SUMMARY
Previous studies have reported that health sciences students are at greater risk for tuberculosis infection, especially in developing countries. The objective of this study was to estimate the prevalence, incidence, and factors associated with latent tuberculosis infection among Health Sciences students in Peru. Students enrolled at private university (in Lima – Peru) are tested annually for tuberculosis infection by tuberculin skin test. Data on tuberculin skin test results between 2002 and 2009 was used in this retrospective cohort study, a total of 4842 students were included. Tuberculin skin test conversion was defined as the change of tuberculin skin test from negative (<10 mm) to positive (≥10 mm) after 48 –72 h of inoculation. Baseline tuberculin skin test positivity was 1.0% (95%CI: 0.6%–1.3%), whereas tuberculin skin test conversion incidence was 12.4 per 100 person-years (95%CI: 11.8–13.0). This study showed that students from clinical careers in close contact with patients had an increased risk of tuberculosis infection in the internship, especially Medicine, Dentistry, Medical Technology and Nursing. Administrative, environmental and personal protection measures should be implemented and evaluated periodically in order to reduce the risk of exposure.
Keywords: Tuberculosis, Undergraduate students, Health occupations, Tuberculin test, Infection, Transmission
1. Introduction
Tuberculosis (TB) is a public health problem worldwide, with an estimated number of 8.8 million new cases and 1.1 million deaths in 2010.1 Greater incidence rates have been observed in developing countries due to high levels of poverty, low income, inadequate distribution of resources and malnutrition, all of which limit the impact of disease control strategies.2 Among Latin American countries, Peru had one of the highest TB incidence rates (106 per 100,000 person-years) in 2010.1
Health workers experience greater vulnerability to TB because of close contact and frequent exposure to TB patients, inappropriate environmental conditions in hospitals, and limited or lack of biosafety measures.3,4 For example, in 1999 at one Peruvian national hospital, the incidence of active TB among health workers was found to be 1.2% per year,5 nine times the national TB incidence rate. Additionally, this report found that 16.6% of patients diagnosed between 1994 and 2007 in the Peruvian TB control program were health workers.5
Prevalence of tuberculosis skin test (TST) positivity in health care workers ranges between 33% and 79%, whereas rates of TST conversion varies between 0.5% and 20%,6–9 although only 5% of newly infected cases develop active disease after two years of infection.10,11
Students of the health sciences often have patient contact during their training and are exposed to TB.12 For this population, annual TST conversion rate fluctuates between 3.4% and 18.1%,13,14 with greater risk during clinical rotations13,15 and the final years of their training.13,16,17 Inappropriate implementation of biosafety measures in hospitals that host clinical rotations18 and limited knowledge about TB transmission mechanisms17 may be responsible for these findings.
The main objective of this study was to estimate the incidence and factors associated with TST conversion among health sciences students at a private university in Lima, Peru. In addition, the baseline prevalence of TST positivity in this group was estimated.
2. Methods
2.1. Study design, setting, and participants
This is a retrospective cohort study using data from baseline and follow-up clinical evaluations performed annually on undergraduate health science students at the Universidad Peruana Cayetano Heredia (UPCH) in Lima, Peru.
UPCH is a private, non-profit university located in Lima, Peru, with eight schools and more than 6000 students per year. UPCH is the leading university in Peru in medicine and health sciences, and provides undergraduate and post-graduate education. The main careers at UPCH are Medicine, Medical Technology, Dentistry, Health Administration, Nursing, Education, Sciences, Veterinary Medicine and Psychology. Each career takes 5 years to complete with the exception of Medicine which is a 7-year career.
We analyzed data from 2002 to 2009. Since this is a secondary analysis, only students with complete information were considered.
2.2. Definition of variables
TST positivity at baseline was defined as a student having a positive TST result (≥10 mm) in the first year (baseline)19,20; whereas TST conversion was defined as the TST change from negative (<10 mm) to positive (≥10 mm) after 48–72 h of inoculation using the Mantoux method during follow-up.21 Students with a positive TST at baseline were excluded from the analysis of TST conversion. Follow-up time was defined as the number of years up to TST conversion among students starting with a negative TST result.
The variable career was categorized into three groups: veterinary, non-clinical and clinical. Clinical careers included Dentistry, Nursing, Medical Technology and Medicine. Careers with infrequent contact with TB patients (Education, Sciences, and Health Administration) were grouped as “non-clinical careers” and used as a reference category. Even among the clinical careers, students do not have contact with patients or hospital environments during their first year. In subsequent years, the curriculum requires training in hospital settings, increasing their contact with patients. The final year for each career is an internship, a full-time practicum at a hospital. Medical students also have an externship during their second to last year, which also implies long-term, close contact with patients in a hospital. Veterinary students have some exposure to animals in their second year; this exposure increases during their 4th and 5th years of study. During their last year, the Veterinary students are also exposed to human patients at a hospital while studying zoonotic diseases.
Other variables considered in the analysis were: age, categorized according to quartiles; body mass index (BMI) categorized as ≤18.5 (underweight), 18.5 to <25 (normal), and ≥25 (overweight/obesity)22; self-reported prior TB contact, asked during their baseline medical exam and defined as having had close contact with a relative with TB in the last year; year of career, defined as the year ended for the student at the moment of the clinical exam; and internship (yes vs. no), defined as being in the last year of the career.
2.3. Procedures
All students are required to go through an annual medical examination which includes a physical examination, as well as questions regarding medical and psychological history. All clinical assessments are performed using routine procedures at a private clinic selected by UPCH. During the evaluations students are tested for TB infection by TST using a standardized protocol.19 Data from these visits was collected through an electronic health record system.
2.4. Data analysis
First, a description of the population was performed comparing students with complete information versus those without complete information using Chi squared tests. All of the remaining analyses only included students with complete information. Second, prevalence and 95% confidence intervals (95%CI) were calculated at baseline and for the last available evaluation for each student. Third, incidence density (per 100 person-years) and 95% CIs were calculated using information on TST conversion including only students with a negative TST at baseline and at least one follow-up evaluation. Those students with a TST conversion during follow-up were not considered in further incidence analysis. Incidence density was also calculated by career, year of career and by calendar year.
Finally, using a forward stepwise technique, incidence rate ratio (IRR) and 95%CI for variables associated with TST conversion were obtained using generalized linear models with binomial family, log link and data analysis for correlated data. In addition, only using information from the last two years of career, a secular trend for TST conversion incidence was calculated using Chi square for trend. All data analysis was performed using STATA 11 (STATA Corporation, College Station, Texas, US).
2.5. Ethical issues
Approval for this project was granted by the Institutional Review Board (IRB) at UPCH. As only de-identified data was used, the requirement for informed consent was waived.
3. Results
3.1. Description of the participants
From the total of 9875 students in the university, between 2002 and 2009, only 5580 students were recorded in the clinic’s database. A total of 18,537 clinical evaluations were obtained from the 5580 students. From those students, 4842 (86.8%) met our inclusion criteria of providing complete data and were included in the analysis. The students’ median age at baseline was 18 years (inter-quartile range: 17–20) and 31.3% were males. Most students belonged to Medicine (23.5%) and Medical Technology (20.9%). Details of other characteristics at baseline of those participating in the study are seen in Table 1.
Table 1.
Demographics characteristics of the study population (n = 5580).
| Evaluated (n = 4842)
|
Not evaluated (n = 738)
|
p | |||
|---|---|---|---|---|---|
| Frequency | (%) | Frequency | (%) | ||
| Age at cohort baseline | |||||
| Under 18 years old | 2001 | (41.3) | 224 | (30.4) | <0.01 |
| 18 Years old | 920 | (19.0) | 181 | (24.5) | |
| Between 18 and 21 years old | 867 | (17.9) | 187 | (25.3) | |
| 21 Years old or more | 1054 | (21.8) | 146 | (19.8) | |
| Male | 1516 | (31.3) | 264 | (35.8) | 0.02 |
| Body mass index at cohort baseline | |||||
| Underweight | 321 | (6.6) | 25 | (3.4) | <0.01 |
| Normal | 3566 | (73.7) | 511 | (69.2) | |
| Overweight/obesity | 955 | (19.7) | 202 | (27.4) | |
| Background | |||||
| TB contact history at cohort baseline | 204 | (4.2) | 89 | (12.1) | <0.01 |
| Career | |||||
| Health administration, science and education | 848 | (17.5) | 144 | (19.5) | <0.01 |
| Veterinary | 393 | (8.1) | 19 | (2.6) | |
| Dentistry | 663 | (13.7) | 62 | (8.4) | |
| Nursing | 789 | (16.3) | 98 | (13.3) | |
| Medical technology | 1012 | (20.9) | 198 | (26.8) | |
| Medicine | 1137 | (23.5) | 217 | (29.4) | |
Baseline TST positivity prevalence was 1.0% (95% CI: 0.6–1.3%), whereas prevalence of TST positivity using the last available evaluation of the students was 38.1% (95% CI: 36.8–39.5%).
3.2. Incidence of TST conversion
The overall incidence density of TST conversion was 12.4 per 100 person-years (95% CI: 11.8–13.0). The annual incidence of TST conversion for students from non-clinical careers was 9.0 per 100 person-years (95% CI: 7.7–10.4), whereas for students from clinical careers was 13.2 (95% CI: 12.5–14.0). Medical Technology and Nursing students had the greatest incidence (see Table 2).
Table 2.
Incidence of TST conversion among health science students (n = 4842).
| Incidence rate (95%CI) | |
|---|---|
| Career: | |
| Administration, science and education | 9.0 (7.8–10.4) |
| Veterinary | 11.2 (9.4–13.4) |
| Dentistry | 11.6 (10.1–13.3) |
| Nursing | 15.8 (14.1–17.7) |
| Medical technology | 15.7 (14.2–17.4) |
| Medicine | 11.1 (10.1–12.3) |
| Year of career | |
| 1st Year | 10.9 (10.0–11.9) |
| 2nd Year | 13.4 (12.1–14.9) |
| 3rd Year | 12.0 (10.7–13.5) |
| 4th Year | 11.9 (10.3–13.7) |
| 5th Year | 16.8 (14.5–19.6) |
| 6th Year | 16.5 (10.8–25.4) |
| 7th Year | 33.9 (21.9–52.5) |
| Internship | |
| No | 11.9 (11.3–12.5) |
| Yes | 22.5 (19.0–26.5) |
| Calendar year | |
| 2002–2003 | 15.2 (13.6–16.9) |
| 2004–2005 | 13.2 (12.2–14.4) |
| 2006–2007 | 10.6 (9.7–11.6) |
| 2008–2009 | 12.0 (10.6–13.6) |
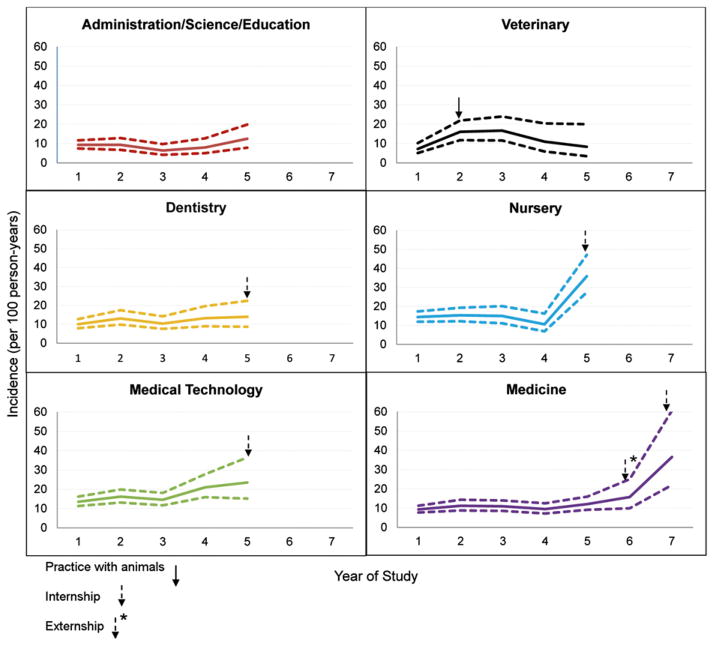
Analysis stratified by career, showed higher incidences in the last two years of Medicine (33.9 per 100 person-years; 95% CI: 21.9–52.5), Medical Technology (22.8; 95% CI: 18.1–28.6) and Nursing (20.8; 95% CI: 16.6–25.9, see Figure 1).
Figure 1.
Incidence of TST conversion among students by career and year of study.
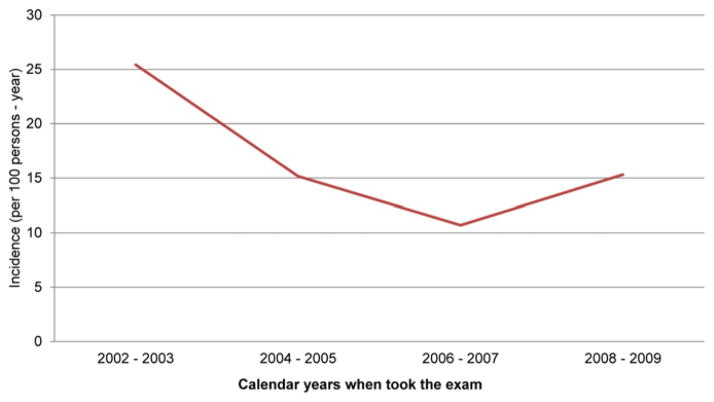
In a restricted analysis including only the last two years of career, overall incidence decreased from 25.4 per 100 person-years (95% CI: 21.0–30.8) in 2002–2003 to 15.3 (95% CI: 11.6–20.2) in 2008–2009 (p < 0.01, Figure 2).
Figure 2.
Incidence of TST conversion including only the last 2 years of schooling by calendar year.
3.3. Factors associated with TST conversion
In multivariable analysis, factors independently associated with TST conversion during follow-up were age (p < 0.001), career (p < 0.01) and internship (p < 0.01, see Table 3).
Table 3.
Factors associated with TST conversion among health science students.
| Univariate
|
Multivariable
|
|||
|---|---|---|---|---|
| IRR (IC95%) | p-Value | IRR (IC95%) | p-Value | |
| Age | ||||
| Under 18 years old | Reference | Reference | ||
| 18 Years old | 3.00 (2.31–3.87) | <0.01 | 2.97 (2.29–3.84) | <0.01 |
| Between 18 and 21 years old | 3.98 (3.14–5.04) | <0.01 | 3.92 (3.09–4.96) | <0.01 |
| 21 Years old or more | 4.50 (3.57–5.66) | <0.01 | 4.00 (3.16–5.06) | <0.01 |
| Male | 0.95 (0.86–1.05) | 0.34 | ||
| Body mass index | ||||
| Normal | Reference | |||
| Underweight | 0.78 (0.61–0.99) | 0.04 | ||
| Overweight/obesity | 1.17 (1.05–1.30) | <0.01 | ||
| TB contact history | 1.38 (1.13–1.68) | <0.01 | ||
| Careers | ||||
| Administration, science and education | Reference | Reference | ||
| Veterinary | 1.32 (1.06–1.63) | 0.01 | 1.23 (0.98–1.54) | 0.07 |
| Dentistry | 1.31 (1.09–1.59) | <0.01 | 1.28 (1.05–1.54) | 0.01 |
| Nursing | 1.80 (1.52–2.13) | <0.01 | 1.61 (1.35–1.92) | <0.01 |
| Medical technology | 1.73 (1.46–2.04) | <0.01 | 1.51 (1.27–1.78) | <0.01 |
| Medicine | 1.31 (1.11–1.54) | <0.01 | 1.14 (0.96–1.35) | 0.15 |
| Internship year | 2.45 (2.09–2.87) | <0.01 | 1.94 (1.64–2.30) | <0.01 |
4. Discussion
Nursing and Medical Technology students had the highest incidence of TST conversion compared to all other careers. Veterinary, Dentistry and Medical students were also at increased risk compared to non-clinical careers. In this study, we found that career, age, and internship were independent factors associated with increased risk of TSTconversion. Of note, the prevalence of TST positivity at baseline was low, indicating that the risk to this population prior to the initiation of their studies was lower than that of the general population in Peru.
The literature shows a wide range of incidence rates among students of clinical careers, ranging from rates of only (1.1–3.9%),12,15,16 to rates similar to our results (10.5–16%),23 and others with higher rates (35%).24 Most past studies have only included medical students, with only one also including nursing students.23 Our study analyzed students in all available careers, allowing for a larger perspective regarding the incidence of TST conversion among health sciences students.
Between second and fourthyear, medical technologyand nursing students had greater incidence compared to medical students (Figure 1). Although during the first years of career, medical technology and nursing students have more contact with patients, the incidence was particularly highest during their final two years of study. This time corresponds to the period with the number of hours spent in the hospital by nursing, medical technology, and medical students, usually more than 72 h per week, which may explain these findings.5,13,18 We also found that internship was an independent factor associated with TST conversion. Moreover, the annual incidence of TST conversion among students in clinical careers was similar when compared to studies targeting health personnel (range: 0.69–45.3%).6–9 The relationship between year of study and risk of tuberculosis infection has been previously described.13,15–17
Evidence overtime showed that the rate of TST conversion in the last 2 years of study in all careers (Figure 2), tended to decrease by calendar time. Different biosafety measures implemented by the University and Ministry of Health authorities as well as the reduction of the number of TB cases at population level might be responsible for these findings.25 One of the measures adopted in 2008 was implement a new ventilation system together with a system of ultraviolet (UV) lights in all the Emergency Rooms at a national hospital, where health workers care for TB patients and students do their rotations. The use of UV lights is a methodology used in the control of TB which can sterilize the circulating air throughout the building.26
This study also found factors associated with TST conversion. Age was associated, with risk of TST conversion owing to increasing exposure to cumulative risk.15,27 TST conversion risk was 61% and 51% higher among nursing and medical technology students respectively, compared to non-clinical careers (sciences, health administration and education). Medical students showed 14% increase in risk compared to non-clinical students with a borderline significance. Thus, our results suggest that students in close contact with patients during their clinical practices are at variable risk. Previous studies support these findings especially among nursing and medical students.7,13,15 Interestingly, Veterinary students experienced greater risk compared to non-clinical students, although this finding was not statistically significant. Their contact with animals that could have other Mycobacterium infections,28,29 and their training at hospitals, including probable exposure to TB patients, could be two of the main factors for these results. TST can give false positive results because of infection by non-tuberculous mycobacteria,30 which could also affect their risk.
Other potential factors, such as contact with a close relative with TB and overweight/obesity status, were not included in our final model. Literature has reported increased risk of infection for those with TB contact.12,19 Our results suggest than close contact with TB patients at hospitals is more important as shown in our results, with exposure to resistant forms. Similarly, a previous study described a log-linear relationship between TB incidence and body mass index, where increasing body mass index was a protection factor to develop tuberculosis.31 Our findings differ with this report possibly due to confounding factors (student’s place of residence or socioeconomic status).
The low baseline TST positivity in this study compared to 35.6% in a 1986 report at the same institution32 could be explained by the reduction of the overall TB incidence in Peru.25 Latent tuberculosis infection prevalence among health sciences students reported in other studies in Peru and abroad varied between 0% and 20.9%13,15,17,33; however, these reports did not include first-year students or other careers.
This study has strengths. Our study benefits from a large sample size and included students from a variety of careers related to health sciences. In addition, students were followed-up for at least two years, previous studies have only included one year of follow-up.13,17,33 However, this report has also some limitations. First, this is a secondary data analysis, therefore, some variables of interest were not available including place of residence and socioeconomic status.2,31 Data from a subset of students requesting a reduction in tuition fees shows that they belong to the upper socioeconomic decile in Lima.34 Overall, medical students were from a higher socioeconomic level compared to other students; this could influence results. Additionally, many of students (40.5%) did not attend their TST reading. Similar problems have been described in other cohort studies,23,24 which could have affected our results. Moreover, evaluated students were not comparable to those not evaluated. As a consequence, results are not inferable to all university students. However, findings were comparable to previous reports.23,24 Additionally, Bacille Calmette-Guerin (BCG) vaccination history was not recorded. Overall coverage of BCG at birth was universal between 1980 and 1990, when most of the students in our cohort were born. BCG vaccination can cause a false positive TST; however, this is primarily a concern in the first 2 years after vaccination and TSTs were evaluated around 16 years after that.16,23 In countries with high TB prevalence and universal BCG vaccination, the threshold we used of ≥10 mm for TST is recommended to exclude reaction due to BGC.17,35 Additionally, this would only be a concern for the baseline prevalence assessment as incident TST during follow-up would not be related to the BCG vaccine, but to recent infection. Finally, according to ATS/CDC/IDSA definition, a TSTconversion is defined as an increment of 10 mm from TST at baseline.19,20 We have defined our study, considering any TSTgreater than 10 mm, as established by the Peruvian Ministry of Health.21 Due to the high incidence of tuberculosis in Peru, the aim is to prevent as many cases as possible to avoid the development of the disease. Lack of information from the variation between baseline TST and follow-up evaluation, may produce an upward bias in the measuring process. We believe this bias would not make a big difference because the results are similar to other different studies.6–9,15
In conclusion, although this study showed that the risk of TB infection for health sciences students had a downward trend in recent years, they are still exposed to unacceptably high levels of risk, calling for more urgent interventions and strategies for prevention, such as administrative control to reduce risk of exposure, environmental control to prevent the spread and reduce concentration of infectious agents in the air, and respiratory protection to reduce the risk of exposure circumstances and special areas should be considered.18,20 Close follow-up for students with history of TB contact and overweight has been implemented, as well as an improved system for collection of information.
Acknowledgments
Funding: None.
To UPCH authorities who facilitated access and use of data for this study.
Footnotes
Competing interests: None declared.
Ethical approval: Not required.
Contributor Information
José E. Pérez-Lu, Email: jose.perez.l@upch.pe.
Cesar P. Cárcamo, Email: cesar.carcamo@upch.pe.
Patricia J. García, Email: patricia.garcia@upch.pe.
Alejandro Bussalleu, Email: alejandro.bussalleu@upch.pe.
Antonio Bernabé-Ortiz, Email: antonio.bernabe@upch.pe.
References
- 1.World Health Organization. Global tuberculosis control 2011. Geneva, Switzerland: WHO; 2011. [Google Scholar]
- 2.Bernabé A. Poverty strikes back: effects on TB-DOTS results in Peru. Revista Medica Herediana. 2007;18:179–80. [Google Scholar]
- 3.Dimitrova B, Hutchings A, Atun R, Drobniewski F, Marchenko G, et al. Increased risk of tuberculosis among health care workers in Samara Oblast, Russia: analysis of notification data. The International Journal of Tuberculosis and Lung Disease. 2005;9:43–8. [PubMed] [Google Scholar]
- 4.Menzies D, Fanning A, Yuan L, Fitzgerald M. Tuberculosis among health care workers. New England Journal of Medicine. 1995;332:92–8. doi: 10.1056/NEJM199501123320206. [DOI] [PubMed] [Google Scholar]
- 5.Accinelli R, Noda J, Bravo E, Galloso M, Lopez L. Tuberculosis disease among health care workers. Acta Medica Peruana. 2009;26:35–47. [Google Scholar]
- 6.Bonifacio N, Saito M, Gilman RH, Leung F, Chavez NC, et al. High risk for tuberculosis in hospital physicians, Peru. Emerging Infectious Diseases. 2002;8:747. doi: 10.3201/eid0807.010506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.González C, Araujo G, Agoglia R, Hernández S, Seguel I, et al. Tuberculosis among health care workers. Medicina (Buenos Aires) 2010;70:23–30. [PubMed] [Google Scholar]
- 8.Joshi R, Reingold AL, Menzies D, Pai M. Tuberculosis among health-care workers in low- and middle-income countries: a systematic review. PLoS Medicine. 2006;3:e494. doi: 10.1371/journal.pmed.0030494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ostrosky-Zeichner L, Rangel-Frausto S, García-Romero E, Vázquez A, Ibarra J, et al. Tuberculosis en trabajadores de la salud: importancia de los programas de vigilancia y control. Salud Publica de Mexico. 2000;42:48–52. [PubMed] [Google Scholar]
- 10.Fica A, Cifuentes M, Ajenjo C, Jemenao I, Zambrano A, et al. Tuberculosis in healthcare workers. Revista Chilena de Infectología. 2008;25:243–55. [PubMed] [Google Scholar]
- 11.Tam C, Leung C. Occupational tuberculosis: a review of the literature and the local situation. Hong Kong Medical Journal. 2006;12:448–55. [PubMed] [Google Scholar]
- 12.Turk A, Angst F, Steffen R. Tuberculosis infection notification in Swiss medical students during their clinical electives. International Journal of Infectious Diseases. 2003;7:268–73. doi: 10.1016/s1201-9712(03)90105-6. [DOI] [PubMed] [Google Scholar]
- 13.Silva V, Cunha A, Oliveira J, Figueira M, Nunes Z, et al. Medical students at risk of nosocomial transmission of Mycobacterium tuberculosis. The International Journal of Tuberculosis and Lung Disease. 2000;4:420–6. [PubMed] [Google Scholar]
- 14.Veeser P, Smith P, Handy B, Martin S. Tuberculosis screening on a health science campus: use of QuantiFERON-TB Gold Test for students and employees. Journal of American College Health. 2007;56:175–80. doi: 10.3200/JACH.56.2.175-180. [DOI] [PubMed] [Google Scholar]
- 15.Hohmuth B, Yamanija J, Dayal A, Nardell E, Salazar J, et al. Latent tuberculosis infection: risks to health care students at a hospital in Lima, Peru. The International Journal of Tuberculosis and Lung Disease. 2006;10:1146–51. [PubMed] [Google Scholar]
- 16.Silva V, Cunha A, Kritski A. Tuberculin skin test conversion among medical students at a teaching hospital in Rio de Janeiro, Brazil. Infection Control and Hospital Epidemiology. 2002;23:591–4. doi: 10.1086/501976. [DOI] [PubMed] [Google Scholar]
- 17.Teixeira E, Menzies D, Comstock G, Cunha A, Kritski A, et al. Latent tuberculosis infection among undergraduate medical students in Rio de Janeiro State, Brazil. The International Journal of Tuberculosis and Lung Disease. 2005;9:841–7. [PubMed] [Google Scholar]
- 18.Huaroto L, Espinoza M. Recommendations for the control of tuberculosis transmission in hospitals. La Revista Peruana de Medicina Experimental y Salud Publica. 2009;26:364–9. [Google Scholar]
- 19.American Thoracic Society/Centers for Disease Control and Prevention. Targeted tuberculin testing and treatment of latent tuberculosis infection. American Journal of Respiratory and Critical Care Medicine. 2000;161:S221–47. doi: 10.1164/ajrccm.161.supplement_3.ats600. [DOI] [PubMed] [Google Scholar]
- 20.Jensen PA, Lambert LA, Lademarco MF, Ridzon R. CDC. Guidelines for preventing the transmission of Mycobacterium tuberculosis in health-care settings. MMWR Recommendations and Reports. 2005;54:1–141. [PubMed] [Google Scholar]
- 21.Perú: Dirección General de Salud de las Personas. Ministerio de Salud Lima; 2006. Estrategia Sanitaria Nacional de Prevención y Control de la Tuberculosis. Norma técnica de salud para el control de la tuberculosis. [Google Scholar]
- 22.World Health Organization. Reducing risks, promoting healthy life. Geneva, Switzerland: WHO; 2002. [Google Scholar]
- 23.Maciel ELN, Meireles W, Silva AP, Fiorotti K, Dietze R. Nosocomial Mycobacterium tuberculosis transmission among healthcare students in a high incidence region, in Vitória, State of Espírito Santo. Revista da Sociedade Brasileira de Medicina Tropical. 2007;40:397–9. doi: 10.1590/s0037-86822007000400004. [DOI] [PubMed] [Google Scholar]
- 24.Arellano A, Fuentes J, Campos R. Respuesta a la prueba de Mantoux en un grupo de estudiantes de medicina, antes y después de su rotación hospitalaria. Revista da Faculdade de Médicas Universidad Francisco Marroquín. 2008;1:12–4. [Google Scholar]
- 25.Bonilla C. Tuberculosis in Peru: current status. Acta Medica Peruana. 2008;25:163–70. [Google Scholar]
- 26.Escombe AR, Moore DAJ, Gilman RH, Navincopa M, Ticona E, et al. Upper-room ultraviolet light and negative air ionization to prevent tuberculosis transmission. PLoS Medicine. 2009;6:e1000043. doi: 10.1371/journal.pmed.1000043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Larsen NM, Biddle CL, Sotir MJ, White N, Parrott P. Risk of tuberculin skin test conversion among health care workers: occupational versus community exposure and infection. Clinical Infectious Diseases. 2002;35:796. doi: 10.1086/342333. [DOI] [PubMed] [Google Scholar]
- 28.Posthaus H, Bodmer T, Alves L, Oevermann A, Schiller I, et al. Accidental infection of veterinary personnel with Mycobacterium tuberculosis at necropsy: a case study. Veterinary Microbiology. 2011;149:374–80. doi: 10.1016/j.vetmic.2010.11.027. [DOI] [PubMed] [Google Scholar]
- 29.Une Y, Mori T. Tuberculosis as a zoonosis from a veterinary perspective. Comparative Immunology, Microbiology & Infectious Diseases. 2007;30:415–25. doi: 10.1016/j.cimid.2007.05.002. [DOI] [PubMed] [Google Scholar]
- 30.Latorre I, De Souza-Galvão M, Ruiz-Manzano J, Lacoma A, Prat C, et al. Evaluating the non-tuberculous mycobacteria effect in the tuberculosis infection diagnosis. European Respiratory Journal. 2010;35:338–42. doi: 10.1183/09031936.00196608. [DOI] [PubMed] [Google Scholar]
- 31.Lönnroth K, Williams BG, Cegielski P, Dye C. A consistent log-linear relationship between tuberculosis incidence and body mass index. International Journal of Epidemiology. 2010;39:149–55. doi: 10.1093/ije/dyp308. [DOI] [PubMed] [Google Scholar]
- 32.Fernández-Concha DB. [Thesis for the degree Bachiller] Lima: Universidad Peruana Cayetano Heredia; 1987. Risk of acquisition of tuberculosis infection among medical students; p. 76. [Google Scholar]
- 33.Arbeláez MP, Ocampo MC, Montoya J, María JL, Jaramillo LM, et al. Evaluation of the tuberculin reaction in health occupation students. Revista Panam Salud Publica. 2000;8:272–9. doi: 10.1590/s1020-49892000000900007. [DOI] [PubMed] [Google Scholar]
- 34.Instituto Nacional de Estadística e Informática INEI, Lima Peru. [accessed 2011 August 2]; Available from: http://www.inei.gob.pe/
- 35.Dixon W, Collins M. Screening and chemoprophylaxis for tuberculosis infection in college populations. Journal of American College Health. 1998;46:171–5. doi: 10.1080/07448489809595605. [DOI] [PubMed] [Google Scholar]