowledgements
Ebba Bergman PhD, at Uppsala Clinical Research Center provided editorial assistance.
References
- 1.Hamm CW, Bassand JP, Agewall S, Bax J, Boersma E, Bueno H, Caso P, Dudek D, Gielen S, Huber K, Ohman M, Petrie MC, Sonntag F, Uva MS, Storey RF, Wijns W, Zahger D. Bax JJ, Auricchio A, Baumgartner H, Ceconi C, Dean V, Deaton C, Fagard R, Funck-Brentano C, Hasdai D, Hoes A, Knuuti J, Kolh P, McDonagh T, Moulin C, Poldermans D, Popescu BA, Reiner Z, Sechtem U, Sirnes PA, Torbicki A, Vahanian A, Windecker S, editors; Windecker S, Achenbach S, Badimon L, Bertrand M, Botker HE, Collet JP, Crea F, Danchin N, Falk E, Goudevenos J, Gulba D, Hambrecht R, Herrmann J, Kastrati A, Kjeldsen K, Kristensen SD, Lancellotti P, Mehilli J, Merkely B, Montalescot G, Neumann FJ, Neyses L, Perk J, Roffi M, Romeo F, Ruda M, Swahn E, Valgimigli M, Vrints CJ, Widimsky P, editors. Authors/Task Force Members, ESC Committee for Practice Guidelines, Document Reviewers. ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: The Task Force for the management of acute coronary syndromes (ACS) in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC) Eur Heart J. 2011;32:2999–3054. doi: 10.1093/eurheartj/ehr236. [DOI] [PubMed] [Google Scholar]
- 2.Wright RS, Anderson JL, Adams CD, Bridges CR, Casey DE, Ettinger SM, Fesmire FM, Ganiats TG, Jneid H, Lincoff AM, Peterson ED, Philippides GJ, Theroux P, Wenger NK, Zidar JP, Anderson JL, Adams CD, Antman EM, Bridges CR, Califf RM, Casey DE, Chavey WE, Fesmire FM, Hochman JS, Levin TN, Lincoff AM, Peterson ED, Theroux P, Wenger NK, Zidar JP American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. 2011 ACCF/AHA focused update incorporated into the ACC/AHA 2007 Guidelines for the Management of Patients with Unstable Angina/Non-ST-Elevation Myocardial Infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines developed in collaboration with the American Academy of Family Physicians, Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons. J Am Coll Cardiol. 2011;57:e215–e367. doi: 10.1016/j.jacc.2011.02.011. [DOI] [PubMed] [Google Scholar]
- 3.Storey RF, Husted S, Harrington R, Heptinstall S, Wilcox RG, Peters G, Wickens M, Emanuelsson H, Gurbel P, Grande P, Cannon CP. Inhibition of platelet aggregation by AZD6140, a reversible oral P2Y12 receptor antagonist, compared with clopidogrel in patients with acute coronary syndromes. J Am Coll Cardiol. 2007;50:1852–1856. doi: 10.1016/j.jacc.2007.07.058. [DOI] [PubMed] [Google Scholar]
- 4.Gurbel PA, Bliden KP, Butler K, Tantry US, Gesheff T, Wei C, Teng R, Antonino MJ, Patil SB, Karunakaran A, Kereiakes DJ, Parris C, Purdy D, Wilson V, Ledley GS, Storey RF. Randomized double-blind assessment of the ONSET and OFFSET of the antiplatelet effects of ticagrelor vs. clopidogrel in patients with stable coronary artery disease: the ONSET/OFFSET study. Circulation. 2009;120:2577–2585. doi: 10.1161/CIRCULATIONAHA.109.912550. [DOI] [PubMed] [Google Scholar]
- 5.Wallentin L, Becker RC, Budaj A, Cannon CP, Emanuelsson H, Held C, Horrow J, Husted S, James S, Katus H, Mahaffey KW, Scirica BM, Skene A, Steg PG, Storey RF, Harrington R. Freij A, Thorsén M, editors. PLATO Investigators. Ticagrelor vs. clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2009;361:1045–1057. doi: 10.1056/NEJMoa0904327. [DOI] [PubMed] [Google Scholar]
- 6.Jernberg T, Payne CD, Winters KJ, Darstein C, Brandt JT, Jakubowski JA, Naganuma H, Siegbahn A, Wallentin L. Prasugrel achieves greater inhibition of platelet aggregation and a lower rate of non-responders compared with clopidogrel in aspirin-treated patients with stable coronary artery disease. Eur Heart J. 2006;27:1166–1173. doi: 10.1093/eurheartj/ehi877. [DOI] [PubMed] [Google Scholar]
- 7.Wiviott SD, Braunwald E, McCabe CH, Montalescot G, Ruzyllo W, Gottlieb S, Neumann F-J, Ardissino D, De Servi S, Murphy SA, Riesmeyer J, Weerakkody G, Gibson CM, Antman EM TRITON-TIMI 38 Investigators. Prasugrel vs. clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2007;357:2001–2015. doi: 10.1056/NEJMoa0706482. [DOI] [PubMed] [Google Scholar]
- 8.Roe MT, Armstrong PW, Fox KAA, White HD, Prabhakaran D, Goodman SG, Cornel JH, Bhatt DL, Clemmensen P, Martinez F, Ardissino D, Nicolau JC, Boden WE, Gurbel PA, Ruzyllo W, Dalby AJ, McGuire DK, Leiva-Pons JL, Parkhomenko A, Gottlieb S, Topacio GO, Hamm C, Pavlides G, Goudev AR, Oto A, Tseng C-D, Merkely B, Gasparovic V, Corbalan R, Cinteză M, McLendon RC, Winters KJ, Brown EB, Lokhnygina Y, Aylward PE, Huber K, Hochman JS, Ohman EM the TRILOGY ACS Investigators. Prasugrel vs. clopidogrel for acute coronary syndromes without revascularization. N Engl J Med. 2012;367:1297–1309. doi: 10.1056/NEJMoa1205512. [DOI] [PubMed] [Google Scholar]
- 9.James S, Åkerblom A, Cannon CP, Emanuelsson H, Husted S, Katus H, Skene A, Steg PG, Storey RF, Harrington R, Becker R, Wallentin L. Comparison of ticagrelor, the first reversible oral P2Y(12) receptor antagonist, with clopidogrel in patients with acute coronary syndromes: Rationale, design, and baseline characteristics of the PLATelet inhibition and patient Outcomes (PLATO) trial. Am Heart J. 2009;157:599–605. doi: 10.1016/j.ahj.2009.01.003. [DOI] [PubMed] [Google Scholar]
- 10.James S, Roe MT, Cannon CP, Cornel JH, Horrow J, Husted S, Katus H, Morais J, Steg PG, Storey RF, Stevens S, Wallentin L, Harrington R PLATO Study Group. Ticagrelor vs. clopidogrel in patients with acute coronary syndromes intended for non-invasive management: substudy from prospective randomised PLATelet inhibition and patient Outcomes (PLATO) trial. BMJ. 2011;342:d3527. doi: 10.1136/bmj.d3527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Amsterdam EA, Peterson ED, Ou F-S, Newby LK, Pollack CV, Gibler WB, Ohman EM, Roe MT. Comparative trends in guidelines adherence among patients with non-ST-segment elevation acute coronary syndromes treated with invasive vs. conservative management strategies: Results from the CRUSADE quality improvement initiative. Am Heart J. 2009;158:748–754. doi: 10.1016/j.ahj.2009.09.008. e1. [DOI] [PubMed] [Google Scholar]
- 12.Alfredsson J, Lindbäck J, Wallentin L, Swahn E. Similar outcome with an invasive strategy in men and women with non-ST-elevation acute coronary syndromes: from the Swedish Web-System for Enhancement and Development of Evidence-Based Care in Heart Disease Evaluated According to Recommended Therapies (SWEDEHEART) Eur Heart J. 2011;32:3128–3136. doi: 10.1093/eurheartj/ehr349. [DOI] [PubMed] [Google Scholar]
- 13.Chan MY, Mahaffey KW, Sun LJ, Pieper KS, White HD, Aylward PE, Ferguson JJ, Califf RM, Roe MT. Prevalence, predictors, and impact of conservative medical management for patients with non-ST-segment elevation acute coronary syndromes who have angiographically documented significant coronary disease. JACC Cardiovasc Interv. 2008;1:369–378. doi: 10.1016/j.jcin.2008.03.019. [DOI] [PubMed] [Google Scholar]
- 14.Yusuf S, Zhao F, Mehta SR, Chrolavicius S, Tognoni G, Fox KK Clopidogrel in Unstable Angina to Prevent Recurrent Events Trial Investigators. Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation. N Engl J Med. 2001;345:494–502. doi: 10.1056/NEJMoa010746. [DOI] [PubMed] [Google Scholar]
- 15.Bhatt DL, Fox KAA, Hacke W, Berger PB, Black HR, Boden WE, Cacoub P, Cohen EA, Creager MA, Easton JD, Flather MD, Haffner SM, Hamm CW, Hankey GJ, Johnston SC, Mak K-H, Mas J-L, Montalescot G, Pearson TA, Steg PG, Steinhubl SR, Weber MA, Brennan DM, Fabry-Ribaudo L, Booth J, Topol EJ CHARISMA Investigators. Clopidogrel and aspirin vs. aspirin alone for the prevention of atherothrombotic events. N Engl J Med. 2006;354:1706–1717. doi: 10.1056/NEJMoa060989. [DOI] [PubMed] [Google Scholar]
- 16.Wiviott SD, White HD, Ohman EM, Fox KAA, Armstrong PW, Prabhakaran D, Hafley G, Lokhnygina Y, Boden WE, Hamm C, Clemmensen P, Nicolau JC, Menozzi A, Ruzyllo W, Widimsky P, Oto A, Leiva-Pons J, Pavlides G, Winters KJ, Roe MT, Bhatt DL. Prasugrel vs. clopidogrel for patients with unstable angina or non-ST-segment elevation myocardial infarction with or without angiography: a secondary, prespecified analysis of the TRILOGY ACS trial. Lancet. 2013;382:605–613. doi: 10.1016/S0140-6736(13)61451-8. [DOI] [PubMed] [Google Scholar]
- 17.Cannon CP, Harrington R, James S, Ardissino D, Becker RC, Emanuelsson H, Husted S, Katus H, Keltai M, Khurmi NS, Kontny F, Lewis BS, Steg PG, Storey RF, Wojdyla D, Wallentin L PLATelet Inhibition and Patient Outcomes Investigators. Comparison of ticagrelor with clopidogrel in patients with a planned invasive strategy for acute coronary syndromes (PLATO): a randomised double-blind study. Lancet. 2010;375:283–293. doi: 10.1016/S0140-6736(09)62191-7. [DOI] [PubMed] [Google Scholar]
- 18.Mehta SR, Bassand JP, Chrolavicius S, Diaz R, Eikelboom JW, Fox KAA, Granger CB, Jolly S, Joyner CD, Rupprecht H-J, Widimsky P, Afzal R, Pogue J, Yusuf S CURRENT-OASIS 7 Investigators. Dose comparisons of clopidogrel and aspirin in acute coronary syndromes. N Engl J Med. 2010;363:930–942. doi: 10.1056/NEJMoa0909475. [DOI] [PubMed] [Google Scholar]
- 19.Mehta SR, Tanguay J-F, Eikelboom JW, Jolly SS, Joyner CD, Granger CB, Faxon DP, Rupprecht H-J, Budaj A, Avezum A, Widimsky P, Steg PG, Bassand JP, Montalescot G, Macaya C, Di Pasquale G, Niemela K, Ajani AE, White HD, Chrolavicius S, Gao P, Fox KAA, Yusuf S CURRENT-OASIS 7 Trial Investigators. Double-dose vs. standard-dose clopidogrel and high-dose vs. low-dose aspirin in individuals undergoing percutaneous coronary intervention for acute coronary syndromes (CURRENT-OASIS 7): a randomised factorial trial. Lancet. 2010;376:1233–1243. doi: 10.1016/S0140-6736(10)61088-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.