Abstract
Objective:
To Compare compliance versus dead space (Vd) targeted positive end-expiratory pressure (PEEP) as regard its effect on lung mechanics and oxygenation.
Materials and Methods:
This study was carried out on 30 adult acute respiratory distress syndrome patients. The ventilator was initially set on volume controlled with tidal volume (Vt) 7 mL/kg predicted body weight (PBW), inspiratory plateau pressure (Ppl) <30 cm H2 O. If the Ppl was >30 cm H2 O with a TV of 6 mL/kg PBW, a step-wise Vt reduction of 1 mL/kg PBW to as low as 4 mL/kg/PBW was allowed. Respiratory rate adjusted to maintain pH 7.30-7.45. FiO2 start at 100%. Best PEEP determined at 2 points, one by titrating PEEP until reaching the highest static compliance (Cst) (PEEP Cst) and the other one is at the lowest Vd/Vt (PEEP Vd/Vt). The following data measured before and 30 min after setting PEEP Cst and PEEP Vd/Vt. Cst, PaCO2 - PetCO2, Vd/Vt, PaO2 /FiO2, Ppl, heart rate, mean arterial pressure and oxygen saturation.
Results:
optimum PEEP determined by Vd/Vt was significantly (P < 0.05) lower than the optimum PEEP determined by Cst. Best PEEP Vd/Vt showed a significant decrease (P < 0.05) in Cst, PaCO2 - PetCO2, Vd/Vt and Ppl in comparison with best PEEP Cst. The PaO2 /FiO2 showed a significant increase (P < 0.05) with best PEEP Vd/Vt in comparison with best PEEP Cst.
Conclusion:
Vd guided PEEP improved compliance and oxygenation with less Ppl. Hence, its use as a guide for best PEEP determination may be useful.
Keywords: Acute respiratory distress syndrome, dead space fraction, positive end expiratory pressure, static compliance
Introduction
Acute respiratory distress syndrome(ARDS) characterized by diffuse alveolar injury, edema, collapse and fibrosis. Protective lung strategy ventilation with low tidal volume (Vt or TV) and appropriate positive end-expiratory pressure (PEEP) improve oxygenation with less incidence of complication. Appropriate PEEP diminishes alveolar collapse, decreases pulmonary edema, maintains airway patency, decreases dead space(Vd) and improves oxygenation without hemodynamic compromise or alveolar overdistension.[1]
There were many methods for determination of optimal PEEP but no one proved to be superior or improved clinical outcomes. One of these methods is compliance guided PEEP, which consider the optimum PEEP that corresponds to the highest static compliance (Cst) achieved through PEEP titration. It was considered to be better than surrogate gas exchange.[2]
Measuring Vd fraction (Vd/Vt) is an indicator of ventilation efficiency; alveolar collapse and recruitment. Increase level of Vd/Vt indicates an increase in ventilation of poorly perfused alveoli secondary to ventilation-perfusion mismatch or overinflation of normal compliant lung units. High-level PEEP may result in increased Vd and PaCO2 − PetCO2 difference.[3]
As a method of optimum PEEP determination in ARDS patients is a matter of debate. This study compared compliance versus Vd targeted PEEP as regard its effect on lung mechanics and oxygenation.
Materials and Methods
This study was carried out in surgical intensive care unit (SICU) in Tanta University Hospital on 30 adult patients of both sexes, age range (31-55 years), diagnosed as ARDS, admitted to the SICU between June 2010 and June 2013 after approval by the Hospital Ethical Committee and written informed consent was required for inclusion, and obtained from the nearest relatives.
Inclusion criteria
Age more than 18 years old, mechanical ventilation via an orotracheal tube or tracheostomy, and after 24 h of fulfilling Berlin definition to confirm criteria of ARDS and exclude other causes of hypoxemia and pulmonary infiltrates.[4]
Components of Berlin definition
Acute, meaning onset over 1 week or less
Bilateral opacities consistent with pulmonary edema on computed tomography (CT) or chest radiograph
PaO2 /FiO2 ratio <300 mmHg with a minimum of 5 cm H2 O PEEP (or continuous positive airway pressure)
This criterion must not be fully explained by cardiac failure or fluid overload, based on available information and “objective assessment” (e.g. echocardiogram) should be performed in most cases if there is no clear cause such as trauma or sepsis.
Exclusion criteria
Intracranial hypertension
Neuromuscular disease
Patients with obstructive lung disease or with a history of bronchial asthma
Left ventricular dysfunction (on echocardiography)
Hemodynamically unstable patients or on high-dose vasopressor or inotropes
Barotrauma as interstitial emphysema, pneumothorax, or subcutaneous emphysema
Pregnant patients.
Ventilatory parameters
The ventilator set on volume controlled using ventilator (“inspiration” LS Ventilator series e-Vent) with Vt 7 mL/kg predicted body weight (PBW) (in female = [0.65 × height in cm] −50.74), (in male = [0.73 × height in cm] −59.42). Inspiratory plateau pressure (Ppl) <30 cm H2 O.
If the Ppl was >30 cm H2 O with a Vt of 6 mL/kg PBW, a stepwise Vt reduction of 1 mL/kg PBW to as low as 4 mL/kg/PBW was allowed. Respiratory rate adjusted to maintain adequate minute ventilation and pH between 7.30 and 7.45. Peak inspiratory flow rate adjusted for inspiratory: Expiratory ratio (I: E) 1:2. FiO2 kept at 100% during the study period then decrease gradually with oxygenation goal of PaO2 55-80 mmHg or oxygen saturation (SpO2 ) 88-95%.
All patients were continuously monitored for heart rate (HR), invasive blood pressure, SpO2 and etCO2 using (Nihon Kohden BSM-2301K) monitor and arterial blood gases done using (AVL-988).
The capnograph sensor was placed between the Y-piece and the endotracheal tube.
Lung recruitment maneuver: Done before PEEP titration by addition of 3 sighs/min, each of them generating Ppl at of 35-40 cm H2 O, followed by return to previous ventilatory setting and start PEEP titration from 4 cm H2 O.[5]
Method of positive end-expiratory pressure static compliance and positive end-expiratory pressure dead space/tidal volume determination
All patients were deeply sedated with midazolam 0.2 mg/kg and paralyzed with cisatracurium 0.03 mg/kg. Patients were on FiO2 100% with incremental increasing levels of PEEP in steps of 2 cm H2 O, beginning at 4 cm H2 O, without an upper PEEP titration limit and during PEEP titration each pressure level was maintained for approximately 30 min unless hemodynamic variables deviated from the baseline by ≥15% or new arrhythmia emerged or increase in desaturation.
The PEEP which coincides with the highest Cst considered to be the best compliance guided PEEP (PEEP Cst). If at two different PEEPs the Cst was identical, we chose the one with the lower Ppl. Cst = Vt/∆P (Ppl-PEEP) at end of inflation hold (2 s). The PEEP at which Vd/Vt is at lowest level considered to be the best Vd guided PEEP (PEEP Vd/Vt), above which Vd start to increase again. Vd/Vt = PaCO2 − PetCO2 /PaCO2. It represents physiologic Vd (anatomical Vd plus alveolar Vd).
It is measured before titration of PEEP, as we did not change anything related to the anatomicVd, and the only change is titration of PEEP which affect the alveolar Vd thus this make any change in Vd/Vt is representing the alveolar Vd.
Measurements
All the following data measured before and 30 min after setting each PEEP level (PEEP Cst and PEEP Vd/Vt) determined by PEEP titration.
The primary outcome
Level of PEEP coinciding with the highest compliance and lowest Vd.
Secondary outcome
PaO2 /FiO2
Cst = Vt/∆P (Ppl − PEEP)
Vd/Vt = PaCO2 − PetCO2 /PaCO2
Ppl
HR, mean arterial pressure (MAP) and SpO2 .
End point of the study to detect the PEEP at which Cst and oxygenation improve and Vd/Vt at lower level.
Statistical analysis
Analytic statistics was performed on IBM compatible computer by using SPSS 11.5 software package under Windows XP operating system. All results presented in the form of mean ± standard deviation. Data compared using paired Student's t-test, P < 0.05 was considered as statistically significant.
Results
In this study best PEEP determined by Vd/Vt was significantly (P < 0.05) lower than best PEEP determined by Cst [Table 1 and Figures 1–3].
Table 1.
Level of optimum PEEP (cm H2O) determined by Cst and by Vd/Vt
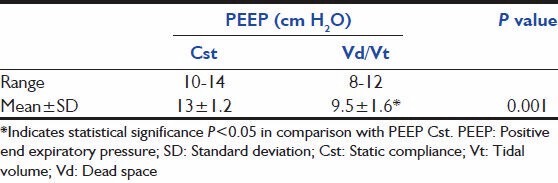
Figure 1.

Effect of positive end expiratory pressure titration on static compliance
Figure 3.

Effect of positive end expiratory pressure titration on PaCO2– PetCO2
Figure 2.

Effect of positive end expiratory pressure titration on dead space/tidal volume
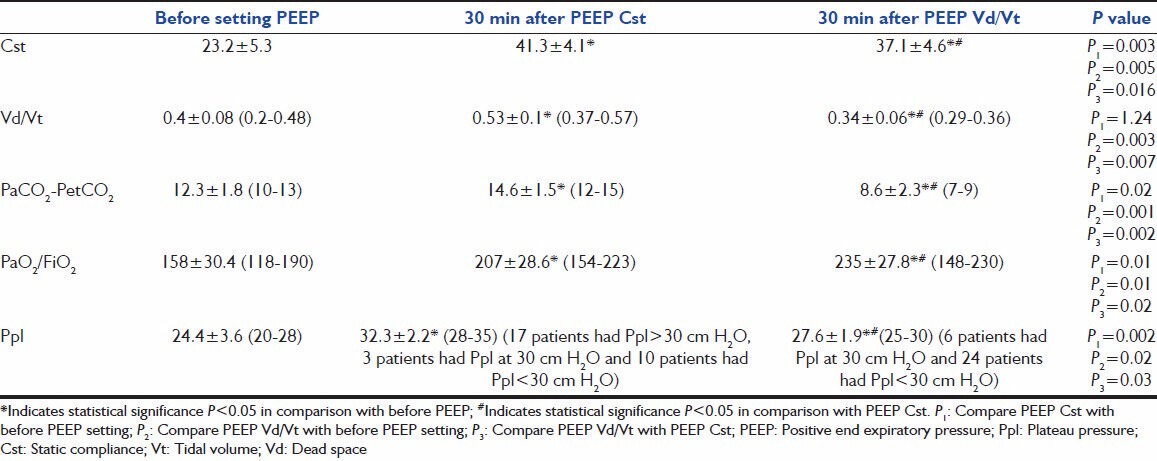
The PEEP Vd/Vt showed a significant decrease (P < 0.05) in Ppl in comparison with PEEP Cst. The PaO2 /FiO2 showed significant increase (P < 0.05) with PEEP Vd/Vt in comparison with PEEP Cst [Table 2]. There was insignificant (P > 0.05) change in MAP, HR and SpO2 between PEEP Cst and PEEP Vd/Vt. Mean number of ventilatory days were (19.4 ± 4.2) and mortality rate was 9/30 (30%). According to the severity of ARDS all patients, PaO2 /FiO2 was 100-200 that is, moderate ARDS with mean value 158 ± 30.4.
Table 2.
Effect of PEEP Cst and PEEP Vd/Vt on lung mechanics and oxygenation
Discussion
In ARDS patients' protective lung ventilation with low Vt and a suitable PEEP level, minimize ventilator-induced lung injury.[1]
Using PEEP maintains atelectatic areas in the lung opened and thereby reduced the risk of hypoxemia and cyclic recruitment/derecruitment. Although PEEP is widely used in clinical practice, its titration to appropriate PEEP level for individuals remains under debate. There are no fixed characteristics for best PEEP, except for having beneficial effect (as recruitment and oxygenation) without harmful effect (as alveolar over distention and barotraumas).[6]
In this study, the level of best PEEP determined by Vd/Vt was lower than PEEP guided by the highest Cst. This data was in agreement with many previous studies which found PEEP to be higher if set according to best compliance.[7,8]
In this study PEEP, Cst improved oxygenation but to a lesser extent than PEEP Vd/Vt and was associated with high Ppl and Vd/Vt.
In contrast with our results, Pintado et al. found compliance guided PEEP had insignificant decrease in Ppl which is explained by improvement in lung recruitment. They conclude that protective mechanical ventilation with best PEEP determined by best compliance had less organ dysfunction without significant effect on oxygenation. They reported problems in identification of PEEP at best compliance due to the need to use the muscle relaxant and also to repeat the test several times which were time consuming.[2]
Suarez-Sipmann et al. found decrement of PEEP after reaching maximum compliance was associated with progressive lung collapse as confirmed by the appearance of atelectasis on the CT scan and was associated with a decrease in oxygenation. Each PEEP step was observed for 10 min.[9]
In ARDS PaCO2 − PetCO2 gradient and shunt increases while oxygenation decreases. Application of PEEP causes reduction in shunt and reduce Vd but excessive PEEP increases PaCO2 − PetCO2 gradient, this makes use of PaCO2 − PetCO2 gradient as guide for best PEEP determination useful.[10]
Many previous studies demonstrate an increase in Vd/Vt early in ARDS, which may reflect alteration of blood flow distribution either due to vasoconstriction or obstruction. Increase in Vd/Vt after application of PEEP may indicate alveolar overdistension.[11,12]
However, in the study by Smith and Fletcher found that PEEP has little effect on the elimination of CO2 after cardiac surgery, and this conflicting result may be because they did not use blood gases and, therefore, they could not measure alveolar Vd or the arterial-end tidal PCO2 difference. Furthermore, their study was on normal lung while this study was on ARDS.[13]
Murate and Muhammed found increase Vd/Vt during positive alveolar pressure mechanical ventilation. When Vd/Vt reaches 0.5, CO2 elimination begins to decrease. Thus, CO2 elimination can be used as a good marker of increased Vd and as a parameter to titrate PEEP.[14]
In a study done by Maisch et al. on patients with healthy lung undergoing surgery under general anesthesia, found PaO2 and functional residual capacity cannot determine best PEEP because they cannot differentiate between increase number of functioning alveolar units and over distention. They suggest the use of compliance and Vd for PEEP determination. In contrast to our study, Cst and Vd/Vt PEEP was identical value. The difference between the two studies may be related to changes in lung mechanics associated with ARDS in our study.[15]
In this study PEEP Vd/Vt showed significant improvement in compliance and oxygenation coincide with the lowest Vd and Ppl in comparison with PEEP Cst.
Conclusion
The individualized PEEP selection based on best Cst is associated with an increase in Vd which may be due to lung overdistension. This indicates the presence of a certain point below the highest Cst at which compliance and oxygenation improved and above which overdistension occur. On the other hand, Vd or PaCO2 − PetCO2 gradient guided PEEP improved compliance and oxygenation with less Vd/Vt and Ppl. Hence, its use as a guide for best PEEP determination may be useful.
Acknowledgments
The authors would like to thank nurses at the intensive care unit of Tanta University Hospital, Tanta, Egypt, for their assistance in conducting the study.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Zhao Z, Steinmann D, Frerichs I, Guttmann J, Möller K. PEEP titration guided by ventilation homogeneity: A feasibility study using electrical impedance tomography. Crit Care. 2010;14:R8. doi: 10.1186/cc8860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pintado MC, de Pablo R, Trascasa M, Milicua JM, Rogero S, Daguerre M, et al. Individualized PEEP setting in subjects with ARDS: A randomized controlled pilot study. Respir Care. 2013;58:1416–23. doi: 10.4187/respcare.02068. [DOI] [PubMed] [Google Scholar]
- 3.Fengmei G, Jin C, Songqiao L, Congshan Y, Yi Y. Dead space fraction changes during PEEP titration following lung recruitment in patients with ARDS. Respir Care. 2012;57:1578–85. doi: 10.4187/respcare.01497. [DOI] [PubMed] [Google Scholar]
- 4.ARDS Definition Task Force. Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, et al. Acute respiratory distress syndrome: The Berlin Definition. JAMA. 2012;307:2526–33. doi: 10.1001/jama.2012.5669. [DOI] [PubMed] [Google Scholar]
- 5.Guerin C, Debord S, Leray V, Delannoy B, Bayle F, Bourdin G, et al. Efficacy and safety of recruitment maneuvers in acute respiratory distress syndrome. Ann Intensive Care. 2011;1:9. doi: 10.1186/2110-5820-1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Badet M, Bayle F, Richard JC, Guérin C. Comparison of optimal positive end-expiratory pressure and recruitment maneuvers during lung-protective mechanical ventilation in patients with acute lung injury/acute respiratory distress syndrome. Respir Care. 2009;54:847–54. doi: 10.4187/002013209793800448. [DOI] [PubMed] [Google Scholar]
- 7.Amato MB, Barbas CS, Medeiros DM, Magaldi RB, Schettino GP, Lorenzi-Filho G, et al. Effect of a protective-ventilation strategy on mortality in the acute respiratory distress syndrome. N Engl J Med. 1998;338:347–54. doi: 10.1056/NEJM199802053380602. [DOI] [PubMed] [Google Scholar]
- 8.Mercat A, Richard JC, Vielle B, Jaber S, Osman D, Diehl JL, et al. Positive end-expiratory pressure setting in adults with acute lung injury and acute respiratory distress syndrome: A randomized controlled trial. JAMA. 2008;299:646–55. doi: 10.1001/jama.299.6.646. [DOI] [PubMed] [Google Scholar]
- 9.Suarez-Sipmann F, Böhm SH, Tusman G, Pesch T, Thamm O, Reissmann H, et al. Use of dynamic compliance for open lung positive end-expiratory pressure titration in an experimental study. Crit Care Med. 2007;35:214–21. doi: 10.1097/01.CCM.0000251131.40301.E2. [DOI] [PubMed] [Google Scholar]
- 10.Murat S, Engin Ok, Ayßegl RT, Muhammed GŸ, Erdogan S. Can arterial minus end-tidal carbon dioxide gradient be used for peep titration? Turk Respir J. 2002;3:94–7. [Google Scholar]
- 11.Gattinoni L, Caironi P, Cressoni M, Chiumello D, Ranieri VM, Quintel M, et al. Lung recruitment in patients with the acute respiratory distress syndrome. N Engl J Med. 2006;354:1775–86. doi: 10.1056/NEJMoa052052. [DOI] [PubMed] [Google Scholar]
- 12.Lucangelo U, Bernabè F, Vatua S, Degrassi G, Villagrà A, Fernandez R, et al. Prognostic value of different dead space indices in mechanically ventilated patients with acute lung injury and ARDS. Chest. 2008;133:62–71. doi: 10.1378/chest.07-0935. [DOI] [PubMed] [Google Scholar]
- 13.Smith RP, Fletcher R. Positive end-expiratory pressure has little effect on carbon dioxide elimination after cardiac surgery. Anesth Analg. 2000;90:85–8. doi: 10.1097/00000539-200001000-00020. [DOI] [PubMed] [Google Scholar]
- 14.Murate S, Muhammed G. Lung carbon dioxide elimination corralates with physiologic dead space volume during mechanical ventilatory support. Turk J Med Sci. 2001;31:529–32. [Google Scholar]
- 15.Maisch S, Reissmann H, Fuellekrug B, Weismann D, Rutkowski T, Tusman G, et al. Compliance and dead space fraction indicate an optimal level of positive end-expiratory pressure after recruitment in anesthetized patients. Anesth Analg. 2008;106:175–81. doi: 10.1213/01.ane.0000287684.74505.49. [DOI] [PubMed] [Google Scholar]


