Abstract
Background
A recent meta-analysis has reported that intensive-dose statin drug increases the risk of incident diabetes. However, doubling of the statin dose generates only a further 6% decrease in low-density lipoprotein cholesterol (LDL-c) on average. This study aimed to determine whether statin therapy with lower intensive-target LDL-c level contributes to higher risk of new-onset diabetes.
Methods
Medline, Embase, and the Cochrane Central Register of Controlled Trials were searched for randomized controlled endpoint trials of statins conducted from 1966 to 2012. We included trials with more than 1000 participants who were followed up for at least 2 years. The included trials were stratified by the target LDL-c level. I 2 statistic was used to measure heterogeneity between trials. We further calculated risk estimates with random-effect meta-analysis. Meta-regression was used to identify the potential risk factors of statin-induced diabetes.
Results
Fourteen trials with a total of 95 102 non-diabetic participants were included. The risks elevated by 33% [odds ratio (OR) = 1.33; 95% confidence interval (CI) 1.14–1.56; I 2 = 7.7%] and 16% (OR = 1.16; 95% CI 1.06–1.28; I 2 = 0.0%) when the intensified target LDL-c levels were ≤1.8 mmol/L and 1.8–2.59 mmol/L, respectively. The risk of incident diabetes did not increase when the target LDL-c level was ≥2.59 mmol/L. Apart from age, female, and baseline level of total cholesterol, meta-regression analysis showed that the target and baseline levels of LDL-c and relative LDL-c reduction were predictors of statin-induced diabetes.
Conclusion
A lower intensified target LDL-c level of statin therapy resulted in a higher risk of incident diabetes.
Introduction
Statin drugs are widely used in the evidence-based lowering of cardiovascular disease (CVD) risk. In a meta-analysis by the Cholesterol Treatment Trialists’ Collaborators of 14 randomized trials of statins involving more than 90 000 participants, statin therapy can safely reduce the 5 year incidence of major vascular events by approximately 20% with per 1.0 mmol/L low-density lipoprotein cholesterol (LDL-c) reduction [1]. Further study concluded that additional lowering of LDL-c to approximately 1 mmol/L to 2 mmol/L with more intensive therapy further reduced the incidence of major vascular events [2]. According to the European Guidelines on CVD prevention in clinical practice (version 2012), the LDL-c goal of <2.6 mmol/L (100 mg/dL) is recommended in high-risk CVD patients. For very high-risk patients, the recommended LDL-c target is <1.8 mmol/L (70 mg/dL) or ≥50% LDL-c reduction when the target LDL-c level cannot be reached [3].
A recent meta-analysis of 13 trials showed that statin therapy is associated with an increased risk of developing type 2 diabetes mellitus (T2DM) [4]. Another meta-analysis combined five trials reported that an excess incidence of new-onset T2DM occurred in patients treated with intensive-dose statin [5]. The intensive-dose statin therapy mentioned above were per day simvastatin 80 mg, atorvastatin 80 mg, pravastatin 80 mg, lovastatin 80 mg, or rosuvastatin 20–40 mg [6]. However, doubling of statin dose generates on average only a further 6% decrease in LDL-c [7]. The guideline requirement for target LDL-c level is difficult to achieve even with high-dose statin drugs. Thus, intensive-dose statin therapy is not the same as intensive-target LDL-c level of statin therapy. Our recent study of eight randomized statin trials investigated the effects of intensive LDL-c lowering with statin drugs (LDL-c level lower than 2.59 mmol/L or relative LDL-c reduction at least 30% of baseline [8]) on new-onset diabetes. The results showed that intensive LDL-c lowering with statin use lead to a 19% increased risk of incident diabetes. Given that an increased trend of incident diabetes appears when LDL-c is lower, we speculate whether the lower target LDL-c achieved contributes to higher risk of incident diabetes. According to the guideline requirement for people at risk of different CVDs [3], a subgroup meta-analysis was conducted in patients whose target LDL-c levels were ≤1.8 mmol/L, within 1.8 mmol/L to 2.59 mmol/L, and ≥2.59 mmol/L. Thus, informed choices were possibly provided by physicians when statin therapy was applied in different kinds of patients. Meanwhile, meta-regression analyses pointed out that statin treatment increases the incidence of new-onset T2DM among old patients, and change in LDL-c concentration is not a risk factor [4]. A study consisted of three large randomized trials of atorvastatin discovered that baseline fasting glucose level, higher triglycerides, higher body mass index (BMI), and hypertension are important predictors of new-onset diabetes [9]. Whether the dose or the target LDL-c level of statin use is associated with diabetes incidence remains unknown.
This study aims to investigate the relationship between target LDL-c level of statin use and new-onset T2DM and identify the potential predictors of statin-induced diabetes. Studies involving 1000 or more patients with a minimum mean follow-up of 2 years and comparison between statin therapy and placebo or standard-care controlled endpoint trials were included.
Materials and Methods
Search strategy and selection criteria
The terms statin, hydroxymethylglutaryl coenzyme A reductase inhibitor and names of individual statins (fluvastatin/mevastatin/compactin/pravastatin/simvastatin/lovastatin/Pitavastatin/rosuvastatin/cerivastatin/atorvastatin) combined with diabetes and diabetes mellitus as title words or keywords were searched in Medline (from 1966 to October 2012), Embase (from 1974 to October 2012), and the Cochrane Central Register of Controlled Trials for large-scale trials. These trials compared statin therapy with placebo group or standard care-controlled group.
The search was in strict accordance with Randomized Controlled Trials performed in humans. Two independent reviewers accessed the reports with the following inclusion criteria: trials performed in 1000 or more individuals with a minimum mean follow-up of 2 years. Trials comparing different kinds of lipid-lowering agents or different doses of the same statin or performed in diabetic participants were excluded. The search commenced on October 2012, and 2841 reports were identified. Any discrepancies were settled by discussion with a third reviewer. The improved Jadad score [10]–[12] was used to evaluate the quality of studies included in the meta-analysis.
Data sources
Of the qualified 23 trials, eight [13]–[20] were available to the authors and six trials [21]–[26] had published data of incident diabetes. For the eight available trials, we referred to another two meta-analyses published in Lancet [4] and JACC [9] for incident diabetes. We inquired the investigators of the other nine trials on the unpublished data for incident diabetes, but no reply was received. A total of 14 trials were included in this study. We also contacted the investigators of some unpublished characteristics of participants (i.e., baseline BMI in LIPID trial [26], mean blood pressure (BP) in LIPID [26] and GISSI PREVENZIONE [20] trials, relative high-density lipoprotein cholesterol (HDL-c) reduction in HPS [22], and GISSI-HF [15] trials). However, we received either rejection or no reply.
The data from the included trials were collected as follows: characteristics of trials (sample size, follow-up), clinical characteristics of the patients (baseline age, gender, current smoker, BMI, BP, HDL-c, LDL-c, triglyceride, and total cholesterol), therapeutic intervention (type and dose of statin), change of serum lipid (endpoint LDL-c level and relative reduction of LDL-c, HDL-c, triglyceride, total cholesterol), other drugs used (aspirin, beta-blocker, and ACE inhibitor), and incident diabetes (including diabetes diagnostic criteria) to identify the risk factors of diabetes (Table 1, Table 2, Table 3, Table 4). A second reviewer checked the extracted data for accuracy.
Table 1. Characters for non-diabetic participants in 14 trials that reported incident diabetes.
| Non-DMpatients | Follow-up year | Diagnosis ofincident diabetes | Intervention | NewDMcase | Numbeassignedstatin | Numberin controlgroup | New DMassignedstatin | New DMin controlgroup | |
| JUPITER | 17802/17802 | 1.9‡ | Physician reported(medication, positive OGTT,raised random glucosewith symptoms, two fastingglucose values ≥7.0 mmol/L) | Rosuvastatin 20 mgvs placebo | 486 | 8901 | 8901 | 270 | 216 |
| SPARCL | 3803/4731 | 4·9 | Two fasting glucose values≥7.0 mmol/L and at leastpost-baseline glucose≥2 mmol/l above baseline | Atorvastatin 80 mgvs placebo | 281 | 1905 | 1898 | 166 | 115 |
| HPS | 14573/20536 | 5.0 | Physician reported; medication | Simvastatin 40 mgvs placebo | 628 | 7291 | 7282 | 335 | 293 |
| ASCOT-LLA | 7773/10305 | 3.3† ‡ | WHO 1999 criteria | Atorvastatin 10 mgvs placebo | 288 | 3910 | 3863 | 154 | 134 |
| CORONA | 3534/5011 | 2.7† ‡ | Physician reported | Rosuvastatin 20 mgvs placebo | 188 | 1771 | 1763 | 100 | 88 |
| PROSPER | 5181/5804 | 3.2 | One fasting glucose value>7.0 mmol/L; medication | Pravastatin 40 mgvs placebo | 292 | 2588 | 2593 | 165 | 127 |
| GISSI-HF | 3378/4574 | 3.9‡ | Two fasting glucose values≥7.0 mmol/L | Rosuvastatin 10 mgvs placebo | 440 | 1660 | 1718 | 225 | 215 |
| 4S | 4243/4444 | 5.4‡ | Physician reported; medication;one fasting glucose value≥7.0 mmol/L | Simvastatin 20–40 mgvs placeb | 391 | 2116 | 2127 | 198 | 193 |
| WOSCOPS | 5974/6595 | 4.8 | Two fasting glucose values≥7.0 mmol/L; medication | Pravastatin 40 mgvs placebo | 168 | 2999 | 2975 | 75 | 93 |
| LIPID§ | 6997/9014 | 6.0 | One fasting glucose value≥7.0 mmol/L; medication | Pravastatin 40 mgvs placebo | 264 | 3496 | 3501 | 126 | 138 |
| AFCAPSTexCAPS | 6211/6605 | 5.2† | Physician reported;medication;one fasting glucosevalue ≥7.0 mmol/L | Lovastatin 20–40 mgvs placebo | 146 | 3094 | 3117 | 72 | 74 |
| ALLHAT-LLT | 6087/10355 | 4.8† | One fasting glucose value≥7.0 mmol/L | Pravastatin 40 mgvs no treatment | 450 | 3017 | 3070 | 238 | 212 |
| MEGA | 6086/7832 | 5.3 | Physician reported; medication;two fasting glucosevalues ≥7.0 mmol/L | Pravastatin 10–20 mgvs no treatment | 33 | 3013 | 3073 | 172 | 164 |
| GISSIPREVENZIONE | 3460/4271 | 2.0‡ | One fasting glucosevalue ≥7.0 mmol/L | Pravastatin 20 mgvs no treatment | 201 | 1743 | 1717 | 96 | 105 |
DM = diabetes mellitus; OGTT = oral glucose tolerance test; WHO = World Health Organization;
Data from total cohort (including diabetes at baseline).
Median.
Includes only patients with normal fasting glycaemia at baseline.
Table 2. Characters for non-diabetic participants in 14 trials that reported incident diabetes.
| MeanAge (yr) | MeanBMI(kg/m2) | Sex(men %) | PriorCHD (%) | PriorStroke (%) | Hypertension(%) | SystolicBP/DiastolicBP (mm Hg) | Smoking(current %) | |
| JUPITER | 66.0‡ | 28.4‡ | 61.8 | 0.0 | Not reported | 0.0 | 134.0/80.0 | 15.8 |
| SPARCL | 62.7 | 27.4 | 59.7 | 0.0 | 69.1 | 61.9 | 138.6/81.7 | 19.2 |
| HPS | 64.7 | 27.2 | 77.6 | 78.3 | Not reported | 41.6 | 143.0/81.0 | 14.7 |
| ASCOT-LLA | 63.1† | 28.6† | 81.1 | 0.0 | 9.7 | 100.0 | 164.2/95.0 | 32.7 |
| CORONA | 73.0† | 27.0† | 76.5 | 100.0 | 12.5 | 63.4 | 129.0/76.0 | 8.6 |
| PROSPER | 75.3 | 26.8 | 48.3 | 44.0 | 11.2 | 61.9 | 154.6/83.8 | 26.8 |
| GISSI-HF | 68.0 | 27.1 | 77.4 | 100.0 | 4.5 | 54.3 | 127.0/77.0 | 14.1 |
| 4S | 58.6 | 26.0 | 81.4 | 100.0 | Not reported | 26.0 | 138.8/83.5 | 25.6 |
| WOSCOPS | 55.2 | 26.0 | 100.0 | 0.0 | Not reported | 15.7 | 135.5/84.0 | 44.0 |
| LIPID§ | 62.0‡ | NA | 83.2 | 100.0 | 4.1 | 41.7 | Not reported | 9.6 |
| AFCAPS TexCAPS | 58.0† | 27.0† | 85.0 | 0.0 | Not reported | 22.0 | 138.0/78.0 | 12.4 |
| ALLHAT-LLT | 66.3 | 29.9 | 51.2 | 14.2 | Not reported | 100.0 | 145.0/84.0 | 23.2 |
| MEGA | 58.3 | 23.8 | 31.6 | 0.0 | 0.0 | 41.8 | 132.2/78.6 | 20.6 |
| GISSIPREVENZIONE | 59.3 | 26·5 | 86.3 | 100.0 | Not reported | 37.0 | Not reported | 11.8 |
BMI = body mass index; CHD = coronary artery heart disease; BP = blood pressure;
Data from total cohort (including diabetes at baseline).
Median.
Includes only patients with normal fasting glycaemia at baseline.
Table 3. Characters for non-diabetic participants in 14 trials that reported incident diabetes.
| BaselineLDL-c(mmol/l) | BaselineHDL-c(mmol/l) | BaselineTotalCholesterol(mmol/l) | BaselineTriglycerides(mmol/l) | Relative (%)LDL-CReduction* | Relative (%)HDL-cReduction* | Relative (%)Total CholesterolReduction* | |
| JUPITER | 2.8 | 1.3 | 4.8 | 3.0 | 50.0 (12 months) | 0.0 | Not reported |
| SPARCL | 3.4 | 1.3 | 5.4 | 3.7 | 42.1 (average in trial) | 2.3 | 28.8 |
| HPS | 3.4 | 1.1 | 5.9 | 2.0 | 29.4 (average in trial) | Not reported | Not reported |
| ASCOT-LLA | 3.4 | 1.3 | 5.5 | 1.7 | 34.8 (12 months) † | −1.5† | 18.2† |
| CORONA | 3.5 | 1.2 | 5.4 | 2.0 | 45.1 (3months)† | 5.0† | Not reported |
| PROSPER | 3.8 | 1.3 | 5.7 | 1.5 | 30.7 (12 months) | 5.0 | Not reported |
| GISSI-HF | 3.2 | Not reported | Not reported | Not reported | 34.9 (12 months) | Not reported | Not reported |
| 4S | 4.9 | 1.2 | 6.7 | 1.5 | 36.7 (12 months) | 7.0 | 26.0 |
| WOSCOPS | 4.9 | 1.1 | 7.0 | 4.2 | 23.7 (12 months) | 5.0 | 20.0 |
| LIPID§ | 3.8 | 0.9 | 5.6 | 3.9 | 25 (during 5 years) | 5.0 | 17.8 |
| AFCAPS TexCAPS | 3.9 | 1.0 | 5.7 | 1.8 | 26.7 (12 months) | 6.0 | 18.0 |
| ALLHAT-LLT | 3.7 | 1.2 | 5.7 | 3.9 | 18.1 (24 months) | 7.1 | 8.4 |
| MEGA | 4.1 | 1.5 | 6.3 | 1.4 | 17.1 (12 months) | 5.0 | 9.0 |
| GISSIPREVENZIONE | 3.9 | 1.2 | 5.9 | 4.3 | 11.5 (12 months) | 0.6 | 7.9 |
LDL-c = low-density lipoprotein cholesterol; HDL-c = high-density lipoprotein cholesterol;
*Difference between the groups in the change from baseline to timepoint in LDL-C.
Data from total cohort (including diabetes at baseline).
Includes only patients with normal fasting glycaemia at baseline.
Table 4. Characters for non-diabetic participants in 14 trials that reported incident diabetes.
| Relative (%)TriglyceridesReduction* | EndpointLDL-C(mmol/l)(statin group) | Aspirin(%) | ACEinhibitor (%) | Beta-blocker(%) | Cardiovascularevents(statin vs placebo) | Total CHDcoronary events(statin vs placebo) | Jadadscore | |
| JUPITER | 16.1 | 1.4 | 16.6 | Not reported | Not reported | 142/251 | Not reported | 6 |
| SPARCL | 10.6 | 1.6 | 87.3 | 28.5 | 17.7 | 864/1094 | 305/475 | 4 |
| HPS | Not reported | 2.4 | Not reported | Not reported | Not reported | Not reported | 619/835 | 4 |
| ASCOT-LLA | 12.6† | 2.2 | 17.0 | Not reported | Not reported | 389/486 | 178/247 | 6 |
| CORONA | 20.5† | 2.0 | Not reported | 80.0 | 75.2 | 1104/1164 | 554/588 | 5 |
| PROSPER | 13.0 | 2.5(3 months) | Not reported | Not reported | Not reported | 454/523 | Not reported | 7 |
| GISSI-HF | Not reported | 2.2 | 45.1 | 77.6 | 62.4 | 1305/1283 | Not reported | 7 |
| 4S | 17.0 | 3.0 | 36.8 | Not reported | 56.8 | 136/207(death) | 353/502 | 4 |
| WOSCOPS | 12.0 | 3.6 | Not reported | Not reported | Not reported | 50/73(death) | 174/248 | 4 |
| LIPID§ | 11.0 | 2.9 | 82.3 | 16.0 | 47.1 | 331/433(death) | 287/373(death) | 4 |
| AFCAPS TexCAPS | 15.0 | 2.9 | 17.1 | 7.6 | 4.5 | 194/255 | 163/215 | 4 |
| ALLHAT-LLT | 3.0 | 2.7 | 30.9 | Not reported | Not reported | 295/300(death) | 380/421 | 2 |
| MEGA | 13.0 | 3.2 | 1.0 | 12.6 | 8.3 | 125/172 | 66/101 | 4 |
| GISSIPREVENZIONE | 4.7 | 3.2 | 78.7 | 41.5 | 42.9 | 101/113(death) | 31/49(death) | 3 |
LDL-c = low-density lipoprotein cholesterol; CHD = coronary artery heart disease;
*Difference between the groups in the change from baseline to timepoint in LDL-C.
Data from total cohort (including diabetes at baseline).
Includes only patients with normal fasting glycaemia at baseline.
Statistical analysis
The 14 trials were stratified according to the target LDL-c level of <1.8 mmol/L, >2.59 mmol/L, and 1.8–2.59 mmol/L. Odds ratio (OR) and 95% confidence interval (CI) were used to compare the mean differences in each subgroup separately. I 2 statistic, which is derived from Cochran’s Q [100×(Q–df/Q)] and provides a measure of the proportion of overall variation attributable to between-trial heterogeneity, was used to quantify statistical heterogeneity between trials [27]. Random-effects models were selected for a more conservative assessment (i.e., wide CIs) of the average effect size. Moreover, an independent analysis restricted to trials of standard LDL-c lowering with statin therapy was carried out (trials did not meet either of the following requirement: (1) target LDL-c level ≤2.59 mmol/L or (2) relative LDL-c reduction of at least 30% of baseline). Meta-regression analyses were used to identify the risk factors of incident diabetes between trials. Stata version 11.0 was used to analyze the data, and P<0.05 was considered statistically significant. Sensitivity analyses were also carried out. A funnel plot and Egger test were used to estimate publication bias [28].
Results
New-onset diabetes stratified with target levels of LDL-c
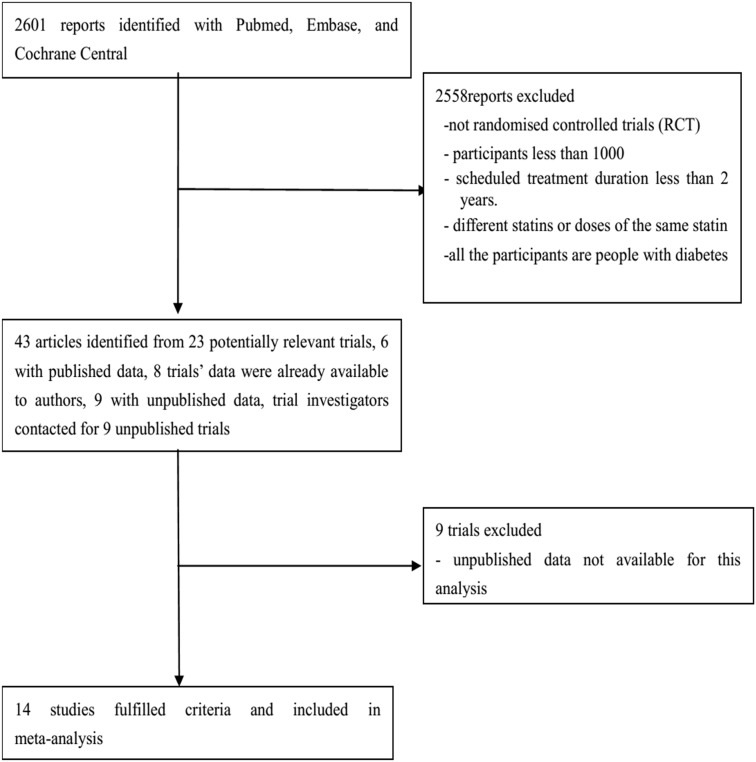
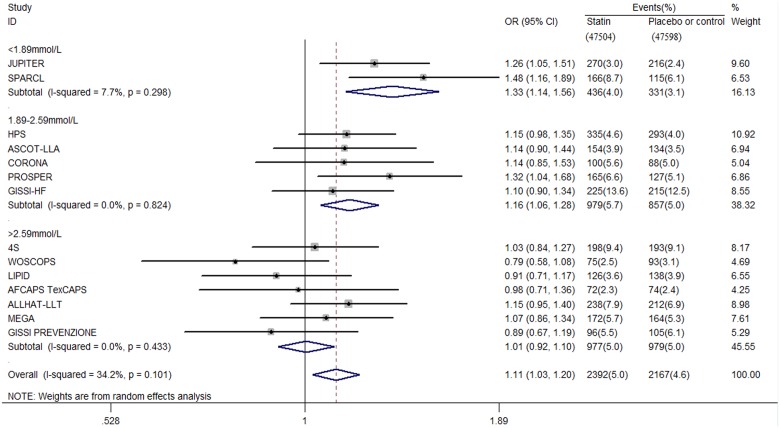
Fourteen eligible trials with a total of 95102 non-diabetic participants were included (Figure 1). The characteristics of the trials are shown in Table 1 to Table 4. Study quality was generally high, 12 (86%) of 14 trials had a Jadad score of ≥4. A noticeable effect of statin therapy on new-onset diabetes was observed when their intensified target LDL-c level was lower than 1.8 mmol/L (OR 1.33, 95% CI 1.14 to 1.56; I 2 = 7.7%) and within 1.8 mmol/L to 2.59 mmol/L (OR 1.16, 95% CI 1.06 to 1.28; I 2 = 0.0%) (Figure 2). However, the risk of incident diabetes did not increase when the target LDL-c level was higher than 2.59 mmol/L (OR 1.01, 95% CI 0.92 to 1.10; I 2 = 0.0%) (Figure 2). In absolute terms, one additional case of diabetes is diagnosed per 103 patients and per 141 patients whose target LDL-c was ≤1.8 mmol/L and within 1.8 mmol/L to 2.59 mmol/L when taking statin therapy for 4 years.
Figure 1. Flow diagram of literature search to identify randomised placebo-controlled and standard care-controlled statin trials.
Figure 2. Association between different target LDL-c level and incident diabetes.
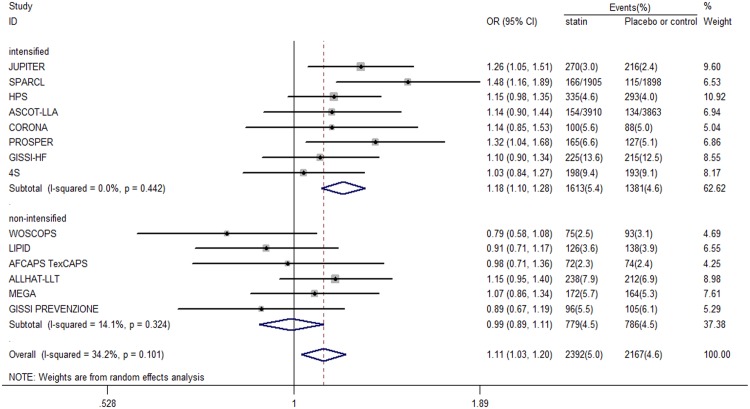
New-onset diabetes in standard LDL-c lowering group
Among the six trials in the standard LDL-c lowering group, no individual trial showed a positive effect of statin therapy on incident diabetes. In the combined data set, no clear association was found between standard LDL-c lowering with statin therapy and incident diabetes compared with placebo or standard care control therapy (OR 0.99, 95% CI 0.89 to 1.11) (Figure 3). The heterogeneity between trials was low (χ2 for heterogeneity = 5.82; P = 0.324; I 2 = 14.1%), which indicates that most variations were attributable to chance alone.
Figure 3. Association between intensified and non-intensified LDL-c level and incident diabetes.
Meta-regression analyses
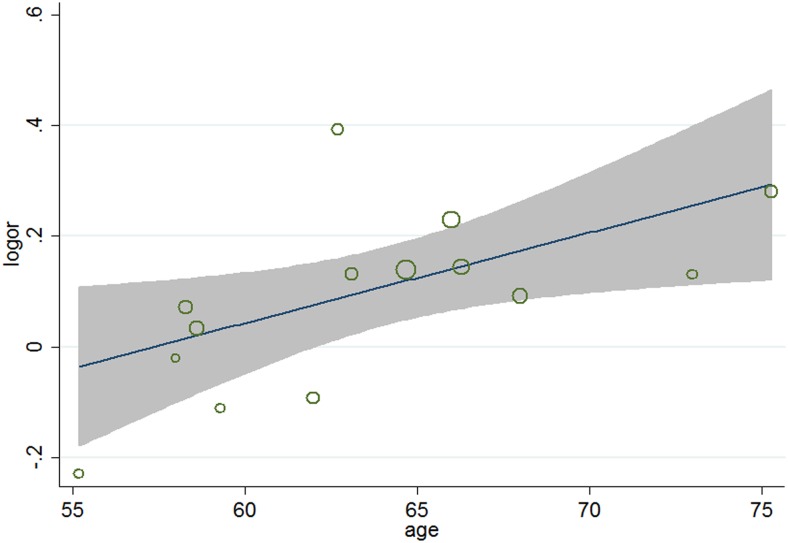
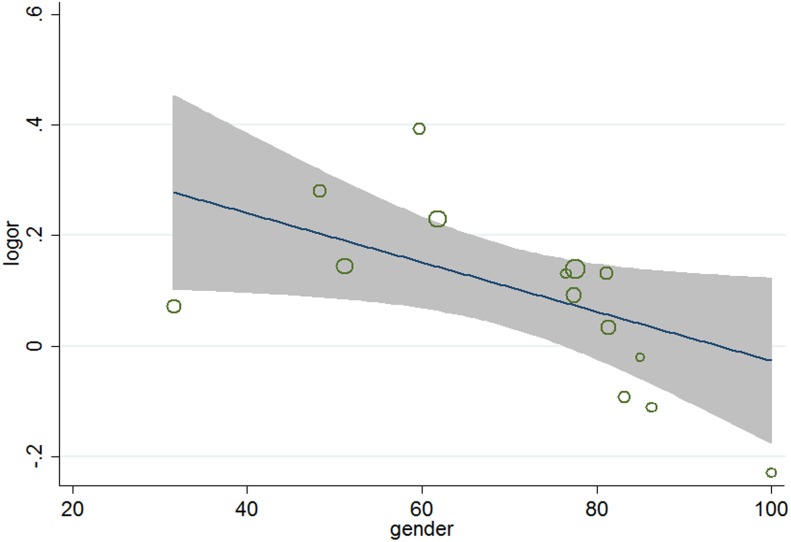
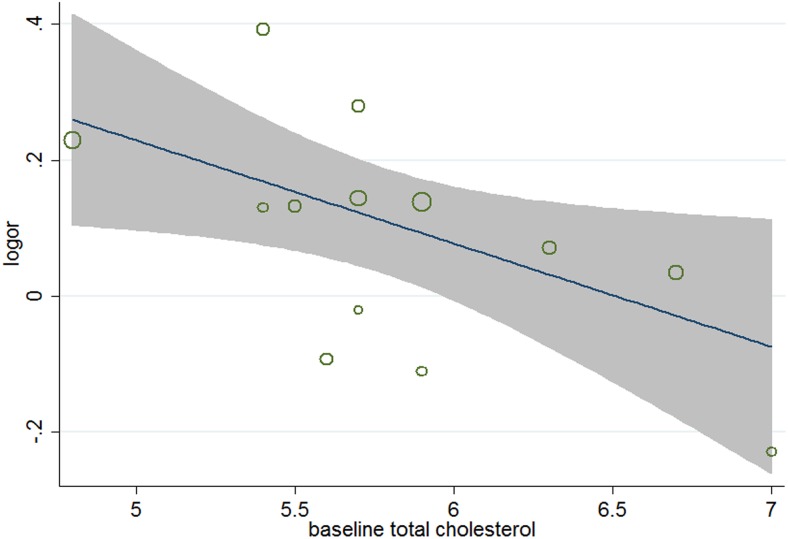
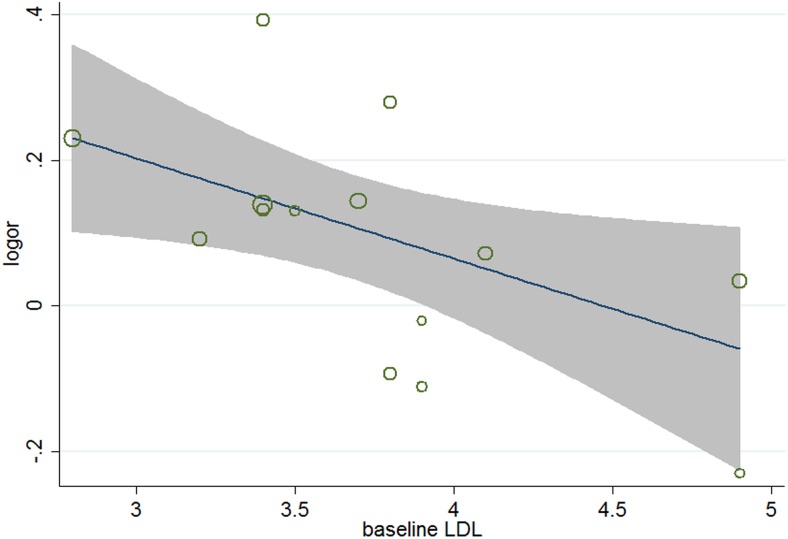
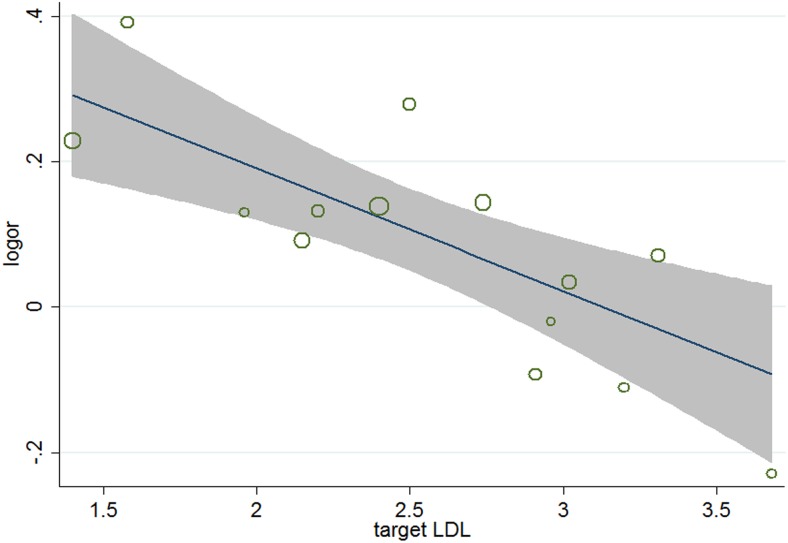
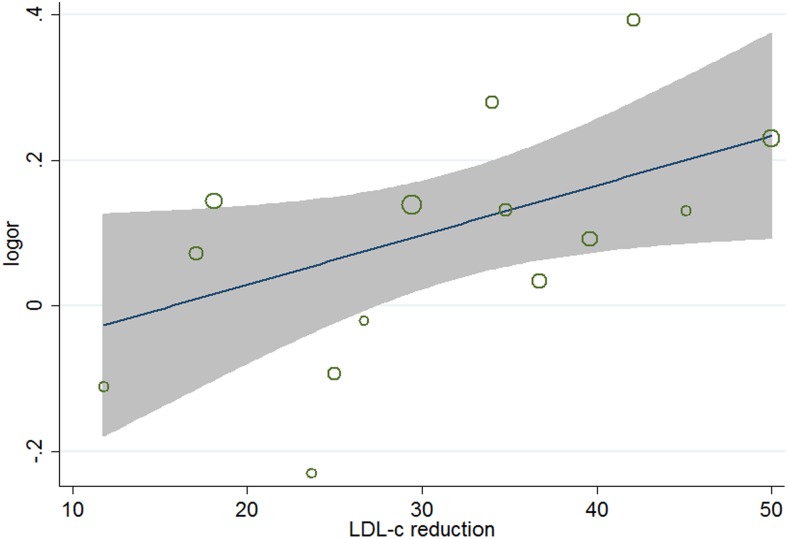
To identify other potential factors of the residual difference between the 14 trials (χ 2 for heterogeneity = 19.77; P = 0.101; I 2 = 34.2%), meta-regression analyses were carried out. The results (Table 5) showed that aside from age (P = 0.026, 95% CI 1.002 to 1.031) (Figure 4), gender (P = 0.038, 95%, CI 0.991 to 0.999) (Figure 5), and baseline total cholesterol (P = 0.034, 95% CI 0.748 to 0.967) (Figure 6), baseline level of LDL-c (P = 0.031, 95% CI, 0.771 to 0.985) (Figure 7), target LDL-c level (P = 0.005, 95% CI, 0.758 to 0.941) (Figure 8), and relative LDL reduction (P = 0.044, 95% CI, 1.021 to 3.907) (Figure 9) were risk factors of new-onset diabetes after statin therapy.
Table 5. Meta-regression of baseline characters for incident diabetes.
| logor | t | P>|t| | [95% Conf. Interval] |
| age | 2.54 | 0.026 | 1.002305 1.030816 |
| sex | −2.34 | 0.038 | .9912401.9996951 |
| target LDL | −3.40 | 0.005 | .7582104.941228 |
| baseline LDL | −2.45 | 0.031 | .771076.9849836 |
| baseline cholesterol | −2.41 | 0.034 | .7478781.9867268 |
| LDL reduction | 2.25 | 0.044 | 1.000208 1.013721 |
| dose | 1.25 | 0.235 | .9979259 1.007709 |
| BMI | 1.29 | 0.224 | .9773928 1.091429 |
| CHD | −1.21 | 0.250 | .9971045 1.000831 |
| stroke | 2.37 | 0.064 | .9995688 1.010495 |
| hypertension | 0.98 | 0.346 | .9983291 1.004423 |
| systolic BP | 0.69 | 0.506 | .9939916 1.011491 |
| diastolic BP | 0.05 | 0.962 | .9809797 1.020278 |
| smoking | −0.34 | 0.742 | .987824 1.009013 |
| baseline HDL | 1.87 | 0.088 | .9145669 3.037582 |
| baseline triglycerides | −0.85 | 0.414 | .8823282 1.057124 |
| Aspirin | −0.23 | 0.823 | .9957346 1.003503 |
| Aceinhibitor | 0.38 | 0.718 | .9945277 1.007432 |
| Beta-block | −0.46 | 0.663 | .9929148 1.004881 |
| HDL Increase | −0.75 | 0.470 | .9485923 1.026537 |
| cholesterol reduction | 0.82 | 0.437 | .987558 1.02625 |
| triglycerides reduction | 0.36 | 0.726 | .9799687 1.028448 |
Figure 4. Meta-regression of baseline age for incident diabetes.
Figure 5. Meta-regression of gender for incident diabetes.
Figure 6. Meta-regression of baseline cholesterol for incident diabetes.
Figure 7. Meta-regression of baseline LDL for incident diabetes.
Figure 8. Meta-regression of target LDL for incident diabetes.
Figure 9. Meta-regression of LDL reduction for incident diabetes.
Sensitivity analyses and publication bias
Sensitivity analyses showed that the results from fixed-effects model (OR 1.33, 95% CI 1.15 to 1.54, I 2 = 7.7%) were similar to random-effects model meta-analysis for incident diabetes when the target LDL-c was ≤1.8 mmol/L. Fixed-effects model meta-analysis (OR 1.16, 95% CI 1.06 to 1.28, I 2 = 0%) and result, except for PROSPER trial for its positive effect (OR 1.13, 95% CI 1.02 to 1.26, I 2 = 0%), produced similar results to original analysis for new-onset diabetes when the target LDL-c was within 1.8 mmol/L to 2.59 mmol/L. A funnel plot and Egger test (P = 0.683, 95% CI −4.140 to 5.504) indicated that the publication bias of this analysis from the five trials was weak. For analysis that targets LDL-c higher than 2.59 mmol/L, the result restricted to placebo-controlled trials (OR 0.95, 95% CI 0.83 to 1.08, I 2 = 0%), and the result without ALLHAT-LLT for its biggest weight (OR 0.97, 0.87 to 1.07, I 2 = 0%) was similar to the primary analysis. The result of the fixed-effects model analysis was also consistent with the random-effects model meta-analysis when pooling data from the six trials. A funnel plot and Egger test (P = 0.046, 95% CI −8.415 to −0.120) revealed that an apparent asymmetry suggested the presence of a potential publication bias, a language bias, inflated estimates by a flawed methodologic design in smaller studies, and/or a lack of publication of small trials with opposite results.
Discussion
Aggressive LDL-c lowering based on coronary heart disease (CHD) risk reflected the potential extra benefits. Lowering LDL-c to less than 2.6 mmol/L and further lower level, e.g., 1.8 mmol/L, was recommended for those with known CHD or at very high risk. In addition, a minimum LDL-c reduction of 30% to 40% was suggested for those considered to be at moderate to very high risk for CHD [29]. A goal target is not always achievable through increasing the dose of statin drug. Doubling the statin dose is associated with an approximately 5% to 6% greater lowering of LDL-c [7], and toxicity is often dose related. A published meta-analysis reported that an intensive dose statin therapy was associated with a higher incidence of T2DM [5]. Given the potential effect of statin drug on new-onset T2DM, we were interested in the relationship between target LDL-c level after statin treatment and new-onset T2DM. The included studies were stratified by the target LDL-c level. The main findings were that statin drugs with lower intensified target LDL-c level led to higher risk of incident diabetes. Incident diabetes did not increase when the target LDL-c level was higher than 2.59 mmol/L. Aside from age, female, and base level of total cholesterol, meta-regression analysis showed that target and baseline levels of LDL-c and relative LDL-c reduction were predictors of statin-induced diabetes.
The obtained results seem at variance with a previous study [5] in that target LDL-c level and relative LDL-c reduction, but not the dose of statin drug, accounted for risk factors of statin-induced diabetes. The level of LDL-c significantly decreased by more than 30% compared with the baseline among most of the intensive dose statin studies in the previous meta-analysis. However, the participants were only stratified by the dose rather than the target goal statistically. Thus, recognizing whether statin-induced diabetes is related with LDL-c level or not from the previous study is difficult. The comparison of the three studies [intensive vs moderate dose statin study [5], intensive LDL-c lowering with statin (1.8≤LDL-c ≤2.59 mmol/L) vs placebo study, intensive LDL-c lowering with statin (LDL-c≤1.8 mmol/L) vs placebo study] showed that the relative LDL-c reductions were 12% to 22%, 29.4% to 45%, and 42% to 50%. The corresponding increased risks of statin-induced diabetes were 12%, 16%, and 33%. According to this stratified LDL-c target goal analysis, doses of statins in trials with intensified target LDL-c levels ≤1.8 mmol/L and within 1.8 mmol/L to 2.59 mmol/L were almost similar (10 mg/d to 40 mg/d), but the risk of diabetes was elevated by 17% as the LDL-c concentration decreased to approximately 0.79 mmol/L. For trials of aggressive LDL-c lowering, the dose of statin drugs was also approximately similar to the standard LDL-c lowering trials ranging from 10 mg to 40 mg per day. However, the relative LDL-c reduction was apparently higher, and the target LDL-c level was lower than the standard LDL-c lowering trials. For the intensive LDL-c lowering trials, LDL-c reduction ranged from 29.4% to 50%, and the target LDL-c level ranged from 1.4 mmol/L to 3.0 mmol/L. For the standard LDL-c lowering trials, the LDL-c reduction ranged from 11.8% to 26.7%, and the target LDL-c level ranged from 2.7 mmol/L to 3.6 mmol/L. Therefore, the exact opposite results revealed that LDL-c reduction may be a relevant factor of statin-induced diabetes. Our findings are inconsistent with the meta-regression analyses of Naveed [4] and Eliano Pio Navarese [30]. The risk for developing diabetes was affected by the ability of statins to reduce cholesterol. The differences between our study and that of Naveed et al. are accounted in the supplementary trial (SPARCL). The SPARCL trial [13] reached a relatively higher reduction of baseline LDL-c and T2DM incidence than other trials in the statin group. The replenishment of significant positive result possibly changed the whole findings. The latter meta-regression analysis recruited the trials and administered one kind of statin with unvaried dose, which may lead to aggregation bias but a relatively better homogeneity.
Less progress has been made in elucidating the mechanisms of statin-induced diabetes. Although still experimental, the potential mechanisms of statin-induced T2DM are associated with LDL-c concentration and the abilities of statins to reduce LDL-c, which are obtained from our study. A possible suggestion is that patients are aware of their treatment allocation during follow up. Those patients with substantially reduced LDL-c will be complacent and assume poorer lifestyles, gain weight, and then develop diabetes [31]. Potential plausible molecular explanations for statin-induced diabetes include impairment in insulin secretion and exacerbation of insulin resistance [32]. HMG CoA reductase inhibitors competitively inhibit the activity of HMG CoA reductase and result in a transient, modest decrease in cellular cholesterol concentration [33]. The decrease in cholesterol concentration activates a cellular signaling cascade culminating in the activation of sterol regulatory element binding protein. This protein is a transcription factor that upregulates the expression of the gene encoding the LDL receptor, which increase uptake of circulating LDL-c [34]. Thus, the more reduction of plasma LDL-c indicates higher HMG CoA reductase inhibited. The more inhibition of HMG-CoA reductase suppresses the synthesis of isoprenoids, which can significantly upregulate insulin-responsive glucose transporter-4, which leads to serious impaired glucose uptake [35]. The high glucokinase inhibition by abundance of plasma-derived LDL-c is another potential biochemical explanation for the observed increase of new-onset diabetes with lower plasma LDL-c [36]. Glucokinase is associated with the cascade of closure of ATP-dependent potassium channel, depolarization, and calcium influx that leads to insulin secretion [37], [38]. Similar to isoprenoids, ubiquinone (CoQ10) synthesis also decreases further as the reduction of circulating LDL-c increases. CoQ10 is an essential factor in the mitochondrial electron-transfer system. Thus, the decrease of CoQ10 will result in inhibition of insulin secretion because of reduced ATP production [35], [39]. In addition, the superabundant oxidation of LDL-c inside the cell may incite an inflammatory cascade. The interplay among inflammation, oxidation, and apoptosis within the β-cells, which is potentially triggered by increased abundance of cell membrane-derived LDL-c caused by the statin-induced inhibition of de-novo cholesterol synthesis [4], [35], [40], could explain higher risk of incident diabetes with lower LDL-c level.
Some limitations exist in this analysis. First, only two trials reached the target LDL-c level less than 1.8 mmol/L; thus, the effect size derived from the two trials was not sufficient and with less comparability. Second, the diagnosis of incident diabetes varied among trials like other similar studies. Third, our analysis had missing data from other large-scale trials, which lowered the statistical power. Notably, the original authors were contacted for unpublished information, but no response was received.
Conclusions
Aside from age, female, and baseline level of total cholesterol, meta-regression analyses showed that target and baseline levels of LDL-c and relative LDL-c reduction were predictors of statin-induced diabetes. The lower intensified target LDL-c level of statin therapy contributed to the higher risk of diabetes. Although the cardiovascular benefit from cholesterol-lowering statin drugs overweighs the diabetes risk, incident diabetes should be considered to weigh the pros and cons when LDL-c reaches a lower level, e.g., less than 1.8 mmol/L, especially in primary prevention low-risk patients.
Supporting Information
PRISMA Checklist.
(DOC)
Acknowledgments
We thank Mr. Q Tang, a librarian of Southeast University, for his help in making the searching strategy of this meta-analysis.
Data Availability
The authors confirm that all data underlying the findings are fully available without restriction. All relevant data are within the paper and its Supporting Information files.
Funding Statement
This work was partially supported by the National Natural Science Foundation of China (No. 81370921, Wang SH; No. 81070638, Wang SH; and No. 81070916, Guo YJ), the Social Development Project of JiangSu Province (No. SBE201170735, Wang SH), the National Nature Science Youth Foundation of China (No. 81200635, Yang Y), and the National Nature Science Foundation of Jiangsu Province (No. SBK201122155, Yang Y). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Baigent C, Keech A, Kearney PM, Blackwell L, Buck G, et al. (2005) Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet 366: 1267–1278. [DOI] [PubMed] [Google Scholar]
- 2. Cholesterol Treatment Trialists C, Baigent C, Blackwell L, Emberson J, Holland LE, et al. (2010) Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet 376: 1670–1681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Perk J, De Backer G, Gohlke H, Graham I, Reiner Z, et al. (2012) European Guidelines on cardiovascular disease prevention in clinical practice (version 2012). The Fifth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of nine societies and by invited experts). European heart journal 33: 1635–1701. [DOI] [PubMed] [Google Scholar]
- 4. Sattar N, Preiss D, Murray HM, Welsh P, Buckley BM, et al. (2010) Statins and risk of incident diabetes: a collaborative meta-analysis of randomised statin trials. Lancet 375: 735–742. [DOI] [PubMed] [Google Scholar]
- 5. Preiss D, Seshasai SR, Welsh P, Murphy SA, Ho JE, et al. (2011) Risk of incident diabetes with intensive-dose compared with moderate-dose statin therapy: a meta-analysis. JAMA: the journal of the American Medical Association 305: 2556–2564. [DOI] [PubMed] [Google Scholar]
- 6. Grundy SM, Cleeman JI, Merz CN, Brewer HB Jr, Clark LT, et al. (2004) Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Circulation 110: 227–239. [DOI] [PubMed] [Google Scholar]
- 7. Nicholls SJ, Brandrup-Wognsen G, Palmer M, Barter PJ (2010) Meta-analysis of comparative efficacy of increasing dose of Atorvastatin versus Rosuvastatin versus Simvastatin on lowering levels of atherogenic lipids (from VOYAGER). The American journal of cardiology 105: 69–76. [DOI] [PubMed] [Google Scholar]
- 8. Smith SC Jr, Benjamin EJ, Bonow RO, Braun LT, Creager MA, et al. (2011) AHA/ACCF Secondary Prevention and Risk Reduction Therapy for Patients with Coronary and other Atherosclerotic Vascular Disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation. Circulation 124: 2458–2473. [DOI] [PubMed] [Google Scholar]
- 9. Waters DD, Ho JE, DeMicco DA, Breazna A, Arsenault BJ, et al. (2011) Predictors of new-onset diabetes in patients treated with atorvastatin: results from 3 large randomized clinical trials. Journal of the American College of Cardiology 57: 1535–1545. [DOI] [PubMed] [Google Scholar]
- 10. Silva Filho CR, Saconato H, Conterno LO, Marques I, Atallah AN (2005) Assessment of clinical trial quality and its impact on meta-analyses. Revista de saude publica 39: 865–873. [DOI] [PubMed] [Google Scholar]
- 11. Moher D, Pham B, Jones A, Cook DJ, Jadad AR, et al. (1998) Does quality of reports of randomised trials affect estimates of intervention efficacy reported in meta-analyses? Lancet 352: 609–613. [DOI] [PubMed] [Google Scholar]
- 12. Gluud LL, Thorlund K, Gluud C, Woods L, Harris R, et al. (2008) Correction: reported methodologic quality and discrepancies between large and small randomized trials in meta-analyses. Annals of internal medicine 149: 219. [DOI] [PubMed] [Google Scholar]
- 13. Amarenco P, Bogousslavsky J, Callahan A 3rd, Goldstein LB, Hennerici M, et al. (2006) High-dose atorvastatin after stroke or transient ischemic attack. The New England journal of medicine 355: 549–559. [DOI] [PubMed] [Google Scholar]
- 14. Shepherd J, Blauw GJ, Murphy MB, Bollen ELEM, Buckley BM, et al. (2002) Pravastatin in elderly individuals at risk of vascular disease (PROSPER): a randomised controlled trial. Lancet 360: 1623–1630. [DOI] [PubMed] [Google Scholar]
- 15. Gissi HFI, Tavazzi L, Maggioni AP, Marchioli R, Barlera S, et al. (2008) Effect of rosuvastatin in patients with chronic heart failure (the GISSI-HF trial): a randomised, double-blind, placebo-controlled trial. Lancet 372: 1231–1239. [DOI] [PubMed] [Google Scholar]
- 16. Pedersen TR, Kjekshus J, Berg K, Haghfelt T, Faergeman O, et al. (1994) Randomized Trial of Cholesterol-Lowering in 4444 Patients with Coronary-Heart-Disease - the Scandinavian Simvastatin Survival Study (4s). Lancet 344: 1383–1389.7968073 [Google Scholar]
- 17. Downs JR, Clearfield M, Weis S, Whitney E, Shapiro DR, et al. (1998) Primary prevention of acute coronary events with lovastatin in men and women with average cholesterol levels: results of AFCAPS/TexCAPS. Air Force/Texas Coronary Atherosclerosis Prevention Study. JAMA: the journal of the American Medical Association 279: 1615–1622. [DOI] [PubMed] [Google Scholar]
- 18. Officers A, Coordinators for the ACRGTA and Lipid-Lowering Treatment to Prevent Heart Attack T (2002) Major outcomes in moderately hypercholesterolemic, hypertensive patients randomized to pravastatin vs usual care: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT-LLT). JAMA : the journal of the American Medical Association 288: 2998–3007. [DOI] [PubMed] [Google Scholar]
- 19. Nakamura H, Arakawa K, Itakura H, Kitabatake A, Goto Y, et al. (2006) Primary prevention of cardiovascular disease with pravastatin in Japan (MEGA Study): a prospective randomised controlled trial. Lancet 368: 1155–1163. [DOI] [PubMed] [Google Scholar]
- 20. Group G-PS (2000) Results of the low-dose (20 mg) pravastatin GISSI Prevenzione trial in 4271 patients with recent myocardial infarction: do stopped trials contribute to overall knowledge? GISSI Prevenzione Investigators (Gruppo Italiano per lo Studio della Sopravvivenza nell’Infarto Miocardico). Italian heart journal: official journal of the Italian Federation of Cardiology 1: 810–820. [PubMed] [Google Scholar]
- 21. Ridker PM, Danielson E, Fonseca FA, Genest J, Gotto AM Jr, et al. (2008) Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. The New England journal of medicine 359: 2195–2207. [DOI] [PubMed] [Google Scholar]
- 22. Collins R, Armitage J, Parish S, Sleigh P, Peto R, et al. (2003) MRC/BHF Heart Protection Study of cholesterol-lowering with simvastatin in 5963 people with diabetes: a randomised placebo-controlled trial. Lancet 361: 2005–2016. [DOI] [PubMed] [Google Scholar]
- 23. Sever PS, Dahlof B, Poulter NR, Wedel H, Beevers G, et al. (2003) Prevention of coronary and stroke events with atorvastatin in hypertensive patients who have average or lower-than-average cholesterol concentrations, in the Anglo-Scandinavian Cardiac Outcomes Trial-Lipid Lowering Arm (ASCOT-LLA): a multicentre randomised controlled trial. Lancet 361: 1149–1158. [DOI] [PubMed] [Google Scholar]
- 24. Kjekshus J, Apetrei E, Barrios V, Bohm M, Cleland JG, et al. (2007) Rosuvastatin in older patients with systolic heart failure. The New England journal of medicine 357: 2248–2261. [DOI] [PubMed] [Google Scholar]
- 25. Shepherd J, Cobbe SM, Ford I, Isles CG, Lorimer AR, et al. (1995) Prevention of coronary heart disease with pravastatin in men with hypercholesterolemia. West of Scotland Coronary Prevention Study Group. The New England journal of medicine 333: 1301–1307. [DOI] [PubMed] [Google Scholar]
- 26. Tonkin A, Aylward P, Colquhoun D, Glasziou P, Harris P, et al. (1998) Prevention of cardiovascular events and death with pravastatin in patients with coronary heart disease and a broad range of initial cholesterol levels. New Engl J Med 339: 1349–1357. [DOI] [PubMed] [Google Scholar]
- 27. Higgins JPT, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. British medical journal 327: 557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Egger M, Smith GD, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. British medical journal 315: 629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Grundy SM, Cleeman JI, Merz CN, Brewer HB Jr, Clark LT, et al. (2004) Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III Guidelines. Journal of the American College of Cardiology 44: 720–732. [DOI] [PubMed] [Google Scholar]
- 31. Preiss D, Sattar N (2011) Statins and the risk of new-onset diabetes: a review of recent evidence. Current opinion in lipidology 22: 460–466. [DOI] [PubMed] [Google Scholar]
- 32. Koh KK, Lim S, Sakuma I, Quon MJ (2012) Caveats to aggressive lowering of lipids by specific statins. International journal of cardiology 154: 97–101. [DOI] [PubMed] [Google Scholar]
- 33. Kumar VH, Dwajani S, Gurjar D, Patil U, Vinodkumar C (2011) Effect of rosuvastatin as an anti-inflammatory agent in albino rats. Asian Journal of Pharmaceutical and Clinical Research 4: 74–76. [Google Scholar]
- 34. Stancu C, Sima A (2001) Statins: mechanism of action and effects. Journal of cellular and molecular medicine 5: 378–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Sattar N, Taskinen MR (2012) Statins are diabetogenic–myth or reality? Atherosclerosis Supplements 13: 1–10. [DOI] [PubMed] [Google Scholar]
- 36. Kruit JK, Brunham LR, Verchere CB, Hayden MR (2010) HDL and LDL cholesterol significantly influence beta-cell function in type 2 diabetes mellitus. Current opinion in lipidology 21: 178–185. [DOI] [PubMed] [Google Scholar]
- 37. Kearney PM, Blackwell L, Collins R, Keech A, Simes J, et al. (2008) Efficacy of cholesterol-lowering therapy in 18,686 people with diabetes in 14 randomised trials of statins: a meta-analysis. Lancet 371: 117–125. [DOI] [PubMed] [Google Scholar]
- 38.Ting RZW, Yang XL, Yu LWL, Luk AOY, Kong APS, et al.. (2010) Lipid control and use of lipid-regulating drugs for prevention of cardiovascular events in Chinese type 2 diabetic patients: a prospective cohort study. Cardiovascular diabetology 9. [DOI] [PMC free article] [PubMed]
- 39. Marder SR, Essock SM, Miller AL, Buchanan RW, Casey DE, et al. (2004) Physical health monitoring of patients with schizophrenia. Am J Psychiat 161: 1334–1349. [DOI] [PubMed] [Google Scholar]
- 40. Nakata M, Uto N, Maruyama I, Yada T (1999) Nitric oxide induces apoptosis via Ca2+-dependent processes in the pancreatic beta-cell line MIN6. Cell Struct Funct 24: 451–455. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
PRISMA Checklist.
(DOC)
Data Availability Statement
The authors confirm that all data underlying the findings are fully available without restriction. All relevant data are within the paper and its Supporting Information files.