Abstract
As patients with carcinoma of the esophagus live longer, complications associated with the use of a gastric conduit are increasing. Ulcers form in the gastric conduit in 6.6% to 19.4% of patients. There are a few reports of perforation of a gastric conduit in the English literature. Almost all of these were associated with serious complications. We report a patient who developed a tension pneumothorax consequent to spontaneous perforation of an ulcer in the gastric conduit 7 years after the index surgery in a patient with carcinoma of the gastroesophageal junction. He responded well to conservative management. Complications related to a gastric conduit can be because of multiple factors. Periodic endoscopic surveillance of gastric conduits should be considered as these are at a higher risk of ulcer formation than a normal stomach. Long term treatment with proton pump inhibitors may decrease complications. There are no guidelines for the treatment of a perforated gastric conduit ulcer and the management should be individualized.
Keywords: Gastric conduit, Ulcer formation, Perforation, Carcinoma of the esophagus, Proton pump inhibitors
Core tip: We report a patient with a spontaneous perforation of an ulcer in the gastric conduit of a patient who had surgery for carcinoma of the gastroesophageal junction. He responded to conservative management with continuous decompression of the conduit with Ryle’s tube aspiration, proton pump inhibitors and enteral nutrition through a feeding jejunostomy for 4 wk. Periodic endoscopic surveillance should be considered as gastric conduits are at a higher risk of ulcer formation than a normal stomach and management of a perforated gastric conduit ulcer should be individualized.
INTRODUCTION
The stomach is preferred as the conduit after esophageal resection. Complications following gastric conduits are being reported more often as patients with carcinoma of the esophagus are living longer after resection. The incidence of an ulcer occurring in a gastric conduit is reported to be between 6.6% and 19.4%[1,2]. Perforation of a gastric conduit ulcer, although rare, may be catastrophic. The ulceration in a gastric conduit is often due to tumor recurrence. However, it may be due to other causes too. We report a patient with spontaneous perforation of a gastric conduit ulcer into the right pleural cavity that was successfully managed conservatively.
CASE REPORT
Figure 1.
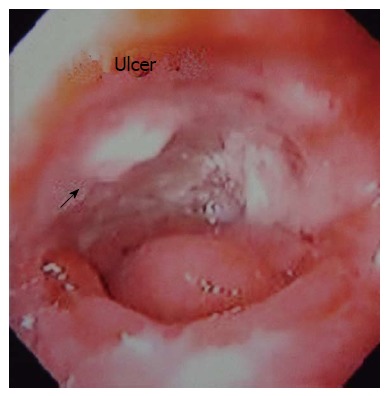
Endoscopic view of gastric conduit ulcer.
Figure 2.
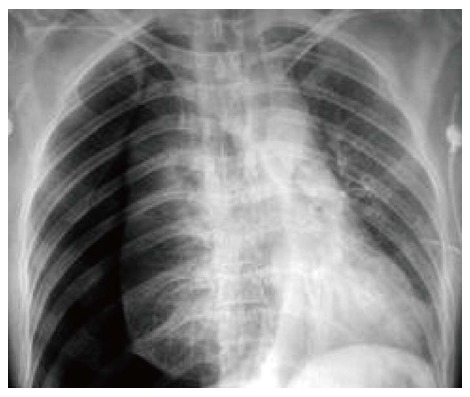
Chest X-ray showing right sided tension pneumothorax with mediastinal shift.
Figure 3.
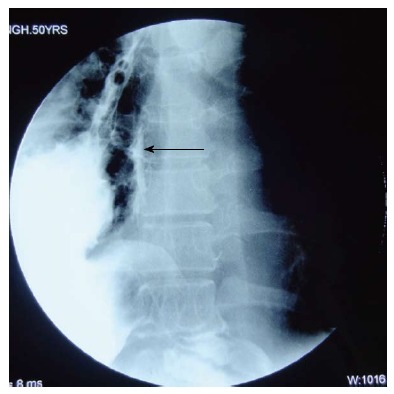
Oral Gastrografin study showing leak of contrast from the medial aspect of upper part of the conduit (arrow).
Figure 4.
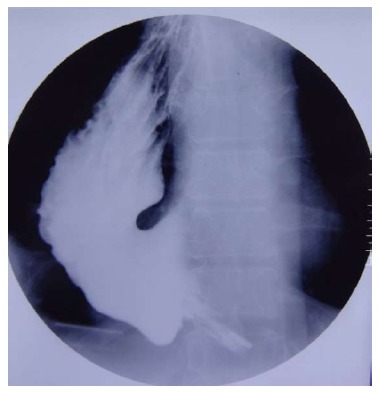
Repeat study after 4 wk shows no evidence of contrast leak.
DISCUSSION
Increasing use of the stomach as a conduit has led to increasing reports of peptic ulcers in the conduit. In a prospective study of annual endoscopic evaluations in 114 patients who underwent gastric tube reconstruction after esophagectomy, 47% of patients had secondary gastric tube diseases, including gastritis [35.1% (40/114)], benign gastric tumors [10.5% (12/114)], gastric ulcers [6.1% (7/114)] and gastric adenocarcinoma [3.5% (4/114)][1]. Gastric tubes are reported to be at a higher risk of developing an ulcer than the normal stomach. The cause of a gastric conduit ulcer remains controversial. Several mechanisms have been postulated for the formation of gastric conduit ulcers, including normalization of the intraluminal pH profile over time, H. pylori infection (especially in patients with a history of peptic ulcer before surgery), delayed gastric emptying as a result of vagal denervation, bile reflux, ischemia due to mobilization of the gastric conduit, radiation, use of non-absorbable sutures and intake of non-steroidal anti-inflammatory drugs (NSAIDs), aspirin or steroids[3]. Most ulcers develop within 20 cm of the esophagogastric anastomosis, as in our patient, because the microcirculation is most disturbed in the upper part of the conduit[2]. The time for development of these ulcers has varied widely, from one month to as long as 150 mo.
Peptic ulcer of the gastric conduit can present with anemia, retrosternal or epigastric pain, fullness after eating or dysphagia[3]. It could be asymptomatic and vagotomy may be one of the reasons for the absence of pain[4]. A gastric conduit ulcer often causes serious complications, such as bleeding and perforation[5]. It may penetrate into any adjacent organ (left ventricular or atrial wall, thoracic aorta and other major vessels) or cavity, including the right pleural cavity, bronchi and pericardial cavity[5].
Only a few cases of gastric conduit perforation have been reported in the English literature and almost all of them had serious complications. More than half the patients were treated conservatively and all of them died[5]. All patients whose conduit ulcer perforated into the tracheobronchial tree or cardiovascular system died. Only patients with perforation into the sternum and thoracic cavity survived. Patients who had a gastric conduit perforation in the thoracic cavity underwent either primary closure of the perforated ulcer or resection of the ulcer followed by an interrupted closure buttressed with a pleural patch. Both these procedures are associated with high leak rates and mortality. In our case, the patient responded to conservative treatment, although we cannot recommend this for all cases.
Endoscopic surveillance should be done at least once every 6 mo as gastric conduits are at a higher risk of ulcer formation than a normal stomach and many such ulcers tend to be asymptomatic. Successful healing of a gastric ulcer by PPIs has been reported[1]. This could prevent potentially lethal complications associated with it.
While complications in the gastric conduit are being reported increasingly, there are no guidelines for the treatment of a perforated gastric conduit ulcer. These patients are usually sick and may not tolerate major surgery. The conservative management protocol cited above resulted in a good outcome in our case, showing that surgery is not always required and the management should be individualized. Avoidance of analgesics and periodic surveillance of the conduit may prevent complications.
COMMENTS
Case characteristics
The patient presented with sudden onset chest pain and difficulty breathing.
Clinical diagnosis
On clinical examination, decreased breath sounds in the right hemithorax with hyper resonant note on percussion.
Differential diagnosis
Differential diagnoses were pneumothorax secondary to spontaneous rupture of pulmonary bullae, acute myocardial infarction and recurrence of disease.
Laboratory diagnosis
Laboratory investigations were inconclusive.
Imaging diagnosis
On imaging, chest X-ray revealed right sided tension pneumothorax with mediastinal shift to left, gastric contents on insertion of intercostal drainage tube and oral Gastrografin study showed leak from the gastric conduit.
Pathological diagnosis
Previous endoscopy showed a large ulcer in the proximal part of gastric conduit, biopsy was consistent with peptic ulcer and also ruled out any recurrence.
Treatment
He was treated conservatively with continuous decompression of the conduit through Ryle’s tube aspiration, proton pump inhibitors and enteral nutrition through feeding jejunostomy for 4 wk.
Experiences and lessons
The possibility that ulceration in the gastric conduit may be due to causes other than tumor recurrence deserves greater recognition. Periodic endoscopic surveillance should be considered as gastric conduits are at a higher risk of ulcer formation than a normal stomach.
Peer review
This is a rare morbid complication of gastric conduit which responded to conservative management. However, a firm conclusion cannot be drawn on the management guidelines of perforated gastric conduit ulcer and treatment should be individualized.
Footnotes
P- Reviewer: Abd Ellatif ME, Boyacioglu AS, Gonzalez AM, Marangoni G S- Editor: Ma YJ L- Editor: Roemmele A E- Editor: Lu YJ
References
- 1.Motoyama S, Saito R, Kitamura M, Suzuki H, Nakamura M, Okuyama M, Imano H, Inoue Y, Ogawa J. Prospective endoscopic follow-up results of reconstructed gastric tube. Hepatogastroenterology. 2003;50:666–669. [PubMed] [Google Scholar]
- 2.Suzuki H, Saito R, Sasaki S, Okuyama M. Analysis of the cases with peptic ulcer of gastric tube after esophageal replacement for esophageal cancer. Rinsho. 1999;54:1075–1079. [Google Scholar]
- 3.Piessen G, Lamblin A, Triboulet JP, Mariette C. Peptic ulcer of the gastric tube after esophagectomy for cancer: clinical implications. Dis Esophagus. 2007;20:542–545. doi: 10.1111/j.1442-2050.2007.00706.x. [DOI] [PubMed] [Google Scholar]
- 4.Texter EC. Ulcer pain mechanisms. The clinical features of active peptic ulcer disease and implications for therapy. Scand J Gastroenterol Suppl. 1987;134:1–20. doi: 10.3109/00365528709090135. [DOI] [PubMed] [Google Scholar]
- 5.Ubukata H, Nakachi T, Tabuchi T, Nagata H, Takemura A, Shimazaki J, Konishi S, Tabuchi T. Gastric tube perforation after esophagectomy for esophageal cancer. Surg Today. 2011;41:612–619. doi: 10.1007/s00595-010-4476-9. [DOI] [PubMed] [Google Scholar]


