Abstract
There is growing acknowledgment that social, structural, and environmental forces produce vulnerability to health harms among people who inject drugs (PWID), and safer environment interventions (SEI) have been identified as critical to mitigating the impacts of these contextual forces on drug-related harm. To date, however, SEIs have been under-theorized in the literature, and how they minimize drug-related risks across intervention types and settings has not been adequately examined. This article presents findings from a systematic review and meta-synthesis of qualitative studies reporting PWID’s experiences with three types of SEIs (syringe exchange programmes, supervised injection facilities and peer-based harm reduction interventions) published between 1997 and 2012. This meta-synthesis seeks to develop a comprehensive understanding of SEIs informed by the experiences of PWID. Twenty-nine papers representing twenty-one unique studies that included an aggregate of more than 800 PWID were included in this meta-synthesis. This meta- synthesis found that SEIs fostered social and physical environments that mitigated drug-related harms and increased access to social and material resources. Specifically, SEIs: (1) provided refuge from street-based drug scenes; (2) enabled safer injecting by reshaping the social and environmental contexts of injection drug use; (3) mediated access to resources and health care services; and, (4) were constrained by drug prohibition and law enforcement activities. These findings indicate that it is critical to situate SEIs in relation to the lived experiences of PWID, and in particular provide broader environmental support to PWID. Given that existing drug laws limit the effectiveness of interventions, drug policy reforms are needed to enable public health, and specifically SEIs, to occupy a more prominent role in the response to injection drug use.
Keywords: syringe exchange programs, supervised injecting facilities, drug use, peer-based interventions, harm reduction, HIV/AIDS, Hepatitis C, qualitative synthesis
INTRODUCTION
It is estimated that more than 13 million people worldwide inject drugs (Mathers et al., 2008). Injection drug use is associated with an array of health harms, including the spread of HIV/AIDS (Mathers et al., 2008) and Hepatitis C (HCV) (Aceijas & Rhodes, 2007). It is estimated that approximately 3 million people who inject drugs (PWID) are living with HIV/AIDS (Mathers et al., 2008), while approximately half of the total injection drug-using population is living with HCV (Aceijas & Rhodes, 2007). Around the globe, public health prevention programmes have been mobilized to minimize drug and health harms among PWID. These interventions have primarily encouraged individuals to enact changes in behaviours to bring about risk reduction. Such individually-focused interventions are founded upon models of rational choice decision-making that assume that risk is the product of individual action and promote concepts of personal responsibility (Rhodes, 2002). PWID are encouraged to modify risk behaviours (e.g., syringe sharing) and those not adhering to risk reduction strategies are often deemed irrational or irresponsible (Rhodes, 2002).
Growing acknowledgement of the limitations of individually-focused interventions in stemming the spread of HIV and HCV among PWID has given rise to greater recognition of the potential of environmental interventions (Blankenship, Bray, & Merson, 2000; Rhodes et al., 2005). Notably, individually-focused interventions often overlook contextual forces that constrain individual agency and shape the production of drug-related harm (Rhodes et al., 2005; Rhodes, 2009). This shift has been propelled by the growing prominence of social-ecological models linking population health outcomes to environmental factors (Galea, Nandi, & Vlahov, 2004) and political and economic conditions (Krieger, 2001).
Central to social ecological studies in substance use research has been an emphasis on ‘risk environments’—that is, social and physical settings in which factors exogenous to the individual converge to increase vulnerability to drug-related harm (Rhodes, 2002; Rhodes et al., 2005). Rhodes’ (2009) ‘risk environment’ framework conceptualizes harm as the product of the interplay between physical (e.g., drug use settings), social (e.g., group norms), economic (e.g., income inequality), and policy (e.g., drug criminalization) dimensions operating across micro-, meso-, and macro-environmental levels. While this framework is not intended as a complete system of categorization for the enumerable and complex contextual forces shaping harm (Richardson, Wood, & Kerr, 2013), it focuses attention on the social, structural, and environmental forces shaping drug use (Rhodes et al., 2005). This approach has informed studies exploring the social-structural contexts of public injecting (Rhodes et al., 2007; Small, Rhodes, Wood, & Kerr, 2007) and drug overdose (Moore, 2004).
Concepts of ‘structural’ and ‘everyday’ violence have proven instructive in further situating the harms produced within ‘risk environments’ in relation to larger debates on social suffering (Bourgois, Prince & Moss, 2004). Structural violence refers to how social arrangements embedded in the organization of society inflict injury upon vulnerable populations, in this case PWID (Farmer, 2005). These social arrangements are determined by large-scale forces (e.g., drug criminalization), rooted in historical and economic processes (e.g., colonialism, globalization), and foster disproportionate suffering among drug-using populations (Farmer, 2005). Everyday violence refers to the normalization of violence in a given context that is rendered invisible due to its pervasiveness (e.g., normalized violence within street-based drug scenes; Bourgois et al., 2004). These concepts give further focus to the social violence produced by contextual forces operating within drug use ‘risk environments’, and underscore the need for social-ecological interventions that alter the social, structural, and environmental contexts of drug use (Rhodes, 2009).
Importantly, even in the event of ‘structural interventions’ (e.g., drug decriminalization) aimed at fostering social and structural conditions favorable to PWID (Blankenship et al., 2000; Duff, 2010; Moore & Dietze, 2005), there would remain a need for targeted public health interventions designed to mitigate the impacts of intersecting social and structural inequities (e.g., poverty, gender inequities) on drug and health harms among PWID. In this regards, the ‘risk environment’ framework identifies ‘safer environment interventions’ (SEIs) as an effective means of reducing drug and health harms among drug-using populations (Rhodes et al., 2005; Rhodes et al., 2006). However, SEIs have received only limited attention in the literature and have been poorly defined and under-theorized, in that a comprehensive understanding of the functions of these interventions has not been developed based on a systematic canvassing of the literature.
For our purposes, we conceive of SEIs as a continuum of programmatic responses that directly intervene to mitigate social, structural, and environmental determinants of risk among PWID. Of primary importance is how SEIs produce social, structural or physical settings that enable risk reduction or otherwise produce positive health outcomes among injection drug-using populations. Rhodes and colleagues (2006) have identified three broad types of SEIs that seek to address unsafe injecting: a) supervised drug consumption sites; b) interventions within existing spatial relations (e.g., peer outreach interventions); and, c) spatial programming and urban design (e.g., lighting, sharps containers distribution). In addition to these, syringe exchange and distribution programs (SEP) are critical in addressing structural and environmental factors (e.g., access to sterile injection equipment) that increase the capacity of PWID to enact risk reduction. Collectively, these diverse types of SEIs range from those designed to increase access to harm reduction materials (e.g., SEPs) to interventions intended reconfigure social networks (e.g., peer support interventions) to those that intervene to create safer drug use settings (e.g., safer injecting facilities, spatial programming).
We undertook this meta-synthesis to develop a comprehensive understanding of SEIs informed by the experiences and perceptions of PWID. We were concerned with exploring the contextual forces that shape these interventions, and how these interventions are directly experienced and perceived by PWID. We focus on three types of interventions best represented in the existing literature: supervised injection facilities (SIF), SEPs, and peer-based harm reduction interventions. Central to this meta-synthesis is the recognition that any analysis that juxtaposes ‘risk’ and SEIs in a straightforward manner obscures the possibility that these interventions themselves may produce risk (Duff, 2010) and it is necessary to also acknowledge the limitations of present approaches.
METHODS
We undertook a systematic search of the qualitative research literature on experiences with SEIs among PWID. We were particularly concerned with how social, structural, and environmental factors influence access to and engagement with these interventions. We used a meta-synthesis approach to integrate and synthesize articles, focusing on the congruence and convergence of themes across interventions and settings. Meta-synthesis is an emerging approach to reviewing qualitative literature that aims to advance beyond narrative reviews through the systematic comparison and synthesis of themes across studies (Jensen & Allen, 1996). It aims to yield a higher level of abstraction, and thus more powerful findings, than any one study can produce on its own (Jensen & Allen, 1996).
Search Strategy
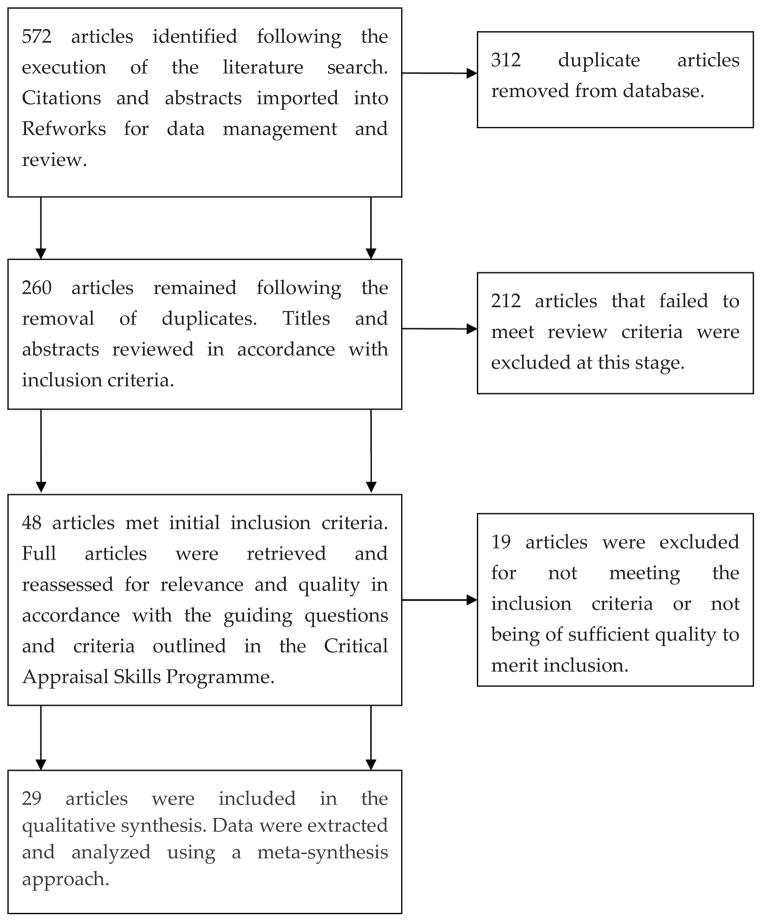
We aimed to identify articles that explored the experiences of PWID with SEIs, with an emphasis on the social, structural, and spatial dimensions that shaped these experiences. Given that qualitative research is poorly indexed in comparison to quantitative research, we executed a comprehensive search strategy to identify relevant papers (see Figure 1 in supplementary online materials). We searched relevant academic databases (PubMed/Medline, EMbase, Sage Publications, Sociological Abstracts, Social Work Abstracts, Psychinfo, Social Sciences Citations Index, Anthropological Index, and Google Scholar) using keywords reflecting the research area and methodology (see Table 1 in supplementary online materials). We hand-searched selected substance use journals with a history of publishing qualitative research, including the International Journal of Drug Policy, Drug & Alcohol Review, Substance Use & Misuse, and Harm Reduction Journal. We used the advanced functions of Google Scholar to identify articles similar to or cited by those identified through the keyword search. We also reviewed reference lists of key articles to identify additional sources. Citations and abstracts of 572 articles were imported into Refworks, a reference management system, to assist with data management, screening, and analysis. 260 articles remained after we removed duplicates.
We applied inclusion and exclusion criteria to the citations and abstracts to identify those eligible for the meta-synthesis. The inclusion criteria were: qualitative methods; English-language; publication in peer-reviewed journal; data collected among PWID; and, focus on SEIs. The exclusion criteria were: quantitative research; opinion articles, commentaries, and editorials; literature reviews; non-English language articles; and, articles published prior to 1997. Articles published before 1997 were excluded in recognition that social-ecological approaches to addressing injection drug use did not gain traction until after this time. 48 articles met the initial inclusion criteria and were retrieved for further review. These articles were reassessed for relevance, quality, and methodological rigour using the Critical Appraisal Skills Programme (CASP) (Collaboration for qualitative methodologies, 1998), a diagnostic tool for evaluating qualitative research. In keeping with the approach outlined by Dixon-Woods and colleagues (2006), we exercised critical judgement during quality assessment, and prioritized the relevance of these articles and their potential contribution to thematic development over minor methodological shortcomings. Ultimately, we excluded an additional 19 articles at this stage, which were determined to lack relevance to our synthesis objectives or had major methodological flaws. (e.g., analyses of nursing records).
Description of articles
We included 29 papers representing 21 unique studies and that included an aggregate number of more than 800 PWID. These articles were published from Canada (n=16), USA (n=6), Russia (4), and other settings (n=4). Twenty-six articles focus on experiences with SEIs, including SEPs, SIFs, and peer-based harm reduction interventions. The remaining three articles report experiences with SEIs as a secondary outcome, but were deemed to contain sufficient information to warrant inclusion in this meta-synthesis. Most studies were undertaken in urban or semi-urban settings with established drug scenes. Most articles (n=22) reported on sanctioned safer environment interventions operated by or in connection with the local health care system, while most of the remaining articles did not describe the broader operational context of these interventions. One article reported on both ‘unsanctioned’ (activist-run) and ‘sanctioned’ (community health agency-run) SEPs operating within one urban area in the United States (Bluthenthal et al., 1997). Three articles reported on peer-based interventions operated by community health agencies or the public health system, while another article reported on a peer-based intervention operated by a drug user-led organization. Four articles reported on syringe exchange programs that placed strict limits (e.g., one-to-one exchange) on the amount of syringes received, while the remaining articles on these interventions either did not describe the operating procedures (n=7) or placed no limits on the numbers of syringes distributed (n=4). All studies were undertaken in settings in which injection drug use is prohibited and regulated primarily through drug law enforcement. Table 2 in the supplementary online materials provides an overview of the key characteristics of these articles.
Analytic Strategy
We reviewed the articles by following the meta-synthesis approach outlined by Noblit and Hare (1988). We first reviewed the articles multiple times to identify and record key themes, as well as details about the study context. The resulting data table was used to identify key ideas and concepts across the studies (i.e., first-order constructs) and determine the ways in which they were related. We then systematically compared and contrasted study findings to identify points of convergence and divergence, translate the themes from studies into one another, and develop thematic categories (i.e., second-order constructs). We then used these ‘second-order’ constructs to develop an overarching interpretation of the functions of SEIs that was rooted in the experiences and perceptions of PWID. Given the overrepresentation of articles by a single research team in Vancouver (Canada), and their potential to bias our findings in regards to the particularities of that setting, we adjusted our analytical procedures to ensure representativeness among our themes. Specifically, we worked to ensure that any themes included in the final interpretation were informed by careful attention to reciprocal and refutational relationships occurring across multiple studies and jurisdictions. Furthermore, we sought to ensure that the themes corresponded to the overall line of argument regarding the functions of SEIs that emerged from our analysis.
RESULTS
Four primary themes emerged from our analysis: First, SEIs were a refuge from the drug scene. Second, interventions were perceived to enable safer injecting practices by reshaping the physical or social context of injection drug use. Third, SEIs were situated within a larger geography of survival and mediated access to a range of social and material resources. Finally, social-structural factors (e.g., drug law enforcement) constrained access to interventions. The distribution of themes across the 29 papers is detailed in Table 3 in the supplementary online materials. Supporting data excerpts are also included in the supplementary online materials (Table 4).
Physical and social environments to escape everyday and structural violence
Providing refuge from street-based drug scenes
Studies included in this synthesis identified structural and everyday violence as defining characteristics of street-based drug scenes, and in particular drug law enforcement (Cooper et al., 2005; Kerr et al., 2007; Kimber & Dolan, 2007; Sarang et al., 2008; Sarang et al., 2010) and gender-based violence (Fairbairn et al., 2008; Fairbairn et al., 2010; Small et al., 2012a). In this context, participants conceptualized SEIs as refuges from structural and everyday violence. Variously referred to as “refuges” (Fairbairn et al., 2008; Small et al., 2012a), “safe havens” (MacNeil & Pauly, 2011), and “safe spaces” (McLean, 2012; Parker et al., 2012), participants positioned these interventions as safe, regulated spaces that mitigated the dangers of the street-based drug scene.
Multiple studies articulated how participants accessed SEIs to minimize the risk of violence. McLean (2012) observed that participants treated a New York-based SEP as a drop-in shelter that they used to shield themselves from policing, as well as potential dangers on the street. Likewise, Fairbairn et al. (2008) explored how a SIF provided “a refuge from the structural and interpersonal violence of the street that also serves to facilitate the safe preparation and injection of drugs” (p. 819). Mobile and peer-based interventions were less able to reshape physical environments but intervened within social and spatial relations to disrupt inequities that typically shape these drug use environments, such as the exploitation of people who require assistance injecting (Sherman et al., 2008; Sherman et al., 2009; Small et al., 2012b). For example, Small et al (2012b) found that a peer injection support programme, which provided safer injecting education and in some cases manual assistance injecting in public settings, “was seen to offer some relief from exploitive relations with ‘hit doctors’” (p. 496).
Contextualizing understandings of ‘safety’
Across multiple studies, participants articulated how they ”felt safe” when accessing these interventions, with understandings of ”safety” reflecting a range of meanings. Several studies highlighted how these interventions increased physical safety by providing environmental supports that negated the risk of physical violence, including police beatings and assault (Fairbairn et al., 2008; McLean, 2012; Small et al., 2012a; Small et al., 2012b). In regard to a SIF, Small et al (2012a) suggested that this facility was perceived to be an injection setting representing “an alternative to the potentially unpredictable character of public injection settings, where conflict and violence can quickly emerge” (p. 316). Other studies highlighted how interventions increased safety from real or perceived stigma (Krusi et al., 2009; MacNeil & Pauly, 2011; McLean, 2012; Parker et al., 2012). For example, MacNeil and Pauly (2011) noted that SEP clients described the intervention as a place free of stigma, discrimination and judgement. Taken together, these findings underscore how SEIs have the profound effect of increasing safety by disrupting violence and stigma.
Enabling safer drug use practices
Reshaping the social and environmental contexts of injecting
Studies emphasized how SEIs changed physical and social environments to mediate safer drug use practices. Most studies reported that SEIs enabled harm reduction by reshaping physical and social environments, which were perceived as critical to fostering social and spatial conditions that reduced drug and health harms (e.g., HIV and HCV transmission, overdose). Changes to physical and social environments varied in accordance with the type of intervention, but were widely identified as conducive to harm reduction practices. Participants frequently articulated how interventions enhanced access to safer injecting equipment, thereby increasing their capacity to practice harm reduction in various injection settings (MacNeil & Pauly, 2011; Ngo et al., 2009; Parker et al., 2012; Power et al., 2005; Sherman et al., 2008; Sherman et al., 2009; Small et al., 2012a). Although limited in their ability to affect the physical injection setting, SEPs altered the risk environment by increasing access to material resources and safer injecting education. In comparison, PWID expressed that SIFs and selected peer-based interventions actively produced social and physical settings that enable safer practices (Fairbairn et al., 2008; Fast et al., 2008; Kerr et al., 2007; Sherman et al., 2008; Small et al., 2012a; Small et al., 2012b). For example, one participant described injecting at a SIF as “the way to do it properly…because it’s not the alley” (Small et al., 2012a, p. 315).
Situating understandings of safer injecting
Experiences with safer injection were articulated across multiple studies and emphasized how these practices were shaped by social and environmental supports. Participants commonly reported that SEIs established situations and spaces that enabled reductions in risk behaviours, such as “rushed injections” (Kerr et al., 2007; Small et al., 2012a) and syringe sharing (Fast et al., 2008; Ngo et al., 2009; Parker et al., 2012; Power et al., 2005; Spittal et al., 2004). Accordingly, these interventions were felt to increase control over the injection process (e.g., access to injecting equipment, space to inject) and minimized the impact of social, structural, and spatial barriers to safer injecting (Fairbairn et al., 2008; Kerr et al., 2007; Krusi et al., 2009; McLean, 2012; Ngo et al., 2009; Parker et al., 2012). In the context of overdose prevention, Kerr et al (2007) observed that a SIF addressed “many contextual factors and social processes that shape injecting practices and mediate overdose risk” (p. 43). Furthermore, understandings of safer injection extended to the environmental features of these interventions, with participants commonly describing interventions as hygienic and clean. Participants contrasted these ”clean” and ”hygienic” environments with alternate, and especially public, injection settings and felt that they reduced an array of risks (e.g., bacterial infection) (Kerr et al., 2007; Small et al., 2012a).
Locating interventions within the geography of survival
Mediating access to support and care
SEIs featured prominently within the geographies of survival of drug-using populations—that is, the spaces and spatial relations that shaped how participants survived within street-based drug scenes (McLean, 2012; Mitchell & Heymen, 2009). Participants in every study were highly marginalized, and in particular disproportionately affected by poverty and homelessness, and challenges to meeting everyday survival needs were common. Participants expressed that SEIs mediated access to ancillary services (e.g., food and shelter) and fostered access to broader health and social supports (MacNeil & Pauly, 2011; Parker et al., 2012; Porter et al., 2002; Power et al., 2005; Sherman et al., 2008; Small et al., 2009; Small et al., 2008). Participants articulated how access to support through these interventions was highly influenced by geographical considerations. In particular, structural and spatial barriers to health and social services were minimized by SEIs that were situated within the everyday spatial practices of participants. Accordingly, participant accounts emphasized that geographical location and low-threshold service delivery models made these interventions ”convenient” and ”easy to access” (MacNeil & Pauly, 2011; McLean, 2012; Parker et al., 2012; Small et al., 2009). Conversely, among the minority of studies reporting on SEPs located outside of street-based drug scenes (Sarang et al., 2008; Sarang et al., 2010), geographic distance was identified as a significant barrier to accessing these services and undermined participants’ ability to enact risk reduction.
Fostering trust to improve access to medical care
Across the majority of studies, trust was identified as a critical factor in mediating access to medical care and support. In the broadest sense, trust between participants and programme staff was seen as important to fostering access to SEIs and ancillary services. Trust was perceived to be an outcome of the non-judgmental, supportive approaches taken by these interventions (Krusi et al., 2009; MacNeil & Pauly, 2011; Porter et al., 2002; Small et al., 2009; Small et al., 2008). SEIs were frequently staffed by health professionals and integrated, to varying degrees, into the health and social care system. Participants commonly reported that these interventions were their primary source of medical care, contrasting these supportive environments with punitive, stigmatizing hospital settings (Krusi et al., 2009; MacNeil & Pauly, 2011; Porter et al., 2002; Small et al., 2009; Small et al., 2008). Several studies reported that, in spite of negative experiences in hospital settings, participants were more likely to accept referrals to these settings by staff at SEIs, insofar as staff’s “lack of judgment of drug use was key to facilitating the development of trust and linkages to other services” (MacNeil & Pauly, 2011, p. 30). However, although these relationships promoted access to care, they could potentially undermine engagement with care, in that some participants were concerned that their continued drug use and drug-related harms might “disappoint” staff (Krusi et al., 2009).
Factors constraining the effectiveness of safer environment interventions
The impact of drug law enforcement
While SEIs altered the risk environment to minimize drug and health harms, studies indicated that access to these interventions was constrained by drug law enforcement, and in particular the threat of detainment for the possession of drugs or harm reduction paraphernalia (Andrade et al., 2001; Bluthenthal et al., 1997; Cooper et al., 2005; Finlinson et al., 2000; Ngo et al., 2009; Rhodes et al., 2003; Sarang et al., 2008; Sarang et al., 2010; Sherman et al., 2008). Studies included in this synthesis were undertaken in settings where the possession of illicit drugs is prohibited and the majority of studies reported law enforcement, and specifically street-level policing, to be the primary response to regulating injection drug use. Studies across multiple settings reported that arbitrary arrests and detainment and police harassment, beatings, and crackdowns were common within local drug scenes (Andrade et al., 2001; Bluthenthal et al., 1997; Cooper et al., 2005; Rhodes et al., 2003; Sarang et al., 2008; Sarang et al., 2010). As a consequence, several studies described how street-level policing fuelled “a pervasive sense of risk and fear of arrest, or detainment, among injection drug users, which in turn is linked to their reluctance to carry needles and syringes” (Sarang et al., 2010. p. 816). Accordingly, participants in multiple studies articulated how street-level policing constrained their capacity to practice harm reduction and thus produced drug and health harms (Andrade et al., 2001; Bluthenthal et al., 1997; Cooper et al., 2005; Rhodes et al., 2003; Sarang et al., 2008; Sarang et al., 2010).
Barriers due to operating procedures and regulations
Several studies explored how the operating procedures and regulations of SEIs restricted access to, and the effectiveness of, these interventions (Bourgois & Bruneau, 2000; Fairbairn et al., 2010; Kerr et al., 2007; Small et al., 2011a; Small et al., 2011b; Small et al., 2012a; Spittal et al., 2004). These restrictions were largely the result of regional or national legal frameworks, which constrained the parameters of harm reduction programmes. Closer attention to these operating procedures and regulations reveals that the resulting programmatic barriers restrict access to SEIs, especially regulations limiting access to new syringes through SEP policies (e.g., one-to-one exchange policies, limits on numbers of syringes distributed) (Bourgois & Bruneau, 2000; Finlinson et al., 1999; Rhodes et al., 2003; Sarang et al., 2008; Sarang et al., 2010; Spittal et al., 2004) and those restricting the range of injection practices permitted at SIFs (e.g., prohibitions on assisted injections) (Fairbairn et al., 2008; Fairbairn et al., 2010; Small et al., 2011a; Small et al., 2011b; Small et al., 2012a; Small et al., 2012b). For example, one study exploring access to syringes in three Russian cities found that policies requiring one-to-one exchange were a disincentive to accessing SEPs because of the considerable risks associated with carrying syringes (e.g., police beatings) and costs to travel to these facilities, which were not located in close proximity to the drug scene (Sarang et al., 2008).
Furthermore, existing legal frameworks and operating regulations inscribed a neoliberal subjectivity on SEIs, in that they promote individual responsibility (e.g., requiring participants to inject themselves or return syringes to receive new ones) and thereby do not account for the contextual factors that constrain individual agency. In this regard, PWID were often unable to access interventions due to these ideological assumptions embedded in these regulatory frameworks and consequently reported engaging in risk behaviours (e.g., syringe-sharing, rushed injections, assisted injections) associated with health harms. For example, studies undertaken in Vancouver, Canada have identified rules prohibiting assisted injections at the local SIF, which are imposed by the federal government, as a programmatic barrier that lead those who require help injecting to seek assisted injections within the local drug scene, which is associated with HIV and HCV transmission (Fairbairn et al., 2010; Small et al., 2011b).
DISCUSSION
In summary, this synthesis highlights how SEIs foster social and physical environments that mediate harm reduction practices, while facilitating access to social and material resources critical to survival. Whereas drug scenes are characterized by structural and everyday violence, SEIs were critical environmental supports that allowed PWID to escape the street, and thereby minimize exposure to violence and street policing. However, SEIs operate within larger societal contexts where drug law enforcement remains the primary response to regulating illicit drug use and are thus subject to policing practices and regulatory frameworks that limit their effectiveness.
Although SEIs are generally characterized as micro-environmental interventions, we found that they mediated meso- and macro-environmental forces that function to produce harm among PWID. Much as risk environments are produced by the interplay between types of environmental factors occurring across levels of environmental influence (Rhodes, 2009), this synthesis demonstrates that SEIs intervene across these environmental dimensions to reshape the social, structural, and environmental contexts of injection drug use. For example, multiple studies illustrated how a SIF in a Canadian setting minimized exposure to meso-environmental risks, such as street-level policing and drug scene violence (Fairbairn et al., 2008; Small et al., 2012b), and established a micro-environmental setting that fostered harm reduction (Fast et al., 2008; Kerr et al., 2007). In this regard, SEIs altered risk environments at the points where these micro-environmental interventions intersected with meso- and macro-environmental factors to disrupt contextual forces that produce harm. Accordingly, whereas empirical studies of risk environments have generally focused on delineating risk within discrete levels of environmental influence (e.g., micro, meso, and macro-level), future research on SEIs may benefit by focusing on the interplay within risk environments to explore how points of convergence between varying types and levels of environmental influence serve to minimize risks.
This synthesis demonstrates that, while the role of SEIs in reducing drug-related harms has been emphasized in the literature, these interventions have a range of additional functions that are critical to their success and were viewed by PWID as of equal importance to risk reduction. Accordingly, conceptualizations of SEIs should be adjusted to acknowledge that these ‘latent functions’ are defining characteristics of these interventions. Furthermore, given that within the situated rationality of injection drug-using populations these other concerns (e.g., maintaining safety, accessing food and shelter) may be elevated above risk reduction (Rhodes, 2009), emphasizing these ‘latent functions’ when designing SEIs may avoid making risk reduction and survival an either/or proposition.
Acknowledging that risk and safety encompass a range of meanings is an important step toward developing interventions situated in relation to the lived experiences of PWID and responsive to meso- and macro-environmental factors that shape these experiences. This synthesis demonstrates that ‘safety from stigma’ is an important function of SEIs that mediates access to these interventions. Several studies illustrated that SEIs fostered social and physical environments that were stigma-free and thereby improved interactions between PWID and care providers (Krusi et al., 2009; MacNeil & Pauly, 2011; McLean, 2012; Parker et al., 2012). These micro-environmental interventions disrupted macro-social stigmatization processes and fostered social inclusion and support that was critical to encouraging engagement with SEIs. Future interventions should further draw upon approaches that have proven successful in minimizing stigma, especially given that PWID are also often stigmatized on the basis of psychiatric or medical co-morbidities. More broadly including PWID in the design and operation of these interventions may only serve to further disrupt stigma and promote greater engagement with SEIs.
An important feature of SEIs is that they mitigate intersecting meso and macro-environmental forces (e.g., policing, poverty) that leave PWID without spaces that they can occupy without the fear of arrest. Drug law enforcement and street-level policing practices erode the spaces that this population can occupy through social regulation and dislocation (Cooper et al., 2005; Small et al., 2006). Globally, PWID experience an array of health harms as a result of these dislocations, notably physical and sexual violence (Cooper et al., 2005; Small et al., 2006) and complications due to unsafe injection practices (Small et al., 2006). SEIs provide a refuge for PWID by serving as places that they can freely occupy and thus escape the structural and everyday violence that characterizes drug scenes. This synthesis suggests that the disruptions in structural and everyday violence produced by providing safe, regulated spaces that PWID could occupy were a defining feature of SEIs. Although SEIs are typically implemented to bring about improvements in health outcomes, these latent benefits are perceived by PWID as part of their primary function. Many SEIs reviewed in this synthesis served as de facto drop-in shelters, highlighting the necessity of providing broader environmental supports alongside harm reduction services in order to maximize their impact. These environmental supports may further prove critical in lessening the stresses that accompany immersion within street-based drug scenes, and additional research is needed to examine their function in promoting access among PWID with complex medical and psychiatric co-morbidities, including blood-borne viral infections.
We found that SEIs mediated access to social and material resources that helped PWID survive within the context of poverty and social marginalization. PWID accessed interventions to meet basic survival needs and receive social support. Of particular importance is the role that SEIs played in mediating access to medical care, which is critical given the high prevalence of infectious diseases (e.g., HIV and HCV) among PWID. Previous epidemiological studies have observed that SEIs are a source of medical care and referrals (Tyndall et al., 2006). Increased attention to the qualitative literature demonstrates how increased access to medical care is a product of the social and spatial contexts of SEIs. Notably, SEIs fostered supportive environments in which PWID were able to receive care or referrals, in large part because they disrupted stigmatization processes and improved trust in programme staff. Because interventions were situated in relation to the everyday spatial practices of injection drug-using populations, they were also convenient and easy to access. Greater attention is needed to these factors during the planning and implementation of SEIs, including incorporating comprehensive health services (e.g., testing and treatment for infectious diseases) into SEIs and siting these facilities in close proximity to key drug scene locales.
Finally, there is an urgent need to embrace SEIs to minimize health harms associated with injection drug use, including the need to address geographical disparities in access to these interventions between and within communities (MacNeil & Pauly, 2010; Tempalski, 2007). Political and community opposition also represent important barriers that prevent the opening of SEIs or precipitate the closing of existing programs. National and international drug law reforms are needed to maximize the availability and effectiveness of these interventions. Globally, law enforcement remains the primary response to regulating injection drug use, with billions of dollars invested annually to enforce supply-side policies seeking to decrease the availability of illicit drugs. In turn, strategies used by law enforcement to regulate PWID, including surveillance and police practices intended to disrupt drug markets and reduce drug-related disorder, are frequently accompanied by police violence and harassment (Maher & Dixon, 1999; Small et al., 2006). Consistent with previous research (Kerr, Small & Wood, 2005), this synthesis has shown that street-level policing constrained access to SEIs and, thereby produced harm. PWID were found to be adversely impacted by arbitrary arrests and police beatings, which made them less likely to access SEIs. Given that the “war on drugs” produces widespread social suffering (Bourgois, 2003; Rhodes et al., 2005), and billions of dollars have been spent supporting policies that have largely proven ineffective, there is a need for global drug policy reforms that shift emphasis away from law enforcement and toward public health (Global Commission on Drug Policy, 2012). These reforms would likely be interpreted as a threat to law enforcement, and thus face considerable resistance, but have the potential to minimize harm and free up funding for demand-side interventions (e.g., drug prevention and treatment) with the potential to decrease drug use.
While not discounting the need for larger legal reforms, police and public health partnerships represent another means to lessen the impact of street-level policing on access to SEIs (Burris et al., 2004; DeBeck et al., 2008). For example, the partnership between police and health agencies in Vancouver, Canada has helped to ensure that policing practices do not restrict access to the local SIF and SEPs (DeBeck et al., 2008). Evidence indicating that these interventions decrease perceived public disorder problems has been critical in establishing police support for these programs (DeBeck et al., 2008). Although policing structures and cultures may hinder the development of these interventions (Kerr et al., 2005), those implementing SEIs may wish to consider developing these partnerships.
There are important limitations to this synthesis. Many articles did not adequately describe their study methodology or theoretical perspective. Several articles were based on the same study, particularly the majority of those on SIFs, and may be limited in the diversity of participant views. Also, most SEIs were implemented in urban areas in a few select countries and may have limited applicability outside of these settings. The extent to which findings are transferable to other interventions and settings warrants further attention. This synthesis also represents only one possible interpretation of these articles and other interpretations, especially those that aim to address different questions, would likely yield different findings. While we employed a systematic search strategy, it is possible that relevant articles were not identified and included in this synthesis.
Importantly, it is worth considering that fully accounting for contextual factors that shape individual studies is beyond scope of qualitative meta-syntheses and the translation of themes across articles necessarily loses many of their individual nuances. Whereas this remains an ongoing limitation of qualitative meta-syntheses, it follows that individual nuances are typically lost when presenting interpretations of any qualitative data (Weed, 2005). As Weed (2005) notes, it is instructive to include as detailed information as is possible regarding the individual cases. To this end, we have included extensive information regarding the individual articles in the supplementary online materials.
Despite these limitations, this synthesis has potential to shape understandings of and approaches to SEIs. A narrow focus on reducing drug-related risks potentially overlooks how these interventions are perceived and utilized by drug-using populations. Future SEIs would benefit from greater consideration of how they can address a range of needs, and constraining forces within broader risk environments, to promote health. Finally, although these interventions are an important step toward reducing harm, the need for broader changes to drug policy persists and the importance of efforts to achieve these reforms cannot be ignored.
Supplementary Material
Figure 1.
Flowchart of meta-synthesis
Table 1.
Search variables
| Intervention | AND | Method |
| Syringe exchange Needle exchange Syringe distribution Needle distribution Peer-baseda Peer interventiona Overdose prevention Overdose response Supervised injection facility Supervised injection room Supervised injection site Supervised drug consumption facility Supervised drug consumption room Safer injection facility Safer injection room Safer injection site Safer drug consumption facility Safer drug consumption room Drug consumption room |
Qualitative Semi-structured interviews In-depth interviews Focus groups Case study Ethnography Ethnographic Participant-observation Naturalistic observation |
Population-specific search terms were added (i.e., injection drug use and drug user) when searching for peer interventions.
Table 2.
Details of retrieved articles (listed chronologically)
| Reference | Country | Aims | Intervention | Sample Characteristics | Data Collection Methods | Key Findings | Key Limitations |
|---|---|---|---|---|---|---|---|
| Bluthenthal et al., 1997 | USA | To examine how law enforcement impacts PWID access to SEPs. | SEP | Unspecified number of PWID accessing SEPs in two cities. | Informal interviews and observation | Police interference with unsanctioned SEP limited access to these services among PWID and discouraged volunteer involvement. PWID cited fear of arrest as a primary reasons for not accessing syringe exchange services. |
Authors do not clearly situate findings in relation to theoretical debates. Authors used mixed methods (including surveys) to determine impact of policing on SEP access, and their overview of the qualitative data was limited. |
| Finlinson et al., 1999 | Puerto Rico | To explore PWID’s access to sterile syringes. | SEP | Unspecified number of PWID accessing 12 SEP sites. Sub-sample of 40 PWID (gender not specified) recruited through SEPs to participate in interviews. | Interviews and observation | Limited operating hours constrained access to syringe exchange services among PWID. Secondary syringe exchange was common among PWID, and viewed as a means to gain access to syringes when harm reduction services not available. |
Authors do not clearly state theoretical perspective. Authors overlook participant perceptions of SEP. |
| Bourgois & Bruneau 2000 | Canada | To explore HIV risks associated with SEP utilization. | SEP | Unspecified number of PWID accessing an SEP. | Observation | Local political conditions led produced restrictive SEP policies (one-to-one exchange) that limited access among PWID, and thus led to the development of informal exchange networks. Specific drug use practices (e.g., binge cocaine use) were critical in shaping access to syringe exchange services, and increased the potential from harm. |
Authors provide only limited information regarding the study methodology, which makes it difficult to assess rigor. |
| Andrade et al., 2001 | Brazil | To describe the opening of an SEP and impact of increased crack cocaine use on SEP utilization. | SEP | 304 PWID accessing four SEPs. Sub-sample of 16 PWID (gender not specified) recruited through the SEPs to participate in in-depth interviews. | In-depth interviews and observation | Limited scope of syringe exchange services constrained access to syringes and led to syringe-sharing among PWID. Syringe-sharing not viewed as potentially harmful among many study participants. Shifts in local drug use patterns after the introduction of crack cocaine led to a substantial decrease in SEP utilization. Street-policing in response to increased crack cocaine use constrained access to SEP among PWID. |
Authors draw on mixed methods (including surveys) and emphasized quantitative findings. Authors do not clearly state theoretical perspective, nor do they situate findings in relation to larger theoretical debates. |
| Porter et al., 2002 | USA | To examine how PWID perceive and use services provided by SEPs. | SEP | 46 PWID (25 male, 21 female), recruitment strategy not specified. | Semi-structured interviews | PWID viewed syringe exchange services as an intervention that mediated access to medical care and referrals. Authors develop a typology for medical care and referrals provided through syringe exchange services (from no access to a primary point of referral). PWID indicated that they trusted syringe exchange workers. |
Potential for positive bias among study participants. Triangulation of data may be needed to verify referrals. |
| Rhodes et al., 2003 | Russia | To explore factors that shape syringe exchange practices. | SEP | 57 PWID (29 male, 28 female), recruited by outreach workers using purposive sampling. | Semi-structured interviews | Fear of being stopped by police exacerbated concerns about the risks of carrying injecting equipment, which in turn was linked to increased syringe sharing and in particular at the point of sale. Myth circulated that it is bad luck to buy syringes in advance. A minority of study participants reported that they had ever been to the two fixed site NEPs, and emphasized the fear of police as a primary barrier. |
Limited data collection among regular SEP clients. |
| Spittal et al., 2004 | Canada | To explore PWID’s access to sterile syringes. | SEP | Unspecified number of IDUs accessing mobile SEP. | Informal interviews and participant observation | Restrictive SEP policies (one-to-one exchange) undermined access to syringes. SEP workers issued “loaners” on an individual basis based on the perceived ability of PWID to return these syringes. Inconsistencies in issuing “loaners” led to tension with PWID, and constrained their access to syringes. |
Limited data collection among PWID. |
| Cooper et al., 2005 | USA | To explore how police crackdowns impact harm reduction practices. | SEP | 40 PWID (21 male, 19 female), recruited through snowball sampling. | In-depth interviews | Intensified street-policing undermined the ability of injection drug users to practice harm reduction (e.g., rushed injections) and interfered with SEP access. Policing practices (e.g., random physical searches, surveillance) reconfigured how injection drug users perceived of their bodies and public spaces. PWID tried to avoid carrying syringes and obtained them primarily from peers prior to injecting. |
Data collection did not begin until the police crackdown was underway, limiting the capacity document changes in SEP access. |
| Power et al., 2005 | Russia | To describe how PWID experience SEP initiatives. | SEP | 38 PWID (27 male, 11 female), recruitment strategy unspecified. | Semi-structured interviews and participant observation | Police harassment, including forced registration with drug use services, undermined access to SEPs. PWID trusted and valued outreach workers, and interacted with them to meet range of health and social care needs. PWID were reluctant to take referrals to other agencies due to concerns about registration with drug use services. |
Limited data collection among regular SEP clients may negatively bias findings. |
| Kerr et al., 2007a | Canada | To examine the impact of a SIF on overdose risk among PWID. | SIF | 50 PWID (28 male, 21 female, 1 transgender), contacted through SIF and purposively sampled to reflect varying levels of use | Semi-structured interviews | Participants felt that the immediacy of the response to overdoses was important, particularly in contrast to other settings. Participants articulated how taking their time—to ‘taste—at the SIF allowed them to implement common overdose prevention strategies and increase safety. Environmental supports mitigated fears of injecting alone without requiring them to share their drugs. Common narrative was that the facility saved lives that would otherwise be lost to overdose. |
Potential for positive bias among study participants. |
| Kimber & Dolan, 2007 | Australia | To explore shooting gallery attendance before and after the opening of a SIF. | SIF | 17 PWID (13 males, 4 female) attending shooting galleries before and after the opening of a SIF, contacted through a peer recruiter and snowball sampling. | Semi-structured interviews | Shooting gallery attendance declined following the opening of supervised injection facility. | Article focused primarily on shooting gallery attendance. Limited discussion of how the opening of the SIF changed the structural-environmental context of the street-based drug scene. Authors do not state theoretical perspective or situating findings in relation to broader theoretical debates. |
| Sarang et al., 2008b | Russia | To explore PWID’s access to sterile syringes. | SEP | 209 PWID (140 males, 69 females) in three cities, recruited by outreach workers using snowball sampling methods. | Semi-structured interviews | Syringe exchange services rarely utilized due to range of factors, including: geographical barriers; and, fear of police interference. Restrictive syringe exchange policies (one-to-one exchange) limited the perceived benefits of SEP attendance (syringe access outweighed by time needed to access services). |
Limited information provided regarding PWID encountered during ethnographic fieldwork. |
| Sherman et al., 2008 | USA | To examine PWID’s experiences with peer-based overdose response. | Peer intervention | 31 PWID (25 male, 6 female), contacted through SEP and researcher referral. | Semi-structured interviews | PWID weighed the fear of legal consequences (i.e., arrest) against desire to save lives when responding to overdose. Peer volunteers were able to intervene (e.g., administer naloxone, revive individuals) when responding to overdoses in diverse drug use settings. |
Authors did not explore how recipients of naloxone experienced this intervention. Authors do not clearly state theoretical perspective. Potential for positive bias among peer volunteers. |
| Fairbairn et al., 2008a | Canada | To examine female PWID’s experiences at a SIF. | SIF | 25 female PWID, contacted through SIF and purposively sampled to reflect varying levels of SIF usage. | Semi-structured interviews | Women accessed SIF to escape structural and everyday violence within the street-based drug scene. Women were able to gain increased access over the injection process, and thereby minimize drug-related risks and exploitation. Women viewed this intervention as a place where they could receive range of supports, and emphasized that it was judgement-free. |
Potential for positive bias among study participants. Study does not account for perspectives of women who face barriers to accessing facility. |
| Fast et al., 2008a | Canada | To explore the delivery of safer injection education in a SIF. | SIF | 50 PWID (28 male, 21 female, 1 transgender), contacted through SIF and purposively sampled to reflect varying levels of use | Semi-structured interviews | Authors identified that gaps in safer injecting knowledge were linked to unsafe injecting practices among PWID.. Safer injecting education was accessible because it was delivered in a drug use setting (i.e., natural context of drug use). Study participants emphasized the supports provided by nurses, together with the broader environmental supports, created a safer injecting environment. |
Potential for positive bias among study participants. Observation of nurse-delivered safer injecting education would have strengthened study findings. Theoretical perspective not clearly stated. |
| Small et al., 2008a | Canada | To investigate the impact of a SIF on PWID’s access to care for injection-related infections. | SIF | 50 PWID (28 male, 21 female, 1 transgender), contacted through SIF and purposively sampled to reflect varying levels of use | Semi-structured interviews | Onsite nurses increased the accessibility of medical care and referrals, especially among PWID who were not otherwise seeking care for injection-related infections. Receipt of medical care in this setting was viewed as critical in addressing infections before they worsened. Participants emphasized the positive interactions with nurses in this setting. |
Potential for positive bias among study participants. Theoretical perspective not clearly stated. |
| Ngo et al., 2009 | Vietnam | To assess the effectiveness of a peer-based SEP. | Peer intervention; SEP | 23 key informants (e.g., public health personnel, government officials, etc.) and unspecified number of IDUs. | Interviews, focus groups, and participant observation | Peer-run syringe exchange services, together with larger advocacy efforts, led to a change in community attitudes toward PWID. Police crackdowns were an ongoing barrier to peer syringe exchange services, with those arrested referred to mandatory drug treatment. Arrests led to a high turnover of peer volunteers, which interfered with the intervention’s sustainability. |
Qualitative findings lack depth and nuance. Authors do not outline how data sources were triangulated. Theoretical perspective not clearly stated. Potential for positive bias among study participants. |
| Sherman et al., 2009 | USA | To examine PWID’s experiences with peer-based overdose response. | Peer intervention | 25 PWID (16 male, 9 female), contacted through intervention using convenience sampling. | Semi-structured interviews | Overdose prevention rarely discussed among PWID despite high prevalence of overdoses in local context. During the intervention, information regarding overdose prevention (peer-administered naloxone) was disseminated more quickly through peer networks and improved perceived safety of injecting. |
Potential for positive bias among study participants. Study did not look at the impact of the program on overdoses or experiences of program recipients. |
| Krusi et al., 2009 | Canada | To evaluate the impact of a supervised injecting room on HIV-positive PWID’s access to HIV care. | SIF | 22 HIV-positive PWID (15 male, 7 female) accessing a care facility with a supervised injecting room, contacted through research advertisements posted at the facility. | Semi-structured interviews | Participants perceived this supervised injection services as increasing the safety associated with injection drug use (e.g., hygiene, overdose prevention, safety). Broader environmental supports strengthened this program (e.g., safer injecting education). Participants emphasized the positive relationship with nurses, and indicated that these mediated access to wider range of services. |
Potential for positive bias among study participants. Theoretical perspective not clearly stated. |
| Small et al., 2009 a | Canada | To examine how SIF use impacts access to health and social services. | SIF | 50 PWID (28 male, 21 female, 1 transgender), contacted through SIF and purposively sampled to reflect varying levels of use | Semi-structured interviews | Supervised injection facility was viewed as “welcoming” environment where PWID could receive a range of supports, including medical care. Facility location was convenient to access, which reduced time and effort needed to access medical care. Study participants received a range of services and referrals in this facility, and indicated that they may not have otherwise received this care. |
Potential for positive bias among study participants. Theoretical perspective not clearly stated. |
| Sarang et al., 2010b | Russia | To explore impact of policing on drug and HIV risks, including access to sterile syringes. | SEP | 209 PWID (140 males, 69 females) in three cities, recruited by outreach workers using snowball sampling methods. | Semi-structured interviews | Study participants expressed that the fear of arrest, detainment, and police violence constrained their access to syringe exchange services. Authors characterize the oppression of PWID as structural violence. |
Limited data collection among regular SEP clients. |
| Fairbairn et al., 2010 | Canada | To explore the context of assisted injection practices in the presence of a SIF. | SIF | 20 PWID (7 male, 13 female) who required assistance injecting in the previous six months, recruited through cohort study and purposively sampled. | Semi-structured interviews | Participants reported that the rule prohibiting assisted injections at the SIF were a significant barrier to accessing that services. | Potential for positive bias among study participants. Theoretical perspective not clearly stated. |
| MacNeil & Pauly, 2011 | Canada | To describe the meanings of SEPs among PWID. | SEP | 33 PWID (23 male, 10 female), recruited using convenience sampling at four SEP sites | Semi-structured interviews | Participants situated their substance use within the context of social suffering. Syringe exchange services were viewed as a “safe haven”, and a place to receive a range of services and supports. Study participants emphasized how the non-judgemental approach taken by syringe exchange workers created a “stigma-free” space. Syringe exchange services helped to establish trust between PWID and health professionals, which was critical in mediating access to wider range of services. |
Potential for positive bias among study participants. |
| Small et al., 2011aa | Canada | To examine PWID’s perspectives on the design and operation of a SIF. | SIF | 50 PWID (28 male, 21 female, 1 transgender), contacted through SIF and purposively sampled to reflect varying levels of use | Semi-structured interviews | Study participants emphasized how the SIF was a hygienic environment, and contrasted this setting with public injection settings. The overall design of the facility improved the ability to safely prepare drugs. Study participants indicated that the limited capacity of the facility was a barrier to access (during peak periods) and also noted that some operating procedures (prohibition of assisted injections) were a barrier. |
Potential for positive bias among study participants. |
| Small et al., 2011ba | Canada | To examine how operating policies and local drug culture impact access to a SIF. | SIF | 50 PWID (28 male, 21 female, 1 transgendered), contacted through SIF and purposively sampled to reflect varying levels of use | Semi-structured interviews and observation | Operating procedures disproportionately impacts those who share particular drugs (e.g., solid pills that must be diluted and cooked) and those individuals may opt to use elsewhere. Individuals taking longer time to inject impeded turnover, particularly during peak periods. Longer waits were viewed as a significant barrier, with PWID opting to inject elsewhere due to the urgency of their needs (e.g., ‘dopesickness’) Rules prohibiting assisted injections were a significant barrier to services, especially among women. |
Authors may overlook additional barriers due to limited observation outside of SIF. |
| McLean, 2012 | USA | To explore the social geography of SEPs. | SEP | Unspecified number of PWID accessing an SEP. Sub-sample of 11 PWID (gender unspecified) recruited through SEP to participate in semi-structured interviews. | Semi-structured interviews and participant observation | Study participants access syringe exchange services to meet a broad range of health and social care needs (‘geography of survival’), and the parameters of service delivery allowed them to have structured relationships with staff. Syringe exchange site served as an informal marketplace where a wide range of resources could be exchanged. Study participants indicated that the SEP was a “safe space” that they could access within the broader context of poverty, homelessness, and displacement. Safety from police harassment was identified as a particularly salient theme. |
Potential for positive bias due to limited observation in other settings. |
| Parker et al., 2012 | Canada | To explore access to harm reduction services among PWID in rural areas. | SEP | 115 PWID (gender unspecified), recruited through fixed site and mobile SEPs and snowball sampling. | Semi-structured interviews | Study participants in urban areas had increased access to syringes due to availability of SEPs, while outreach services did increase access in rural areas. Syringes were reused or shared by study participants when unable to access services (e.g., outside of operating hours). SEPs were viewed as a unique and supportive space where PWID could receive a range of services and supports, and interact with SEP workers and nurses without experiencing stigma. |
Potential for positive bias among study participants. Theoretical perspective not clearly stated. |
| Small et al., 2012a | Canada | To explore the development, operation, and impact of an assisted injecting intervention. | Peer intervention | 10 peer outreach workers and 9 PWID programme participants (gender unspecified). Unspecified number of programme participants observed. | In-depth interviews and observation | Peer support intervention was critical in mediating access to safer injecting education in natural drug use settings (e.g., alleyways, etc.). Assistance provided by peers was viewed as critical in decreasing reliance upon ‘hit doctors’ in the street-based drug scene, and thus minimizing violence and exploitation. |
Potential for positive bias among study participants. Limited data collection among program recipients. |
| Small et al., 2012ba | Canada | To examine how PWID’s perceptions of risk shape SIF attendance. | SIF | 50 PWID (28 male, 21 female, 1 transgendered), contacted through SIF and purposively sampled to reflect varying levels of use | Semi-structured interviews | SIF was viewed as the “proper” place to inject, and contrasted with other injecting settings. Study participants viewed SIF as critical in minimizing risks associated with injection drug use (e.g., overdose, injection-related infections, etc.) by allowing them to inject “properly”. Participants emphasized the importance of a sanctioned injecting environment, and noted the benefits of police not interfering with intervention. Participants cited safety as a primary motivator of accessing SIF, with safety encompassing a range of meanings. |
Potential for positive bias among study participants. |
SIF: supervised injection facility; SEP: syringe exchange programme; PWID: people who inject drugs.
Based on data collected as part of an evaluation of a supervised injection facility.
Based on data collected as part of a larger study of HIV risk in three Russian cities.
Table 3.
Distribution of themes and sub-themes across included articles.
Table 4.
Selected data excerpts from included articles.
| Physical and social environments to escape everyday and structural violence |
| Providing refuge from the drug scene |
|
“ ‘Cause a lot of stuff that happens on the street, it’s like, they [clients] have street beefs and, y’know, if they run into each other there, and they start arguing with one another there. That gets shut down right away. If it does [start], it gets shut down real quick. So it’s a nice thing… Another safety factor for people there. [Male injection drug user discussing a SIF, Canada] (Small et al., 2012a, p. 316) “At the beginning the police were always around the place and we were very scared to go. But one of the outreach workers told us the police were staying away and it would be safe. They had come to some kind of an arrangement. So I took a chance and went one day and it was okay and there’s been no trouble since. I hope it stays that way.” [Male injection drug user discussing a syringe exchange program, Russia] (Power et al., 2005, p. 74) |
| Understandings the contexts of safety |
|
Yeah, yeah, it’s looked after, and like I said I feel safe in there. Like, I don’t have to worry about someone coming up and like, if I’m high and I’m sitting there, and fuckin’ me around ’cause I’m high. They know they can take advantage of the situation. I know I don’t have to worry about that. I don’t feel rushed. I don’t feel threatened or insecure by any means. [Female injection drug user discussing a supervised injection facility, Canada] (Fairbairn et al. 2008, p. 819) … It’s not like [SEPs] are drug stores or anything. They don’t look down upon you for being here. And they [SEP staff] socialize with you. It’s a comfortable environment anyway. It’s not like when you walk into a drug store and ask for a bag of needles, and they go behind the counter and give you a stare that could kill you. [Male injection drug user discussing a syringe exchange programme, Canada] (Parker et al., 2012, p. 158) |
| Enabling safer drug use practices |
| Reshaping the social and environment contexts of injecting |
| “I think they’re a lot more careful at the Insite than they would be outside of the site. Like I said, you’re in a big hurry [when injecting outside] and you’re wondering, so you do everything really quick so you’re not as careful in the alley as you would [be] at the Insite [i.e., supervised injection facility].” [Female injection drug user discussing a supervised injection facility, Canada] (Kerr et al., 2007, p. 39) “[A friend] was staying with me – her and her fiancé – and ‘I knew that she went out [overdosed]. I pulled up like one CC and just had it there and I said to her fiancé, ‘hold onto ‘this’ … Because I didn’t give him too many instructions or anything, but I just wanted to if she goes out and she’s not coming back… I said ‘just shoot it in her thigh,’ because I had already pulled up the right amount, you know what I mean, and I put the cap back on there, and I just left it there. Because I didn’t want him fumbling for anything, I just wanted him to know that, that needle right there had stuff that would bring his girlfriend back.” [Male injection drug user describing peer-based naloxone distribution program, USA] (Sherman et al., 2009, p. 140) |
| Situating understandings of safer injecting |
|
They offer cleanliness and hygiene, it’s real good. Now I use an alcohol swab more, I didn’t use them before … That’s why a lot of people get abscesses, because of the hygiene. And, plus after 27 years of using, I wasn’t doing it right. [Male injection drug user discussing supervised injection services integrated into an HIV/AIDS care facility, Canada] (Krusi et al., 2009, p. 640) “[The medically-supervised injection centre] doesn’t cost. That’s the main factor… 99% would say they would go there and think—well I would go there because I know it’s clean, it’s safe, it’s medically supervised…nothing can go wrong virtually…Why would someone pick to pay $10 to go to a filthy dirty room [i.e., shooting gallery] that you could get hepatitis A just from touching the benches to go to a safe environment? That would be just silly.” [Injection drug user, gender not specified, Australia] (Kimber & Dolan, 2007, p. 216) |
| Locating interventions within the geography of survival |
| Mediating access to support and care |
|
“Well, number one, it’s something to do when you are…You can get a cup of coffee here [syringe exchange programme]. You can get some food here. Because a lot of money doesn’t go on food. Another reason is because it’s just getting out of the house. I feel, personally, closed in sometimes, and you think more about your withdrawal feeling.” [Female syringe exchange client, Canada] (Parker et al., 2012, p. 158) “There’s a bunch of other things you can go there for, you know, health problems. If you need to talk to someone, they’re there. I mean they’re very friendly and helpful in a lot of ways. I mean, I went there before ‘cause I had a toothache, and they told me where to go … because I didn’t know where else to go. And I was like, well the needle exchange, let me ask one of them. Maybe they know. And, and they told me where to go. And I got the help I needed.” [Male client of syringe exchange, USA] (Porter et al., 2002, p. 1314) |
| Fostering trust to improve access to medical care |
|
“People here are great. My spouse is HIV positive and has hepatitis C so have a lot of questions. Had a lot of questions which I have had answered. They’ve given me multiple times to come back and talk to them.” [Syringe exchange client, Canada] (MacNeil & Pauly, 2010, p. 29) “I think it’s actually a good thing. Because you [the nursing staff] get to know what drug addicts are as individuals. And without making an 8 act play about your life, they just got to get to know you … It builds a relationship.” [Male injection drug user discussing supervised injection services at an HIV/AIDS care facility, Canada] (Krusi et al., 2009, p. 640) |
| Factors constraining the effectiveness of safer environment interventions |
| The impact of drug law enforcement |
| “Fear. Fear. This is the very main reason [for sharing syringes]. And not only fear of being caught, but fear that you will be caught, and you won’t be able to get a fix. So on top of being pressured and robbed [by police], there’s the risk you’ll also end up being sick. And that’s why you’ll use whatever syringe is available right then and there.” [Female injection drug user, Russia] (Sarang et al. 2010, p. 818). “[We] were on a roof [injecting] and [the police] came running up there and they literally beat us down with sticks…We were basically cleaning up and they came up, searched us…took [the syringes], broke them, and commenced beating.” [Male injection drug user, USA] (Cooper et al. 2005, p. 679). |
| Barriers due to operating procedures and regulations |
| “I: What about that rule at [Canadian supervised injection facility] where you can’t get help with an injection? R: That’s the reason why I won’t go there. I think that sucks. That, it’s not good, it’s, they should do something about something like that. ‘Cause what happens if I want to go in there, and need help and nobody will help me? Well what’s this place here for then?” [Male injection drug user describing barrier to supervised injection facility, Canada] (Fairbairn et al., 2010, p. 5) “There is this programme in the AIDS centre, they exchange, but you have to bring one [used syringe], and they give you a new one in exchange, so it’s like ‘one-to-one’, so I think just more money will be spent on the transport, its much simpler just to buy [a syringe in a pharmacy]”. [Male injection drug user discussing syringe exchange policies, Russia] (Sarang et al., 2008, p. S30) |
Highlights.
Synthesizes findings from qualitative articles on safer environment interventions (SEI) for people who inject drugs (PWID).
SEIs enable PWID to enact risk reduction by reshaping the environmental contexts of injection drug use.
SEIs serve as a “refuge” from drug scene violence and facilitate access to resources, including health care services.
Drug law enforcement and restrictive operating policies often undermine PWID’s access to SEIs.
Urgent need for global drug policy reforms to enable SEIs to occupy a primary role in the response to injection drug use.
Acknowledgments
We thank Thomas Kerr, Kate Shannon, and Amy Hanser for comments on an earlier draft of this manuscript. We also thank the staff of the British Columbia Centre for Excellence in HIV/AIDS for their research and administrative support. The study was supported by the National Institutes of Health (R01DA033147). Ryan McNeil and Will Small are supported by the Michael Smith Foundation for Health Research.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Aceijas C, Rhodes T. Global estimates of prevalence of HCV infection among injecting drug users. International Journal of Drug Policy. 2007;18(5):352–358. doi: 10.1016/j.drugpo.2007.04.004. [DOI] [PubMed] [Google Scholar]
- Andrade T, Lurie P, Medina MG, Anderson K, Dourado I. The opening of South America’s first needle exchange program and an epidemic of crack use in Salvador, Bahai-Brazil. AIDS and Behavior. 2001;5(1):51–64. [Google Scholar]
- Bastos FI, Strathdee SA. Evaluating effectiveness of syringe exchange programmes: Current issues and future prospects. Social Science & Medicine. 2000;51(12):1771–1782. doi: 10.1016/s0277-9536(00)00109-x. [DOI] [PubMed] [Google Scholar]
- Blankenship KM, Bray SJ, Merson MH. Structural interventions in public health. AIDS. 2000;14:S2, S11–21. doi: 10.1097/00002030-200006001-00003. [DOI] [PubMed] [Google Scholar]
- Bluthenthal RN, Kral AH, Lorvick J, Watters JK. Impact of law enforcement on syringe exchange programs: A look at Oakland and San Francisco. Medical Anthropology. 1997;18(1):61–83. doi: 10.1080/01459740.1997.9966150. [DOI] [PubMed] [Google Scholar]
- Bourgois P. Crack and the political economy of social suffering. Addiction Research & Theory. 2003;11(1):31–37. [Google Scholar]
- Bourgois P, Bruneau J. Needle exchange, HIV infection, and the politics of science: Confronting Canada’s cocaine injection epidemic with participant observation. - Medical Anthropology. 2000;(4):325. [Google Scholar]
- Bourgois P, Prince B, Moss A. The everyday violence of hepatitis C among young women who inject drugs in San Francisco. Human Organization. 2004;63(3):253–264. doi: 10.17730/humo.63.3.h1phxbhrb7m4mlv0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burris S, Blankenship KM, Donoghoe M, et al. Addressing the “risk environment” for injection drug users: The mysterious case of the missing cop. The Milbank Quarterly. 2004;82(1):125–156. doi: 10.1111/j.0887-378X.2004.00304.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell R, Pound P, Pope C, et al. Evaluating meta-ethnography: A synthesis of qualitative research on lay experiences of diabetes and diabetes care. Social Science & Medicine. 2003;56(4):671–684. doi: 10.1016/s0277-9536(02)00064-3. [DOI] [PubMed] [Google Scholar]
- Collaboration for qualitative methodologies. Critical appraisal skills programme. 1998 Retrieved April 15, 2012, from http://www.phru.nhs.uk.
- Cooper H, Moore L, Gruskin S, Krieger N. The impact of a police drug crackdown on drug injectors’ ability to practice harm reduction: A qualitative study. Social Science & Medicine. 2005;61(3):673–684. doi: 10.1016/j.socscimed.2004.12.030. [DOI] [PubMed] [Google Scholar]
- DeBeck K, Wood E, Zhang R, Tyndall M, Montaner J, Kerr T. Police and public health partnerships: Evidence from the evaluation of Vancouver’s supervised injection facility. Substance Abuse Treatment, Prevention, and Policy. 2008;3:11. doi: 10.1186/1747-597X-3-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dixon-Woods M, Cavers D, Agarwal S, et al. Conducting a critical interpretive synthesis of the literature on access to healthcare by vulnerable groups. BMC Medical Research Methodology. 2006;6:35. doi: 10.1186/1471-2288-6-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duff C. Enabling places and enabling resources: New directions for harm reduction research and practice. Drug and Alcohol Review. 2010;29(3):337–344. doi: 10.1111/j.1465-3362.2010.00187.x. [DOI] [PubMed] [Google Scholar]
- Fairbairn N, Small W, Shannon K, Wood E, Kerr T. Seeking refuge from violence in street-based drug scenes: Women’s experiences in North America’s first supervised injection facility. Social Science & Medicine. 2008;67(5):817–823. doi: 10.1016/j.socscimed.2008.05.012. [DOI] [PubMed] [Google Scholar]
- Fairbairn N, Small W, Van Borek N, Wood E, Kerr T. Social structural factors that shape assisted injecting practices among injection drug users in Vancouver, Canada: A qualitative study. Harm Reduction Journal. 2010;7:20. doi: 10.1186/1477-7517-7-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farmer P. Pathologies of power: Health, human rights, and the new war on the poor. Berkeley: University of California Press; 2005. [Google Scholar]
- Fast D, Small W, Wood E, Kerr T. The perspectives of injection drug users regarding safer injecting education delivered through a supervised injecting facility. Harm Reduction Journal. 2008;5:32. doi: 10.1186/1477-7517-5-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finlinson HA, Oliver-Vélez D, Colón HM, et al. Syringe acquisition and use of syringe exchange programs by Puerto Rican drug injectors in New York and Puerto Rico: Comparisons based on quantitative and qualitative methods. AIDS and Behavior. 2000;4(4):341–351. [Google Scholar]
- Fraser S. ‘It’s your life!’: Injecting drug users, individual responsibility and hepatitis C prevention. Health: An Interdisciplinary Journal for the Social Study of Health, Illness and Medicine. 2004;8(2):199–221. doi: 10.1177/1363459304041070. [DOI] [PubMed] [Google Scholar]
- Galea S, Nandi A, Vlahov D. The social epidemiology of substance use. Epidemiologic Reviews. 2004;26(1):36–52. doi: 10.1093/epirev/mxh007. [DOI] [PubMed] [Google Scholar]
- Global Commission on Drug Policy. Report of the global commission on drug policy 2012 [Google Scholar]
- Finlinson HA, Colon HM, Robles RR, et al. Access to sterile syringes by injection drug users in Puerto Rico. Human Organization. 1999;58(2):201–211. [Google Scholar]
- Jensen LA, Allen MN. Meta-synthesis of qualitative findings. Qualitative Health Research. 1996;6(4):553–560. [Google Scholar]
- Kerr T, Small W, Moore D, Wood E. A micro-environmental intervention to reduce the harms associated with drug-related overdose: Evidence from the evaluation of Vancouver’s safer injection facility. International Journal on Drug Policy. 2007;18(1):37–45. doi: 10.1016/j.drugpo.2006.12.008. [DOI] [PubMed] [Google Scholar]
- Kerr T, Small W, Wood E. The public health and social impacts of drug market enforcement: A review of the evidence. International Journal of Drug Policy. 2005;16(4):210–220. [Google Scholar]
- Kimber J, Dolan K. Shooting gallery operation in the context of establishing a medically supervised injecting center: Sydney, Australia. Journal of Urban Health. 2007;84(2):255–266. doi: 10.1007/s11524-006-9145-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger N. Theories for social epidemiology in the 21st century: An ecosocial perspective. International Journal of Epidemiology. 2001;30(4):668–677. doi: 10.1093/ije/30.4.668. [DOI] [PubMed] [Google Scholar]
- Krusi A, Small W, Wood E, Kerr T. An integrated supervised injecting program within a care facility for HIV-positive individuals: A qualitative evaluation. AIDS Care. 2009;21(5):638–644. doi: 10.1080/09540120802385645. [DOI] [PubMed] [Google Scholar]
- MacNeil J, Pauly B. Impact: A case study examining the closure of a large urban fixed site needle exchange in Canada. Harm Reduction Journal. 2010;7:11. doi: 10.1186/1477-7517-7-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacNeil J, Pauly B. Needle exchange as a safe haven in an unsafe world. Drug and Alcohol Review. 2011;30(1):26–32. doi: 10.1111/j.1465-3362.2010.00188.x. [DOI] [PubMed] [Google Scholar]
- Maher L, Dixon D. Policing and public health: Law enforcement and harm minimization in a street-level drug market. British Journal of Criminology. 1999;39(4):488–512. [Google Scholar]
- Mathers BM, Degenhardt L, Phillips B, et al. Global epidemiology of injecting drug use and HIV among people who inject drugs: A systematic review. The Lancet. 2008;372(9651):1733–1745. doi: 10.1016/S0140-6736(08)61311-2. [DOI] [PubMed] [Google Scholar]
- McLean K. Needle exchange and the geography of survival in the South Bronx. The International Journal on Drug Policy. 2012;23(4):295–302. doi: 10.1016/j.drugpo.2012.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell D, Heynen N. The geography of survival and the right to the city: Speculations on surveillance, legal innovation, and the criminalization of intervention. Urban Geography. 2009;30(6):611–632. [Google Scholar]
- Moore D. Governing street-based injecting drug users: A critique of heroin overdose prevention in Australia. Social Science & Medicine. 2004;59(7):1547–1557. doi: 10.1016/j.socscimed.2004.01.029. [DOI] [PubMed] [Google Scholar]
- Moore D, Dietze P. Enabling environments and the reduction of drug-related harm: Re-framing Australian policy and practice. Drug and Alcohol Review. 2005;24(3):275–284. doi: 10.1080/09595230500170258. [DOI] [PubMed] [Google Scholar]
- Ngo AD, Schmich L, Higgs P, Fischer A. Qualitative evaluation of a peer-based needle syringe programme in Vietnam. International Journal of Drug Policy. 2009;20(2):179–182. doi: 10.1016/j.drugpo.2007.12.009. [DOI] [PubMed] [Google Scholar]
- Parker J, Jackson L, Dykeman M, Gahagan J, Karabanow J. Access to harm reduction services in Atlantic Canada: Implications for non-urban residents who inject drugs. Health & Place. 2012;18(2):152–162. doi: 10.1016/j.healthplace.2011.08.016. [DOI] [PubMed] [Google Scholar]
- Porter J, Metzger D, Scotti R. Bridge to services: Drug injectors’ awareness and utilization of drug user treatment and social service referrals, medical care, and HIV testing provided by needle exchange programs. Substance Use & Misuse. 2002;37(11):1305–1330. doi: 10.1081/ja-120014080. [DOI] [PubMed] [Google Scholar]
- Power R, Nozhkina N, Kanarsky I. Injecting drug users’ experiences of targeted harm reduction in the Russian Federation. Drug and Alcohol Review. 2005;24(1):69–77. doi: 10.1080/09595230500124990. [DOI] [PubMed] [Google Scholar]
- Rhodes T, Mikhailova L, Sarang A, et al. Situational factors influencing drug injecting, risk reduction and syringe exchange in Togliatti city, Russian Federation: A qualitative study of micro risk environment. Social Science & Medicine. 2003;57(1):39–54. doi: 10.1016/s0277-9536(02)00521-x. [DOI] [PubMed] [Google Scholar]
- Rhodes T, Watts L, Davies S, Martin A, Smith J, Clark D, et al. Risk, shame and the public injector: A qualitative study of drug injecting in south wales. Social Science & Medicine. 2007;65(3):572–585. doi: 10.1016/j.socscimed.2007.03.033. [DOI] [PubMed] [Google Scholar]
- Rhodes T. The ‘risk environment’: A framework for understanding and reducing drug-related harm. International Journal of Drug Policy. 2002;13(2):85–94. [Google Scholar]
- Rhodes T. Risk environments and drug harms: A social science for harm reduction approach. International Journal of Drug Policy. 2009;20(3):193–201. doi: 10.1016/j.drugpo.2008.10.003. [DOI] [PubMed] [Google Scholar]
- Rhodes T, Kimber J, Small W, Fitzgerald J, Kerr T, Hickman M, et al. Public injecting and the need for “safer environment interventions” in the reduction of drug-related harm. Addiction. 2006;101(10):1384–1393. doi: 10.1111/j.1360-0443.2006.01556.x. [DOI] [PubMed] [Google Scholar]
- Rhodes T, Singer M, Bourgois P, Friedman SR, Strathdee SA. The social structural production of HIV risk among injecting drug users. Social Science & Medicine. 2005;61(5):1026–1044. doi: 10.1016/j.socscimed.2004.12.024. [DOI] [PubMed] [Google Scholar]
- Richardson L, Wood E, Kerr T. The impact of social, structural and physical environmental factors on transitions into employment among people who inject drugs. Social Science & Medicine. 2013;76(0):126–133. doi: 10.1016/j.socscimed.2012.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarang A, Rhodes T, Platt L. Access to syringes in three Russian cities: Implications for syringe distribution and coverage. The International Journal on Drug Policy. 2008;19(S1):S25–36. doi: 10.1016/j.drugpo.2007.11.008. [DOI] [PubMed] [Google Scholar]
- Sarang A, Rhodes T, Sheon N, Page K. Policing drug users in Russia: Risk, fear, and structural violence. Substance use & Misuse. 2010;45(6):813–864. doi: 10.3109/10826081003590938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherman SG, Gann DS, Scott G, Carlberg S, Bigg D, Heimer R. A qualitative study of overdose responses among Chicago IDUs. Harm Reduction Journal. 2008;5:2. doi: 10.1186/1477-7517-5-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherman SG, Gann DS, Tobin KE, Latkin CA, Welsh C, Bielenson P. “The life they save may be mine”: Diffusion of overdose prevention information from a city sponsored programme. International Journal on Drug Policy. 2009;20(2):137–142. doi: 10.1016/j.drugpo.2008.02.004. [DOI] [PubMed] [Google Scholar]
- Small W, Ainsworth L, Wood E, Kerr T. IDU perspectives on the design and operation of North America’s first medically supervised injection facility. Substance use & Misuse. 2011a;46(5):561–568. doi: 10.3109/10826084.2010.517714. [DOI] [PubMed] [Google Scholar]
- Small W, Van Borek N, Fairbairn N, Wood E, Kerr T. Access to health and social services for IDU: The impact of a medically supervised injection facility. Drug and Alcohol Review. 2009;28(4):341–346. doi: 10.1111/j.1465-3362.2009.00025.x. [DOI] [PubMed] [Google Scholar]
- Small W, Kerr T, Charette J, Schechter MT, Spittal PM. Impacts of intensified police activity on injection drug users: Evidence from an ethnographic investigation. International Journal of Drug Policy. 2006;17(2):85–95. [Google Scholar]
- Small W, Moore D, Shoveller J, Wood E, Kerr T. Perceptions of risk and safety within injection settings: Injection drug users’ reasons for attending a supervised injecting facility in Vancouver, Canada. Health, Risk & Society. 2012a;14(4):307–324. [Google Scholar]
- Small W, Rhodes T, Wood E, Kerr T. Public injection settings in Vancouver: Physical environment, social context and risk. International Journal of Drug Policy. 2007;18(1):27–36. doi: 10.1016/j.drugpo.2006.11.019. [DOI] [PubMed] [Google Scholar]
- Small W, Shoveller J, Moore D, Tyndall M, Wood E, Kerr T. Injection drug users’ access to a supervised injection facility in Vancouver, Canada: The influence of operating policies and local drug culture. Qualitative Health Research. 2011b;21(6):743–756. doi: 10.1177/1049732311400919. [DOI] [PubMed] [Google Scholar]
- Small W, Wood E, Lloyd-Smith E, Tyndall M, Kerr T. Accessing care for injection-related infections through a medically supervised injecting facility: A qualitative study. Drug and Alcohol Dependence. 2008;98(1–2):159–162. doi: 10.1016/j.drugalcdep.2008.05.014. [DOI] [PubMed] [Google Scholar]
- Small W, Wood E, Tobin D, Rikley J, Lapushinsky D, Kerr T. The injection support team: A peer-driven program to address unsafe injecting in a Canadian setting. Substance use & Misuse. 2012b;47(5):491–501. doi: 10.3109/10826084.2012.644107. [DOI] [PubMed] [Google Scholar]
- Spittal PM, Small W, Wood E, Johnston C, Charette J, Laliberté N, et al. How otherwise dedicated AIDS prevention workers come to support state-sponsored shortage of clean syringes in Vancouver, Canada. International Journal of Drug Policy. 2004;15(1):36–45. [Google Scholar]
- Tempalski B. Placing the dynamics of syringe exchange programs in the United States. Health & Place. 2007;13(2):417–431. doi: 10.1016/j.healthplace.2006.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tyndall MW, Kerr T, Zhang R, King E, Montaner JG, Wood E. Attendance, drug use patterns, and referrals made from North America’s first supervised injection facility. Drug and alcohol dependence. 2006;83(3):193–198. doi: 10.1016/j.drugalcdep.2005.11.011. [DOI] [PubMed] [Google Scholar]
- Weed M. “Meta interpretation”: A method for the interpretive synthesis of qualitative research. Forum: Qualitative Social Research. 2005;6(1):37. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.