Description
This manuscript details potential benefits for using a research-practice partnership to adapt collaborative depression care for public community long-term care agencies serving older adults. We used sequential, multi-phase, and mixed methods approaches for documenting the process of adaptation within a case study. Systematic adaptation strategies are described, such as leveraging long-term research-practice collaborations, consulting with multiple stakeholders across all levels and disciplines, and balancing demands to monitor treatment fidelity, clinical outcomes, and implementation results. These examples demonstrate that researchers interested in implementation science need skills to negotiate the competing demands that arise from both the research and practice settings.
Keywords: Depression, collaborative care, research-practice partnerships, state agencies, implementation
Introduction
A number of federal reports (i.e., the Quality Chasm report, Institute of Medicine, 2006; the President’s New Freedom Commission Report, USDHHS, 2003; the National Institute of Health’s Road Ahead, USDHHS, 2006) and translational research initiatives (National Institute of Health’s Dissemination and Implementation Research in Health, PAR-07-086) bemoan the long lag-- typically 15 to 20 years-- between the discovery of effective treatments and their use in routine care. This gap is often attributed to the system, organizational, provider, and client differences between practice settings and research settings (Gotham, 2004). Transporting treatments in one setting top down into other settings is risky (Greenlaugh, Robert, MacFarlane, Bate, & Kyriakidou, 2004) and usually proves unsuccessful. Thus, it is increasingly recognized that successful and sustainable implementation usually requires adaptation of evidence-based care to meet the needs and realities of the practice setting (World Health Organization, 2009). Among the most underdeveloped topics in implementation science include the strategies, processes and outcomes of treatment adaptation, and the approaches for forging partnerships between multiple stakeholders engaged in bringing evidence-based treatments into new settings.
With the goal of adding to the growing literature on the science of partnerships (Bradshaw & Haynes, 2012), this case study showcases how a partnership approach is potentially feasible and beneficial for adaptation efforts. We define adaptation as the process of modifying an intervention to real-world contexts without necessarily changing the intervention’s internal logic or core elements (Zayas, Bellamy, & Proctor, 2012). This case of a decade-long research-practice partnership’s adaptation of an empirically supported depression treatment for older adults in community long-term care (CLTC) illustrates how a partnership approach may help maximize fit with the service context while retaining fidelity to the model. The paper is organized to provide descriptions of the context of the practice setting, the research-based intervention, the development of the research-practice partnership, and the adaptation procedures and results. Ultimately, this case study helps specify how treatment adaptations benefit from local practice knowledge, and how partnerships may be linked to positive implementation outcomes such as acceptability, feasibility, and clinical appropriateness (Lenze et al., 2012).
The Practice Setting: Community Long Term Care (CLTC)
The community long-term care practice setting offers an important service context for understanding how partnerships may engage in treatment adaptations due to its far reach across the U.S., the need for integrated care for depression, and the real-world pressures faced by busy caseworkers responding to complex client needs. Every U.S. state provides publicly funded CLTC services, which aim to help low-income people with chronic conditions compensate for functional disabilities and maintain community residence (O’Shaughnessy, 2008). CLTC systems offer assessment, service referral and linkages, and case management. A range of supportive services may be coordinated by CLTC, such as in-home personal care, homemaker services, respite, and adult day services. Thus, CLTC fits as a recommended setting for integrated care because CLTC has first-contact care, conducts comprehensive assessments tapping the family and community context, and acts as “gatekeepers” for the health, mental health, and psychosocial referrals (President’s New Freedom Commission, USDHHS, 2003).
Although the CLTC system is not mandated to respond to depression, many older adults in public CLTC suffer disproportionately high levels of depression (Morrow-Howell, et al., 2008). Despite the potential to reach vulnerable, isolated older adults at high risk of depression, CLTC services system typically identifies depression in one out of four clients with depression (Proctor, Morrow-Howell, Choi, & Lawrence, 2008). In most states’ CLTC systems, caseworkers (usually bachelor-level social workers or other human service workers) have large caseloads, lack in-depth mental health training, and have minimal access to clinical staff internally (Munson, Proctor, Morrow-Howell, Fedoravicius, & Ware, 2008). Moreover, clients’ high functional disability and low income present competing demands to depression care (Proctor, Hasche, Morrow-Howell, Shumway, & Snell, 2008). While CLTC has potential for responding to depression in large numbers of socially and economically disadvantaged older adults, very little research has addressed how to improve depression care in the CLTC setting.
In the year 2000, to address this gap, academic researchers formed a partnership with a Midwestern state’s publicly-funded CLTC agency, which resulted in over a decade of service systems research regarding depression. The research agenda began in response to the state’s administrator’s interest in foundational service systems research and clinical epidemiology to understand the prevalence, associative factors, and implications of clients’ depression on service use (Morrow-Howell, et al., 2008; Hasche, Morrow-Howell, Proctor, 2010; Proctor, Morrow-Howell, et al., 2008). Epidemiologic and services research informed subsequent pre-implementation and intervention developmental work, such as focus groups with stakeholders (Munson et al. 2007) and in-depth client interviews (Proctor, Hasche, et al., 2008). This research revealed three primary challenges to transporting empirically supported depression treatment to CLTC: (1) depression would have to be assessed within the context of competing demands unique to this setting, (2) the system’s resource constraints required targeting depression care to the highest priority clients, and (3) the fragmented system of care that extends across multiple settings required development of communication protocols. Knowing these local challenges from our prior work, the partnership next sought to incorporate broader research knowledge of effective treatments for depression.
The Research-Based Intervention: Collaborative Care
Extensive evidence supports the use of collaborative care models for treating depression among older adults within primary medical care settings (Gilbody, Bower, Fletcher, Richards, & Sutton, 2006). Core components of collaborative care include a depression care manager who has psychiatric supervision, a stepped care algorithm, and regular tracking of depression outcomes by a systematic screen (Katon, Unutzer, Wells, & Jones, 2010). Yet, confining collaborative care to primary care may limit its reach to populations who have routine access to primary care (Clairborne & Vandenburgh, 2001). Two treatment models provided the basis for adapting collaborative depression care to CLTC. First, the IMPACT model (Unutzer et al., 2002) located an on-site depression care manager in primary care settings to coordinate treatment of major depression or dysthymic disorder. The IMPACT model provided the basis for training the depression care manager and revising the training manual, forms, and treatment protocols in our study. Second, the PEARLS model used a depression care manager in supportive housing and geriatric case management to treat minor depression or dysthymia (Ciechanowski et al, 2004). For our study the PEARLS model provided guidelines for subthreshold depression in a non-primary care setting.
This adaptation of collaborative care was further informed by published descriptions of barriers to implementation (Unützer et al., 2005). Typical barriers include organizational culture, limited resources for sustaining staff, and poor infrastructure (Grympa, Haverkamp, Little, & Unützer, 2006; Mosher Henke, Chou, Chanin, Zides, & Hudson Scholle, 2008; Rundall et al., 2002). Other literature makes clear that implementation may be hindered or facilitated by such factors as the intervention’s fit with both the internal agency, the outer community setting, and the characteristics of clients, staff, and administrators (Damshroeder, Aron, Keith, Kirsch, Alexander, & Lowery, 2009). Strained resources are further exacerbated by many physicians operating in small, geographically distinct locations without connections to large organization that collaborative care often targets (Barry & Frank, 2006). For example, providing medical information with consulting providers and to coordinate care across systems becomes problematic without a shared electronic health record system. Lastly, payment systems do not currently cover collaborative care models adequately, and many health reform initiatives (e.g., pay-for-performance and accountable care organizations) hint at possible solutions to these funding barriers (Bao et al., 2011). Thus, given the need to consider multilevel barriers facing collaborative care and the diverse stakeholder’s priorities, the research-practice partnership pursued a formalized approach and specified team of researchers and practitioners to guide adaptation efforts.
The Research-Practice Team
A research-practice team of CLTC administrators and academic researchers began a joint exploration, vetting, and decision-making process to assess how the collaborative care model may be adapted for CLTC given the client population, the organizational context, and the potential effectiveness of the intervention (Kitson, Harvey, & McCormack, 1998). For example, in 2004, three CLTC administrators (two at the state-level, one at the regional-level) and three members of the university-based research team traveled to local and national conferences on empirically supported model of collaborative care (e.g., Improving Mood-Promoting Access to Collaborative Treatment, IMPACT, Unutzer et al., 2002; and Program to Encourage Active, Rewarding Lives for Seniors, PEARLS, Ciechanowski, et al., 2004).
Then, with support of an intervention development (R34) grant received in 2006, partnership received resources to support a more formalized partnership with the CLTC system. The research-practice team invited key stakeholders to participate in ongoing meetings for the adaptation of collaborative care to CLTC. The research-practice team consisted of university-based researchers and a practice team of a CLTC regional manager, CLTC office supervisor, and a CLTC caseworker. The core team involved the researchers and a primary liaison from CLTC (co-author MK). Additional consultants included local providers (i.e., primary care provider, specialty mental health providers in psychiatry, psychology, & social work) and national collaborative care treatment developers. The research-practice partnership team’s goal was to implement an adapted model of collaborative care in CLTC that would have maximum acceptability and sustainability while maintaining clinical effectiveness of the empirically supported treatment.
Adaptation Procedures
Figure 1 reflects our model for adapting and implementing collaborative care in CLTC by leveraging a research-practice partnership. Implementing empirically supported treatments is fraught with many challenges, and in any given setting, professionals react individually, experience unique barriers and evidence differential uptake (Ferlie, Fitzgerald, & Wood, 2000). One of our overarching guiding principles was to incorporate and respect two types of knowledge or evidence: that from research, or “global knowledge” and that from practice, or “local knowledge,” derived from the perspectives and expertise of multiple stakeholders across disciplines and levels of practice (Duan, 2002; Greer, 1988). From the start, we sought to give equal weight to all stakeholders’ opinions and to maximize and maintain treatment fidelity (Greenlaugh, et al. 2004). Per Inouye and colleagues (2006), we focused on adaptations along the treatment’s “soft peripheral” while maintaining fidelity to the original core components. From the outset, it was clear that the research settings for testing collaborative care differed significantly from the practice setting for this adaptation effort. For example, unlike primary medical care, CLTC agencies do not have diagnostic or prescribing privileges or routine connections with primary care. Plus, CLTC agencies’ limited staffing and resources hinder efforts for systematic screening, for use of electronic records to support tracking outcomes, and for communication with primary and specialty care providers (Munson, et al., 2008).
Figure 1.
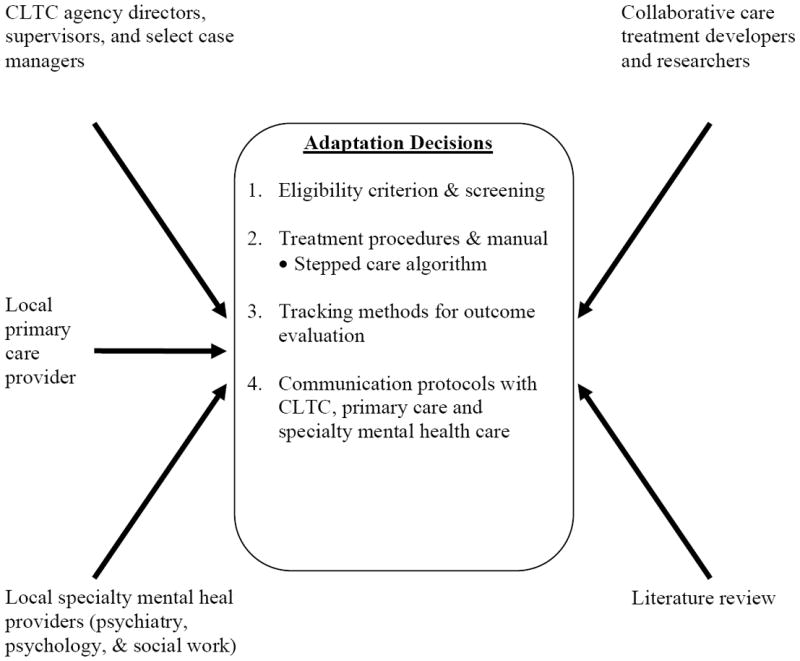
Model of practice-research adaptation process utilizing stakeholder input to adapt collaborative care for community long-term care (CLTC) services.
Recognizing the considerable differences, we initiated a structured, stepwise process to adapt collaborative care for CLTC. With guidance from IMPACT implementation materials (Unutzer et al., 2002; see impact-uw.org) and drawing from challenges facing the CLTC service setting identified by our previous research and grant preparation, we focused our adaptation work on four core components: (1) screening and eligibility criteria, (2) treatment procedures and manual, including the stepped care algorithm, (3) tracking methods for outcome evaluation, and (4) communication protocols with CLTC, primary care and specialty mental health care. We followed a sequential multi-phase, mixed methods approach to systematically document all aspects of our collaborative care adaptation; we were seeking, ultimately, to maintain the intervention’s effectiveness while promoting its feasibility and acceptability for a new service system. Washington University’s Institutional Review Board approved all research activities.
During the initial five-month period of funding, the treatment adaptation activities consisted of consultation meetings and efforts to revise the IMPACT training manual, forms, and communication procedures. First, researchers gathered and summarized written materials summarizing relevant literature, along with agency leadership provision of CLTC service setting characteristics and client descriptions. Second, the core team of researchers and the practice liaison (co-author, MK) proposed adaptation recommendations to all practice-research team members and to external consultants through a series of conference calls. Conference calls included representatives from CLTC (the practice team), the local researchers, and the external consultants—both locally and nationally. The conversations comprised problem solving and negotiation to reach agreement on necessary adaptations. One researcher (principle investigator for the R34 grant) facilitated calls to ensure everyone could express their unique and often divergent views. During the meetings, detailed notes were recorded to capture decisions made about each core components along with the rationale for each recommended adaptation decision. Following meetings, detailed notes were sent to consultants and team members. At the start of the next conference call, decisions at prior meetings were revisited, and opinions about the decisions were invited. This process was repeated until consensus was achieved.
The adapted treatment model was then pilot tested over an 18-month period from May 2007 until September 2008, with the aims to identify further adaptations and to examine the clients’ and providers’ perceptions of acceptability and feasibility. Results, which are reported elsewhere (Lenze et al., 2012), indicate that client and CLTC staff viewed the adapted model as acceptable and that depression scores significantly decreased between treatment initiation and discharge per the Patient Health Questionnaire (PHQ-9, Kroenke, et al., 2001). Throughout the pilot study, the researchers continued weekly team meetings, during which the depression care manager (treatment provider) and the liaison from the CLTC practice setting (regional manger level) continued to review, evaluate, and sometimes modify decisions about how collaborative care could be delivered with fidelity while accommodating practice realities. CLTC state and regional administrators were provided updates monthly and collaborative care expert consultants were contacted as needed. To illustrate, the amount of changes required, we submitted 13 IRB modifications during the first year of the pilot project. Modifications included revisions to consent procedures, addition of CLTC agency sites for recruitment, revisions to screening and assessment forms, and alterations to study methods to expand how outcomes were measured (i.e., in-depth interviews, focus groups). Table 1 and the following sections detail IMPACT and PEARLS collaborative care protocols, the CLTC setting’s features prompting adaptations, and the resultant adaptation for the four core components.
Table 1.
Adapted collaborative care treatment components for community long-term care.
| Component | Protocols | Initial Adaptation | Final Adaptation |
|---|---|---|---|
| Eligibility Criteria & Screening | IMPACT & PEARLS: PHQ-2 ≥ 3, then PHQ-9 ≥ 10 a with symptom profile for Major Depression or Dysthymia | CLTC agency workers used PHQ-2. DCMb used PHQ-9. Inclusion criteria:
|
Some CLTC agencies did not screen all clients.
|
| Stepped Care Treatment Procedures |
IMPACT: client preference for medication or psychotherapy as initial treatment PEARLS: first psychotherapy; medication initiated as second treatment |
Stepped Treatment:d
|
Due to severity and complexity of psychosocial needs, co-occurring psychiatric conditions, an arm of enhanced referral to other medical, social, and psychiatric services was added |
| Tracking Methods | IMPACT and PEARLS: DCM used electronic medical record to track depression severity. Separate researchers test effectiveness. | DCM completes paper files and documents, including PHQ-9 at visits. Randomly assigned comparison group proposed. | DCM assessment includes baseline measure of outcomes. Research assistant conducted 6-month follow-up (PHQ-9 and SF-8f). No comparison group per agency request, low numbers. |
| Communication Protocols |
IMPACT: DCM in primary care, shared electronic medical record PEARLS: DCM shares files with consulting psychiatrist who contacted primary care |
Created record releases forms for DCM (CLTC, primary care, consulting psychiatrist). With permission, DCM mails introductory letter, depression screen to the primary care upon intake. | Forms were adapted on an as needed basis to share information with other medical and social service providers. |
Depression Care Manager;
Treatment protocols: (a) Watchful waiting for minor depression with duration less than 6 months. Includes behavior activation prompt and DCM follow-up at 2 months; (b) Support treatment for any client with current antidepressant use. Offered behavior activation, monitor symptoms with PHQ-9 and discuss medication adherence/response; (c) Problem Solving Treatment, with behavior activation and DCM follow-up; (d) Initiate contact to primary care for medications, with behavior activation and DCM follow-up; (e) Refer for psychiatric care per team consult; and (f) Adapt treatment for moderate cognitive impairment (Short Blessed ≥ 6; Katzman et al., 1983). Includes assessment, linking to primary care, DCM follow-up, and frequent consult with geriatric psychiatrist, team.
Short Form Health Survey (Ware, Kosinski, Dewey, & Gandek, 2001)
Adaptation I: Eligibility & Screening
It was immediately clear that the first core treatment component needing adaptation to this practice setting was the type of depression. Extant models of collaborative care have targeted either major depression (e.g., IMPACT) or subthreshold (e.g., PEARLS). However our team’s clinical epidemiological research showed that 6 percent of CLTC clients meet criteria for major depression and additional 19 percent of CLTC clients exhibited subthreshold depression (Morrow-Howell et al., 2008), suggesting that clients with both conditions needed treatment. However, CLTC stakeholders voiced that budgetary constraints may minimize their treatment capacity for all those in need, given one-fourth of new clients’ evidenced depressive symptoms.
Accordingly, through consensus among the partners, we reached a decision that clients would be triaged with a stepped-care model based on assessment of depression severity, current use of antidepressant medications, client preference, and other comorbidities. Clients with current major depression or suicide risk would be highest priority for treatment. In addition, we determined that clients with subthreshold depression persisting 6 months or longer would also be eligible for the adapted collaborative care. For clients with subthreshold depression less than 6 months and for clients already receiving antidepressants from primary care, we would provide watchful waiting per a stepped-care model (van’t Veer-Tazelaar et al., 2009). This adaptation was informed by our research knowledge that more than half of the clients with depression showed improvements upon reassessment at six-months (Morrow-Howell, et al., 2008).
Similar to IMPACT and PEARLS, we encouraged systematic screening followed by the depression care manager’s in-depth assessment. Per our practice partner’s insights about agencies’ current assessment practices, they recommended we allow agencies to vary in their approach to screening depression (e.g., the Patient Health Questionnaire-2 [PHQ-2], Lowe, Kroenke, & Grafe, 2005; the Patient Health Questionnaire-9 [PHQ-9], Kroenke et al., 2001; the Geriatric Depression Scale-15 [GDS-15] Arthur, Jagger, Lidesay, Graham, & Clarke, 1999). Some agencies asked all clients and others selectively asked per caseworkers’ judgment. The depression care manager conducted assessments on depression severity, duration, psychosocial comorbidities, and antidepressant use. Overall, using this screening approach required a more in-depth assessment by the depression care manager. The research-practice partnership was essential for strategizing how to implement screening within the diverse CLTC agency contexts. However, buy-in for systematic screening was not universal across agencies due to concerns for how screening fit within each agencies’ unique context and service protocols.
Adaptation II: Treatment Procedures
The pilot project highlighted a second pivotal issue for adaptation of the treatment procedures. As reported in our prior work, depressed CLTC clients have high levels of medical, functional, and psychosocial comorbidities (Morrow-Howell et al., 2008; Proctor, Hasche, et al., 2008). The impact of comorbidities was even more apparent during the pilot project. IMPACT’s stepped care treatment algorithm, with the choice of problem-solving treatment or pharmacotherapy, provided the basis for our adapted procedures. The following six treatment arms were initially developed during concensus meetings: (1) watchful waiting, (2) evaluate and support current treatment, (3) problem-solving treatment, (4) initiate contact to primary care for medications, (5) refer to psychiatric care, and (6) adapt treatment for moderate cognitive impairment.
During the pilot study, additional treatment procedures were developed to provide for enhanced referral to other medical, social, and human services. For example, clients presented with high risk needs, such as being evicted from their home, severe substance use problems, and medical crises warranting surgery or institutionalized long term care. To explicate these adaptations, a WELL program manual was created based on the IMPACT training manual. Additional detail described protocols for working with both CLTC caseworkers and in-home personal care aides. The manual covered content for talking to clients about depression, motivational communication, monitoring depression severity, monitoring medication compliance for clients receiving psychotropic medications, and procedures for engaging in enhanced referral to other medical or social services. It included scripts and protocols for assuring confidentiality of client health information, all necessary forms, and a protocol for 24-hour access to telephone consultation with a psychiatrist or mental health specialist in case of emergency. Throughout the pilot project, the research-practice partnership helped facilitate creative responses for the enhanced referrals while the researchers focused on documenting these process changes and linking them to existing scholarship.
Adaptation III: Tracking Methods for Outcome Evaluation
Our pilot project resulted in a new set of tracking methods to evaluate the clinical outcomes related to depression. IMPACT had a specific web-based data management system that records assessment information and treatment plans, tracks clinical encounters, and prompts the depression care manager to contact clients as specified in the stepped care treatment algorithm. We were unable to achieve co-location of the depression care manager within the multiple agencies, since state regulations permitted office space for agency employees only; moreover, because these agencies did not have electronic records, the data management system was converted to a paper file. Finally, unlike the bounded systems in which IMPACT has been tested and implemented, CLTC clients used a wide range of outside providers (e.g., CLTC workers, primary care physicians, mental health specialists). Thus tracking clients’ contact with these providers was another big challenge. Thus, we expanded the IMPACT tracking forms to monitor treatment processes with a variety of providers (e.g., appointments made, appointments attended, medications prescribed, in-home service schedules). The depression care manager conducted and documented bi-weekly in-person or telephone follow-ups to assess clients’ depression severity.
As is often recommended in implementation research, our grant proposal included plans for a separate evaluation involving a randomly assigned comparison group. Unfortunately, due to low recruitment and the CLTC stakeholders’ concerns about the poor quality of usual care, the research-practice partnership decided together that any CLTC clients recruited and identified in need of treatment would receive the treatment. However, as described in Lenze and colleagues (2012) brief report, alternative methods for evaluating outcomes were utilized (i.e., abstraction from client files of depression, acceptability, and feasibility data for pre-/post- quantitative analysis, in-depth interviews with enrolled and ineligible clients, focus groups with CLTC caseworkers). As with many adaptation projects, we learned how important it is to seek consensus within the research-practice partnership and to utilize mixed research methodologies to complete the evaluation across process, clinical, and implementation outcomes throughout the project.
Adaptation IV: Communication Protocols
We also needed to develop protocols to effectively and efficiently communicate with the CLTC workers, the clients’ primary care physicians, other in-home providers, and other referral sources that were not housed within the same health and social service system. These protocols involved developing standard procedures for obtaining consent to share and receive information across service systems, setting time frames for the frequency and means of contact across systems, and identifying primary contact persons within each system. The depression care manager was responsible for initiating, logging, and following-up on all contacts made. This coordination and communication across systems of care was time consuming and required a detail-oriented, well-organized depression care manager. For these adaptations, the research partners relied on the practice partners to contribute examples of forms (e.g., release of information forms, letters to physicians) and to share preferences for communicating across service systems (e.g., frequency, mode, templates for phone messages).
Evaluating the Collaborative Care Depression Treatment Adaptation
While results of the feasibility, acceptability, and clinical outcomes of the pilot study are reported elsewhere (Lenze, et al., 2012), we additionally assessed CLTC workers’ opinions regarding this adapted collaborative care model during a focus group at the conclusion of the pilot project. We transcribed and conducted content analysis of the focus group transcription. These data reflected a positive response to the program. They also captured provider’s clearly voiced needs in this system for additional mental health screening, treatment, and support to clients, as this treatment was able to provide. The majority of agency workers viewed the depression screening questions as acceptable, stating that they “fit really easy into our assessments” and were “comfortable.” However, a few agency workers expressed concerns for the complexity of their clients’ needs, such as “people tend to minimize their depression, so it would be better if there were someone who was actually trained to ask these [screener] questions…”, “a broader scope would be a huge benefit to the population,” and “we’re plagued by mentally ill younger people.” They voiced that the depression care manager was beneficial as an “expert” and “an additional support and eyes and ears for us.” Thus, CLTC workers voiced value in an adapted collaborative care model for CLTC, if it could meet their strained system and complex client needs.
Discussion and Implications
Our project uses a case study of a research-practice partnership to illustrate that adapting collaborative care for CLTC required several compromises to maintain core components of the treatment model while fitting the treatment to the practice context. Moreover, the processes we describe reflect the continued need for the partnership to enact changes throughout the adaptation work. While the partnership retained the core component of the research-based intervention of using a dedicated depression care manager with psychiatric clinical supervision, the partnership’s revisions to the intervention resulted in several distinct changes (i.e., providing treatment across the continuum of depressive disorders, adding watchful waiting as a treatment option along with both PST and medication options, expanding communication patterns across medical and social service systems of care, and developing enhanced referral protocols for psychosocial comorbidities) to meet the needs of clients who were poor, functionally dependent, and enrolled with the public CLTC system. This case study demonstrates how the research-practice partnership facilitated the ongoing adaptations through open dialogue and shared problem-solving. One visible benefit of the partnership was achieving a high level of acceptability while maintaining treatment effectiveness (Lenze, et al., 2012). However, like other adaptation and research-practice partnership studies, the findings can appear idiosyncratic, complicated, and ill fit with typical research procedures such as IRB issues (Chaney, et al., 2008; Hutton, Eccles, & Grimshaw, 2008).
Even with the success of the research-practice partnership, this case study encountered a few limitations. While we assert that this approach to engaging in implementation research via a research-practice partnership may be generalizable to other service systems and empirically supported treatments, we acknowledge that the outcomes may not be generalizable. Furthermore, the partnership’s procedures and resulting adaptations may be attributed to historic changes in this CLTC service system involving the structure and eligibility criterion for Medicaid. During the study period, the CLTC assessment and follow-up procedures changed. CLTC workers’ contact with clients decreased from two-visits per year to one-visit and one follow-up phone call from a centralized call center, which stored all client records. CLTC state policy changes barred providing desk space for any external providers, including the depression care manager, as we initially proposed. These historic changes required open communication, clear direction, and creative problem-solving from the practice members of the partnership. Without the practice members’ investment in the partnership, such historic changes may have stalled the progression of the study.
Concerns for sustainability and feasibility in this time-sensitive, research-practice partnership were evident. For example, once the NIH grant support to the researchers ended, this adapted model of collaborative care was not sustainable due to decereased Medicaid funding for the CLTC system in 2008, to system reorganization, and to leadership changes. The CLTC agencies did not choose to establish a full-time depression care manager employee position because of feasibility and cost concerns (e.g., budget line for new employee position). Concern for sustainability of the adapted treatment model was evident soon after the grant was funded since co-location was not achieved.
The partnership was sustained, even after grant funding, through trainings within the state, grant-writing, and advocating policy changes on a state level. On a promising note, even though the model had limited sustainability, the sustained partnership provided the foundation for a larger state initiative around geriatric mental health care through a Substance Abuse and Mental Health Services Administration transformation grant. This initiative pursued an alternative adaptation of collaborative care for community-based social services for older adults that has demonstrated promise for both effectiveness and sustainability—Healthy IDEAS (Casado et al., 2008). Healthy IDEAS used a community-based coalition to adapt collaborative care and did not attempt to place a specialized depression care manager in a single provider system. Instead, Healthy IDEAS focused on immersing the training, screening, and treatment protocols throughout all case managers within an agency. To date, eight CLTC agencies within the state completed Healthy IDEAS trainings. Thus, this use of a community-based coalition, the awareness of barriers (such as the feasibility concerns for using a “specialist” model for depresion care management within CLTC), and the leveraging of practice-research partnerships, may promote successful implementation.
The Future of Adaptation Research in Implementation Science
The partnership approach and experiences reflected in this paper has implications for researchers across implementation science, services research, and even effectiveness. The project exemplifies how partnered research brings competing demands from both research and practice settings. Treatment researchers often place highest priority on fidelity and emphasize rigorous randomized control trial methodologies. Institutional Review Boards demand approval for each and every protocol change. On the other hand, the demands and realities of real-world practice settings place a premium on delivering the adapted treatment quickly, flexibly, and with wide reach to clients in order to address unmet need. Research-practice partnerships must reconcile conflicts where the practice setting’s preferred adaptations could jeopardize treatment fidelity, systematic observation, and repeated measurement. Every practice setting brings its own external and historical influences, which may impact external validity, implementation success, and the ability to study the implementation process itself. Thus, considerable time and effort must be spent on partnership building and processes of negotiating adaptations. Partnered research requires skills in setting and adhering to clear expectations, skillfully communicating and negotiating discussions, conveying understanding and respect for competing demands, and equitable sharing of leadership and decision-making. In short, implementation research requires and extends many of the key components of treatment development, effectiveness research, and health services research—all of which benefit from well-developed and sustained partnerships between practice and research.
The theory (Aarons, Hulburt, & Horowitz, 2011, Damshroeder, et al., 2009, Mendel, Meredith, Schoenbaum, Sherbourne, & Wells, 2008) and methods (Palinkas, Aarons, Horwitz, Chamberlain, Hulburt, & Landsverk, 2011) of implementation science uniquely recognize and respond to the complex, multilevel and contextual challenges facing health and public social service agencies that partner with researchers. Accordingly, implementation research examines outcomes that combine research and practice interests, such as feasibility, fidelity, penetration, acceptability, sustainability, uptake and costs (Proctor, Landsverk, et al. 2009). Our findings contribute to the emerging knowledge base in implementation science by illustrating the importance of (1) devoting time to the partnership building, (2) negotiating and revising rigid priorities, protocols, and timelines, (3) considering the role of systematically assessing organizational fit prior to the implementation process, and (4) addressing the financial and political constraints to sustainability of the treatment models upfront. Future research would benefit from utilizing assessments of organizational context (Gagnon, Labarthe, Legare, Ouimet et al., 2011; Glisson, Landsverk, Schoenwald, Kelleher, et al., 2008) and further explication of the strategies and processes that promote effective research-practice partnerships. Finally, implementation practice and science demand greater understanding of how to sustain adapted treatments once the resources of external grants end.
Acknowledgments
The authors acknowledge support from the National Institute of Mental Health’s pre-doctoral and post-doctoral trainee program (1T32MH19960) and grant support (R34 MH071632-01A2; 9/06 - 1/09) at the Center for Mental Health Services Research at the George Warren Brown School of Social Work, Washington University. We also express appreciation for ongoing the support from the leaders and caseworkers at the partnering public community long-term care agency
Contributor Information
Leslie K. Hasche, Assistant Professor, Graduate School of Social Work, University of Denver, 2148 S. High Street, Denver, CO 80208; leslie.hasche@du.edu; Phone: 303-871-4816; Fax: 303-871-2845
Shannon Lenze, Instructror, Department of Psychiatry, Washington University School of Medicine; Lenzes@psychiatry.wustl.edu
Teresa Brown, Former Depression Care Manager; tbrown33@me.com
Lisa Lawrence, Expedited Review Specialist, Human Research Protection Office, Washington University School of Medicine; lawrencel@wusm.wustl.edu
Mike Nickel, Regional Manager Missouri Division of Senior and Disability Services (Retired); mnickel@gwbmail.wustl.edu
Nancy Morrow-Howell, Ralph and Muriel Pumphrey Professor of Social Work, George Warren Brown School of Social Work, Washington University in St. Louis; morrow-howell@wustl.edu
Enola K. Proctor, Frank J. Bruno Professor of Social Work Research, George Warren Brown School of Social Work, Washington University in St. Louis; ekp@wustl.edu
References
- Aarons GA, Hulburt M, Horwitz SM. Advancing a conceptual model of evidence-based practice implementation in public service sectors. Administration and Policy in Mental Health and Mental Health Services Research. 2011;38:4–23. doi: 10.1007/s10488-010-0327-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arthur A, Jagger C, Lindesay J, Graham C, Clarke M. Using an annual over-75 health check to screen for depression: Validation of the short Geriatric Depression Scale (GDS-15) within general practice. International Journal of Geriatric Psychiatry. 1999;14:431–439. doi: 10.1002/(SICI)1099-1166(199906)14:6<431. [DOI] [PubMed] [Google Scholar]
- Bao Y, Casalino LP, Ettner SL, Bruce ML, Solberg LI, Unutzer J. Designing payment for collaborative care for depression in primary care. Health Services Research. 2011 doi: 10.1111/j.1475-6773.2011.01272.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barry CL, Frank RG. Commentary: An economic perspective on implementing evidence-based depression care. Administration and Policy in Mental Health and Mental Health Services Research. 2006;33:21–25. doi: 10.1007/s10488-005-4234-2. [DOI] [PubMed] [Google Scholar]
- Bradshaw CP, Haynes KT. Building a science of partnership-focused research: Forging and sustaining partnerships to support child mental health prevention and service research. Administration and Policy in Mental Health and Mental Health Services Research. 2012;39:221–224. doi: 10.1007/s10488-012-0427-7. [DOI] [PubMed] [Google Scholar]
- Casado BL, Quijano LM, Stanley MA, Cully JA, Steinberg EH, Wilson NL. Healthy IDEAS: Implementation of a depression program through community-based case management. The Gerontologist. 2008;48:828–838. doi: 10.1093/geront/48.6.828. [DOI] [PubMed] [Google Scholar]
- Chaney E, Rabuck LG, Uman J, Mittman DC, Simons C, Simon BF, Ritchie M, et al. Human subjects protection issues in QUERI implementation research: QUERI Series. Implementation Science. 2008;3(10):1–12. doi: 10.1186/1748-5908-3-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciechanowski P, Wagner E, Schmaling K, Schwartz S, Williams B, Diehr P, Kulzer J, et al. Community-integrated home-based depression treatment in older adults: A randomized controlled trial. Journal of American Medical Association. 2004;291:1569–1577. doi: 10.1001/jama.291.13.1569. [DOI] [PubMed] [Google Scholar]
- Clairborne N, Vandenburgh H. Social workers’ role in disease management. Health Social Work. 2001;26:217–225. doi: 10.1093/hsw/26.4.217. [DOI] [PubMed] [Google Scholar]
- Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: A consolidated framework for advancing implementation science. Implementation Science. 2009;4(50) doi: 10.1186/1748-5908-4-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duan N. A quest for evidence beyond evidence-based medicine: Unleashing clinical experience through evidence farming; Symposium conducted at the 15th Biannual International Conference on Mental Health Service Research; April 13; Washington, D.C. 2002. Jun, [Google Scholar]
- Ferlie W, Fitzgerald L, Wood M. Getting evidence into clinical practice: An organizational behaviour perspective. Journal of Health Services Research & Policy. 2000;5(2):96–102. doi: 10.1177/135581960000500207. [DOI] [PubMed] [Google Scholar]
- Gagnon M, Labarthe J, Legare F, Ouimet M, Estabrooks CA, Roch G, Ghandour EK, Grimshaw J. Measuring organizational readiness for knowledge translation in chronic care. Implementation Science. 2011;6(1):1–10. doi: 10.1186/1748-5908-6-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbody S, Bower P, Fletcher J, Richards D, Sutton AJ. Collaborative care for depression: a cumulative meta-analysis and review of longer-term outcomes. Archives of Internal Medicine. 2006;166:2314–2321. doi: 10.1001/archinte.166.21.2314. [DOI] [PubMed] [Google Scholar]
- Glisson C, Landsverk J, Schoenwald SK, Kelleher K, Hoagwood KE, Mayberg S, et al. the Research Network on Youth Mental Health. Assessing the organizational social context (OSC) of mental health services for implementation research and practice. Administration and Policy in Mental Health and Mental Health Services Research. 2008;35(1-2):98–113. doi: 10.1007/s10488-007-0148-5. [DOI] [PubMed] [Google Scholar]
- Gotham HJ. Diffusion of Mental Health and Substance Abuse Treatments: Development, Dissemination, and Implementation. Clinical Psychology: Science and Practice. 2004;11:160–176. doi: 10.1093/clipsy.bph067. [DOI] [Google Scholar]
- Greenhalgh T, Robert G, MacFarlane F, Bate P, Kyriakidou O. Diffusion of innovations in service organizations: Systematic review and recommendations. The Milbank Quarterly. 2004;82:581–629. doi: 10.1111/j.0887-378X.2004.00325.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greer AL. The state of the art vs. the state of the science. International Journal of Technological Assessment. 1988;4:5–26. doi: 10.1017/s0266462300003202. [DOI] [PubMed] [Google Scholar]
- Grypma L, Haverkamp R, Little S, Unützer J. Taking an evidence-based model of depression care from research to practice: making lemonade out of depression. General Hospital Psychiatry. 2006;28:101–107. doi: 10.1016/j.genhosppsych.2005.10.008. [DOI] [PubMed] [Google Scholar]
- Hasche L, Morrow-Howell N, Proctor E. Quality of life outcomes for depressed and nondepressed older adults in community long-term care. American Journal of Geriatric Psychiatry. 2010;18:544–553. doi: 10.1097/JGP.0b013e3181cc037b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutton JL, Eccles MP, Grimshaw JM. Ethical issues in implementation research: a discussion of the problems in achieving informed consent. Implementation Science. 2008;3:52–60. doi: 10.1186/1748-5908-3-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inouye SK, Baker DI, Fugal P, Bradley EH. Dissemination of the Hospital Elder Life Program: Implementation, adaptation, and successes. Journal of the American Geriatric Society. 2006;54:1492–1499. doi: 10.1111/j.1532-5415.2006.00869.x. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine (IOM) Improving the quality of health care for mental and substance-use conditions. Washington DC: National Academy of Sciences; 2006. [Google Scholar]
- Katon W, Unutzer J, Wells K, Jones L. Collaborative depression care: history, evolution and ways to enhance dissemination and sustainability. General Hospital Psychiatry. 2010;32:456–464. doi: 10.1016/j.genhosppsych.2010.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katzman R, Brown T, Fuld P, Peck A, Schechter R, Schimmel H. Validation of a short orientation-memory concentration test of cognitive impairment. American Journal of Psychiatry. 1983;140:734–739. doi: 10.1176/ajp.140.6.734. [DOI] [PubMed] [Google Scholar]
- Kitson A, Harvey G, McCormack B. Enabling the implementation of evidence-based practice a conceptual framework. Quality in Health Care. 1998;7:149–158. doi: 10.1136/qshc.7.3.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lenze SN, Hasche L, Brown T, Lawrence L, Morrow-Howell N, Proctor E. Implementing collaborative care for depression in community long term care for older adults. International Journal of Geriatric Psychiatry. 2012;27:545–546. doi: 10.1002/gps.2765. [DOI] [PubMed] [Google Scholar]
- Lowe B, Kroenke K, Grafe K. Detecting and monitoring depression with a two-item questionnaire (PHQ-2) Journal of Psychosomatic Research. 2005;58:163–171. doi: 10.1016/j.jpsychores.2004.09.006. [DOI] [PubMed] [Google Scholar]
- Mendel P, Meredith LS, Schoenbaum M, Sherbourne CD, Wells KB. Interventions in organizational and community context: A framework for building evidence on dissemination and implementation in health services research. Administration and Policy in Mental Health and Mental Health Services Research. 2008;35(1-2):21–37. doi: 10.1007/s10488-007-0144-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrow-Howell N, Proctor EK, Choi S, Lawrence L, Brooks A, Hasche L, Blinne W, et al. Depression in community long-term care: Implications for intervention development. Journal of Behavioral Health Services & Research. 2008;35:37–51. doi: 10.1007/s11414-007-9098-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mosher Henke R, Chou AF, Chanin JC, Zides AB, Hudson Scholle S. Physician attitude toward depression care interventions: Implications for implementation of quality improvement initiatives. Implementation Science, 2008. 2008;3:40. doi: 10.1186/1748-5908-3-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munson M, Proctor E, Morrow-Howell N, Fedoravicius N, Ware N. Case managers speak out: responding to depression in community long-term care. Psychiatric Services. 2007;58:1124–1127. doi: 10.1176/appi.ps.58.8.1124. [DOI] [PubMed] [Google Scholar]
- O’Shaughnessy CV. The Aging Services Network: Broad mandate and increasing responsibilities. Public Policy & Aging Report. 2008;18(3):1–18. [Google Scholar]
- Palinkas L, Aarons GA, Horwitz S, Chamberlain P, Hurlburt M, Landsverk J. Mixed method designs in implementation research. Administration and Policy in Mental Health and Mental Health Services Research. 2011;38:44–53. doi: 10.1007/s10488-010-0314-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- President’s New Freedom Commission on Mental Health. Achieving the promise: Transforming mental health in America—Final Report (DHHS Publication No SMA-03-3832) Rockville, MD: Author; 2003. [Google Scholar]
- Proctor E, Hasche L, Morrow-Howell N, Shumway M, Snell G. Perceptions about competing psychosocial problems and treatment priorities among older adults with depression. Psychiatric Services. 2008;59:670–675. doi: 10.1176/appi.ps.59.6.670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Proctor EK, Landsverk J, Aarons G, Chambers D, Glisson C, Mittman B. Implementation research in mental health services: An emerging science with conceptual, methodological, and training challenges. Administration and Policy in Mental Health and Mental Health Services Research. 2009;36:24–34. doi: 10.1007/s10488-008-0197-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Proctor EK, Morrow-Howell N, Choi S, Lawrence L. Notation of depression in case records of older adults in community long-term care. Social Work. 2008;53:243–253. doi: 10.1093/sw/53.3.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rundall TG, Shortell SM, Wang MC, Casalino L, Bodenheimer T, Gillies RR, Schmitdiel JA, Oswald N, Robinson JC. As good as it gets? Chronic care management in nine leading U.S. physician organizations. British Medical Journal. 2002;325:958–961. doi: 10.1136/bmj.325.7370.958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U. S. Department of Health and Human Services. The road ahead: Research partnerships to transform services. Rockville, MD: Author; 2006. [Google Scholar]
- Unützer J, Katon W, Callahan CM, Williams JW, Hunkeler E, Harpole L, et al. Collaborative care management of late life depression in the primary care setting: A randomized controlled trial. Journal of American Medical Association. 2002;288:2836–2845. doi: 10.1001/jama.288.22.2836. [DOI] [PubMed] [Google Scholar]
- van’t Veer-Tazelaar PJ, van Marwijk HWJ, van Oppen P, van Hout HPJ, van der Horst HE, Cuipers P, Smit F, Beekman ATF. Stepped-care prevention of anxiety and depression in late life. Archives of General Psychiatry. 2009;66:297–304. doi: 10.1001/archgenpsychiatry.2008.555. [DOI] [PubMed] [Google Scholar]
- Ware JE, Kosinski M, Dewey JE, Gandek B. A manual for users of the SF-8 Health Survey. Lincoln, R.I.: QualityMetric Incorporated; 2001. [Google Scholar]
- World Health Organization. Practical guidance for scaling up health service innovations. Geneva, Switzerland: World Health Organization Press; 2009. [Google Scholar]
- Zayas LH, Bellamy JL, Proctor EK. Considering the multiple service contexts in cultural adaptations of evidence-based practice. In: Brownson RC, Colditz GA, Proctor EK, editors. Dissemination and Implementation Research in Health: Translating Science to Practice. Oxford University Press; 2012. [Google Scholar]


