Abstract
Lung carcinoma is the leading cause of cancer-related deaths and is the primary source for choroidal metastasis in over 20% cases. Non-small-cell lung cancer (NSCLC) accounts for 85% of all lung cancer cases. Patients with metastatic NSCLC have a median survival of one year. Successful treatment of systemic metastasis from NSCLC using erlotinib has been documented. The effect of oral erlotinib on choroidal metastasis has been rarely reported. We document a case and study the effect of oral erlotinib on choroidal metastasis from NSCLC. A 48-year-old Caucasian female presented with biopsy-proven primary NSCLC with systemic metastasis and solitary choroidal metastasis of 4.8 mm thickness in the right eye. The patient was treated with 100 mg daily dose of oral erlotinib. Two weeks after starting erlotinib therapy, the patient showed complete regression of choroidal metastasis to a flat scar with resolution of subretinal fluid and improvement of visual acuity from 20/100 to 20/25. There was no evidence of recurrence at five-month follow-up. Erlotinib is an alternative therapy for choroidal metastasis from NSCLC.
Keywords: Choroidal metastasis, erlotinib, lung cancer, non-small-cell lung cancer
Introduction
Lung cancer is the leading cause of cancer-related death in both men and women, accounting for an estimated 160,340 deaths in the United States in 2012.[1] Lung cancer is subdivided into two main types including small cell lung cancer (SCLC) (15% of cases), also known as oat cell carcinoma, and non-small-cell lung cancer (NSCLC) (85% of cases).[2] Tobacco smoke remains the most common cause of lung cancer, followed by air pollution, occupational exposure, and second-hand tobacco smoke. In a review of 520 eyes of 420 patients with uveal metastases by Shields et al., lung cancer was the primary cancer site in 21% cases, accounting for primary source in 40% of males and 12% of females.[3]
The median survival of patients with metastatic NSCLC is approximately one year, and only 3.5% of patients with metastatic NSCLC survive five years after diagnosis.[2,4] Tumor expression of epidermal growth factor receptor (EGFR) interrupts apoptosis, stimulates tumor invasion, and initiates tumor-induced neovascularization, resulting in metastasis.[4] In 40-80% of patients with NSCLC, EGFR is overexpressed, a factor associated with poor prognosis.[2] Erlotinib (Tarceva, Genentech, San Francisco, CA) is a highly specific small molecule that inhibits EFGR tyrosinase kinase by competitively blocking the binding site and thereby inhibiting autophosphorylation with blockage of downstream signaling.[4] Downstream intracellular pathways that lead to cancer cell proliferation, angiogenic growth factor production, and cancer-cell invasion are thus disrupted with this medication.
Erlotinib has been successfully used in the treatment of systemic metastasis in patients with NSCLC with tumor control lasting more than four years.[5] The response of NSCLC choroidal metastasis to oral erlotinib has been rarely studied.[6,7,8] Herein, we report a case of complete rapid regression of choroidal metastasis with single-agent erlotinib.
Case Report
A 48-year-old Caucasian female presented with a three-month history of blurred vision in the right eye (OD). There was past history of smoking over ten years ago and biopsy-proven primary NSCLC diagnosed one month previously. The patient had stage IV disease with brain and bone metastases.
On examination, visual acuity was 20/100 OD and 20/25 left eye (OS). Anterior segment examination was normal in both eyes (OU). Fundus evaluation revealed a 10 × 8 × 4.8 mm solitary juxtapapillary yellow-white choroidal metastasis superior to the optic disc OD [Figures 1a and b]. Extensive subretinal fluid was found extending beneath the foveola and inferiorly [Figure 1c]. The left fundus showed no evidence of tumor. Owing to systemic and choroidal metastasis, the patient was started on 100 mg oral erlotinib daily under the supervision of a medical oncologist.
Figure 1.
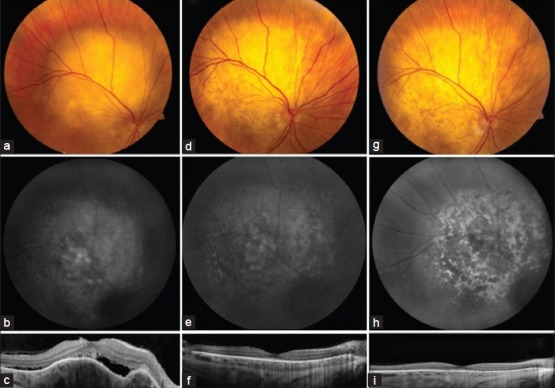
Choroidal metastasis from lung adenocarcinoma. Fundus examination (a) showed a 10 × 8 × 4.8 mm juxtapapillary choroidal mass with subretinal fluid with (b) slight hyperautofluorescence and (c) subretinal fluid and undulating choroidal mass on enhanced depth imaging optical coherence tomography (EDI-OCT). Complete regression of tumor and subretinal fluid (d, e, f) was seen two weeks after starting treatment with oral erlotinib with persistent regression (g, h, i) at five months follow-up
Subsequent ocular examination two weeks later showed complete regression of choroidal metastasis to a flat scar. The subretinal fluid was resolved OD [Figures 1d–f]. No new tumor was detected OS. Visual acuity improved to 20/25 OD and 20/20 OS. The tumor remained regressed with preservation of visual acuity OU at five months follow-up [Figures 1g–i]. Trichiasis and trichomegaly of two eyelashes OS were noted and were epilated. The patient is under continuous monitoring for systemic metastasis.
Discussion
The treatment of choroidal metastasis depends on systemic status, number of tumors, laterality, and presence of subretinal fluid.[9] Treatment options include observation if the patient is pre-terminal or the metastases appear regressed; chemotherapy, immunotherapy, hormone therapy, or whole eye radiotherapy if the metastases are multifocal, bilateral, or associated with extensive subretinal fluid; plaque radiotherapy for solitary metastasis; and enucleation for blind and painful eyes secondary to metastasis.[9]
Systemic chemotherapy was regarded as the first choice of treatment for our patient owing to multiple systemic metastasis and choroidal metastasis. Oral erlotinib has been used to treat patients with locally advanced or metastatic NSCLC.[2,4] Erlotinib can be taken orally as a once-a-day pill and is comfortable for patients to self-administer.
In November 2004, Food and Drug Administration (FDA) approved oral erlotinib as first-line treatment for patients with an EGFR mutation and second-line treatment in advanced NSCLC if there is a relapse or disease progression after the first-line platinum-based combination treatment.[4] Based on clinical trials, patients with EGFR mutation have higher response rates and longer progression-free survival than those without the mutation.[4]
Regarding tumor control within the eye with this medication, Kim et al. reported a 57-year-old female with stage IV NSCLC with multiple choroidal metastases treated with combination intravitreal bevacizumab and oral erlotinib and showing complete regression of choroidal metastases with three one-monthly intravitreal bevacizumab injections and two months of 150 mg daily dose of oral erlotinib.[6] Fujiu et al. described a 49-year-old female with choroidal metastasis from NSCLC who responded to treatment with 100 mg of oral erlotinib, with visual acuity improvement from 20/200 to 20/16 in four days after starting on erlotinib.[7] Daniels et al. described a 43-year-old male with choroidal metastasis from NSCLC, with shrinkage of the choroidal lesion within three days of starting erlotinib and over the course of the next three months, the tumor completely disappeared.[8] In our case, the choroidal metastasis regressed within two weeks of starting single-agent 100 mg oral erlotinib from 4.8 mm thickness to flat with no evidence of recurrence at five months follow-up.
The two most common systemic adverse effects of erlotinib treatment include skin rash (75%) and diarrhea (55%).[4] No systemic side effects were found in our patient. The rare ocular side-effects of EGFR inhibitors include eyelid margin telangiectasia, meibomianitis, tear film dysfunction, and trichomegaly with hyperpigmented, tortuous eyelashes.[10] Our patient had trichomegaly and trichiasis of two eyelashes OS, which were epilated.
In summary, we present a case of NSCLC with complete regression of choroidal metastasis with single-agent erlotinib. This medication is a promising alternative treatment for choroidal metastasis in a few selected cases of NSCLC that demonstrate overexpression of EGFR.
Acknowledgment
Acknowledgement to Carlos G. Bianciotto, M.D.
Footnotes
Source of Support: Support provided by the Eye Tumor Research Foundation, Philadelphia, PA (CLS)
Conflict of Interest: None declared.
References
- 1.Siege R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin. 2012;62:10–29. doi: 10.3322/caac.20138. [DOI] [PubMed] [Google Scholar]
- 2.Molina JR, Yang P, Cassivi SD, Schild SE, Adjei AA. Non-small cell lung cancer: Epidemiology, risk factors, treatments, and survivorship. Mayo Clin Proc. 2008;83:584–94. doi: 10.4065/83.5.584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shields CL, Shields JA, Gross NE, Schwartz GP, Lally SE. Survey of 520 eyes with uveal metastases. Ophthalmology. 1997;104:1265–76. doi: 10.1016/s0161-6420(97)30148-1. [DOI] [PubMed] [Google Scholar]
- 4.Cataldo VD, Gibbons DL, Perez-Soler R, Quintas-Cardama A. Treatment of non-small-cell lung cancer with erlotinib or gefitinib. N Eng J Med. 2011;364:947–55. doi: 10.1056/NEJMct0807960. [DOI] [PubMed] [Google Scholar]
- 5.Weber B, Sorensen BS, Knap MM, Madsen HH, Nexo E, Meldgaard P. Complete pathologic response in lung tumors in two patients with metastatic non-small cell lung cancer treated with erlotinib. J Thorac Oncol. 2011;6:1946–9. doi: 10.1097/JTO.0b013e31822e71f2. [DOI] [PubMed] [Google Scholar]
- 6.Kim S, Kim MJ, Huh K, Oh J. Complete regression of choroidal metastasis secondary to non-small-cell lung cancer with intravitreal bevacizumab and oral erlotinib combination therapy. Ophthalmologica. 2009;223:411–3. doi: 10.1159/000229307. [DOI] [PubMed] [Google Scholar]
- 7.Fujiu K, Kobayashi N, Miyamoto H, Suzuki H. A case of choroidal metastasis of lung cancer successfully treated with erlotinib. Gan To Kagaku Ryoho. 2012;39:269–71. [PubMed] [Google Scholar]
- 8.Daniels AB, Miller ML, Kotecha A, Abramson DH. Uveal metastasis from nonsmall cell lung carcinoma with dramatic response to erlotinib. Retin Cases Brief Rep. 2010;4:390–3. doi: 10.1097/ICB.0b013e3181e180e6. [DOI] [PubMed] [Google Scholar]
- 9.Shields JA, Shields CL. An Atlas and Textbook. 2nd ed. Philadelphia: Lippincott Williams and Wilkins; 2008. Metastatic tumors to the intraocular structures. In: Intraocular Tumors; pp. 198–227. [Google Scholar]
- 10.Zhang G, Basti S, Jampol LM. Acquired trichomegaly and symptomatic external ocular changes in patients receiving epidermal growth factor receptor inhibitors: Case reports and a review of literature. Cornea. 2007;26:858–60. doi: 10.1097/ICO.0b013e318064584a. [DOI] [PubMed] [Google Scholar]


