Abstract
Acute gastrointestinal bleeding (AGIB) is a prevalent condition with significant influence on healthcare costs. Endoscopy is essential for the management of AGIB with a pivotal role in diagnosis, risk stratification and management. Recently, hemostatic powders have been added to our endoscopic armamentarium to treat gastrointestinal (GI) bleeding. These substances are intended to control active bleeding by delivering a powdered product over the bleeding site that forms a solid matrix with a tamponade function. Local activation of platelet aggregation and coagulation cascade may be also boosted. There are currently three powders commercially available: hemostatic agent TC-325 (Hemospray®), EndoClot™ polysaccharide hemostatic system, and Ankaferd Bloodstopper®. Although the available evidence is based on short series of cases and there is no randomized controlled trial yet, these powders seem to be effective in controlling GI bleeding from a variety of origins with a very favorable side effects profile. They can be used either as a primary therapy or a second-line treatment, and they seem to be especially indicated in cases of cancer-related bleeding and lesions with difficult access. In this review, we will comment on the mechanism of action, efficacy, safety and technical challenges of the use of powders in several clinical scenarios and we will try to define the main current indications of use and propose new lines of research in this area.
Keywords: Gastrointestinal hemorrhage, Endoscopy, Powders, Endoscopic hemostasis
Core tip: Hemostatic powders are a new endoscopic therapeutic modality for gastrointestinal bleeding. Based on their characteristics and mechanism of action, they may be very useful in controlling bleeding in some situations. In the last two years, a large number of studies, mainly short series of cases, have been published on this topic but their role in the management algorithm is not yet defined. In this review, we will comment on the efficacy and safety of the use of powders in several clinical scenarios and we will try to define the main current indications of use and propose new lines of research in this area.
INTRODUCTION
Acute gastrointestinal bleeding is a prevalent condition with significant influence on healthcare costs. The annual rate of hospitalizations from acute upper GI bleeding (AUGIB) in the United States is around 160 hospital admissions per 100000 population[1], leading to approximately 300000 hospitalizations annually. Between 36% and 50% of AUGIB episodes in most published series are due to non-variceal causes, mainly peptic ulcer[2,3]. Despite improvements in medical and endoscopic therapy, mortality from AUGIB remains around 10%, with higher rates for variceal bleeding and malignancy[2]. On the other hand, severe acute lower GI bleeding (ALGIB), mainly caused by diverticular disease, vascular lesions and ischemic colitis, is an emerging cause of hospital admission[4]. In one study, the ratio of hospitalization rates between upper and lower GI complications decreased from 4.3 to 1.4 in 10 years[5].
Endoscopy plays a pivotal role in the management of both types of GI bleeding, allowing diagnosis, risk stratification and treatment[6-8]. Endoscopic hemostatic therapy is the basis of treatment in patients with active bleeding or with endoscopic features that predict an increased risk of further hemorrhage. However, endoscopic therapy in clinical practice has some drawbacks that limit its efficacy. For instance, despite being highly effective in achieving hemostasis in UAGIB, in 5%-10% of patients this bleeding will not be initially controlled or they will experience a recurrence[9]. In patients with severe acute bleeding and a difficult anatomy (e.g., posterior duodenal wall or the upper region of the lesser gastric curvatures), endoscopic therapy can be challenging, often requiring a high level of technical expertise. Finally, this life-threatening condition can also present outside normal working hours when a less skilled endoscopist is on call. Therefore, a simple and effective hemostatic tool might have a significant impact on endoscopic therapy efficacy of AGIB.
Recently, hemostatic powders have been added to our endoscopic armamentarium to treat GI bleeding. They are intended to control active bleeding by delivering a substance over the bleeding site using a catheter through the working channel of the endoscope. Perhaps the main advantage of this technology is that less precision is needed, allowing for treatment of lesions with difficult access and refractory to standard therapy[10]. There are three hemostatic powders currently available for endoscopic usage (Table 1): hemostatic agent TC-325 (Hemospray™), EndoClot™ polysaccharide hemostatic system (PHS), and Ankaferd Bloodstopper® (ABS). In this review, we will describe the mechanism of action, efficacy in different clinical scenarios, safety of the hemostatic powders, and will comment on the possible role of this tool in the endoscopic treatment of GI bleeding.
Table 1.
Hemostatic powders currently available
| Name | Composition | Mechanism of action | Regulatory clearance |
| Hemospray™ | Mineral | Absorption of water | Approved in Europe and Canada1 |
| Concentration of platelets and clotting factors | Under evaluation in United States | ||
| Mechanical tamponade | |||
| EndoClot™ PHS | Absorbable hemostatic polysaccharides | Absorption of water | Approved in Turkey, Europe, Malaysia and Australia |
| Concentration of platelets and clotting factors | |||
| Mechanical tamponade | |||
| Ankaferd® Blood Stopper | Mixture of plants | Encapsulated protein network that provides focal points for erythrocyte aggregation | Approved in Turkey |
For non-variceal upper gastrointestinal bleeding.
MECHANISM OF ACTION
All three powders are designed to be applied through the working channel of the endoscope over the bleeding area. Their components, in contact with moisture, form a stable mechanical barrier that covers the bleeding site, inducing hemostasis. Therefore, they should only be applied if there is an active bleeding. Slight differences are found because of their different chemical composition.
HemosprayTM (TC-325)
TC-325 (Hemospray™, Cook Medical Inc, Winston-Salem, NC, United States) is a proprietary inorganic powder containing no human or animal proteins, botanicals or allergens. It is neither absorbed nor metabolized, therefore it is considered metabolically inert and nontoxic (information provided by the manufacturer). The precise mechanism of action is unknown but it is hypothesized that the powder, in contact with water, forms an adhesive covering that seals the tissue, producing a mechanical tamponade (Table 1). In 24-72 h, this adherent coat sloughs off into the lumen and is completely eliminated from the GI tract[11]. Water absorption also leads to concentration of platelets and clotting factors with activation of platelets and the coagulation cascade[12]. The in vitro effects of TC-325 on standardized coagulation and platelet function have been studied, showing that both prothrombin time and activated partial thromboplastin are reduced in a dose-dependent way in the presence of the powder[13]. These results suggest that Hemospray™ may facilitate local hemostasis.
EndoClot™ PHS
EndoClot™ PHS (EndoClot Plus Inc, Santa Clara, California, United States) is a starch-derived compound that consists of biocompatible absorbable hemostatic polysaccharides. In contact with blood, it rapidly absorbs water, causing a high concentration of platelets, red blood cells and coagulation proteins at the bleeding site, thus accelerating the physiological clotting cascade (Table 1). A gelled matrix is formed that adheres to and seals the bleeding tissue. This matrix is cleared from the bleeding site in a few hours or days[14]. When applied to skin wounds, it seems to improve healing by activating fibroblasts and transforming growth factor (TGF)-β1 release[15], but this effect has not been studied in the GI mucosa.
ABS
This is a mixture of plants, including Thymus vulgaris, Glycyrrhiza glabra, Vitis vinifera, Alpinia officinarum and Urtica dioica. In vitro and ultrastructural studies suggest that ABS rapidly forms an encapsulated protein network that provides focal points for erythrocyte and activated leukocyte aggregation (Table 1)[16,17]. This network stems from interactions between ABS and blood proteins, such as fibrinogen, inducing protein agglutination. Total protein, albumin and globulin levels also decrease in serum, probably via agglutination of these molecules in the growing protein network. However, most coagulation factors are not affected by the addition of ABS to fresh normal plasma or serum[18].
ABS also has functional properties, inhibiting fibrinolysis and some natural anticoagulant pathways via interaction with the protein C anticoagulation pathway. On one hand, it enhances the expression of plasminogen activator inhibitor 1 (PAI-1), one of the major inhibitors of fibrinolysis, thus increasing clot stability. On the other hand, ABS has also been shown to down-regulate the endothelial cell protein C receptor (EPCR), a natural enhancer of protein C activity, therefore taking part in inactivation of factors Va and VIIa[19].
EVIDENCE SUPPORTING THE ROLE OF POWDERS IN ENDOSCOPIC HEMOSTASIS
The evidence supporting the role of powders in GI bleeding is of moderate quality and based mainly on short series of cases and retrospective studies without a control group.
Hemospray™ (TC-325)
Animal models: This powder has been tested in animal models of arterial gastrointestinal bleeding. Giday et al[10] performed a randomized controlled trial on 10 pigs allocated to treatment with TC-325 or sham after surgical creation of an arterial bleeding from a gastroepiploic vessel opened up to the gastric lumen. The endpoint of the study was the proportion of animals in which hemostasis was achieved at 1 h. In the treatment group, acute hemostasis was achieved in the whole group with no rebleeding in the first 6 h compared to 0% of animals in the sham group. Mean time to hemostasis was 13.8 min.
Ulcer bleeding: Sung et al[11] carried out a pilot study on the efficacy of TC-325 as the primary hemostatic method in 20 patients with active peptic ulcer bleeding. Hemostasis was achieved in all but one (95%), a patient with a Forrest Ia ulcer who ultimately needed embolization to stop bleeding. Two patients met the criteria for rebleeding during follow-up, but no active bleeding was detected in the second-look endoscopy. However, it must be pointed out that most treated bleedings were moderate and the only patient with a high risk lesion had a worse outcome.
Cancer-related GI bleeding: Conventional therapy in this kind of bleeding has moderate success and high rates of rebleeding. Chen et al[20] reported on a short series of 5 patients with upper GI bleeding secondary to gastroduodenal tumors. The authors reported control of bleeding in all cases with only one case of rebleeding in a patient with disseminated intravascular coagulation. Leblanc et al[21] treated 5 patients with bleeding from GI neoplasms (2 esophageal, 2 gastric and 1 pancreatic) with TC-325. Successful hemostasis was achieved in all patients. Two patients showed recurrent bleeding, again successfully treated with TC-325.
Patients on antithrombotic therapy: Hostel et al[22] evaluated 16 patients with upper GI bleeding treated with TC-325 either as a monotherapy or as salvage therapy. In 9 patients, the source of bleeding was a peptic ulcer and in 2, a neoplasm. Eight patients were on antithrombotic therapy (ATT), including patients on antiplatelet agents, NSAIDs or VKA/heparin. Initial hemostasis was achieved in 5/8 patients on ATT and in all patients of the non-ATT group (P = 0.2). The source of bleeding was a spurting arterial vessel in two of the three failures of TC-325 in patients of the ATT group. Rates of rebleeding were similar in both groups (around 25%) and in most cases bleeding was retreated with TC-325.
Bleeding secondary to a therapeutic intervention: Leblanc et al[21] used TC-325 to control bleeding after a therapeutic endoscopic intervention in 13 patients (5 esophageal EMR, 4 duodenal EMR, 2 ampullary resections and 1 biliary sphincterotomy). The powder achieved complete hemostasis in all patients, either as a first-line treatment or a rescue therapy, including 2 cases with spurting arterial vessels. There were no rebleedings. Very recently, TC-325 has been successfully applied to a severe bleeding after endoscopic ultrasound-guided pseudocyst drainage which had been refractory to adrenaline and fibrin glue injection[23], and in a case of bleeding after a rectal submucosal endoscopic dissection[24].
Bleeding related to portal hypertension: TC-325 has been used in cases of both esophageal and gastric variceal bleeding with good short-term results[25-27]. Smith et al[28] controlled acute bleeding from severe portal hypertensive gastropathy in 3 patients. However, it is only able to control the initial bleeding and cannot prevent further bleedings.
Lower GI bleeding: TC-325 has also been used for lower GI bleeding[29] which is currently not a licensed use of the powder. In the largest series published to date, 9 patients with lower GI bleeding were treated with TC-325, 4 of them with post-polypectomy bleedings. Successful initial hemostasis was achieved in all patients, with 2 cases (22%) of rebleeding[30]. Smith et al[28] treated one patient with a portal hypertensive colopathy with TC-325, achieving a decrease in transfusion requirements. Very recently, Kraft et al[31] described the use of TC-325 for the treatment of a lower GI bleeding from diffuse colonic ulcers secondary to diclofenac.
Larger case series: A multicenter European trial has been published on the use of Hemospray™ in non-variceal upper GI bleeding[32]. In this trial, 63 patients with a variety of indications, including ulcers, tumors and post-therapeutic bleeding, were treated with Hemospray™ as either monotherapy or second-line therapy. Primary hemostasis was achieved in 85% of patients when Hemospray was used as monotherapy. Seven patients rebled by the 7th day, therefore 15 patients (27%) failed to achieve sustained hemostasis. The 3 patients who rebled from a peptic ulcer had a Forrest Ia lesion. Hemospray was used as a second-line therapy in 8 patients, with two early rebleedings.
Very recently, a case series from two Swiss hospitals evaluated the performance of Hemospray™ on 16 patients with bleeding from different sources. In most cases, the powder was used as a rescue therapy with an initial hemostasis rate of 93%. Two patients rebled (12.5%), both presenting with oozing bleeding in the previous endoscopy[33].
EndoClot
There is only one publication in a peer reviewed journal reporting on EndoClot in control and prevention of EMR-related bleeding. EndoClot was applied to mucosal defects after resection of 181 lesions (82 patients) regardless of if there was immediate post-resection bleeding. Among them, 20 lesions in 18 patients had early bleeding (five of them showing spurting bleeding). Bleeding was controlled with a single round of spray in 18 lesions (90%) and two cases needed hot biopsy forceps applied to achieve hemostasis. Bleeding recurred in three of these 18 patients but no therapy was needed. The authors concluded that EndoClot effectively achieves hemostasis in controlling and preventing EMR-related bleeding[34]. Two trials on the prevention of bleeding after endoscopic mucosal resection (NCT01496781 and NCT01735786) are ongoing but there are no data available yet[35,36]. Finally, there are some studies presented only in abstract form on short series of patients with a variety of bleeding lesions, reporting a success rate of around 80%, including some with coagulation disorders[37-39].
ABS
This agent has been approved in Turkey (Table 1) for clinical hemorrhages refractory to conventional hemostatic measures. There are several reports on the mechanism of action and clinical efficacy of ABS, almost all from the same Turkish groups.
Animal studies: Several authors have shown that ABS has a clinically meaningful hemostatic effect in rats and swine models with arterial sections, skin lacerations and liver puncture wounds, even if they were treated with warfarin[40-43].
Peptic ulcer bleeding: ABS has shown efficacy in peptic ulcer bleeding in some reports with a very low number of patients, including a child and a patient with thrombocytopenia[44,45].
Cancer-related GI bleeding: Several studies have assessed ABS efficacy on malignant GI bleeding, showing a good performance[46,47]. Clinical observation suggests that the hemostatic effect of ABS on malignant bleeding persists for a long time after its delivery. Some authors have suggested that this may be due to an inhibitory effect of ABS on tumor angiogenesis. A decrease in microvessel density (MVD) in tumoral sections stained with CD34 after treatment with Ankaferd has been described[48].
Other indications: Case reports on the treatment with ABS of post-sphincterotomy bleeding[49], Mallory-Weiss syndrome[44,50] and gastric post-polypectomy bleeding[51] have been reported. Two reports on the use of ABS to control esophageal variceal bleeding have also been published[52,53].
Lower GI bleeding: ABS has been applied in patients with radiation proctitis, with transient control of bleeding, but with no effect on telangiectasias[54]. There are also anecdotal cases of ABS use on post-polypectomy bleeding[50,51] and solitary rectal ulcer[55].
Larger case series: The most recent series on the use of ABS to control upper GI bleeding included 27 patients with active non-variceal UGIB[56]. Bleeding lesions were not described. In one patient, bleeding ceased after spraying isotonic saline and in the other, 26 ABS was applied. Bleeding stopped in 19 cases (73%). In 6 of the remaining 7 patients, ABS was sprayed again plus another endoscopic hemostatic method (clip, injection, APC), achieving an adequate control in all cases. The overall rate of rebleeding was 20%. Bleeding control with ABS was more difficult in patients with a coagulopathy or who were taking AAS.
TECHNICAL ISSUES
Hemospray™
The Hemospray™ package includes a delivering device with a powder syringe (20 g each), two catheters (7 and 10 F, suitable for a working channel of 2.8 and 3.7 respectively) and a CO2 cartridge (Figure 1). The latter is activated by turning a red knob placed at the base of the handle until it stops. Before inserting the catheter in the working channel of the endoscope, blood must be removed as much as possible and the bleeding site must be identified. Then, air is flushed through the accessory channel and the catheter is slowly advanced through it until the catheter tip is visualized. Care must be taken in not placing the catheter directly in contact with blood or the mucosa to avoid occlusion. It is advisable to maintain a 1-2 cm distance from the bleeding site during the procedure. Then, after turning the red valve placed at the top of the delivery device to the open position, TC-325 is ready to be delivered by depressing the red trigger button in 1-2 s pulses. Following the manufacturer´s instructions, no more than 3 devices (60 g) should be applied per patient. However, some authors have used up to 7 syringes in one patient without any secondary effect[11].
Figure 1.
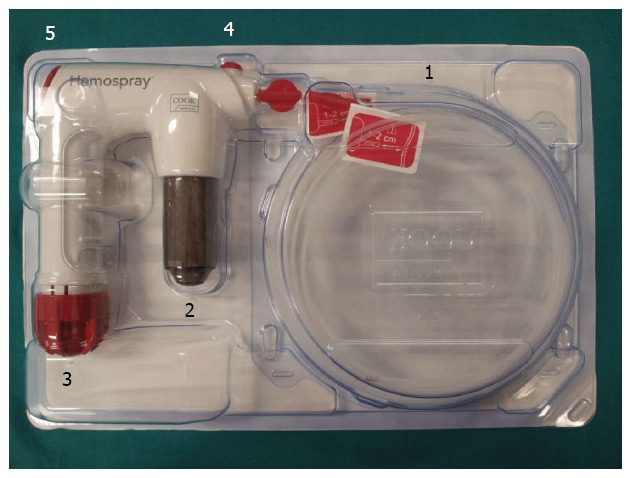
Hemospray™ package. 1: Spray catheters; 2: Powder cartridge; 3: Activation knob; 4: Security valve; 5: Trigger.
In a large trial, 7 of 63 patients (11%) treated with Hemospray suffered technical-related complications[32]. There were 3 blockages of the application catheter, 2 cases of the endoscope transiently adhering to the esophageal mucosa after use with the endoscope in retroflexion, 1 occlusion of the working channel of the endoscope and 1 malfunction of the CO2 cartridge. In spite of this, most of the examiners felt that Hemospray was easier to use than conventional hemostatic methods[32].
Special indications suppose some technical challenges. Powder application is feasible with a duodenoscope, but caution must be taken with the use of the elevator to prevent plication of the catheter[21,57]. Hemospray cannot be used to control bleeding during EMR or ESD because it would obscure the resection field. However, Hemospray can be used at the end of the procedure if indicated.
EndoClot
The EndoClot™ PHS consists of a canister containing 1, 2 or 3 g of the powder, an air compressor that propels air down the catheter and a powder-gas mixing chamber attached to a delivery catheter that is introduced through the working channel of the endoscope[14]. After spraying, the bleeding site must be observed for 5 min. If bleeding recurs, the powder can be reapplied[34].
ABS
ABS can be delivered through the working channel of the endoscope by injecting 50-mL vials through a disposable catheter. Topical application of ABS must completely cover the bleeding surface. Following the author´s recommendations, a spray catheter or a wash pipe should be used. The amount of powder to be applied is dependent on the extent of bleeding. During administration of ABS, a local discoloration may be observed that together with the network formation may hamper the detection of the bleeding point. Therefore, the application of ABS should be performed only after precise location of source of bleeding.
SAFETY
The main theoretical concerns of using powders on an active bleeding site are local damage because of foreign body reactions and systemic embolization because of the introduction of particles into the blood stream. Embolization is of concern, especially in the case of Hemospray™ and Endoclot™ in which the powder is delivered by means of a system of positive outflow pressure. Another theoretical problem for the three powders may be bowel obstruction, caused by the formed matrix itself when it is sloughed off from the gastrointestinal mucosa a few days after its application. These secondary effects have been more extensively studied for HemosprayTM, while there are very few available data about secondary effects of Endoclot and Ankaferd.
Preclinical studies
Studies with TC-325 carried out on animal models with open wounds showed endothelial and transmural damage in transected vessels in pigs, along with small clots and powder residues in lungs[58]. However, these studies referred to external wounds and more severe vessel injuries than the standard vessel defect in a GI bleeding. In the animal study by Giday et al[10] on gastric arterial bleeding, necropsy of the animals treated with TC-325 showed no foreign body granuloma and no signs of embolization in brain or lungs. The same group, in a study designed to identify local and systemic secondary effects following endoscopic application of TC-325, showed no local or regional particulate effects and no distance embolic effects[59]. In similar studies using Ankaferd, these secondary effects have also not been described[42]. Bowel obstruction has not been described in animals[59].
Clinical studies
There are no trials specifically designed to address secondary effects of powders. However, a recent European multicenter study has shown no secondary effects when using TC-325 for a variety of indications, including peptic ulcers, vascular lesions, malignancies and post-therapeutic bleedings[32]. No secondary effects of Ankaferd and EndoClot have been described in the scarce literature available. Bowel obstruction has not been described with TC-325, even when maximum doses were delivered[11]. Intestinal blockage seems to be rare with EndoClot because in most cases bleeding is controlled only with 3 g of powder and starch particles are rapidly degraded in the GI tract.
Regarding Hemospray™, specific concerns have been raised for some indications. For instance, when treating bleeding from esophageal or gastric varices, thromboembolism may be an issue because particles might enter the vascular system. In fact, its use in this setting is contraindicated by the manufacturer. However, the Hemospray™ outflow pressure is less than the intravariceal pressure of a bleeding varix when applied from a distance of 1-2 cm and no embolism has been shown in this indication[25,27]. In vitro coagulation time modifications caused by TC-325 do not seem to pose any clinical problem in cirrhotic patients[25]. A case of biliary blockage has been described when TC-325 was applied in a patient with post-sphincterotomy bleeding[57].
The application of a pressure spray on the resection area after EMR could theoretically cause a perforation. However, no perforation was detected in a small series[21]. Only one case of bowel perforation after treatment of a severe portal hypertensive gastropathy with TC-325 has been reported[28] but it was not clear if the perforation was related to the procedure. Following the manufacturer´s instructions, Hemospray™ use is contraindicated in patients with suspected GI perforation or those at high risk of perforation during the endoscopic procedure (information provided by the manufacturer). Some secondary effects of TC-325 when applied in the large bowel have been described. A case of abdominal cramps after each application of Hemospray™ on a resection area in the rectum was described. This patient did not show any long-term secondary effect[22].
CONCLUSION
Randomized controlled trials comparing powders with standard endoscopic methods are not yet available, thus the current evidence must be considered as moderate at best. The precise role of this technology in the therapeutic algorithm or GI bleeding is yet to be defined but from the present review some practical conclusions can be drawn.
Topical hemostatic powders seem to be effective to control both upper and lower gastrointestinal bleeding from a variety of sources. They can be used as a primary method or a second-line therapy and in combination with standard hemostatic methods. However, there is a substantial proportion of patients who fail to achieve primary hemostasis, mainly Forrest Ia peptic ulcer bleedings. In case of a primary failure, an adjuvant conventional endoscopic method can be applied after removing the adherent matrix with water flushing. There is some risk of rebleeding in the first week after the initial hemorrhagic episode, probably because the mineral matrix sloughs off from the mucosa after 24-72 h. A second-look endoscopy may be appropriate in this subset of patients with special risk of rebleeding.
Perhaps the most specific indication for the use of powders in GI bleeding is hemorrhage from a neoplastic lesion, which may have several bleeding points. Powders may be very useful in this setting because, when applied, they cover a large area of mucosa. Failure to achieve hemostasis with conventional methods is the other main indication for powders (Table 2).
Table 2.
Possible indications for the use of hemostatic powders
| Primary hemostatic method | Adjuvant therapy |
| Lesions with a difficult endoscopic access | Failure of conventional methods |
| Less experienced examiner | |
| Malignant gastrointestinal bleeding | |
| Massive bleeding as a mean to achieve an initial hemostasis |
However, active research is needed to clarify grey areas, like secondary effects and long-term efficacy. Future areas of research should be the development of well-designed randomized trials to assess efficacy of powders vs conventional endoscopic treatment as a primary therapeutic option, paying special attention to safety issues. Possible outcomes would be rates of rebleeding, need for adjuvant endoscopic therapy, and transfusion requirements. Sample size should be large enough to evaluate the efficacy of powders in the management of high risk bleeding lesions (e.g., Forrest Ia). Rebleeding may be an underreported event in the literature; therefore, long-term efficacy must be addressed in the incoming trials. Long-term secondary effects on GI mucosa should also be addressed. Finally, since many conventional hemostatic methods are considerably cheaper, an economic analysis of the use of powders on GI bleeding should also be carried out. Larger trials, which may give response to some of these answers, are eagerly awaited.
Footnotes
P- Reviewer: Fallone CA, Hokama A, Kate V, Li YY, Thomopoulos KC S- Editor: Ji FF L- Editor: Roemmele A E- Editor: Lu YJ
References
- 1.Lewis JD, Bilker WB, Brensinger C, Farrar JT, Strom BL. Hospitalization and mortality rates from peptic ulcer disease and GI bleeding in the 1990s: relationship to sales of nonsteroidal anti-inflammatory drugs and acid suppression medications. Am J Gastroenterol. 2002;97:2540–2549. doi: 10.1111/j.1572-0241.2002.06037.x. [DOI] [PubMed] [Google Scholar]
- 2.Hearnshaw SA, Logan RF, Lowe D, Travis SP, Murphy MF, Palmer KR. Acute upper gastrointestinal bleeding in the UK: patient characteristics, diagnoses and outcomes in the 2007 UK audit. Gut. 2011;60:1327–1335. doi: 10.1136/gut.2010.228437. [DOI] [PubMed] [Google Scholar]
- 3.Pérez Aisa A, Nuevo J, López Morante AA, González Galilea A, Martin de Argila C, Aviñoa Arreal D, Feu F, Borda Celaya F, Gisbert JP, Pérez Roldan F, et al. [Current management of nonvariceal upper gastrointestinal bleeding in Spain] Gastroenterol Hepatol. 2012;35:468–475. doi: 10.1016/j.gastrohep.2012.02.007. [DOI] [PubMed] [Google Scholar]
- 4.Hreinsson JP, Gumundsson S, Kalaitzakis E, Björnsson ES. Lower gastrointestinal bleeding: incidence, etiology, and outcomes in a population-based setting. Eur J Gastroenterol Hepatol. 2013;25:37–43. doi: 10.1097/MEG.0b013e32835948e3. [DOI] [PubMed] [Google Scholar]
- 5.Lanas A, García-Rodríguez LA, Polo-Tomás M, Ponce M, Alonso-Abreu I, Perez-Aisa MA, Perez-Gisbert J, Bujanda L, Castro M, Muñoz M, et al. Time trends and impact of upper and lower gastrointestinal bleeding and perforation in clinical practice. Am J Gastroenterol. 2009;104:1633–1641. doi: 10.1038/ajg.2009.164. [DOI] [PubMed] [Google Scholar]
- 6.Rockey DC. Lower gastrointestinal bleeding. Gastroenterology. 2006;130:165–171. doi: 10.1053/j.gastro.2005.11.042. [DOI] [PubMed] [Google Scholar]
- 7.Laine L, McQuaid KR. Endoscopic therapy for bleeding ulcers: an evidence-based approach based on meta-analyses of randomized controlled trials. Clin Gastroenterol Hepatol. 2009;7:33–47; quiz 1-2. doi: 10.1016/j.cgh.2008.08.016. [DOI] [PubMed] [Google Scholar]
- 8.Green BT, Rockey DC. Lower gastrointestinal bleeding--management. Gastroenterol Clin North Am. 2005;34:665–678. doi: 10.1016/j.gtc.2005.10.001. [DOI] [PubMed] [Google Scholar]
- 9.Gralnek IM, Barkun AN, Bardou M. Management of acute bleeding from a peptic ulcer. N Engl J Med. 2008;359:928–937. doi: 10.1056/NEJMra0706113. [DOI] [PubMed] [Google Scholar]
- 10.Giday SA, Kim Y, Krishnamurty DM, Ducharme R, Liang DB, Shin EJ, Dray X, Hutcheon D, Moskowitz K, Donatelli G, et al. Long-term randomized controlled trial of a novel nanopowder hemostatic agent (TC-325) for control of severe arterial upper gastrointestinal bleeding in a porcine model. Endoscopy. 2011;43:296–299. doi: 10.1055/s-0030-1256125. [DOI] [PubMed] [Google Scholar]
- 11.Sung JJ, Luo D, Wu JC, Ching JY, Chan FK, Lau JY, Mack S, Ducharme R, Okolo P, Canto M, et al. Early clinical experience of the safety and effectiveness of Hemospray in achieving hemostasis in patients with acute peptic ulcer bleeding. Endoscopy. 2011;43:291–295. doi: 10.1055/s-0030-1256311. [DOI] [PubMed] [Google Scholar]
- 12.Cox ED, Schreiber MA, McManus J, Wade CE, Holcomb JB. New hemostatic agents in the combat setting. Transfusion. 2009;49 Suppl 5:248S–255S. doi: 10.1111/j.1537-2995.2008.01988.x. [DOI] [PubMed] [Google Scholar]
- 13.Holster ILDM MP, Ducharme R, Kuipers EJ, Tjwa ET. In vivo examination of the effects of the hemostatic powder (HemosprayTM) on coagulation and thrombus formation in humans. Gastrointest Endosc. 2012:AB240. [Google Scholar]
- 14.AMP technology. Polymer Solution for hemostasis. 2011. Available from: http: //endoclot.com/technology.html. Last accessed: May 2014. [Google Scholar]
- 15.Wang Y, Xu M, Dong H, Liu Y, Zhao P, Niu W, Xu D, Ji X, Xing C, Lu D, et al. Effects of PerClot® on the healing of full-thickness skin wounds in rats. Acta Histochem. 2012;114:311–317. doi: 10.1016/j.acthis.2011.06.012. [DOI] [PubMed] [Google Scholar]
- 16.Beyazit Y, Kurt M, Kekilli M, Goker H, Haznedaroglu IC. Evaluation of hemostatic effects of Ankaferd as an alternative medicine. Altern Med Rev. 2010;15:329–336. [PubMed] [Google Scholar]
- 17.Haznedaroglu BZ, Haznedaroglu IC, Walker SL, Bilgili H, Goker H, Kosar A, Aktas A, Captug O, Kurt M, Ozdemir O, et al. Ultrastructural and morphological analyses of the in vitro and in vivo hemostatic effects of Ankaferd Blood Stopper. Clin Appl Thromb Hemost. 2010;16:446–453. doi: 10.1177/1076029609343706. [DOI] [PubMed] [Google Scholar]
- 18.Goker H, Haznedaroglu IC, Ercetin S, Kirazli S, Akman U, Ozturk Y, Firat HC. Haemostatic actions of the folkloric medicinal plant extract Ankaferd Blood Stopper. J Int Med Res. 2008;36:163–170. doi: 10.1177/147323000803600121. [DOI] [PubMed] [Google Scholar]
- 19.Esmon CT, Esmon NL. Regulatory mechanisms in hemostasis. In: Hoffman RBEJ, Silberstein LE, Heslop HE, Wietz JI, Anastasi J, et al., editors. Hematology: basic principles and practice. 6th ed. Eselvier; 2013. [Google Scholar]
- 20.Chen YI, Barkun AN, Soulellis C, Mayrand S, Ghali P. Use of the endoscopically applied hemostatic powder TC-325 in cancer-related upper GI hemorrhage: preliminary experience (with video) Gastrointest Endosc. 2012;75:1278–1281. doi: 10.1016/j.gie.2012.02.009. [DOI] [PubMed] [Google Scholar]
- 21.Leblanc S, Vienne A, Dhooge M, Coriat R, Chaussade S, Prat F. Early experience with a novel hemostatic powder used to treat upper GI bleeding related to malignancies or after therapeutic interventions (with videos) Gastrointest Endosc. 2013;78:169–175. doi: 10.1016/j.gie.2013.03.006. [DOI] [PubMed] [Google Scholar]
- 22.Holster IL, Kuipers EJ, Tjwa ET. Hemospray in the treatment of upper gastrointestinal hemorrhage in patients on antithrombotic therapy. Endoscopy. 2013;45:63–66. doi: 10.1055/s-0032-1325793. [DOI] [PubMed] [Google Scholar]
- 23.Tarantino I, Barresi L, Granata A, Curcio G, Traina M. Hemospray for arterial hemorrhage following endoscopic ultrasound-guided pseudocyst drainage. Endoscopy. 2014;46 Suppl 1:E71. doi: 10.1055/s-0033-1359164. [DOI] [PubMed] [Google Scholar]
- 24.Curcio G, Granata A, Traina M. Hemospray for multifocal bleeding following ultra-low rectal endoscopic submucosal dissection. Dig Endosc. 2014;26:606–607. doi: 10.1111/den.12301. [DOI] [PubMed] [Google Scholar]
- 25.Holster IL, Poley JW, Kuipers EJ, Tjwa ET. Controlling gastric variceal bleeding with endoscopically applied hemostatic powder (Hemospray™) J Hepatol. 2012;57:1397–1398. doi: 10.1016/j.jhep.2012.07.024. [DOI] [PubMed] [Google Scholar]
- 26.Ibrahim M, El-Mikkawy A, Mostafa I, Devière J. Endoscopic treatment of acute variceal hemorrhage by using hemostatic powder TC-325: a prospective pilot study. Gastrointest Endosc. 2013;78:769–773. doi: 10.1016/j.gie.2013.07.037. [DOI] [PubMed] [Google Scholar]
- 27.Stanley AJ, Smith LA, Morris AJ. Use of hemostatic powder (Hemospray) in the management of refractory gastric variceal hemorrhage. Endoscopy. 2013;45 Suppl 2:E86–E87. doi: 10.1055/s-0032-1326258. [DOI] [PubMed] [Google Scholar]
- 28.Smith LA, Morris AJ, Stanley AJ. The use of hemospray in portal hypertensive bleeding; a case series. J Hepatol. 2014;60:457–460. doi: 10.1016/j.jhep.2013.10.008. [DOI] [PubMed] [Google Scholar]
- 29.Granata A, Curcio G, Azzopardi N, Barresi L, Tarantino I, Traina M. Hemostatic powder as rescue therapy in a patient with H1N1 influenza with uncontrolled colon bleeding. Gastrointest Endosc. 2013;78:451. doi: 10.1016/j.gie.2013.07.010. [DOI] [PubMed] [Google Scholar]
- 30.Holster IL, Brullet E, Kuipers EJ, Campo R, Fernández-Atutxa A, Tjwa ET. Hemospray treatment is effective for lower gastrointestinal bleeding. Endoscopy. 2014;46:75–78. doi: 10.1055/s-0033-1344988. [DOI] [PubMed] [Google Scholar]
- 31.Kratt T, Lange J, Königsrainer A, Malek N, Adam P, Bösmüller H, Goetz M. Successful Hemospray treatment for recurrent diclofenac-induced severe diffuse lower gastrointestinal bleeding avoiding the need for colectomy. Endoscopy. 2014;46 Suppl 1:E173–E174. doi: 10.1055/s-0034-1365100. [DOI] [PubMed] [Google Scholar]
- 32.Smith LA, Stanley AJ, Bergman JJ, Kiesslich R, Hoffman A, Tjwa ET, Kuipers EJ, von Holstein CS, Oberg S, Brullet E, et al. Hemospray Application in Nonvariceal Upper Gastrointestinal Bleeding: Results of the Survey to Evaluate the Application of Hemospray in the Luminal Tract. J Clin Gastroenterol. 2013:Dec 10; Epub ahead of print. doi: 10.1097/MCG.0000000000000054. [DOI] [PubMed] [Google Scholar]
- 33.Sulz MC, Frei R, Meyenberger C, Bauerfeind P, Semadeni GM, Gubler C. Routine use of Hemospray for gastrointestinal bleeding: prospective two-center experience in Switzerland. Endoscopy. 2014;46:619–624. doi: 10.1055/s-0034-1365505. [DOI] [PubMed] [Google Scholar]
- 34.Huang R, Pan Y, Hui N, Guo X, Zhang L, Wang X, Zhang R, Luo H, Zhou X, Tao Q, et al. Polysaccharide hemostatic system for hemostasis management in colorectal endoscopic mucosal resection. Dig Endosc. 2014;26:63–68. doi: 10.1111/den.12054. [DOI] [PubMed] [Google Scholar]
- 35.Liu Z. EndoClot for preventing rebleeding after endoscopic mucosal resection (EMR) 2013. Available from: http: //clinicaltrials.gov/show/NCT01735786. Last accessed: may 2014. [Google Scholar]
- 36.Liu Z. EndoClot for Hemostasis and preventing post-procedure bleeding after endoscopic mucosal resection (EMR) 2013. Available from: http: //clinicaltrials.gov/show/NCT01496781. Accessed on May 2014. [Google Scholar]
- 37.Halkerston K, Evans J, Ismail D, Catnach S, Chaudhary R, Fullard M, King A, Leahy A. Early clinical experience of EndoclotTM in the treatment of acute gastro-intestinal bleeding. Gut. 2013;62(Suppl 1):A149. [Google Scholar]
- 38.Müller-Gerbes D, Beek A, Dormann A. Erfahrungen mit EndoClotTM PHS bei blutungen im oberen gastrointestinaltrakt. Z Gastroenterol. 2013;51:K457. [Google Scholar]
- 39.Sörensen AS, Kalmar G, Schmidt A, Caca K. Endoskopische bluststillung mit absorbierbaren modifizierten polymeren (AMP; EndoClotTM)-erste Erfahrungen im oberen gastrointestinaltrakt. Z Gastroenterol. 2013;51:K270. [Google Scholar]
- 40.Bilgili H, Kosar A, Kurt M, Onal IK, Goker H, Captug O, Shorbagi A, Turgut M, Kekilli M, Kurt OK, et al. Hemostatic efficacy of Ankaferd Blood Stopper in a swine bleeding model. Med Princ Pract. 2009;18:165–169. doi: 10.1159/000204344. [DOI] [PubMed] [Google Scholar]
- 41.Cipil HS, Kosar A, Kaya A, Uz B, Haznedaroglu IC, Goker H, Ozdemir O, Koroglu M, Kirazli S, Firat HC. In vivo hemostatic effect of the medicinal plant extract Ankaferd Blood Stopper in rats pretreated with warfarin. Clin Appl Thromb Hemost. 2009;15:270–276. doi: 10.1177/1076029608329578. [DOI] [PubMed] [Google Scholar]
- 42.Kandemir O, Buyukates M, Kandemir NO, Aktunc E, Gul AE, Gul S, Turan SA. Demonstration of the histopathological and immunohistochemical effects of a novel hemostatic agent, Ankaferd Blood Stopper, on vascular tissue in a rat aortic bleeding model. J Cardiothorac Surg. 2010;5:110. doi: 10.1186/1749-8090-5-110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kosar A, Cipil HS, Kaya A, Uz B, Haznedaroglu IC, Goker H, Ozdemir O, Ercetin S, Kirazli S, Firat HC. The efficacy of Ankaferd Blood Stopper in antithrombotic drug-induced primary and secondary hemostatic abnormalities of a rat-bleeding model. Blood Coagul Fibrinolysis. 2009;20:185–190. doi: 10.1097/MBC.0b013e32831c4cb0. [DOI] [PubMed] [Google Scholar]
- 44.Ozaslan E, Purnak T, Yildiz A, Haznedaroglu IC. The effect of a new hemostatic agent for difficult cases of non-variceal gastrointestinal bleeding: Ankaferd blood stopper. Hepatogastroenterology. 2010;57:191–194. [PubMed] [Google Scholar]
- 45.Yarali N, Oruc M, Bay A, Dalgic B, Bozkaya IO, Arıkoglu T, Kara A, Tunc B. A new hemostatic agent--Ankaferd blood stopper: management of gastrointestinal bleeding in an infant and other experiences in children. Pediatr Hematol Oncol. 2010;27:592–596. doi: 10.3109/08880018.2010.503337. [DOI] [PubMed] [Google Scholar]
- 46.Kurt M, Akdogan M, Onal IK, Kekilli M, Arhan M, Shorbagi A, Aksu S, Kurt OK, Haznedaroglu IC. Endoscopic topical application of Ankaferd Blood Stopper for neoplastic gastrointestinal bleeding: A retrospective analysis. Dig Liver Dis. 2010;42:196–199. doi: 10.1016/j.dld.2009.05.006. [DOI] [PubMed] [Google Scholar]
- 47.Zulfikar OB, Emiroglu HH, Kebudi R. Nasogastric application of topical Ankaferd Blood Stopper for bleeding from primary esophageal adenocarcinoma in a child with disseminated intravascular coagulation. Dig Liver Dis. 2011;43:247–248. doi: 10.1016/j.dld.2010.10.002. [DOI] [PubMed] [Google Scholar]
- 48.Turhan N, Kurt M, Shorbagi A, Akdogan M, Haznedaroglu IC. Topical Ankaferd Blood Stopper administration to bleeding gastrointestinal carcinomas decreases tumor vascularization. Am J Gastroenterol. 2009;104:2874–2877. doi: 10.1038/ajg.2009.431. [DOI] [PubMed] [Google Scholar]
- 49.Beyazit Y, Köklü S, Akbal E, Kurt M, Kekilli M, Haznedaroglu IC. Successful treatment of endoscopic sphincterotomy-induced early hemorrhage with application of Ankaferd Blood Stopper. Gastrointest Endosc. 2010;72:1325–1326. doi: 10.1016/j.gie.2010.03.1119. [DOI] [PubMed] [Google Scholar]
- 50.Kurt M, Onal I, Akdogan M, Kekilli M, Arhan M, Sayilir A, Oztas E, Haznedaroglu I. Ankaferd Blood Stopper for controlling gastrointestinal bleeding due to distinct benign lesions refractory to conventional antihemorrhagic measures. Can J Gastroenterol. 2010;24:380–384. doi: 10.1155/2010/896819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Karaman A, Torun E, Gürsoy S, Yurci A, Ozbakir O. Efficacy of Ankaferd Blood Stopper in postpolypectomy bleeding. J Altern Complement Med. 2010;16:1027–1028. doi: 10.1089/acm.2010.0089. [DOI] [PubMed] [Google Scholar]
- 52.Tuncer I, Doganay L, Ozturk O. Instant control of fundal variceal bleeding with a folkloric medicinal plant extract: Ankaferd Blood Stopper. Gastrointest Endosc. 2010;71:873–875. doi: 10.1016/j.gie.2009.08.021. [DOI] [PubMed] [Google Scholar]
- 53.Ozaslan E, Purnak T, Yildiz A, Haznedaroglu IC. Bleeding due to slippage of elastic band during variceal ligation: successful use of Ankaferd blood stopper. Indian J Gastroenterol. 2010;29:166–168. doi: 10.1007/s12664-010-0043-y. [DOI] [PubMed] [Google Scholar]
- 54.Ozaslan E, Purnak T, Ozyigit G, Akyol F, Yildiz A, Haznedaroglu IC. No prolonged effect of Ankaferd Blood Stopper on chronic radiation proctitis. Endoscopy. 2010;42 Suppl 2:E271–E272. doi: 10.1055/s-0030-1255773. [DOI] [PubMed] [Google Scholar]
- 55.Ibis M, Kurt M, Onal IK, Haznedaroglu IC. Successful management of bleeding due to solitary rectal ulcer via topical application of Ankaferd blood stopper. J Altern Complement Med. 2008;14:1073–1074. doi: 10.1089/acm.2008.0314. [DOI] [PubMed] [Google Scholar]
- 56.Gungor G, Goktepe MH, Biyik M, Polat I, Tuna T, Ataseven H, Demir A. Efficacy of ankaferd blood stopper application on non-variceal upper gastrointestinal bleeding. World J Gastrointest Endosc. 2012;4:556–560. doi: 10.4253/wjge.v4.i12.556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Moosavi S, Chen YI, Barkun AN. TC-325 application leading to transient obstruction of a post-sphincterotomy biliary orifice. Endoscopy. 2013;45 Suppl 2:E130. doi: 10.1055/s-0032-1326370. [DOI] [PubMed] [Google Scholar]
- 58.Kheirabadi BS, Mace JE, Terrazas IB, Fedyk CG, Estep JS, Dubick MA, Blackbourne LH. Safety evaluation of new hemostatic agents, smectite granules, and kaolin-coated gauze in a vascular injury wound model in swine. J Trauma. 2010;68:269–278. doi: 10.1097/TA.0b013e3181c97ef1. [DOI] [PubMed] [Google Scholar]
- 59.Giday S, Van Alstine W, Van Vleet J, Ducharme R, Brandner E, Florea M, Johnston K, Negron-Garcia J, Ringenberger K. Safety analysis of a hemostatic powder in a porcine model of acute severe gastric bleeding. Dig Dis Sci. 2013;58:3422–3428. doi: 10.1007/s10620-013-2846-z. [DOI] [PubMed] [Google Scholar]


