Abstract
Background
Physical therapy intervention is the primary treatment for gait ataxia and imbalance in individuals with cerebellar damage. Our aim was to determine if a home balance exercise program is feasible for improving locomotor and balance abilities in these individuals.
Methods
Fourteen subjects with cerebellar ataxia participated in a six-week individualized home-based balance exercise program and attended five testing sessions (2 pre-training, 1 mid-training, 1 post-training, and 1 one month follow-up visit). Pre-training, post-training, and follow-up testing included a neurological assessment, clinical gait and balance tests, and laboratory assessments of balance and walking. Subjects kept logs of the frequency and level of balance challenge during their training.
Results
Walking speed improved across visits, as did stride length, percent double limb support time, timed up and go (TUG), and dynamic gait index. Post-hoc comparison in these measures revealed that significant rehabilitative improvements occurred over the six-week training period, and all but TUG were retained one month later. There were no changes across the other measures for the group. Regression analysis indicated that improvements in walking speed were affected by the level of balance challenge but not by age, ataxia severity, proprioception, or duration of exercise.
Conclusions
Improvement in locomotor performance in people with cerebellar ataxia was observable after a six-week home balance exercise program. The exercise program must be designed to provide a significant challenge to the person's balance.
Keywords: ataxia, exercise therapy, neurodegenerative diseases/rehabilitation, treatment outcome
Introduction
Individuals with cerebellar degenerative disease exhibit progressive worsening of motor coordination, or ataxia. In walking, ataxia is evident by a shortened stride length, high step pattern, and decreased push-off and veering.1 These gait deviations have been closely linked to the severity of the individual's balance deficits.2 These deficits lead to taxing and unsafe mobility. Without any available disease-modifying pharmacological treatments for ataxia,3 physical therapy intervention is the primary treatment option. 4 However, efforts to restore normal movement are complicated because individuals with cerebellar disease also have deficits in motor learning.5 It has therefore been reasoned that these patients may get limited benefit from rehabilitation that relies on motor learning.6
Despite these considerable challenges, recent evidence suggests that individuals with cerebellar disease may benefit from long-term motor training. Following an intensive, high-level four-week training program, cerebellar patients showed the ability to improve motor skills and functional performance.4, 7-9 These studies, however, involved supervised exercise in a clinical setting. Beyond these studies and some case studies, research concerning exercise and physical therapy for ataxia is severely lacking. 10,11-15
Here we asked if a home-based balance exercise program could improve locomotor and balance abilities in individuals with degenerative cerebellar disease. Given that voluntary leg-coordination deficits play less of a role than balance deficits in gait ataxia,2 the exercise program focused on static and dynamic balance activities rather than direct gait training. The exercises included balancing in both sitting and standing positions, which allows both highly functional individuals (able to stand on one leg) and more severely affected individuals (requiring hand support to standing) to use the program. Clinical and laboratory measures were used to assess changes in balance and gait over the course of training and one month later. We also examined the influence of age, ataxia severity, duration of exercise, and level of balance challenge on training-induced changes in walking speed.
Methods
Participants
Individuals with cerebellar damage degenerative diseases participated in the study. All participants were able to stand and take steps, although four participants used walkers and one used a cane for walking. Cerebellar damage for all participants was confirmed by magnetic resonance imaging or a computer tomography scan. Results of genetic testing were obtained when available. Individuals who had a genetic disease that primarily involved the cerebellum (e.g., spinocerebellar ataxia (SCA) 6) or had extra-cerebellar signs (e.g., SCA2, SCA3) were enrolled as long as their primary problem was ataxia. Clinically, all participants had evidence of at least mild ataxia (International Cooperative of Ataxia Rating Scale (ICARS) score > 5)16 for over three months. Participants were excluded if they had other neurological diseases (e.g., Parkinson's disease), cognitive impairment (e.g., Mini-Mental State exam score < 22), or if they were medically unstable (e.g., uncontrolled hypertension, unstable angina). All participants gave informed consent according to the human studies guidelines of the Johns Hopkins Institutional Review Board.
Of the 25 participants who were screened and consented, 14 participated in the complete study, and only their data are included in the results. Four participants were unable to ambulate sufficiently for laboratory measures to be determined; three participants discontinued the study due to burden of travel; two discontinued due to unrelated medical complications; and two participants did not meet the testing schedule and exercise compliance requirements.
Paradigm
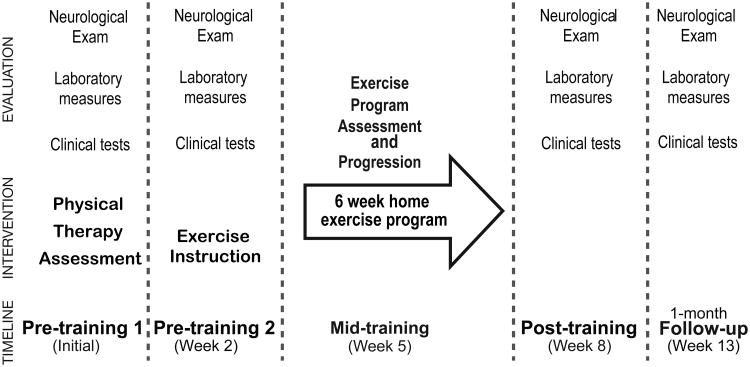
All participants performed a home-based balance exercise program for six weeks and attended five testing sessions (two pre-training, one mid-training, and two post-training visits) (Figure 1). Participants served as their own controls since we included two pre-training visits spaced two weeks apart. The exercise intervention was initiated at the second pre-training visit. A physical therapist contacted the participants weekly by email or phone to answer any questions about the exercise protocol. One mid-training visit three weeks into the program was used for evaluating the program's progression. Participants logged their exercise effort both in terms of frequency and level of balance challenge. Participants were retested when the training ended and again four weeks later to assess the longevity of the rehabilitation effects. Each testing session included a neurology assessment, clinical gait and balance tests, and laboratory assessment of balance and walking kinematics.
Figure 1. Study paradigm.
All subjects performed a home-based exercise program for six weeks. Two sets of pre-training measurements were taken two weeks apart to assess repeatability of our measures. One mid-training visit was used to reevaluate the program progression. Subjects were retested after six weeks of training and again four weeks after the completion of training to assess retention.
Assessment tools
Ataxia severity was measured using the International Cooperative Ataxia Rating Scale (ICARS).16 The ICARS evaluates the degree of ataxia in four domains: posture and gait, limb kinetics, speech, and oculomotor. We also assessed fine touch in the great toe using Semmes Weinstein monofilaments and proprioception via clinical assessment of great toe motion. Spasticity and hyperreflexia at the ankle and knee were assessed and, if present, noted.
The following clinical gait and balance tests were performed according to established protocols: 1) the Dynamic Gait Index (DGI),17 2) the Timed Up and Go Test (TUG),18 3) the Functional Reach Test (FR),19 and 4) the Activities Specific Balance Confidence Scale (ABC).20
Static standing balance was assessed by measuring postural sway during two, 20-second trials. Participants stood with arms crossed over their chest and feet shoulder-width apart under two conditions: eyes open and eyes closed. Data were collected at 1000 Hz using a Kistler 9281 force plate (Kistler Instrument AG; Winterhur, Switzerland). Balance deficits were calculated as the magnitude of postural sway (sway amplitude) using custom Matlab software (MathWorks Inc.; Natick, MA).
For the walking assessment, participants walked as fast as possible on a 12-meter runway six times, and we averaged the times of trials 3-6. Walking speed was our main outcome measure. We also collected marker position data from infrared emitting diodes placed bilaterally at the fifth metatarsal heads, lateral malleoli, lateral knee joint spaces, greater trochanters, pelvic crests, and acromiums at 100 Hz using a three-dimensional Optotrak motion capture system (Northern Digital, Inc.; Ontario, Canada). Custom Matlab software was used to calculate joint position and determine walking parameters. Stride length was calculated as the distance between initial foot contact of one foot and the next contact of the same foot. The percent time in double limb support was the time that both feet were in contact with the floor expressed as a percentage of the stride time.
Intervention
The six-week home-based exercise program focused on balance training. Both static and dynamic exercises were done in sitting and standing positions. For each subject, a tailored home balance exercise program was developed by a physical therapist based on the testing results of the first pre-training visit. Due to the range of ataxia severity in the subjects, sitting exercises were performed using one of four surfaces: standard chair, 6 in dense foam, exercise ball (standard or peanut shaped), or balance disc. Similarly, the amount of upper extremity support used for safety during the sitting or standing exercises varied from holding on to a stable object (i.e. walker, chair) with two hands to no support. Exercises started with stabilizing in a challenging static position and progressed to dynamic arm and leg movements in the same or modified position. Subjects were given six study exercises designed to challenge their balance. Depending on the subject, an additional warm-up exercise was given to allow time to adjust to the equipment. Table 2 describes examples of the different types of exercises that were given. The categories and type of exercise were tailored to each subject's abilities. Subjects were instructed to perform the exercises for approximately three to five minutes each for a total minimum of 20 minutes per day, four to six days per week. At the end of the six-week program, subjects were told they no longer were required to do the exercises as part of the study.
Table 2.
Examples of balance exercises.
| Exercise category | Description |
|---|---|
| Seated, stable surface |
|
| Seated, dynamic surface |
|
| Standing, stable surface progressing to foam surface. |
|
| Stepping and stooping |
|
Subjects were provided with instructions on how to perform the exercises using PhysioTools™ General Exercises 1st Edition software (PhysioTools; Tampere, Finland), in-person demonstrations, and a DVD for home review. Subjects acknowledged understanding of the exercise program through return demonstration initially and at the mid-training visit. General exercise guidelines, with an emphasis on safety, were reviewed and provided in a booklet. An exercise log was provided for entering dates and duration (minutes) of exercise. Additionally, subjects were asked to rate their confidence with each exercise on a 100% scale; where 0% was no confidence at maintaining their balance during the task and 100% was complete confidence. The level of challenge of each exercise was defined as 100% minus the confidence rating. The average challenge rating of the six exercises on day one was used as an overall measure of the level of balance challenge for each participant.
Data Analysis
Intraclass correlation coefficients (ICC) were calculated to determine repeatability of the measures taken during the two pre-training visits. ICC (1,2) was used for the laboratory measures, which were averages of more than one trial, and ICC (1,1) was used for the clinical one-trial measures.21 The averages of the measures from the two pre-training visits were used in the rest of the analyses. We used ANOVA to determine change across visits. Repeated measures ANOVA were used for laboratory data. Friedman's ANOVA (nonparametric measures) was used for clinical rating scale data, which did not meet assumptions for parametric tests. Post-hoc tests of Tukey HSD or Wilcoxon matched pairs test were used to compare the change over the training period and retention of any benefits at one month. Coefficient of variation was determined for stride length data and repeated measures ANOVA was used to assess for change across visits. A forward stepwise regression was used to assess the extent to which walking speed change in the group was affected by age, ataxia severity, duration of exercise in number of days performed, and level of balance challenge.
Results
Demographic data and exercise log results of the fourteen participants who completed the study are shown in Table 1. Pretest assessment of the group showed that they had considerable ataxia, with an average overall ICARS score of 39 ±15. The gait and posture ICARS subscore for the group was 15 ± 7. The clinical measures showed impairments in gait (DGI median 14, range 6-22), balance (TUG 15.2 ± 9.5 s; FR 12.25 ± 3.25 in) and decreased confidence with mobility (ABC median 61%, range 36-85%). Proprioception was intact in the lower extremity as tested in the great toe for all but four subjects (#4, 11, 13, 14). Light touch sensation was present for all but three subjects (# 4, 7, 11), who showed loss of protective sensation (light touch sensation impaired >10 g force via 5.07 Semmes Weinstein monofilament). Reflexes were increased at the patella in two subjects (#4, 9).
Table 1.
Subject characteristics pre-training and exercise log summary.
| Subject | Diagnosis | Disease duration (y) | Sex | Age (y) | ICARS (total) | Exercise Duration (days) | Exercise Challenge (%) |
|---|---|---|---|---|---|---|---|
| 1 | SCA 8 | 10 | M | 35 | 46 | 23 | 10 |
| 2 | SCA 6 | 20 | M | 74 | 55 | 27 | 18 |
| 3 | SCA 17 | 5 | M | 56 | 49 | 26 | 33 |
| 4 | Sporadic | 20 | F | 53 | 57 | 30 | 13 |
| 5 | SCA 5 | 5 | M | 56 | 35 | 24 | 40 |
| 6 | ADCA | 20 | F | 30 | 8 | 18 | 50 |
| 7 | ADCA | 10 | M | 57 | 10 | 19 | 68 |
| 8 | SCA 6 | 5 | F | 56 | 29 | 16 | 53 |
| 9 | Sporadic | 20 | M | 53 | 56 | 14 | 70 |
| 10 | Sporadic | 10 | F | 37 | 33 | 28 | 73 |
| 11 | SCA 3 | 20 | F | 61 | 58 | 16 | 60 |
| 12 | Sporadic | 20 | M | 49 | 36 | 20 | 65 |
| 13 | Sporadic | 20 | F | 60 | 37 | 23 | 53 |
| 14 | Sporadic | 5 | F | 57 | 40 | 35 | 49 |
|
| |||||||
| Mean (SD) | 7M/7F | 52 (11) | 39 (15) | 23 (6) | 47 (20) | ||
ICARS = International Cooperative Ataxia Rating Scale (total score, 100 possible); ADCA=autosomal dominant cerebellar ataxia; SCA= spinocerebellar ataxia.
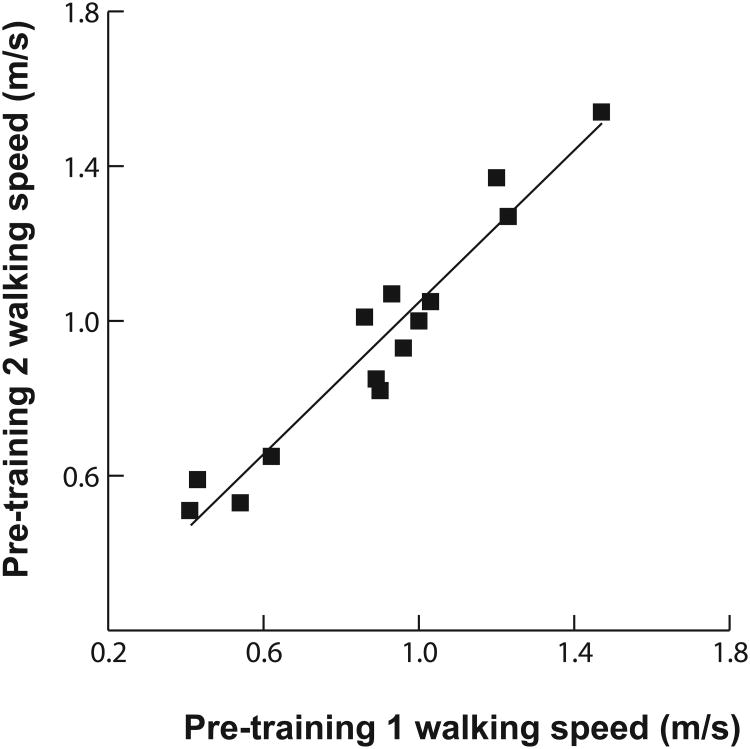
The pretest laboratory measures were as follows: walking speed at fastest possible pace was 0.9 ± 0.3 m/s; stride length was 1.08 ± 0.22 m; percent stance time was 64 ± 4 s; percent double support time was 14 ± 4 s. Postural sway amplitude in static standing (eyes open feet apart) was 10.4 ± 4.6 mm. Despite the inherent variability seen in the movement patterns of the participants, the intra-class correlation coefficients for most of our measures was high: walking speed 0.90; stride length 0.84, percent double support 0.72, static standing 0.99, ICARS (total) 0.91, DGI 0.72, TUG 0.94, FR 0.99, ABC 1.00. Figure 2 depicts this strong relationship for walking speed.
Figure 2.
Walking speed reliability across the two pre-training sessions was high (ICC = 0.9). The scatter plot shows walking speeds for both pre-training visits for all participants.
Overall, participants were compliant with the exercise program, although a few reported difficulty in challenging their balance at home (Table 1). Eleven of the fourteen participants performed their individualized home program three or more days per week. Ten of the participants reported at least 40% balance challenge (i.e., 60% confidence) with the exercises. Comparing ratings of the first and second halves of training, each subject's challenge rating of their exercises was within 5% of the value listed in Table 1 except for two subjects (#12 increased 10%; #13 decreased 25%). Four weeks after the training period (i.e., follow-up visit), four subjects indicated they had discontinued all balance exercises. Across the remaining ten subjects a reduction in frequency and duration of performance was reported. No subjects reported falls while performing the exercises.
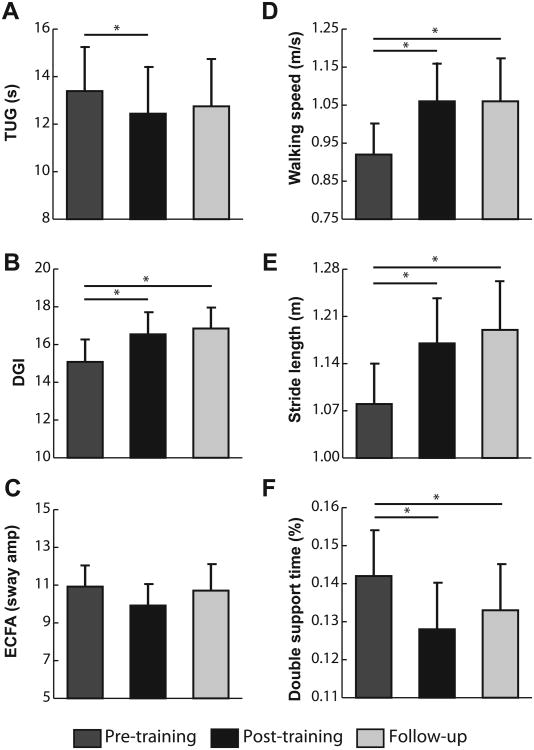
The group showed a significant improvement across pre-training, post-training, and follow-up visits in both clinical measures and laboratory tests (Figure 3). Note that subject #11 was unable to complete all clinical measures on the final visit due to illness, and therefore is excluded from the overall clinical analysis. Of our clinical measures, ANOVA of TUG and DGI revealed improvements in gait and balance across visits (p=0.02 and p<0.001, respectively). Post-hoc tests of these measures between pre-training and post-training visits revealed that significant rehabilitation effects occurred in the six-week training period (both p<0.05, Figure 3A and 3B). Pre-training to follow-up visit comparisons showed the effects were retained one month later in the DGI (p=0.002) but not the TUG (p>0.05). The FR, ABC, and ICARS scores did not change across visits for the group (all p>0.05), although there were individual participants who improved in each of these measures.
Figure 3. Results of training.
Selected results from the comparison across pre-training, post-training, and follow-up visits. Clinical measures: timed up and go (A), dynamic gait index (B). Static balance measure: sway amplitude for eyes closed condition (average of all subjects except #9, 11, 12, 13, who were unable to perform the task) (C). Walking parameters: walking speed (D), stride length (E), double support time percent (F). Average values ± 1 standard error indicated for all measures; asterisks indicate post-hoc comparison for measures with significant differences (p<0.05).
An ANOVA revealed an effect of visit for our primary outcome measure, average walking speed (p<0.001), which increased 15% from pre-training to post-training. This is nearly three times the minimally important difference reported for people with other neurological disorders. 22, 23 Post-hoc comparison showed the difference was significant between pre-training and post-training, indicating change occurred over the six-week training period (Figure 3D, p<0.001). The change was also significant from the pre-training to the follow-up visit, indicating the improvement was retained (p<0.001). Of the other walking parameters, ANOVA revealed that stride length and percent double support time also showed improvement across visits (p<0.001 and p<0.01, Figure 3E and 3F, respectively), while percent stance time did not show significant change (p>0.05). Note that subjects #2 and 4 were not included in the percent stance and percent double support analyses due to marker occlusion from their walkers. Postural sway amplitude did not change significantly across visits (p>0.05). Results for postural sway amplitude for condition two (eyes closed) are shown in Figure 3C.
We also measured the coefficient of variation of stride length to assess stride-to-stride variability within each subject. Higher values of this measure indicate more variability. The pre-training group average was 9.2 ± 1.6, post-training was 6.1 ± 1.3, and follow-up was 6.0 ± 1.1. Repeated measures ANOVA showed a trend toward less variability after training (p=0.10).
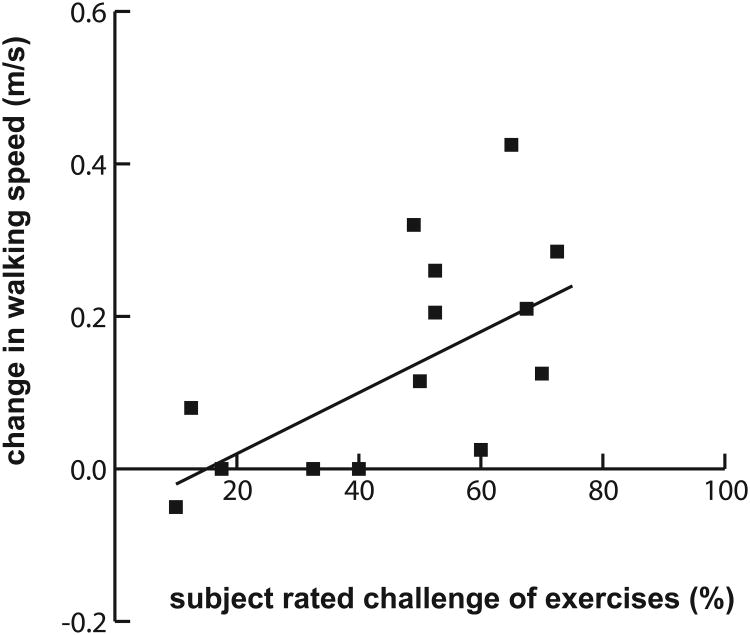
Regression analysis indicated that the change in group walking speed was affected only by the level of balance challenge (Figure 4), and not by age, ICARS gait and posture subscore, proprioception, or duration of exercise. We used the ICARS gait and posture subscore in this regression since it correlated with pre-training walking speed, and was thus a good indicator of walking impairment.
Figure 4. Effect of degree of balance challenge.
Scatter plot showing the correlation between change in walking speed and self-rated challenge of exercises. Regression equation: Δ WS = -0.06 + 0.004*challenge; R2=0.43; p=0.01.
Discussion
We found that cerebellar patients with ataxia can benefit from a home exercise program focused on balance training. Despite only including 14 patients, we found statistically and clinically significant improvements after just six weeks. An important finding is that the level of challenge to balance was more important than the duration of exercise in producing positive effects. Therefore, individualizing the program and offering continued training and progression might be necessary to see effect retention. This study provides valuable new insight, as very few previous studies have looked at exercise programs for cerebellar ataxia and in particular home programs with limited one-on-one practice with a therapist.3, 7, 24 In addition to the well-known benefits that come from improving walking parameters, the advantages of the observed effects in this study may include increased sense of control and independence and improved quality of life. The home program may also provide a means to optimize the use of financial and healthcare resources in the face of the often functionally-limiting progressive disease of degenerative cerebellar ataxia.25
The pre-training tests indicated that while our group of patients was ambulatory, they were severely affected relative to individuals with ataxia who have been previously studied: the average fast walking speed of 0.9 m/s is comparable to self-selected walking speeds reported in other studies of individuals with degenerative cerebellar disease. 4 Although more severe ataxia results in greater variability of movement, we were able to get stable pre-training measurements, which suggests that our subjects could validly serve as their own controls.
The exercise intervention was individualized to optimize challenge and ensure safety. Sitting balance exercises were an important component of the program as the level of challenge could be varied by varying the support surface. Standing exercises were often limited to dynamic arm and trunk movements performed from a stable starting point. For most participants, balance tasks during walking were too challenging to be done safely without assistance. Direct instruction in the program was limited to the second pre-training visit, with reassessment and progression at mid-training (week three of six). Even with the limited training, the group demonstrated significant improvement in both clinical and laboratory measures after six weeks.
Walking improved significantly for the group across the pre-training, post-training, and follow-up visits. A significant increase in fast walking speed was observed after training and was retained one month later. This is an important result as walking speed has been shown to reflect overall functional independence and good quality of life. Two other locomotor features were improved: stride length increased and percent double support time decreased. Thus, subject could take longer steps and spent less time transitioning from one foot to the other. Both of our clinical measures of walking, TUG and DGI, also improved. The DGI improvement may reflect changes in functional skills (e.g., stepping around cones and over an obstacle) that may be more impacted by leg placement deficits where visual guidance is needed, in addition to deficits in balance or general walking. Improvements in walking are striking considering that balance training was primarily done in sitting and standing positions with little focus on gait activities.
With the observed gains in walking, it is surprising that we did not find changes in our clinical standing balance measure (functional reach) or in our laboratory balance measure (postural sway during static standing). We can only speculate that training, which included both dynamic and static balance exercises, affected dynamic balance more than static balance, and we did not test dynamic balance. Improving dynamic balance during gait may be reflected in the trend towards reduced variability in stride length across visits. In the future a dynamic balance test, such as shift of center of gravity, should be assessed.26, 27
ICARS and ABC scores did not change over the 13 weeks. Previously, we showed that the ICARS is a sensitive measure for assessing the decline in degenerative ataxia over a one-year period.27 Since other measures were sensitive to improvement in this study, it appears that the ICARS is not sensitive to more subtle improvements that occur over shorter timeframes.
The ABC scale measures participants' balance confidence, but many participants were unable to recall the last time they had attempted many of the skills rated in the scale (e.g., standing on a chair, walking on ice). In future studies another measure for perceived change should be used, such as the individualized measure of the goal attainment score.
Interestingly, there were self-reports of improvements in everyday life after training. Three participants, for example, noted that they were able to close their eyes in the shower when washing their hair, which they were previously unable to do. Two noted greater confidence starting and stopping while walking in the city, and one participant no longer needed a hiking stick to walk and work in the family farm.
We wanted to determine what factors influenced the changes observed following participation in the home exercise program. Previously, we showed that the posture and gait subscore of the ICARS is a predictor of severity of ataxia and function at one year after testing for degenerative cerebellar disease.27 We suspected that in addition to severity of ataxia, age, balance challenge, and duration of practice could be factors that would predict improvement. However, we found that higher level of balance challenge was the only factor that predicted greater improvement in walking speed. Without a control group this finding is limited but does emphasize the importance of designing an appropriately challenging program, as well as determining an individual's ability to follow a home program. This finding is in contrast to that of Ilg et al.,7 who found that frequency was an important factor in retaining changes.
The improvements in walking speed after the six-week exercise program are similar in magnitude to those seen after an intensive program with direct intervention.4 It is valuable to demonstrate that a home program can be as effective as direct care. Home programs are less costly, require less travel, and may be more convenient for patients who do not have access to a clinic. With the necessity of challenging an individual's balance, direct intervention, however, may be necessary for individuals who are unable to safely challenge their balance alone at home.
Determining the appropriate dose of intervention is an important next step. While rehabilitation will not prevent progression of cerebellar degeneration, future longitudinal studies can examine what doses of training optimize function throughout the course of the disease. Additionally, since our program primarily included sitting and standing balance exercises, individuals who are no longer able to walk can potentially use the program. Safer transfers and greater mobility in later stages of cerebellar degeneration would greatly improve patients' quality of life.
As with most home programs, participant compliance both in terms of frequency and quality of performance was limited to monitoring by self-report and demonstration at follow-up. Challenging balance in the home was emphasized but for safety reasons was difficult for some subjects. Since our results suggest that greater levels of challenge of the exercises is crucial for improvement, for participants who could not safely challenge themselves at home additional training sessions or direct supervision of the exercise program may have been more beneficial.
Conclusions
This study demonstrates improvement in both clinical and laboratory measures of mobility in cerebellar patients with ataxia after a six-week home training program. After limited one-on-one practice with a therapist, the home exercise program, which focused on balance training, improved locomotion. Individualizing the training program may be critical, as our results suggest that challenging balance is more important for improving walking characteristics and speed than increasing exercise frequency. Continued training and progression of the program may be necessary to see optimal retention of results.
Acknowledgments
The authors would like to thank Kristin Musselman for helpful review of this manuscript. This study was supported by NIH R01 HD040289.
Footnotes
Author Roles: J. Keller: acquisition, analysis, and interpretation of data; writing of manuscript. A Bastian: study concept and design; acquisition, analysis, and interpretation of data; writing of manuscript; study supervision.
Full Financial Disclosures of all Authors for the Past Year: The authors have no conflicts of interest to report.
References
- 1.Bastian AJ. Moving, sensing and learning with cerebellar damage. Curr Opin Neurobiol. 2011;21(4):596–601. doi: 10.1016/j.conb.2011.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Morton SM, Bastian AJ. Relative contributions of balance and voluntary leg-coordination deficits to cerebellar gait ataxia. J Neurophysiol. 2003;89(4):1844–1856. doi: 10.1152/jn.00787.2002. [DOI] [PubMed] [Google Scholar]
- 3.Trujillo-Martin MM, Serrano-Aguilar P, Monton-Alvarez F, Carrillo-Fumero R. Effectiveness and safety of treatments for degenerative ataxias: a systematic review. Mov Disord. 2009;24(8):1111–1124. doi: 10.1002/mds.22564. [DOI] [PubMed] [Google Scholar]
- 4.Ilg W, Synofzik M, Brotz D, Burkard S, Giese MA, Schols L. Intensive coordinative training improves motor performance in degenerative cerebellar disease. Neurology. 2009;73(22):1823–1830. doi: 10.1212/WNL.0b013e3181c33adf. [DOI] [PubMed] [Google Scholar]
- 5.Morton SM, Bastian AJ. Cerebellar contributions to locomotor adaptations during splitbelt treadmill walking. J Neurosci. 2006;26(36):9107–9116. doi: 10.1523/JNEUROSCI.2622-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Thach WT, Bastian AJ. Role of the cerebellum in the control and adaptation of gait in health and disease. Prog Brain Res. 2004;143:353–366. doi: 10.1016/s0079-6123(03)43034-3. [DOI] [PubMed] [Google Scholar]
- 7.Ilg W, Brotz D, Burkard S, Giese MA, Schols L, Synofzik M. Long-term effects of coordinative training in degenerative cerebellar disease. Mov Disord. 2010;25(13):2239–2246. doi: 10.1002/mds.23222. [DOI] [PubMed] [Google Scholar]
- 8.Miyai I. Challenge of neurorehabilitation for cerebellar degenerative diseases. Cerebellum. 2012;11(2):436–437. doi: 10.1007/s12311-011-0327-5. [DOI] [PubMed] [Google Scholar]
- 9.Miyai I, Ito M, Hattori N, et al. Cerebellar ataxia rehabilitation trial in degenerative cerebellar diseases. Neurorehabil Neural Repair. 2012;26(5):515–522. doi: 10.1177/1545968311425918. [DOI] [PubMed] [Google Scholar]
- 10.Balliet R, Harbst KB, Kim D, Stewart RV. Retraining of functional gait through the reduction of upper extremity weight-bearing in chronic cerebellar ataxia. Int Rehabil Med. 1987;8(4):148–153. doi: 10.3109/03790798709166204. [DOI] [PubMed] [Google Scholar]
- 11.Freund JE, Stetts DM. Use of trunk stabilization and locomotor training in an adult with cerebellar ataxia: a single system design. Physiother Theory Pract. 2010;26(7):447–458. doi: 10.3109/09593980903532234. [DOI] [PubMed] [Google Scholar]
- 12.Freund JE, Stetts DM. Continued recovery in an adult with cerebellar ataxia. Physiother Theory Pract. 2013;29(2):150–158. doi: 10.3109/09593985.2012.699605. [DOI] [PubMed] [Google Scholar]
- 13.Karakaya M, Kose N, Otman S, Ozgen T. Investigation and comparison of the effects of rehabilitation on balance and coordination problems in patients with posterior fossa and cerebellopontine angle tumours. J Neurosurg Sci. 2000;44(4):220–225. [PubMed] [Google Scholar]
- 14.Perez-Avila I, Fernandez-Vieitez JA, Martinez-Gongora E, Ochoa-Mastrapa R, Velazquez-Manresa MG. Effects of a physical training program on quantitative neurological indices in mild stage type 2 spinocerebelar ataxia patients. Rev Neurol. 2004;39(10):907–910. [PubMed] [Google Scholar]
- 15.Vaz DV, Schettino Rde C, Rolla de Castro TR, Teixeira VR, Cavalcanti Furtado SR, de Mello Figueiredo E. Treadmill training for ataxic patients: a single-subject experimental design. Clin Rehabil. 2008;22(3):234–241. doi: 10.1177/0269215507081578. [DOI] [PubMed] [Google Scholar]
- 16.Trouillas P, Takayanagi T, Hallett M, et al. International Cooperative Ataxia Rating Scale for pharmacological assessment of the cerebellar syndrome. The Ataxia Neuropharmacology Committee of the World Federation of Neurology. J Neurol Sci. 1997;145(2):205–211. doi: 10.1016/s0022-510x(96)00231-6. [DOI] [PubMed] [Google Scholar]
- 17.Shumway-Cook A, Woollacott MH. Motor control: theory and practical applications. Williams & Wilkins Baltimore; 1995. [Google Scholar]
- 18.Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142–148. doi: 10.1111/j.1532-5415.1991.tb01616.x. [DOI] [PubMed] [Google Scholar]
- 19.Duncan PW, Weiner DK, Chandler J, Studenski S. Functional reach: a new clinical measure of balance. J Gerontol. 1990;45(6):M192–7. doi: 10.1093/geronj/45.6.m192. [DOI] [PubMed] [Google Scholar]
- 20.Powell LE, Myers AM. The Activities-specific Balance Confidence (ABC) Scale. J Gerontol A Biol Sci Med Sci. 1995;50A(1):M28–34. doi: 10.1093/gerona/50a.1.m28. [DOI] [PubMed] [Google Scholar]
- 21.Rankin G, Stokes M. Reliability of assessment tools in rehabilitation: an illustration of appropriate statistical analyses. Clin Rehabil. 1998;12(3):187–199. doi: 10.1191/026921598672178340. [DOI] [PubMed] [Google Scholar]
- 22.Musselman KE, Yang JF. Walking tasks encountered by urban-dwelling adults and persons with incomplete spinal cord injuries. J Rehabil Med. 2007;39(7):567–574. doi: 10.2340/16501977-0090. [DOI] [PubMed] [Google Scholar]
- 23.Perera S, Mody SH, Woodman RC, Studenski SA. Meaningful change and responsiveness in common physical performance measures in older adults. J Am Geriatr Soc. 2006;54(5):743–749. doi: 10.1111/j.1532-5415.2006.00701.x. [DOI] [PubMed] [Google Scholar]
- 24.Martin CL, Tan D, Bragge P, Bialocerkowski A. Effectiveness of physiotherapy for adults with cerebellar dysfunction: a systematic review. Clin Rehabil. 2009;23(1):15–26. doi: 10.1177/0269215508097853. [DOI] [PubMed] [Google Scholar]
- 25.Barlow J, Wright C, Sheasby J, Turner A, Hainsworth J. Self-management approaches for people with chronic conditions: a review. Patient Educ Couns. 2002;48(2):177–187. doi: 10.1016/s0738-3991(02)00032-0. [DOI] [PubMed] [Google Scholar]
- 26.Ilg W, Synofzik M, Brotz D, Burkard S, Giese MA, Schols L. Intensive coordinative training improves motor performance in degenerative cerebellar disease. Neurology. 2009;79(20):2056–2060. doi: 10.1212/WNL.0b013e3181c33adf. [DOI] [PubMed] [Google Scholar]
- 27.Morton SM, Tseng YW, Zackowski KM, Daline JR, Bastian AJ. Longitudinal tracking of gait and balance impairments in cerebellar disease. Mov Disord. 2010;25(12):1944–1952. doi: 10.1002/mds.23169. [DOI] [PMC free article] [PubMed] [Google Scholar]