Abstract
The majority of proximal humerus fractures are low-energy osteoporotic injuries in the elderly and their incidence is increasing in the light of an ageing population. The diversity of fracture patterns encountered renders objective classification of prognostic value challenging. Non-operative management has been associated with good functional outcomes in stable, minimally displaced and certain types of displaced fractures. Absolute indications for surgery are infrequent and comprise compound, pathological, multi-fragmentary head-splitting fractures and fracture dislocations, as well as those associated with neurovascular injury. A constantly expanding range of reconstructive and replacement options however has been extending the indications for surgical management of complex proximal humerus fractures. As a result, management decisions are becoming increasingly complicated, in an attempt to provide the best possible treatment for each individual patient, that will successfully address their specific fracture configuration, comorbidities and functional expectations. Our aim was to review the management options available for the full range of proximal humerus fractures in adults, along with their specific advantages, disadvantages and outcomes.
Keywords: Proximal humerus fracture, Reconstruction, Non-operative management, Hemiarthroplasty, Reverse polarity total shoulder arthroplasty
Core tip: Non-operative management is associated with good outcomes in the majority of proximal humerus fractures in adults. There is currently insufficient evidence to suggest superiority of one treatment option over the others. Any surgical intervention should have clear aims and indications and the appropriate technique should be selected for each individual patient. Decision-making should involve detailed fracture evaluation, careful patient selection with thorough consideration of individual patient characteristics, comorbidities and functional expectations and profound understanding of the benefits and limitations of each management option.
INTRODUCTION
Epidemiology
Fractures of the proximal humerus are relatively common injuries in adults, representing 4%-5% of all fractures presenting to the accident and emergency department[1] and approximately 5% of fractures of the appendicular skeleton[2,3]. The vast majority are low-energy osteoporotic fractures resulting from simple falls from standing height[4] with a 2-3 to 1 female to male preponderance[2,3,5].
Classification
Proximal humerus fractures may either occur in isolation or be associated with concurrent dislocation of the glenohumeral joint. Additional injuries to the shoulder girdle may also be present, such as co-existing scapular fractures giving rise to the “floating shoulder” variety. As such, a wide range of fracture patterns has been described[6-10], rendering accurate and reproducible classification of prognostic value complex and difficult. Neer’s classification[10] remains the most commonly used system[11], although additional classification systems have been described more recently[12-14].
Neer’s classification system is based on six groups and four main fracture segments (parts) comprising the head, greater tuberosity, lesser tuberosity and shaft[10]. Displacement is defined as more than 1cm of translation or 45 degrees of angulation of the respective fracture part. Group I includes all fracture configurations with minimum displacement. Group II includes two-part fractures of the anatomical neck with articular-segment displacement. Group III comprises three types of displaced two-part surgical neck fractures (i.e., angulated, separated and comminuted surgical neck fractures) with shaft displacement. Group IV consists of two- or three-part fractures with greater tuberosity displacement. Group V includes two- or three-part fractures with lesser tuberosity displacement. Groups IV and V merge in the four-part fracture where both tuberosities are displaced in addition to the head and shaft. Group VI comprises true fracture-dislocation of two-, three- or four-part fractures with ligamentous injury and is subdivided into anterior and posterior dislocations of the glenohumeral joint and partial dislocations of the humeral head with articular surface fractures (i.e., impression fracture and head-splitting fracture).
The AO/OTA classification employs a combination of letters and numbers to describe different levels and patterns of proximal humerus fractures. Proximal humerus fractures are described as 11 fractures with further subdivision into unifocal extra-articular denoted as 11-A, bifocal extra-articular denoted as 11-B and articular fractures denoted as 11-C. Further numbers are assigned according to fracture configuration with 3 representing more complex configurations than 1 and 2, giving rise to a total of twenty-seven subtypes[14].
Nevertheless, both interobserver reliability and intraobserver reproducibility of proximal humerus fracture classification systems have been shown to be poor[15], even when 3-D CT reconstructions are utilised[16,17].
Radiological assessment
Plain radiographs are the main baseline investigation for the diagnosis, classification and management planning of proximal humerus fractures. The proximal humerus should be imaged in a minimum of two planes. Routine assessment includes true anteroposterior and either transcapular “Y” or axillary lateral views, if tolerated by the patient. Additional investigations are then performed as necessary, on the basis of clinical and plain radiographic findings.
Doppler ultrasound examination may be used for the evaluation of associated vascular injuries, as well as of concomitant rotator cuff tears.
Computerised tomography (CT) is employed in the evaluation of complex fracture patterns, whilst it also allows quantification of available bone stock and assessment of the extent and position of fracture union.
CT angiography may accurately diagnose and guide interventional management of co-existing arterial injuries.
Magnetic resonance arthrography and angiography are additional high-quality imaging tools for the assessment of periarticular soft tissue and vascular injuries respectively.
Aim of study
The challenges of proximal humerus fracture classification, alongside individual patient characteristics and functional expectations, surgeon expertise, implant characteristics and availability of rehabilitation services render management decisions complicated and difficult. Our aim was therefore to perform a concise review of the available literature on the current management options of these complex injuries, with a particular focus on their respective advantages, disadvantages and outcomes.
LITERATURE REVIEW
A thorough literature search of the Embase, Ovid Medline(R), Ovid Medline(R) In-Process and Other Non-Indexed Citations, Ovid Journals and the Cochrane Library databases was conducted by two investigators. The search terms used included the title terms proximal AND humerus AND fractur* and the limits were set to adult (> 19 years of age) human trials, English language and published in the last 5 years. This search yielded 368 hits.
PubMed was also searched using the following MeSH term search strategy: (“Shoulder Fractures/analysis”[Majr] OR “Shoulder Fractures/anatomy and histology”[Majr] OR “Shoulder Fractures/classification”[Majr] OR “Shoulder Fractures/complications”[Majr] OR “Shoulder Fractures/diagnosis”[Majr] OR “Shoulder Fractures/epidemiology”[Majr] OR “Shoulder Fractures/etiology”[Majr] OR “Shoulder Fractures/history”[Majr] OR “Shoulder Fractures/mortality”[Majr] OR “Shoulder Fractures/physiopathology”[Majr] OR “Shoulder Fractures/prevention and control”[Majr] OR “Shoulder Fractures/radiography”[Majr] OR “Shoulder Fractures/rehabilitation”[Majr] OR “Shoulder Fractures/surgery”[Majr] OR “Shoulder Fractures/therapy”[Majr]), which yielded an additional 1738 hits. Limiting these to Clinical Trials, Controlled Clinical Trials and Reviews in Humans published within the last 5 years resulted in 112 hits.
The 480 studies obtained were searched manually for exclusion of duplicate hits and irrelevant publications. Case reports, studies focusing on pain management and biology of fracture healing were excluded. Additional relevant studies were identified through scrutinising the reference lists of the studies included.
DISCUSSION
The management of proximal humerus fractures in adults encompasses a constantly expanding range of non-operative, reconstructive and prosthetic replacement options. Good outcomes are highly dependent upon appropriate management decisions, which should be based on a thorough, combined evaluation of fracture-, patient- and treatment centre-related factors.
Non-operative management
Conservative treatment generally consists of analgesia and a period of immobilisation in a sling, with various rehabilitation and physiotherapy regimes. Early physiotherapy commencing within two weeks from injury has been associated with better functional results than prolonged immobilisation[18-20]. Hanging casts are perceived to be less useful than simple collar and cuff slings, as they do not seem to improve reduction and may in fact contribute to fracture distraction and non-union[21,22]. Hospital admission may be required in up to 43% of patients, as the majority of these injuries tend to be osteoporotic fractures in elderly patients culminating in loss of independence and inability to cope[5].
Complications encountered with closed treatment include malunion, subacromial impingement, avascular necrosis, shoulder pain and stiffness secondary to osteoarthritis and rotator cuff deficiency[22]. Most conservatively treated fractures will progress to full union with an estimated risk of non-union between 1.1% and 10%[23].
A number of studies have revealed very good functional results in conservatively managed minimally displaced, stable fractures of the proximal humerus[10,18,24]. Such fractures were classified by Neer as group I fractures, and were estimated to comprise over 85% of all proximal humerus fractures[10]. More recent studies have reported lower rates of minimally displaced fractures, ranging between 42% and 49%[4,5]. Despite higher rates of displaced fractures however, the majority of patients are still being treated non-operatively, in view of their advanced age at presentation, lower functional demands and significant comorbidities[5].
Non-operative management has also been successful in certain types of displaced fractures. These include translated two-part fractures of the proximal humerus with minimal alteration of the neck-shaft angle[24], valgus and varus impacted fractures of the proximal humerus[7,8]. Increasing degrees of displacement and instability, as seen in conservatively managed Neer three- and four-part fracture configurations, are associated with less optimal results than one- or two-part fractures[21]. Certain types of fixation of however, have been shown to confer no benefit to non-operative management in unstable displaced Neer three- and four-part fractures[25].
Operative management
Operative interventions for the management of proximal humerus fractures are constantly evolving and may be broadly classified into reconstructive and prosthetic replacement options.
Reconstruction
A wide range of joint preserving reconstructive techniques have been employed in the management of proximal humerus fractures. These aim to reduce complications and optimize function by restoring anatomy and conferring stability for early rehabilitation and promotion of fracture union. Reduction may be achieved closed, through a minimally invasive approach (mini-open) or open, while fixation may be performed percutaneously (pins, wires, screws) or internally (intramedullary nails, trans-osseous sutures, tension-band constructs or plates and screws).
Closed or mini-open reduction and percutaneous fixation
This technique utilizes image intensifier-guided closed manipulation or mini-open fracture reduction by means of ‘joystick’ pins, followed by fixation with a constellation of threaded pins to confer stability[26]. Its main advantages include soft-tissue preservation, cosmesis, reduced blood loss and postoperative pain. Disadvantages include possibility of axillary nerve injury during percutaneous pin insertion[27,28], fixation failure[29], intra-articular pin migration during fracture collapse leading to re-operation and need for elective removal of metalwork[30].
Stable fixation to allow early range of motion has been demonstrated in patients with two- and three-part fractures fixed percutaneously with 2.5 mm threaded Schantz or Dynamic Hip Screw guide pins, alongside good functional results and a union rate of 94% at an average of 2.6 mo[29]. This type of fixation however is not suitable for patients with four-part fractures, due to a high risk of avascular necrosis and fixation failure. Herscovici et al[29] have also demonstrated a 100% failure rate with smooth Kirschner wires and recommend the use of threaded pins. Brunner et al[30] have shown successful maintenance of reduction in 91% of 58 displaced proximal humerus fractures treated with the “humerus block”. They have reported no intraoperative complications, but had a 40% unplanned re-operation rate, secondary to wire migration and associated fracture displacement[30].
Closed or open reduction and intramedullary nailing
Closed or open reduction and internal fixation by means of a statically locked intramedullary nail is a further joint preserving reconstructive option. Nails are usually inserted anterogradely through a small proximal incision and locked percutaneously. As such, they allow preservation of the periosteal blood supply and surrounding soft tissue envelope, whilst their intramedullary position confers greater stability than other minimally invasive fixation techniques. The benefits of soft tissue preservation and enhanced biomechanical stability render long nails ideal for internal stabilisation of severely osteoporotic and pathological fractures and for prophylactic fixation of impending pathological fractures. In this context, long nails provide protection from additional periprosthetic and skip lesion fractures and allow adjuvant radiotherapy to proceed as necessary with minimal wound healing concerns.
A number of studies using a range of intramedullary nails have produced good results with union rates between 96% and 100%[31-34] in patients with two- and three-part fractures. In a prospective randomised trial comparing locking intramedullary nails to locking plates in the treatment of two-part surgical neck fractures, the authors reported less complications in the nail cohort with equivalent functional scores between the two groups at three years[35].
Complications reported include avascular necrosis and pain especially in four-part fractures[36], proximal screw migration[31,34], loss of proximal fixation[37,38], infection, non-union, impingement[31] and rotator cuff pain and dysfunction[39]. Entry point proximity to the rotator cuff tendons may lead to long-term rotator cuff dysfunction-related morbidity, though new designs of straight instead of curvilinear nails have shown reduced rates of rotator cuff-related symptoms and re-operations[39].
Open reduction and internal fixation
Open reduction can be achieved through various approaches to the proximal humerus. The extended deltopectoral approach remains the most commonly utilised exposure, despite its limited access to the lateral and posterior aspects of the proximal humerus[40]. An alternative extended deltoid-splitting approach has been described, with a view to improve access to the posterior aspect of the shoulder[41] through direct lateral[40] or anterolateral acromial incisions[42]. A recent study by Buecking et al[43] has demonstrated no difference in complications, re-operations, fluoroscopy use, function and pain scores between the extended deltoid-splitting and the anterior deltopectoral approach.
Internal fixation has historically been achieved through various implants and techniques ranging from trans-osseous suture fixation[44] and tension-band wiring of fracture fragments[25] to application of semi-tubular[45], buttress and cloverleaf plates. These have currently been superseded by the use of pre-contoured mono- or polyaxial locking proximal humerus plates[22,46], which have been shown to significantly increase fixation stability in osteoporotic bone[38,47,48] (Figure 1A).
Figure 1.
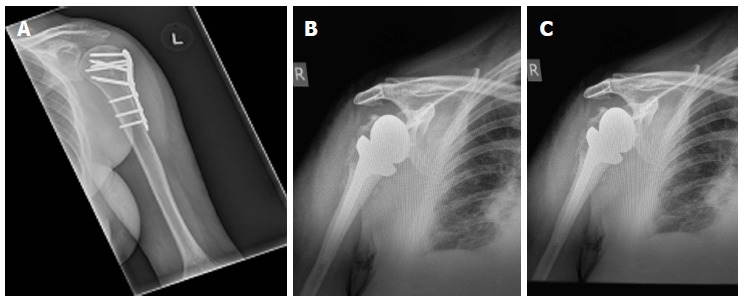
Plain radiograph. A: Showing internal fixation of a left proximal humerus fracture with a locking plate; B: Showing a cemented right shoulder hemiarthroplasty; C: Showing a reverse polarity right total shoulder arthroplasty.
Proximal humerus locking plates may provide reliable fixation in two-, three- and four-part fractures, as well as in some pathological fractures of the proximal humerus[49], particularly when used in conjunction with cement augmentation[50]. Application of the plate may facilitate indirect reduction of the distal diaphyseal fragment to the proximal parts, upon insertion of the working screw[49]. Through a combination of meticulous plate application and appropriately placed rotator cuff tendon fibre-wire suture loops, near anatomical indirect reduction of the tuberosities to the head and shaft fragments becomes possible, without additional soft tissue stripping and compromise to the blood supply[49]. Locking plates may also be used in conjunction with bone autograft, allograft[51-53], as well as devices such as the “Da Vinci System”[54], in cases of comminuted fractures with substantial metaphyseal bone voids and loss of the medial column. As such, unstable three- and four-part fractures may be adequately reconstructed.
Anatomical reduction and restoration of the neck-shaft angle are of paramount importance in reducing the risk of locking plate fixation failure[55,56], while several clinical and cadaveric studies have demonstrated the benefit of medial support screws in maintaining reduction of unstable three- and four-part fractures[57-59]. Good results with union rates of 97%-98% have been reported[60,61] and minimally invasive techniques have been developed to minimise soft tissue dissection[62].
Complications include intra-articular screw penetration, subacromial impingement, varus collapse of fracture and osteonecrosis. These may lead to unplanned re-operations in 13%[60] to 19%[63] of patients, with a predilection for those older than 60 years of age with unstable three- and four-part fractures[56,60]. In some patient series with high rates of three- and four-part fractures, revision surgery to arthroplasty was required in more than 50% of the patients, whilst screw penetration-mediated glenoid erosion, significantly limited revision options and adversely affected long-term outcomes[64]. Displaced four-part fractures and fracture-dislocations with a high risk of osteonecrosis may therefore qualify for primary replacement surgery, particularly in the elderly, low-demand patient.
In high-demand, younger patients however, it is the authors’ opinion that reconstruction followed by close monitoring should be attempted first. In the event of failure, early conversion to hemiarthroplasty remains an option, whilst satisfactory tuberosity reduction at reconstruction, may improve function following revision to hemiarthroplasty. Non-reconstructible fractures may still be converted to hemiarthroplasty intraoperatively and adequate preoperative planning should allow for this.
Replacement
Despite significant advances in surgical technique and a constantly expanding armamentarium of reconstructive options, adequate fixation of metalwork in osteoporotic bone remains a problem[61,64]. Joint replacement options for proximal humerus fractures include shoulder hemiarthroplasty, stemmed total shoulder and reverse polarity total shoulder replacements. These may be used either primarily in elderly patients with displaced four-part fractures, fracture dislocations and head-splitting fractures with a high risk of avascular necrosis, or as salvage procedures following failed reconstruction. Primary replacement surgery, however, is less attractive in young active patients, given the expected longevity of the prosthesis and potential need for several revision operations[65].
Hemiarthroplasty
Hemiarthroplasty is the most commonly used replacement option[66] (Figure 1B). It is indicated in non-reconstructible four-part fractures, fracture-dislocations and head-splitting fractures and for the revision of failed reconstructions, provided the tuberosities remain intact. A number of investigators have emphasised the importance of anatomical tuberosity re-attachment and proper implant positioning in terms of component version, height and offset in restoring rotator cuff function and optimising outcome following hemiarthroplasty[46,67-69]. The upper border of the pectoralis major tendon insertion provides a reliable landmark for estimation of prosthesis height and version[70] and its use has been associated with good clinical and radiological results[71]. Modular implant design improvements enable fine adjustments in the height, offset and version of the prosthesis following stem insertion and along with meticulous surgical technique and rehabilitation have been associated with better outcomes[67,72]. The overall implant survival for shoulder hemiarthroplasty has been reported to be 96.9% at one year, 95.3% at five and 93.9% at ten years[69].
In the event of revision surgery, certain modular implants allow conversion of hemiarthroplasty to total shoulder reverse polarity arthroplasty, without the need for stem removal and lead to shorter operative times and good mid-term outcomes[73].
Complications reported with hemiarthroplasty include infection, dislocation, loosening, reflex sympathetic dystrophy, subacromial impingement, intraoperative or periprosthetic fractures, rotator cuff dysfunction secondary to tuberosity displacement and resorption and heterotopic ossification[22,74]. Poor results have been associated with advanced patient age, implant malpositioning resulting in head-glenoid mismatch, increasing degree of tuberosity displacement, persistent neurological deficit, postoperative complications requiring early re-operation and use of hemiarthroplasty for salvage of previous failed conservative management or operative reconstruction[67,69,72]. In the long-term, hemiarthroplasty has been shown to achieve satisfactory pain relief, but overall functional outcome remains less predictable[69,74,75].
Reverse polarity total shoulder arthroplasty
Reverse polarity total shoulder arthroplasty was originally designed to treat glenohumeral arthritis with rotator cuff arthropathy[76,77]. It is currently also employed in the management of proximal humerus fractures (Figure 1C), in which re-attachment of the tuberosities to a hemiarthroplasty is impossible[78-80]. Reverse polarity total shoulder arthroplasty may be inserted primarily or as a salvage of failed hemiarthroplasty secondary to glenoid arthritis or tuberosity resorption-induced shoulder pseudoparesis[81,82].
Cuff et al[81] have compared primary hemiarthroplasty to primary reverse polarity total shoulder arthroplasty and noted improved forward elevation following reverse polarity total shoulder arthroplasty with similar complication rates between the two groups. In a further comparison by Boyle at al[83] reverse polarity total shoulder arthroplasty was associated with better 5-year functional outcomes compared to hemiarthroplasty, with similar revision and 1-year mortality rates. Previous studies have failed to demonstrate statistically significant differences between functional outcomes of hemiarthroplasty and reverse polarity total shoulder arthroplasty[84]. Forward elevation however, appears to be consistently slightly better in patients treated primarily with reverse polarity total shoulder arthroplasty[81,83-85], albeit at the expense of increased treatment cost in a group of patients with potentially limited life expectancy[85].
A high rate of complications with reverse polarity total shoulder arthroplasty has been reported by Brorson et al[66] in a recent systematic review of the literature. These included dislocation, infection, haematoma, instability, neurological injury, intraoperative and periprosthetic fracture, baseplate failure, reflex sympathetic dystrophy and scapular notching[66], which in the long-term has been associated with component loosening and glenoid bone loss[80]. Nevertheless, reverse polarity total shoulder arthroplasty remains a good option for independent elderly patients with non-reconstructible fractures and associated cuff deficiency, as well as a valuable salvage solution for failed first-line reconstructive or prosthetic replacement management.
CONCLUSION
The management of proximal humerus fractures in adults is a challenging and demanding task. Good outcomes depend on detailed fracture evaluation, careful patient selection with thorough consideration of individual patient characteristics, comorbidities and functional expectations and advanced surgical expertise across a wide range of reconstructive and joint replacement options. A multi-disciplinary team approach should be utilised with experienced musculoskeletal radiologists, geriatricians and specialised physiotherapists for optimal rehabilitation.
Treatment of these complex injuries requires careful planning and should therefore be provided in centres, with appropriate resources and expertise in their management and rehabilitation. There is at present not enough evidence to suggest superiority of one treatment option over the others[11]. The ProFHER trial is an ongoing UK-based multi-centre randomised controlled trial that aims to compare the effectiveness and cost-effectiveness of surgical versus non-operative management for displaced fractures of the proximal humerus in adults[86]. Currently available evidence however suggests that treatment should be individualised and tailored to specific fracture-, patient- and treatment centre-related factors[46].
Footnotes
P- Reviewer: Lorbach O, Nouh MR S- Editor: Wen LL L- Editor: A E- Editor: Wu HL
References
- 1.Horak J, Nilsson BE. Epidemiology of fracture of the upper end of the humerus. Clin Orthop Relat Res. 1975;(112):250–253. [PubMed] [Google Scholar]
- 2.Court-Brown CM, Caesar B. Epidemiology of adult fractures: A review. Injury. 2006;37:691–697. doi: 10.1016/j.injury.2006.04.130. [DOI] [PubMed] [Google Scholar]
- 3.Lind T, Krøner K, Jensen J. The epidemiology of fractures of the proximal humerus. Arch Orthop Trauma Surg. 1989;108:285–287. doi: 10.1007/BF00932316. [DOI] [PubMed] [Google Scholar]
- 4.Court-Brown CM, Garg A, McQueen MM. The epidemiology of proximal humeral fractures. Acta Orthop Scand. 2001;72:365–371. doi: 10.1080/000164701753542023. [DOI] [PubMed] [Google Scholar]
- 5.Roux A, Decroocq L, El Batti S, Bonnevialle N, Moineau G, Trojani C, Boileau P, de Peretti F. Epidemiology of proximal humerus fractures managed in a trauma center. Orthop Traumatol Surg Res. 2012;98:715–719. doi: 10.1016/j.otsr.2012.05.013. [DOI] [PubMed] [Google Scholar]
- 6.Robinson CM, Page RS. Severely impacted valgus proximal humeral fractures. Results of operative treatment. J Bone Joint Surg Am. 2003;85-A:1647–1655. doi: 10.2106/00004623-200309000-00001. [DOI] [PubMed] [Google Scholar]
- 7.Court-Brown CM, Cattermole H, McQueen MM. Impacted valgus fractures (B1.1) of the proximal humerus. The results of non-operative treatment. J Bone Joint Surg Br. 2002;84:504–508. doi: 10.1302/0301-620x.84b4.12488. [DOI] [PubMed] [Google Scholar]
- 8.Court-Brown CM, McQueen MM. The impacted varus (A2.2) proximal humeral fracture: prediction of outcome and results of nonoperative treatment in 99 patients. Acta Orthop Scand. 2004;75:736–740. doi: 10.1080/00016470410004111. [DOI] [PubMed] [Google Scholar]
- 9.Robinson CM, Wylie JR, Ray AG, Dempster NJ, Olabi B, Seah KT, Akhtar MA. Proximal humeral fractures with a severe varus deformity treated by fixation with a locking plate. J Bone Joint Surg Br. 2010;92:672–678. doi: 10.1302/0301-620X.92B5.22849. [DOI] [PubMed] [Google Scholar]
- 10.Neer CS. Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Joint Surg Am. 1970;52:1077–1089. [PubMed] [Google Scholar]
- 11.Handoll HH, Ollivere BJ, Rollins KE. Interventions for treating proximal humeral fractures in adults. Cochrane Database Syst Rev. 2012;12:CD000434. doi: 10.1002/14651858.CD000434.pub3. [DOI] [PubMed] [Google Scholar]
- 12.Edelson G, Kelly I, Vigder F, Reis ND. A three-dimensional classification for fractures of the proximal humerus. J Bone Joint Surg Br. 2004;86:413–425. doi: 10.1302/0301-620x.86b3.14428. [DOI] [PubMed] [Google Scholar]
- 13.Marsh JL, Slongo TF, Agel J, Broderick JS, Creevey W, DeCoster TA, Prokuski L, Sirkin MS, Ziran B, Henley B, et al. Fracture and dislocation classification compendium - 2007: Orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma. 2007;21:S1–133. doi: 10.1097/00005131-200711101-00001. [DOI] [PubMed] [Google Scholar]
- 14.Müller ME, Koch P, Nazarian S The comprehensive classification of fractures of long bones: Springer-Verlag Berlin; 1990 [Google Scholar]
- 15.Sidor ML, Zuckerman JD, Lyon T, Koval K, Cuomo F, Schoenberg N. The Neer classification system for proximal humeral fractures. An assessment of interobserver reliability and intraobserver reproducibility. J Bone Joint Surg Am. 1993;75:1745–1750. doi: 10.2106/00004623-199312000-00002. [DOI] [PubMed] [Google Scholar]
- 16.Foroohar A, Tosti R, Richmond JM, Gaughan JP, Ilyas AM. Classification and treatment of proximal humerus fractures: inter-observer reliability and agreement across imaging modalities and experience. J Orthop Surg Res. 2011;6:38. doi: 10.1186/1749-799X-6-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bruinsma WE, Guitton TG, Warner JJ, Ring D. Interobserver reliability of classification and characterization of proximal humeral fractures: a comparison of two and three-dimensional CT. J Bone Joint Surg Am. 2013;95:1600–1604. doi: 10.2106/JBJS.L.00586. [DOI] [PubMed] [Google Scholar]
- 18.Koval KJ, Gallagher MA, Marsicano JG, Cuomo F, McShinawy A, Zuckerman JD. Functional outcome after minimally displaced fractures of the proximal part of the humerus. J Bone Joint Surg Am. 1997;79:203–207. doi: 10.2106/00004623-199702000-00006. [DOI] [PubMed] [Google Scholar]
- 19.Kristiansen B, Angermann P, Larsen TK. Functional results following fractures of the proximal humerus. A controlled clinical study comparing two periods of immobilization. Arch Orthop Trauma Surg. 1989;108:339–341. doi: 10.1007/BF00932441. [DOI] [PubMed] [Google Scholar]
- 20.Lefevre-Colau MM, Babinet A, Fayad F, Fermanian J, Anract P, Roren A, Kansao J, Revel M, Poiraudeau S. Immediate mobilization compared with conventional immobilization for the impacted nonoperatively treated proximal humeral fracture. A randomized controlled trial. J Bone Joint Surg Am. 2007;89:2582–2590. doi: 10.2106/JBJS.F.01419. [DOI] [PubMed] [Google Scholar]
- 21.Rasmussen S, Hvass I, Dalsgaard J, Christensen BS, Holstad E. Displaced proximal humeral fractures: results of conservative treatment. Injury. 1992;23:41–43. doi: 10.1016/0020-1383(92)90124-b. [DOI] [PubMed] [Google Scholar]
- 22.Murray IR, Amin AK, White TO, Robinson CM. Proximal humeral fractures: current concepts in classification, treatment and outcomes. J Bone Joint Surg Br. 2011;93:1–11. doi: 10.1302/0301-620X.93B1.25702. [DOI] [PubMed] [Google Scholar]
- 23.Cadet ER, Yin B, Schulz B, Ahmad CS, Rosenwasser MP. Proximal humerus and humeral shaft nonunions. J Am Acad Orthop Surg. 2013;21:538–547. doi: 10.5435/JAAOS-21-09-538. [DOI] [PubMed] [Google Scholar]
- 24.Court-Brown CM, Garg A, McQueen MM. The translated two-part fracture of the proximal humerus. Epidemiology and outcome in the older patient. J Bone Joint Surg Br. 2001;83:799–804. doi: 10.1302/0301-620x.83b6.11401. [DOI] [PubMed] [Google Scholar]
- 25.Zyto K, Ahrengart L, Sperber A, Törnkvist H. Treatment of displaced proximal humeral fractures in elderly patients. J Bone Joint Surg Br. 1997;79:412–417. doi: 10.1302/0301-620x.79b3.7419. [DOI] [PubMed] [Google Scholar]
- 26.Naidu SH, Bixler B, Capo JT, Moulton MJ, Radin A. Percutaneous pinning of proximal humerus fractures: a biomechanical study. Orthopedics. 1997;20:1073–1076. doi: 10.3928/0147-7447-19971101-13. [DOI] [PubMed] [Google Scholar]
- 27.Kamineni S, Ankem H, Sanghavi S. Anatomical considerations for percutaneous proximal humeral fracture fixation. Injury. 2004;35:1133–1136. doi: 10.1016/j.injury.2003.08.008. [DOI] [PubMed] [Google Scholar]
- 28.Rowles DJ, McGrory JE. Percutaneous pinning of the proximal part of the humerus. An anatomic study. J Bone Joint Surg Am. 2001;83-A:1695–1699. doi: 10.2106/00004623-200111000-00012. [DOI] [PubMed] [Google Scholar]
- 29.Herscovici D, Saunders DT, Johnson MP, Sanders R, DiPasquale T. Percutaneous fixation of proximal humeral fractures. Clin Orthop Relat Res. 2000;(375):97–104. doi: 10.1097/00003086-200006000-00012. [DOI] [PubMed] [Google Scholar]
- 30.Brunner A, Weller K, Thormann S, Jöckel JA, Babst R. Closed reduction and minimally invasive percutaneous fixation of proximal humerus fractures using the Humerusblock. J Orthop Trauma. 2010;24:407–413. doi: 10.1097/BOT.0b013e3181c81b1c. [DOI] [PubMed] [Google Scholar]
- 31.Giannoudis PV, Xypnitos FN, Dimitriou R, Manidakis N, Hackney R. “Internal fixation of proximal humeral fractures using the Polarus intramedullary nail: our institutional experience and review of the literature”. J Orthop Surg Res. 2012;7:39. doi: 10.1186/1749-799X-7-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rajasekhar C, Ray PS, Bhamra MS. Fixation of proximal humeral fractures with the Polarus nail. J Shoulder Elbow Surg. 2001;10:7–10. doi: 10.1067/mse.2001.109556. [DOI] [PubMed] [Google Scholar]
- 33.Sforzo CR, Wright TW. Treatment of acute proximal humerus fractures with a polarus nail. J Surg Orthop Adv. 2009;18:28–34. [PubMed] [Google Scholar]
- 34.Popescu D, Fernandez-Valencia JA, Rios M, Cuñé J, Domingo A, Prat S. Internal fixation of proximal humerus fractures using the T2-proximal humeral nail. Arch Orthop Trauma Surg. 2009;129:1239–1244. doi: 10.1007/s00402-008-0789-1. [DOI] [PubMed] [Google Scholar]
- 35.Zhu Y, Lu Y, Shen J, Zhang J, Jiang C. Locking intramedullary nails and locking plates in the treatment of two-part proximal humeral surgical neck fractures: a prospective randomized trial with a minimum of three years of follow-up. J Bone Joint Surg Am. 2011;93:159–168. doi: 10.2106/JBJS.J.00155. [DOI] [PubMed] [Google Scholar]
- 36.Adedapo AO, Ikpeme JO. The results of internal fixation of three- and four-part proximal humeral fractures with the Polarus nail. Injury. 2001;32:115–121. doi: 10.1016/s0020-1383(00)00154-6. [DOI] [PubMed] [Google Scholar]
- 37.Bernard J, Charalambides C, Aderinto J, Mok D. Early failure of intramedullary nailing for proximal humeral fractures. Injury. 2000;31:789–792. doi: 10.1016/s0020-1383(00)00150-9. [DOI] [PubMed] [Google Scholar]
- 38.Foruria AM, Carrascal MT, Revilla C, Munuera L, Sanchez-Sotelo J. Proximal humerus fracture rotational stability after fixation using a locking plate or a fixed-angle locked nail: the role of implant stiffness. Clin Biomech (Bristol, Avon) 2010;25:307–311. doi: 10.1016/j.clinbiomech.2010.01.009. [DOI] [PubMed] [Google Scholar]
- 39.Lopiz Y, Garcia-Coiradas J, Garcia-Fernandez C, Marco F. Proximal humerus nailing: a randomized clinical trial between curvilinear and straight nails. J Shoulder Elbow Surg. 2014;23:369–376. doi: 10.1016/j.jse.2013.08.023. [DOI] [PubMed] [Google Scholar]
- 40.Robinson CM, Murray IR. The extended deltoid-splitting approach to the proximal humerus: variations and extensions. J Bone Joint Surg Br. 2011;93:387–392. doi: 10.1302/0301-620X.93B3.25818. [DOI] [PubMed] [Google Scholar]
- 41.Robinson CM, Khan L, Akhtar A, Whittaker R. The extended deltoid-splitting approach to the proximal humerus. J Orthop Trauma. 2007;21:657–662. doi: 10.1097/BOT.0b013e3180ce833e. [DOI] [PubMed] [Google Scholar]
- 42.Gardner MJ, Boraiah S, Helfet DL, Lorich DG. The anterolateral acromial approach for fractures of the proximal humerus. J Orthop Trauma. 2008;22:132–137. doi: 10.1097/BOT.0b013e3181589f8c. [DOI] [PubMed] [Google Scholar]
- 43.Buecking B, Mohr J, Bockmann B, Zettl R, Ruchholtz S. Deltoid-split or deltopectoral approaches for the treatment of displaced proximal humeral fractures? Clin Orthop Relat Res. 2014;472:1576–1585. doi: 10.1007/s11999-013-3415-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dimakopoulos P, Panagopoulos A, Kasimatis G. Transosseous suture fixation of proximal humeral fractures. Surgical technique. J Bone Joint Surg Am. 2009;91 Suppl 2 Pt 1:8–21. doi: 10.2106/JBJS.H.01290. [DOI] [PubMed] [Google Scholar]
- 45.Sehr JR, Szabo RM. Semitubular blade plate for fixation in the proximal humerus. J Orthop Trauma. 1988;2:327–332. doi: 10.1097/00005131-198802040-00010. [DOI] [PubMed] [Google Scholar]
- 46.Maier D, Jäger M, Strohm PC, Südkamp NP. Treatment of proximal humeral fractures - a review of current concepts enlightened by basic principles. Acta Chir Orthop Traumatol Cech. 2012;79:307–316. [PubMed] [Google Scholar]
- 47.Walsh S, Reindl R, Harvey E, Berry G, Beckman L, Steffen T. Biomechanical comparison of a unique locking plate versus a standard plate for internal fixation of proximal humerus fractures in a cadaveric model. Clin Biomech (Bristol, Avon) 2006;21:1027–1031. doi: 10.1016/j.clinbiomech.2006.06.005. [DOI] [PubMed] [Google Scholar]
- 48.Edwards SL, Wilson NA, Zhang LQ, Flores S, Merk BR. Two-part surgical neck fractures of the proximal part of the humerus. A biomechanical evaluation of two fixation techniques. J Bone Joint Surg Am. 2006;88:2258–2264. doi: 10.2106/JBJS.E.00757. [DOI] [PubMed] [Google Scholar]
- 49.Plecko M, Kraus A. Internal fixation of proximal humerus fractures using the locking proximal humerus plate. Oper Orthop Traumatol. 2005;17:25–50. doi: 10.1007/s00064-005-1120-8. [DOI] [PubMed] [Google Scholar]
- 50.Weiss KR, Bhumbra R, Biau DJ, Griffin AM, Deheshi B, Wunder JS, Ferguson PC. Fixation of pathological humeral fractures by the cemented plate technique. J Bone Joint Surg Br. 2011;93:1093–1097. doi: 10.1302/0301-620X.93B8.26194. [DOI] [PubMed] [Google Scholar]
- 51.Russo R, Visconti V, Lombardi LV, Ciccarelli M, Giudice G. The block-bridge system: a new concept and surgical technique to reconstruct articular surfaces and tuberosities in complex proximal humeral fractures. J Shoulder Elbow Surg. 2008;17:29–36. doi: 10.1016/j.jse.2007.03.027. [DOI] [PubMed] [Google Scholar]
- 52.Gerber C, Werner CM, Vienne P. Internal fixation of complex fractures of the proximal humerus. J Bone Joint Surg Br. 2004;86:848–855. doi: 10.1302/0301-620x.86b6.14577. [DOI] [PubMed] [Google Scholar]
- 53.Gardner MJ, Boraiah S, Helfet DL, Lorich DG. Indirect medial reduction and strut support of proximal humerus fractures using an endosteal implant. J Orthop Trauma. 2008;22:195–200. doi: 10.1097/BOT.0b013e31815b3922. [DOI] [PubMed] [Google Scholar]
- 54.Russo R, Visconti V, Lombardi LV, Ciccarelli M, Cautiero F. Da Vinci System: clinical experience with complex proximal humerus fractures. Musculoskelet Surg. 2010;94 Suppl 1:S57–S64. doi: 10.1007/s12306-010-0066-7. [DOI] [PubMed] [Google Scholar]
- 55.Lee CW, Shin SJ. Prognostic factors for unstable proximal humeral fractures treated with locking-plate fixation. J Shoulder Elbow Surg. 2009;18:83–88. doi: 10.1016/j.jse.2008.06.014. [DOI] [PubMed] [Google Scholar]
- 56.Krappinger D, Bizzotto N, Riedmann S, Kammerlander C, Hengg C, Kralinger FS. Predicting failure after surgical fixation of proximal humerus fractures. Injury. 2011;42:1283–1288. doi: 10.1016/j.injury.2011.01.017. [DOI] [PubMed] [Google Scholar]
- 57.Zhang L, Zheng J, Wang W, Lin G, Huang Y, Zheng J, Edem Prince GA, Yang G. The clinical benefit of medial support screws in locking plating of proximal humerus fractures: a prospective randomized study. Int Orthop. 2011;35:1655–1661. doi: 10.1007/s00264-011-1227-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Gardner MJ, Weil Y, Barker JU, Kelly BT, Helfet DL, Lorich DG. The importance of medial support in locked plating of proximal humerus fractures. J Orthop Trauma. 2007;21:185–191. doi: 10.1097/BOT.0b013e3180333094. [DOI] [PubMed] [Google Scholar]
- 59.Ponce BA, Thompson KJ, Raghava P, Eberhardt AW, Tate JP, Volgas DA, Stannard JP. The role of medial comminution and calcar restoration in varus collapse of proximal humeral fractures treated with locking plates. J Bone Joint Surg Am. 2013;95:e113(1–e1137). doi: 10.2106/JBJS.K.00202. [DOI] [PubMed] [Google Scholar]
- 60.Owsley KC, Gorczyca JT. Fracture displacement and screw cutout after open reduction and locked plate fixation of proximal humeral fractures [corrected] J Bone Joint Surg Am. 2008;90:233–240. doi: 10.2106/JBJS.F.01351. [DOI] [PubMed] [Google Scholar]
- 61.Moonot P, Ashwood N, Hamlet M. Early results for treatment of three- and four-part fractures of the proximal humerus using the PHILOS plate system. J Bone Joint Surg Br. 2007;89:1206–1209. doi: 10.1302/0301-620X.89B9.18528. [DOI] [PubMed] [Google Scholar]
- 62.Ruchholtz S, Hauk C, Lewan U, Franz D, Kühne C, Zettl R. Minimally invasive polyaxial locking plate fixation of proximal humeral fractures: a prospective study. J Trauma. 2011;71:1737–1744. doi: 10.1097/TA.0b013e31823f62e4. [DOI] [PubMed] [Google Scholar]
- 63.Konrad G, Bayer J, Hepp P, Voigt C, Oestern H, Kääb M, Luo C, Plecko M, Wendt K, Köstler W, et al. Open reduction and internal fixation of proximal humeral fractures with use of the locking proximal humerus plate. Surgical technique. J Bone Joint Surg Am. 2010;92 Suppl 1 Pt 1:85–95. doi: 10.2106/JBJS.I.01462. [DOI] [PubMed] [Google Scholar]
- 64.Jost B, Spross C, Grehn H, Gerber C. Locking plate fixation of fractures of the proximal humerus: analysis of complications, revision strategies and outcome. J Shoulder Elbow Surg. 2013;22:542–549. doi: 10.1016/j.jse.2012.06.008. [DOI] [PubMed] [Google Scholar]
- 65.Soliman OA, Koptan WM. Four-part fracture dislocations of the proximal humerus in young adults: results of fixation. Injury. 2013;44:442–447. doi: 10.1016/j.injury.2012.09.005. [DOI] [PubMed] [Google Scholar]
- 66.Brorson S, Rasmussen JV, Olsen BS, Frich LH, Jensen SL, Hróbjartsson A. Reverse shoulder arthroplasty in acute fractures of the proximal humerus: A systematic review. Int J Shoulder Surg. 2013;7:70–78. doi: 10.4103/0973-6042.114225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Esen E, Doğramaci Y, Gültekin S, Deveci MA, Suluova F, Kanatli U, Bölükbaşi S. Factors affecting results of patients with humeral proximal end fractures undergoing primary hemiarthroplasty: a retrospective study in 42 patients. Injury. 2009;40:1336–1341. doi: 10.1016/j.injury.2009.06.019. [DOI] [PubMed] [Google Scholar]
- 68.Krause FG, Huebschle L, Hertel R. Reattachment of the tuberosities with cable wires and bone graft in hemiarthroplasties done for proximal humeral fractures with cable wire and bone graft: 58 patients with a 22-month minimum follow-up. J Orthop Trauma. 2007;21:682–686. doi: 10.1097/BOT.0b013e31815917e0. [DOI] [PubMed] [Google Scholar]
- 69.Robinson CM, Page RS, Hill RM, Sanders DL, Court-Brown CM, Wakefield AE. Primary hemiarthroplasty for treatment of proximal humeral fractures. J Bone Joint Surg Am. 2003;85-A:1215–1223. doi: 10.2106/00004623-200307000-00006. [DOI] [PubMed] [Google Scholar]
- 70.Torrens C, Corrales M, Melendo E, Solano A, Rodríguez-Baeza A, Cáceres E. The pectoralis major tendon as a reference for restoring humeral length and retroversion with hemiarthroplasty for fracture. J Shoulder Elbow Surg. 2008;17:947–950. doi: 10.1016/j.jse.2008.05.041. [DOI] [PubMed] [Google Scholar]
- 71.Greiner SH, Kääb MJ, Kröning I, Scheibel M, Perka C. Reconstruction of humeral length and centering of the prosthetic head in hemiarthroplasty for proximal humeral fractures. J Shoulder Elbow Surg. 2008;17:709–714. doi: 10.1016/j.jse.2008.03.004. [DOI] [PubMed] [Google Scholar]
- 72.Taller S, Krivohlávek M, Lukás R, Srám J, Král M. Hemiarthroplasty for management of proximal humeral fractures. Acta Chir Orthop Traumatol Cech. 2007;74:262–267. [PubMed] [Google Scholar]
- 73.Castagna A, Delcogliano M, de Caro F, Ziveri G, Borroni M, Gumina S, Postacchini F, De Biase CF. Conversion of shoulder arthroplasty to reverse implants: clinical and radiological results using a modular system. Int Orthop. 2013;37:1297–1305. doi: 10.1007/s00264-013-1907-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kontakis G, Koutras C, Tosounidis T, Giannoudis P. Early management of proximal humeral fractures with hemiarthroplasty: a systematic review. J Bone Joint Surg Br. 2008;90:1407–1413. doi: 10.1302/0301-620X.90B11.21070. [DOI] [PubMed] [Google Scholar]
- 75.Antuña SA, Sperling JW, Cofield RH. Shoulder hemiarthroplasty for acute fractures of the proximal humerus: a minimum five-year follow-up. J Shoulder Elbow Surg. 2008;17:202–209. doi: 10.1016/j.jse.2007.06.025. [DOI] [PubMed] [Google Scholar]
- 76.Baulot E, Sirveaux F, Boileau P. Grammont’s idea: The story of Paul Grammont’s functional surgery concept and the development of the reverse principle. Clin Orthop Relat Res. 2011;469:2425–2431. doi: 10.1007/s11999-010-1757-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Grammont PM, Baulot E. Delta shoulder prosthesis for rotator cuff rupture. Orthopedics. 1993;16:65–68. doi: 10.3928/0147-7447-19930101-11. [DOI] [PubMed] [Google Scholar]
- 78.Lenarz C, Shishani Y, McCrum C, Nowinski RJ, Edwards TB, Gobezie R. Is reverse shoulder arthroplasty appropriate for the treatment of fractures in the older patient? Early observations. Clin Orthop Relat Res. 2011;469:3324–3331. doi: 10.1007/s11999-011-2055-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Klein M, Juschka M, Hinkenjann B, Scherger B, Ostermann PA. Treatment of comminuted fractures of the proximal humerus in elderly patients with the Delta III reverse shoulder prosthesis. J Orthop Trauma. 2008;22:698–704. doi: 10.1097/BOT.0b013e31818afe40. [DOI] [PubMed] [Google Scholar]
- 80.Cazeneuve JF, Cristofari DJ. [Grammont reversed prosthesis for acute complex fracture of the proximal humerus in an elderly population with 5 to 12 years follow-up] Rev Chir Orthop Reparatrice Appar Mot. 2006;92:543–548. doi: 10.1016/s0035-1040(06)75911-6. [DOI] [PubMed] [Google Scholar]
- 81.Cuff DJ, Pupello DR. Comparison of hemiarthroplasty and reverse shoulder arthroplasty for the treatment of proximal humeral fractures in elderly patients. J Bone Joint Surg Am. 2013;95:2050–2055. doi: 10.2106/JBJS.L.01637. [DOI] [PubMed] [Google Scholar]
- 82.Levy J, Frankle M, Mighell M, Pupello D. The use of the reverse shoulder prosthesis for the treatment of failed hemiarthroplasty for proximal humeral fracture. J Bone Joint Surg Am. 2007;89:292–300. doi: 10.2106/JBJS.E.01310. [DOI] [PubMed] [Google Scholar]
- 83.Boyle MJ, Youn SM, Frampton CM, Ball CM. Functional outcomes of reverse shoulder arthroplasty compared with hemiarthroplasty for acute proximal humeral fractures. J Shoulder Elbow Surg. 2013;22:32–37. doi: 10.1016/j.jse.2012.03.006. [DOI] [PubMed] [Google Scholar]
- 84.Young SW, Segal BS, Turner PC, Poon PC. Comparison of functional outcomes of reverse shoulder arthroplasty versus hemiarthroplasty in the primary treatment of acute proximal humerus fracture. ANZ J Surg. 2010;80:789–793. doi: 10.1111/j.1445-2197.2010.05342.x. [DOI] [PubMed] [Google Scholar]
- 85.Garrigues GE, Johnston PS, Pepe MD, Tucker BS, Ramsey ML, Austin LS. Hemiarthroplasty versus reverse total shoulder arthroplasty for acute proximal humerus fractures in elderly patients. Orthopedics. 2012;35:e703–e708. doi: 10.3928/01477447-20120426-25. [DOI] [PubMed] [Google Scholar]
- 86.Handoll H, Brealey S, Rangan A, Torgerson D, Dennis L, Armstrong A, Chuang LH, Cross B, Dumville J, Gardner S, et al. Protocol for the ProFHER (PROximal Fracture of the Humerus: Evaluation by Randomisation) trial: a pragmatic multi-centre randomised controlled trial of surgical versus non-surgical treatment for proximal fracture of the humerus in adults. BMC Musculoskelet Disord. 2009;10:140. doi: 10.1186/1471-2474-10-140. [DOI] [PMC free article] [PubMed] [Google Scholar]


