Dear Editor:
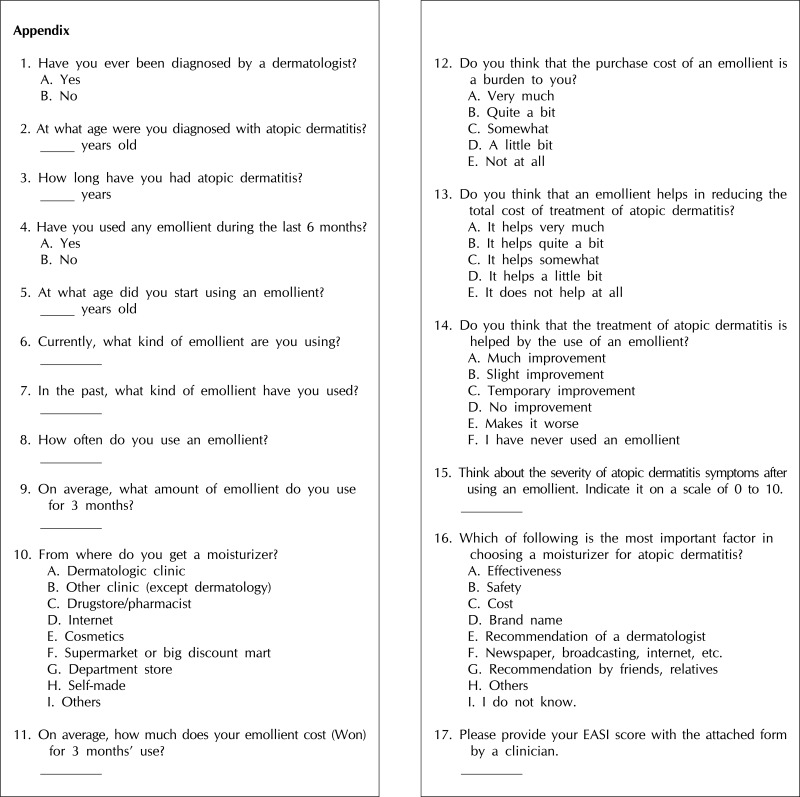
Atopic dermatitis (AD) is a chronic, relapsing, pruritic, inflammatory skin disease. It is caused by abnormalities in the skin barrier function, allergen sensitization, and recurrent skin infections. Deficiency of filaggrin, lack of intercellular lipid in the stratum corneum, inadequate ratios between components (cholesterol, essential fatty acids, and ceramides), imbalance between protease and antiprotease levels, and disruption of the barrier can lead to transepidermal water loss and inflammation in AD1. The use of emollients in patients with AD helps restore and preserve the stratum corneum barrier and may decrease the need for topical glucocorticoids, especially in long-term management2. However, misunderstanding, lack of information, and inadequate compliance hamper the appropriate use of emollients, often resulting in unsatisfactory treatment. In this study, we assessed the awareness about, effectiveness of, and behaviors toward the use of emollients in patients with AD through a questionnaire survey. A written questionnaire was distributed to 154 patients who visited the outpatient dermatologic clinics of 7 university hospital affiliates, 145 of whom completed the survey. The questionnaire consisted of 16 items (Appendix). AD was diagnosed by a dermatologist on the basis of the criteria given by Hanifin and Rajka; the severity of AD was determined by using the eczema area and severity index (EASI) score3,4. The severity of AD was graded as mild (≤10) or moderate to severe (>10) according to the EASI score. The present study was approved by the institutional review board of the Catholic University of Korea (Approved No. XC12QCMI0081). Data were statistically analyzed with SPSS ver. 12.0 for Windows (SPSS Inc., Chicago, IL, USA). We used analysis of variance and χ2 tests to compare the differences according to the severity of AD. A p-value of <0.05 was considered statistically significant.
The characteristics of patients are summarized in Table 1. In this study, AD was found to be more prevalent in women (female : male=1.46 : 1), as in previous studies5. The details of emollient use in children and adults are shown in Table 2, respectively.
Table 1.
Patient characteristics (n=145)
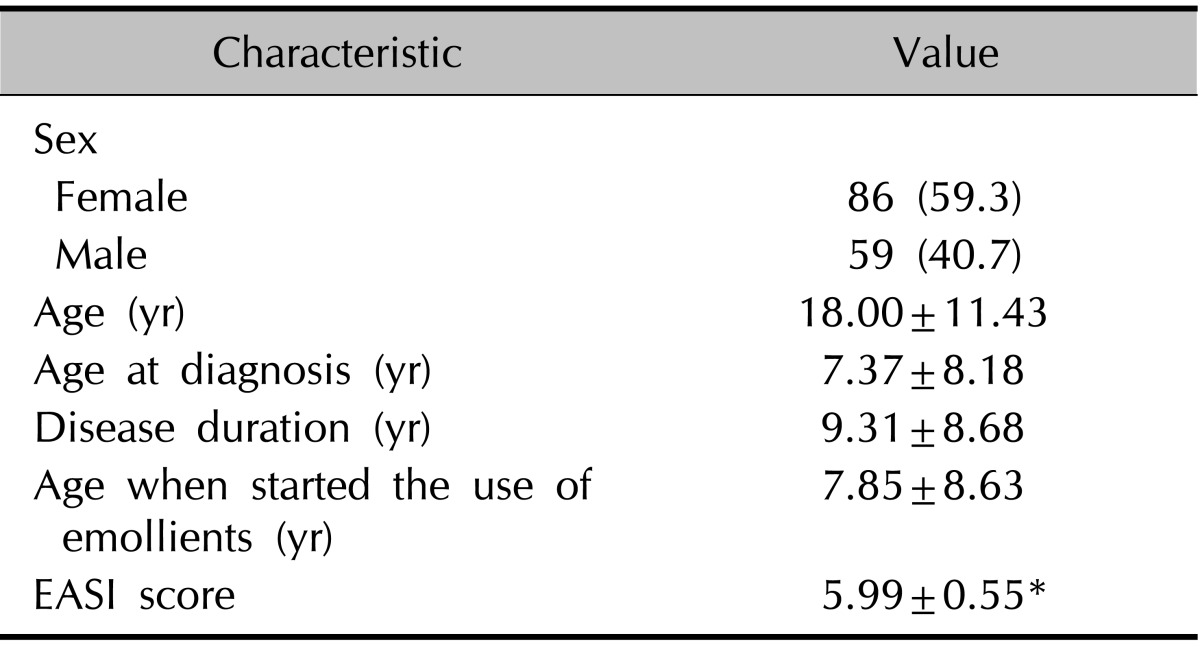
Values are presented as number (%) or mean±standard deviation. EASI: eczema area and severity index.
*Value: mean±stanadard error.
Table 2.
Details of emollient use in children and adults
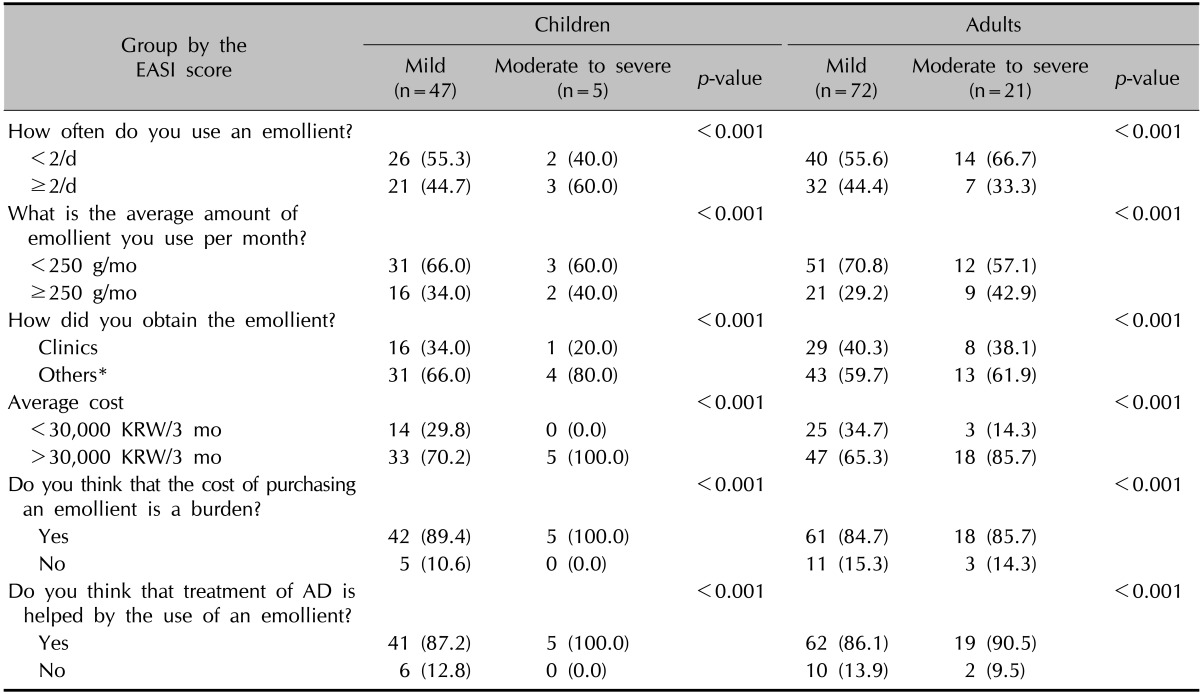
Values are presented as number (%). EASI: eczema area and severity index, AD: atopic dermatitis, KRW: Korean won.
*Others refers to drugstore, pharmacist, internet, cosmetics, supermarket, big discount mart, department store, and self-made.
Most children experience a substantial reduction in the severity of their AD over time. Others continue to have severe disease as adults6. In this study, the severity of AD differed significantly between older and younger patients, with higher EASI scores in older patients (>8 years old) (p=0.015). In a previous study, 96.2% of preschool children (0~6 years) with AD had mild cases, as determined by using the EASI score (3.91±4.73)7. The overall EASI score (5.99) of our patients was higher than that of other studies, and this may be because only outpatients were included.
The existing AD guidelines have not provided consistent recommendations about the optimal application frequency of emollients. Recent guidelines state that emollients should be prescribed in adequate amounts (minimum of 250 g/wk) and used frequently (at least twice daily) on noninflamed skin8. Our results indicate that at least 56.6% of patients with AD did not use emollients as frequently as recommended, and most patients did not use an adequate amount. Furthermore, 10.3% of patients reported that they had not used emollients at all in the preceding 6 months. On the basis of our results, dermatologists should pay more attention to educating patients with AD about using emollients as a basic and adjuvant therapy to maintain skin hydration, avoiding or minimizing factors that trigger or aggravate AD, and preventing secondary infections.
In this study, the patients with AD purchased emollients from the clinics (37.2%), internet (20.0%), supermarket (20%), drugstore (11.0%), cosmetic store (5.5%), department store (4.1%), or others (2.2%). When choosing an emollient, the patients with AD considered effectiveness (62.1%), safety (24.8%), and recommendation by a dermatologist (11.0%). This result implies that patients with mild AD are more positive about the therapeutic effectiveness of emollients in pediatric and adult patients with AD. Additionally, skin symptoms improved and less medication was needed after completing an educational program9. Thus, instruction about emollient use should be implemented as an adjunct to conventional therapy for AD.
Recent estimates showed that the annual cost for parents to manage a child with mild, and severe AD was Australian dollar (Aus$) 330, and Aus$ 1,225, respectively10. In this study, we report a significant difference in the average cost of treatment between patients with mild AD and those with moderate to severe AD. Of the patients with AD, 86.9% thought that the cost of purchasing emollients was an economic burden. Thus, the cost of emollients may limit their adequate use. Of the patients, 88.3% answered that the use of an emollient reduces the total cost of treatment. Interestingly, there was a significant difference between the patients with mild AD and those with moderate to severe AD in their view on whether an emollient helps reduce the total cost of long-term treatment (p=0.009). We speculate that the use of emollients could be more helpful in decreasing the total financial burden of treatment in patients with mild AD than in patients with severe AD.
As might be predicted, emollients were believed to improve skin symptoms by 87.6% of the survey responders. Interestingly, analysis of the 2 groups classified according to the EASI score (>10 or ≤10) identified a significant EASI score-dependent difference in the relief of AD symptoms (visual analogue scale). The subjective symptom scale after using emollients (question 15, mean±standard deviation), which was judged by the patients themselves, was 5.13±2.21 for patients with mild AD and 6.17±2.28 for those with moderate to severe AD (p=0.023). Thus, emollient therapy may have higher efficacy in improving symptoms among patients with milder cases of AD.
Future studies with more participants will be necessary to elucidate the differences between groups in detail. Despite these limitations, our survey yielded interesting data on the attitudes and behaviors about emollient use in Korean patients with AD. Our results suggest that the use of emollients, especially in patients with mild AD, may be an important component of treatment. We recommend that emollient use be reserved for the treatment of AD and should be closely monitored by a physician.
ACKNOWLEDGMENT
This study was supported by a grant from the Dermatology Alumni Fund of the Catholic University of Korea in the program year 2011.
Appendix
References
- 1.Palmer CN, Irvine AD, Terron-Kwiatkowski A, Zhao Y, Liao H, Lee SP, et al. Common loss-of-function variants of the epidermal barrier protein filaggrin are a major predisposing factor for atopic dermatitis. Nat Genet. 2006;38:441–446. doi: 10.1038/ng1767. [DOI] [PubMed] [Google Scholar]
- 2.Przybilla B, Eberlein-König B, Ruëff F. Practical management of atopic eczema. Lancet. 1994;343:1342–1346. doi: 10.1016/s0140-6736(94)92474-0. [DOI] [PubMed] [Google Scholar]
- 3.Hanifin JM, Rajka G. Diagnostic features of atopic dermatitis. Acta Derm Venereol Suppl (Stockh) 1980;92(Suppl):44–47. [Google Scholar]
- 4.Hanifin JM, Thurston M, Omoto M, Cherill R, Tofte SJ, Graeber M EASI Evaluator Group. The eczema area and severity index (EASI): assessment of reliability in atopic dermatitis. Exp Dermatol. 2001;10:11–18. doi: 10.1034/j.1600-0625.2001.100102.x. [DOI] [PubMed] [Google Scholar]
- 5.Leung DYM, Eichenfield LF, Boguniewicz M. Atopic dermatitis. In: Goldsmith LA, Katz SI, Gilchrest AB, Paller AS, Leffell DJ, Wolff K, editors. Fitzpatrick's dermatology in general medicine. 8th ed. New York: McGraw-Hill; 2012. pp. 165–182. [Google Scholar]
- 6.Salt BH, Boguniewicz M, Leung DY. Severe refractory atopic dermatitis in adults is highly atopic. J Allergy Clin Immunol. 2007;119:508–509. doi: 10.1016/j.jaci.2006.11.006. [DOI] [PubMed] [Google Scholar]
- 7.Choi WJ, Ko JY, Kim JW, Lee KH, Park CW, Kim KH, et al. Prevalence and risk factors for atopic dermatitis: a cross-sectional study of 6,453 Korean preschool children. Acta Derm Venereol. 2012;92:467–471. doi: 10.2340/00015555-1252. [DOI] [PubMed] [Google Scholar]
- 8.Hanifin JM, Cooper KD, Ho VC, Kang S, Krafchik BR, Margolis DJ, et al. Guidelines of care for atopic dermatitis, developed in accordance with the American Academy of Dermatology (AAD)/American Academy of Dermatology Association "Administrative Regulations for Evidence-Based Clinical Practice Guidelines". J Am Acad Dermatol. 2004;50:391–404. doi: 10.1016/j.jaad.2003.08.003. [DOI] [PubMed] [Google Scholar]
- 9.Ring J, Alomar A, Bieber T, Deleuran M, Fink-Wagner A, Gelmetti C, et al. European Dermatology Forum; European Academy of Dermatology and Venereology; European Task Force on Atopic Dermatitis; European Federation of Allergy; European Society of Pediatric Dermatology; Global Allergy and Asthma European Network. Guidelines for treatment of atopic eczema (atopic dermatitis) Part II. J Eur Acad Dermatol Venereol. 2012;26:1176–1193. doi: 10.1111/j.1468-3083.2012.04636.x. [DOI] [PubMed] [Google Scholar]
- 10.Su JC, Kemp AS, Varigos GA, Nolan TM. Atopic eczema: its impact on the family and financial cost. Arch Dis Child. 1997;76:159–162. doi: 10.1136/adc.76.2.159. [DOI] [PMC free article] [PubMed] [Google Scholar]