Abstract
Striking variation exists in rates of feeding tube insertion for persons with dementia. For nursing home residents with advanced dementia hospitalized with an infection or dehydration, we determined whether the attending physician was a 1) hospitalist, 2) nonhospitalist generalist, 3) subspecialist or 4) a mixture of these physician types and then examined whether the rate of feeding tube insertion differed between them. Feeding tube insertions were highest when the attending was a subspecialist (11.0%) or there was a mixture of the attending physician type (15.6%) as compared to when a hospitalist or nonhospitalist generalist cared for the patient exclusively (1.6% and 2.2%, respectively). Over time, mixture of the type of attending physician caring for hospitalized dementia patients increased from 28.9% (2001) to 38.3% (2010). Efforts to improve decision-making should target improved communication amongst physicians and the education of subspecialists regarding the efficacy of feeding tubes in this population.
Introduction
It is estimated that 5.2 million persons age 65 and older are afflicted by Alzheimer’s Dementia and that 16 million persons will be afflicted by 2050.(1) Alzheimer’s Dementia is the 5th leading cause of death among those 65 and older in the US, despite being underreported on death certificates.(2, 3) The majority of family members state the desired goal of care is to focus on the patient’s comfort.(4) Nevertheless, persons with dementia are often subjected to unnecessary hospitalizations, burdensome transitions,(5) and interventions that are not consistent with the goal of comfort care.(4–6) Feeding tube insertion is an example of an intervention where the harms may outweigh the benefits from a perspective of comfort care.
Eating problems are an important concern for persons with advanced dementia with an estimated 86% of persons with advanced dementia becoming afflicted with this concern.(4) Dating back to 1999, two articles published in the Journal of the American Medical Association (JAMA)(7) and the New England Journal of Medicine(8) have questioned the efficacy of feeding tube insertion in persons suffering from advanced dementia. Newer research has confirmed these findings, demonstrating that having a feeding tube inserted is not associated with improved survival(9) and, potentially, may result in adverse effects.(10) Nonetheless, there is a ten-fold state variation in the use of feeding tubes.(11) The majority of Percutaneous Endoscopic Gastrostomy (PEG) feeding tubes in persons with dementia are inserted during a hospital stay, usually with an admitting diagnosis of infection or dehydration.(12) Regions of the country with a higher rates of transitions in the last 3 days of life or multiple hospitalizations for expected infectious complications of dementia are also more likely to have a higher rate of feeding tubes insertions prior to death.(5)
For nearly two-thirds of nursing home residents with advanced dementia, the hospital is the locus of feeding tube decisions.(12) Our research has found substantial variation in hospitals’ rate of PEG feeding tube insertions(13) and important opportunities exist to improve the process of decision-making.(14) In 2009, 69% of Medicare Beneficiaries were hospitalized in the last 90 days of life with 11% of Medicare fee-for-service decedents hospitalized 3 or more times.(15) One of the striking changes in hospital organization over the past decade has been the growth of hospitalists. Although the use of hospitalists should be viewed as an increase in specialization compared to past models in which patients received care from the same physician in the inpatient and outpatient setting(16). Hospital medicine has developed its own board certification pathways; most hospitalists are general internists (i.e., generalists). Research suggests that having a hospitalist service is associated with reduced health care costs and shorter length of stay.(17–19)
In this study, we examined use of PEG feeding tubes in hospitalized nursing home residents with advanced dementia in order to determine whether changes in the type of attending physician during hospitalization affected feeding tube utilization.
Methods
Data Sources
We utilized data from comprehensive assessments from the Minimum Data Set (MDS) that Medicare and Medicaid certified nursing homes are required to complete to evaluate nursing home residents in terms of their cognition, function, mood, and other characteristics. Cognition was assessed using the Cognitive Performance Scale which is a scale from 0 (no impairment) to 6 (severe impairment). On average, a CPS score of 4 is equivalent to a Mini Mental Status Exam (MMSE) of 6.9, indicating a profound level of impairment; while CPS scores 5 and 6 are equivalent to an average MMSE score of 5.1 and 0.4, respectively.(20) These assessments are collected at the time of admission, yearly, and with any change in the status of the patient.
Cohort definition
We studied feeding tube decision-making in fee for service Medicare beneficiaries who were long stay (>=100 days) nursing home residents with advanced dementia as measured by a CPS score of 4, 5, or 6 at two time periods separated by at least 60 days. To create a more uniform cohort, we only included subjects who were hospitalized for a urinary track infection, sepsis, pneumonia, or dehydration based on the Disease Related Group (DRG) classifications. We excluded hospital admissions with an ICU stay, surgery other than for a PEG feeding tube insertion, and required a minimum 3-day length of stay according to the Medicare hospital claims. These exclusions were chosen to reduce the chance that the attending physician might be switched due to a change in the patients’ condition, thereby reducing the potential for selection bias in the comparisons. Because length of stay may affect continuity of care, we repeated the analysis among those cases with a 3–7 day stay.
Assignment of physician specialty
Using Kuo’s claims-based definition of a hospitalist(21), we examined the growth of hospitalists (defined as 90% physician billing for evaluation and management in the acute care hospital for general internist, family practitioner, or geriatrician) acting as the attending physician for hospitalized nursing home residents with advanced dementia hospitalized for an infection or dehydration. Only one physician may submit a bill to Medicare as the attending physician on a given hospital day. On that bill, there is a unique physician identifier that allows the categorization of the specialty of the physician. The specialty listed in the Medicare Claims files is specific to the practice setting in which the service is provided and more likely than the unique physician identification number (UPIN) registry to provide the most accurate specialty data for a specific hospitalization claim.(22) Thus, these codes and claims do not reflect referral to or visits by consultants regardless of their specialty. Based on the pattern of the attending physician, we created the following categories: 1) a hospitalist acted as the attending physician; 2) a nonhospitalist generalist (i.e., a general practitioner, geriatrician, general internist, or family physician who predominately billed in the outpatient setting) acted as the attending physician; 3) subspecialist acted as the attending physician; and 4) mixture of the type of attending physicians that usually involved a sub-specialist with either a hospitalist or a nonhospitalist generalist.
Outcomes
A PEG feeding tube insertion was identified using Medicare Hospital Claims data and only those hospitalizations where a PEG feeding tube was the sole surgical procedure were included for analysis. We used billing codes to identify cases. Those codes have been documented in detail in the appendix to a previously published paper(13).
Statistical Analyses
We tabulated the characteristics of the hospitalized nursing home residents by the category of the type of attending physician into which their pattern of Medicare claims best fit. A multivariate, hospital fixed effect model was used to examine whether a feeding tube was inserted during that hospital stay after adjusting for patient age, sex, race, rural location, medical diagnoses based on Section J of MDS 2.0, the hospital admitting diagnosis, cognitive performance score(20), physical functioning as measured by the 0–28 Late Loss Activities of Daily Living scale(23), medical orders in the nursing home to limit life sustaining treatment (i.e., Do Not Resuscitate Order, Do Not Hospitalize, and physician order to limit feeding tube insertions), and the year of the hospitalization. As a sensitivity analyses, we examine only those cases with the most severe dementia (CPS score of 6) or a short hospital stay (3–7 days) to examine whether there was similar association in these sub-populations. All analyses were conducted in STATA vs. 12.
Results
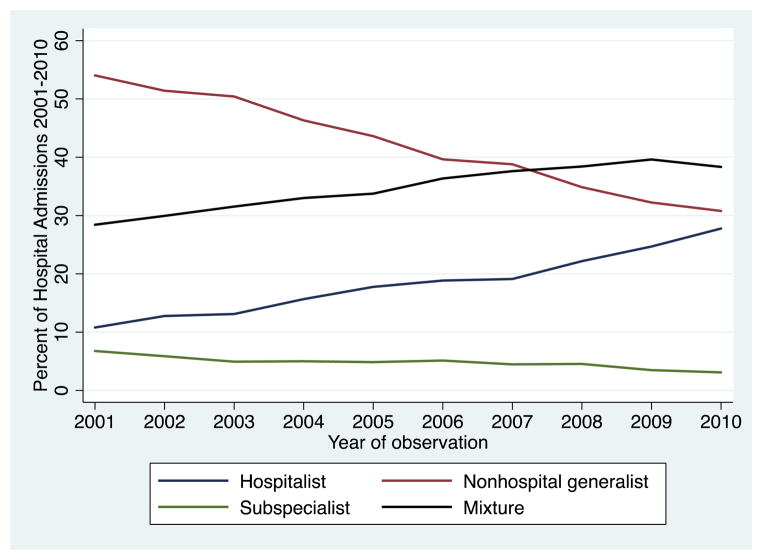
Between 2001 and 2010, we identified 53,492 hospitalizations of nursing home residents with advanced dementia (mean age 84.6, 71.4% female, 12.3% black). Over time, the proportion of such patients for which a hospitalist acted as the attending physician for the entire admission increased from 10.8% (in 2001) to 27.8% (2010). A nonhospitalist generalist, acting as the attending physician for these patients for the entire admission, decreased from 54.0% to 30.8%, while admissions characterized by a mixture of hospitalists, nonhospitalist generalist, and specialists involved in caring for such demented patients increased from 28.4% to 38.3% of all such admissions (See Exhibit 1).
Exhibit 1.
Ten year trends in the pattern of attending physician.
Source: Medicare Claims Data 2001–2010
Notes: The exhibit depicts the ten-year changes in the pattern of attending physician with a hospitalist acting as the attending physician going from 10.8% (2001) to 27.8%(2010) and a mixture of the attending physicians increasing from 28.4 (2001) to 38.3% (2010).
Characteristics of the nursing home residents cared for by these different categories of the attending physician are shown in Exhibit 2. Patients’ age and gender distributions are similar among the 4 categories of attending physician. Blacks were less likely to be cared for by nonhospitalist generalist. Care that involved either all subspecialists or a mixture of attending physician type, tend to occur in persons with lower cognitive performance scores. However, the 30-day mortality rate was similar across the four patient groups (from 23.6% to 25.1%). Nursing home residents residing in a rural region were less likely to be cared for by a subspecialist.
EXHIBIT 2.
Characteristics of Attending Physicians Types
Characteristics of hospitalized nursing home residents based on the pattern of the attending physician
| All hospitalists | All nonhospitalaist generalist | All subspecialists | Mixture of attending physicians | |
|---|---|---|---|---|
| CHARACTERISTICS | ||||
|
| ||||
| N | 8,913 | 23,850 | 2,723 | 18,006 |
| Age (Mean, SD) | 84.7 (7.3) | 84.9 (7.3) | 84.4 (7.4) | 84.2 (7.4) |
| Gender (%Female) | 72.7 | 72.3 | 68.3 | 70.1 |
|
| ||||
| MARITAL STATUS | ||||
|
| ||||
| Married (%) | 23.4 | 24.8 | 24.6 | 24.4 |
|
| ||||
| RACE | ||||
|
| ||||
| White | 82.9 | 86.3 | 73.1 | 76.6 |
| Black | 12.1 | 9.8 | 17.2 | 15.0 |
| Hispanic | 3.9 | 2.6 | 5.9 | 6.5 |
| Other race | 1.1 | 1.3 | 3.8 | 1.9 |
|
| ||||
| DISEASE | ||||
|
| ||||
| Diabetes mellitus | 26.7 | 26.2 | 25.5 | 27.2 |
| Arteriosclerotic heart | 13.2 | 15.2 | 16.4 | 15.7 |
| Congestive heart failure | 23.1 | 24.3 | 22.5 | 22.2 |
| Hip fracture | 4.9 | 4.9 | 5.4 | 4.6 |
| Cancer | 5.5 | 5.9 | 7.6 | 6.4 |
| Pneumonia | 6.2 | 6.3 | 8.1 | 6.7 |
|
| ||||
| COGNITIVE PERFORMANCE SCALE (CPS) (0–28) | ||||
|
| ||||
| 4 | 33.5 | 33.3 | 38.2 | 38.2 |
| 5 | 33.2 | 32.3 | 28.6 | 30.1 |
| 6 | 33.3 | 34.4 | 33.2 | 31.7 |
| ADL (Mean, SD) | 22.7 (5.6) | 22.8 (5.5) | 22.8 (5.6) | 22.7 (5.5) |
|
| ||||
| CLINICAL CARE PROCESSES | ||||
|
| ||||
| Do not resuscitate (DNR) | 63.0 | 63.5 | 49.6 | 52.6 |
| Feeding tube restriction | 9.9 | 10.0 | 9.8 | 8.8 |
|
| ||||
| CHARACTERISTICS OF HOSPITAL (%) | ||||
|
| ||||
| For profit | 71.8 | 70.9 | 71.0 | 72.1 |
| Medical school affiliated | 35.1 | 26.4 | 39.1 | 40.9 |
| Graduate medical education (GME) | 25.0 | 17.4 | 28.7 | 30.0 |
| Bed (Mean, SD) | 286.5 (288.2) | 220.2 (217.3) | 335.5 (247.8) | 335.9 (267.7) |
|
| ||||
| RURAL | ||||
|
| ||||
| 31.7 | 41.9 | 10.4 | 13.0 | |
|
| ||||
| 30 Day Mortality | ||||
|
| ||||
| 23.6 | 23.8 | 23.8 | 25.1 | |
Source: Medicare Claims Data 2001–2010
Notes: Exhibit 2 characterized the hospitalized NH residents with based on pattern of the attending physician finding that subspecialist and mixture of attending physician was more likely to black, less likely to have a DNR order, and more likely to receive their care at hospital with medical school affiliation.
Exhibit 3 presents the rate of PEG feeding tube insertion with and without adjustment for nursing home resident case-mix differences. Feeding tube insertions were highest when there was mixture in the type of attending physicians with a rate of 15.6% of admissions. Admissions that were cared for by hospitalists or nonhospitalist generalist for the entire stay had the lowest rate of feeding tube insertions (1.6% and 2.2%, respectively). These differences persisted after adjustment for age, gender, function, severity of dementia, and other factors. Given that changes in physicians during a hospitalization may be higher when the long length of stay is longer, we conducted a sensitivity analysis among only those subjects hospitalized for 3 and 7 days. The findings remained unchanged. A second sensitivity analyses done among subjects with the most advanced dementia defined as CPS score of 6 reflected the same conclusions.
EXHIBIT 3.
Association of Type of Physician and Feeding Tube Insertion
Association of the pattern of attending physician and the rate of feeding tube insertions.
| All hospitalists | ALL non-hospitalist Generalist | All subspecialists | Mixture of attending physicians | |
|---|---|---|---|---|
| Unadjusted Results | ||||
|
| ||||
| N | 8,913 | 23,850 | 2,723 | 18,006 |
| Feeding tube Insertion (%) | 1.6 | 2.2 | 11.0 | 15.6 |
| Feeding tube insertions among those with CPS =6 | 1.8 | 3.1 | 14.5 | 20.6 |
|
| ||||
| Adjusted Results | ||||
|
| ||||
| Feeding tube Insertion (AOR 95% CI) | 0.78 (0.62–0.99) | Reference | 5.0 (4.1–6.0) | 8.8 (7.7–10.0) |
| Feeding tube insertion among persons with CPS =6 | 0.65 (.43-.97) | Reference | 5.1 (3.7–7.1) | 9.5 (7.6–11.9) |
Source: Medicare Claims Files 2001–2010
Notes: Exhibit 3 presents the univariate and multivariate association of the type of attending physician and PEG feeding tube insertion. The PEG feeding tube insertion rate was lowest when the hospitalized NH resident was cared for by hospitalist or non-hospitalist generalist for the entire hospitalization.
Discussion
Examining hospital admissions of nursing home residents with advanced dementia, hospitalized with an infection or dehydration, we found that the type of attending physician (i.e., a hospitalist, nonhospitalist generalist, subspecialist, or mixture) influences whether a PEG feeding tube is inserted during that hospitalization. Feeding tube insertions are more common when a subspecialist provides care and when there is a mixture of nonhospitalist generalist, hospitalist and specialists taking care of a patient during hospitalization. Although the rate of care by subspecialists acting as the attending physician for the entire hospitalization has been declining slowly over time, the rate of a mixed pattern of attending physician coverage has been increasing over time. These changes suggest changes in hospital staffing patterns that may have accompanied the rise of hospitalists and the decrease in primary care physicians serving patients admitted from the nursing home.
Recent work by Kuo and colleagues utilized a Medicare claims based validated measure that identifies hospitalists to study the impact of the hospitalist as the primary provider, confirming previously reported reductions in hospital length of stay and health care costs.(24–26) Our results found that having hospitalists providing care for the entire hospital admission was not associated with an increased rate of feeding tube insertion, rather nursing home residents with advanced dementia hospitalized with an infection or dehydration cared for by a subspecialist or a mixed pattern of attending physicians were more likely to have a PEG feeding tube insertion.
While the influence of patients’ race and ethnicity has been extensively studied in decision-making for the seriously ill,(27) physician related factors such as specialty, experience in caring for patient’ disease, etc. and role in decision-making have not been extensively studied. Two papers from the Study to Understand Prognoses and Preferences for Risks and Outcomes of Treatments (SUPPORT) using a propensity match design comparing care by a subspecialist to care by a non-specialist found no difference in survival, physicians’ understanding of patient preferences, or use of life sustaining treatment for hospitalized patients with advanced Chronic Obstructive Pulmonary Disease (COPD) or cancer.(28, 29) In contrast, Auerbach and colleagues examining SUPPORT patients with Congestive Heart Failure (CHF) found those patients treated by a cardiologist received more costly care, but survived longer.(30) There are limitations to these studies since only five academic medical centers with only 38 oncologists were studied(29) and the Regueiro study(28) of COPD patients compared pulmonologists to all other physicians.
In the current national study, we examined whether the nursing home resident was cared for by a hospitalist, nonhospitalist generalist, a subspecialist, or mixture of these types of physician and whether there was an association with the rate of feeding tube insertion. Our results demonstrate that the rate of PEG feeding tube insertion was highest when a subspecialist was the attending physician for the entire hospitalization or when there was a mixture of the type of the attending physician. While it may be the case that a subspecialist would be involved in hospitalizations of sicker patients, we attempted to ameliorate this concern by examining only those hospitalizations of persons with advanced dementia associated with an infection or dehydration. Furthermore, we adjusted for the nursing home residents’ cognitive and physical functioning and their preferences as measured by documentation of Do Not Resuscitate Order or orders noted in the nursing home to limit the use of feeding tubes. Finally, two sensitivity analyses were performed finding that even if you restricted the sample to the most severe dementia cases or only those persons with a 3 to 7 day hospital stay, the results are similar.
Our finding that the subspecialist had a higher rate of PEG feeding tube insertion may also reflect their lack of experience providing care for persons with advanced dementia. The relationship between higher patient volume and better clinical outcomes has generated a large body of research over the last three decades, particularly for hospital and surgical outcomes.(31–35) Few studies have examined the effect of experience in caring for nursing home residents with a life defining illness. However, some evidence does suggest that hospices with a higher volume of persons with dementia had improved bereaved family members’ perceptions of the quality of care.(36)
Our category of the mixture of physician type may in part reflect the effect of attending physician continuity. To date, most research on provider continuity in the outpatient setting and transitions between the outpatient and hospital setting. In the outpatient setting, provider continuity is associated with reduced hospitalization and fewer emergency room visits.(37) Few studies have examined the discontinuity that may occur when hospitalists’ act as the attending physician. For example, Epstein and colleagues found that discontinuity of the attending physician was associated with a longer length of stay. A 10% increase in fragmentation of the attending physician role was associated with an increase of 0.39 days of hospital length of stay for pneumonia.(38)
Policy Implications
Some have cautioned that the growth of the hospitalist movement has introduced a new physician, thereby diminishing the involvement of the primary care physician. While Kuo and colleagues observed reductions in hospital length of stay and health care costs with the increasing use of hospitalists(24–26) they also found that patients cared for by a hospitalist were less likely to be discharged home and experienced a higher 30-day hospital readmission rate. Our research focusing on frail, older persons with advanced dementia found a lower rate of PEG feeding tube insertions when the hospitalist cared for the patient throughout the entire hospitalization. However, we also see that a change in the type of the physician serving as the “attending” during the course of the hospitalization was associated with a higher rate of PEG feeding tube insertions. Future research is needed to understand these findings. There may be a lack of care coordination when there is a handoff of patients’ care between attending physicians, some of whom may be more likely to make referrals when patients aren’t eating, an action that likely begins the cascade of events that end with a PEG feeding tube insertion. Increasing educational interventions to ensure that subspecialists are aware of the risks and benefits of feeding tube insertion in persons with advanced dementia is prudent, especially in light of official recommendations and best practice guidelines. The American Academy of Hospice and Palliative Medicine and American Geriatrics Society both recommend hand feeding rather than a feeding tube for this patient population.
High quality medical tries to make sure that the right persons gets the right care in the right location. An important policy question our study raises is the appropriateness of hospitalizing frail, older institutionalized persons with advanced dementia. Interviews with family member of persons with advanced dementia find their overwhelming goal is comfort.(4) Furthermore, emerging research finds that patients with pneumonia can be managed safely in the nursing home setting. Both a randomized control trial of pneumonia treatment in nursing home residents(39) and observation studies find that a pneumonia can often be treated in the nursing home setting without increases in mortality, decreases in function, or worsening health related quality of life.(40, 41)
About one in ten nursing home residents with advanced dementia have multiple hospitalizations in the last 90 days of life, often for expected complications of dementia such as pneumonia, urinary tract infection, or dehydration. Under the fee-for-service system, the incentives are to hospitalize nursing home residents with severe dementia to re-qualify that patient for skilled nursing home services. Bundling of payments and Institutional Special Needs Programs that reverse the financial incentives to hospitalize a nursing home resident so they qualify for skilled services in the nursing home may reduce expenditures and improve the quality of care of the nursing home resident with advanced dementia by avoiding burdensome transitions and stress of relocation for persons with advance dementia.
Conclusion
Decisions to insert a PEG feeding tube or to hospitalize patients with advanced dementia must weigh the potential benefits/burdens and should be consistent with a person’s goals and values. Our previous research has found striking variations in hospitalizations, and has shown that regions with a higher rate of such transitions also have a higher rate of PEG feeding tube insertions. Additionally, a five state study found important opportunities to improve decision-making. Here we document the fact that when the attending physician is a subspecialist, or there was a mixture of the type of attending physician, there was a higher rate of PEG feeding tube insertions. Hospitals should educate physicians about the lack of efficacy of PEG feeding tubes in persons with advanced dementia. Further, hospitals should examine how they staff the role of attending physician and ensure coordination of care with handoffs of patients changes in attending physicians.
Acknowledgments
Funding for this research was provided by National Institute on Aging Program Project Grant No. AG027296.
References
- 1.Hebert LE, Scherr PA, Bienias JL, Bennett DA, Evans DA. Alzheimer disease in the US population: prevalence estimates using the 2000 census. Arch Neurol. 2003;60(8):1119–22. doi: 10.1001/archneur.60.8.1119. [DOI] [PubMed] [Google Scholar]
- 2.Statistics NCfH. National Vital Statistics Reports. 2011 [cited 2011 August 25]. Available from: http://www.cdc.gov/nchs/data/nvsr/nvsr59/nvsr59_04.pdf.
- 3.Wachterman M, Kiely DK, Mitchell SL. Reporting dementia on the death certificates of nursing home residents dying with end-stage dementia. JAMA : the journal of the American Medical Association. 2008;300(22):2608–10. doi: 10.1001/jama.2008.768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mitchell SL, Teno JM, Kiely DK, Shaffer ML, Jones RN, Prigerson HG, et al. The clinical course of advanced dementia. N Engl J Med. 2009;361(16):1529–38. doi: 10.1056/NEJMoa0902234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gozalo P, Teno J, Mitchell SL, Skinner J, Bynum JP, Tyler D, et al. End-of-life Transitions among Nursing Home Residents with Cognitive Issues. N Engl J Med. 2011;365(13):1212–21. doi: 10.1056/NEJMsa1100347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Teno JM, Mitchell S, Rhodes R, Intrator O, Brostrup-Jenson C, Mor V. Health Care Transitions and Incident Feeding Tube Insertion Among Persons with Advanced Cognitive Impairment: Lost in Transition. Journal of the American Geriatrics Society. 2007 [Google Scholar]
- 7.Finucane TE, Christmas C, Travis K. Tube feeding in patients with advanced dementia: a review of the evidence. JAMA. 1999;282(14):1365–70. doi: 10.1001/jama.282.14.1365. [DOI] [PubMed] [Google Scholar]
- 8.Gillick MR. Rethinking the role of tube feeding in patients with advanced dementia. N Engl J Med. 2000;342(3):206–10. doi: 10.1056/NEJM200001203420312. [DOI] [PubMed] [Google Scholar]
- 9.Teno JM, Gozalo PL, Mitchell SL, Kuo S, Rhodes RL, Bynum JP, et al. Does Feeding Tube Insertion and Its Timing Improve Survival? J Am Geriatr Soc. 2012 doi: 10.1111/j.1532-5415.2012.04148.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Teno JM, Gozalo P, Mitchell SL, Kuo S, Fulton AT, Mor V. Feeding tubes and the prevention or healing of pressure ulcers. Arch Intern Med. 2012;172(9):697–701. doi: 10.1001/archinternmed.2012.1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Teno JM, Mor V, DeSilva D, Kabumoto G, Roy J, Wetle T. Use of feeding tubes in nursing home residents with severe cognitive impairment. JAMA. 2002;287(24):3211–2. doi: 10.1001/jama.287.24.3211. [DOI] [PubMed] [Google Scholar]
- 12.Kuo S, Rhodes RL, Mitchell SL, Mor V, Teno JM. Natural history of feeding-tube use in nursing home residents with advanced dementia. J Am Med Dir Assoc. 2009;10(4):264–70. doi: 10.1016/j.jamda.2008.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Teno JM, Mitchell SL, Gozalo PL, Dosa D, Hsu A, Intrator O, et al. Hospital characteristics associated with feeding tube placement in nursing home residents with advanced cognitive impairment. JAMA. 2010;303(6):544–50. doi: 10.1001/jama.2010.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Teno JM, Mitchell SL, Kuo SK, Gozalo PL, Rhodes RL, Lima JC, et al. Decision-Making and Outcomes of Feeding Tube Insertion: A Five-State Study. Journal of the American Geriatrics Society. 2011 doi: 10.1111/j.1532-5415.2011.03385.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Teno J, Gozalo P, Bynum J, Leland N, Miller S, Morden N, et al. Change in end of life care for Medicare beneficiaries: Site of death, place of care, and health care transitions 2000, 2005, and 2009. JAMA. doi: 10.1001/jama.2012.207624. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Meltzer D. Hospitalists and the doctor-patient relationship. J Legal Stud. 2001;30(2):589–606. doi: 10.1086/339294. [DOI] [PubMed] [Google Scholar]
- 17.Peterson MC. A systematic review of outcomes and quality measures in adult patients cared for by hospitalists vs nonhospitalists. Mayo Clinic proceedings Mayo Clinic. 2009;84(3):248–54. doi: 10.4065/84.3.248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.White HL, Glazier RH. Do hospitalist physicians improve the quality of inpatient care delivery? A systematic review of process, efficiency and outcome measures. BMC Med. 2011;9:58. doi: 10.1186/1741-7015-9-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Coffman J, Rundall TG. The impact of hospitalists on the cost and quality of inpatient care in the United States: a research synthesis. Medical care research and review : MCRR. 2005;62(4):379–406. doi: 10.1177/1077558705277379. [DOI] [PubMed] [Google Scholar]
- 20.Morris JN, Fries BE, Mehr DR, Hawes C, Phillips C, Mor V, et al. MDS Cognitive Performance Scale. J Gerontol. 1994;49(4):M174–82. doi: 10.1093/geronj/49.4.m174. [DOI] [PubMed] [Google Scholar]
- 21.Kuo YF, Sharma G, Freeman JL, Goodwin JS. Growth in the care of older patients by hospitalists in the United States. The New England journal of medicine. 2009;360(11):1102–12. doi: 10.1056/NEJMsa0802381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Baldwin LM, Adamache W, Klabunde CN, Kenward K, Dahlman C, JLW Linking physician characteristics and medicare claims data: issues in data availability, quality, and measurement. Med Care. 2002;40(8 Suppl):IV-82–95. doi: 10.1097/00005650-200208001-00012. [DOI] [PubMed] [Google Scholar]
- 23.Morris JN, Fries BE, Morris SA. Scaling ADLs within the MDS. J Gerontol A Biol Sci Med Sci. 1999;54(11):M546–53. doi: 10.1093/gerona/54.11.m546. [DOI] [PubMed] [Google Scholar]
- 24.Kuo YF, Goodwin JS. Association of hospitalist care with medical utilization after discharge: evidence of cost shift from a cohort study. Annals of internal medicine. 2011;155(3):152–9. doi: 10.1059/0003-4819-155-3-201108020-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Howrey BT, Kuo YF, Goodwin JS. Association of Care by Hospitalists on Discharge Destination and 30-day Outcomes After Acute Ischemic Stroke. Medical care. 2011;49(8):701–7. doi: 10.1097/MLR.0b013e3182166cb6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kuo YF, Goodwin JS. Effect of hospitalists on length of stay in the medicare population: variation according to hospital and patient characteristics. Journal of the American Geriatrics Society. 2010;58(9):1649–57. doi: 10.1111/j.1532-5415.2010.03007.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Frost DW, Cook DJ, Heyland DK, Fowler RA. Patient and healthcare professional factors influencing end-of-life decision-making during critical illness: a systematic review. Critical care medicine. 2011;39(5):1174–89. doi: 10.1097/CCM.0b013e31820eacf2. [DOI] [PubMed] [Google Scholar]
- 28.Regueiro CR, Hamel MB, Davis RB, Desbiens N, Connors AF, Jr, Phillips RS. A comparison of generalist and pulmonologist care for patients hospitalized with severe chronic obstructive pulmonary disease: resource intensity, hospital costs, and survival. SUPPORT Investigators. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatment. The American journal of medicine. 1998;105(5):366–72. doi: 10.1016/s0002-9343(98)00290-3. [DOI] [PubMed] [Google Scholar]
- 29.Rose JH, O’Toole EE, Dawson NV, Thomas C, Connors AF, Jr, Wenger N, et al. Generalists and oncologists show similar care practices and outcomes for hospitalized late-stage cancer patients. SUPPORT Investigators. Study to Understand Prognoses and Preferences for Outcomes and Risks for Treatment. Medical care. 2000;38(11):1103–18. doi: 10.1097/00005650-200011000-00005. [DOI] [PubMed] [Google Scholar]
- 30.Auerbach AD, Hamel MB, Davis RB, Connors AF, Jr, Regueiro C, Desbiens N, et al. Resource use and survival of patients hospitalized with congestive heart failure: differences in care by specialty of the attending physician. SUPPORT Investigators. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments. Annals of internal medicine. 2000;132(3):191–200. doi: 10.7326/0003-4819-132-3-200002010-00004. [DOI] [PubMed] [Google Scholar]
- 31.Halm EA, Lee C, Chassin MR. Is volume related to outcome in health care? A systematic review and methodologic critique of the literature. Annals of internal medicine. 2002;137(6):511–20. doi: 10.7326/0003-4819-137-6-200209170-00012. [DOI] [PubMed] [Google Scholar]
- 32.Birkmeyer JD, Siewers AE, Finlayson EV, Stukel TA, Lucas FL, Batista I, et al. Hospital volume and surgical mortality in the United States. The New England journal of medicine. 2002;346(15):1128–37. doi: 10.1056/NEJMsa012337. [DOI] [PubMed] [Google Scholar]
- 33.Birkmeyer JD, Finlayson EV, Birkmeyer CM. Volume standards for high-risk surgical procedures: potential benefits of the Leapfrog initiative. Surgery. 2001;130(3):415–22. doi: 10.1067/msy.2001.117139. [DOI] [PubMed] [Google Scholar]
- 34.Thiemann DR, Coresh J, Oetgen WJ, Powe NR. The association between hospital volume and survival after acute myocardial infarction in elderly patients. The New England journal of medicine. 1999;340(21):1640–8. doi: 10.1056/NEJM199905273402106. [DOI] [PubMed] [Google Scholar]
- 35.Luft HS, Bunker JP, Enthoven AC. Should operations be regionalized? The empirical relation between surgical volume and mortality. The New England journal of medicine. 1979;301(25):1364–9. doi: 10.1056/NEJM197912203012503. [DOI] [PubMed] [Google Scholar]
- 36.Miller SC, Kiely DK, Teno JM, Connor SR, Mitchell SL. Hospice care for patients with dementia: does volume make a difference? Journal of pain and symptom management. 2008;35(3):283–91. doi: 10.1016/j.jpainsymman.2007.12.001. [DOI] [PubMed] [Google Scholar]
- 37.van Walraven C, Oake N, Jennings A, Forster AJ. The association between continuity of care and outcomes: a systematic and critical review. J Eval Clin Pract. 2010;16(5):947–56. doi: 10.1111/j.1365-2753.2009.01235.x. [DOI] [PubMed] [Google Scholar]
- 38.Epstein K, Juarez E, Epstein A, Loya K, Singer A. The impact of fragmentation of hospitalist care on length of stay. J Hosp Med. 2010;5(6):335–8. doi: 10.1002/jhm.675. [DOI] [PubMed] [Google Scholar]
- 39.Loeb M, Carusone SC, Goeree R, Walter SD, Brazil K, Krueger P, et al. Effect of a clinical pathway to reduce hospitalizations in nursing home residents with pneumonia: a randomized controlled trial. JAMA. 2006;295(21):2503–10. doi: 10.1001/jama.295.21.2503. [DOI] [PubMed] [Google Scholar]
- 40.Casarett DJ. Differences between patients referred to hospice from academic vs. non-academic settings. J Pain Symptom Manage. 2001;21(3):197–203. doi: 10.1016/s0885-3924(00)00260-8. [DOI] [PubMed] [Google Scholar]
- 41.Saliba D, Kington R, Buchanan J, Bell R, Wang M, Lee M, et al. Appropriateness of the decision to transfer nursing facility residents to the hospital. J Am Geriatr Soc. 2000;48(2):154–63. doi: 10.1111/j.1532-5415.2000.tb03906.x. [DOI] [PubMed] [Google Scholar]