Abstract
Objective
The decision to admit a patient to the intensive care unit (ICU) is complex, reflecting patient factors and available resources. Previous work has shown that ICU census does not impact mortality of patients admitted to the ICU. However, the effect of ICU bed availability on patients outside the ICU is unknown. We sought to determine the association between ICU bed availability, ICU readmissions, and ward cardiac arrests.
Design
In this observational study using data collected between 2009 and 2011, rates of ICU readmission and ward cardiac arrest were determined per 12-hour shift. The relationship between these rates and the number of available ICU beds at the start of each shift (accounting for census and nursing capacity), were investigated. Grouped logistic regression was used to adjust for potential confounders.
Setting
Five specialized adult ICUs comprising 63 adult ICU beds in an academic medical center.
Patients
Any patient admitted to a non-ICU inpatient unit was counted in the ward census and considered at risk for ward cardiac arrest. Patients discharged from an ICU were considered at risk for ICU readmission.
Measurements and Main Results
Data were available for 2086 of 2190 shifts. The odds of ICU readmission increased with each decrease in the overall number of available ICU beds (OR=1.06 [95% CI, 1.00–1.12], p=0.03), with a similar but not statistically significant association demonstrated in ward cardiac arrest rate (OR= 1.06 [95% CI, 0.98–1.14], p=0.16). In subgroup analysis, the odds of ward cardiac arrest increased with each decrease in the number of medical ICU beds available (OR= 1.26 [95% CI, 1.06–1.49], p=0.01).
Conclusions
Reduced ICU bed availability is associated with increased rates of ICU readmission and ward cardiac arrest. This suggests that systemic factors are associated with patient outcomes and flexible critical care resources may be needed when demand is high.
MeSH keywords: in-hospital cardiac arrest, intensive care unit, patient readmission
Introduction
An analysis of trends in critical care use from 2000–2005 in the United States reported that the number of intensive care unit (ICU) beds, days, and occupancy rates have all increased over time (1). Importantly, demand for critical care resources increased at a greater rate than the ICU bed supply (1) with further increases in demand expected due to an aging population with increased comorbidities (2). As demand for ICU beds outpaces the supply, the number of available ICU beds will become increasingly limited, potentially resulting in sicker patients being left on the wards.
Reports on the association between limited ICU bed availability and adverse effects in ICU patient populations have been mixed. A large study of the APACHE database demonstrated no association between bed availability and ICU mortality (3). However, decreased ICU bed availability has been shown to be associated with increased severity of illness in patients admitted to the ICU (4), (5), (6), suggesting that bed availability plays a role in triage decisions. Some studies have demonstrated a shorter ICU length of stay associated with limited bed availability, which may indicate increased pressure to discharge patients when beds are limited (3), (5), (6). Finally, one study of a neurological ICU demonstrated an association between increased patient flow rates and increased rates of readmission to the ICU (7).
Meanwhile, studies of the effects of the ICU bed availability on patients outside the ICU have only examined high-risk ward patients that are evaluated for transfer to the ICU (8), (9), (10), (11), (12), (13). In these populations, decreased ICU bed availability has been associated with decreased rates of transfer into the ICU (8), (9), (12), (14), and an increase in mortality among patients refused transfer to the ICU (8), (13), (14). However, the effects of ICU bed availability on ward patients may extend beyond those patients directly evaluated for transfer to the ICU.
Determining the impact of limited ICU bed availability on outcomes both on the wards and in the ICU has important implications for the health and safety of hospitalized patients. The aims of this study were to examine the effects of ICU bed availability on both the general ward and ICU patient populations. We hypothesized that decreased ICU bed availability would be associated with an increase in readmission to the ICU within twenty-four hours. Additionally, we hypothesized that decreased ICU bed availability would be associated with an increase in the rate of cardiac arrest on the general wards.
Materials and Methods
Study Population and Setting
We conducted an observational cohort study between January 1, 2009 and December 31, 2011 at a tertiary care academic medical center with 63 total adult ICU beds, including specialized medical, cardiac, surgical, and neurological ICUs, and 272 adult general inpatient ward beds. Our hospital has had a rapid response team (RRT) in place since 2008 composed of a critical care nurse, with the availability of a respiratory therapist and hospital medicine or critical care attending as previously described (15). RRT trigger criteria are general, such as “tachypnea” and “staff worry,” and are not tied to specific vital signs. This study was approved by the Institutional Review Board at the University of Chicago. A waiver of informed consent was granted on the basis of minimal risk and general impracticability. Collection of patient information was designed to comply with the Health Insurance Portability and Accountability Act of 1996 (HIPAA) regulations.
Data Collection
ICU bed availability was collected in a hand written institutional log. At the start of each 7am and 7pm shift the ICU manager or charge nurse recorded the census and capacity of each ICU. The census refers to the number of patients within the ICU at the start of the shift. The capacity refers to the total number of beds available to accommodate patients with the available nurses for the shift. Therefore, if there were ten physical beds, but only enough nurses to care for eight patients, then the capacity would have been logged as eight. Bed availability represents the capacity minus the census. Data from each log were entered into a spreadsheet (Microsoft Excel 2010, Microsoft, Redmond, WA) independently by two authors (MH, JT). Shifts with missing or incomplete data were excluded. When there was a difference in data entry between MH and JT (representing a transcription error by one or both of the authors), author TY examined the handwritten log and resolved the difference by entering the correct data point in the final data set. All data were entered, checked, and finalized prior to being merged with the outcomes data. As such, all authors were blinded to outcomes at the point of data entry. Once merged with outcomes, no changes were made to the data. Demographic data and hospital ward occupancy at the start of each shift was obtained from electronic administrative databases.
ICU readmission was defined, a priori, as an ICU readmission or a ward cardiac arrest within 24 hours of discharge from an ICU to a ward. The ICU readmission rate was calculated per shift using the total number of discharges as the denominator and the number of those patients who had an ICU readmission as the numerator. ICU readmission rate was analyzed as a proportion rather than as a whole number to account for variation in transfer rates out of the ICU. ICU readmission data were obtained from the Admission-Discharge-Transfer administrative database. Cardiac arrest was defined as the loss of palpable pulse with attempted resuscitation on any general inpatient ward (medical or surgical). The cardiac arrest rate was calculated per shift using the number of patients on the general wards as the denominator and the number of arrests as the numerator. The cardiac arrest rate was reported as arrests per 10,000 ward patients per shift for simplicity. Cardiac arrests were identified using a prospectively collected and verified quality improvement database previously described (16). Comfort care deaths (e.g. deaths in patients with a DNAR order) were excluded from analysis.
Statistical Analysis
Analyses were performed using a statistical software application (Stata version 11.0, Statacorp, College Station, TX). Descriptive statistics were compared using Student’s t-test, χ2 test, or Wilcoxon rank sum test as appropriate. The associations between ICU bed availability and ICU readmission rate or cardiac arrest rate on the general inpatient wards were analyzed using grouped logistic regression. The final models were adjusted for potential confounders by adding the variables of calendar year (i.e. 2008, 2009, etc.), season (i.e. Summer, Spring, etc.), day of week (i.e. Monday, Tuesday, etc.), and time of day (day versus night). A sub-group analysis was conducted by separately analyzing the data using medical ICU (MICU) and non-MICU bed availability. All tests of statistical significance used a two-sided p<0.05.
Results
Over the study period, there were 60,355 admissions over 2,190 consecutive shifts, of which 2,086 (95.3%) had complete data. Shifts with missing data were evenly distributed by year, season, day of week, and day versus night. The mean age of all admitted patients was 54 ± 18 years, 43% were male, and 24% were surgical admissions. The median length of hospital stay was 3 days (IQR 2–6). There were 8238 discharges from the ICU with 245 (3%) readmitted within twenty-four hours. There were 117 ward cardiac arrests, resulting in a ward cardiac arrest rate of 2.63 per 10,000 patient-shifts. Descriptive statistics of bed availability are shown in Table 1.
Table 1.
Results
| Total Shifts, n | 2190 |
| Shifts with complete data, n (%) | 2086 (98.5) |
| Ward occupancy, median (IQR) | 218 (201 – 231) |
| Combined ICU beds, median (IQR) | 61 (58 – 63) |
| Medical ICU | 16 (15 – 16) |
| Non-medical ICU | 42 (38 – 44) |
| Combined ICU bed availability, median (IQR) | 5 (3 – 7) |
| MICU bed availability | 1 (0 – 2) |
| Non-MICU bed availability | 3 (2 – 5) |
| Shifts with zero available ICU beds, n (%) | |
| Any ICU bed | 6 (0.3) |
| Medical ICU bed | 557 (2.7) |
| Non-medical ICU bed | 65 (3.1) |
| Total ICU to ward discharges, n | 8238 |
| ICU Discharges per shift, median (IQR) | 4 (3–6) |
| Total ICU readmissions, n | 245 |
| ICU readmission per 100 discharges | 2.63 |
| Total Cardiac arrests (n) | 117 |
| Cardiac arrest rate per 10,000 ward patient-shifts | 2.63 |
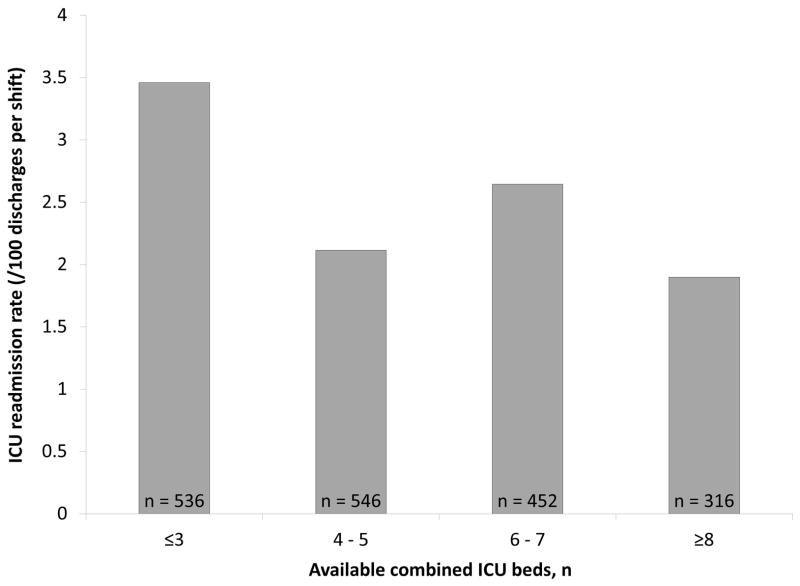
ICU readmission rates by ICU bed availability in quartiles are illustrated in Figure 1. The odds of readmission to the ICU significantly increased with each unit decrease in total ICU bed availability after adjusting for potential confounders (OR=1.06 [95% CI, 1.00–1.12], p=0.03) (Figure 2).
Figure 1.
Adjusted Intensive Care Unit (ICU) readmission rate by combined ICU bed availability, n = number of 12-hour shifts, p = 0.03.
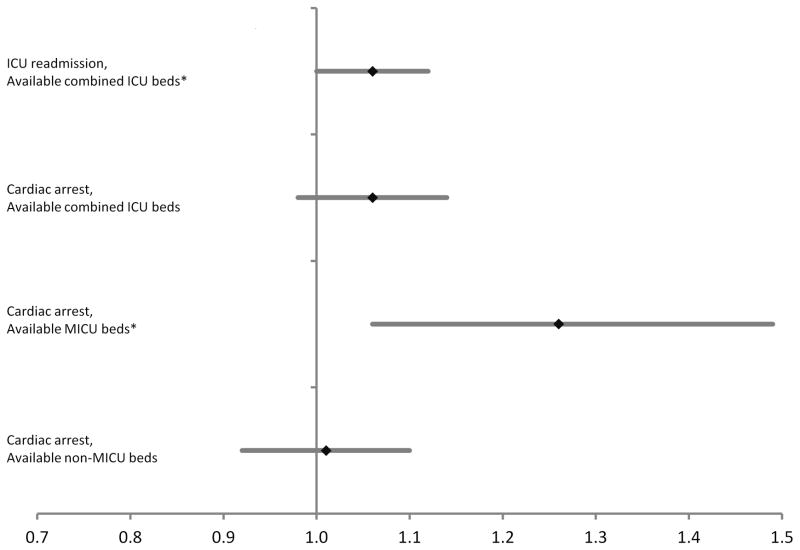
Figure 2.
Odds ratios and 95% confidence intervals for ICU readmission and ward cardiac arrest per unit decrease in ICU bed availability using grouped logistic regression and adjusted for academic year, season, time of day, and day of week. The odds ratio for ward cardiac arrest was also calculated for subgroups of available Medical ICU (MICU) and non-MICU beds. *p<0.05
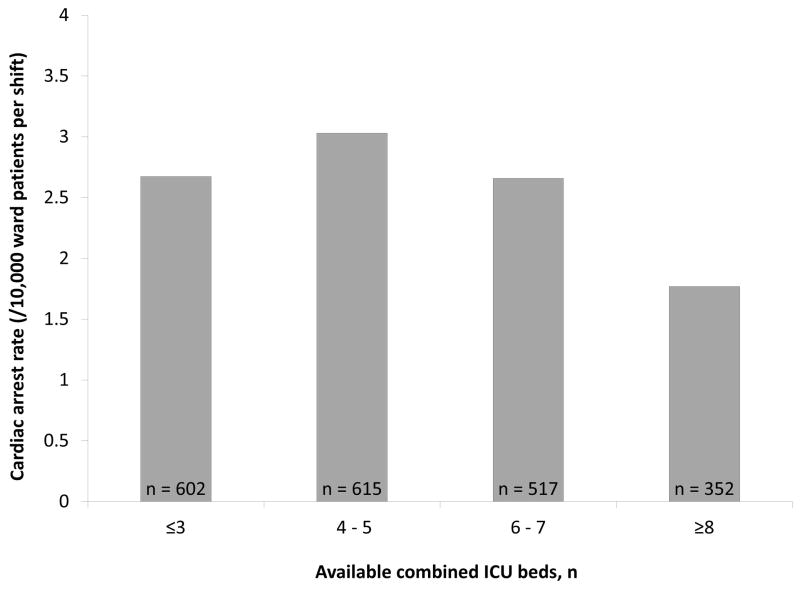
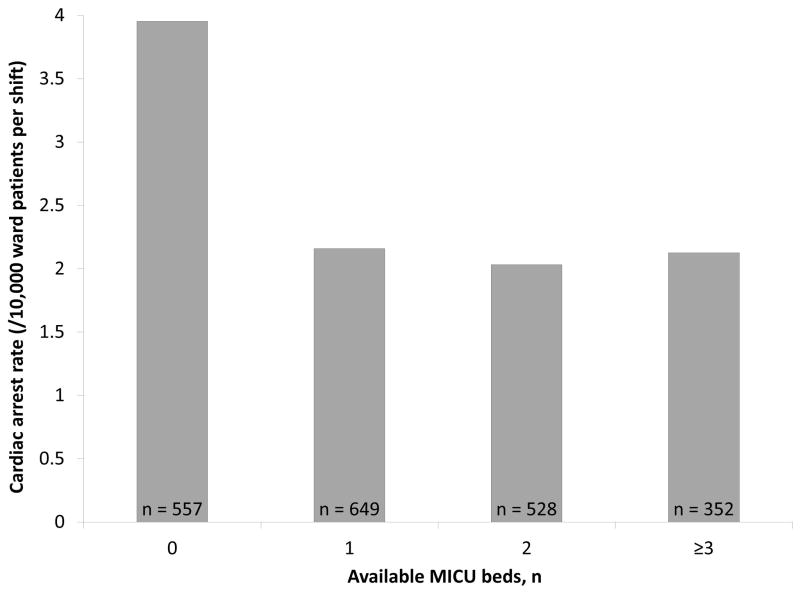
Figure 3 shows the ward cardiac rates by ICU bed availability in quartiles. The association between the number of available ICU beds and ward cardiac arrest rates was similar to that of ICU readmissions but was not statistically significant (OR 1.06 [95% CI, 0.98–1.14], p = 0.16). In unadjusted analysis of the MICU bed availability, the rate of cardiac arrest on the general wards nearly doubled when comparing zero versus one or more available MICU beds (3.89 vs. 2.11 per 10,000 patients-shifts, p=0.01) (Figure 4). After adjusting for potential confounders, MICU bed availability was significantly associated with ward cardiac arrest rates (OR= 1.25 [95% CI, 1.06–1.49], p=0.01). Non-MICU bed availability was not associated with ward cardiac arrest rates (OR 1.01, [95% CI, 0.92–1.10], p = 0.86).
Figure 3.
Ward cardiac arrest rate by combined ICU bed availability, n = number of 12-hour shifts, p = 0.16.
Figure 4.
Ward cardiac arrest rate by medical ICU (MICU) bed availability, n = number of 12-hour shifts, p = 0.01.
Discussion
In this study, we found that the ICU readmission rate increased significantly as ICU bed availability decreased. In addition, the cardiac arrest rate among all ward patients increased with decreasing medical ICU bed availability. This is the first study to demonstrate this association, which was most pronounced when the MICU was full as compared to when one or more MICU beds were available, as the unadjusted rates of cardiac arrest nearly doubled when the MICU was full. This study demonstrates that limited ICU bed availability is associated with adverse effects in the hospital population at large, including both ward and ICU patients.
Associations between the outcomes of ICU patients (including readmission) and various indicators of ICU activity such as ICU census (3), admission volume and occupancy (17) (18), workload (19), and patient turnover (7) have previously been reported. Our study is unique in that it analyzes multiple specialized ICUs within our institution over an extended period of ICU traffic from a systems-level perspective. Lack of ICU bed vacancy was a significant risk factor for ICU readmission in one study (20), however, the authors defined readmission using a longer window of 7 days from ICU discharge and did not specifically account for nursing staffing in their ICU bed availability data.
The increased rate of cardiac arrest on the wards with reduced ICU bed availability is consistent with previous studies showing increased mortality in patients refused transfer to the ICU (6) (8) (9) (14), or who experience delays in critical care (21) (22) at times of limited ICU bed availability. Robert and colleagues furthered this and showed an association between refusal of ICU transfer due to a full ICU and increased patient mortality (13). Despite the previous work on outcomes of patients evaluated for ICU admission in the face of ICU bed limitations, we are not aware of any other studies examining the effects of ICU bed limitations on the hospital population as a whole
In subgroup analysis, the increased rate of cardiac arrest with limited ICU bed availability was driven by the availability of MICU beds, which is a unique finding. Over the data collection period, 72% of ward cardiac arrests occurred in patients on a medical service (data not shown). In our hospital, had clinical deterioration been identified in these patients before cardiac arrest, they most likely would have been referred for transfer to the MICU rather than another ICU. Our findings may indicate unintended effects of a higher barrier to ICU admission as sicker patients may remain on the wards where they are at risk for deterioration.
Our study has several implications. The first is the demonstrated need for improved triage of ward patients into the ICU when ICU beds are scarce. While numerous decision-making tools for ICU admission exist, none has proven to improve outcomes (23) (24). Our findings also suggest the need to respond acutely to perturbations in ICU bed availability, particularly accounting for MICU bed availability. During times of increased critical care strain, a flexible, system wide process may help to meet unpredictable surges in critical care demand (25) (26) (27) (28). In addition, the implementation of previously described quality improvement practices to reduce ICU length of stay may increase the number of available beds (29) (30) (31).
There are several important strengths of our study. First, we used prospectively collected data in a large population of both medical and surgical patients. In addition, we accounted for both physical beds and staffing resources in the determination of bed availability, which was not specifically accounted for in earlier studies (23). Finally, our study included all patients at-risk in the general wards rather than just those evaluated by the ICU team.
This study has several limitations. First, this was a single-center study at an academic hospital. Institutional factors, including policies for admission to individual ICUs, may make the findings less generalizable. We conducted our analysis at the shift level and therefore patient-specific data were not available. We therefore did not determine whether the ward patients who suffered cardiac arrest were evaluated for transfer to the ICU prior to their arrest. In addition, we defined our subgroups of medical and non-medical ICUs by the physical bed location rather than admitting service. However, the vast majority of patients in the MICU are on the MICU service. We acknowledge that this is an observational study of a complex system and cannot establish causality between the ICU readmission rate and ICU bed availability. Finally, we examined bed availability per shift rather than ICU turnover or bed availability in real time.
In conclusion, we demonstrated an association between decreased total ICU bed availability and increased rates of unplanned ICU readmissions within twenty-four hours. We also demonstrated an association between decreased total ICU bed availability and increased rates of cardiac arrest on the wards, driven by MICU bed availability. These findings suggest sub optimal triage of patients into the ICU and premature discharge of patients from the ICU when ICU beds are scarce. Additional research is needed to establish optimal triage practices and hospital-wide bed allocation to maximize ICU bed availability for high-risk patients.
Acknowledgments
Financial support: Dr. Edelson is supported by a career development award from the National Heart, Lung, and Blood Institute (K23 HL097157-01).
We thank Nicole Twu, MS for her expert edits and help with the submission. We would like to thank Zahed Haseeb and Munir Gomaa for assistance with data extraction.
Footnotes
Author Contributions: DE obtained the data and supervised the study. MH, JT and TY obtained and transcribed the raw data. Statistical analysis was performed by MC and TY. All authors contributed to the study design and manuscript preparation.
Preliminary versions of these data were presented as an oral presentation at the SHM conference on April 3, 2012 (Orlando, FL) and ATS conference on May 22, 2012 (San Francisco, CA).
Copyright form disclosures: Dr. Edelson received support for article research from NIH, disclosed ownership interest in Quant HC (Chicago, IL), and has a patent pending (ARCD.P0535US.P2). Her institution received grant support from the National Heart, Lung, and Blood Institute; Philips Healthcare; and Laerdal Medical and her institution consulted for EarlySense Inc. Dr. Town is employed by Internal Medicine Residency. The remaining authors disclosed that they do not have any potential conflicts of interest.
References
- 1.Halpern NA, Pastores SM. Critical care medicine in the united states 2000–2005: An analysis of bed numbers, occupancy rates, payer mix, and costs. Crit Care Med. 2010;38:65–71. doi: 10.1097/CCM.0b013e3181b090d0. [DOI] [PubMed] [Google Scholar]
- 2.Needham DM, Bronskill SE, Calinawan JR, et al. Projected incidence of mechanical ventilation in ontario to 2026: Preparing for the aging baby boomers. Crit Care Med. 2005;33:574–579. doi: 10.1097/01.ccm.0000155992.21174.31. [DOI] [PubMed] [Google Scholar]
- 3.Iwashyna TJ, Kramer AA, Kahn JM. Intensive care unit occupancy and patient outcomes. Crit Care Med. 2009;37:1545–1557. doi: 10.1097/CCM.0b013e31819fe8f8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Strauss MJ, LoGerfo JP, Yeltatzie JA, et al. Rationing of intensive care unit services. JAMA. 1986;255:1143–1146. [PubMed] [Google Scholar]
- 5.Singer DE, Mulley AG, Thibault GE. Rationing intensive care - physician responses to a resource shortage. NEJM. 1983;309:1155–1160. doi: 10.1056/NEJM198311103091905. [DOI] [PubMed] [Google Scholar]
- 6.Sinuff T, Kahnamoui K, Cook DJ, et al. Rationing critical care beds: A systematic review. Crit Care Med. 2004;32:1588–1597. doi: 10.1097/01.ccm.0000130175.38521.9f. [DOI] [PubMed] [Google Scholar]
- 7.Baker DR, Pronovost PJ, Morlock LL, et al. Patient flow variability and unplanned readmissions to an intensive care unit. Crit Care Med. 2009;37:2882–2887. doi: 10.1097/ccm.0b013e3181b01caf. [DOI] [PubMed] [Google Scholar]
- 8.Simchen E, Sprung CL, Galai N, et al. Survival of critically ill patients hospitalized in and out of intensive care units under paucity of intensive care unit beds. Crit Care Med. 2004;32:1654–1661. doi: 10.1097/01.ccm.0000133021.22188.35. [DOI] [PubMed] [Google Scholar]
- 9.Iapichino G, Corbella D, Minelli C, et al. Reasons for refusal of admission to intensive care and impact on mortality. Intens care med. 2010;36:1772–1779. doi: 10.1007/s00134-010-1933-2. [DOI] [PubMed] [Google Scholar]
- 10.Metcalfe MA, Sloggett A, McPherson K. Mortality among appropriately referred patients refused admission to intensive-care units. Lancet. 1997;350:711. doi: 10.1016/S0140-6736(96)10018-0. [DOI] [PubMed] [Google Scholar]
- 11.Garrouste-Orgeas M, Montuclard L, Timsit JF, et al. Triaging patients to the icu: A pilot study of factors influencing admission decisions and patient outcomes. Intens Care Med. 2003;29:774–781. doi: 10.1007/s00134-003-1709-z. [DOI] [PubMed] [Google Scholar]
- 12.Stelfox HT, Hemmelgarn BR, Bagshaw SM, et al. Intensive care unit bed availability and outcomes for hospitalized patients with sudden clinical deterioration. Arch Intern Med. 2012;172:467–474. doi: 10.1001/archinternmed.2011.2315. [DOI] [PubMed] [Google Scholar]
- 13.Robert R, Reignier J, Tournoux-Facon C, et al. Association des Reanimateurs du Centre Ouest G. Refusal of intensive care unit admission due to a full unit: Impact on mortality. Am J Respir Crit Care Med. 2012;185:1081–1087. doi: 10.1164/rccm.201104-0729OC. [DOI] [PubMed] [Google Scholar]
- 14.Garrouste-Orgeas M, Montuclard L, Timsit J-Fo, et al. Predictors of intensive care unit refusal in french intensive care units: A multiple-center study*. Crit Care Med. 2005;33:750–755. doi: 10.1097/01.ccm.0000157752.26180.f1. [DOI] [PubMed] [Google Scholar]
- 15.Churpek MM, Yuen TC, Edelson DP. Risk stratification of hospitalized patients on the wards. Chest. 2013;143:1758–1765. doi: 10.1378/chest.12-1605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Churpek MM, Yuen TC, Huber MT, et al. Predicting cardiac arrest on the wards: A nested case-control study. Chest. 2012;141:1170–1176. doi: 10.1378/chest.11-1301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Iapichino G, Gattinoni L, Radrizzani D, et al. Volume of activity and occupancy rate in intensive care units. Association with mortality. Intens Care Med. 2004;30:290–297. doi: 10.1007/s00134-003-2113-4. [DOI] [PubMed] [Google Scholar]
- 18.Glance LG, Li Y, Osler TM, et al. Impact of patient volume on the mortality rate of adult intensive care unit patients. Crit Care Med. 2006;34:1925–1934. doi: 10.1097/01.CCM.0000226415.93237.84. [DOI] [PubMed] [Google Scholar]
- 19.Tarnow-Mordi WO, Hau C, Warden A, et al. Hospital mortality in relation to staff workload: A 4-year study in an adult intensive-care unit. Lancet. 2000;356:185–189. doi: 10.1016/s0140-6736(00)02478-8. [DOI] [PubMed] [Google Scholar]
- 20.Chrusch CA, Olafson KP, McMillan PM, et al. High occupancy increases the risk of early death or readmission after transfer from intensive care. Crit Care Med. 2009;37:2753–2758. doi: 10.1097/CCM.0b013e3181a57b0c. [DOI] [PubMed] [Google Scholar]
- 21.Cardoso LT, Grion CM, Matsuo T, et al. Impact of delayed admission to intensive care units on mortality of critically ill patients: A cohort study. Crit Care. 2011;15:R28. doi: 10.1186/cc9975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sprung CL, Geber D, Eidelman LA, et al. Evaluation of triage decisions for intensive care admission. Crit Care Med. 1999;27:1073–1079. doi: 10.1097/00003246-199906000-00021. [DOI] [PubMed] [Google Scholar]
- 23.Cuthbertson BH, Smith GB. A warning on early-warning scores! BJA. 2007;98:704–706. doi: 10.1093/bja/aem121. [DOI] [PubMed] [Google Scholar]
- 24.DeVita MA, Smith GB, Adam SK, et al. “Identifying the hospitalised patient in crisis”--a consensus conference on the afferent limb of rapid response systems. Resuscitation. 2010;81:375–382. doi: 10.1016/j.resuscitation.2009.12.008. [DOI] [PubMed] [Google Scholar]
- 25.Teres D. Civilian triage in the intensive care unit: The ritual of the last bed. Crit Care Med. 1993;21:598–606. doi: 10.1097/00003246-199304000-00022. [DOI] [PubMed] [Google Scholar]
- 26.Resar R, Nolan K, Kaczynski D, et al. Using real-time demand capacity management to improve hospitalwide patient flow. Jt Comm J Qual Patient Saf. 2011;37:217–227. doi: 10.1016/s1553-7250(11)37029-8. [DOI] [PubMed] [Google Scholar]
- 27.Ryckman FC, Yelton PA, Anneken AM, et al. Redesigning intensive care unit flow using variability management to improve access and safety. Jt Comm J Qual Patient Saf. 2009;35:535–543. doi: 10.1016/s1553-7250(09)35073-4. [DOI] [PubMed] [Google Scholar]
- 28.Soremekun OA, Zane RD, Walls A, et al. Cancellation of scheduled procedures as a mechanism to generate hospital bed surge capacity-a pilot study. Prehosp Disaster Med. 2011;26:224–229. doi: 10.1017/S1049023X11006248. [DOI] [PubMed] [Google Scholar]
- 29.Ely EW, Baker AM, Dunagan DP, et al. Effect on the duration of mechanical ventilation of identifying patients capable of breathing spontaneously. NEJM. 1996;335:1864–1869. doi: 10.1056/NEJM199612193352502. [DOI] [PubMed] [Google Scholar]
- 30.Kress JP, Pohlman AS, O’Connor MF, et al. Daily interruption of sedative infusions in critically ill patients undergoing mechanical ventilation. NEJM. 2000;342:1471–1477. doi: 10.1056/NEJM200005183422002. [DOI] [PubMed] [Google Scholar]
- 31.Girard TD, Kress JP, Fuchs BD, et al. Efficacy and safety of a paired sedation and ventilator weaning protocol for mechanically ventilated patients in intensive care (awakening and breathing controlled trial): A randomised controlled trial. Lancet. 2008;371:126–134. doi: 10.1016/S0140-6736(08)60105-1. [DOI] [PubMed] [Google Scholar]