Abstract
Objectives
This study examined the prevalence of clinically significant anxiety among informal hospice caregivers and identified characteristics of caregivers who experienced anxiety of this severity.
Methods
An exploratory secondary analysis of data pooled from three separate studies of informal hospice caregivers (N=433) was conducted. Researchers employed descriptive statistics to calculate anxiety prevalence and used logistic regression to model the associations between the covariates (i.e., caregiver characteristics) and anxiety.
Results
Overall, 31% of informal hospice caregivers reported moderate or higher levels of anxiety. Caregivers associated with the research site in the Northwest were less likely to be anxious than those in the Southeast [χ2(3, N = 433) = 7.07, p = .029], and employed caregivers were less likely to be anxious than unemployed caregivers (OR = 0.56, 95% CI = 0.33, 0.96). The likelihood of being anxious decreased with increasing physical quality of life (OR = 0.77, 95% CI = 0.69, 0.85), and younger female caregivers were more likely to be anxious than male caregivers and older females (OR = 0.95, CI = 0.91, 0.99).
Significance of Results
A noteworthy portion of informal hospice caregivers experience clinically significant levels of anxiety. Increased efforts to screen and address anxiety in this population are recommended.
Keywords: anxiety, hospice care, caregivers, family
Introduction
As a model of end-of-life care, hospice is designed to support the quality of life of patients and their families through management of the full range of bio-psycho-social-spiritual concerns that arise as death nears (Waldrop & Meeker, 2012). Critical to the provision of hospice services are informal hospice caregivers. Informal hospice caregivers are the spouses, adult children, and other relatives and friends who provide typically unpaid care to an individual receiving hospice services. As the dying trajectory advances, hospice patients often require increasing levels of help from informal caregivers who assist with medication administration, activities of daily living, and communication with health care professionals. Informal caregivers are also a significant source of emotional and spiritual support for many hospice patients (Haley et al., 2002; McMillan, 2005; National Hospice and Palliative Care Organization, 2005).
Because the philosophy underpinning hospice care conceptualizes both the patient and his or her loved ones as the “unit of care,” informal hospice caregivers are simultaneously regarded as co-providers and co-recipients of support. While informal caregivers may derive personal benefits from caring for their dying loved one, such as a sense of inner peace, personal growth, and an enhanced appreciation for life, they may also experience social isolation, sleep disturbances, and challenges finding time to engage in self-care (Funk et al., 2010). Additional potential stressors include perceived loss of control, communication challenges, financial difficulties, and unsolicited critiques regarding caregiving quality (Wittenberg-Lyles et al., 2012). For some caregivers, these stressors are associated with experiences of psychological distress, including symptoms of anxiety (Chentsova-Dutton et al., 2000).
Informal Hospice Caregiving and Anxiety
It is well established in the literature that caring for a dying individual may result in significant stress and subsequently pose serious risks to one’s psychological health (Chentsova-Dutton et al., 2000; Given et al., 2004; Haley et al., 2002; Williams & McCorkle, 2011); however, relatively little research has examined anxiety as a distinct type of psychological distress experienced by informal caregivers of adults receiving hospice services. Of the small number of studies examining anxiety specifically, results have established that rates of anxiety are higher among hospice caregivers than demographically comparable non-caregivers (Chentsova-Dutton et al., 2000) and that psychosocial interventions, such as problem-solving therapy, hold promise in reducing caregiver anxiety (Demiris et al., 2010; Demiris et al., 2012).
An examination of the literature on caregiving and anxiety more broadly, however, yields a much larger body of research. For example, researchers have long established a connection between informal caregiving for dementia patients and anxiety, finding higher rates of anxiety to be associated with poor caregiver physical health and high perceived caregiving (Cooper, Katona, Orrell, & Livingston, 2008) and high levels of emotional exhaustion and depersonalization (Yilmaz, Turan, & Gundogar, 2009). Results of studies testing the impact of psychosocial interventions on those caring for a loved one with dementia have been labeled “promising,” yet the small number and diverse nature of these tested interventions preclude drawing meaningful conclusions from existing research (Schulz et al., 2002).
The cancer literature also sheds light on the connection between caregiving and anxiety. Here again, anxiety rates are found to be higher among informal caregivers than population norms, at least in the “late palliatve” phase of care (Grov, Dahl, Moum, & Fossa, 2005). In addition, in at least one study of breast cancer caregiving, informal caregivers were more likely to be anxious than the care recipients/patients themselves (Grunfeld et al., 2004), lending support to the assertion that caregiver distress warrants attention. Other research detected increases in caregiver anxiety as the care recipient/patient’s functional status declined (Dumont et al., 2006), underscoring the likelihood of caregiver anxiety as a pressing concern as end of life nears.
Purpose of the Study
The purpose of this study was to generate an in-depth understanding of the extent to which informal hospice caregivers experience symptoms of anxiety and to identify characteristics of caregivers who experience clinically significant (i.e., moderate or higher) levels of anxiety. Given the lack of research specifically investigating anxiety among informal hospice caregivers, we adopted an exploratory research approach, seeking to address the following research questions: 1) What is the prevalence of anxiety among informal hospice caregivers? 2) What are the characteristics of anxious informal hospice caregivers?
Methods
Data Sources
Researchers conducted a secondary analysis of data pooled from three separate original studies: two randomized controlled trials of psychosocial interventions for informal hospice caregivers (R01NRXXXXXX, AUTHOR, Principal Investigator; R01NRXXXXXX, AUTHOR, Principal Investigator) and one observational study of informal hospice caregivers’ stress and coping experiences (Hartford Geriatric Social Work Scholars Research Grant, AUTHOR, Principal Investigator). All original studies were approved by the Institutional Review Board of the respective researchers’ academic institutions prior to initiation. These pooled studies used similar protocols and instruments to capture a broad range of caregivers’ backgrounds, experiences, and health outcomes. Data drawn from the three projects were originally collected between 2010 and 2013 in geographically distinct areas of the United States including the Northwest, the Midwest, and the Southeast. To ensure that the interventions tested in two of the original studies did not impact the outcome of the analysis, researchers selected only baseline (pre-intervention) measures for this study.
Study Variables
Demographic characteristics
The following demographic characteristics were considered: age, gender, site of research participation (Northwest, Midwest, or Southeast), employment status (employed part- or full-time outside the home, not employed outside the home), and residence (co-resides with hospice patient, does not co-reside with hospice patient). Cases drawn from studies conducted in the Southeast and Northwest included data related to amount of caregiving (number of hours per week engaged in caregiving tasks), and duration of caregiving (number of weeks providing care).
Quality of life
Cases drawn from studies conducted in the Midwest and Northwest included data from the Caregiver Quality of Life Index-Revised (CQLI-R) (Courtney, Demiris, Oliver, & Porock, 2005). The CQLI-R consists of four single-item subscales that measure physical, emotional, social, and financial quality of life on a scale of 0-10, with higher scores indicating higher quality of life in each of the four domains. The CQLI-R’s satisfactory psychometrics have been established in previous research (Courtney et al., 2005). Cases drawn from the Southeast research site included data only on physical quality of life, measured using a single-item scale of 1 to 5, with higher scores indicating a higher physical quality of life. To allow for comparisons among research sites, physical quality of life scores from the Southeast site were doubled prior to analysis; because 0 was not a response option, the comparisons are approximate rather than exact.
Caregiver anxiety
Caregiver anxiety was measured with the Generalized Anxiety Disorder 7-item (GAD-7) scale (Spitzer, Kroenke, Williams, & Lowe, 2006), which measures the frequency with which respondents experience symptoms of anxiety such as restlessness, difficulty relaxing, and uncontrollable worrying. GAD-7 total scores range from 0 to 21, with higher scores indicating more anxiety. Total scores of 5, 10, and 15 represent thresholds for mild, moderate, and severe anxiety, respectively. Total scores of 10 or higher are generally considered clinically significant, signaling a need for additional evaluation and possible intervention (Spitzer et al., 2006). Previous studies have established that the internal consistency of the GAD-7 is excellent (Cronbach’s alpha = 0.92), and its test-retest reliability has been shown to be very good (intra-class correlation = 0.83) (Spitzer et al., 2006).
Data Analysis
Descriptive statistics for demographic and baseline self-rated health outcomes were used to describe informal hospice caregivers from each study site. Between-site comparisons of baseline covariates were conducted using one-way analysis of variance or t-tests for continuous variables and chi-square tests for categorical variables.
Logistic regression was used to model the associations between the covariates and caregiver anxiety. The primary analysis used covariates common to all sites (demographic characteristics, living with the patient, employment status, and physical quality of life). Supplemental analyses incorporated additional covariates (amount and duration of caregiving; social, emotional, and financial quality of life) available at specific site(s). All analyses were conducted using Stata 12.1 (StataCorp, College Station, TX).
Results
The original pooled sample size was 460 caregivers; however, the final analytic sample consisted of 433 caregivers after 27 caregivers with missing data were excluded. Caregivers in the analytic sample did not differ significantly from those in the dropped sample on anxiety and only differed on one covariate of interest – caregivers from the Southeast and Midwest had more missing data than those from the Northwest. A summary of demographic information about participant cases drawn from the original studies is provided in Table 1. Caregivers participating in the three original studies were predominately women (77.1%), Caucasian (91.5%), and were mostly either adult children (50.8%) or spouses (30.7%). Caregivers ranged in age from 19 to 96, with an average age of 60.8. Slightly over half the sample (53.8%) lived with the patient and 37% were employed either full or part-time. In general, background characteristics were similar among research sites except for employment; caregivers living in the Southeast (23.1%) were less likely to be employed than those in the Midwest (41%) and Northwest (45%) (p < .001).
Table 1.
Characteristics of Informal Hospice Caregivers
| Characteristic | Southeast (n = 134) |
Midwest (n = 139) |
Northwest (n = 160) |
Total (N = 433) |
|---|---|---|---|---|
| Age, mean (SD) | 61.8 (12.0) | 60.1 (13.1) | 60.6 (12.2) | 60.8 (12.4) |
| Female, % | 80.6 | 73.4 | 77.5 | 77.1 |
| White, % | 90.3 | 94.2 | 90.0 | 91.5 |
| Relationship to patient, % | ||||
| Adult Child | 46.3 | 52.5 | 53.1 | 50.8 |
| Spouse or Partner | 33.6 | 24.5 | 33.8 | 30.7 |
| Other | 20.2 | 23.0 | 13.1 | 18.5 |
| Lives with Patient, % | 62.7 | 46.8 | 52.5 | 53.8 |
| Employeda, % | 23.1 | 41.0 | 45.0 | 37.0 |
| Caregiving > 20 hr/wk, % | 74.6 | – | 56.3 | |
| Caregiving > 1 yr, % | 57.9 | – | 70.6 | |
| Quality of Life, mean (SD)b | ||||
| Physical | 6.9 (2.1) | 6.9 (2.3) | 7.1 (2.2) | 7.0 (2.2) |
| Social | – | 6.9 (2.8) | 8.0 (2.3) | |
| Emotional | – | 7.2 (2.2) | 7.3 (2.2) | |
| Financial | – | 6.4 (3.1) | 7.0 (2.6) |
Note. Measures of amount of care provided, duration of caregiving, and quality of life were not collected at all sites. All site comparisons p > .05 except for employed (p < .001), caregiving > 20 hr/wk (p = .001), caregiving > 1 yr (p = .023), and social quality of life (p < .001).
Employed full or part-time vs. not employed.
Higher scores indicate better quality of life.
Anxiety Prevalence among Informal Hospice Caregivers
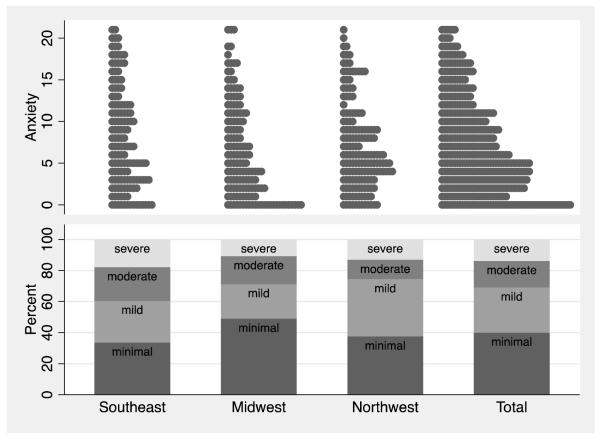
Figure 1 illustrates the distribution of caregiver anxiety and severity across the sites and for the pooled sample. Although the distributions of anxiety scores are characterized by right skewed distributions with a modal score of 0, categorization of severity indicates that 31% of all caregivers reported a moderate or higher level of anxiety. GAD-7 scores ranged from 0 to 21, with a mean score of 7.2 and a median score of 6 (Table 2). The percentage of caregivers experiencing anxiety (GAD-7 ≥ 10) ranged from 25.6% in the Northwest, to 28.8% in the Midwest, to 39.5% in the Southeast [χ2(3, N = 433) = 7.07, p = .029].
Figure 1.
Distribution of Informal Hospice Caregiver Anxiety and Severity
Table 2.
Informal Hospice Caregiver Anxiety and Severity (GAD-7)
| Southeast (n = 134) |
Midwest (n = 139) |
Northwest (n = 160) |
Total (N = 433) |
|
|---|---|---|---|---|
| Anxiety Score, mean (SD) | 8.1 (5.9) | 6.4 (5.7) | 7.1 (5.2) | 7.2 (5.6) |
| Anxiety Score, median (IRQ) | 7 (3–12) | 5 (2–10) | 6 (3–10) | 6 (3–11) |
| Anxiety Severity, % | ||||
| Minimal, (0-4) | 33.6 | 48.9 | 37.5 | 40.0 |
| Mild, (5-9) | 26.9 | 22.3 | 36.9 | 29.1 |
| Moderate, (10-14) | 21.6 | 18.0 | 12.5 | 17.1 |
| Severe, (15-21) | 17.9 | 10.8 | 13.1 | 13.9 |
Note. GAD-7 = Generalized Anxiety Disorder 7-item scale. IRQ = Interquartile range. Both score (p = .037) and severity (p = .012) differed by site.
Characteristics of Anxious Informal Hospice Caregivers
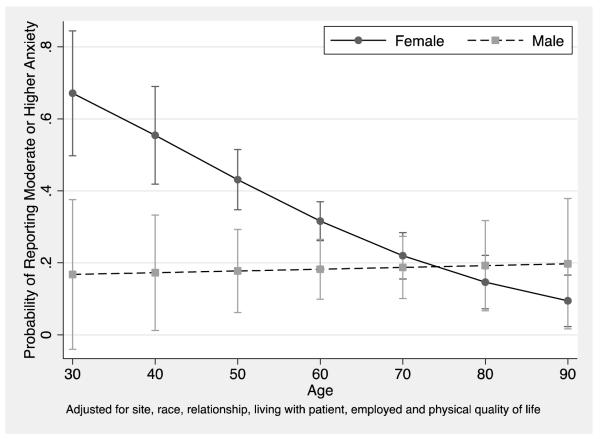
The differential association of caregiver characteristics with anxiety (GAD-7 ≥ 10) was examined using a multivariate logistic regression model (Table 3). According to the model, after adjusting for other covariates, caregivers in the Northwest were less likely to be anxious than those in the Southeast (odds ratio [OR] = 0.54, 95% confidence interval [95% CI] = 0.31 – 0.93) and employed caregivers were less likely to be anxious than unemployed caregivers (OR = 0.56, 95% CI = 0.33, 0.96). The model further indicated that the probability of being anxious decreased with increasing physical quality of life (OR = 0.77, 95% CI = 0.69, 0.85). Younger female caregivers were more likely to be anxious than male caregivers and older females (OR = 0.95, CI = 0.91, 0.99). The relationship between gender and anxiety is contingent on the age of the caregiver (Figure 2). Females have a significantly higher probability of being anxious than males until about the age of 60 years.
Table 3.
Logistic Regression Predicting Anxiety among Informal Hospice Caregivers
| Variable | Odds Ratio |
95% CI for Odds Ratio |
p value |
|---|---|---|---|
| Study Site a | |||
| Northwest | 0.54 | 0.31–0.93 | .027 |
| Midwest | 0.62 | 0.36–.09 | .099 |
| Age b | 1.00 | 0.96 – 1.04 | .872 |
| Female | 1.97 | 1.08 – 3.58 | .026 |
| White | 1.31 | 0.58 – 3.00 | .516 |
| Relationship to Patient c | |||
| Adult child | 1.14 | 0.61 – 2.13 | .675 |
| Other | 0.57 | 0.26 – 1.25 | .161 |
| Lives with Patient | 0.72 | 0.44 – 1.18 | .194 |
| Employed | 0.56 | 0.33 – 0.96 | .035 |
| Physical Quality of Life | 0.77 | 0.69 – 0.85 | <.001 |
| Age × Female | 0.95 | 0.91 – 0.99 | .018 |
| Intercept | 2.47 | 0.66 – 9.20 | .653 |
| Model fit statistics | |||
| Area under ROC curve | 0.73 | ||
| Hosmer-Lemeshow χ2(8) | 5.59 | 0.693 |
Note. CI = Confidence Interval
Referent category = Southeast.
Age was centered at the mean.
Referent category = Spouse or partner.
Figure 2.
Association of Age with Experiencing Anxiety by Gender
Supplemental analyses
A series of supplemental analyses were conducted to examine the association of covariates (amount and duration of caregiving; social, emotional, and financial quality of life) with caregiver anxiety that were only available at specific site(s). These covariates were added to the basic model previously examined in the pooled sample.
Amount and duration of caregiving (Southeast and Northwest)
Due to sparse cells in contingency tables with anxiety severity, these variables were re-coded as dichotomous variables indicating greater than 20 hours per week caregiving and caregiving for over one year, respectively. The overall pattern of results was similar to that for the pooled sample. However, neither amount (OR = 1.44, 95% CI = 0.71, 2.89) nor duration of caregiving (OR = 0.88, 95% CI = 0.48, 1.61) had a significant association with being anxious.
Quality of life (Midwest and Northwest)
The Midwest and Northwest sites collected data on social, emotional, and financial quality of life domains in addition to physical quality of life. The inclusion of these additional domains was indicated by the Likelihood ratio test (χ2(3) = 41.01, p < .0001). Emotional quality of life was the only domain that was statistically significant (OR = 0.68, 95% CI = 0.58, 0.81), and the inclusion of all four of the quality of life domains rendered insignificant the previously noted association between physical quality of life and anxiety severity (OR = 0.95, 95% CI = 0.82, 1.11).
Discussion
Of the 433 caregivers represented in this study, nearly one-third (31%) reported moderate or higher levels of anxiety. Caregivers living in the Southeast, who were unemployed while caregiving, who reported poor physical quality of life, or who were both young and female were particularly likely to experience anxiety. Supplemental analyses based on smaller samples indicated that neither amount nor duration of caregiving was significantly associated with anxiety. Similarly, no statistically significant relationship was identified between anxiety and financial or social quality of life. While a significant relationship was detected between anxiety and emotional quality of life, this finding was expected, as the presence of anxiety would almost necessarily compromise one’s overall emotional quality of life. Interestingly, when all four quality of life domains (financial, physical, social, and emotional) were included in the model in the supplemental analyses, the significant relationship between physical quality of life and severity of anxiety disappeared. While this may be due to the smaller and more geographically restricted sample included in the supplemental analyses, it may also suggest that caregivers’ emotional responses to having poor physical health are more important than the mere reality of poor physical health, at least as it pertains to related experiences of anxiety.
It is challenging to compare results of the present study with previous research, given the extreme variability in the anxiety literature with regard to instrumentation, operational definitions of anxiety and specific disorders, and additional variables examined (Bryant, Jackson, & Ames, 2008); however, it is possible to arrive at some general conclusions. In terms of prevalence, the 31% of informal hospice caregivers who reported moderate or greater levels of anxiety in the present study is higher than nearly all published reports of anxiety prevalence in the general population (Weisberg, 2009); however, given that the average age of participants in the present study (60.8 years) is significantly higher than that of the general population, non-caregiving older adults likely represent a more useful comparison group than adults in general. Among community-dwelling older adults, estimates of anxiety prevalence range from 1.2% to 15% - less than half the prevalence identified in the present study (Bryant et al., 2008). This difference between non-caregiving controls and those involved in actively caring for a family member or friend is consistent with earlier research on hospice caregivers (Chentsova-Dutton et al., 2000) and makes intuitive sense, given the number of stressors experienced when caring for a dying significant other.
Caregiver characteristics, particularly gender and age, have been studied fairly extensively with regard to their impact on psychological distress and, to a lesser extent, anxiety specifically. The finding that women experience anxiety at higher rates than men (Pigott, 2003) - but that this difference lessens with increasing age (Krasucki, Howard, & Mann, 1998) - is consistent with previous research of the general adult population, although researchers are still speculating about the complex biological, psychological, and social factors that give rise to this gender/age interaction. Additional research is also needed to explain the impact of differences in employment on anxiety; it is reasonable to conclude that variables not considered in this exploratory study (e.g., financial remuneration, satisfaction with employment status and conditions, degree of social support in the workplace) play a role. Finally, while the inverse relationship between physical health and anxiety identified in this study is consistent with previous findings (e.g., Sareen, Cox, Clara, & Asmundson, 2005), future research of a longitudinal nature will help determine whether pre-existing physical health problems are risk factors for negative outcomes in caregiving, if caregiving demands themselves lead to poor physical health, or if both are true to varying degrees for different individuals.
While anxiety is a reality for a noteworthy number of informal hospice caregivers, no concerted effort exists to even screen for, much less treat, anxiety in this population. This is the case despite a plethora of available tools such as the GAD-7, which is available online and free of charge. Further, a number of psychosocial interventions exist to address anxiety, many of which are supported by robust bodies of research. Of these interventions, very few have been tested in hospice settings; however, problem-solving therapy (Demiris et al., 2010; Demiris et al., 2012) and cognitive schema development (Lindstrom & Mazurek Melnyk, 2013) have both shown promise in early testing. The results of this study provide strong support for additional development of tools to both screen and respond to symptoms of anxiety experienced by informal hospice caregivers.
Limitations
A number of study limitations warrant attention. First, although the study sample included participants from geographically diverse areas of the United States, findings cannot be assumed to be generalizable to all informal hospice caregivers. Moreover, since participants were not randomly selected from their respective geographic regions, we cannot conclude that differences noted among research sites are attributable to geography. In addition, conclusions drawn from findings regarding the relationship between physical quality of life and caregiver anxiety must be regarded as approximate rather than exact, given differences in instrumentation among the three research sites. Finally, some measures included in the supplemental analyses, specifically amount and duration of caregiving, must be regarded as estimates rather than precise figures, as caregivers may have struggled to identify the exact number of hours spent engaged in caregiving tasks and/or the moment at which they assumed a caregiving role in addition to their pre-existing relationship (e.g., spouse/partner, adult child) with the hospice patient. Finally, the cross-sectional and exploratory nature of this study limits its ability to identify causal factors or to inform extant caregiving theories. Future research, focused on a more restricted set of variables over time, is recommended to further advance knowledge in this area.
Acknowledgements
This work was supported by the John A. Hartford Social Work Scholars Program (PI: AUTHOR); the National Institute of Nursing Research Award Number R01NRXXXXXX (PI: AUTHOR) registered as clinical trial record NCTXXXXXXXX; and the National Institute of Nursing Research Award Number R01NRXXXXXX (PI: AUTHOR) registered as clinical trial record NCTXXXXXXXX. The content is solely the responsibility of the authors and does not necessarily represent the official views of the John A. Hartford Foundation, the National Institute of Nursing Research, or the National Institutes of Health.
References
- Bryant C, Jackson H, Ames D. The prevalence of anxiety in older adults: Methodological issues and a review of the literature. Journal of Affective Disorders. 2008;109(3):233–250. doi: 10.1016/j.jad.2007.11.008. doi: 10.1016/j.jad.2007.11.008. [DOI] [PubMed] [Google Scholar]
- Chentsova-Dutton Y, Shucter S, Hutchin S, Strause L, Burns K, Zisook S. The psychological and physical health of hospice caregivers. Annals of Clinical Psychiatry. 2000;12(1):19–27. doi: 10.1023/a:1009070826012. doi: 10.3109/10401230009147083. [DOI] [PubMed] [Google Scholar]
- Cooper C, Katona C, Orrell M, Livingston G. Coping strategies, anxiety and depression in caregivers of people with Alzheimer’s disease. International Journal of Geriatric Psychiatry. 2008;23(9):929–936. doi: 10.1002/gps.2007. doi: 10.1002/gps.2007. [DOI] [PubMed] [Google Scholar]
- Courtney K, Demiris G, Oliver DP, Porock D. Conversion of the Caregiver Quality of Life Index to an interview instrument. European Journal of Cancer Care (English Language Edition) 2005;14(5):463–464. doi: 10.1111/j.1365-2354.2005.00612.x. doi: 10.1111/j.1365-2354.2005.00612.x. [DOI] [PubMed] [Google Scholar]
- Demiris G, Oliver DP, Washington K, Fruehling LT, Haggarty-Robbins D, Doorenbos A, Berry D. A Problem Solving Intervention for hospice caregivers: A pilot study. Journal of Palliative Medicine. 2010;13(8):1005–1011. doi: 10.1089/jpm.2010.0022. doi: 10.1089/jpm.2010.0022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demiris G, Parker Oliver D, Wittenberg-Lyles E, Washington K, Doorenbos A, Rue T, Berry D. A noninferiority trial of a problem-solving intervention for hospice caregivers: In person versus videophone. Journal of Palliative Medicine. 2012;15(6):653–660. doi: 10.1089/jpm.2011.0488. doi: 10.1089/jpm.2011.0488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dumont S, Turgeon J, Allard P, Gagnon P, Charbonneau C, Vezina L. Caring for a loved one with advanced cancer: Determinants of psychological distress in family caregivers. Journal of Palliative Medicine. 2006;9(4):912–921. doi: 10.1089/jpm.2006.9.912. doi: 10.1089/jpm.2006.9.912. [DOI] [PubMed] [Google Scholar]
- Funk L, Stajduhar K, Toye C, Aoun S, Grande G, Todd C. Part 2: Home-based family caregiving at the end of life: A comprehensive review of published qualitative research (1998-2008) Palliative Medicine. 2010;24(6):594–607. doi: 10.1177/0269216310371411. doi: 10.1177/0269216310371411. [DOI] [PubMed] [Google Scholar]
- Given B, Wyatt G, Given C, Sherwood P, Gift A, DeVoss D, Rahbar M. Burden and depression among caregivers of patients with cancer at the end of life. Oncology Nursing Forum. 2004;31(6):1105–1117. doi: 10.1188/04.ONF.1105-1117. doi: 10.1188/04.onf.1105-1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grov EK, Dahl AA, Moum T, Fossa SD. Anxiety, depression, and quality of life in caregivers of patients with cancer in late palliative phase. Annals of Oncology. 2005;16(7):1185–1191. doi: 10.1093/annonc/mdi210. [DOI] [PubMed] [Google Scholar]
- Grunfeld E, Coyle D, Whelan T, Clinch J, Reyno L, Earle CC, Glossop R. Family caregiver burden: Results of a longitudinal study of breast cancer patients and their principal caregivers. CMAJ: Canadian Medical Association Journal. 2004;170(12):1795–1801. doi: 10.1503/cmaj.1031205. doi: http://dx.doi.org/10.1503/cmaj.1031205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haley WE, Allen RS, Reynolds SA, Chen H, Burton A, Gallagher-Thompson D. Family issues in end-of-life decision making and end-of-life care. American Behavioral Scientist. 2002;46(2):284–298. doi: 10.1177/000276402236680. [Google Scholar]
- Krasucki C, Howard R, Mann A. The relationship between anxiety disorders and age. International Journal of Geriatric Psychiatry. 1998;13(2):79–99. doi: 10.1002/(sici)1099-1166(199802)13:2<79::aid-gps739>3.0.co;2-g. doi: 10.1002/(SICI)1099-1166(199802)13:2<79::AID-GPS739>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- Lindstrom KB, Mazurek Melnyk B. Feasibility and preliminary effects of an intervention targeting schema development for caregivers of newly admitted hospice patients. Journal of Palliative Medicine. 2013;16(6):680–685. doi: 10.1089/jpm.2012.0198. doi: 10.1089/jpm.2012.0198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMillan SC. Interventions to facilitate family caregiving at the end of life. Journal of Palliative Medicine. 2005;8(Suppl 1):S132–139. doi: 10.1089/jpm.2005.8.s-132. doi: 10.1089/jpm.2005.8.s-132. [DOI] [PubMed] [Google Scholar]
- National Hospice and Palliative Care Organization End-of-life caregiving. 2005 http://www.caringinfo.org/userfiles/File/EOL_Caregiver_booklet.pdf.
- National Hospice and Palliative Care Organization NHPCO Facts and Figures: Hospice Care in America. 2012 http://www.nhpco.org/sites/default/files/public/Statistics_Research/2012_Facts_Figures.pdf.
- Pigott TA. Anxiety disorders in women. Psychiatric Clinics of North America. 2003;26(3):621–672. vi–vii. doi: 10.1016/s0193-953x(03)00040-6. [DOI] [PubMed] [Google Scholar]
- Sareen J, Cox BJ, Clara I, Asmundson GJ. The relationship between anxiety disorders and physical disorders in the U.S. National Comorbidity Survey. Depression and Anxiety. 2005;21(4):193–202. doi: 10.1002/da.20072. doi: 10.1002/da.20072. [DOI] [PubMed] [Google Scholar]
- Schulz R, O’Brien A, Czaja S, Ory M, Norris R, Martire LM, Stevens A. Dementia caregiver intervention research: In search of clinical significance. Gerontologist. 2002;42(5):589–602. doi: 10.1093/geront/42.5.589. doi: 10.1093/geront/42.5.589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing Generalized Anxiety Disorder: The GAD-7. Archives of Internal Medicine. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Waldrop DP, Meeker MA. Hospice decision making: Diagnosis makes a difference. Gerontologist. 2012;52(5):686–697. doi: 10.1093/geront/gnr160. doi: 10.1093/geront/gnr160. [DOI] [PubMed] [Google Scholar]
- Weisberg RB. Overview of Generalized Anxiety Disorder: Epidemiology, presentation, and course. Journal of Clinical Psychiatry. 2009;70(Suppl 2):4–9. [PubMed] [Google Scholar]
- Williams AL, McCorkle R. Cancer family caregivers during the palliative, hospice, and bereavement phases: A review of the descriptive psychosocial literature. Palliat Support Care. 2011;9(3):315–325. doi: 10.1017/S1478951511000265. doi: 10.1017/s1478951511000265. [DOI] [PubMed] [Google Scholar]
- Wittenberg-Lyles E, Demiris G, Parker Oliver D, Washington K, Burt S, Shaunfield S. Stress variances among informal hospice caregivers. Qualitative Health Research. 2012;22(8):1114–1125. doi: 10.1177/1049732312448543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yilmaz A, Turan E, Gundogar D. Predictors of burnout in the family caregivers of Alzheimer’s disease: Evidence from Turkey. Australas J Ageing. 2009;28(1):16–21. doi: 10.1111/j.1741-6612.2008.00319.x. doi: 10.1111/j.1741-6612.2008.00319.x. [DOI] [PubMed] [Google Scholar]