Abstract
The patterns of comorbidity among prevalent mental disorders in adults lead them to load on ‘externalizing,’ ‘distress,’ and ‘fears’ factors. These factors are themselves robustly correlated, but little attention has been paid to this fact. As a first step in studying the implications of these inter-factor correlations, confirmatory factor analyses were conducted on diagnoses of 11 prevalent DSM-IV mental disorders in a nationally representative sample. A model specifying correlated externalizing, distress, and fears factors fit well, but an alternative model was tested in which a ‘general’ bifactor was added to capture what these disorders share in common. There was a modest but significant improvement in fit for the bifactor model relative to the 3-factor oblique model, with all disorders loading strongly on the bifactor. Tests of external validity revealed that the fears, distress, and externalizing factors were differentially associated with measures of functioning and potential risk factors. Nonetheless, the general bifactor accounted for significant independent variance in future psychopathology, functioning, and other criteria over and above the fears, distress, and externalizing factors. These findings support the hypothesis that these prevalent forms of psychopathology have both important common and unique features. Future studies should determine if this is because they share elements of their etiology and neurobiological mechanisms. If so, the existence of common features across diverse forms of prevalent psychopathology could have important implications for understanding the nature, etiology, and outcomes of psychopathology.
Keywords: psychopathology, comorbidity, confirmatory factor analysis
Psychopathology phenotypes, whether they are treated as discrete mental disorders or continuous dimensions, are substantially correlated (Angold & Costello, 2009; Krueger & Markon, 2006a). Multiple studies reviewed by Krueger and Markon (2006a) indicate that prevalent mental disorders are organized by these correlations into higher-order ‘externalizing’ and ‘internalizing’ factors. Furthermore, when the internalizing spectrum is divided into fear and distress factors, as proposed by Krueger (1999), the 3-factor model generally fits better than the 2-factor internalizing-externalizing model. Indeed, Krueger and Markon (2006a) found that the 3-factor model provided the best fit in a meta-analytic review of the factor structure of 11 mental disorders in multiple representative samples (total N = 23,557).1
It is important to note that the fears, distress, and externalizing factors are themselves substantially correlated (Angold & Costello, 2009; Angold, Costello, & Erkanli, 1999; Krueger & Markon, 2006a). This is potentially important because it suggests the testable hypothesis that higher-order distress, fear, and externalizing factors are correlated because they are influenced by a broadly shared set of etiologic factor(s) that are distinct from the ones that cause the specific disorders to correlate together on the externalizing, fears, and distress factors. If substantiated, this hypothesized “general” factor would have important implications for how the nature and etiology of mental disorders is conceptualized and studied.
The present analyses provide initial tests of alternative hypotheses by comparing the fit of Krueger’s (1999) 3-factor (distress, fears, and externalizing) model to an alternative model that also includes a general psychopathology bifactor (Gibbons & Hedeker, 1992) on which every prevalent mental disorder loads. We first tested whether this alternative model fits better than Krueger’s 3-factor model, then examined the extent to which each factor was correlated with important external variables to provide an initial test of their external validity.
METHODS
The data on diagnoses used in these analyses were from the first wave of the National Epidemiologic Study of Alcohol and Related Conditions (NESARC) (Grant, Stinson, Dawson et al., 2004). The data on the external criteria were drawn from the first wave and the second waves of NESARC conducted three years later (http://pubs.niaaa.nih.gov/publications/NESARC_DRM2/NESARC2DRM.pdf). In the first wave of NESARC, structured diagnostic interviews were conducted of 43,093 18–64 year old individuals representative of the noninstitutionalized civilian population of the United States. One person per household was randomly selected, but adults aged 18–24 years were oversampled at a rate 2.25 times greater than other ages. African American and Hispanic households were oversampled, achieving 19.1% non-Hispanic African American 19.3% Hispanic households. The sample was weighted in all analyses to adjust for probabilities of selection, nonresponse, the selection of one person per household, and oversampling. Once weighted, the data were representative of the US population (Grant, Stinson, Dawson et al., 2004). Three years later, 34,653 of these participants were re-interviewed in Wave 2. The participation rate was 81.0% in wave 1 and 86.7% in wave 2. The present analyses were conducted on individuals who were 18–65 years old in Wave 1 (Wave 1 N = 35,336; Wave 2 N = 28,958).
Measures
The Alcohol Use Disorder and Associated Disabilities Interview Schedule–DSM-IV Version (AUDADIS-IV) (Grant et al., 2003) was administered in person. Twelve-month DSM-IV diagnoses used in these analyses were major depression, dysthymia, social phobia, specific phobia, generalized anxiety disorder, agoraphobia/panic disorder, antisocial personality disorder, tobacco dependence, marijuana dependence, alcohol dependence and other drug dependence. The diagnosis of major depression ruled out bereavement, and all mood and anxiety disorders due to general medical conditions were ruled out. No other exclusion criteria were used. The AUDADIS-IV is both reliable (Grant et al., 2003) and valid (Grant, Dawson et al., 2004; Grant, Hasin et al., 2004; Grant, Stinson, Hasin et al., 2004).
External criterion variables that may reflect risk factors for psychopathology were drawn from both waves of NESARC. Participants answered questions regarding parental history of psychopathology, experiences of harsh parenting and physical and sexual abuse during childhood or adolescence, and reported on psychopathology, health, income, and other aspects of functioning in structured interviews. Data on future mental health problems and adaptive functioning were drawn from wave 2 of NESARC. Test-retest reliability and internal consistency of these measures has been found to be good to excellent (Ruan et al., 2008).
Statistical Analyses
We compared the fit of three viable alternative nested structural models of the tetrachoric correlations among the 11 prevalent mental disorders (Table 1): (1) a 2-factor oblique model specifying internalizing and externalizing factors; (2) a 3-factor oblique model specifying fears, distress, and externalizing factors; and (3) a model that specifies a general bifactor (Gibbons & Hedeker, 1992) on which every mental disorder loaded in addition to the externalizing, distress, and fears factors. Consistent with the bifactor model, covariances among general and domain-specific factors were fixed to zero.
Table 1.
Comparisons of alternative nested models of correlations among mental disorders in confirmatory factor analysis
| SB Model χ2 | Model d.f. | P | AIC | BIC | Sample Size Adjusted BIC | Comparative Tests of Model Fit | P | |
|---|---|---|---|---|---|---|---|---|
| 1. 2-factor model oblique (externalizing, internalizing) | 1851.4 | 2023 | 0.9972 | 120222.0 | 120416.9 | 120343.8 | ||
| 2. 3-factor oblique model (externalizing, distress, fears) | 1818.4 | 2021 | 0.9995 | 119861.1 | 120072.9 | 119993.5 | 2 vs. 1: χ2(2) = 177.29 | <.0001 |
| 3. General bifactor model (externalizing, distress, fears, plus general psychopathology) | 1780.12 | 2013 | 0.9999 | 119756.7 | 120036.3 | 119931.4 | 3 vs. 2: χ2(8) = 52.78 | <.0001 |
Note: SB = Satorra-Bentler adjustment; d.f. = degrees of freedom; BIC = Bayesian Information Criterion.
Data were analyzed using scripts submitted to the Census Bureau with permission of the National Institute on Alcohol Abuse and Alcoholism (NIAAA). Because NESARC used complex probability sampling, all analyses were weighted proportionally to the inverse of sampling probability to accurately represent the population. Tetrachoric correlations among 11 discrete mental disorder diagnoses were subjected to confirmatory factor analysis (CFA) using maximum-likelihood estimation with both robust standard errors (MLR) and weighted least-squares (WLSMV) with virtually identical results from the two estimations in Mplus 6.1 (Muthén & Muthén, 2008). The fit of nested models was compared statistically using likelihood ratio tests and the Bayesian Information Criterion (BIC). BIC serves to balance fit and parsimony, with lower BICs indicating better fit.
Associations of each factor with each external criterion variable were tested in structural equation modeling (SEM) by regressing each external criterion jointly on the fears, distress, and externalizing factors in the 3-factor oblique model, and on these three factors and the general bifactor in the bifactor model using WLSMV. Separate analyses were run for each external criterion. The CFA of psychopathology in each of these alternative models constituted the measurement model for predictors in these SEMs.
RESULTS
As shown in Table 1, like previous studies (Krueger & Markon, 2006a), the 3-factor oblique model of distress, fears, and externalizing factors (Model 1) fit better than the 2-factor internalizing and externalizing model using both MLR and WSLMV (not tabled). Figure 1A shows that correlations among the externalizing, distress, and fears disorders in the 3-factor oblique (Model 2) ranged from .59 to .82 using MLR, similar to the corresponding correlations in the meta-analysis of Krueger and Markon (2006a). As reported in Table 1, the model specifying externalizing, distress, and fears factors, plus the general bifactor (Figure 1B), fit modestly but significantly better than Model 1 (Figure 1A).
Figure 1.
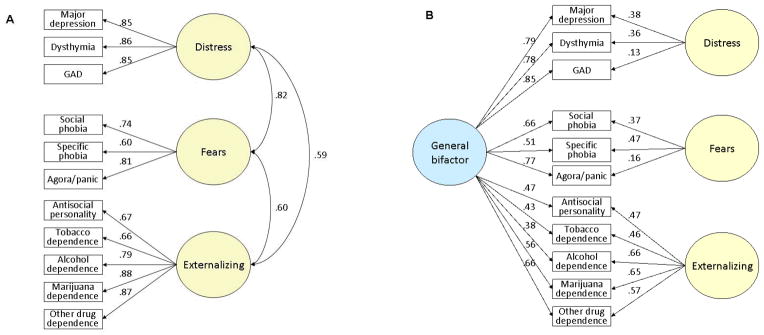
The best fitting models of the correlational structure of 11 mental disorders from the present confirmatory factor analyses of data from the NESARC sample (A) without a general psychopathology factor (Model 2 in Table 2), and (B) with a general psychopathology bifactor (Model 3 in Table 2).
As reported in Table 2, tests of external validity conducted in SEM showed that the fears and distress factors were differentially associated with the external criteria in both the 3-factor oblique and bifactor models when age, sex, and race-ethnicity were controlled. In both models, the externalizing factor was associated with most, but not all external criteria. In the bifactor model, the general bifactor was broadly associated with the external criteria.
Table 2.
Fully standardized regression coefficients testing associations with external criterion variables of latent factors in alternative models
| 3-Factor Oblique Model | Bifactor Model | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| History of Psychopathology in Either Biological Parent | Time-frame | Wave | Prospective | Fears | Distress | Externalizing | General | Fears | Distress | Externalizing |
| Depression | Ever | 1 | No | 0.077 | 0.344**** | 0.100** | 0.468 **** | 0.000 | 0.125* | 0.025 |
| Antisocial | Ever | 1 | No | 0.154* | 0.002 | 0.362**** | 0.343**** | 0.170 | 0.084 | 0.290**** |
| Alcohol/drug problems | Ever | 1 | No | 0.072 | −0.055 | 0.400**** | 0.275**** | 0.064 | 0.012 | 0.295**** |
| Potential Risk Factors | ||||||||||
| Physically abused | <18 yrs | 2 | No | 0.092 | 0.072 | 0.265**** | 0.378**** | −0.065 | −0.018 | 0.122* |
| Sexually abused | <18 yrs | 2 | No | 0.141* | 0.104 | 0.195**** | 0.407**** | −0.051 | −0.015 | 0.060 |
| Neglected by caregivers | <18 yrs | 2 | No | 0.112 | 0.096 | 0.228**** | 0.459**** | −0.153 | −0.124 | 0.006 |
| Wave 2 Functioning | ||||||||||
| Personal income | Last 12 months | 2 | Yes | 0.061 | −0.145**** | −0.125**** | −0.134**** | −0.001 | −0.129**** | −0.106**** |
| Disability income | Last 12 months | 2 | Yes | 0.139 | 0.272**** | −0.021 | 0.348**** | 0.024 | 0.154*** | −0.030 |
| Work impaired by emotion/pain | Last 4 weeks | 2 | Yes | −0.050 | 0.305**** | 0.135**** | 0.322**** | −0.040 | 0.134**** | 0.087**** |
| Incarcerated | Lifetime | 2 | Partly | −0.151* | −0.030 | 0.594**** | 0.257**** | −0.116 | −0.018 | 0.417**** |
| Wave 2 Mental Health | ||||||||||
| Alcohol abuse/dependence | SLI | 2 | Yes | −0.233** | −0.084 | 0.827**** | 0.285**** | −0.052 | 0.125 | 0.354 **** |
| Cannabis abuse/dependence | SLI | 2 | Yes | −0.224 | 0.096 | 0.563**** | 0.256**** | −0.055 | 0.069 | 0.415**** |
| Other drug abuse/dependence | SLI | 2 | Yes | −0.159 | 0.144 | 0.469*** | 0.285**** | −0.052 | 0.125 | 0.354**** |
| Count of APD symptoms | SLI | 2 | Yes | −0.035 | 0.047 | 0.224 **** | 0.116**** | 0.052 | 0.098**** | 0.214**** |
| Count of fear symptoms | SLI | 2 | Yes | 0.393**** | −0.039 | −0.046 | 0.252**** | 0.235** | 0.040 | −0.002 |
| Suicide attempt | Ever | 2 | Partly | 0.059 | 0.292**** | 0.264**** | 0.514**** | −0.048 | 0.119** | 0.153**** |
| Non-suicidal self-harm | Ever | 2 | Partly | −0.062 | 0.323**** | 0.301**** | 0.474**** | −0.090 | 0.090 | 0.164*** |
| Wave 2 Physical Health | ||||||||||
| Body mass index1 | Current | 2 | Yes | 0.146**** | 0.091** | −0.195**** | 0.082**** | 0.040 | 0.044 | −0.155**** |
| Unintentional injury | Last 12 months | 2 | Yes | 0.020 | 0.001 | 0.042**** | 0.054**** | −0.008 | −0.006 | 0.024* |
< .05;
< .01;
< .001;
< .0001
Latent variable covariance matrix not positive definite for bifactor model.
Note: GAD = generalized anxiety disorder; SLI = since last interview.
DISCUSSION
These results confirm previous findings that three factors of distress, fears, and externalizing disorders account well for the correlations among the specific prevalent mental disorders that load most strongly on those factors. Further, the 3-factor model fit significantly better than the 2-factor oblique internalizing-externalizing model in which all fears and distress disorders loaded on the internalizing factor (Krueger & Markon, 2006a; Vollebergh et al., 2001). This close replication of earlier findings is impressive given that both a different sample and a somewhat different list of mental disorders were used in the present and previous studies.
Importantly, as in previous studies (Krueger & Markon, 2006a), the correlations among the latent fears, distress, and externalizing factors in the 3-factor oblique model were substantial (Figure 1A). These robust correlations must be addressed to fully understand the structure of psychopathology. Therefore, we explored the hypothesis that these correlations can be accounted for by a general bifactor on which all 11 mental disorders directly load. It is important to note that we did not specify a supraordinate internalizing factor on which the distress and fears loaded, which is an alternative but equivalent parameterization of the 3-factor model in Figure 1A (Krueger & Markon, 2006a). Rather, we fit a substantively different model in which we account for the correlations among fears, distress, and externalizing by allowing every specific mental disorder to load directly on an orthogonal general bifactor.
When the general bifactor was added, the model fit significantly better based on log-likelihoods than the 3-factor model. It is notable that the general bifactor model fit also fit somewhat better according to BIC, even though BIC penalizes less parsimonious models to avoid the most complex model always being the best-fitting. Thus, both the 3-factor and the general bifactor models fit well enough to be considered plausible alternative models of the correlational structure of psychopathology.
External validity analyses also supported both alternative models, but revealed strong evidence supporting the general bifactor. As shown in the middle columns of Table 2, the fears and distress factors in the 3-factor oblique model were differentially associated with multiple external criteria. These significant associations with the fears factor were consistent with current conceptions of psychopathology (e.g., the wave 1 fears factor was associated with a history of sexual abuse and predicted future fears in wave 2). Similarly, the distress factor was associated with a family history of depression, with several indices of functioning, and with suicide and self-harm as expected. Fears and distress were almost always associated with different external criteria, which is consistent with the proposal to split internalizing into fears and distress (Krueger & Markon, 2006a).
The externalizing factor was found to be associated with 17 of 19 of the selected external criteria in the 3-factor model. All of these associations are consistent with the current literature, and some of the associations were appropriately differential. For example, wave 1 externalizing predicted future antisocial behavior but not future fears. The broad external correlates of the externalizing factor may indicate that, consistent with the mission of NESARC as a study of alcohol use and related disorders, most of the external criterion variables were more useful for validating externalizing than internalizing psychopathology.
Consistent with the meaning of the general bifactor, which was specified to capture what these 11 mental disorders share in common, the general bifactor accounted for robust and significant independent variance in future psychopathology, concurrent and future functioning, self-harm, and other external criteria. As shown in the right columns of Table 2, in the bifactor model, regression coefficients for the fears, distress, and externalizing factors with the external criteria were usually smaller than in the 3-factor oblique model, indicating that at least some of the variance in the external criteria explained by fears, distress, and externalizing was common to the general bifactor. Perhaps most importantly, the general bifactor measured in wave 1 prospectively predicted future psychopathology and functioning assessed in wave 2, over and above the variance accounted for by the fears, distress, and externalizing factors. Interestingly, the general bifactor was strongly associated with measures of physical or sexual abuse and neglect by caregivers, whereas the fears, distress, and externalizing factors were at best only weakly related to these measures (only 1 of 9 associations exceeding a p < 0.05) when the general bifactor was included in the model. Thus, these variables, which may reflect etiologic processes, may be associated with psychopathology in more general than specific ways. Any interpretations must be cautious because of the retrospective measurement of these variables, however.
Neither alternative model was refuted by the external criterion analyses. Given that both models were supported in both sets of analyses, it is important to consider exactly how the 3-factor oblique and general bifactor models differ. Because these two models both specify the same three factors of prevalent psychopathology and differ only in how the robust correlations among these factors are modeled, the relatively small difference in their fits is not surprising. The implications of the difference in handling these correlations in the two alternative models have very important implications for how we conceptualize and study psychopathology. The 3-factor oblique model allows correlations among fears, distress, and externalizing, but the bifactor model explicitly encourages the study of what these 11 dimensions of psychopathology share in common. By specifying a bifactor on which all 11 disorders significantly load, the general bifactor model explicitly suggests the need to understand what is common to all of these prevalent mental disorders.
Alternative Interpretations of the Bifactor Model
At least four alternative interpretations of the general bifactor and its broad correlations with external criterion variables should be tested in future studies:
1. Implicit theories of psychopathology
It is possible that the high correlations among the fears, distress, and externalizing factors are partly due to biases in reporting symptoms. That is, people who experience one symptom may also report other symptoms that have not actually been experienced, inflating correlations among symptoms. Such potential biases might reflect implicit theories of psychopathology. There is evidence that persons hold implicit theories of personality such that when one trait-like characteristic is observed other unobserved characteristics are expected (Schneider, 1973). If people in a culture similarly share implicit theories of which symptoms of psychopathology co-occur, and if these expectations are strong enough to override their actual experiences, they may report unexperienced symptoms, inflating correlations that are consistent with their implicit theories. This also could include biased reporting of expected associations with external criterion variables in ways that create correlations that do not actually exist.
Implicit theories of psychopathology must be considered in interpreting all observed correlations, even the correlations that give rise to well-accepted specific syndromes, such as depression, and the correlations of these syndromes with external criterion variables. It is important, however, to consider whether the bifactor could simply be an artifact of implicit theories of psychopathology. This could be the case only if our implicit theories indicate that every symptom of psychopathology tends to co-occur with every other symptom and with every external criterion variable. Much remains to be learned, but if implicit theories of psychopathology exist and bias reporting, it seems more plausible that they would generate less correlated factors than observed in this study. In our culture, we may expect people who experience one fear to experience other fears and for people who worry to be unhappy, etc. It seems less likely that people in our culture expect antisocial individuals who abuse drugs to also worry, be fearful, and be sad and guilt-ridden. Yet, because these correlations are part of what the bifactor represents, this topic clearly merits further study.
2. Individual differences in biased symptom reporting
The high correlations among factors could reflect individual differences in a tendency to portray oneself in generally negative (or positive) terms (Pettersson & Turkheimer, 2010). Such tendencies could bias the reporting of both symptoms and external criteria in ways that could create the correlations among the three dimensions that support the bifactor model and its broad associations with external criteria. Note, however, that this explanation is substantive. That is, a general tendency to describe oneself in negative terms actually could be one of the psychological processes that actually does create risk for all forms of prevalent psychopathology.
3. Associations with dimensions of personality
It is possible that the widespread comorbidity among prevalent forms of psychopathology can be understood in terms of their associations with broad dimensions of personality. For example, the trait of disinhibition has been found to be specific to externalizing disorders, but neuroticism is high in individuals with fear, distress, and externalizing psychopathology (Krueger & Markon, 2006b). This raises another substantive explanation for the bifactor: The biopsychological processes underlying the broad trait of neuroticism may lie at the heart of the correlations among fears, distress, and externalizing psychopathology that are captured in the general bifactor. This topic also merits further study.
4. Shared etiology
Perhaps the most important substantive explanation for the general bifactor is that it may reflect the influence of etiologic factors that are shared by all mental disorders (Krueger & Markon, 2006a). That is, it is possible that the 11 prevalent mental disorders in the present analyses are correlated partly (or even predominantly) because they are all influenced, albeit to varying degrees, by the same or correlated sets of genetic and environmental factors.
To determine if this hypothesis is supportable, it is necessary to parse the genetic and environmental influences that are associated with the correlations among these prevalent forms of psychopathology. A recent twin study of psychopathology in children and adolescents (Lahey, Van Hulle, Singh, Waldman, & Rathouz, 2011) did just that, supporting this etiologic hypothesis. In a representative sample of 1,571 pairs of 9–17 year old monozygotic and dizygotic twins, three separate variance/covariance matrices were derived from multivariate biometric analyses (Neale & Cardon, 1992) for genetic, shared environmental, and nonshared environmental sources of correlation among prevalent dimensions of psychopathology. Strikingly, the best-fitting structural model for the genetic correlations included a general genetic risk factor very much like the general bifactor in Figure 1B. The robust genetic loadings of every dimension of psychopathology on this factor, and the mostly modest disorder-specific genetic loadings, suggested that a high proportion of the genetic liability for each dimension of psychopathology was shared by all disorders. In contrast, the great majority of the environmental influences detected in this study of children and adolescents was specific to each dimension of psychopathology. Crucially, a recent study of adult twins similarly found that the correlations among a wide range of prevalent mental disorders were almost entirely due to shared genetic influences (Kendler et al., 2011).
The results of these large twin studies are consistent with a “generalist genes/specialist environments” etiologic model, like the one posited for general and specific intellectual abilities (Kovas & Plomin, 2007). In the case of psychopathology, a generalist genes/specialist environments hypothesis asserts that four sets of genetic factors (reflected in the general, distress, fears, and externalizing factors) each pleiotropically increase risk for multiple mental disorders (causing the observed pattern of correlations), whereas it is mostly disorder-specific nonshared environmental experiences that are responsible for differentiating the various mental disorders.
Critically, the bifactor model implies that studies of the causes and biobehavioral mechanisms shared by all prevalent mental disorders will be far more efficient if these multiple mental disorders are studied together in the same samples. This is because the hypothesized joint risk can only be modeled as a bifactor if multiple disorders are studied. Thus, it may be inefficient to continue to study one disorder at a time to understand the nature of psychopathology.
Limitations and Future Studies
Like previous studies, the present study was based on the correlations among a relatively limited number of discrete diagnoses of mental disorders. It would be very useful to repeat the present analyses using a larger set of disorders, especially with psychopathology measured dimensionally (e.g., counts of symptoms), to determine if the same picture emerges. This would be advantageous partly because the reliability of categorical diagnoses measured by all structured interviews is modest. Unfortunately, the NESARC, like other studies of large representative samples, used diagnostic interviews with skip patterns that result in the complete list of symptoms of each disorder being queried only when it is possible for the individual to meet diagnostic criteria for the mental disorder, preventing the use of counts of symptoms. It is also important to note that the external criterion variables were not necessarily assessed in ideal ways. In particular, reports from the participants of their parents’ histories of psychopathology and other measures were based on retrospective recall, which is known to underestimate events and be subject to biases (Lalande & Bonanno, 2011). In addition, as noted, different results may have emerged had the external criteria included more variables relevant to fears and distress.
The most informative future tests of the validity of the general bifactor model will use external criteria relevant to the neurobiological systems associated with psychopathology. Genetic variants increase risk for psychopathology by coding for proteins in neurons, glands, and other organs that constitute risk for psychopathology. Therefore, a strong test of the bifactor model will determine how the general and specific factors in the bifactor model are associated with genetic variants and neurobiological systems. It will also be important to determine if the bifactor model has implications for clinical practice. The present findings suggest that assessing a broad range of disorders and focusing on the total deviance captured in the bifactor could substantially improve prognostic predictions of future psychopathology and functioning.
The hypothesized general bifactor model will be useful only if, relative to other models, it facilitates discovery of the correlates, neural mechanisms, and outcomes that are common and specific to mental disorders.
Acknowledgments
This study was supported by grant R21 MH086099. The authors have no financial disclosures. Dr. Hakes had full access to all data, and along with Dr. Lahey, he takes responsibility for the integrity of the data and the accuracy of the data analysis. We sincerely appreciate the support of Howard Moss and Bridget Grant of NIAAA. We also are grateful to Kristian Markon and Robert Krueger for supplying the unpublished parameters for Figure 1B. Any views expressed on statistical and methodological issues are those of the authors and not necessarily those of the U.S. Census Bureau.
Footnotes
In most studies in which Krueger’s 3-factor model (Krueger & Markon, 2006a) was tested, a supraordinate internalizing factor was included on which both the distress and the fears factors loaded. As previously noted (Krueger & Markon, 2006a), however, the 3-factor model (fears, distress, externalizing) with a higher-order internalizing factor is an equivalent reparameterization of the same 3-factor model without the internalizing factor. When the higher-order internalizing factor is included, the correlation between fears and distress is represented by their loadings on the internalizing factor, and the correlations of both fears and distress with externalizing are represented in the correlation between the internalizing and externalizing factors. Each of these alternative parameterizations of the 3-factor model may be heuristic for different purposes, but they have exactly the same factor loadings and fits (Krueger & Markon, 2006a).
Contributor Information
Benjamin B. Lahey, University of Chicago
Brooks Applegate, Western Michigan University
Jahn K. Hakes, U.S. Census Bureau
David H. Zald, Vanderbilt University
Ahmad R. Hariri, Duke University
Paul J. Rathouz, University of Wisconsin
References
- Angold A, Costello EJ. Nosology and measurement in child and adolescent psychiatry. Journal of Child Psychology and Psychiatry. 2009;50:9–15. doi: 10.1111/j.1469-7610.2008.01981.x. [DOI] [PubMed] [Google Scholar]
- Angold A, Costello EJ, Erkanli A. Comorbidity. Journal of Child Psychology and Psychiatry and Allied Disciplines. 1999;40:57–87. [PubMed] [Google Scholar]
- Gibbons RD, Hedeker DR. Full-Information Item bifactor analysis. Psychometrika. 1992;57:423–436. [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, Chou PS, Kay W, Pickering R. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): Reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug and Alcohol Dependence. 2003;71:7–16. doi: 10.1016/s0376-8716(03)00070-x. [DOI] [PubMed] [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, Chou SP, Dufour MC, Pickering RP. The 12-month prevalence and trends in DSM-IV alcohol abuse and dependence: United States, 1991–1992 and 2001–2002. Drug and Alcohol Dependence. 2004;74:223–234. doi: 10.1016/j.drugalcdep.2004.02.004. [DOI] [PubMed] [Google Scholar]
- Grant BF, Hasin DS, Stinson FS, Dawson DA, Chou SP, Ruan WJ, et al. Prevalence, correlates, and disability of personality disorders in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry. 2004;65:948–958. doi: 10.4088/jcp.v65n0711. [DOI] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders - Results from the national epidemiologic survey on alcohol and related conditions. Archives of General Psychiatry. 2004;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Hasin DS, Dawson DA, Chou SP, Anderson K. Immigration and lifetime prevalence of DSM-IV psychiatric disorders among Mexican Americans and non-Hispanic Whites in them United States - Results from the national epidemiologic survey on alcohol and related conditions. Archives of General Psychiatry. 2004;61:1226–1233. doi: 10.1001/archpsyc.61.12.1226. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Aggen SH, Knudsen GU, Roysamb E, Neale MC, Reichborn-Kjennerud T. The structure of genetic and environmental risk factors for syndromal and subsyndromal common DSM-IV axis I and axis II disorders. American Journal of Psychiatry. 2011;168:29–39. doi: 10.1176/appi.ajp.2010.10030340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovas Y, Plomin R. Learning abilities and disabilities: Generalist genes, specialist environments. Current Directions in Psychological Science. 2007;16:284–288. doi: 10.1111/j.1467-8721.2007.00521.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF, Markon KE. Reinterpreting comorbidity: A model-based approach to understanding and classifying psychopathology. Annual Review of Clinical Psychology. 2006a;2:111–133. doi: 10.1146/annurev.clinpsy.2.022305.095213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF, Markon KE. Understanding psychopathology: Melding behavior genetics, personality, and quantitative psychology to develop an empirically based model. Current Directions in Psychological Science. 2006b;15:113–117. doi: 10.1111/j.0963-7214.2006.00418.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB, Van Hulle CA, Singh AL, Waldman ID, Rathouz PJ. Higher-order genetic and environmental structure of prevalent forms of child and adolescent psychopathology. Archives of General Psychiatry. 2011;68:181–189. doi: 10.1001/archgenpsychiatry.2010.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lalande KM, Bonanno GA. Retrospective memory bias for the frequency of potentially traumatic events: A prospective study. Psychological Trauma-Theory Research Practice and Policy. 2011;3:165–170. [Google Scholar]
- Muthén B, Muthén L. Mplus 5.1. Los Angeles: Muthén & Muthén; 2008. [Google Scholar]
- Neale MC, Cardon LR. Methodology for genetic studies of twins and families. Boston: Kluwer Academic; 1992. [Google Scholar]
- Pettersson E, Turkheimer E. Item selection, evaluation, and simple structure in personality data. Journal of Research in Personality. 2010;44:407–420. doi: 10.1016/j.jrp.2010.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruan WJ, Goldstein RB, Chou SP, Smith SM, Saha TD, Pickering RP, et al. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): Reliability of new psychiatric diagnostic modules and risk factors in a general population sample. Drug and Alcohol Dependence. 2008;92:27–36. doi: 10.1016/j.drugalcdep.2007.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider DJ. Implicit personality theory: Review. Psychological Bulletin. 1973;79:294–309. doi: 10.1037/h0034496. [DOI] [PubMed] [Google Scholar]
- Vollebergh WAM, Iedema J, Bijl RV, de Graaf R, Smit F, Ormel J. The structure and stability of common mental disorders - The NEMESIS Study. Archives of General Psychiatry. 2001;58:597–603. doi: 10.1001/archpsyc.58.6.597. [DOI] [PubMed] [Google Scholar]


