Abstract
Nowadays, fracture surgery represents a big part of the orthopedic surgeon workload, and usually has associated major clinical and social cost implications. These fractures have several complications. Some of these are medical, and other related to the surgical treatment itself. Medical complications may affect around 20% of patients with hip fracture. Cognitive and neurological alterations, cardiopulmonary affections (alone or combined), venous thromboembolism, gastrointestinal tract bleeding, urinary tract complications, perioperative anemia, electrolytic and metabolic disorders, and pressure scars are the most important medical complications after hip surgery in terms of frequency, increase of length of stay and perioperative mortality. Complications arising from hip fracture surgery are fairly common, and vary depending on whether the fracture is intracapsular or extracapsular. The main problems in intracapsular fractures are biological: vascularization of the femoral head, and lack of periosteum -a major contributor to fracture healing- in the femoral neck. In extracapsular fractures, by contrast, the problem is mechanical, and relates to load-bearing. Early surgical fixation, the role of anti-thromboembolic and anti-infective prophylaxis, good pain control at the perioperative, detection and management of delirium, correct urinary tract management, avoidance of malnutrition, vitamin D supplementation, osteoporosis treatment and advancement of early mobilization to improve functional recovery and falls prevention are basic recommendations for an optimal maintenance of hip fractured patients.
Keywords: Hip fracture, Complications, Morbidity, Mortality, Anesthesia
Core tip: Over 90% of hip fracture patients are older than 65-year-old and have preexisting medical comorbidities. Both factors have an important influence in its prognosis and treatment. Even with optimal care, elderly trauma patients suffer a higher morbidity and mortality rate when compared with the general population, and often demand for expensive hospital aftercare. Because of that, surgical treatment of hip fracture in these patients has exceptional clinical challenges, and needs strategies to optimize patient care. Acute orthogeriatric units, with medical co-management of these patients, offer the best chance for a successful outcome.
COMPLICATIONS OF HIP FRACTURES
Overall importance
Nowadays, hip fracture surgery represents a large quota of the orthopedic surgeon activity, and normally has associated major clinical and social cost implications[1]. Though hip fracture incidence has declined in many countries during the last decade, it still represents around 1/4 of the geriatric fractures that require hospital admission, and in spite of the enhancements in both surgical and medical services, its morbidity and mortality remains elevated[2]. Over 90% of hip fracture patients are older than 65 years old and have preexisting medical comorbidities. Both factors have an important influence in its prognosis and treatment[3]. Even with optimal care, elderly trauma patients suffer a higher morbidity and mortality rate when compared with the general population, and often demand for expensive hospital aftercare. Because of that, surgical treatment of hip fracture in these patients has exceptional clinical challenges, and needs strategies to optimize patient care. Acute orthogeriatric units, with a medical co-management of these patients, offer the best chance for a successful outcome[4-6], with some studies demonstrating a decrease in postoperative complications and mortality[7-9]. Early surgical fixation, the role of anti-thromboembolic and anti-infective prophylaxis, good pain control at the perioperative, detection and management of delirium, correct urinary tract management, avoidance of malnutrition, vitamin D supplementation, osteoporosis treatment and promotion of early mobilization to improve functional recovery and falls prevention are basic recommendations for an optimal care of hip fractured patients.
Medical complications of hip fractures
Though a retrospective cohort study has reported that most patients have no medical problems after hip fracture repair[10], postoperative complications of this procedure are still relevant, and may affect around 20% of patients with hip fracture[11]. Cognitive and neurological alterations, cardiopulmonary affections (alone or combined), venous thromboembolism, gastrointestinal tract bleeding, urinary tract complications, perioperative anemia, electrolytic and metabolic disorders, and pressure scars are the most important medical complications after hip surgery in terms of frequency, increase of length of stay and perioperative mortality[6,12] (Table 1).
Table 1.
Medical complications after hip fracture surgery
| Medical complications | Perioperative incidence | Intervention/recommendation1 | |
| Cognitive and neurological | Cognitive alterations | 10% | Preventive interventions in high-risk patients |
| Postoperative delirium | 13.5%-33% | Preventive role of antipsychotics (haloperidol) | |
| Cardiac and vascular | Arrhythmia | Evaluation and care of patients with previous heart affectation | |
| Heart failure/Myocardial ischemia | 35%-42% | Restoration of fluid status to euvolemic. Beta-blockers if necessary | |
| DVT/PE | 27%/1.4%-7.5% | Thromboembolism prophylaxis | |
| Early mobilization | |||
| Pulmonary | PPCs (exacerbation of chronic lung disease, atelectasis, respiratory failure, PE, ARDS) | 4% | Evaluation and care of patients with previous lung disease |
| Adequate postoperative fluid balance and pain control | |||
| Hospital-acquired pneumonia | 7% | Thromboembolism prophylaxis | |
| Timely diagnosis, adequate antibiotic treatment and accurate monitoring | |||
| Gastrointestinal | PGICs (dyspepsia, abdominal distension, reflexes ileum and constipation) | 5% | Adequate postoperative fluid, diet, pain and medication management |
| Gastrointestinal postoperative stress ulcer/ gastrointestinal bleeding | 1.9% | Gastrointestinal bleeding prevention with pump inhibitors | |
| Urinary tract | Urinary retention Urinary tract infections | 12%-61% | Urinary catheters should be taken out as soon as possible, preferably within 24 h after insertion |
| Timely diagnosis and adequate antibiotic treatment | |||
| Preventive identification of pre, peri or postoperative medical or surgical risk factors | |||
| AKI (prerenal, renal or postrenal) | 11% | Timely diagnosis, adequate treatment and accurate monitoring | |
| Hematologic | Anemia | 24%-44% | Preventive identification of pre, peri or postoperative medical or surgical risk factors |
| Correct hemoglobin level to ≥ 10 g/dL before surgery | |||
| In anticoagulated patients, correct international normalized ratio to ≤ 1.5 preoperatively | |||
| Timely diagnosis, adequate treatment and accurate monitoring | |||
| Endocrino-metabolic | Protein-caloric malnutrition | 20%-70% | Nutritional supplements in peroperative period |
| Diabetes | 17% | Maintain glucose levels between 100 and 180 mg/dL | |
| Vitamin D insufficiency-deficiency | Vitamin D supplementation | ||
| Other | Pressure scars | 7%-9% | Early surgery fixation (within 24-48 h in stable patients) |
| Alternating pressure mattresses, pressure-relieving beds and equipment, aggressive skin care and proper nutrition, prevention-focused nursing | |||
DVT/PE: Deep vein thrombosis/pulmonary embolism; PPCs: Postoperative pulmonary complications; PGICs: Postoperative gastrointestinal complications; AKI: Acute kidney injuries.
Each patient needs a preoperative functional assessment, joint orthopedic-geriatric care is of benefit, reducing inpatient complications, length of stay and mortality.
The American Society of Anesthesiologists (ASA) classification can be a useful risk-stratification system for aged patients who have a hip fracture. In a retrospective study, medical complications were more usual in patients in ASA class 3 and 4 (P ≤ 0.001) than those in ASA class 2, having respectively 3.78 and 7.39 times greater probability of suffering complications of this type[13]. With a similar clinical usefulness, a recent prospective study has demonstrated that advanced age (OR = 1.09), poor Barthel index (OR = 2.21) and low hemoglobin at admission (OR = 0.76) are factors associated with the development of medical inpatient complications[12].
Cognitive and neurological complications
Cognitive complications appear in approximately 10% of patients after hip fracture surgery, being more common in elderly (> 65 years) than younger patients. Most of them suffer mild problems after surgery (inability to concentrate, write, read a book, etc.) but are able to overcome activities of daily living[14].
The physiopathology of postoperative cognitive problems has not been yet clearly elucidated. Probably, its responsible mechanisms are heterogeneous and multifactorial, and may be related to preoperative health status, level of cognition (cognitive reserve), the neurotoxic effects of anesthetic agents and perioperative events related to the surgery itself[15]. In this sense, the use of acrylic cement for prosthetic implantation can cause an inflammatory response that may possibly be associated with the occurrence of postoperative cognitive complications[16]. Upcoming research must be focused on actions to prevent and treat postoperative cognitive complications in patients at high-risk[14].
Postoperative delirium in patients with hip fracture appears normally after surgery, and affects 13.5% to 33% of these patients[17]. It has a variable presentation, and patients may reveal hyperactive, hypoactive, or mixed cognitive and motor statuses. While hyperactive patients present augmented psychomotor activity (pressured speech, irritability and uneasiness), hypoactive ones normally exhibit quiet appearance, carelessness, reduced mobility and trouble to answer simple questions about themselves and/or special-temporal orientation[18]. Hypoactive delirium may be misdiagnosed as depression or fatigue[14]. Causes of postoperative delirium are multifactorial and include advanced age, history of cognitive impairment, history of alcohol abuse, preoperative medication (especial attention to unrecognized benzodiazepine use), type of anesthetic used during surgery, infection, urinary retention and fluid or electrolyte disturbance[15,19]. Postoperative delirium amplifies the risk of poorer outcomes, medical complications, mortality and institutionalization in patients with hip fracture[6], being necessary to establish early prevention and treatment interventions to reduce its incidence in high-risk patients.
Regional anesthesia (especially spinal anesthetic with very light sedation) probably reduces the incidence of delirium early after surgery[20]. Supplemental oxygen (3-4 L/min) continually till day 2 post-surgery, or while patient’s oxygen saturation is not ≥ 95% without oxygen, have proven to reduce delirium risk[21]. Because pain can contribute to delirium, an adequate postoperative analgesia minimizing the use of sedative drugs and anticholinergic medications seems to decrease its risk. It is necessary to take in count that narcotics also produce sedation and may contribute to its appearance. Though the preventive role of certain medications (antipsychotics, sedatives and cholinesterase inhibitors) has not been yet clearly elucidated[6], some studies have proven that low doses of haloperidol are effective in delirium prevention in this patient population.
Cardiac and vascular complications
A report of the American College of Cardiology and the American Heart Association (ACC/AHA 2007 Guidelines on Perioperative Cardiovascular Evaluation and Care for Noncardiac Surgery) estimates at less than 5% the risk of cardiac complication in postoperative after orthopedic major surgeries, but the 1-year recorded mortality exceeds 20% in patients with hip fracture[22].
The main reasons of in-hospital cardiac related mortality after hip fracture are heart failure and myocardial ischemia, which normally come out quick after fracture in patients with previous heart affectation[23]. The general incidence of perioperative myocardial ischemia in aged patients suffering hip fracture surgery has been informed to be 35% to 42%[24]. Deep venous thrombosis (DVT) is one of the principal causes of perioperative morbidity and mortality. In lack of thromboembolism prophylaxis, the prevalence of venography-detected proximal DVT ascend to 27% of patients[25]. The incidence of fatal pulmonary embolism oscillates between 1.4% to 7.5% of patients within 3 mo of hip fracture surgery[25]. Thromboembolism prophylaxis reduces the rate of DVT by approximately 60%[26]. Regional anesthesia significantly reduces as well these complications, probably in relation with its capability to generate peripheral vasodilatation and to maintaining venous blood flow in the lower extremities, as well as to promote a local inhibition of platelet aggregation and stabilization of endothelial cells[27].
Pulmonary complications
Postoperative pulmonary complications (PPCs) were defined as anomalies of the lung resulting in an identifiable disease with adverse impact in the clinical course of the patient[28]. They are quite common (4% of patients) and suppose an increase length of stay, morbidity and mortality, in patients who had undergone hip fracture surgery. For those reasons, PPCs occurrence may predict long-term survival, particularly among patients older than 70-year-old[28]. Clinical important PPCs after hip fracture surgery comprise exacerbation of chronic lung disease, atelectasis, respiratory failure, pneumonia, pulmonary thromboembolism and acute respiratory distress syndrome[28].
A high number of PPCs risk factors have been identified, such as disorders of central nervous system, medication reducing alertness, treatment with dopamine antagonists, etc. Adequate postoperative fluid balance and pain control may help to diminish PPCs by enabling earlier ambulation and improving the patient’s ability to take deep breaths. Hospital-acquired pneumonia has a high incidence and an important clinical relevance in-between PPCs, being currently the second most frequent nosocomial infection[6]. In addition to other PPCs risk factors, this entity is associated to immunosenescence, a change in the immune response associated with increased age, which causes higher rates of infection and impaired wound healing[29]. Moreover, age-related changes of the lung epithelium contribute to the higher susceptibility to chest infections, since fibrillation frequency and clearance of the respiratory epithelium decrease with higher age[28]. If a chest infection occurs after hip fracture surgery, timely diagnosis, treatment and accurate monitoring are required[21].
Gastrointestinal complications
Common postoperative gastrointestinal complications after hip fracture surgery include dyspepsia, abdominal distention, reflexes ileum and constipation[6]. Gastrointestinal postoperative stress ulcer and secondary bleeding are well documented as a medical complication after hip surgery[6], especially in patients with a history of previous gastroduodenal ulcers. Prevention of gastrointestinal bleeding with pump inhibitors, antacids, etc. is extremely important in this clinical situation, in order to minimize the morbidity and mortality associated with it.
Urinary tract complications
The most common postoperative urinary tract complications after hip surgery are urinary retention, urinary infections and acute kidney injuries[6].
Controlled trials have found that patients who had scheduled intermittent catheterization immediately after surgery or their catheter removed the morning after surgery, had lower rates of urinary retention[30]. For those reasons, urinary catheters should be removed as soon as possible, though the evidence is already limited[6].
Urinary tract infections are the leading cause of nosocomial infection and affect 12% to 61% of all patients with hip fractures[31]. Urinary tract infections are considered an important delirium factor risk, and are responsible to prolong the hospital stay for another 2.5 d and even a higher mortality rate[21]. Urinary catheters are the single most important risk related to this type of postoperative infection. Therefore, indwelling catheters should be preferably removed within 24 h after insertion[32].
The incidence of acute kidney injuries (AKI) among aging patients undergoing arthroplasty for femoral neck fractures ranges from 16% to 24.4%[33]. Postoperative AKI (prerenal, renal or postrenal acute failure) is often multifactorial and may be related to pre, peri or postoperative medical or surgical factors (age, emergency surgery or longer preparation time, dehydration, malnutrition, nephrotoxic drug use, including NSAID, type of surgical procedure, chronic obstructive pulmonary disease, congestive heart disease, peripheral vascular occlusive disease, chronic kidney disease, etc.)[33].
If an AKI occurs after hip fracture surgery, timely treatment and accurate monitoring are required, in order to minimize the risk of permanent kidney damage[33].
Hematologic complications
The prevalence of perioperative anemia in hip fractured patients ranges from 24% to 44%, being even higher if consider only the postoperative one (51% to 87%)[34].
Oscillation of hemoglobin during a hip fracture hospital stay can be attributed to several causes. Preoperative ones are normally related to the fracture itself, because blood loss from a hip fracture can be up to 500 mL[35], while intraoperative ones comprise fluid shifting and significant blood loss during surgery. Postoperative anemia can happen from repeated phlebotomy or hemodilutional anemia[34].
Perioperative anemia has been consistently connected to adverse events in patients undergoing hip fracture surgery. It is related to other medical complications and increased hospitalization duration, rate of readmission and death. Risk factors linked up with this bigger rate of complications include age, inadequate pre-fracture functional level, cardiovascular or pulmonary diseases, low hemoglobin, fracture type, anesthetic type (neuraxial anesthesia and associated sympathetic blockade reduces intraoperative bleeding even under normotensive conditions), length of surgery, and the degree of intraoperative bleeding[15]. Values of hemoglobin concentration ≤ 10 g/dL at admission are an independent predictor of increased mortality at 30 d in patients with hip fractures[36].
Endocrine-metabolic complications
Malnutrition, which is in general prevalent among the elderly population, is even more frequent among patients hospitalized for hip fracture, with rates ranging from 20% to 70%[6]. Malnutrition affects many organs and corporal systems, causing sarcopenia and impairing mental, cardiac and immune function. Consecutively, patients with a protein-caloric malnutrition have higher medical and surgical complication rates (including pressure scars and perioperative infectious complications), lower functional capability and a higher mortality[6,37].
Lower values of Body Mass Index and/or triceps skinfold, albumin, retinol binding protein and cholesterol are related to malnutrition and increase in a dependent way the risk of mortality in institutionalized elderly patients[38]. Men with hip fractures have normally inferior nutritional status than women, which may be one of the factors that explain their increased mortality[38]. Several studies have found a lower acute mortality in patients with hip fracture whom a nutritional supplement is administered in the perioperative period[6].
Diabetes, either type 1 or 2, is frequent in patients with hip fracture. In fact, type 2 diabetics are 70% more likely to suffer this type of fracture. Diabetes decompensation is a quite common preoperative complication of patients that undergo hip fracture surgery, and is associated with both increased risk of asymptomatic coronary heart disease and perioperative infection.
Other complications
Pressure scars result from an imbalance between extrinsic mechanical forces acting on skin and soft tissue, and the intrinsic susceptibility to tissue to collapse. Acute hip fractures are their most frequent causes. Close to 35% of decubitus ulcers occur at the conclusion of the first week of hospitalization.
Risk factors of pressure scars include age, malnutrition, history of smoking and systemic illnesses[34]. The use of foam or alternating pressure mattresses, special beds and equipment to relieve pressure, aggressive skin care, nursing focused on prevention, and good nutrition help prevent the evolution to ulceration[34].
Per and postoperative mortality
Hip fracture has an overall 1 year mortality rate that varies from 14% to 36% among patients aged 65 or above, being higher among men and women, especially after 5 to 10 years after fracture[15,39], and in addition, the survivors have a shorter life expectancy[34]. Mortality is significantly influenced by preoperative cognitive state, medical comorbidities and mobility. Dementia, chronic obstructive pulmonary disease, chest infection, heart failure, anemia, abnormal sodium (low or raised), elevated urea, elevated creatinine and malignancy, have all been described as risk factors for increased mortality in the months following a hip fracture. Patients with an acute heart failure or a postoperative chest infection had a high 30-d mortality of 65% and 43%, respectively[6]. However, postoperative complications increase short and long-term mortality[3].
From the anesthetic and surgical point of view, patients with a high ASA score and patients treated non-operatively have a higher mortality rate[40]. Patients operated within 48 h appear to have a better outcome than those with a delayed surgical intervention. However, in medically unstable patients, a delay of surgery does not result in a statistically significant difference in mortality compared to patients treated surgically[15].
The Nottingham Hip Fracture Score has been validated as a useful tool to predict hip fracture mortality at 30 d. Independent predictors of mortality in patients with hip fracture included masculine sex, age > 86-year-old, two or more comorbidities, anemia, and a mini mental test score ≤ 6 of 10[36].
Clinical and surgical decision making may be personalized to each patient according to an accurate mortality risk assessment[13]. Complication and mortality scoring systems may allow a better informed discussion between doctors and patients.
Anesthetic complications of hip fractures
The incidence of anesthetic complications during hip fracture surgery is influenced not only by the anesthetic technique used, but also by patient comorbidities, the delay between admission and operation, and the surgical technique employed.
A number of meta-analyses report that an operative delay of over 48 h leads to increased morbidity (e.g., pressure scars, pneumonia, thromboembolic phenomena) and even to increased mortality[41-43].
The most frequently-encountered anesthetic complication is arterial hypotension, defined as a preoperative drop in mean arterial blood pressure of more than 30%, or a presurgical pressure reading of 60-70 mmHg[44]. Arterial hypotension has been reported in 15%-33% of patients during the first 20 min after spinal anesthesia induction. This form of anesthesia prompts a sympathetic nervous system block, leading to decreased venous return and thus to impaired peripheral vascular resistance. But hypotension may arise independently of the anesthetic technique used: patients are often hypovolemic due to a fracture-induced loss in blood volume, to the ingestion of diuretics, or to inappropriate fluid intake resulting from immobility, dementia or other causes. All these factors can enhance the hypotensive effect of anesthetics.
Around 25% of hip fracture patients display at least one episode of cognitive dysfunction during hospitalization[42]. A systematic review published by Cochrane in 2004 suggests that the use of spinal anesthesia may reduce the incidence of postoperative confusion. Since spinal anesthesia is also associated with a lower incidence of deep venous thrombosis, recent meta-analyses recommend this as the technique of choice for hip fracture repair, as long as it is not contraindicated[42,43].
Another complication which, though much less common, may prove fatal, is the use of bone cement, which can give rise to the so-called bone cement implantation syndrome (BCIS)[42,45]. Clinical features of this poorly-understood syndrome include hypoxia, hypotension, cardiac arrhythmias, lung hypertension, and a decline in cardiac output. The cardiopulmonary complications of BCIS can be reduced through modern cementing techniques, appropriate anesthesia interventions, and adequate patient preparation, as well as by avoiding the use of cement altogether.
In short, it is impossible to apply a single protocol for hip fracture repair, valid for all patients. The protocol has to be adjusted to reflect patient comorbidities, with a view to minimizing complications. It would seem to be generally accepted, nonetheless, that hip fracture surgery should be performed within 48 h of the patient’s admission to hospital, and that the patient should be provided with an appropriate analgesic, bearing in mind that in most cases the best analgesic is surgical treatment[42].
Surgical complications of hip fractures
Complications arising from hip fracture surgery are fairly common, and vary depending on whether the fracture is intracapsular or extracapsular. The main problems in intracapsular fractures are biological: vascularization of the femoral head, and lack of periosteum -a major contributor to fracture healing- in the femoral neck. In extracapsular fractures, by contrast, the problem is mechanical, and relates to load-bearing.
Though age, comorbidities, ASA classification and delay in surgery are correlated with both medical and surgical postoperative complications and a significantly prolonged hospital stay, there is not a well-designed study that demonstrates a relation between precisely medical complications with particularly surgical ones. Nevertheless malnutrition and diabetes seem to be clearly related to deep infections. Despite the fact that osteoporosis and poor bone quality are related to some surgical complications, the most frequent concomitant osteoporotic fractures (radial and humeral fractures) seem not influence in length of hospitalization, in-hospital mortality, complication rate, and function[46].
Intracapsular fractures
Two major complications may arise following treatment of an intracapsular fracture by osteosynthesis: non-unions and avascular necrosis.
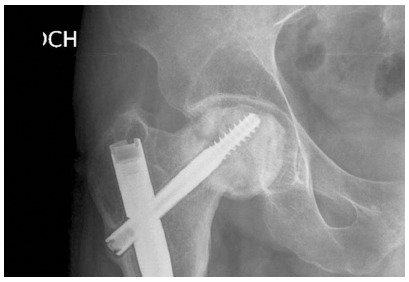
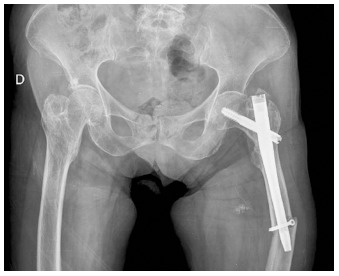
Factors influencing the appearance of non-unions include patient age, degree of displacement, fracture line, degree of comminution and quality of reduction; non-unions are reported in between 10% and 45% of patients undergoing osteosynthesis[47] (Figure 1).
Figure 1.

Intracapsular fracture. Non-union.
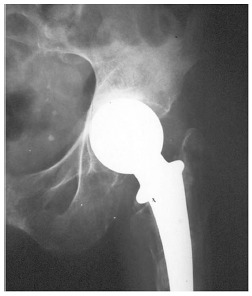
Avascular necrosis of the femoral head occurs in 9%-18% of patients, between two and eight years post-fracture; risk factors include the degree of fracture displacement, patient age and delay in surgical treatment[48-50] (Figure 2).
Figure 2.
Femoral head necrosis.
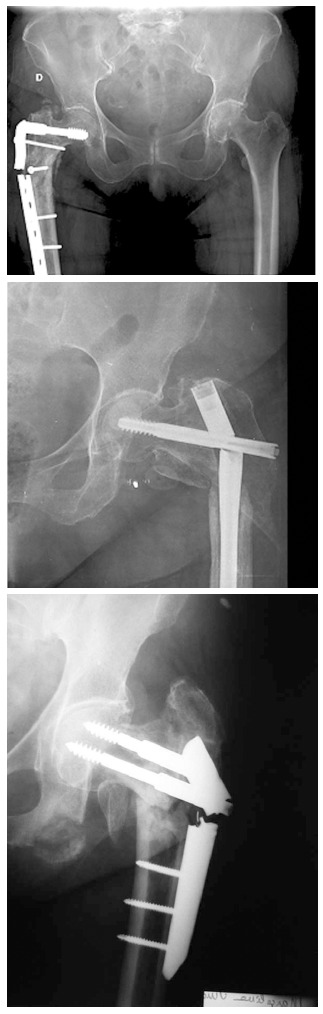
In view of the high complication rates recorded among patients undergoing osteosynthesis, often leading to repeat surgery, several works have compared arthroplasty with osteosynthesis to treat intracapsular fractures. The results indicate significantly (P < 0.001) lower complication and reoperation rates in patients undergoing arthroplasty[47,48]. A number of authors therefore recommend arthroplasty for the treatment of all intra-articular fractures in elderly patients. However, arthroplasty to treat the femoral neck fracture is associated with a number of complications. Dislocation (Figure 3) is most commonly seen in total hip arthroplasty. Acetabular erosion often occurs in active patients undergoing hemiarthroplasty (Figure 4); to avoid this complication, many experts recommend total arthroplasty in these patients[51]. Thigh pain is more frequently reported in uncemented arthroplasty[52]. Moreover, though uncemented arthroplasty may result in higher hip scores, it appears to carry an unacceptably high risk of later femoral fractures[53] (Figure 5).
Figure 3.

Total hip arthroplasty. Dislocation.
Figure 4.
Acetabular erosion.
Figure 5.

Uncemented hip arthroplasty. Femoral fracture.
Extracapsular fractures
A number of postoperative complications have been reported following surgery for extracapsular fractures. The three most common are screw cut-out, femur fracture and implant failure.
Screw cut-out (Figure 6) occurs in between 1.1% and 6.3% of patients treated for an extracapsular fracture, and accounts for 85% of fixation failures[54]. The main causes of cut-out are fracture instability[55], and especially, the incorrect placement of the lag screw. The greatest predictor for the appearance of cut-out is the distance from the screw tip to the subchondral bone. Baumgaertner et al[56], have demonstrated the importance of screw placement and tip-apex distance (TAD) (Figure 7): when TAD was greater than 35 mm, the cut-out rate was 30%, while when TAD exceeded 45 mm, the cut-out rate rose to 60%. The best results have been reported with a TAD of less than 5 mm[49]. Equally important is the positioning of the lag screw in the femoral head, the ideal position being center-center; any other position of the screw tip leads to a higher cut-out rate, which a reportedly rise to 58%[49]. To avoid serious implant failure due to screw cut-out is largerly conditioned by the ability of the surgeon to positioning the lag screw in the femoral head.
Figure 6.
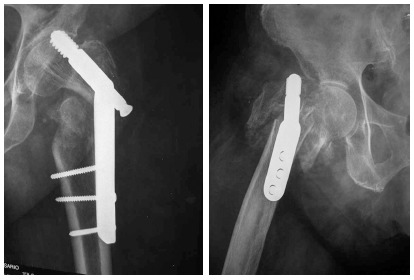
Cut-out.
Figure 7.
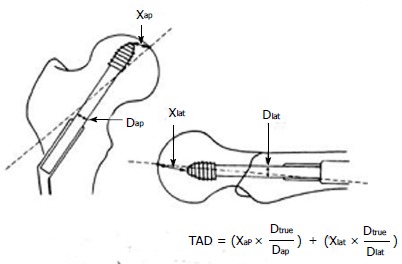
Tip-apex distance.
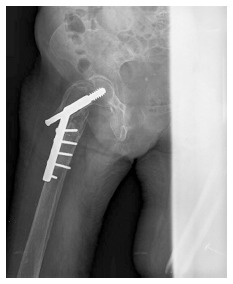
Femoral shaft fracture occurs much more frequently in patients treated with intramedullary nails, and particularly with first-generation nails with a larger distal diameter; according to one meta-analysis, these nails were associated with a femoral fracture rate of 5.3%[57] (Figure 8). Second-generation intramedullary nails, with reduced distal diameter and reduced valgus offset, have prompted a considerable decline in the incidence of femoral fractures[58]. Special mention should be made of reverse obliquity intertrochanteric fractures, in which extramedullary devices are associated with a failure rate of 36%, compared to only 5% for intramedullary nails, since the latter offer improved load-bearing capacity[59]. It should be borne in mind that reverse obliquity fractures of the proximal femur have biomechanical characteristics different from those of other intertrochanteric fractures. It is not yet clear whether nail length influences healing in these fractures[60].
Figure 8.
Femoral fracture in intramedullary nail.
Implant failure usually appears as a result of poor fracture reduction, mechanical stress or fracture instability, but may also be caused by technical error. Implant failure is more common when there is greater rigidity of the fraction fixation device (Figure 9).
Figure 9.
Different implant failures.
Other complications are less frequently reported. Excessive screw sliding (Figure 10) has been linked to impaired postoperative mobility: patients with > 187 mm of sliding display the least postoperative mobility[54]. Thigh pain appears mainly in patients receiving first-generation intramedullary devices, and is linked to the use of two distal interlocking screws. Non-unions are much less common in extracapsular than in intracapsular fractures, and are reported mainly in severely comminuted fractures with bone loss.
Figure 10.
Excessive screw sliding.
CONCLUSION
Even with optimal care, elderly trauma patients suffer a higher morbidity and mortality rate when compared with the general population, and often demand for expensive hospital aftercare. Because of that, surgical treatment of hip fracture in these patients has exceptional clinical challenges, and needs strategies to optimize patient care. Preoperative early clinical assessment helps to identify patients at high-risk and to prevent unnecessary delays. Orthogeriatric units, with a medical co-management of these patients, offer the best chance for a successful outcome, reducing length of stay, in-patient problems and mortality, allowing the patient to recover his previous ambulatory state.
Further research is necessary to evaluate those interventions and recommendations that improve medical management of aged patients with hip fractures, in order to achieve a reduction in morbidity and mortality in these at risk population.
Footnotes
P- Reviewer: Maruyama T, Makishima M, Schoeffl V S- Editor: Wen LL L- Editor: A E- Editor: Wu HL
References
- 1.Bergström U, Jonsson H, Gustafson Y, Pettersson U, Stenlund H, Svensson O. The hip fracture incidence curve is shifting to the right. Acta Orthop. 2009;80:520–524. doi: 10.3109/17453670903278282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.British Orthopaedic Association. The care of patients with fragility fracture. London: British Orthopaedic Association; 2007. pp. 8–11. [Google Scholar]
- 3.Menzies IB, Mendelson DA, Kates SL, Friedman SM. The impact of comorbidity on perioperative outcomes of hip fractures in a geriatric fracture model. Geriatr Orthop Surg Rehabil. 2012;3:129–134. doi: 10.1177/2151458512463392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Auron-Gomez M, Michota F. Medical management of hip fracture. Clin Geriatr Med. 2008;24:701–719, ix. doi: 10.1016/j.cger.2008.07.002. [DOI] [PubMed] [Google Scholar]
- 5.Marsland D, Colvin PL, Mears SC, Kates SL. How to optimize patients for geriatric fracture surgery. Osteoporos Int. 2010;21:S535–S546. doi: 10.1007/s00198-010-1418-8. [DOI] [PubMed] [Google Scholar]
- 6.Chong CP, Savige JA, Lim WK. Medical problems in hip fracture patients. Arch Orthop Trauma Surg. 2010;130:1355–1361. doi: 10.1007/s00402-009-1038-y. [DOI] [PubMed] [Google Scholar]
- 7.Vidán M, Serra JA, Moreno C, Riquelme G, Ortiz J. Efficacy of a comprehensive geriatric intervention in older patients hospitalized for hip fracture: a randomized, controlled trial. J Am Geriatr Soc. 2005;53:1476–1482. doi: 10.1111/j.1532-5415.2005.53466.x. [DOI] [PubMed] [Google Scholar]
- 8.Fisher AA, Davis MW, Rubenach SE, Sivakumaran S, Smith PN, Budge MM. Outcomes for older patients with hip fractures: the impact of orthopedic and geriatric medicine cocare. J Orthop Trauma. 2006;20:172–178; discussion 172-178. doi: 10.1097/01.bot.0000202220.88855.16. [DOI] [PubMed] [Google Scholar]
- 9.Chong C, Christou J, Fitzpatrick K, Wee R, Lim WK. Description of an orthopedic-geriatric model of care in Australia with 3 years data. Geriatr Gerontol Int. 2008;8:86–92. doi: 10.1111/j.1447-0594.2008.00453.x. [DOI] [PubMed] [Google Scholar]
- 10.Lawrence VA, Hilsenbeck SG, Noveck H, Poses RM, Carson JL. Medical complications and outcomes after hip fracture repair. Arch Intern Med. 2002;162:2053–2057. doi: 10.1001/archinte.162.18.2053. [DOI] [PubMed] [Google Scholar]
- 11.Roche JJ, Wenn RT, Sahota O, Moran CG. Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort study. BMJ. 2005;331:1374. doi: 10.1136/bmj.38643.663843.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Monte-Secades R, Peña-Zemsch M, Rabuñal-Rey R, Bal-Alvaredo M, Pazos-Ferro A, Mateos-Colino A. Risk factors for the development of medical complications in patients with hip fracture. Rev Calid Asist. 2011;26:76–82. doi: 10.1016/j.cali.2010.09.003. [DOI] [PubMed] [Google Scholar]
- 13.Donegan DJ, Gay AN, Baldwin K, Morales EE, Esterhai JL, Mehta S. Use of medical comorbidities to predict complications after hip fracture surgery in the elderly. J Bone Joint Surg Am. 2010;92:807–813. doi: 10.2106/JBJS.I.00571. [DOI] [PubMed] [Google Scholar]
- 14.Monk TG, Price CC. Postoperative cognitive disorders. Curr Opin Crit Care. 2011;17:376–381. doi: 10.1097/MCC.0b013e328348bece. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sciard D, Cattano D, Hussain M, Rosenstein A. Perioperative management of proximal hip fractures in the elderly: the surgeon and the anesthesiologist. Minerva Anestesiol. 2011;77:715–722. [PubMed] [Google Scholar]
- 16.Donaldson AJ, Thomson HE, Harper NJ, Kenny NW. Bone cement implantation syndrome. Br J Anaesth. 2009;102:12–22. doi: 10.1093/bja/aen328. [DOI] [PubMed] [Google Scholar]
- 17.Dolan MM, Hawkes WG, Zimmerman SI, Morrison RS, Gruber-Baldini AL, Hebel JR, Magaziner J. Delirium on hospital admission in aged hip fracture patients: prediction of mortality and 2-year functional outcomes. J Gerontol A Biol Sci Med Sci. 2000;55:M527–M534. doi: 10.1093/gerona/55.9.m527. [DOI] [PubMed] [Google Scholar]
- 18.Lipowski ZJ. Delirium in the elderly patient. N Engl J Med. 1989;320:578–582. doi: 10.1056/NEJM198903023200907. [DOI] [PubMed] [Google Scholar]
- 19.Sieber FE, Zakriya KJ, Gottschalk A, Blute MR, Lee HB, Rosenberg PB, Mears SC. Sedation depth during spinal anesthesia and the development of postoperative delirium in elderly patients undergoing hip fracture repair. Mayo Clin Proc. 2010;85:18–26. doi: 10.4065/mcp.2009.0469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Papaioannou A, Fraidakis O, Michaloudis D, Balalis C, Askitopoulou H. The impact of the type of anaesthesia on cognitive status and delirium during the first postoperative days in elderly patients. Eur J Anaesthesiol. 2005;22:492–499. doi: 10.1017/s0265021505000840. [DOI] [PubMed] [Google Scholar]
- 21.Dovjak P, Iglseder B, Mikosch P, Gosch M, Müller E, Pinter G, Pils K, Gerstofer I, Thaler H, Zmaritz M, et al. Treatment and prevention of postoperative complications in hip fracture patients: infections and delirium. Wien Med Wochenschr. 2013;163:448–454. doi: 10.1007/s10354-013-0228-y. [DOI] [PubMed] [Google Scholar]
- 22.Fleisher LA, Beckman JA, Brown KA, Calkins H, Chaikof EL, Fleischmann KE, Freeman WK, Froehlich JB, Kasper EK, Kersten JR, et al. ACC/AHA 2007 Guidelines on Perioperative Cardiovascular Evaluation and Care for Noncardiac Surgery: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines on Perioperative Cardiovascular Evaluation for Noncardiac Surgery) Developed in Collaboration With the American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Rhythm Society, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, and Society for Vascular Surgery. J Am Coll Cardiol. 2007;50:1707–1732. doi: 10.1016/j.jacc.2007.09.001. [DOI] [PubMed] [Google Scholar]
- 23.Smeets SJ, Poeze M, Verbruggen JP. Preoperative cardiac evaluation of geriatric patients with hip fracture. Injury. 2012;43:2146–2151. doi: 10.1016/j.injury.2012.08.007. [DOI] [PubMed] [Google Scholar]
- 24.Huddleston JM, Gullerud RE, Smither F, Huddleston PM, Larson DR, Phy MP, Melton LJ, Roger VL. Myocardial infarction after hip fracture repair: a population-based study. J Am Geriatr Soc. 2012;60:2020–2026. doi: 10.1111/j.1532-5415.2012.04205.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Beaupre LA, Jones CA, Saunders LD, Johnston DW, Buckingham J, Majumdar SR. Best practices for elderly hip fracture patients. A systematic overview of the evidence. J Gen Intern Med. 2005;20:1019–1025. doi: 10.1111/j.1525-1497.2005.00219.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Geerts WH, Bergqvist D, Pineo GF, Heit JA, Samama CM, Lassen MR, Colwell CW. Prevention of venous thromboembolism: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition) Chest. 2008;133:381S–453S. doi: 10.1378/chest.08-0656. [DOI] [PubMed] [Google Scholar]
- 27.Ho HH, Lau TW, Leung F, Tse HF, Siu CW. Peri-operative management of anti-platelet agents and anti-thrombotic agents in geriatric patients undergoing semi-urgent hip fracture surgery. Osteoporos Int. 2010;21:S573–S577. doi: 10.1007/s00198-010-1416-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lo IL, Siu CW, Tse HF, Lau TW, Leung F, Wong M. Pre-operative pulmonary assessment for patients with hip fracture. Osteoporos Int. 2010;21:S579–S586. doi: 10.1007/s00198-010-1427-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Busse PJ, Mathur SK. Age-related changes in immune function: effect on airway inflammation. J Allergy Clin Immunol. 2010;126:690–699; quiz 700-701. doi: 10.1016/j.jaci.2010.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schneider MA. Prevention of catheter-associated urinary tract infections in patients with hip fractures through education of nurses to specific catheter protocols. Orthop Nurs. 2012;31:12–18. doi: 10.1097/NOR.0b013e3182419619. [DOI] [PubMed] [Google Scholar]
- 31.Johansson I, Athlin E, Frykholm L, Bolinder H, Larsson G. Intermittent versus indwelling catheters for older patients with hip fractures. J Clin Nurs. 2002;11:651–656. doi: 10.1046/j.1365-2702.2002.00646.x. [DOI] [PubMed] [Google Scholar]
- 32.Gould CV, Umscheid CA, Agarwal RK, Kuntz G, Pegues DA. Guideline for prevention of catheter-associated urinary tract infections 2009. Infect Control Hosp Epidemiol. 2010;31:319–326. doi: 10.1086/651091. [DOI] [PubMed] [Google Scholar]
- 33.Ulucay C, Eren Z, Kaspar EC, Ozler T, Yuksel K, Kantarci G, Altintas F. Risk factors for acute kidney injury after hip fracture surgery in the elderly individuals. Geriatr Orthop Surg Rehabil. 2012;3:150–156. doi: 10.1177/2151458512473827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bateman L, Vuppala S, Porada P, Carter W, Baijnath C, Burman K, Lee R, Hargus J. Medical management in the acute hip fracture patient: a comprehensive review for the internist. Ochsner J. 2012;12:101–110. [PMC free article] [PubMed] [Google Scholar]
- 35.Lewis JR, Hassan SK, Wenn RT, Moran CG. Mortality and serum urea and electrolytes on admission for hip fracture patients. Injury. 2006;37:698–704. doi: 10.1016/j.injury.2006.04.121. [DOI] [PubMed] [Google Scholar]
- 36.Maxwell MJ, Moran CG, Moppett IK. Development and validation of a preoperative scoring system to predict 30 day mortality in patients undergoing hip fracture surgery. Br J Anaesth. 2008;101:511–517. doi: 10.1093/bja/aen236. [DOI] [PubMed] [Google Scholar]
- 37.Avenell A, Handoll HH. Nutritional supplementation for hip fracture aftercare in older people. Cochrane Database Syst Rev. 2010;(1):CD001880. doi: 10.1002/14651858.CD001880.pub5. [DOI] [PubMed] [Google Scholar]
- 38.Carpintero P, Lopez P, Leon F, Lluch M, Montero M, Aguilera C. Men with hip fractures have poorer nutritional status and survival than women: a prospective study of 165 patients. Acta Orthop. 2005;76:331–335. [PubMed] [Google Scholar]
- 39.Orwig DL, Chan J, Magaziner J. Hip fracture and its consequences: differences between men and women. Orthop Clin North Am. 2006;37:611–622. doi: 10.1016/j.ocl.2006.08.003. [DOI] [PubMed] [Google Scholar]
- 40.Jain R, Basinski A, Kreder HJ. Nonoperative treatment of hip fractures. Int Orthop. 2003;27:11–17. doi: 10.1007/s00264-002-0404-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shiga T, Wajima Z, Ohe Y. Is operative delay associated with increased mortality of hip fracture patients? Systematic review, meta-analysis, and meta-regression. Can J Anaesth. 2008;55:146–154. doi: 10.1007/BF03016088. [DOI] [PubMed] [Google Scholar]
- 42.Griffiths R, Alper J, Beckingsale A, Goldhill D, Heyburn G, Holloway J, Leaper E, Parker M, Ridgway S, White S, et al. Management of proximal femoral fractures 2011: Association of Anaesthetists of Great Britain and Ireland. Anaesthesia. 2012;67:85–98. doi: 10.1111/j.1365-2044.2011.06957.x. [DOI] [PubMed] [Google Scholar]
- 43.Maxwell L, White S. Anaesthetic management of patients with hip fractures: an update. Critical Care Pain. 2013;13:179–183. [Google Scholar]
- 44.Hartmann B, Junger A, Klasen J, Benson M, Jost A, Banzhaf A, Hempelmann G. The incidence and risk factors for hypotension after spinal anesthesia induction: an analysis with automated data collection. Anesth Analg. 2002;94:1521–159, table of contents. doi: 10.1097/00000539-200206000-00027. [DOI] [PubMed] [Google Scholar]
- 45.Khanna G, Cernovsy J, Bone cement and the implications for anaesthesia. Anaesthesia. Critical Care Pain. 2012:4; 213–216. [Google Scholar]
- 46.Buecking B, Wack C, Oberkircher L, Ruchholtz S, Eschbach D. Do concomitant fractures with hip fractures influence complication rate and functional outcome? Clin Orthop Relat Res. 2012;470:3596–3606. doi: 10.1007/s11999-012-2419-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Blomfeldt R, Törnkvist H, Ponzer S, Söderqvist A, Tidermark J. Comparison of internal fixation with total hip replacement for displaced femoral neck fractures. Randomized, controlled trial performed at four years. J Bone Joint Surg Am. 2005;87:1680–1688. doi: 10.2106/JBJS.D.02655. [DOI] [PubMed] [Google Scholar]
- 48.Lu-Yao GL, Keller RB, Littenberg B, Wennberg JE. Outcomes after displaced fractures of the femoral neck. A meta-analysis of one hundred and six published reports. J Bone Joint Surg Am. 1994;76:15–25. doi: 10.2106/00004623-199401000-00003. [DOI] [PubMed] [Google Scholar]
- 49.Kyle RF, Cabanela ME, Russell TA, Swiontkowski MF, Winquist RA, Zuckerman JD, Schmidt AH, Koval KJ. Fractures of the proximal part of the femur. Instr Course Lect. 1995;44:227–253. [PubMed] [Google Scholar]
- 50.Jain R, Koo M, Kreder HJ, Schemitsch EH, Davey JR, Mahomed NN. Comparison of early and delayed fixation of subcapital hip fractures in patients sixty years of age or less. J Bone Joint Surg Am. 2002;84-A:1605–1612. doi: 10.2106/00004623-200209000-00013. [DOI] [PubMed] [Google Scholar]
- 51.Rodríguez-Merchán EC. Displaced intracapsular hip fractures: hemiarthroplasty or total arthroplasty? Clin Orthop Relat Res. 2002;(399):72–77. [PubMed] [Google Scholar]
- 52.Khan RJ, MacDowell A, Crossman P, Datta A, Jallali N, Arch BN, Keene GS. Cemented or uncemented hemiarthroplasty for displaced intracapsular femoral neck fractures. Int Orthop. 2002;26:229–232. doi: 10.1007/s00264-002-0356-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Langslet E, Frihagen F, Opland V, Madsen JE, Nordsletten L, Figved W. Cemented versus uncemented hemiarthroplasty for displaced femoral neck fractures: 5-year followup of a randomized trial. Clin Orthop Relat Res. 2014;472:1291–1299. doi: 10.1007/s11999-013-3308-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lorich DG, Geller DS, Nielson JH. Osteoporotic pertrochanteric hip fractures: management and current controversies. Instr Course Lect. 2004;53:441–454. [PubMed] [Google Scholar]
- 55.Kim WY, Han CH, Park JI, Kim JY. Failure of intertrochanteric fracture fixation with a dynamic hip screw in relation to pre-operative fracture stability and osteoporosis. Int Orthop. 2001;25:360–362. doi: 10.1007/s002640100287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Baumgaertner MR, Curtin SL, Lindskog DM, Keggi JM. The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J Bone Joint Surg Am. 1995;77:1058–1064. doi: 10.2106/00004623-199507000-00012. [DOI] [PubMed] [Google Scholar]
- 57.Parker MJ, Pryor GA. Gamma versus DHS nailing for extracapsular femoral fractures. Meta-analysis of ten randomised trials. Int Orthop. 1996;20:163–168. doi: 10.1007/s002640050055. [DOI] [PubMed] [Google Scholar]
- 58.Saudan M, Lübbeke A, Sadowski C, Riand N, Stern R, Hoffmeyer P. Pertrochanteric fractures: is there an advantage to an intramedullary nail?: a randomized, prospective study of 206 patients comparing the dynamic hip screw and proximal femoral nail. J Orthop Trauma. 2002;16:386–393. doi: 10.1097/00005131-200207000-00004. [DOI] [PubMed] [Google Scholar]
- 59.Sadowski C, Lübbeke A, Saudan M, Riand N, Stern R, Hoffmeyer P. Treatment of reverse oblique and transverse intertrochanteric fractures with use of an intramedullary nail or a 95 degrees screw-plate: a prospective, randomized study. J Bone Joint Surg Am. 2002;84-A:372–381. [PubMed] [Google Scholar]
- 60.Okcu G, Ozkayin N, Okta C, Topcu I, Aktuglu K. Which implant is better for treating reverse obliquity fractures of the proximal femur: a standard or long nail? Clin Orthop Relat Res. 2013;471:2768–2775. doi: 10.1007/s11999-013-2948-0. [DOI] [PMC free article] [PubMed] [Google Scholar]


