Abstract
Background:
Keloids are characterised by their continued growth following trauma, extension into normal tissue and their high recurrence rate following excision. Auricular keloids are common following ear piercing or flame burns. These lesions are highly conspicuous and cosmetically unappealing. Multiple methods including surgery, radiotherapy, antimitotic agents, silicone sheet, pressure clips and cryotherapy have been advocated. The risk of recurrence and the need to prevent distortion of the three-dimensional structure of the ear following resection is a challenge to the cutaneous surgeon.
Objectives:
To devise a standard protocol for management of auricular keloids with minimal distortion and recurrence.
Setting and Design:
The patients underwent day-care surgery and subsequent out-patient follow-up for a minimum period of 1 year.
Methods:
Ten patients presenting with 22 ear keloids were enrolled into a keloid protocol: (a) surgical excision and keloid rind flap cover with (b) intra-operative and post-operative intra-lesional steroid and (c) silicone sheet application. Subjective assessment on follow-up was using Patient Observer Scar Assessment Scale and objective assessment was by Beausang scale.
Statistical Analysis used:
Microsoft Excel and Statistical Package for the Social Sciences (SPSS). Kaplan-Meier survival analysis curve used to calculate Recurrence Free period.
Results:
Two out of 22 (9.1%) keloids developed post-excision recurrence after a mean follow -up period of 16 months. The average keloid recurrence free interval was 21 months.
Conclusion:
Triple combination therapy for keloids on the ear is a simple technique for management with preservation of contour of the ear and a low recurrence rate.
KEYWORDS: Auricular keloid, intra-lesional steroid, keloid rind flap, keloid recurrence, triple combination therapy
INTRODUCTION
A keloid is a benign growth of dense fibrous tissue developing from an abnormal healing response to a cutaneous injury. It is characterised by extension beyond the borders of the original wound and growth in a pseudotumour fashion with tissue distortion and high recurrence rates after excision. The term keloid comes from the Greek ‘chele’ meaning crab claw like and was coined by Alibert (cheloide) in 1806 to differentiate keloids from cancerous overgrowths.[1] Areas more commonly affected are the anterior chest, shoulders, flexor surfaces of extremities and the ears.
Keloid of pinna has become increasingly common following the trend of ear piercing and these have cosmetic implications that significantly curtail the quality of life. The incidence of keloids is reported to be 2.5% of all ear piercings.[2] Studies have shown that ear piercing after the age of 11 years is associated with a higher incidence of keloid formation.[3] They may also follow drainage of auricular haematomas, repair of auricular trauma and as secondary recurrences following excision of keloids.
Surgery is the gold standard to treat any size of keloid, as it corrects the obvious distortion of the pinna and reduces the mass of the lesion. Several strategies to prevent post-excision recurrence of keloids have been mentioned including silicone occlusive dressing, mechanical compression, radiation, cryosurgery, topical imiquimod application, bleomycin tattooing, intra-lesional injections of steroids, 5-fluorouracil as well as interferon alpha, -beta and -gamma.[1] The primary goals while planning a treatment protocol should be a low recurrence rate, significant aesthetic and symptomatic improvement and minimal adverse effects.[4]
The present study aimed to devise a standard protocol for treatment of auricular keloids with surgery and a combination of intra-lesional steroid injection and silicone sheet application. The rate of recurrence was assessed after a mean 16-month follow-up.
METHODS
This cohort study was carried out in outpatients presenting to the plastic surgery department of a tertiary care centre from January 2012 to December 2013. Approval for the study was obtained from the Institutional Ethical Committee. Patients were admitted into the study after due informed written consent. The exclusion criteria were pregnant and lactating mothers, concomitant illnesses (renal failure, hepatic disease, acid peptic disease, diabetes and hypertension) as a contraindication to steroids, history of treatment received for keloid in previous 6 months, duration of keloid less than 1 year, female patients unwilling to postpone pregnancy for 1 year and immunocompromised patients.
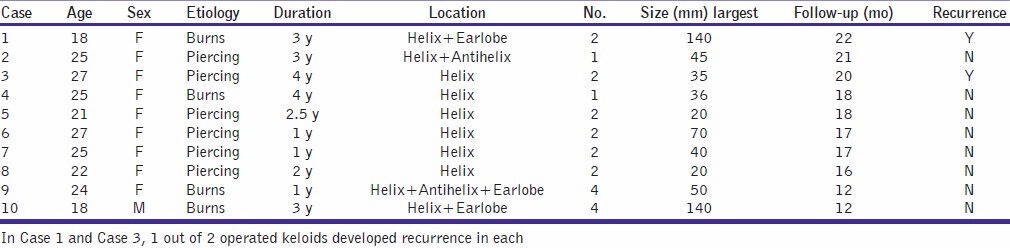
Ten patients presented with keloids and the total number of keloids operated on was 22. The anatomical location of the keloid was noted to be the helix in all our cases with two patients having extension into the earlobe and two patients having involvement of antihelix [Table 1].
Table 1.
Patient and keloid details
The patients underwent intra-lesional excision of pinna keloid with resurfacing of defect using keloid fillet flap. Intra-lesional steroid was injected into margins of keloid excision intra-operatively. Steroid used was triamcinolone acetonide 10 mg/ml, diluted in ratios with equal quantity of 2% lignocaine and given as 1 ml per cm2. Special emphasis was on achieving a tension-free closure, accurate coaptation of skin edges, adequate haemostasis, atraumatic handling of tissues and asepsis. A pressure dressing was applied at the end of surgery for 48 hours.
Suture removal was done on the 14th day. On the 21st day, the second dose of steroid was given and the patient was commenced on silicone sheet application. On the pinna, microporous tape was used to hold the sheets in situ. This was worn for 12 hours per day at night-time for 3 months. The patient presented to Out-patient Department (OPD) after 6, 9 and 12 weeks for the subsequent steroid doses and thereafter at 6, 9 and 12 months for review.
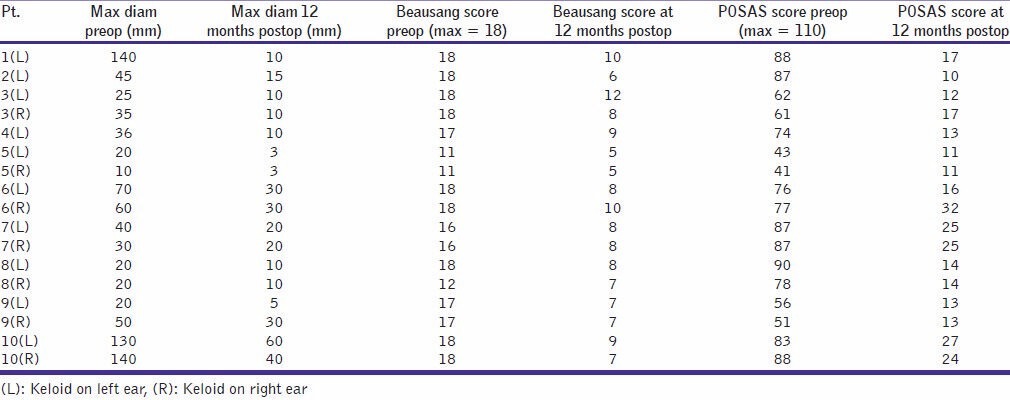
Patients were examined using serial measurements of maximum dimension of scar in two perpendicular planes using callipers and serial photographic documentation. A subjective assessment using Patient Observer Scar Assessment Scale (POSAS)[5] and an objective assessment by an independent observer using Beausang scale was performed at each visit. For POSAS assessment, the patient and observer assessed the operated ear while looking at a mirror in standard lighting in the OPD. For Beausang scale, an independent observer, blinded to time from surgery, assessed the patient in OPD. The data regarding scar assessment on follow-up is given in Table 2.
Table 2.
Scar assessment data
The therapeutic aim of our study was to achieve at least 50% reduction of lesion by surface area with no recurrence at 12-months follow-up. Recurrence was denoted as post-operative emergence of growing or persistently symptomatic scar tissue. Symptoms were defined as pain, itching or pigmentation whereas growing scar was defined as thickening of scar, distortion of surrounding tissue or stiff raised scar. The patients were instructed to avoid further ear piercing or other trauma and to inspect the ear daily for any signs of recurrence. They were educated regarding side effects of the steroids and female patients were advised to avoid pregnancy for 1 year. After completion of 12 months, patients were contacted telephonically to report any recurrence. Recurrent cases received intra-lesional steroid as per the size of scar and were managed on OPD follow-up.
RESULTS
Of the ten cases studied, six were secondary to ear piercing and four were secondary to burn injury. Female: male ratio was 9:1. All patients were in the age group of 18-30 years (mean: 23.2 years). Duration of the lesions ranged from 1 to 4 years. Three cases (30%) were relapsed pinna keloids having previously undergone surgical excision. Five cases had undergone multiple sessions of injectable steroids.
Overall, 22 keloids were operated and all achieved total excision with coverage with keloid rind flap. Post-operative course was uneventful in all cases with no surgical site infections or flap necrosis. After healing by primary intention, all patients went on to receive the second to fifth dose of steroids while continuing silicone sheet application.
One case developed adverse side effect of steroid (gastritis) during treatment necessitating postponement of one dose, whereas two patients developed menorrhagia after completing the dosage schedule and were managed conservatively. Telangiectasia and pigmentation were noted in two patients who resolved on follow-up. Patients were followed up from between 12-21 months (mean 16 months). Figures 1–3 portrays the clinical course of a post-burn helical keloid with no recurrence post-excision at 12 months.
Figure 1.

Preoperative view of post flame burns keloid involving helix and earlobe
Figure 3.

Good contour and no recurrence at 12 months
Figure 2.

Keloid core excision with helical contour restored with fillet flap
Over the course of 12 months, the POSAS scores were consistently better than Beausang scores, denoting a high rate of patient satisfaction compared to physician assessment [Figure 4]. In the 12-month follow-up period, no patient received adjuvant steroid or silicone therapy after the first 3 months. Recurrence was noted in two of 22 operated keloids after the 12 month OPD follow-up, giving a recurrence rate of 9.1%. These were in the form of increased thickness of the scar at the site of excision. Each recurrence received three doses of intra-lesional steroid 3 weekly and showed satisfactory regression. No patient underwent repiercing of the operated ear. Using Kaplan-Meier survival test, a keloid recurrence free interval of 20.86 months was calculated (P < 0.05)
Figure 4.
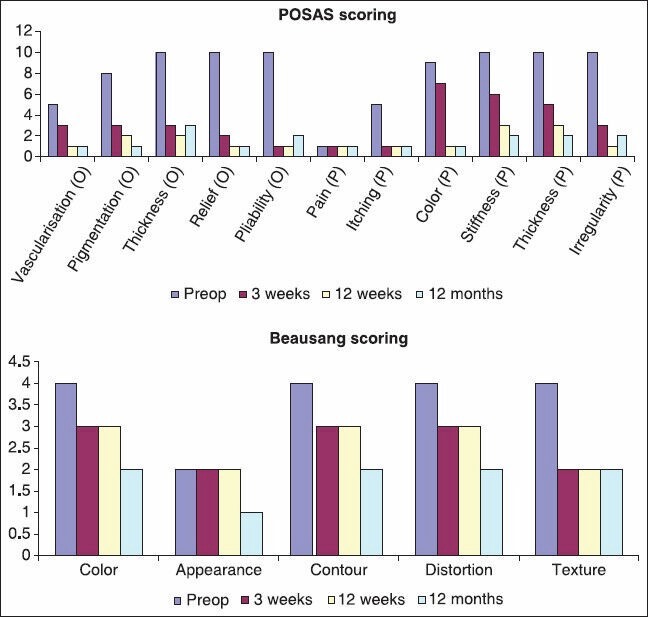
Graph of POSAS vs Beausang score in case 1
DISCUSSION
Keloids and hypertrophic scars are benign fibro proliferative lesions associated with proliferation of dermal fibroblasts. They usually present with tissue distortion, itching and hyperpigmentation. The etiopathogenesis of keloids is not clear, with many hypotheses being put forward, hence the development of a targeted intervention is difficult. Several mechanisms have been implicated in the formation of keloid tissue, including growth factor abnormalities, defective collagen turnover, changes in the orientation of collagen fibres due to tension, immune system dysfunction or hypersensitivity to sebum.
A practical approach would be to classify keloids as small and/or single versus large and/or multiple. The role of surgery in the former would be a single stage complete resection whereas in the latter it would result in a reduction in keloid mass.[6] Non surgical conservative therapies alone are not effective for treating keloids.[7]
Surgical excision of auricular keloids can be challenging because of the need to preserve the underlying three dimensional cartilage framework of the ear and the absence of surrounding tissue laxity.[8] If recurrence occurs, the keloid can invade more local soft tissue and can grow to compromise the underlying cartilage.[9]
Intralesional excision has been favoured in ear keloids where traditional scar revision may distort anatomic structures. The benefits include primary closure, no distortion of anatomic landmarks, no sacrifice of important structures and a debulking effect.[8] Lee described keloid core excision developing a keloid rind flap which is nourished by a subcapsular vascular plexus.[10] Kim in 2005 published his experience with the fillet flap and stressed on the 5 As and 1 B i.e. asepsis, a traumatic technique, absence of raw surface, avoidance of tension, accurate approximation of wound margin and haemostatic control.[11]
Corticosteroid injections can be used to treat keloids in three ways: as adjuvant therapy combined with surgery, as monotherapy treatment of keloids and, as a component of multimodal therapy for the treatment of symptoms.[6] Corticosteroids reduce fibroblast proliferation, collagen and glycosaminoglycan synthesis and suppress pro-inflammatory mediators. The commonest used corticosteroid is triamcinolone acetonide. Its dose range varies from 10-40 mg/ml and it is given at durations between 3 to 6 weeks. Common side effects of triamcinolone are hypo and hyperpigmentation, skin atrophy, telangiectasia and ulceration.[4] In our study, telangiectasia resolved on completion of steroid dosing and the decrease in pigmentation benefited all patients with a good response of pigmentation seen in POSAS scores. Three patients developed minor systemic steroid related complications. However, we were able to complete all cycles of steroid therapy in all three cases.
Post surgical wounds following keloid excision injected immediately with triamcinolone have shown decreased pro alpha 1(I) collagen transcripts, which are normally associated with keloid dermis.[12] The intra-operative dose is thus shown to be the most critical dose which arrests the initiation of hypertrophy and keloid development.[9]
Occlusive dressings such as silicone gel sheets have been recommended for a minimum of 12 hours per day on scars and keloids.[13] Occlusion and hydration are the major effects of silicone dressing. They also bring about a significant reduction in pain, pruritus and erythema.
Radiation modality was not employed in this study due to non-feasibility of referral for radiotherapy on an outpatient basis.
The fillet flap technique used by this study results in superior aesthetics as it provides local tissue of similar colour and contour for resurfacing the defect. Intra-lesional excision with preservation of a keloid rind splints the suture line thus avoiding tension. Preservation of the subcapsular plexus in the keloid ring flap preserves vascularity and allows uneventful healing. There is no donor site morbidity associated with this procedure. Since there is no requirement for graft take, intra-operative instillation of corticosteroid causes no problem of tissue healing. In our study, all patients progressed with uneventful wound healing and with no incidence of flap necrosis. This enabled timely post-operative steroid prophylaxis to continue.
In a previous study, triple keloid therapy has been demonstrated to result in 12.5% recurrences at 13 months.[14] However, the process has been described as tedious, time-intensive and expensive. Patients in another study underwent surgery and steroids weekly for 5 doses and then monthly for 4-6 doses, documenting symptomatic relief after 5 weeks.[15] Our study limited steroid dosing to five doses commencing intra-operatively and subsequently at 3 weekly periods and demonstrated a 9.1% recurrence rate at a mean of 16-months follow-up. Since the primary presentation was with pinna distortion, all patients achieved symptom relief in the immediate post-operative period. All studied patients said they would recommend the procedure to an acquaintance with pinna keloid. This promises a simpler, less radical method of managing pinna keloids with greater patient satisfaction and compliance.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Prabhu A, Sreekar H, Powar R, Uppin VM. A randomized controlled trial comparing the efficacy of intralesional 5-fluorouracil versus triamcinolone acetonide in the treatment of keloids. J Sci Soc. 2012;39:19–25. [Google Scholar]
- 2.Sand M, Sand D, Brors D, Altmeyer P, Mann B, Bechara FG. Cutaneous lesions of the external ear. Head Face Med. 2008;4:2. doi: 10.1186/1746-160X-4-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lane JE, Waller JL, Davis LS. Relationship between age of ear piercing and keloid formation. Pediatrics. 2005;115:1312–14. doi: 10.1542/peds.2004-1085. [DOI] [PubMed] [Google Scholar]
- 4.Gupta S, Sharma VK. Standard guidelines of care: Keloids and hypertrophic scars. Indian J Dermatol Venereol Leprol. 2011;77:94–100. doi: 10.4103/0378-6323.74968. [DOI] [PubMed] [Google Scholar]
- 5.Draaijers J, Tempelman FR, Botman YA, Tuinebreijer WE, Middelkoop E, Kreis RW, et al. The patient and observer scar assessment scale: A reliable and feasible tool for scar evaluation. Plast Reconstr Surg. 2004;113:1960–5. doi: 10.1097/01.prs.0000122207.28773.56. [DOI] [PubMed] [Google Scholar]
- 6.Ogawa R. The most current algorithms for the treatment and prevention of hypertrophic scars and keloids. Plast Reconstr Surg. 2010;125:557–68. doi: 10.1097/PRS.0b013e3181c82dd5. [DOI] [PubMed] [Google Scholar]
- 7.Mustoe TA, Cooter RD, Gold MH, Hobbs FD, Ramelet AA, Shakespeare PG, et al. International Advisory Panel on Scar Management. International Clinical recommendations on Scar Management. Plast Reconstr Surg. 2002;110:560–71. doi: 10.1097/00006534-200208000-00031. [DOI] [PubMed] [Google Scholar]
- 8.Yang JY, Yang SY. Are auricular keloids and persistent hypertrophic scars resectable. The role of intrascar excision? Ann Plast Surg. 2012;69:637–42. doi: 10.1097/SAP.0b013e318274d876. [DOI] [PubMed] [Google Scholar]
- 9.Rosen DJ, Patel D, Freeman P, Weiss P. A primary protocol for the management of keloids: Results of excision combined with intraoperative and postoperative steroid injections. Plast Reconstr Surg. 2007;120:1395–400. doi: 10.1097/01.prs.0000279373.25099.2a. [DOI] [PubMed] [Google Scholar]
- 10.Lee Y, Minn K, Baek RM, Hong JJ. A new surgical treatment of keloid: Keloid core excision. Ann Plast Surg. 2001;46:135–40. doi: 10.1097/00000637-200102000-00008. [DOI] [PubMed] [Google Scholar]
- 11.Kim DY, Kim ES, Eo SR, Kim KS, Lee SY, Cho BH. A surgical approach for earlobe keloid: Keloid fillet flap. Plast Reconstr Surg. 2004;113:1668–74. doi: 10.1097/01.prs.0000117199.47891.4f. [DOI] [PubMed] [Google Scholar]
- 12.Kauh YC, Rouda S, Mondragon G, Tokarek R, diLeonardo M, Tuan RS, et al. Major suppression of pro-alpha1(I) type I collagen gene expression in the dermis after keloid excision and immediate intrawound injection of triamcinolone acetonide. J Am Acad Dermatol. 1997;37:586–9. doi: 10.1016/s0190-9622(97)70176-2. [DOI] [PubMed] [Google Scholar]
- 13.Berman B, Perez OA, Konda S, Kohut BE, Viera MH, Delgado S, et al. A review of the biologic effects, clinical efficacy, and safety of silicone elastomer sheeting for hypertrophic and keloid scar treatment and management. Dermatol Surg. 2007;33:1291–302. doi: 10.1111/j.1524-4725.2007.33280.x. [DOI] [PubMed] [Google Scholar]
- 14.Agbenorku P. Triple keloid therapy: A combination of steroids, surgery and silicone gel strip/sheet for keloid treatment. Eur J Plast Surg. 2000;23:150–1. [Google Scholar]
- 15.Chowdri NA, Masarat M, Mattoo A, Darzi MA. Keloids and hypertrophic scars: Results with intraoperative and serial postoperative corticosteroid injection therapy. Aust N Z J Surg. 1999;69:655–9. doi: 10.1046/j.1440-1622.1999.01658.x. [DOI] [PubMed] [Google Scholar]


