Abstract
There is a growing research literature suggesting that racism is an important risk factor undermining the health of Blacks in the United States. Racism can take many forms, ranging from interpersonal interactions to institutional/structural conditions and practices. Existing research, however, tends to focus on individual forms of racial discrimination using self-report measures. Far less attention has been paid to whether structural racism may disadvantage the health of Blacks in the United States. The current study addresses gaps in the existing research by using novel measures of structural racism and by explicitly testing the hypothesis that structural racism is a risk factor for myocardial infarction among Blacks in the United States. State-level indicators of structural racism included four domains: (1) political participation; (2) employment and job status; (3) educational attainment; and (4) judicial treatment. State-level racial disparities across these domains were proposed to represent the systematic exclusion of Blacks from resources and mobility in society. Data on past-year myocardial infarction were obtained from the National Epidemiologic Survey on Alcohol and Related Conditions (non-Hispanic Black: N = 8245; non-Hispanic White: N = 24,507), a nationally representative survey of the U.S. civilian, non-institutionalized population aged 18 and older. Models were adjusted for individual-level confounders (age, sex, education, household income, medical insurance) as well as for state-level disparities in poverty. Results indicated that Blacks living in states with high levels of structural racism were generally more likely to report past-year myocardial infarction than Blacks living in low-structural racism states. Conversely, Whites living in high structural racism states experienced null or lower odds of myocardial infarction compared to Whites living in low-structural racism states. These results raise the provocative possibility that structural racism may not only harm the targets of stigma but also benefit those who wield the power to enact stigma and discrimination.
Keywords: Structural racism, Stigma, Health inequalities, Cardiovascular disease
Introduction
Over the past few decades, researchers have directed considerable attention toward the study of racial discrimination and its effects on the health of Blacks in the United States. Much of this research has been undertaken with the goal of explaining racial disparities in morbidity and mortality. Indeed, despite adjustments for socioeconomic status and health behaviors, racial disparities persist in such outcomes as life expectancy and mortality from leading causes of death including heart disease, hypertension, and diabetes (CDC, 2011).
Researchers have postulated that racial discrimination is an important factor undermining the health of Blacks relative to Whites (e.g., Jones, 2000; Krieger, 2012; Williams & Mohammed, 2009). Krieger (2012), for example, proposes an “ecosocial” theory of racism and health. According to this model, racism becomes “embodied” over the life-course, adversely affecting the health of oppressed populations through multiple pathways, ranging from exposure to toxins to economic and social deprivation (Krieger, 2012). Importantly, Krieger's model highlights the potential duality of the impact of racism on health—a process that both harms subordinate social groups while providing benefits to dominant ones.
The power dynamic central to the ecosocial model is consistent with other theories of structural stigma (Link, 2014; Link & Phelan, 2001) and systemic racism (Feagin, 2000; 2006; Feagin & Bennefield, 2013). Racism may be conceptualized as a tool employed by those in power to maintain privilege and control over resources (for example, wealth, knowledge, prime land and housing) that ultimately benefit health (Link, 2014; Link & Phelan, 1995). Furthermore, as Bonilla-Silva (1997) asserts, the pervasive nature of racism, and the “racialized social systems” (p. 469) that define it, extend beyond ideology and class conflict to permeate the structure of society and shape “life chances” (p. 470) in a racialized way across multiple domains (e.g., political, social, and economic). Although structural racism as proposed in the ecosocial model is hypothesized to harm the health of Blacks while potentially bolstering that of Whites, few empirical studies have directly assessed this relationship. In outlining the ecosocial hypothesis, Krieger, Chen, Koshelva, and Waterman (2012) provide some data examining the effects of Jim Crow legislation on mortality in the United States. Comparing mortality among Whites and persons of color in states with and without Jim Crow legislation, a tiered relationship emerged (namely in the decade between 1960 and 1970), with the highest rates of mortality occurring in populations of color within Jim Crow states and the lowest rates of mortality occurring among Whites in these highly racist environments. The current study expands the literature on structural racism and encompasses two primary aims. First, we examine whether structural racism serves as a risk factor for myocardial infarction among Blacks in the United States. Second, consistent with the above theories, we evaluate whether the cardiac health of Whites is enhanced under conditions of structural racism against Blacks.
Cardiovascular health has been of particular interest to discrimination researchers (Williams & Mohammed, 2009; Wyatt et al., 2003). Indeed, multiple lines of evidence document associations between reporting discrimination and markers for cardiovascular disease among Blacks, including hypertension (Davis, Liu, Quarells, & Din-Dzietharn, 2005; Guyll, Matthews, & Bromberger, 2001; Krieger, 1990; Krieger & Sidney, 1996; Roberts, Vines, Kaufman, & James, 2007; Sims et al., 2012), subclinical carotid disease (Troxel, Matthews, Bromberger, & Sutton-Tyrrell, 2003), coronary artery calcification (Lewis et al., 2006), coronary artery obstruction (Ayotte, Hausmann, Whittle, & Kressin, 2012), elevated low-density lipoprotein (LDL) cholesterol, visceral abdominal fat deposits (Lewis, Kravitz, Janssen, & Powell, 2011), increased C-reactive protein (Lewis, Aiello, Leurgans, Kelly, & Barnes, 2010), and, in experimental designs, cardiovascular reactivity in response to acute discriminatory stress (Lepore et al., 2006; Smart Richman, Bennett, Pek, Siegler, & Williams, 2007). One of the reasons that cardiovascular health has garnered such attention among discrimination researchers is that both theoretical and empirical work indicates that discrimination serves as a chronic stressor for Black Americans (Clark, Anderson, Clark, & Williams, 1999). As such, discrimination can be linked to poor cardiovascular outcomes through stress-response systems (Dimsdale, 2008; Sawyer, Major, Casad, Townsend, & Mendes, 2012; Williams & Mohammed, 2009; Wyatt et al., 2003), providing a plausible set of biological mechanisms through which discrimination may influence myocardial infarctions. Methodologically, we focused the present study on myocardial infarctions because, unlike other self-reported health outcomes, measures of heart attack and angina have been found to be highly reliable (Bergmann, Byers, Freedman, & Mokdad, 1998; Bush, Miller, Golden, & Hale, 1989; Lampe, Walker, Lennon, Whincup, & Ebrahim, 1999).
Measuring interpersonal and structural forms of racism
Racism acts through discrimination at various levels of society, from interpersonal events (e.g., victimization) to structural (also called institutional) practices and conditions (Krieger, Rowley, Herman, Avery, & Phillips, 1993; Meyer, 2003). Interpersonal discrimination can include actions that are intentional and unintentional, and it manifests itself in several different ways, including “lack of respect, suspicion, devaluation, scapegoating, and dehumanization” (Jones, 2000, p. 1213). In contrast to forms of discrimination that occur on an individual or interpersonal level, structural discrimination refers to macro-level conditions that constrain the opportunities, resources, and well-being of socially disadvantaged groups (Link & Phelan, 2001). These conditions are embedded in structural relations that maintain and perpetuate greater social influence among majority group members (Bonilla-Silva, 1997; Jones, 2000; Link & Phelan, 2001) and are therefore considered independent of individual-level discrimination (Bonilla-Silva, 1997; Meyer, Schwartz, & Frost, 2008).
The vast majority of studies examining racial discrimination and health, including cardiovascular health, have relied on self-report measures of interpersonal events (Paradies, 2006; Williams & Mohammed, 2009). The most commonly used measures of interpersonal discrimination, or perceived discrimination, query respondents about whether they have been discriminated against in a variety of major life domains (e.g., healthcare, education, employment) or in everyday circumstances (e.g., followed in stores, called names or insulted), as a result of their race (Williams & Mohammed, 2009). These self-report, check-list measures, however, are vulnerable to measurement error. For instance, individuals who experience discrimination may not be willing to report these sensitive events (Krieger, 1999; Meyer, 2003; Williams & Mohammed, 2009) or may vary in their perceptions and interpretations of these events (Krieger, 1999; Meyer, 2003), potentially resulting in biased estimates of the relationship between discrimination and health (Krieger 1999; Meyer, 2003; Williams & Mohammed, 2009).
In addition, measures of perceived discrimination often cannot capture structural forms of discrimination (Hatzenbuehler, McLaughlin, Keyes, & Hasin, 2010; Meyer, 2003). Although a number of researchers have called for the development of such measures (Krieger, 2012; Lauderdale, 2006; Shavers et al., 2012; Williams & Mohammed, 2009), few measures of structural discrimination are currently available. There are at least three reasons for the relative absence of structural measures in the extant literature. One is the tendency of public health research to focus on individual-level risk factors, often perceived as more amenable to intervention (Feagin & Bennefield, 2013; Susser, Schwartz, Morabia, & Bromet, 2006).
A second formidable barrier lies in the identification and development of measures that legitimately represent this construct. Indeed, measuring structural racism presents a significant challenge to researchers given the shift over the past half-century from overt, and often legally sanctioned, forms of discrimination to largely “aversive” ones characterized by avoidance of racial/ethnic minorities and implicit expressions of racism (Bonilla-Silva, 1997; Dovidio & Gaertner, 2004; Gaertner & Dovidio, 1986; Krieger, 2012). Because aversive forms of racism often exist outside of conscious awareness, traditional self-report measures cannot be used to reliably evaluate this construct. Structural racism can also be obscured or “misrecognized” (Bourdieu, 1979) through processes such as White racial framing (Feagin, 2006) and “stigma power” (Link, 2014). Given the difficulty of capturing structural forms of racism that are frequently concealed, researchers have been hard pressed to find individual examples of structural racism that have adequate construct validity. Because of this challenge, the development of multiple (rather than single) indicators that represent a pattern of racial inequity at a structural level might strengthen the body of evidence in the field. Third, structural racism is often ubiquitous, making it especially difficult to identify measures that capture sufficient variation to predict health outcomes.
Existing research on structural racism and health
Given the paucity of measures of structural discrimination, relatively few studies have assessed the health effects of racism at a structural level. One exception is structural racism in the form of neighborhood context, notably neighborhood segregation, (Kramer & Hogue, 2009; Williams & Collins, 2001). Neighborhood segregation is conceptualized as an exemplar of structural racism, given policies and institutional practices (e.g., “redlining”) that prevented Blacks in the United States from living in neighborhoods where Whites predominantly resided (Williams, 1999). Early work by Harburg et al. (1973) identified a relationship between areas of high “socioecological stress” (marked by economic deprivation, residential and family instability, crime, and density) and elevated blood pressure. This relationship was stronger among Blacks compared with Whites living in Detroit. Other more recent studies have found some evidence for associations between residential segregation and hypertension (Kershaw et al., 2011; Thorpe et al., 2008). Neighborhood socioeconomic characteristics have also been linked among Blacks to risk factors for heart disease, such as blood pressure and smoking. However, the pattern of these associations has been inconsistent across locality (Diez-Roux et al., 1997; Manfredi et al., 1992).
Although neighborhood-level measures are important, indicators of structural racism extend beyond neighborhood contexts to include national, state, and local laws, institutional policies, and political infrastructures that differentially and adversely affect members of a particular racial group (Krieger, 2012). Relative to Whites, Blacks face significant disadvantages with regard to educational attainment, income, wealth, credit, employment, and incarceration (CDC, 2011; Jones, 2000; Kaufman, Cooper, & McGee, 1997; Pager & Shepherd, 2008; Uggen & Manza, 2002; Williams & Collins, 1995). This pattern of disparity reflects, and in many instances was caused by, a legacy of slavery and racial oppression in this country that continues through institutional policies and practices to advantage Whites over Blacks (Feagin, 2006; Feagin & Bennefield, 2013; Wakefield & Uggen, 2010).
Racial differences in drug related incarceration provide a particularly stark example. The enactment of anti-drug legislation (i.e., 1986 Anti-Drug Abuse Act) instituting mandatory minimum sentences and more severe punishment for crack versus powder forms of cocaine has severely and disproportionately impacted Blacks. While Whites are more likely to be convicted of powder cocaine crimes carrying more lenient penalties, Blacks are far more likely to be convicted of crack cocaine offenses (Vigins & McCurdy, 2006). At the same time, population-based surveys indicate that use of crack and other illicit drugs among Blacks is similar to, or even lower than, that among Whites (SAMSA, 2005; Vigins & McCurdy, 2006). States vary in their application of these and other drug laws, and substantially differ on disenfranchisement of individuals once convicted of a drug-related crime (Uggen & Manza, 2002). For example, in 2004, 19 states impeded drug felons from applying for temporary public assistance and 17 states did not allow drug felons to apply for food stamps. These restrictions on basic social welfare affect Blacks to a greater extent than Whites due to the systematic and well-documented inequality in punitive damages for drug offenses among Blacks compared to Whites (Drucker, 2011). In total, these restrictions create potentially deleterious institutional climates that affect participation of Black Americans in the political process, investment in their communities, and influence over future rights and policies (Schnittker, Massoglia, & Uggen, 2011; Uggen & Manza, 2002).
The current study
The current study expands upon existing research by systematically investigating the relationship between structural racism and myocardial infarction, using a national sample of both Blacks and Whites. As defined in this study, structural racism is the systematic exclusion of non-White racial groups from resources and mobility in society as a means to secure or maintain power (Carmichael & Hamilton, 1967; Feagin, 2000; Krieger, 1999). Extending beyond neighborhood-level inequality characterizing much of the work in this field, this study examines the health effects of various forms of structural racism occurring at the state level.
Focusing on variation in structural racism at the state level is one potentially profitable approach to examining structural discrimination given that states vary substantially in their past and present policies, laws, and institutional practices that systematically disadvantage Blacks, thereby creating unique cultures of racism. For example, racial differences in rates of incarceration fluctuate considerably across states. While in Iowa Blacks are imprisoned at a rate that is almost 14 times that of Whites, in Hawaii this increased rate of incarceration is only two-fold (Mauer & King, 2007). As another example, in 2011 six states passed laws that require a driver's license or other official government photo identification to vote; these laws have been demonstrated to systematically exclude racial/ethnic minorities from voting, as they are less likely than Whites to have official government identification (Parson & McLaughlin, 2007). Previous work by Hatzenbuehler, Keyes, and Hasin (2009) and Hatzenbuehler et al. (2010) has shown that state-level variation in policies and laws has substantial consequences for the health of minority groups. For example, sexual minorities (i.e., lesbians, gays, and bisexuals) living in US states with policies and laws restricting rights (e.g., constitutional amendments banning same-sex marriage, lack of protections against employment discrimination based on sexual orientation) have higher rates of substance use and psychiatric disorders. This research suggests that living in particular states can structure opportunities and resources differently for minority and majority group members and therefore that the US state is a meaningful areal unit in which to examine variation in structural racism.
Building upon this work, in the present study we examine whether state-level variation in measures of structural racism spanning political participation, employment, educational attainment, and incarceration differentially predicts the prevalence of myocardial infarction among Blacks and Whites in the United States. Drawing from the theories of structural racism presented above, we specifically hypothesize that among Blacks, structural racism will be associated with a higher prevalence of myocardial infarction. Among Whites, however, who may potentially benefit from the exploitative processes inherent in structural racism, we hypothesize that structural racism will be associated with a lower prevalence of myocardial infarction. A strong test of our research questions requires access to three kinds of data: (1) a large sample of Blacks and Whites who report myocardial infarction in sufficient numbers to allow for meaningful racial comparisons (and enhance statistical conclusion validity); (2) representation across all 50 states to provide substantial geographic variation in exposure to structural racism, which is necessary for state-level comparisons (and external validity); and (3) measures of multiple risk factors that may serve as potential confounders of the relationship between structural racism and myocardial infarction (to improve internal validity). Few datasets meet these criteria, but we were able to take advantage of one such dataset that affords a rare opportunity to explore the impact of structural racism on myocardial infarction.
Methods
Sample
This sample consists of participants in the 2001–2002 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), a nationally representative survey of the U.S. civilian, non-institutionalized population aged 18 and older. Respondents completed face-to-face interviews on a variety of topics related to mental and physical health as well as health behaviors. The National Institute on Alcohol Abuse and Alcoholism (NIAAA) sponsored the study and supervised the fieldwork, conducted by the U.S. Bureau of the Census. Young adults, Hispanics, and non-Hispanic Blacks were oversampled; the overall response rate was 81%. Further details of the sampling frame, demographics of the sample, training of interviewers and field quality control are described elsewhere (Grant et al., 2007; Grant, Moore, & Kaplan, 2003; Grant et al., 2004). The present study focuses on self-identified non-Hispanic Black (N = 8245) and non-Hispanic White (N = 24,507) participants for a total sample size of 32,752. The research protocol, including informed consent procedures, received full ethical review and approval from the U.S. Census Bureau and U.S. Office of Management and Budget.
Measures of structural racism
Our measures of structural racism included four domains: (1) political participation; (2) employment and job status; (3) educational attainment; and (4) judicial treatment. Table 1 describes the individual items that comprised these four domains as well as the sources from which these measures were obtained. Consistent with our definition of structural racism, state-level racial disparities across these domains were proposed to represent the systematic exclusion of Blacks from resources and mobility in society.
Table 1.
Description of measures of structural racism.
| Measure of structural racism | Data source/Year |
|---|---|
| Political participation | |
| Registered to vote | US Census Bureau, Current Population Survey, 2002 |
| Voted | US Census Bureau, Current Population Survey, 2002 |
| State elected officials | National Conference of State Legislatures, 2003 |
| Employment and job status | |
| Civilian labor | US Department of Labor & Statistics, 2000 |
| Employed | US Department of Labor & Statistics, 2000 |
| Executive/managerial position | US Department of Labor & Statistics, 2000 |
| Professional specialty | US Department of Labor & Statistics, 2000 |
| Educational attainment | |
| Bachelor's degree or higher | US Census Bureau, Decennial Census Data, 2000 |
| Judicial treatment | |
| Incarcerated | US Department of Justice, Bureau of Justice Statistics, 2005 |
| Disenfranchised | US Department of Justice, Bureau of Justice Statistics, 2000 |
| Death row | US Department of Justice, Bureau of Justice Statistics, 2002 |
Under political participation, measures included the relative proportions of Blacks to Whites in each state who were registered to vote, who actually voted, and who were elected to the state legislature. Data for voting registration and practice were derived from the U.S. Census Bureau, Current Population Survey (2002; http://www.census.gov/cps/), and data for elected officials were obtained from National Conference of State Legislatures (2003; http://www.ncsl.org/).
The domain of employment and job status similarly comprised ratio measures of Blacks to Whites at the state-level who were in the civilian labor force, who were employed, who were in executive or managerial positions, and who were in professional specialties (For executive and managerial occupations and professional specialty occupations, see U.S. Department of Labor, Bureau of Labor Statistics, Standard Occupation Classification System). These data (year 2000) were obtained from the U.S. Department of Labor & Statistics (2002; http://www.bls.gov/).
Educational attainment was reflected in relative proportions of Whites versus Blacks in the state who had attained high-level education achievement, specifically a bachelor's level degree or higher. These statistics were derived from the U.S. Census Bureau, Decennial Census (2000a; http://www.census.gov/acs/www/).
Finally, judicial treatment encompassed ratio measures of incarceration (jails and prisons), disenfranchisement, and death sentencing. Measures of incarceration and death sentencing at the state level were derived from the U.S. Department of Justice, Bureau of Justice Statistics (incarceration: 2005, Mauer & King, 2007; death row: 2002, U.S. Department of Justice, 2003; http://bjs.ojp.usdoj.gov/). Statistics regarding state-level disenfranchisement were obtained from data compiled by Uggen and Manza (2002), using year 2000 data from the U.S. Department of Justice, Bureau of Justice Statistics.
Each state-level measure of structural racism was dichotomized using a median cut-point. While other potential cut-points in the continuous measures of structural discrimination were explored, the change in risk after the 50th percentile was relatively consistent among those above the 50th percentile as well as those below the 50th percentile. Therefore, for consistency and ease of interpretation, all measures were dichotomized at the 50th percentile to indicate high versus low exposure to structural discrimination. We also conducted sensitivity analyses using other cut-points (e.g., quartiles); although this reduced variation and statistical power, the direction and magnitude of the results were similar.
Self-reported myocardial infarction
Respondents were asked whether they had experienced a heart attack or myocardial infarction within the past 12 months. If respondents indicated that they had experienced such an event, they were then asked whether the event was confirmed by a doctor or other health professional. In the study sample, 1.2% (N = 395) of respondents reported a past-year heart attack or myocardial infarction, and 94.0% of those reported that the diagnosis was confirmed by a physician or health professional (N = 372). Self– report measures for heart attack and angina are highly correlated with actual events (Bergmann et al., 1998; Bush et al., 1989; Lampe et al., 1999). However, to increase validity of reporting, we used physician or professional-confirmed reports of past-year myocardial infarction as our outcome. The prevalence of myocardial infarction among Blacks (1.3%) was somewhat higher than that among Whites (1.1%) in the sample; however, this difference was not statistically significant (χ2 (1, 31,895) = 0.008, p = 0.93).
Covariates
In order to separate the effects of structural racism from individual-level factors that may influence the prevalence of myocardial infarction, analyses were adjusted for respondent age, sex, education, household income, and medical insurance. Age and education were measured in years, and the measure of medical insurance included four types: Medicare, Medicaid, private, and military insurance. To further specify the effects of structural racism and to distinguish the construct from that of poverty alone, we also controlled for state-level racial disparities in poverty measured as relative proportions of Blacks to Whites who were below the poverty-level in each state in 1999. Data for this variable were derived from the U.S. Census Bureau (Census 2000b; http://www.census.gov/).
Statistical analysis
State-level measures of structural racism were linked to individual-level data from the NESARC through the use of federal information processing standards codes (FIPS codes). Respondents were assigned a value for all state-level measures based on state of residence at the time of the survey.
Higher levels of racial disparity for each measure, indicating higher levels of structural racism, were used to predict the outcome of self-reported past 12-month myocardial infarction. State-level measures of structural racism were closely matched in their time frame to the years 2001–2002 during which the outcome measure was obtained. Logistic regression analyses were used to evaluate the relationship between indicators of structural racism and self-reported myocardial infarction. Separate models were used for each measure of structural racism.
We chose to use Generalized Estimating Equations (GEE) for these analyses rather than the commonly used multi-level models for two main reasons. First, our research question is explicitly regarding the population average of state-level effects predicting individual-level health outcomes rather than between-state variance (Hubbard et al., 2010). Thus, the GEE model better corresponds to our research question. Second, clustering by state is inappropriate in national surveys with complex sampling design without making problematic assumptions, as individuals are not sampled to be representative of the state (Little, 1991, 2004; Rao, 2003).
Analyses were weighted to the general population based on demographic distributions from the 2000 U.S. Census and adjusted for the NESARC's complex sampling design using the Taylor Series Linearization approach employed by SAS statistical software. Models were also adjusted for individual-level age, sex, education, household income, medical insurance and state-level disparities in poverty.
The analysis proceeded in three steps. First, we examined the relationship between structural racism and myocardial infarction among non–Hispanic Blacks. Second, we examined the relationship between structural racism and myocardial infarction among non–Hispanic Whites. Finally, we tested the interaction between race and structural racism in predicting myocardial infarction using a multiplicative interaction term in the logistic regression model.
Results
Distribution of measures of structural racism
The means of the distributions for the ratio measures representing political participation, employment and job status, and educational attainment were all below 1.0, indicating that Blacks were under-represented in these domains relative to Whites (Table 2). In voter registration, for example, the percentage of Blacks who were registered to vote by state was 0.85 times lower on average than the percentage of registered Whites.
Table 2.
Distribution of measures of structural racism.
| Measure of structural racism | Mean ratiosa (SE) | Range |
|---|---|---|
| Political participation | ||
| Registered to vote | 0.86 (0.10) | 0.42–1.03 |
| Voted | 0.85 (0.12) | 0.44–1.09 |
| State elected officials | 0.13 (0.08) | 0.00–0.35 |
| Employment and job status | ||
| Civilian labor | 0.99 (0.07) | 0.80–1.21 |
| Employed | 0.95 (0.07) | 0.75–1.14 |
| Executive or managerial position | 0.66 (0.19) | 0.004–1.47 |
| Professional specialty | 0.76 (0.22) | 0.003–1.66 |
| Educational attainment | ||
| Bachelor's degree or higher | 0.57 (0.10) | 0.23–1.32 |
| Judicial treatment | ||
| Incarcerated | 6.68 (2.53) | 1.90–19.00 |
| Disenfranchised | 7.33 (5.65) | 1.94–68.82 |
| Death row | 6.01 (6.17) | 0.00–33.35 |
Ratios refer to relative proportions of Blacks to Whites within each state. The mean ratio scores across all states are represented here.
For measures of judicial treatment, however, mean ratios were above 1.0, indicating that Blacks were over-represented in this domain. For example, in the case of incarceration, the proportion of Blacks jailed or imprisoned by state was 6.68 times higher on average than that of Whites. The over-representation of Blacks in jail or prison ranged from a 1.9-fold increase in Hawaii to a 19.0-fold increase in the District of Columbia.
Relationship between structural racism and myocardial infarction among Blacks
Consistent with study hypotheses, high levels of structural racism in the domains of political participation, employment, and judicial treatment were generally associated with greater odds of myocardial infarction among Blacks (Table 3). In models adjusting for individual-level risk factors and state-level racial disparities in poverty, these associations were statistically significant for representation in state legislature (OR = 1.35; 95% confidence interval, CI: 1.09, 1.69), participation in the civilian labor force (OR = 1.22; 95% CI: 1.04, 1.44), employment (OR = 1.74; 95% CI: 1.48, 2.04), incarceration (OR = 1.32, 95% CI: 1.12, 1.56), and disenfranchisement (OR = 1.28, 95% CI: 1.08, 1.52). These results indicate that Blacks living in states with higher levels of structural racism were more likely to report past-year myocardial infarction than Blacks living in low-structural racism states.
Table 3.
Structural racism is associated with increased risk of myocardial infarction among Blacks, and lower risk among Whites: National epidemiologic survey on alcohol and related conditions (2001–2002).
| Measure of structural racism | Myocardial infarctiona | Interactions between race & racism | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Black | White | |||||
|
|
|
|
||||
| Or (95% CI) | P-Value | Or (95% CI) | P-Value | Wald Chi square | P-Value | |
| Political participation | ||||||
| Registered to vote | 1.08 (0.92, 1.27) | 0.37 | 1.01 (0.87, 1.18) | 0.90 | 0.68 | 0.41 |
| Voted | 0.97 (0.81, 1.15) | 0.70 | 0.85 (0.74, 0.98) | 0.02 | 3.42 | 0.06 |
| State elected officials | 1.35 (1.09, 1.69) | 0.007 | 0.80 (0.70, 0.91) | 0.001 | 20.15 | <0.0001 |
| Employment and job status | ||||||
| Civilian labor | 1.22 (1.04, 1.44) | 0.01 | 0.94 (0.82, 1.07) | 0.34 | 2.19 | 0.14 |
| Employed | 1.74 (1.48, 2.04) | <0.0001 | 0.90 (0.78, 1.04) | 0.14 | 25.95 | <0.0001 |
| Executive or managerial position | 0.76 (0.65, 0.89) | 0.0005 | 1.07 (0.94, 1.21) | 0.31 | 9.06 | 0.002 |
| Professional specialty | 0.55 (0.46, 0.65) | <0.0001 | 1.03 (0.89, 1.19) | 0.72 | 39.75 | <0.0001 |
| Educational attainment | ||||||
| Bachelor's degree or higher | 1.12 (0.91, 1.38) | 0.29 | 1.10 (0.97, 1.24) | 0.14 | 0.16 | 0.69 |
| Judicial treatment | ||||||
| Incarcerated | 1.32 (1.12, 1.56) | 0.001 | 0.84 (0.74, 0.96) | 0.009 | 15.31 | <0.0001 |
| Disenfranchised | 1.28 (1.08, 1.52) | 0.005 | 1.04 (0.90, 1.20) | 0.58 | 1.77 | 0.18 |
| Death row | 1.14 (0.95, 1.37) | 0.17 | 0.86 (0.74, 1.00) | 0.05 | 1.44 | 0.23 |
Adjusted for individual-level age, sex, education, income, medical insurance, and state-level racial disparities in poverty.
In contrast to study hypotheses, high levels of structural racism in measures of job status (i.e., executive or managerial position: OR = 0.76; 95% CI: 0.65, 0.89; and professional specialty: OR = 0.55; 95% CI: 0.46, 0.65) were associated with significantly lower odds of myocardial infarction among Blacks.
Relationship between structural racism and myocardial infarction among Whites
Contrary to the observed pattern among Blacks, high levels of structural racism across domains of political participation, employment, and judicial treatment were generally associated with inverse or null effects on myocardial infarction among Whites (Table 3). For example, Whites living in states with high racial disparities in voting practices (OR = 0.85; 95% CI: 0.74, 0.98), state elected officials (OR = 0.80; 95% CI: 0.70, 0.91), incarceration (OR = 0.84; 95% CI: 0.74, 0.96), and death sentencing (OR = 0.86; 95% CI: 0.74, 1.00) were significantly less likely to report myocardial infarction in the past year than those living is low disparity states. These results indicate that Whites living in states with higher levels of structural racism against Blacks report better cardiovascular health (i.e., lower prevalence of myocardial infarction) than Whites living in low-structural racism states.
Interactions between structural racism and race
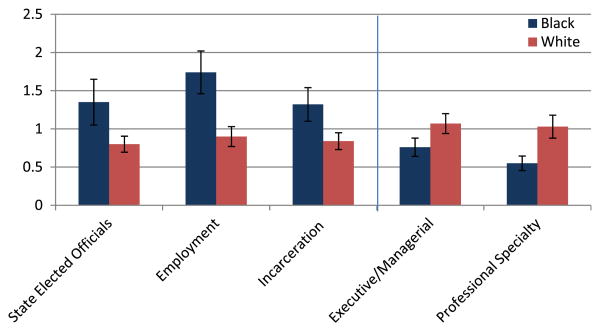
The association between structural racism and myocardial infarction differed between Blacks and Whites across most indicators (Table 3 and Fig. 1). Interactions between structural racism and race were statistically significant for measures of state elected officials (β = −0.14, s.e. = 0.03, p < 0.0001), employment (β = −0.14, s.e. = 0.03, p < 0.0001), incarceration (β = −0.10, s.e. = 0.03, p = <0.0001), representation in executive or managerial positions (β = 0.08, s.e. = 0.03, p = 0.002), and professional specialties (β = 0.18, s.e. = 0.03, p < 0.0001).
Fig. 1.
Interactions between race & racism on myocardial infarction.
Negative interactions for state elected officials, employment, and incarceration indicated that the effect of these measures of structural racism on myocardial infarction among Blacks differed significantly from that of Whites. Specifically, while the associations between structural racism and myocardial infarction were positive among Blacks (resulting in higher prevalence of myocardial infarction), they were negative among Whites (resulting in lower prevalence of myocardial infarction) (Fig. 1). For job status, interactions were reversed and positive; among Blacks, structural racism was associated with lower prevalence of myocardial infarction, and among Whites these effects were null (Fig. 1).
Discussion
This study demonstrates adverse effects of structural racism—specifically state-level racial disparities disadvantaging Blacks in political representation, employment, and incarceration—on past 12-month myocardial infarction. These adverse effects, however, were specific to Blacks, and among Whites, indicators of structural racism appear to have a benign or even beneficial effect on cardiac health. It is important to note that individual-level risk factors including age, sex, education, income, and medical insurance do not account for these findings. Furthermore, lending support to the construct validity of our measures of structural racism, the effects persist above and beyond those of state-level racial disparities in poverty.
Measures of structural racism pertaining to job status did not follow the expected pattern of association, and were inversely associated with myocardial infarction among Blacks. While this finding was unexpected, it is in line with results from previous studies that have documented that Black Americans in high status positions report greater exposure to interpersonal discrimination (Paradies, 2006). This increased exposure, coupled with potential pressures to assimilate and to defy negative racist stereotypes, may in turn place high status Blacks at greater risk for adverse health outcomes. Our results similarly suggest that Black Americans in states with greater representation of Blacks in high status positions are at higher risk for heart attack.
The construct of John Henryism, marked by sustained, high effort coping in the face of psychosocial stressors (James, 1994; James & Thomas, 2000), may help to understand increased cardiovascular risk in these social contexts. James (1994) posits that John Henryism, derived from the African American folktale, reflects the “larger protracted struggle of African American[s]… to free themselves from pervasive and deeply entrenched systems of social and economic oppression” (p. 167). Prolonged efforts towards “upward social mobility” (Bonham, Sellers, & Neighbors, 2004, p. 737) in the face of significant racial barriers may exact a heavy toll on the health of Black Americans (James, 1994; James & Thomas, 2000). Some evidence suggests that John Henryism is a common strategy used by some Blacks to cope with stigma-related stressors (James, 1994), and it is associated with elevations in heart rate and systolic blood pressure, contributing to an increased risk of hypertension—possibly myocardial infarction (James, 1994; James & Thomas, 2000).
The varying health impact of structural racism by race is consistent with several theories, including Krieger's ecosocial model (2012), Feagin's articulation of systemic racism (Feagin, 2000, 2006; Feagin, & Bennefield, 2013), Link & Phelan's (2001) conceptualization of stigma, and Link's theory of “stigma power” (Link, 2014), which all highlight the potential function of stigma and stigma processes in securing or maintaining power differentials. Structural racism may harm the health of groups that are targeted with discrimination, but at the same time benefit those in a position of dominance. Findings from this study highlight the complexities of the power dynamics underlying the social structure of race, and how shifts in the balance of these relationships may have divergent effects on the health of minority and majority group members.
The mechanisms through which structural racism affects health, including cardiac health, are not well understood. Researchers have focused heavily on the stress process as one potential pathway (Williams & Mohammed, 2009; Wyatt et al., 2003). Given evidence implicating stress in the development of cardiovascular disease (for a review, see Dimsdale, 2008), researchers have similarly postulated that exposure to racial discrimination may cause psychological distress, which may in turn compromise the function of the immune, neuroendocrine, and autonomic systems (Williams & Mohammed, 2009; Williams, Neighbors, & Jackson, 2003). The stress caused by discrimination may also precipitate unhealthy coping behaviors such as smoking, drug abuse and poor eating habits (Pascoe & Smart Richman, 2009), consistent with findings from the broader stress literature (Adam & Epel, 2007; Keyes, Barnes, & Bates, 2011; Piazza & Le Moal, 1998). Other pathways through which discrimination may harm health is by limiting access to critical resources and power, such as education, employment, safe housing and living environments, quality healthcare, and political representation (Feagin, 2000; Feagin & Bennefield, 2013; Krieger, 2012; Link & Phelan, 2001). Applying Geronimus' “weathering” hypothesis (1994; 1996), the cumulative effects of sustained socioeconomic disadvantage and concomitant stress may erode the health of Blacks, resulting in poor cardiac outcomes. Research that elucidates the multiple mechanisms through which larger structural forces affect individuals across the lifespan is critical to understanding the complex ways through which racism undermines health.
This study has addressed gaps in the existing literature on discrimination and health by identifying innovative indicators of structural racism and applying them to the study of cardiac outcomes among Blacks and Whites. However, limitations should be noted. First, although we obtained numerous measures of structural racism, these measures do not fully capture the construct of structural racism. Future research should expand on these ecologic indicators to include such measures as wealth, bank lending practices, racial profiling, racist attitudes, access to high quality education, and similar practices and policies that disproportionately disadvantage Blacks vis-a-vis Whites.
Second, structural racism may operate at various levels of organization, both more macro (e.g., at a country level) and more micro (e.g., at the county level). Consequently, our results require replication across different spatial scales to determine the generalizability of the results.
Third, myocardial infarction was based on self-report of the respondent rather than a clinical diagnosis. While good reliability and validity of self-report measures of cardiovascular health have been reported (Bergmann et al., 1998; Bush et al., 1989; Lampe et al., 1999), clinical outcomes would be preferable. Although we controlled for health insurance, there may be racial differences in healthcare access for a diagnosis of myocardial infarction, and clinical outcomes would partially circumvent this potential selection bias. Future studies should include a more comprehensive examination of health outcomes using objective measures to better understand the relationship between structural racism and health.
Fourth, given that mortality from cardiovascular disease is higher among Blacks than Whites (CDC, 2011), the prevalence of myocardial infarction among Blacks relative to Whites may be underestimated in the sample. The bias may result in disproportionate selection out of the sample for Blacks, especially those in states with high levels of racism. Selection out among Blacks exposed to a high degree of structural racism, however, would attenuate the effects of structural racism on cardiovascular health among Blacks observed in this sample, and may account for some of the null or marginally significant findings in this group.
Finally, missing data for some measures of structural racism, namely voter registration, voting, and death sentencing, was just over 10% and may be another factor contributing to the null or weak associations between structural racism and myocardial infarction. However, we note that the states with missing data were also more likely to be high in structural racism. Thus, our results are likely an under-estimate of the relationship between structural racism and myocardial infarction.
Despite these limitations, this study presents compelling evidence of the deleterious effects of structural racism on the cardiac health of Blacks in the United States. These effects likely stem from a history of racial exploitation in this country and its legacy in our current racialized society. Cross-cultural studies comparing the prevalence and patterns of racial health disparities between the United States and countries with similar and divergent histories of racial oppression would be useful in replicating and specifying our findings. As one example of this type of work, Muennig and Murphy (2011) found that racial disparities in health and mortality, as well as the effects of racism on health, varied between the United States and United Kingdom. Examining the extent to which associations between structural racism and health generalize to other racial/ethnic groups within the United States represents another important area for further inquiry.
In many cases, the relationships between structural racism and health are linked to state-level policies and practices that are ultimately amenable to change. For example, the civil rights movement in the 1960s precipitated legislation and policies that reduced Black-White gaps in wages, wealth, and representation in government and professional jobs (Darity & Mason, 1998; Grodsky & Pager, 2001), which in turn contributed to a substantial reduction in Black-White health disparities, such as infant mortality (Almond, Chay, & Greenstone, 2006), in the following decade (Krieger, 2012). This trend towards equality, particularly with regard to indicators of wealth, has since been reversed (Kochhar, Fry, & Taylor, 2011), as have the concomitant improvements in racial health disparities. One of the advantages of focusing on state-level indicators of structural racism in this study is its direct application to the development of policy interventions that may protect against discrimination and promote equal opportunities and access to health-enhancing resources among Blacks in the United States.
Acknowledgments
This research was supported in part by a T32 postdoctoral fellowship (5-T32-MH 13043) and by the National Institute of Drug Abuse (DA 032558).
References
- Adam TC, Epel ES. Stress, eating, and the reward system. Physiological Behavior. 2007;91:449–558. doi: 10.1016/j.physbeh.2007.04.011. [DOI] [PubMed] [Google Scholar]
- Almond D, Chay K, Greenstone M. Mit department of economics working paper No. 07-04. 2006 http://dx.doi.org/10.2139/ssrn.961021. Available at: SSRN http://ssrn.com/abstract=961021.
- Ayotte BJ, Hausmann LRM, Whittle J, Kressin NR. The relationship between perceived discrimination and coronary artery obstruction. American Heart Journal. 2012;163:677–683. doi: 10.1016/j.ahj.2012.01.006. [DOI] [PubMed] [Google Scholar]
- Bergmann MM, Byers T, Freedman DS, Mokdad A. Validity of self-reported diagnoses leading to hospitalization: a comparison of self-reports with hospital records in a prospective study of American adults. American Journal of Epidemiology. 1998;147(10):969–977. doi: 10.1093/oxfordjournals.aje.a009387. [DOI] [PubMed] [Google Scholar]
- Bonham V, Sellers S, Neighbors HW. John Henryism and self-reported physical health among high SES African American men. American Journal of Public Health. 2004;94:737–738. doi: 10.2105/ajph.94.5.737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonilla-Silva E. Rethinking racism: toward a structural interpretation. American Sociological Review. 1997;62(3):465–480. [Google Scholar]
- Bourdieu P. Symbolic power. Critique of Anthropology. 1979;4:77–85. [Google Scholar]
- Bush TL, Miller SR, Golden AL, Hale WE. Self-report and medical record report agreement of selected medical conditions in the elderly. American Journal of Public Health. 1989;79(11):1554–1556. doi: 10.2105/ajph.79.11.1554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carmichael S, Hamilton CV. Black power: The politics of liberation in America. New York: Vintage; 1967. [Google Scholar]
- Centers for Disease Control and Prevention. CDC health disparities and Inequalities report-United States, 2011. Morbidity and Mortality Weekly Report. 2011;60(Supplement) http://www.cdc.gov/mmwr/pdf/other/su6001.pdf. [Google Scholar]
- Clark R, Anderson NB, Clark VR, Williams DR. Racism as a stressor for African Americans. A biopsychosocial model. The American Psychologist. 1999;54(10):805–816. doi: 10.1037//0003-066x.54.10.805. [DOI] [PubMed] [Google Scholar]
- Darity WA, Mason PL. Evidence on discrimination in employment: codes of color, codes of gender. The Journal of Economic Perspectives. 1998;12(2):63–90. [Google Scholar]
- Davis SK, Liu Y, Quarells RC, Din-Dzietharn R. Stress-related racial discrimination and hypertension likelihood in a population-based sample of African Americans: the Metro Atlanta Heart Disease Study. Ethnicity & Disease. 2005;15(4):585–593. [PubMed] [Google Scholar]
- Diez-Roux AV, Nieto FJ, Muntaner C, Tyroler HA, Comstock GW, Shahar E, et al. Neighborhood environments and coronary heart disease: a multilevel analysis. American Journal of Epidemiology. 1997;146:48–63. doi: 10.1093/oxfordjournals.aje.a009191. [DOI] [PubMed] [Google Scholar]
- Dimsdale JE. Psychological stress and cardiovascular disease. Journal of the American College of Cardiology. 2008;51(13):1237–1246. doi: 10.1016/j.jacc.2007.12.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dovidio JF, Gaertner SL. Aversive racism. In: Zanna MP, editor. Advances in experimental social psychology. Vol. 36. San Diego, CA: Academic Press; 2004. pp. 1–51. [Google Scholar]
- Drucker E. A plague of prisons: The epidemiology of mass incarceration in America. New York: New Press; 2011. [Google Scholar]
- Feagin JR. Racist America. New York: Routledge; 2000. [Google Scholar]
- Feagin JR. Systemic racism: A theory of oppression. New York: Routledge; 2006. [Google Scholar]
- Feagin JR, Bennefield Systemic racism. Social Science & Medicine. 2013 doi: 10.1016/j.socscimed.2013.09.006. submitted to this special issue. [DOI] [PubMed] [Google Scholar]
- Gaertner SL, Dovidio JF. The aversive form of racism. In: Dovidio JF, Gaertner SL, editors. Prejudice, discrimination, and racism. Orlando, FL: Academic Press; 1986. pp. 61–89. [Google Scholar]
- Geronimus AT. The health of African American women and infants: implications for reproductive strategies and policy analysis. In: Sen G, Snow R, editors. Power and decision: The social control of reproduction. Cambridge, MA: Harvard University Press; 1994. [Google Scholar]
- Geronimus AT. Black/White differences in the relationship of maternal age to birthweight: a population based test of the weathering hypothesis. Social Science & Medicine. 1996;42(4):589–597. doi: 10.1016/0277-9536(95)00159-x. [DOI] [PubMed] [Google Scholar]
- Grant BF, Harford TC, Muthen BO, Yi HY, Hasin DS, Stinson FS. DSM-IV alcohol dependence and abuse: further evidence of validity in the general population. Drug and Alcohol Dependence. 2007;86:154–166. doi: 10.1016/j.drugalcdep.2006.05.019. [DOI] [PubMed] [Google Scholar]
- Grant BF, Moore TC, Kaplan K. Source and accuracy statement: Wave 1 national epidemiologic survey on alcohol and related conditions (NESARC) Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2003. Available at www.niaaa.nih.gov. [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the national epidemiologic survey on alcohol and related conditions. Archives of General Psychiatry. 2004;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- Grodsky E, Pager D. The structure of disadvantage: individual and occupational determinants of the black-white wage gap. American Sociological Review. 2001;66:542–567. [Google Scholar]
- Guyll M, Matthews KA, Bromberger JT. Discrimination and unfair treatment: relationship to cardiovascular reactivity among Black and European American women. Health Psychology. 2001;20(5):315–325. doi: 10.1037//0278-6133.20.5.315. [DOI] [PubMed] [Google Scholar]
- Harburg E, Erfurt JC, Hauenstein LS, Chape C, Schull WJ, Schork MA. Socio-ecological stress, suppressed hostility, skin color, and black-white male blood pressure: Detroit. Psychosomatic Medicine. 1973;35:276–296. doi: 10.1097/00006842-197307000-00003. [DOI] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Keyes KM, Hasin DS. State-level policies and psychiatric morbidity in lesbian, gay, and bisexual populations. American Journal of Public Health. 2009;99(12):2275–2281. doi: 10.2105/AJPH.2008.153510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, McLaughlin KA, Keyes KM, Hasin DS. The impact of institutional discrimination on psychiatric disorders in lesbian, gay, and bisexual populations: a prospective study. American Journal of Public Health. 2010;100(3):452–459. doi: 10.2105/AJPH.2009.168815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hubbard AE, Ahern J, Fleischer NL, et al. To GEE or not to GEE: comparing population average and mixed models for estimating the associations between neighborhood risk factors and health. Epidemiology. 2010;21(4):467–474. doi: 10.1097/EDE.0b013e3181caeb90. [DOI] [PubMed] [Google Scholar]
- James SA. John Henryism and the health of African Americans. Culture, Medicine, and Psychiatry. 1994;18:163–182. doi: 10.1007/BF01379448. [DOI] [PubMed] [Google Scholar]
- James SA, Thomas PE. John Henryism and blood pressure in Black populations: a review of the evidence. African American Research Perspectives. 2000;6(3):1–10. [Google Scholar]
- Jones CP. Levels of racism: a theoretic framework and a gardener's tale. American Journal of Public Health. 2000;90(8):1212–1215. doi: 10.2105/ajph.90.8.1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman JS, Cooper RS, McGee DL. Socioeconomic status and health in blacks and whites: the problem of residual confounding and the resiliency of race. Epidemiology. 1997;8(6):621–628. [PubMed] [Google Scholar]
- Kershaw KN, Diez Roux AV, Burgard SA, Lisabeth LD, Mujahid MS, Schulz AJ. Metropolitan-level racial residential segregation and Black-White disparities in hypertension. American Journal of Epidemiology. 2011;174(5):537–545. doi: 10.1093/aje/kwr116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes KM, Barnes DM, Bates LM. Stress, coping, and depression: testing a new hypothesis in a prospectively studied general population sample of U.S.-born Whites and Blacks. Social Science & Medicine. 2011;72(5):650–659. doi: 10.1016/j.socscimed.2010.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kochhar R, Fry R, Taylor P. Wealth gaps rise to record highs between Whites, Blacks and Hispanics. Pew Research Center's Social& Demographic Trends. 2011 http://pewresearch.org/pubs/2069/housing-bubble-subprime-mortgages-hispanics-blacks-household-wealth-disparity.
- Kramer MR, Hogue CR. Is segregation bad for your health? Epidemiologic Reviews. 2009;31:178–194. doi: 10.1093/epirev/mxp001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger N. Racial and gender discrimination: risk factors for high blood pressure? Social Science & Medicine. 1990;30(12):1273–1281. doi: 10.1016/0277-9536(90)90307-e. [DOI] [PubMed] [Google Scholar]
- Krieger N. Embodying inequality: a review of concepts, measures and methods for studying health consequences of discrimination. International Journal of Health Services. 1999;29:295–352. doi: 10.2190/M11W-VWXE-KQM9-G97Q. [DOI] [PubMed] [Google Scholar]
- Krieger N. Methods for the scientific study of discrimination and health: an ecosocial approach. American Journal of Public Health. 2012;102(5):936–944. doi: 10.2105/AJPH.2011.300544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger N, Chen JT, Koshelva A, Waterman PD. Figure 2: the Jim Crow geography of mortality: US racial/ethnic inequities in all-cause mortality, 1960–2006. American Journal of Public Health. 2012;102(5):936–944. [Google Scholar]
- Krieger N, Rowley DL, Herman AA, Avery B, Phillips MT. Racism, sexism, and social class: implications for studies of health, disease, and well-being. American Journal of Preventive Medicine. 1993;9(6 Suppl):82–122. [PubMed] [Google Scholar]
- Krieger N, Sidney S. Racial discrimination and blood pressure: the CARDIA Study of young black and white adults. American Journal of Public Health. 1996;86(10):1370–1378. doi: 10.2105/ajph.86.10.1370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lampe FC, Walker M, Lennon LT, Whincup PH, Ebrahim S. Validity of a self-reported history of doctor-diagnosed angina. Journal of Clinical Epidemiology. 1999;52(1):73–81. doi: 10.1016/s0895-4356(98)00146-2. [DOI] [PubMed] [Google Scholar]
- Lauderdale DS. Birth outcomes for Arabic-named women in California before and after September 11. Demography. 2006;43(1):185–201. doi: 10.1353/dem.2006.0008. [DOI] [PubMed] [Google Scholar]
- Lepore SL, Revenson RA, Weinberger SL, Weston P, Frisina PG, Robertson R, et al. Effects of social stressors on cardiovascular reactivity in Black and White women. Annals of Behavioral Medicine. 2006;31(2):120–127. doi: 10.1207/s15324796abm3102_3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis TT, Aiello AE, Leurgans S, Kelly J, Barnes LL. Self-reported experiences of everyday discrimination are associated with elevated C-reactive protein levels in older African-American adults. Brain Behavior & Immunity. 2010;24:438–443. doi: 10.1016/j.bbi.2009.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis TT, Everson-Rose SA, Powell LH, Matthews KA, Brown C, Karavolos K, et al. Chronic exposure to everyday discrimination and coronary artery calcification in African-American women: the SWAN Heart Study. Psychosomatic Medicine. 2006;68(3):362–368. doi: 10.1097/01.psy.0000221360.94700.16. [DOI] [PubMed] [Google Scholar]
- Lewis TT, Kravitz HM, Janssen I, Powell LH. Self-reported experiences of discrimination and visceral fat in middle-aged African-American and Caucasian women. American Journal of Epidemiology. 2011;173(11):1223–1231. doi: 10.1093/aje/kwq466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Link B. Stigma power. Social Science & Medicine. 2014;103:24–32. doi: 10.1016/j.socscimed.2013.07.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Link B, Phelan J. Social conditions as fundamental causes of disease. Journal of Health and Social Behavior, Extra Issue. 1995:80–94. [PubMed] [Google Scholar]
- Link B, Phelan J. Conceptualizing stigma. Annual Review of Sociology. 2001;27:363–385. [Google Scholar]
- Little RR. Inference with survey weights. Journal of Official Statistics. 1991;7:405–424. [Google Scholar]
- Little RR. To model or not to model? Competing modes of inference for finite population sampling. Journal of the American Statistical Association. 2004;99(466):546–555. [Google Scholar]
- Manfredi C, Lacey L, Warnecke R, Buis M. Smoking related behavior, beliefs, and social environment of young black women in subsidized public housing in Chicago. American Journal of Public Health. 1992;82:267–272. doi: 10.2105/ajph.82.2.267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mauer M, King RS. Uneven justice: State rates of incarceration by race and ethnicity. Washington, DC: The Sentencing Project; 2007. [Google Scholar]
- Meyer IH. Prejudice as stress: conceptual and measurement problems. American Journal of Public Health. 2003;93(2):262–265. doi: 10.2105/ajph.93.2.262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer IH, Schwartz S, Frost DM. Social patterning of stress and coping: does disadvantaged social statuses confer more stress and fewer coping resources? Social Science & Medicine. 2008;67(3):368–379. doi: 10.1016/j.socscimed.2008.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muennig P, Murphy M. Does racism affect health? Evidence from the United States and the United Kingdom. Journal of Health Politics, Policy and Law. 2011;36(1):187–214. doi: 10.1215/03616878-1191153. [DOI] [PubMed] [Google Scholar]
- National Conference of State Legislatures. Legislator & legislative staff information. 2003 http://www.ncsl.org/
- Pager D, Shepherd H. The sociology of discrimination: racial discrimination in employment, housing, credit, and consumer markets. Annual Review of Sociology. 2008;34:181–209. doi: 10.1146/annurev.soc.33.040406.131740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paradies Y. A systematic review of empirical research on self-reported racism and health. International Journal of Epidemiology. 2006;35(4):888–901. doi: 10.1093/ije/dyl056. [DOI] [PubMed] [Google Scholar]
- Parson E, McLaughlin M. The persistence of racial bias in voting: voter ID, the new battleground for pretextual race neutrality. The Journal of Law in Society. 2007;8(2):75–104. [Google Scholar]
- Pascoe EA, Smart Richman L. Perceived discrimination and health: a meta-analytic review. Psychological Bulletin. 2009;135:531–554. doi: 10.1037/a0016059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piazza PV, Le Moal ML. The role of stress in drug self-administration. Trends in Pharmacological Sciences. 1998;19:67–74. doi: 10.1016/s0165-6147(97)01115-2. [DOI] [PubMed] [Google Scholar]
- Rao JNK. Small area estimation. Hoboken, N.J.: John Wiley; 2003. [Google Scholar]
- Roberts CB, Vines AI, Kaufman JS, James SA. Cross-sectional association between perceived discrimination and hypertension in African-American men and women: the Pitt County Study. American Journal of Epidemiology. 2007;167(5):624–632. doi: 10.1093/aje/kwm334. [DOI] [PubMed] [Google Scholar]
- Sawyer PJ, Major B, Casad BJ, Townsend SS, Mendes WB. Discrimination and the stress response: psychological and physiological consequences of anticipating prejudice in interethnic interactions. American Journal of Public Health. 2012;102(5):1020–1026. doi: 10.2105/AJPH.2011.300620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnittker J, Massoglia M, Uggen C. Incarceration and the health of the African American community. Du Bois Review. 2011;8:133–141. [Google Scholar]
- Shavers VL, Fagan P, Jones D, Klein WMP, Boyington J, Moten C, et al. The state of research on racial/ethnic discrimination in the receipt of health care. American Journal of Public Health. 2012;102(5):953–966. doi: 10.2105/AJPH.2012.300773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sims M, Diez-Roux AV, Dudley A, Gebreab S, Wyatt SB, Bruce MA, et al. Perceived discrimination and hypertension among African Americans in the Jackson Heart Study. American Journal of Public Health. 2012;102:S258–S265. doi: 10.2105/AJPH.2011.300523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smart Richman L, Bennett G, Pek J, Siegler IC, Williams RB. Discrimination, dispositions, and cardiovascular responses to stress. Health Psychology. 2007;26:675–683. doi: 10.1037/0278-6133.26.6.675. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA) Results from the 2005 national survey on drug use and health: detailed tables, 1.45A. 2005 http://www.samhsa.gov.
- Susser E, Schwartz S, Morabia A, Bromet EJ. Psychiatric epidemiology: Searching for the causes of mental disorders. Oxford: Oxford University Press; 2006. [Google Scholar]
- Thorpe RJ, Jr, Brandon DT, LaVeist TA. Social context as an explanation for race disparities in hypertension: findings from the exploring health disparities in integrated communities (EHDIC) study. Social Science & Medicine. 2008;67(10):1604–1611. doi: 10.1016/j.socscimed.2008.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troxel WM, Matthews KA, Bromberger JT, Sutton-Tyrrell K. Chronic stress burden, discrimination, and subclinical carotid artery disease in African American and Caucasian women. Health Psychology. 2003;22(3):300–309. doi: 10.1037/0278-6133.22.3.300. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. Decennial census data on educational attainment. 2000a http://www.census.gov/
- U.S. Census Bureau. State Legislative District Summary File. 2000b http://www.census.gov/
- U.S. Census Bureau. Current population survey. 2002 http://www.census.gov/cps/
- U.S. Department of Justice. Capital punishment. 2003 http://bjs.ojp.usdoj.gov/
- U.S. Department of Labor & Statistics. Geographical profile of employment and unemployment, 2000. 2002 http://www.bls.gov/
- Uggen C, Manza J. Demographic contraction? Policitcal consequences of felon disenfranchisement in the United States. American Sociological Review. 2002;67:777–803. [Google Scholar]
- Vigins DJ, McCurdy J. Cracks in the system: Twenty years of the unjust federal crack cocaine law. Washington, DC: American Civil Liberties Union; 2006. [Google Scholar]
- Wakefield S, Uggen C. Incarceration and stratification. Annual Review of Sociology. 2010;36:387–406. [Google Scholar]
- Williams DR. Race, socioeconomic status, and health: the added effects of racism and discrimination. Annals of the New York Academy of Sciences. 1999;896:1973–1988. doi: 10.1111/j.1749-6632.1999.tb08114.x. [DOI] [PubMed] [Google Scholar]
- Williams DR, Collins C. US socioeconomic and racial differences in health: patterns and explanations. Annual Review of Sociology. 1995;21:349–386. [Google Scholar]
- Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Reports. 2001;116:404–416. doi: 10.1093/phr/116.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Mohammed SA. Discrimination and racial disparities in health: evidence and needed research. Journal of Behavioral Medicine. 2009;32(1):20–47. doi: 10.1007/s10865-008-9185-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Neighbors HW, Jackson JS. Racial/Ethnic discrimination and health: findings from community studies. American Journal of Public Health. 2003;93(2):200–208. doi: 10.2105/ajph.93.2.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wyatt SB, Williams DR, Calvin R, Henderson FC, Walker ER, Winters K. Racism and cardiovascular disease in African Americans. The American Journal of the Medical Sciences. 2003;325(6):315–331. doi: 10.1097/00000441-200306000-00003. [DOI] [PubMed] [Google Scholar]