Abstract
Progressive Audiologic Tinnitus Management (PATM) is based on the premise that tinnitus is managed most efficiently using a hierarchy of clinical services that address different levels of need. PATM includes five levels of management: (a) triage; (b) audiologic evaluation; (c) group education; (d) tinnitus evaluation; and (e) individualized management. This article provides an overview of PATM and focuses on the procedures that make up the Level 2 Audiologic Evaluation. The evaluation is conducted to assess the potential need for medical, audiologic (hearing loss, tinnitus, hyperacusis), and/or mental health services. The Tinnitus Handicap Inventory, Hearing Handicap Inventory, and Tinnitus and Hearing Survey are used to differentiate effects of tinnitus and hearing loss. If indicated, patients are interviewed with the Tinnitus-Impact Screening Interview. Patients requiring amplification receive hearing aids. Often, management of hearing loss at Level 2 addresses any problems that were attributed to the tinnitus, which obviates further tinnitus-specific intervention.
Keywords: auditory, hearing disorders, hearing aids, intervention, assessment, rehabilitation, tinnitus
The method of Audiologic Tinnitus Management (ATM) is a specific and comprehensive protocol for the management of tinnitus by audiologists (J. A. Henry, Zaugg, & Schechter, 2005a, 2005b). Progressive ATM expands on the ATM methodology to create five hierarchical levels of tinnitus-management education and support so that patients are clinically managed only to the degree necessary to meet their needs (J. A. Henry, Zaugg, Myers, & Schechter, 2008). Progressive ATM is a complete program of assessment and intervention but also can serve as a framework to involve other forms of therapy.
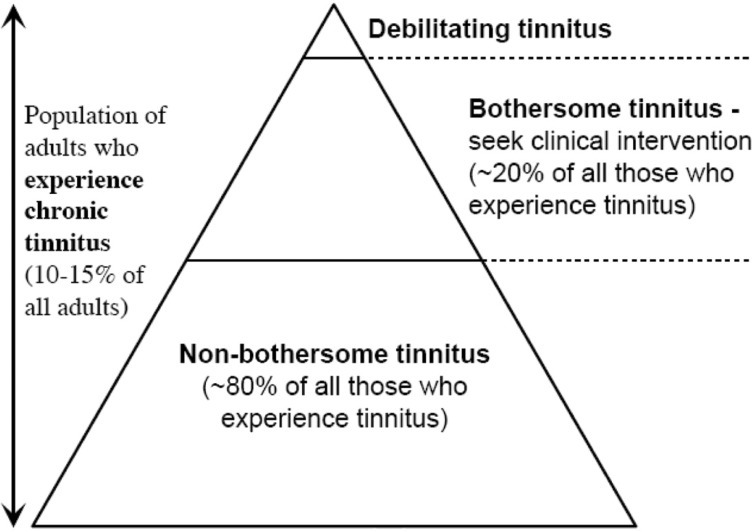
Epidemiological studies indicate that about 10% to 15% of all adults in different countries experience tinnitus (Hoffman & Reed, 2004). Of those, only about 20% require some degree of clinical intervention for their tinnitus (Davis & Refaie, 2000; Jastreboff & Hazell, 1998). These percentages are in general agreement with the American Tinnitus Association's (www.ata.org) estimates that 50 million Americans experience tinnitus, of which 12 million seek clinical care and 2 million are debilitated by their tinnitus. There are, thus, varying degrees of tinnitus effect across the population of all people who experience tinnitus, as illustrated by the “tinnitus pyramid” (see Figure 1; Dobie, 2004). This range of needs is what necessitates a progressive management approach.
Figure 1.
The tinnitus pyramid.
Source: Dobie (2004).
Note: The pyramid includes the entire population of people who experience tinnitus. The majority of these people (in the lower part of the pyramid) are not particularly bothered by it. Many of these people only want assurance that their tinnitus does not reflect some serious medical condition. Relatively few have tinnitus that requires some degree of clinical intervention (bothersome tinnitus). A very small fraction has debilitating tinnitus (in the tip of the pyramid).
The overall goal of Progressive ATM is to minimize the effect of tinnitus on the patient's life as efficiently as possible for both the patient and the audiologist.
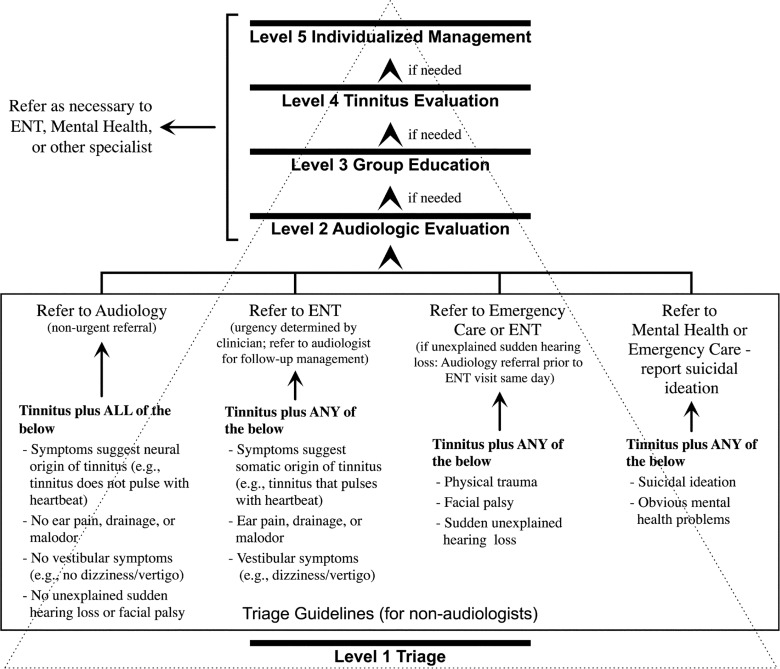
This approach effectively reduces the effort and expenses incurred by the patient and conserves hearing health care management costs. The Progressive ATM model is based on a series of controlled clinical studies that were completed at the National Center for Rehabilitative Auditory Research (NCRAR) and on many years of clinical experience providing tinnitus management services. The model is designed to be maximally efficient, while still addressing the needs of all patients who complain about tinnitus. The Progressive ATM flowchart (see Figure 2) shows the five levels of progressive tinnitus management. Levels 2 through 5 are conducted by audiologists. It is essential, however, that patients are referred to other clinics as necessary to meet any needs that are outside of the scope of practice of audiologists. Each of the five levels is described below. As the main focus of this article, Level 2 is described in detail. Briefer summaries are provided for the other levels.
Figure 2.
The five levels of Progressive Audiologic Tinnitus Management.
Note: Level 1 (triage) is the point of contact for a patient who complains about tinnitus. The referral guidelines (enclosed in the rectangle) at the triage level are intended for non-audiologists who encounter patients complaining of tinnitus. Levels 2 through 5 are administered by audiologists, with referral to other clinics as appropriate. ENT = ear, nose, and throat (otolaryngology)
Level 1 Triage
Patients report tinnitus to health care providers in many different clinics. These providers may be unaware of tinnitus management resources that are available. The triage guidelines that we have developed are intended for use by non-audiologists who encounter patients complaining of tinnitus. These guidelines are shown in Figure 2 (in the rectangle) and indicate four general referral categories (from right to left in the rectangle): (a) psychiatric emergency (refer for immediate mental health assessment or emergency care); (b) medical emergency (refer for immediate otolaryngology examination or emergency care); (c) nonemergency medical condition (refer for near-future otolaryngology and audiology examination); and (d) apparent neural-origin tinnitus with no other symptoms (refer for near-future Level 2 Audiologic Evaluation). The guidelines reflect accepted clinical practices.
Level 2 Audiologic Evaluation
Tinnitus is a symptom of dysfunction within the auditory system and usually is associated with some degree of hearing loss (Coles, 1995; Dobie, 2004). Thus, it is necessary for patients who complain about tinnitus to be evaluated audiologically. The evaluation should assess the potential need for medical and audiologic intervention. (Audiologic intervention refers to hearing intervention and/or tinnitus intervention. In addition, some patients require intervention for reduced sound tolerance.) It sometimes also is appropriate to screen for mental health conditions that can interfere with successful self-management of tinnitus.
The Level 2 evaluation always includes a standard audiologic evaluation and written questionnaires to assess the relative effect of self-perceived hearing problems versus tinnitus problems. When indicated, the Level 2 evaluation also can include a brief structured tinnitus interview and mental health screening questionnaires. A workbook with information about tinnitus and tinnitus management is offered to any patient who experiences problematic tinnitus (J. A. Henry, Zaugg, Schechter, & Myers, 2008). (Contact the first author for information about how to obtain the workbook.) Patients who require amplification receive hearing aids, which often can result in satisfactory tinnitus management with minimal education and support specific to tinnitus. If patients require further tinnitus intervention, then they are referred to attend the Level 3 Group Education sessions.
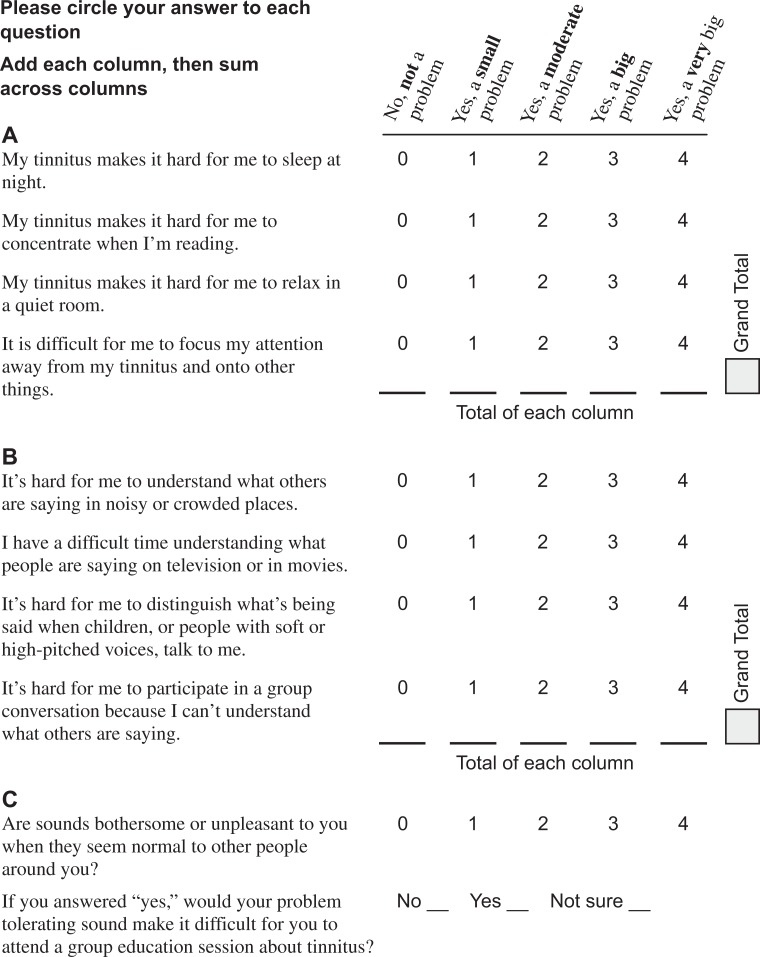
Tinnitus and Hearing Survey
A primary objective of the Level 2 Audiologic Evaluation is to determine if the patient needs audiologic intervention for hearing, tinnitus, or both. Making this determination may not be straightforward because patients often confuse effects of hearing loss with effects of tinnitus (Coles, 1995; Dobie, 2004; Zaugg, Schechter, Fausti, & Henry, 2002). A patient who reports a problem with tinnitus may actually be experiencing a problem only with hearing that is erroneously attributed to the tinnitus. It is difficult to plan appropriate intervention if it is not clear whether the reported distress is due primarily to hearing problems, tinnitus problems, or a combination of the two. The Tinnitus and Hearing Survey (THS; see Appendix A) is an easy-to-administer instrument that is designed to assist in rapidly estimating how much of a reported problem is due to tinnitus and how much is due to a hearing problem. (Note that the THS is not a validated outcome instrument and should not be used as the primary measure of outcomes.) The THS also is used to screen for reduced sound tolerance.
The THS contains three sections that include a total of 10 statements, each with fixed response choices. The four Section A statements describe tinnitus-specific problems that are unrelated to hearing loss. A statement from Section A is, “My tinnitus makes it hard for me to concentrate when I'm reading.” It is clear that trouble concentrating while reading would not be caused by a hearing problem and, thus, tinnitus-specific intervention would be indicated. Section B contains statements that focus on common hearing problems. These statements were selected because they eliminate, or at least minimize, any perceived effects of tinnitus on hearing. An example from Section B is, “It's hard for me to understand what others are saying in noisy or crowded places.” The patient may believe that trouble hearing in a background of sound is caused by tinnitus; however, the problem is best managed with traditional strategies for managing hearing problems and would not be helped by tinnitus-specific intervention.
Patients' ratings for the individual statements in Sections A and B of the THS are added to produce a sum total for each section. Higher numbers for Section A indicate a tinnitus-specific problem, whereas higher numbers for Section B indicate a hearing problem. These results, along with findings from the hearing assessment and written questionnaires, should provide sufficient information to differentiate tinnitus-specific problems from problems associated with hearing loss. This information can be used to assist in identifying an intervention that will best address the problems that are most bothersome to the patient. Management options for Section A problems include provision of the self-help workbook (J. A. Henry, Zaugg, Schechter, & Myers, 2008) and participation in Level 3 Group Education. Management options for Section B include amplification, assistive listening devices, and aural rehabilitation classes.
In Section C of the THS, the first of the two statements determines if the patient has self-perceived hypersensitivity to everyday sounds. If the response is “no,” then screening for reduced sound tolerance is negative and the second statement does not require a response. If the response is “yes,” then the screen is positive and the patient rates the degree of the self-perceived problem (small, moderate, big, or very big). Any patient with a positive screen is given a special loudness tolerance handout (see Appendix B). A positive screen also requires a response to the second statement to determine if the patient feels that the sound tolerance problem would make it difficult to attend a group tinnitus workshop (i.e., Level 3 Group Education). If so, then the patient should have the option of bypassing Level 3 and scheduling a Level 4 Tinnitus Evaluation. These patients require special procedures to assess and treat the sound hypersensitivity. Management options include the special loudness tolerance handout (Appendix B) and, possibly, sound desensitization procedures (J. A. Henry et al., 2005b).
The main purpose of using the THS is to differentiate tinnitus-specific from hearing-specific problems, which is critical for determining if a patient should attend Level 3 Group Education. The THS can be used to informally monitor progress with tinnitus problems relative to progress with hearing problems. This is an important distinction because tinnitus problems and hearing problems may improve at different rates and within different timeframes. The THS also can be used to informally monitor progress with a loudness tolerance problem.
Using the Tinnitus and Hearing Survey to Determine Candidacy for Group Education
The THS is used to assist in determining if a patient should attend the Level 3 Group Education. Following the steps below can help to ensure that patients don't attend the class with the misconception that they will learn to manage a hearing-in-noise problem (which patients often believe is the result of the tinnitus blocking sounds they are trying to hear.)
Explain that group education focuses on finding ways to manage the problems in Section A of the survey. The class does not focus on the Section B problems.
Confirm that the patient is interested in attending a class that addresses the problems in Section A.
Ensure that the patient understands that participating in Level 3 Group Education does not preclude receiving concurrent services for managing hearing problems.
Ensure that the patient did not report a loudness tolerance problem that would make it difficult to attend the Level 3 Group Education.
If requirements 1 through 4 are met, then the patient is likely a candidate for Level 3 Group Education.
Using the Tinnitus and Hearing Survey to Determine Need for Intervention for Reduced Sound Tolerance
Section C of the THS is used to assist in determining if a patient needs intervention for reduced sound tolerance. Following the steps below can help to ensure that reduced loudness tolerance is addressed when needed.
Any patient who reports a sound tolerance problem (of any degree) should receive the sound tolerance handout (Appendix B).
Any patient who reports that a sound tolerance problem would make it difficult to attend group education sessions should be scheduled directly for a Level 4 Tinnitus Evaluation (which includes assessment of loudness tolerance). Level 3 Group Education can be bypassed for these relatively uncommon patients. The Level 4 evaluation should focus on assessing the reduced loudness tolerance, with assessment for tinnitus being a secondary objective.
Tinnitus Handicap Inventory
Standardized tinnitus questionnaires are used to obtain a global index score of a patient's perceived tinnitus severity. It is essential to acquire a baseline index score using a validated outcome instrument prior to conducting any testing or counseling. The Tinnitus Handicap Inventory (THI; Newman, Jacobson, & Spitzer, 1996; Newman, Sandridge, & Jacobson, 1998) is suggested for use as a standardized tinnitus questionnaire because it is widely used, easy to administer, and well documented in the literature. The THI contains 25 statements, and response choices are “no” (0 points), “sometimes” (2 points), and “yes” (4 points). The index score thus can range from 0 to 100. The THI has been documented for internal consistency reliability (Cronbach's α = .93) and test-retest stability (r = .92) (Newman et al., 1998). Handicap severity can be categorized based on the THI index score: severe (58-100), moderate (38-56), mild (18–36), and no handicap (0–16). A change in the total index score of at least 20 points indicates a statistically and clinically significant change in self-perceived tinnitus handicap at the 95% confidence level (Newman & Sandridge, 2004). The THI also includes three subscales: functional, emotional, and catastrophic responses.
The THI and THS are used to accomplish different objectives, and each is important for Progressive ATM. The THI is a statistically validated and widely recognized tool for assessing self-perceived tinnitus handicap, making it appropriate for standardized assessment of management outcomes. A THI index score, however, can be spuriously inflated when patients experience hearing difficulties that they attribute to the tinnitus. Therefore, because the THI index score may at least partially reflect a self-perceived hearing problem, it should not be used by itself to determine candidacy for Level 3 Group Education, which specifically addresses tinnitus problems and not hearing problems. Use of the THS in conjunction with the THI usually provides the information needed for this purpose.
Hearing Handicap Inventory
The Hearing Handicap Inventory (HHI) is used to assess self-perceived hearing handicap. Use of the HHI is recommended as a standard assessment tool for all patients during Level 2 Audiologic Evaluation. Three versions of this questionnaire can be used. The Hearing Handicap Inventory for the Elderly (HHIE) is for patients age 65 and older (Ventry & Weinstein, 1982). The Hearing Handicap Inventory for Adults (HHIA) is for patients younger than 65 years of age (Newman, Weinstein, Jacobson, & Hug, 1990). Both the HHIE and HHIA are 25-item self-assessment scales that include two subscales (emotional and social/situational). The HHIA differs from the HHIE only in that it includes questions about occupational effects of hearing loss. The screening version of the HHIE (HHIE-S) includes 10 items and can be completed in 5 minutes (Lichtenstein, Bess, Logan, & Burger, 1990; Ventry & Weinstein, 1983).
The HHI is a validated instrument that is used routinely in many audiology clinics to determine a patient's self-perceived hearing handicap. Administering the HHI adds little time to the evaluation, and the information obtained contributes toward making a more accurate interpretation of patients' responses to the THI and THS. Results of the HHI provide additional information to better understand how much of a patient's complaints about tinnitus may be attributable to hearing loss.
Evaluate Auditory Function
A standard audiologic assessment provides the information necessary to determine need for referral for medical evaluation and to determine candidacy for audiologic hearing intervention. This is routine practice for audiologists, thus, it is not necessary herein to describe detailed criteria for determining need for medical assessment and audiologic intervention for hearing problems. However, some of the procedures warrant special considerations when patients present with tinnitus.
Otoscopy is performed routinely prior to placing earphones for audiometric testing. Even a small amount of cerumen on the tympanic membrane can create a mass effect resulting in a high frequency conductive hearing loss and tinnitus (Schechter & Henry, 2002). If cerumen management is not performed by a trained audiologist, then patients should be referred as appropriate (ideally to otolaryngology). Referring to other than otolaryngology may introduce increased risk. Ideally, referring physicians will perform otoscopy (and cerumen removal if appropriate) prior to placing an audiology consult.
Pulsed tones often are recommended for use when evaluating pure-tone thresholds in patients with tinnitus (Douek & Reid, 1968; Fulton & Lloyd, 1975; Green, 1972; Yantis, 1994). Investigations, however, have revealed that hearing thresholds generally are the same whether tones are presented in the pulsed or continuous mode (J. A. Henry & Meikle, 1999; Hochberg & Waltzman, 1972; Mineau & Schlauch, 1997). Therefore, it is acceptable to use either pulsed or continuous tones for threshold testing, although the use of pulsed tones may assist some patients in distinguishing between the tones and the tinnitus, especially when the tinnitus pitch is close to the test frequency.
Some patients with tinnitus have trouble tolerating louder sounds, and some report that loud sounds make their tinnitus louder. Therefore, it is important to use caution when conducting suprathreshold audiometric testing. The following guidelines can be helpful: (a) use the softest effective masking sounds during traditional audiometry (the need for masking can be reduced by using insert earphones that increase interaural attenuation); (b) use conservative levels of sound during word recognition testing; and (c) approach reflex threshold and decay testing with particular caution—avoid altogether if not necessary. Full assessment for a complaint of reduced loudness tolerance normally occurs at the Level 4 Tinnitus Evaluation.
Determine Potential Need for Otolaryngology Exam
Ideally, every patient complaining of tinnitus would be examined by an otolaryngologist/otologist (Perry & Gantz, 2000). However, this is not practical or realistic in many cases. Audiologists sometimes are the only health care providers who evaluate patients who complain of tinnitus. Therefore, audiologists must be aware of symptoms and conditions that indicate the need for referral to otolaryngology, which include (a) symptoms consistent with vestibular schwannoma or other retrocochlear pathology; (b) symptoms consistent with Meniere's disease; (c) symptoms consistent with somatic origin (i.e., vascular, muscular, respiratory, or TMJ) of tinnitus; (d) ear pain, drainage, or malodor; (e) vestibular symptoms; (f) new-onset tinnitus or hearing loss; (g) progressive tinnitus; (h) significant conductive loss of undetermined etiology; and (i) unilateral or grossly asymmetrical hearing loss.
The most common type of tinnitus is associated with noise-induced hearing loss (Axelsson & Barrenas, 1992; Penner & Bilger, 1995). These patients usually report that their tinnitus has been fairly stable for years. This common form of tinnitus cannot be corrected surgically, nor is it life threatening. Although a medical exam always is in the patient's best interest, it is reasonable to consider forgoing an otologic exam if all of the following conditions apply: (a) patient reports a history of noise exposure and concurrent or subsequent onset of tinnitus; (b) tinnitus is symmetrical and nonpulsatile; (c) tinnitus is stable and of long duration (6 months or more); and (d) audiogram is consistent with a diagnosis of symmetrical sensorineural hearing loss.
Administer Tinnitus-Impact Screening Interview (if warranted)
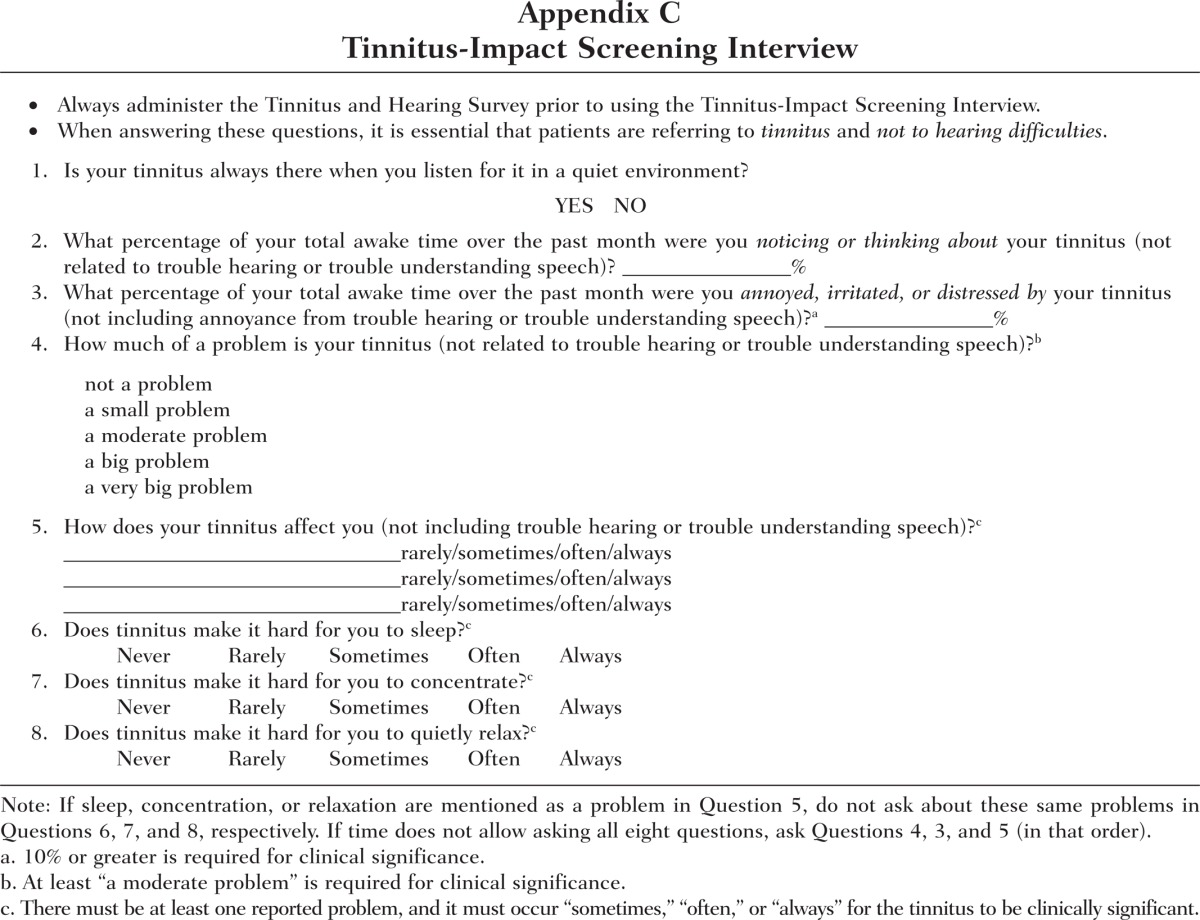
When the above procedures have been completed, the findings should be reviewed with the patient. The patient should understand that complaints listed in Section A of the THS (Appendix A) are specific to tinnitus and are addressed in Level 3 Group Education and that Section B complaints are addressed routinely by audiologists and are not covered in the Level 3 workshops. If there is uncertainty about the patient's candidacy for Group Education, then the Tinnitus-Impact Screening Interview (TISI; J. A. Henry, Schechter, Regelein, & Dennis, 2004; J. A. Henry et al., 2006) can be administered (see Appendix C). The TISI is an eight-question interview that facilitates one-on-one questioning about the most common tinnitus problems and can assist in determining if the tinnitus problem is clinically significant. The TISI can be administered in as little as 5 to 10 minutes but may require up to 15 to 20 minutes.
To assist in determining if a patient's tinnitus is clinically significant, response criteria are provided below. These criteria are, of course, only a general guide and should not be considered definitive.
The tinnitus should be bothersome at least 10% of the time (question 3).
The tinnitus should be reported as a “moderate,” “big,” or “very big” problem (question 4). Individuals who report that their tinnitus is a “small” problem may require only some basic information that can be provided in the course of administering the TISI.
The tinnitus should interfere with some life activity “sometimes,” “often,” or “always.” The activity could be sleep (question 6), concentration (question 7), relaxation (question 8), or any activity reported in question 5 that cannot be explained by a hearing deficit.
The THS (Appendix A) should be adequate for determining if the patient requires further intervention for a tinnitus problem. The TISI (Appendix C) can be used to gain further information if needed. However, the greatest value of the TISI at the Level 2 Audiologic Evaluation may be that it provides a structure to efficiently identify the main tinnitus concerns. With this information, the patient can be counseled more effectively, specifically by pointing out portions of the workbook (J. A. Henry, Zaugg, Schechter, & Myers, 2008) that are most relevant. This can help the patient to appreciate the value of the workbook relative to the particular tinnitus-problem situations, thus increasing the likelihood that the workbook will be used. An additional benefit of using the TISI is that it facilitates one-on-one interaction with the patient, which can help to establish rapport and make the patient feel heard and valued.
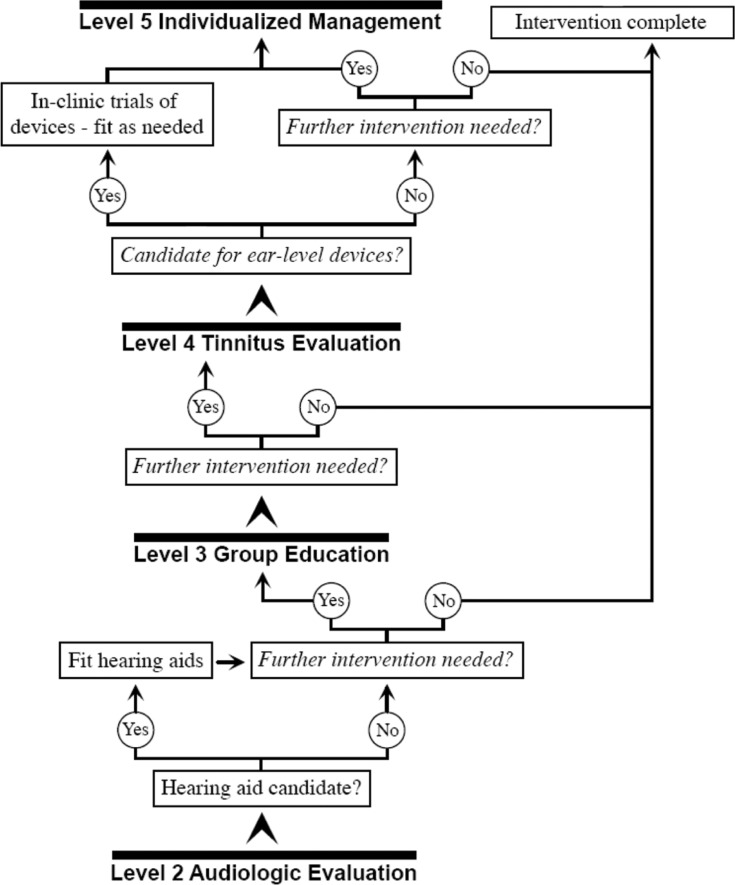
Note: Level 1 is the triage level and does not involve audiology services. The focus of this flowchart is to show how decisions are normally made with regard to the evaluation and fitting of different ear-level devices (hearing aids, noise generators, and combination instruments) that can be used for tinnitus management.
Evaluate for Hearing Aids (if warranted)
Most patients with tinnitus have some degree of hearing loss, and hearing aids sometimes can adequately ameliorate both their hearing and tinnitus problems (Searchfield, 2005; Sheldrake & Jastreboff, 2004). All patients should be advised of the potential for use of hearing aids to reduce the effects of tinnitus as a secondary benefit. They also should be advised about the availability of combination instruments (ear-level devices that combine a noise generator with amplification). In some instances, hearing aids can be used primarily to manage tinnitus, with improved hearing being a secondary benefit (J. A. Henry et al., 2005b).
Figure 3 shows a flowchart of clinical actions for Progressive ATM Levels 2 through 5, with the focus on ear-level devices. At Level 2, hearing-impaired candidates can be offered amplification, assistive listening devices, and education in communication strategies as necessary to maximize their hearing function. Because impaired hearing may be the patient's primary problem (often unknowingly), it is essential to optimize hearing function to the extent possible. Furthermore, patients who progress to Level 3 Group Education require adequate hearing for them to follow the presentation and participate in group discussion. During the workshop, patients who are new hearing aid (and/or assistive listening device) users will receive instruction in how to use these devices (along with many other uses of sound and sound devices) to help manage their tinnitus.
Figure 3.
Flowchart of clinical actions for Progressive Audiologic Tinnitus Management Levels 2 through 5.
Note: Level 1 is the triage level and does not involve audiology services. The focus of this flowchart is to show how decisions are normally made with regard to the evaluation and fitting of different ear-level devices (hearing aids, noise generators, and combination instruments) that can be used for tinnitus management.
During the Level 3 Group Education workshops, patients learn how to use sound (from many sources) to manage their tinnitus. Some of these patients will acquire the skills needed to satisfactorily self-manage their tinnitus and will not need further intervention. Others who require further help after completing the workshops are considered for a Level 4 Tinnitus Evaluation that may include an evaluation for ear-level noise generators and combination instruments (see Figure 3). Because of their personal experience using sound to manage the tinnitus at Level 3, these patients should be well prepared to participate fully in any decision about these special ear-level devices.
For dispensing audiologists, the provision of hearing aids is a routine service with an established skill set. Audiologists are trained and experienced in the selection and fitting of hearing aids for the purpose of improving hearing. If hearing aids are used for tinnitus management, then the audiologist already has most of the skills necessary to perform this service (J. A. Henry et al., 2005a). The method of Progressive ATM makes full use of these existing skills to apply them directly to patients with tinnitus. There are, however, special considerations for the use of hearing aids with these patients, including the following:
The ear canal should be left open as much as possible (or venting should be maximal—as appropriate for slope and degree of loss) to allow normal entry of environmental sound (especially lowest frequency sounds that are not amplified by the hearing aids) and to reduce the sensation of occlusion. Both of these factors can contribute to reducing tinnitus perception.
Hearing aids with feedback reduction circuitry can facilitate the use of open-ear design hearing aids, or larger vent diameters.
Special noise suppression circuitry can actually be a detriment to patients with tinnitus, because noise suppression can reduce background sound that might be helpful in managing tinnitus. What may be a goal for optimal hearing aid performance may be at cross-purposes for tinnitus management. If a patient has hearing aids with multiple memories, then a consideration is to use the “tinnitus” microphone set to omnidirectional and adjusted to minimize the reduction of background sound. (Some hearing aids offer “music” settings, or other settings that minimize use of algorithms to eliminate nonspeech sounds.)
Reduced levels of internal noise also can be detrimental to tinnitus management (in older hearing aids, the floor noise often was helpful when tinnitus was present).
Beneficial effects on tinnitus from the use of amplification may be due to (a) amelioration of communicative difficulties caused by hearing loss but attributed to tinnitus; (b) alleviation of stress associated with difficult listening situations; (c) increase in ambient sound that can mask tinnitus or make it less noticeable; and (d) stimulating impaired portions of the auditory system that have been deprived of sound.
As shown in Figure 3, the preferred approach to providing patients with ear-level instruments is to dispense only hearing aids at Level 2 and not to provide combination instruments or noise/sound generators until after patients have completed Level 3 Group Education. Noise generators and combination instruments should not be an option for patients until they have learned about and implemented different strategies of using sound for tinnitus management, which takes place during Level 3 Group Education. The knowledge and experience gained during Level 3 positions patients to make informed decisions about using noise generators and combination instruments. It always is preferable for patients to learn how to self-manage their tinnitus without having to purchase special devices. These devices can be costly, and their proper use requires multiple appointments with an audiologist who is skilled in the different methods of using the devices. There are additional concerns specific to combination instruments. Combination instruments are produced by only a few hearing aid manufacturers. The concern about using combination instruments has always been that the hearing aid portion has limited features relative to dedicated hearing aids. Thus, although combination instruments have the additional feature of generating broadband noise, that feature may come at the cost of reduced hearing aid performance.
Evaluate for Mental Health Referral (if warranted)
Certain mental health disorders are known to be correlated with the presence and severity of tinnitus (Hoffman & Reed, 2004). Clinical depression and anxiety often affect patients who experience the most problematic tinnitus (Dobie, 2003; Halford & Anderson, 1991; Kirsch, Blanchard, & Parnes, 1989). In addition, some patients suffer from posttraumatic stress disorder (PTSD). Although PTSD often is thought to be specific to military veterans, it actually affects all strata of the population (Department of Veterans Affairs, 2005). PTSD is suspected if the patient reports nightmares, flashbacks, exaggerated startle responses, or excessive anxiety or fear. Although depression, anxiety, and PTSD commonly are associated with tinnitus, many other mental health disorders also may present along with tinnitus. These can include substance abuse (opiates, amphetamines, sedatives, cocaine, marijuana, hallucinogens, etc.), bipolar disorder, psychotic disorders, attention-deficit disorder, panic, phobias, and obsessive-compulsive disorder. All of these conditions, and others, present in clinical settings in varying degrees. Thus, it is important to not limit screening and referral to only mental health conditions that have known or suspected interactions with tinnitus. Failure to properly refer patients for possible mental health conditions reduces the likelihood of achieving the desired outcomes from any tinnitus intervention.
If indicated by the patient's comments or behavior, screening for depression, anxiety, and PTSD can be performed. An audiologist can screen for anxiety using the six-item short form of the state scale of State-Trait Anxiety Inventory (STAI; Spielberger, 1983). The STAI is copyright protected and must be purchased by a qualified provider. A number of self-administered questionnaires are available to screen for depression, including the nine-item Patient Health Questionnaire depression module (PHQ-9; Kroenke, Spitzer, & Williams, 2001). A very brief screening instrument is the two-item version of the PHQ depression module (PHQ-2; Kroenke, Spitzer, & Williams, 2003). Both the PHQ-9 and PHQ-2 have been validated and are available in the public domain (free rights to the public).
The Primary Care PTSD screening tool (PC-PTSD) is available to detect possible PTSD and to initiate appropriate referral (Department of Veterans Affairs, 2005; Prins et al., 2004). The PC-PTSD was designed for use in primary care and other medical settings and currently is used widely to screen for PTSD in military veterans. The four-item instrument enables rapid screening with high sensitivity but low specificity. The PC-PTSD is effective for capturing patients who require further evaluation for possible PTSD (although patients can have active symptoms and fail the screen). A more thorough screen for PTSD can be done using the PTSD Checklist (PCL; Blanchard, Jones-Alexander, Buckley, & Forneris, 1996). The PCL asks about all 17 PTSD symptoms and employs a 5-point response metric. It requires about 7 to 10 minutes to complete (sometimes less). Both the PC-PTSD and the PCL are public domain instruments.
Audiologists must be cautious in dealing with any issues related to anxiety, depression, stress disorders, suicide, and so on because this is not their area of expertise. Audiologists must use the mental health screening tools only to aid in making appropriate referrals and cannot provide diagnostic interpretation of test scores. Some patients may feel uncomfortable with these types of questions or that the questioning is inappropriate and intrusive. For example, patients who have made a suicide attempt in the past or who have been hospitalized for mental health problems might not feel comfortable sharing this information with someone who is not a mental health provider. It is, therefore, important to ask for permission to explore these issues (e.g., “If you don't mind, I would like to ask you some questions about your mood or other psychological questions. Sometimes ringing in the ears is made worse when other conditions are present at the same time”).
The disorder-specific screening tools that we have suggested (STAI, PHQ-2, PHQ-9, PC-PTSD, PCL) address mental health disorders that have been observed commonly to co-occur with tinnitus. Use of these tools, however, does not adequately address the range of other mental health problems that can exist in these patients. Another approach is to use a symptom checklist, which often is included as part of general intake questionnaires in medical clinics. Use of a symptom checklist might reduce a patient's perceived stigma of mental health problems. In some settings, health services are centralized to primary care providers (PCPs). Thus, it might be necessary to refer a patient to a PCP when there is any suspicion of a mental health or sleep disorder. The PCP then assesses the appropriateness of referral to a mental health or sleep clinic. It also is important for audiologists to always seek medical records and scan for comorbid conditions if records are available. Systematic screening is not necessary to justify referring out. The reason for referral often is simply that the audiologist perceives that there are problems outside his or her field of expertise.
Evaluate for Sleep Disorders Referral (if warranted)
Sleep disorders are the most common problem reported by patients with tinnitus (Axelsson & Ringdahl, 1989; Jakes, Hallam, Chambers, & Hinchcliffe, 1985; Meikle, Creedon, & Griest, 2004; Tyler & Baker, 1983). Patients with sleep disorders also tend to have the most severe tinnitus (Erlandsson, Hallberg, & Axelsson, 1992; Folmer & Griest, 2000; Meikle, Vernon, & Johnson, 1984; Scott, Lindberg, Melin, & Lyttkens, 1990). Determining the extent to which tinnitus is the primary or secondary source of sleeping difficulties can be clinically challenging. The patient's sleep patterns over the past month should be queried, either in a questionnaire or in an interview. Two very brief questionnaires are available to screen patients for sleep disorders: the Brief Sleep Questionnaire (BSQ; Rains & Poceta, 2006) and the Epworth Sleepiness Scale (ESS; Johns, 1991). The BSQ is used to screen headache patients for sleep disorders but can be used for patients with tinnitus (by replacing the word headache, which appears three times, with tinnitus). The ESS is the most widely used standardized tool for assessing sleepiness. Completing the ESS provides an index score that can be compared to normative data.
Patients generally are candid about reporting sleep problems because they are less stigmatizing than mental health symptoms. Factors that promote and interfere with good sleep hygiene should be assessed as well as symptoms that suggest other disorders (apnea, nightmares, night terrors, night sweats, overmedication, medication side effects, abuse of stimulants—legal and illegal, hormonal problems, current high psychosocial stressors, chronic pain, home environmental conditions that might interfere with sleep, excessive worry associated with general anxiety disorder, etc.). Patients who have anatomic and functional sleep problems (such as central or obstructive sleep apnea) require medical evaluation for timely diagnosis and treatment. Other symptoms might suggest the need for a psychological or psychiatric evaluation, or assessment by a PCP. For example, psychological interventions can be extremely useful for insomnia, delayed/advanced sleep phase syndrome, and other issues such as nocturnal worry/anxiety and poor sleep hygiene. A PCP referral may be recommended when a patient complains of morning headaches, snoring, waking up gasping for air, excessive daytime sleepiness (e.g., falling asleep at stop signs when driving), restless legs, cataplexy, and so on. If there is doubt, then referral to a PCP is probably the best recourse. It also is important, however, to not refer every patient who complains of a sleep problem for a sleep study, which can be time consuming and expensive. Sleep studies are important for diagnosis and treatment of sleep apnea and other anatomical sleep disorders but are not essential for other sleep-related problems.
If a patient's sleep disorder is a direct consequence of the tinnitus, then effective tinnitus management may bring resolution to the problem. This requires the appropriate use of sound in the sleep environment (J. A. Henry, Zaugg, Myers, & Schechter, 2008). The use of sound is inexpensive and generally harmless. Certain caveats should be considered, however, with respect to the use of therapeutic sound for patients with tinnitus who also complain about sleep. First, if referral is indicated, then a trial of sound therapy prior to investigating the extent and severity of a sleep disorder would be inappropriate. Second, the use of sound can be aversive to some patients. For patients with PTSD, certain sounds may be potent triggers of intrusions, flashbacks, panic attacks, and nightmares. These patients may not like therapeutic sound if it interferes with their hypervigilance (i.e., they may feel that the sound is causing them to miss something in the environment). For these kinds of concerns, it may be prudent to use a general survey of conditions that cause sleep disturbances.
Provide Tinnitus Self-Help Information (if needed)
Tinnitus self-help information should be offered to patients at the end of the evaluation. The information should include specific instructions for using sound as well as recommendations for lifestyle changes to minimize the tinnitus. As already mentioned, we developed a book specific to Progressive ATM that is offered to patients at the end of the evaluation (J. A. Henry, Zaugg, Schechter, & Myers, 2008). The book provides detailed instructions for creating a personalized self-management program based on using sound most effectively (J. A. Henry, Zaugg, Myers, & Schechter, 2008). Frequently asked questions about tinnitus are answered in the book. It is especially important for patients to read the book prior to attending Level 3 Group Education.
Progressive Audiologic Tinnitus Management Approach to Managing Loudness Tolerance Problems
It has been reported by numerous tinnitus clinicians and researchers that a relatively high percentage of tinnitus patients suffer from hyperacusis. In reality, however, most patients who are identified as hyperacusic do not require intervention specific to loudness tolerance. Treatment for reduced sound tolerance in general requires a program of systematic exposure to sound. Patients who use sound to manage their tinnitus with Progressive ATM participate in a systematic program of sound therapy, which indirectly addresses their reduced sound tolerance. By virtue of using sound to manage their tinnitus, these patients are, in effect, receiving the needed sound exposure that would be the key component of treatment for hyperacusis. Therefore, if Progressive ATM patients who have reduced sound tolerance are able to comfortably participate in a program of sound-based tinnitus management, then this tinnitus intervention should be the starting point for these patients. If the reduced sound tolerance is so severe as to preclude sound-based tinnitus management, then these patients should be scheduled for a Level 4 Tinnitus Evaluation that focuses on assessment and management of hyperacusis.
Level 3 Group Education
The Level 2 Audiologic Evaluation addresses the concerns of many patients such that no further tinnitus services are needed. Patients who need more support can participate in the next higher level of intervention, which is Level 3 Group Education.
Recent evidence supports the use of group education as a basic form of tinnitus intervention. Group education has been shown to be effective as part of a hierarchical tinnitus rehabilitation program at a major tinnitus clinic (Newman & Sandridge, 2005; Sandridge & Newman, 2005). We completed a randomized clinical trial evaluating group education for tinnitus in almost 300 patients who showed significantly more reduction in tinnitus severity for those in the education group as compared with control groups (J. A. Henry et al., 2007). Some advantages to using a group education format include the following: (a) education and support can be provided to more patients in less time, maximizing available resources; (b) patients are empowered to make informed decisions about self-management and further tinnitus intervention options; and (c) patients can support and encourage each other.
Level 3 Group Education normally includes two sessions separated by about 2 weeks. During the first session, the principles of using sound to manage tinnitus are explained, and each participant uses the Sound Plan Worksheet (J. A. Henry, Zaugg, Myers, & Schechter, 2008; J. A. Henry, Zaugg, Schechter, & Myers, 2008) to develop an individualized “sound plan” to use to manage their most bothersome tinnitus situation. (The Sound Plan Worksheet can be seen in the appendix of the companion article in this issue of Trends in Amplification.) Using the worksheet involves six steps, the first four of which make up the sound plan: (a) Write down the most bothersome tinnitus situation; (b) select one or more of three strategies for using sound to manage the situation; (c) write down the type of sound that will be used with each strategy; (d) write down the type of sound-generating device that will be used with each strategy; (e) implement the plan for at least 1 week; and (f) evaluate the effectiveness of the plan for managing the most bothersome tinnitus situation. Additional details of these six steps can be found in the companion article (J. A. Henry, Zaugg, Myers, & Schechter, 2008). Patients are instructed to use the sound plan until the second workshop, at which time they discuss their experiences using the plan and its effectiveness. The audiologist facilitates the discussion and addresses any questions or concerns. Further information about managing tinnitus is then presented, and the participants revise their sound plan based on the discussion and new information. Further workshops can be scheduled if needed.
The main goal of the two workshops is for the participants to go through the process of developing a plan for using sound to manage their most bothersome tinnitus situation, to use the plan, and to learn how to modify the plan. The entire process is broken down into small achievable steps, which is consistent with principles of self-efficacy for facilitating motivation to perform a beneficial behavior (Bandura, 1977a, 1977b). The worksheet is intended to be used on an ongoing basis to develop individual plans to use sound to manage any situation in which the tinnitus is problematic.
Level 4 Tinnitus Evaluation
Many patients can satisfactorily self-manage their tinnitus after participating in Level 3 Group Education. Patients who need more support and education than is available at Level 3 can progress to the Level 4 Tinnitus Evaluation to determine their needs for further intervention. As previously described (J. A. Henry et al., 2005a), a comprehensive tinnitus evaluation includes an intake interview and a tinnitus psychoacoustic assessment. Administration of the intake interview is the primary means of determining if one-on-one individualized tinnitus management is needed. If so, then the audiologist and patient begin to formulate a management plan. Special procedures are used to select devices for tinnitus management, including ear-level noise generators and combination instruments as well as personal listening devices.
Systematic progression through the different levels of Progressive ATM effectively ensures that patients reaching the Level 4 Tinnitus Evaluation have a tinnitus problem sufficiently severe as to warrant a comprehensive tinnitus assessment. Due to the severity of their tinnitus, these patients also are more likely to have comorbid mental health conditions or sleep disorders that would require a multidisciplinary approach to management. Screening for mental health conditions and sleep disorders, therefore, is normally conducted at the Level 4 Tinnitus Evaluation. We have described above the different screening tools that can be used for this purpose. A routine battery of screening tests can involve use of the STAI, PHQ-2, PC-PTSD, BSQ, and ESS. Use of these tests will screen for anxiety, depression, PTSD, and sleep disorders—the conditions that have been observed to co-occur most commonly in patients with severe tinnitus. The screening requires about 15 minutes, and the results can be very helpful in determining the potential need to involve other disciplines in the patient's management.
Following completion of the Level 4 Tinnitus Evaluation, patients must meet certain criteria to be considered for Level 5 Individualized Management: (a) Levels 1 through 4 of Progressive ATM have not met their needs. (b) They have been evaluated and referred as appropriate for care by other health care disciplines (otolaryngology, mental health, etc.). (c) They are motivated and capable of complying with all requirements of Level 5 Individualized Management. If these criteria are met, then a management plan is discussed (including device options and potential duration of management). Patients need to understand the requirements of the management program and agree to the requirements. If so, then they are scheduled for an initial appointment to start the management program.
Level 5 Individualized Management
Individualized management is needed by relatively few patients. Level 5 Individualized Management involves use of the same principles of using sound to manage tinnitus that are presented in Level 3 Group Education. However, at Level 5, there is evaluation for use of ear-level sound generators or combination instruments, and the education and support is provided in a one-on-one format with more intense and individualized assistance in using sound to manage tinnitus. Implementing the Progressive ATM model of using sound to manage tinnitus (J. A. Henry, Zaugg, Myers, & Schechter, 2008) at Level 5 best capitalizes on all of the education provided to the patient up to this point. If the patient does not make satisfactory progress after about 6 months, then a different form of management can be considered. Further options for intervention at Level 5 include (in alphabetical order) Cognitive-Behavioral Therapy (J. L. Henry & Wilson, 2001), Neuromonics Tinnitus Treatment (Davis, Paki, & Hanley, 2007), Tinnitus Masking (Vernon & Meikle, 2000), and Tinnitus Retraining Therapy (Jastreboff & Hazell, 2004). There is no definitive evidence that any one of these behavioral methods is more effective than any other.
Conclusion
People who experience tinnitus often do not have access to clinical services. Moreover, intervention that is offered may include any number of unproven remedies. Professional standards specifying minimum elements of tinnitus management do not exist, and such standards are greatly needed. Nonetheless, several behavioral methodologies are available that can be implemented effectively for the majority of people who complain of tinnitus. Clinicians should be aware that tinnitus usually is experienced as a relatively innocuous condition that does not require clinical intervention. Patients who do require intervention differ greatly with respect to the extent of intervention needed. Management approaches also are affected by individual patient characteristics, such as personality, emotional state, degree of hearing loss, general health, and life circumstances. Most of these factors can be adequately assessed during the Level 2 Audiologic Evaluation, using the tools that have been described in this article. A proper assessment is essential to determine the most expedient course of action for the patient.
Progressive ATM as it is described here is designed for application at any audiology clinic that desires to optimize resourcefulness, cost efficiency, and expedience in its practice of tinnitus management. Use of these recommendations should lead to more widespread and consistent tinnitus assessment and management by both VA and non-VA audiologists.
Appendix A: Tinnitus and Hearing Survey
Appendix B: What To Do When Everyday Sounds Are Too Loud (not related to using hearing aids)
Bill Smith is bothered by everyday sounds. (This problem is sometimes called hyperacusis.) Kitchen sounds and the vacuum cleaner are too loud for him. He is bothered by road noise when he drives. It seems like everything at church is too loud. What should Bill do? Believe it or not, being around more sound can make things better! And, staying away from sound can make his problem worse! What??? He should add more sound??? Keep reading and we'll explain…
There are three things you can do if everyday sounds are too loud for you
Keep yourself surrounded with sound that is comfortable for you.
Listen to sounds that you enjoy as often as you can.
Only wear hearing protection when you really need to.
1. Keep yourself surrounded with sound that is comfortable for you
Why should I keep myself surrounded with sound? Let's start by thinking about your eyes and how they adjust to light. Imagine sitting in a dark movie theater and then going outside into the daylight. Everything seems brighter to you than it does to people who were not sitting in the dark. Your eyes had adjusted to the dark and now they have to readjust to the daylight.
Your ears adjust to sound kind of like your eyes adjust to light. If you stay away from sound, your ears will slowly adjust to the quiet. After a while, everyday sounds will seem louder and harder to tolerate. Avoiding sound will only make the problem worse.
If you keep yourself surrounded with sound, your ears will readjust. It will slowly become easier for you to tolerate everyday sounds. You should only use sounds that are comfortable for you. It usually takes at least a few weeks of being around sound for this change to happen.
How do I keep myself surrounded with sound? You can use any sound that is not annoying. (The sound can be either neutral or pleasant.) Here are some ideas:
listen to music at a comfortable level
listen to radio shows
play recordings of nature sounds
keep a fan running
use a tabletop water fountain
Another choice: Some people wear small devices in their ears that make a “shhh” sound. These devices are called in-the-ear noise generators or maskers. Your audiologist can tell you more about them.
2. Listen to sounds that you enjoy as often as you can.
Why should I listen to sounds that I enjoy as often as I can? We just talked about the problem of everyday sounds being too loud (hyperacusis). Many people also have another problem. They just don't like certain sounds, but not because they are too loud. (This problem is sometimes called misophonia.) If you don't like certain sounds, you should make a point of listening to sounds that you enjoy. Spending time enjoying sound can help you get better at tolerating everyday sounds that you don't like.
3. Only wear hearing protection when you really need to.
Why should I use ear protection only when I really need to? When everyday sounds seem too loud, some people start using ear protection all the time. Remember that avoiding sound will make the problem worse. Only use ear protection when sounds are dangerously loud or uncomfortably loud. As soon as the sound around you is at a safe and comfortable level, take the ear protection off. The goal is to wear ear protection only when needed.
Use earplugs or earmuffs only when:
sounds around you are uncomfortably loud
-
you are around dangerously loud sounds like:
lawn mowers
loud concerts
power tools
guns
etc.
Is there any research? Yes. In 2002 Dr. Craig Formby1 and Susan Gold studied sound tolerance.
-
There were two groups of people:
One group wore earplugs for 2 weeks
The other group wore in-the-ear noise generators (maskers) that make a “shhh” sound
-
After 2 weeks:
The people who wore earplugs could tolerate less sound than before
The people who wore maskers could tolerate more sound than before
-
This study showed that:
Adding sound makes it easier to tolerate sound
Staying in quiet makes it harder to tolerate sound
Bottom line
If everyday sounds bother you:
Surrounding yourself with comfortable sound will help
Avoiding sound will make the problem worse
How long does it take?
It can take weeks or months for your ears to adjust.
Talk to your audiologist if you have any questions.
Appendix C: Tinnitus-Impact Screening Interview
Footnotes
Formby, C., & Gold, S. L. (2002). Modification of loudness discomfort level: Evidence for adaptive chronic auditory gain and its clinical relevance. Seminars in Hearing, 23, 21–21.
References
- Axelsson A., Barrenas M.-L. (1992). Tinnitus in noise-induced hearing loss. In Dancer A. L., Henderson D., Salvi R. J., Hamnernik R. P. (Eds.), Noise-induced hearing loss (pp. 269–276). St. Louis, MO: Mosby-Year Book [Google Scholar]
- Axelsson A., Ringdahl A. (1989). Tinnitus: A study of its prevalence and characteristics. British Journal of Audiology, 23, 53–62 [DOI] [PubMed] [Google Scholar]
- Bandura A. (1977a). Self-efficacy: Toward a unifying theory of behavioral change. Psychological Review, 84(2), 191–215 [DOI] [PubMed] [Google Scholar]
- Bandura A. (1977b). Social learning theory. Englewood Cliffs, NJ: Prentice Hall [Google Scholar]
- Blanchard E. B., Jones-Alexander J., Buckley T. C., Forneris C. A. (1996). Psychometric properties of the PTSD Checklist (PCL). Behaviour Research and Therapy, 34(8), 669–673 [DOI] [PubMed] [Google Scholar]
- Coles R.R.A. (1995). Classification of causes, mechanisms of patient disturbance, and associated counseling. In Vernon J. A., Moller A. R. (Eds.), Mechanisms of tinnitus (pp. 11–19). Needham Heights, MA: Allyn & Bacon [Google Scholar]
- Davis A., Refaie A. E. (2000). Epidemiology of tinnitus. In Tyler R. (Ed.), Tinnitus handbook (pp. 1–23). San Diego: Singular [Google Scholar]
- Davis P. B., Paki B., Hanley P. J. (2007). Neuromonics Tinnitus Treatment: Third clinical trial. Ear and Hearing, 28(2), 242–259 [DOI] [PubMed] [Google Scholar]
- Department of Veterans Affairs. (2005). Screening for PTSD in a primary care setting. Retrieved March 12, 2005, from http://www.ncptsd.va.gov/facts/disasters/fs_screen_disaster.html
- Dobie R. A. (2003). Depression and tinnitus. Otolaryngologic Clinics of North America, 36(2), 383–388 [DOI] [PubMed] [Google Scholar]
- Dobie R. A. (2004). Overview: Suffering from tinnitus. In Snow J. B. (Ed.), Tinnitus: Theory and management (pp. 1–7). Lewiston, NY: BC Decker [Google Scholar]
- Douek E., Reid J. (1968). The diagnostic value of tinnitus pitch. Journal of Laryngology and Otology, 82, 1039–1042 [DOI] [PubMed] [Google Scholar]
- Erlandsson S. I., Hallberg L.R.M., Axelsson A. (1992). Psychological and audiological correlates of perceived tinnitus severity. Audiology, 31, 168–179 [DOI] [PubMed] [Google Scholar]
- Folmer R. L., Griest S. E. (2000). Tinnitus and insomnia. American Journal of Otolaryngology, 21(5), 287–293 [DOI] [PubMed] [Google Scholar]
- Formby C., Gold S. L. (2002). Modification of loudness discomfort level: Evidence for adaptive chronic auditory gain and its clinical relevance. Seminars in Hearing, 23, 21–35 [Google Scholar]
- Fulton R. T., Lloyd L. L. (1975). Auditory assessment of the difficult-to-test. Baltimore: Williams & Wilkins Co. [Google Scholar]
- Green D. S. (1972). Pure tone air conduction thresholds. In Katz J. (Ed.), Handbook of clinical audiology (1st ed., pp. 67–86). Baltimore: Williams & Wilkins Co. [Google Scholar]
- Halford J.B.S., Anderson S. D. (1991). Anxiety and depression in tinnitus sufferers. Journal of Psychosometric Research, 35, 383–390 [DOI] [PubMed] [Google Scholar]
- Henry J. A., Loovis C., Montero M., Kaelin C., Anselmi K. A., Coombs R., et al. (2007). Randomized clinical trial: Group counseling based on Tinnitus Retraining Therapy. Journal of Rehabilitation Research and Development, 44(1), 21–32 [DOI] [PubMed] [Google Scholar]
- Henry J. A., Meikle M. B. (1999). Pulsed versus continuous tones for evaluating the loudness of tinnitus. Journal of the American Academy of Audiology, 10, 261–272 [PubMed] [Google Scholar]
- Henry J. A., Schechter M. A., Regelein R. T., Dennis K. C. (2004). Veterans and tinnitus. In Snow J. B. (Ed.), Tinnitus: Theory and management (pp. 337–355). Lewiston, NY: BC Decker [Google Scholar]
- Henry J. A., Schechter M. A., Zaugg T. L., Griest S. E., Jastreboff P. J., Vernon J. A., et al. (2006). Outcomes of clinical trial: Tinnitus Masking vs. Tinnitus Retraining Therapy. Journal of the American Academy of Audiology, 17, 104–132 [DOI] [PubMed] [Google Scholar]
- Henry J. A., Zaugg T. L., Myers P. J., Schechter M. A. (2008). Using therapeutic sound with Progressive Audiologic Tinnitus Management. Trends in Amplification, 12, 188–209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henry J. A., Zaugg T. L., Schechter M. A. (2005a). Clinical guide for Audiologic Tinnitus Management I: Assessment. American Journal of Audiology, 14, 21–48 [DOI] [PubMed] [Google Scholar]
- Henry J. A., Zaugg T. L., Schechter M. A. (2005b). Clinical guide for Audiologic Tinnitus Management II: Treatment. American Journal of Audiology, 14, 49–70 [DOI] [PubMed] [Google Scholar]
- Henry J. A., Zaugg T. L., Schechter M. A., Myers P. J. (2008). How to manage your tinnitus: A step-by-step workbook. Portland, OR: VA National Center for Rehabilitative Auditory Research [Google Scholar]
- Henry J. L., Wilson P. H. (2001). The psychological management of chronic tinnitus. Needham Heights, MA: Allyn & Bacon [Google Scholar]
- Hochberg I., Waltzman S. (1972). Comparison of pulsed and continuous tone thresholds in patients with tinnitus. Audiology, 11, 337–342 [DOI] [PubMed] [Google Scholar]
- Hoffman H. J., Reed G. W. (2004). Epidemiology of tinnitus. In Snow J. B. (Ed.), Tinnitus: Theory and management (pp. 16–41). Lewiston, NY: BC Decker [Google Scholar]
- Jakes S. C., Hallam R. S., Chambers C., Hinchcliffe R. (1985). A factor analytical study of tinnitus complaint behaviour. Audiology, 24, 195–206 [DOI] [PubMed] [Google Scholar]
- Jastreboff P. J., Hazell J.W.P. (1998). Treatment of tinnitus based on a neurophysiological model. In Vernon J. A. (Ed.), Tinnitus treatment and relief (pp. 201–217). Needham Heights, MA: Allyn & Bacon [Google Scholar]
- Jastreboff P. J., Hazell J.W.P. (2004). Tinnitus Retraining Therapy: Implementing the neurophysiological model. New York: Cambridge University Press [Google Scholar]
- Johns M. W. (1991). A new method for measuring daytime sleepiness: The Epworth Sleepiness Scale. Sleep, 14(6), 540–545 [DOI] [PubMed] [Google Scholar]
- Kirsch C. A., Blanchard E. B., Parnes S. M. (1989). Psychological characteristics of individuals high and low in their ability to cope with tinnitus. Psychosomatic Medicine, 51, 209–217 [DOI] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R. L., Williams J. B. (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R. L., Williams J. B. (2003). The Patient Health Questionnaire-2: Validity of a two-item depression screener. Medical Care, 41(11), 1284–1292 [DOI] [PubMed] [Google Scholar]
- Lichtenstein M. J., Bess F. H., Logan S. A., Burger M. C. (1990). Deriving criteria for hearing impairment in the elderly: A functional approach. Journal of the American Academy of Audiology, 1(1), 11–22 [PubMed] [Google Scholar]
- Meikle M. B., Creedon T. A., Griest S. E. (2004). Tinnitus archive (2nd ed.). Retrieved April 15, 2008, from http://www.tinnitusarchive.org/
- Meikle M. B., Vernon J., Johnson R. M. (1984). The perceived severity of tinnitus. Otolaryngology—Head and Neck Surgery, 92(6), 689–696 [DOI] [PubMed] [Google Scholar]
- Mineau S. M., Schlauch R. S. (1997). Threshold measurement for patients with tinnitus: Pulsed or continuous tones. American Journal of Audiology, 6, 52–56 [Google Scholar]
- Newman C. W., Jacobson G. P., Spitzer J. B. (1996). Development of the Tinnitus Handicap Inventory. Archives of Otolaryngology—Head and Neck Surgery, 122, 143–148 [DOI] [PubMed] [Google Scholar]
- Newman C. W., Sandridge S. A. (2004). Tinnitus questionnaires. In Snow J. B. (Ed.), Tinnitus: Theory and management (pp. 237–254). Lewiston, NY: BC Decker [Google Scholar]
- Newman C. W., Sandridge S. A. (2005). Incorporating group and individual sessions into a tinnitus management clinic. In Tyler R. S. (Ed.), Tinnitus treatment: Clinical protocols (pp. 187–197). New York: Thieme [Google Scholar]
- Newman C. W., Sandridge S. A., Jacobson G. P. (1998). Psychometric adequacy of the Tinnitus Handicap Inventory (THI) for evaluating treatment outcome. Journal of the American Academy of Audiology, 9, 153–160 [PubMed] [Google Scholar]
- Newman C. W., Weinstein B. E., Jacobson G. P., Hug G. A. (1990). The Hearing Handicap Inventory for Adults: Psychometric adequacy and audiometric correlates. Ear and Hearing, 11, 430–433 [DOI] [PubMed] [Google Scholar]
- Penner M. J., Bilger R. C. (1995). Psychophysical observations and the origin of tinnitus. In Vernon J. A., Moller A. R. (Eds.), Mechanisms of tinnitus (pp. 219–230). Needham Heights, MA: Allyn & Bacon [Google Scholar]
- Perry B. P., Gantz B. J. (2000). Medical and surgical evaluation and management of tinnitus. In Tyler R. S. (Ed.), Tinnitus handbook (pp. 221–241). San Diego: Singular [Google Scholar]
- Prins A., Ouimette P., Kimerling R., Cameron R. P., Hugelshofer D. S., Shaw-Hegwer J., et al. (2004). The Primary Care PTSD screen (PC-PTSD): Development and operating characteristics. Primary Care Psychiatry, 9, 9–14 [Google Scholar]
- Rains J. C., Poceta J. S. (2006). Headache and sleep disorders: Review and clinical implications for headache management. Headache, 46(9), 1344–1363 [DOI] [PubMed] [Google Scholar]
- Sandridge S. A., Newman C. W. (2005). Benefits of group informational counseling. In Dauman R. (Ed.), VIIIth International Tinnitus Seminar (pp. 106). Bordeaux, France: Ear, Nose, and Throat Department, University Hospital of Bordeaux [Google Scholar]
- Schechter M. A., Henry J. A. (2002). Assessment and treatment of tinnitus patients using a “masking approach.” Journal of the American Academy of Audiology, 13, 545–558 [PubMed] [Google Scholar]
- Scott B., Lindberg P., Melin L., Lyttkens L. (1990). Predictors of tinnitus discomfort, adaptation and subjective loudness. British Journal of Audiology, 24, 51–62 [DOI] [PubMed] [Google Scholar]
- Searchfield G. D. (2005). Hearing aids and tinnitus. In Tyler R. S. (Ed.), Tinnitus treatment: Clinical protocols (pp. 161–175). New York: Thieme [Google Scholar]
- Sheldrake J. B., Jastreboff M. M. (2004). Role of hearing aids in management of tinnitus. In Snow J. B. (Ed.), Tinnitus: Theory and management (pp. 310–313). Lewiston, NY: BC Decker [Google Scholar]
- Spielberger C. D. (1983). State-Trait Anxiety Inventory for Adults. Palo Alto, CA: Mind Garden [Google Scholar]
- Tyler R. S., Baker L. J. (1983). Difficulties experienced by tinnitus sufferers. Journal of Speech and Hearing Disorders, 48, 150–154 [DOI] [PubMed] [Google Scholar]
- Ventry I. M., Weinstein B. E. (1982). The Hearing Handicap Inventory for the Elderly: A new tool. Ear and Hearing, 3, 128–134 [DOI] [PubMed] [Google Scholar]
- Ventry I. M., Weinstein B. E. (1983). Identification of elderly people with hearing problems. Asha, 25(7), 37–42 [PubMed] [Google Scholar]
- Vernon J. A., Meikle M. B. (2000). Tinnitus masking. In Tyler R. S. (Ed.), Tinnitus handbook (pp. 313–356). San Diego: Singular [Google Scholar]
- Yantis P. A. (1994). Puretone air-conduction threshold testing. In Katz J. (Ed.), Handbook of clinical audiology (pp. 97–108). Baltimore: Williams & Wilkins Co. [Google Scholar]
- Zaugg T. L., Schechter M. A., Fausti S. A., Henry J. A. (2002). Difficulties caused by patients' misconceptions that hearing problems are due to tinnitus. In Patuzzi R. (Ed.), Proceedings of the Seventh International Tinnitus Seminar (pp. 226–228). Crawley: University of Western Australia [Google Scholar]