Abstract
Introduction:
Recent research on the association between delusions and violence has suggested complex and differing pathways. Furthermore, it has been emphasized that temporal proximity is fundamental when investigating these relationships. We reanalyzed data from the MacArthur Violence Risk Assessment Study utilizing a different methodological approach to investigate associations between specific delusions and violence.
Methods:
Longitudinal study of 1136 male and female civil psychiatric inpatients after discharge. Delusions, affect due to delusions, and violence were measured at baseline and in 5 follow-up assessments. Serious violence was established using the MacArthur Community Violence Interview. Logistic mixed-effect models for repeated measures were performed.
Results:
A “prospective” model confirmed previous findings that delusions do not predict later violence. However, reanalysis, considering temporal proximity, indicated a relationship between specific delusions and outcome including: being spied upon (adjusted OR [AOR] = 1.62, 95% CI = 1.06–2.47, P = .027), being followed (AOR = 1.90, 95% CI = 1.29–2.80, P = .001), being plotted against (AOR = 1.70, 95% CI = 1.14–2.52, P = .009), being under control of person/force (AOR = 1.92, 95% CI = 1.24–2.97, P = .003), thought insertion (AOR = 1.63, 95% CI = 1.00–2.66, P = .048), and having special gifts/powers (AOR = 1.95, 95% CI = 1.31–2.92, P = .001). All these delusions were associated with angry affect (P < .05). Inclusion of anger in the model significantly attenuated the main effects (except grandiose delusions), indicating an indirect pathway.
Conclusions:
Temporal proximity is crucial when investigating relationships between delusions and violence. Anger due to delusions is the key factor in this pathway. Our findings have important implications for identification of psychotic patients at risk for violent behavior and, most importantly, management of their risk.
Key words: psychosis, anger, delusions implying threat, indirect pathway, management of risk for violence
Introduction
Key findings from the MacArthur Violence Risk Assessment Study (MVRAS),1 which showed that delusions do not predict violence among recently discharged psychiatric patients, had a profound impact on research in this field. Furthermore, several epidemiological surveys and case register studies found that, at the population level, psychosis showed little or no association with violence,2–5 which was explained almost entirely by comorbid substance misuse, or psychosocial adversity and environmental stressors more common in the lives of persons with severe mental illness.3
More recently, researchers have reevaluated associations between violence and psychosis and observed contrasting findings according to whether the aim is to identify (statistical) predictors of violence or to establish relationships that allow consideration of causality. Reanalysis of data from the National Epidemiologic Survey of Alcohol and Related Conditions revealed a positive association between major mental illness and violence, demonstrating that temporal proximity between dependent and independent variables is crucial when investigating these relationships.6 Predictors derived from studies measuring symptoms or diagnoses at various points over the lifetime and comparing them with self-report or criminal records over extended periods cannot establish valid associations. Furthermore, because acute psychotic symptoms may present for relatively short periods, predictors which are identified over the lifespan may not be specific for psychosis and may apply equally to incidents of violence among the general (nonpsychotic) population.
Studies taking into consideration temporal proximity between exposure and outcome have confirmed associations between delusions and violence, albeit of a complex nature and involving more than 1 pathway. Findings from the Clinical Antipsychotic Trials of Interventions Effectiveness Study showed that hallucinations accompanied by delusional interpretations, and delusional thinking associated with suspiciousness and feelings of persecution, were related to serious violence among patients with schizophrenia.7 Anger due to delusional beliefs was the key factor explaining the association between first episode psychosis and violence in a UK study.8 Three highly prevalent delusions of persecution, being spied upon, and conspiracy demonstrated associations with serious violence, but only when the delusions made the patients angry. Anger is intrinsically and reciprocally related to threat perception and drives violent behavior in the absence of self-regulatory controls.9 Actively paranoid patients are more likely to misidentify neutral facial expressions as angry than those whose symptoms are not active.10 It appears that a subset of delusional beliefs lead to “tense situations,”11 and that angry affect is an important component in a causal model of mental illness and violence.
When MVRAS1 was conducted, emphasis was placed on a “prospective” approach to overcome methodological shortcomings of previous research on the relationship between delusions and violence. To investigate direct pathways, delusional beliefs assessed in the past 10 weeks were modeled as predictors for serious violence in the following 10 weeks. However, based on the relevance of temporal proximity when studying these associations, there are compelling reasons to reexamine the MVRAS findings. Furthermore, confirmation is needed as to whether angry affect is an important mediator in the pathway between delusions and violence in a clinical sample with different diagnostic composition, and where only a minority of patients were in their first episode. We therefore carried out a statistical reanalysis of MVRAS data, utilizing a different approach, to examine associations between delusions and serious violence to investigate: (1) whether there is a direct pathway; (2) whether associations are confounded/mediated by diagnosis, trait anger, or affect due to delusional belief; and (3) which delusional beliefs have the strongest effect on outcome (serious violence).
Methods
Study Design and Sample
Data for this study were collected as part of MVRAS. A detailed description has been given elsewhere.1,12,13 In brief, MVRAS is a longitudinal study of 1136 male and female civil patients from 3 acute inpatient facilities (Western Psychiatric Institute and Clinic, Pittsburgh, PA; Western Missouri Mental Health Center, Kansas City, MO; and Worcester State Hospital and the University of Massachusetts Medical Center, Worcester, MA) conducted between 1992 and 1995. After complete description of the study to the participants, written informed consent was obtained.
Procedures
The sample was composed using a stratified random sampling design (stratification by gender, ethnicity, and age). Within each stratum, a random sample of eligible patients were approached for inclusion in the study. Continuous enrollment occurred until a quota for each stratum was reached.
Patients were interviewed at baseline and then recontacted in the community by the research interviewers and interviewed at 5 time points (every 10 weeks) in the year following discharge. A collateral informant was also interviewed on the same schedule. At each time point, data were collected to determine the occurrence of delusions, affect due to delusions, and serious violence occurring during the previous 10 weeks. Of the 1136 patients entering the study, 859 were reinterviewed at time 1 (75.6%), 818 at time 2 (72.0%), 756 at time 3 (66.6%), 739 at time 4 (65.1%), and 726 at time 5 (63.9%).
A set of questions taken mostly from the Diagnostic Interview Schedule14 was administered at baseline and each of the 5 follow-up interviews to determine whether a patient had been delusional within the previous 10-week period. Positive answers to these questions were then judged by the interviewers as to whether they constituted possible or definite delusional beliefs (“yes”) or overvalued ideas (“no”). As in the original study,1 delusions only occurring in the context of substance use were included. Possible/definite delusions investigated in this study are listed in table 2.
Table 2.
Delusions and Serious Violence
| Delusion of: | Adjusteda | Adjustedb | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P | OR | 95% CI | P | |
| Being spied upon | 1.40 | 0.96–2.04 | .077 | 1.62 | 1.06–2.47 | .027 |
| Being followed | 1.61 | 1.11–2.33 | .013 | 1.90 | 1.29–2.80 | .001 |
| Being tested/experimented on | 1.04 | 0.60–1.79 | .896 | 1.14 | 0.65–2.02 | .642 |
| Being plotted against | 1.30 | 0.89–1.91 | .181 | 1.70 | 1.14–2.52 | .009 |
| Having mind read | 0.54 | 0.29–1.02 | .059 | 0.59 | 0.30–1.17 | .130 |
| Being able to hear others’ thoughts | 1.52 | 0.91–2.54 | .113 | 2.07 | 1.23–3.49 | .006 |
| Others’ being able to hear R’s thoughts | 0.88 | 0.51–1.52 | .637 | 1.17 | 0.67–2.06 | .576 |
| Being under control of person/force | 1.50 | 0.98–2.30 | .065 | 1.92 | 1.24–2.97 | .003 |
| Thought insertion | 1.28 | 0.79–2.05 | .317 | 1.63 | 1.00–2.66 | .048 |
| Thoughts could be stolen | 0.96 | 0.49–1.88 | .896 | 1.26 | 0.63–2.49 | .515 |
| Being send messages through TV/radio | 0.89 | 0.54–1.46 | .645 | 1.11 | 0.66–1.87 | .686 |
| Strange forces working on R | 1.33 | 0.77–2.32 | .308 | 1.84 | 1.05–3.22 | .034 |
| Worthlessness/guilt | 0.85 | 0.49–1.48 | .569 | 1.13 | 0.62–2.03 | .693 |
| Having special gifts/powers | 1.57 | 1.07–2.32 | .023 | 1.95 | 1.31–2.92 | .001 |
| Body parts have changed/not working | 1.15 | 0.49–2.68 | .752 | 1.64 | 0.69–3.87 | .264 |
aAdjusted for the effects of time.
bAdjusted for the effects of time, drug and alcohol use at each time point, age, gender, ethnicity, socioeconomic status, primary diagnosis at T0, psychopathy, length of illness before baseline admission, number of previous hospitalizations before baseline admission.
The MacArthur-Maudsley Assessment of Delusions Schedule (MMADS)13,15 was also administered at baseline and at each of the 5 follow-up interviews to assess affect due to delusions occurring within the previous 10-week period. The MMADS measures elation, depression, fear, anxiety, and anger due to delusions, which were coded as either “present” or “absent.” Further information on the MMADS and its psychometric properties have been reported elsewhere.13
Primary diagnoses were established at baseline according to the Diagnostic and Statistical Manual of Mental Disorders, Third Revised Edition (DSM-III-R) Checklist16 based on chart diagnosis or the Structured Clinical Interview for DSM-III-R personality disorders17 when no eligible axis I diagnosis was present. Checklist diagnoses corresponded to a chart diagnosis in 85.7% of the cases and discrepant diagnoses were resolved by a consultant psychiatrist at each study site. Psychopathy and trait anger were also assessed at baseline using the Psychopathy Checklist: Screening Version18 and the Novaco Anger Scale,9 respectively. We used the recommended cutoff of 18+ to determine a diagnosis of psychopathy and the total score from the Novaco Anger Scale to determine the level of trait anger.
Outcome
At baseline and each of the 5 follow-up interviews, study participants and collaterals were asked as to whether the patient had engaged in several categories of aggressive behavior in the previous 10 weeks. This information was supplemented by a review of the patients’ hospitalization and arrest records. As in the original study,1 actions were considered to constitute serious violence if they were (1) batteries that resulted in physical injury or involved the use of a weapon; (2) sexual assaults; or (3) threats made with a weapon in hand. Acts judged to be committed in self-defense were not counted as violent behavior.
Statistical Analyses
In order to take advantage of the longitudinal study design, multilevel modeling was applied. These models account for the dependence of data collected longitudinally by modeling the relatedness of repeated measurement within the same individual as random effects. Unlike other approaches, such as ANOVA, mixture models do not require that data are complete for individuals at each time point or imputation of data which may result in bias.19 By making use of all available data, multilevel models are therefore particularly powerful in longitudinal studies where individuals are often lost to follow-up.
Logistic mixed models were used to investigate associations between delusions and affect related to delusions, and delusions and violence occurring within the same follow-up period. Data from all 6 study periods were included in the analyses: baseline period (the 2 months before baseline interview) and 5 subsequent follow-up periods, each lasting 10 weeks. In order to estimate the effects of the exposure on outcome over the entire study period regardless of time point, we included time as a covariate. The logistic mixed models therefore provided a single estimate (OR), CIs, and significance value of the relationship between co-occurring delusions and violence and delusions and affect over the entire course of the study.
To ensure temporal proximity between the dependent and independent variables, we investigated the association between predictor and outcome variables observed at baseline and during each follow-up period. However, in order to test the original findings of MVRAS, the same statistical models were run using the “prospective” approach taken in the original study1 to test whether delusions present at the previous time point predicted subsequent violent behavior in the following 10 weeks.
Mixed-effect models are robust to missing data provided that these are either missing at random or variables associated with missingness are included as covariates. In order to identify these covariates, we investigated the relationship between demographic and clinical characteristics measured at baseline and the number of missing values throughout the follow-up period using Poisson regression models. In these analyses, missingness was associated with female gender (incidence rate ratio [IRR] = 0.60, 95% CI = 0.51–0.72, P < .001; inverse), a primary diagnosis of substance use/dependence (IRR = 1.39, 95% CI = 1.08–1.73, P = .009), and psychopathy (IRR = 1.54, 95% CI = 1.21–1.95, P < .001). These covariates were therefore included in all of the adjusted models.
To take into consideration specific sample characteristics, age, ethnicity, socioeconomic status, primary diagnosis, a proxy of length of illness (age at baseline admission minus age at first admission), and number of previous hospitalizations were included as further covariates. Moreover, to account for the effects of alcohol and drug use on outcome, substance abuse/intoxication leading to baseline admission and substance use measured at the 5 follow-up points were included as adjustments.
Mediation analyses were carried out by testing the required triangle associations: statistically significant relationship between (1) independent (delusion) and dependent variable (serious violence); (2) independent and hypothesized mediator variable (temporarily following the independent variable: affect); and (3) mediator and dependent variable. Substantial attenuation in magnitude of effect of the association between a specific delusion and serious violence after covariation of the mediator variable was interpreted as indirect pathway (mediation via associated affect).
All statistical analyses were conducted in STATA version 12.0 (STATACorp). An alpha level of P < .05 was adopted throughout.
Results
Sample Characteristics
At baseline, the mean age of the sample was 29.7 years (SD = 6.2 years, range 18–40). More than half were male (n = 667, 58.7%), and the majority were white (n = 785, 69.1%). Primary diagnoses at admission were nonaffective psychosis (n = 245, 21.6%), affective disorder including depression and bipolar disorder (n = 596, 52.5%), substance abuse/dependence (n = 274, 24.0%), and personality disorder (n = 21, 1.9%). On average, the sample reported 5.7 prior admissions to a psychiatric hospital (SD = 5.8) with a minority being admitted for the first time at baseline (n = 328, 29.4%). The mean time in years between first and current admission was 5.7 years (SD = 6.8 years).
Of the total sample, 328 (28.9%) were deluded at baseline, 189 (22.0%) at time 1, 184 (22.5%) at time 2, 160 (21.2%) at time 3, 137 (18.5%) at time 4, and 136 (18.7%) at time 5. A serious violent act was committed by 198 study participants (17.4%) at baseline, 115 (13.4%) at time 1, 84 (10.3%) at time 2, 52 (6.9%) at time 3, 56 (7.6%) at time 4, and 46 (6.3%) at time 5.
Affect Related to Delusions and Serious Violent Outcome
As shown in table 1, after adjustment for demographic variables and clinical characteristics, elation and anger due to delusions were significantly associated with serious violence and the inclusion of trait anger as further covariate had little effect on the strength of either of these associations. Fear due to delusions was inversely associated with serious violence indicative of a protective effect on violent behavior.
Table 1.
Affect due to Delusions and Serious Violence
| OR | 95% CI | P | |
|---|---|---|---|
| Elation | |||
| Adjusteda + time, other affects | 1.53 | 0.98–2.38 | .061 |
| Adjustedb + demographic and clinical variables | 1.79 | 1.14–2.81 | .011 |
| Adjustedc + anger | 1.82 | 1.16–2.85 | .009 |
| Depression | |||
| Adjusteda + time, other affects | 1.20 | 0.67–2.14 | .532 |
| Adjustedb + demographic and clinical variables | 1.20 | 0.67–2.16 | .543 |
| Adjustedc + anger | 1.22 | 0.68–2.20 | .503 |
| Fear | |||
| Adjusteda + time, other affects | 0.58 | 0.34–0.99 | .044 |
| Adjustedb + demographic and clinical variables | 0.60 | 0.35–1.02 | .061 |
| Adjustedc + anger | 0.55 | 0.32–0.94 | .030 |
| Anxiety | |||
| Adjusteda + time, other affects | 1.06 | 0.57–1.95 | .858 |
| Adjustedb + demographic and clinical variables | 1.18 | 0.63–2.19 | .606 |
| Adjustedc + anger | 1.20 | 0.64–2.23 | .570 |
| Anger | |||
| Adjusteda + time, other affects | 2.04 | 1.16–3.59 | .013 |
| Adjustedb + demographic and clinical variables | 2.28 | 1.28–4.06 | .005 |
| Adjustedc + anger | 2.13 | 1.19–3.81 | .011 |
Note: Participants who were not deluded at follow-up were coded “0” on the MMADS affect variables.
aTo test for independent effects of affect, all 5 variables were entered simultaneously. Furthermore, the model was adjusted for the effects of time.
bAdditional adjustments included drug and alcohol use at each time point, age, gender, ethnicity, socioeconomic status, primary diagnosis at baseline (T0), psychopathy, length of illness before baseline admission, number of previous hospitalizations before baseline admission.
cIn the final model trait anger measured at T0 was included as additional covariate.
Content of Delusions and Serious Violence
As can be seen in table 2, more than half of the 15 delusions under study demonstrated significant main effects on outcome. These included delusions of being spied upon, being followed, being plotted against, being able to hear others’ thoughts, being under the control of a person/force, thought insertion, strange forces working on R, and having special gifts/powers.
The majority of these associations was negatively confounded by demographic and clinical characteristics and demonstrated a significant relationship with outcome only after covariation of additional variables. This negative confounding was largely the result of the association of these delusions, primary diagnosis, and violence. Each of these was significantly (P <.05) related with a diagnosis of psychosis (ie, less prevalent in those with an alternative diagnosis) with a decreased risk of violence in those with primary diagnosis of psychotic disorder.
Affect and Delusions
Nine of the 15 delusions demonstrated a significant association with anger (P < .05) before and after adjustment for alcohol/drug use at each time point, age, gender, ethnicity, socioeconomic status, primary diagnosis at baseline, psychopathy, length of illness before baseline admission, and number of previous hospitalizations.
These included delusions of being spied upon (adjusted OR [AOR] = 6.68, 95% CI = 3.83–11.65), being followed (AOR = 5.81, 95% CI = 3.38–9.99), being tested/experimented on (AOR = 2.43, 95% CI = 1.21–4.88), being plotted against (AOR = 3.97, 95% CI = 2.31–6.82), being under control of person/force (AOR = 5.15, 95% CI = 2.80–9.46), thought insertion (AOR = 2.66, 95% CI = 1.36–5.20), being send messages through TV/radio (AOR = 0.37, 95% CI = 0.19–0.74; inverse), worthlessness/guilt (AOR = 29.4, 95% CI = 15.35–56.31), and having special gifts/powers (AOR = 2.98, 95% CI = 1.67–5.30).
Only 2 delusions were significantly associated with elation: being send messages through TV/radio (AOR = 4.74, 95% CI = 2.38–9.46) and having special gifts/powers (AOR = 65.42, 95% CI = 35.05–122.10). The associations were statistically significant (P < .05) before and after adjustment.
Are Effects of Delusions on Violence Mediated by Angry or Elated Affect?
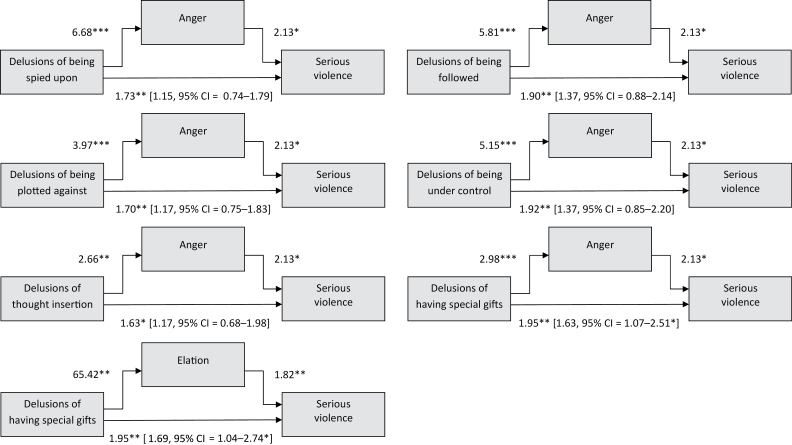
As depicted in figure 1, 6 delusions were tested in mediation analyses due to their significant relationship with both anger and serious violence. After inclusion of anger as covariate, there was substantial attenuation in the magnitude of effect of delusions of being spied upon, being followed, being plotted against, being under external control, and thought insertion on violent outcome, with the main effects of these delusions no longer statistically significant (AORs and 95% CIs are in brackets). These findings are not supportive of the assumption of a direct pathway between these delusions and violence but suggest an indirect pathway, where the association is mediated via angry affect due to delusions. After adjustment for anger, the relationship between delusions of having special gifts/powers and serious violence was still significant, with some attenuation of adjusted OR, suggestive of a direct pathway.
Fig. 1.
Delusions, affect, and serious violence. *P < .05, **P < .01, ***P < .001.
Only 1 specific delusion (having special gifts/powers; see figure 1) was significantly associated with both elation due to delusions and violent outcome. This association remained significant following adjustment for elated affect, indicating a direct pathway from this delusion to serious violence.
Do Delusions Predict Serious Violence?
None of the delusional beliefs under study predicted subsequent violent outcome (P > .10) using a “prospective” method to investigate whether these symptoms in the previous 10 weeks predicted violence in the subsequent 10 weeks. Furthermore, after adjustment, none of the 5 affects due to delusional beliefs were significantly associated with subsequent violent behavior (P > .05).
Discussion
We confirmed the original findings of MVRAS,1 reaffirming that delusions do not statistically predict subsequent serious violent behavior among discharged psychiatric patients. However, when we reanalyzed the data taking into account the temporal proximity between delusions and violent outcome, we revealed strong associations with delusional beliefs implying threat to the individual. As previously observed,8 these associations were complex and involved more than 1 pathway. We further confirmed strong associations between anger due to delusions and violence. This effect remained significant after adjusting for demographic characteristics, comorbid psychopathology (including alcohol/drug use disorders), and substance use at each follow-up typically associated with violence in the general population, which attenuates associations with diagnostic categories and violence.2–5 In addition, we excluded the possibility that our findings were confounded by trait anger.
No associations were found between serious violent behavior and affective states of depression and anxiety. Fear due to delusions had a protective effect, which may have been due to social withdrawal from potentially violent encounters and accentuated harm avoidance in these patients on the basis of their delusional beliefs. Elation was significantly associated with serious violence after adjustment, indicative of negative confounding due to the demographic and clinical characteristics of the sample.
Following adjustments, more than half of the delusions resulted in angry affect, including being spied upon, being followed, being tested/experimented on, being plotted against, being under control of a person/force, having thoughts inserted, worthlessness/guilt, and having special powers. The majority of these delusional beliefs implied threat and/or actual harm for the individual. It could be hypothesized that level of self-esteem and attributional styles are contributing/mediating factors in this association.20 Future research is necessary to establish this. The majority of delusions of thought/mind interference was not associated with anger due to delusional content. Only 2 delusions were associated with feelings of elation: being sent messages through the TV/radio and having special gifts/powers.
Pathways From Delusions to Serious Violent Behavior
Consistent with what would be expected in a causal relationship, we found that angry affect was the intermediate variable in the pathway from 5 delusions to serious violence: being spied upon, being followed, being plotted against, having thoughts inserted, and being under external control. These delusions imply threat and/or harm to the individual and the findings are almost identical to a recent study, where threat delusions of being spied upon, persecutory delusions, and delusions of conspiracy were also mediated by anger due to delusional content on the pathway to serious violence.8
We identified a further pathway between having special gifts/powers and serious violence. This same delusion, when associated with elation or anger, showed a direct pathway to serious violence irrespective of affect due to the belief.
Methodological Considerations
In contrast to earlier analyses of MVRAS,1 we found strong associations between specific delusions and violence in the current study. Several methodological reasons may explain these differences. First, in the original study, the data were analyzed using a “prospective” approach, ensuring temporal ordering of delusions and violence, but neglecting temporal proximity. Of those individuals diagnosed as deluded at baseline, approximately half were no longer deluded at the first follow-up assessment. This was to be expected considering that this sample was treated and followed up after discharge. Furthermore, about 11% of those nondeluded at baseline reported the emergence of delusions when assessed at first follow-up. It is therefore unsurprising that no significant association was found between delusions and violence because in a substantial number of patients the predictor variable (delusion) was no longer present when the violent incidents were measured.
Secondly, we disaggregated the combined categories of delusions originally used1 and carried out analyses on individual delusional beliefs. This allowed a more in-depth analyses of specific delusions and may have further contributed to the contrasting findings.
The similarities of results of the current study with recently reported findings from the East London First Episode Psychosis Study (ELFEPS)8 are striking. This is of particular importance because both samples under study were of a different composition. ELFEPS is a study of first episode psychosis patients where psychotic symptoms and violence were measured over the previous 12 months prior to first contact with services. The sample was ethnically diverse and included only patients with diagnosis of nonaffective and affective psychosis. In contrast, the MVRAS sample (primarily of white ethnic origin) demonstrated a broad range of mental disorders (including a substantial number of patients with alcohol and drug abuse/dependence), and patients were at different stages in the course of their illness. Identification of identical pathways between specific delusions implying threat and serious violence—mediated by angry affect due to delusional beliefs—in different samples therefore indicates that these findings are independent of diagnostic categories and support the notion of the relevance of research on clusters of psychotic symptoms and violent behavior.21
It can be assumed that anger due to delusional beliefs as measured in this study is not dichotomous but lies on a continuum. A continuous measure would provide greater power to detect associations with delusions and violence and would also allow the investigation of a dose-response relationship. The MMADS13,15 measures anger as a consequence of delusional beliefs, and we excluded the possibility that trait anger is the determining factor in this association. However, other factors may trigger anger, which were not measured in this study, and the intensity of anger may be influenced by the length of the delusional episode or other external factors. Furthermore, anger may play an important role in the pathogenesis and maintenance of delusional beliefs.22 Future research should aim to clarify this.
Delusions and Risk Management
The contrasting results provided by the original and the current methodological approach have important implications for research in the field of psychosis and violence, and for identification of those at risk and their risk management. To investigate the association of dynamic variables, temporal proximity is of utmost importance. The predictive (“prospective”) approach of MVRAS1 suggested that delusions demonstrated no predictive power and correspondingly would be unsuitable for inclusion in a risk assessment instrument designed to estimate the probability of future violence. Delusions are dynamic in nature and may be active for only short time periods over the life course. Failure to take into account positive treatment response and periods of remission will inevitably lead to failure to identify key associations because symptoms are no longer present. Consideration of temporal proximity demonstrated the relevance of the effects of active delusions on serious violence. Specific delusions implying threat to the individual resulting in anger could be seen as indicators of an increased risk state23 and should therefore be a warning sign for serious violence and key targets for risk management interventions. Further research should determine whether to prevent violence it is necessary to intervene effectively with delusional beliefs, anger due to these beliefs, or whether successful interventions with both are required.
Funding
UK National Institute for Health Research under its Program Grants for Applied Research funding scheme (RP-PG-0407-10500 to S.U., R.K., and J.W.C.).
Acknowledgments
We thank Professor John Monahan, University of Virginia, for his very helpful comments on this manuscript. The views expressed in this article are those of the authors and not necessarily those of the U.K. National Health System, the NIHR or the U.K. Department of Health. The authors have declared that there are no conflicts of interest in relation to the subject of this study.
References
- 1. Appelbaum PS, Robbins PC, Monahan J. Violence and delusions: data from the MacArthur Violence Risk Assessment Study. Am J Psychiatry. 2000;157:566–572 [DOI] [PubMed] [Google Scholar]
- 2. Coid J, Yang M, Roberts A, et al. Violence and psychiatric morbidity in a national household population—a report from the British Household Survey. Am J Epidemiol. 2006;164:1199–1208 [DOI] [PubMed] [Google Scholar]
- 3. Elbogen EB, Johnson SC. The intricate link between violence and mental disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2009;66:152–161 [DOI] [PubMed] [Google Scholar]
- 4. Fazel S, Grann M, Carlström E, Lichtenstein P, Långström N. Risk factors for violent crime in Schizophrenia: a national cohort study of 13,806 patients. J Clin Psychiatry. 2009;70:362–369 [DOI] [PubMed] [Google Scholar]
- 5. Fazel S, Lichtenstein P, Grann M, Goodwin GM, Långström N. Bipolar disorder and violent crime: new evidence from population-based longitudinal studies and systematic review. Arch Gen Psychiatry. 2010;67:931–938 [DOI] [PubMed] [Google Scholar]
- 6. Van Dorn R, Volavka J, Johnson N. Mental disorder and violence: is there a relationship beyond substance use? Soc Psychiatry Psychiatr Epidemiol. 2012;47:487–503 [DOI] [PubMed] [Google Scholar]
- 7. Swanson JW, Swartz MS, Van Dorn RA, et al. A national study of violent behavior in persons with schizophrenia. Arch Gen Psychiatry. 2006;63:490–499 [DOI] [PubMed] [Google Scholar]
- 8. Coid JW, Ullrich S, Kallis C, et al. The relationship between delusions and violence: findings from the East London first episode psychosis study. JAMA Psychiatry. 2013;70:465–471 [DOI] [PubMed] [Google Scholar]
- 9. Novaco R. Anger as a risk factor for violence among the mentally disordered. In: Monahan J, Steadman H, eds. Violence and Mental Disorder: Development in Risk Assessment. Chicago, IL: Unversity of Chicago Press; 1996:21–59 [Google Scholar]
- 10. Pinkham AE, Brensinger C, Kohler C, Gur RE, Gur RC. Actively paranoid patients with schizophrenia over attribute anger to neutral faces. Schizophr Res. 2011;125:174–178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hiday VA. The social context of mental illness and violence. J Health Soc Behav. 1995;36:122–137 [PubMed] [Google Scholar]
- 12. Monahan J, Steadman HJ, Silver E, et al. Rethinking Risk Assessment. The MacArthur Study of Mental Disorder and Violence. New York, NY: Oxford University Press; 2001 [Google Scholar]
- 13. Appelbaum PS, Robbins PC, Roth LH. Dimensional approach to delusions: comparison across types and diagnoses. Am J Psychiatry. 1999;156:1938–1943 [DOI] [PubMed] [Google Scholar]
- 14. Robins LN, Cottler L, Bucholz K, Compton W. The Diagnostic Interview Schedule, Version IV. St Louis, MO: Washington University; 1995 [Google Scholar]
- 15. Taylor PJ, Garety P, Buchanan A, et al. Delusions and violence. In: Monahan J, Steadman HJ, eds. Violence and Mental Disorder: Developments in Risk Assessments. Chicago, IL: University of Chicago Press; 1994:161–182 [Google Scholar]
- 16. Hudziak JJ, Helzer JE, Wetzel MW, et al. The use of the DSM-III-R Checklist for initial diagnostic assessments. Compr Psychiatry. 1993;34:375–383 [DOI] [PubMed] [Google Scholar]
- 17. Spitzer RL, Williams JBW, Gibbon M, First MB. Structured Clinical Interview for DSM-III-R Personality Disorders. Washington, DC: American Psychiatric Press; 1990 [Google Scholar]
- 18. Hart SD, Cox DM, Hare RD. The Hare Psychopathy Checklist: Screening Version (PCL: SV). Ontario, Canada: Multi Health Systems; 1995 [Google Scholar]
- 19. Gueorguieva R, Krystal JH. Move over ANOVA: progress in analyzing repeated-measures data and its reflection in papers published in the Archives of General Psychiatry. Arch Gen Psychiatry. 2004;61:310–317 [DOI] [PubMed] [Google Scholar]
- 20. Freeman D, Dunn G, Fowler D, et al. Current paranoid thinking in patients with delusions: the presence of cognitive-affective biases [published online ahead of print December 07, 2012]. Schizophr Bull. doi: 10/1093/schbul/sbs145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Douglas KS, Guy LS, Hart SD. Psychosis as a risk factor for violence to others: a meta-analysis. Psychol Bull. 2009;135:679–706 [DOI] [PubMed] [Google Scholar]
- 22. Garety PA, Kuipers E, Fowler D, Freeman D, Bebbington PE. A cognitive model of the positive symptoms of psychosis. Psychol Med. 2001;31:189–195 [DOI] [PubMed] [Google Scholar]
- 23. Skeem J, Mulvey E. Monitoring the violence potential of mentally disordered offender being treated in the community. In: Buchanan A, ed. Care of the Mentally Disordered Offender in the Community. New York, NY: Oxford University Press; 2002:111–142 [Google Scholar]