Abstract
[Purpose] The purpose of this study was to investigate differences in effects caused by variation in the intervention frequency of outpatient pulmonary rehabilitation, in terms of the pulmonary function, lower-limb muscle strength, exercise tolerance, and quality of life (QOL). [Subjects and Methods] A total of 36 patients with mild to severe chronic obstructive pulmonary disease (COPD) were studied. These patients were all men over the age of 40 who did not require assistance for activities of daily living (ADL). Groups undergoing intervention once a month (M1 group) and once a week (W1 group) were compared in terms of the effects of outpatient pulmonary rehabilitation for a period of 12 weeks. Intervention during this time included supervised and home-based exercise. [Results] Comparison of before and after intervention revealed that the rate of change in the W1 group was significantly higher than that in the M1 group in terms of the QOL, lower-extremity muscle strength, and 6-minute walking distance. [Conclusion] Outpatient pulmonary rehabilitation programs yielded greater improvements in the W1 group than in the M1 group in terms of the QOL and exercise tolerance.
Key words: COPD, Pulmonary rehabilitation as outpatient, Frequency of intervention
INTRODUCTION
Pulmonary rehabilitation is important for the treatment of chronic obstructive pulmonary disease (COPD), which is considered a systemic disease. Pulmonary rehabilitation is described as a first-line treatment for COPD patients in the World Health Organization (WHO) guidelines1)and is considered a treatment superior to drug therapy. In Japan, pulmonary rehabilitation has been established as a routine part of outpatient medical practice.
Reportedly, 2–3 months are required to obtain an effect of exercise therapy on COPD2), and intervention is continued for a specific period. However, the frequency varies among outpatient clinics. The guidelines recommend 2–3 times a week3), but no consensus has been reached with regard to the intervention frequency; for example, a similar effect was obtained by a once-a-week program in one study4), and once every 4 weeks was used for a maintenance program in another study5).
In this study, patients were allocated to 2 groups undergoing outpatient pulmonary rehabilitation once every 4 weeks (M1 group) and once a week (W1 group), and they participated in an intervention centering on home-based exercise (Home ex) for 12 weeks to investigate differences in the effect on exercise tolerance and QOL between the groups.
SUBJECTS AND METHODS
Subjects
The subjects were 36 male COPD patients aged 40 years or older. The inclusion criteria were the absence of home oxygen therapy (HOT) and orthopedic diseases and independence in ADL. All patients were receiving drug therapy, such as bronchodilator treatment, and they continued to receive it during the study. Consent to participate in this study was obtained from the patients after sufficient explanation of the study content. This study was performed with the consent of the ethics committee of Kanetsu Central Hospital.
Methods
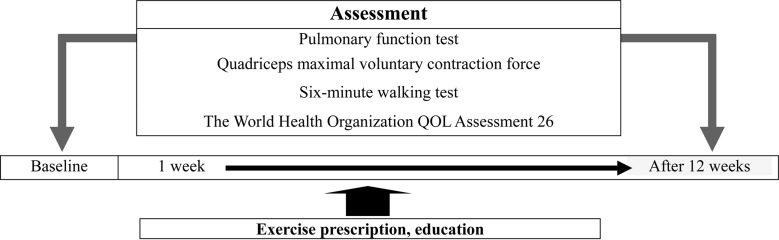
The subjects were divided into the M1 and W1 groups based on the intervention frequency, and underwent 12 weeks of physical therapy. Guidance, setting, and evaluation of Home ex were performed when they visited the outpatient clinic (Fig. 1).
Fig. 1.
Pulmonary rehabilitation protocol for outpatients
As Home ex, the patients received guidance on breathing practice, respiratory, upper limb, and lower limb muscle training, stretching exercise for the respiratory muscles6), and walking training (free walking). They were asked to indicate their daily walking distance along with the contents of the Home ex in a diary.
The breathing practice started with relaxation, and then pursed-lips breathing and abdominal breathing in recumbency were performed. In respiratory muscle training, after guidance on abdominal breathing in recumbency, respiratory muscle exercise with an abdominal load was performed. In upper limb muscle training, anterior and posterior arm raises with a weight were performed in a sitting posture. In lower limb muscle training, the patients were instructed with respect to a tiptoe standing movement in a standing position, a repeated standing-sitting motion, and stepping. A load within the range of 500 g to 2 kg was set for individual patients when possible. The number of repetitions of each item was set at 20–50, which is appropriate for Home ex, and the patients were recommended to perform this program twice a day (in the morning and evening).
The patients were examined before and after the 12 weeks of outpatient pulmonary rehabilitation. The examination before rehabilitation started with a respiratory function test. All patients were examined with respect to vital capacity (VC), % predicted VC (%VC), forced expiratory volume in 1 second (FEV1.0), % predicted FEV1.0 (%FEV1.0), and forced expiratory volume in 1 second % (FEV1.0%) by the one physical therapist using a spirometer in a specific room. In lower limb muscle strength measurement, the knee extensor strength in isometric contraction was measured in a sitting position with 90° flexion of the knee joint using a dynamometer (μ-tas1, ANIMA Corp., Tokyo, Japan) 3 times for each leg, employing a unit of N, and the maximum value was adopted. This value was divided by the body weight (N/kg) and evaluated as a quadriceps maximal voluntary contraction force (QMVC)7, 8). Regarding exercise tolerance, the 6-minute walking distance (6MWD) was measured. Following the American Thoracic Society (ATS) criteria, the patients walked without encouragement. The walking distance along a walkway (one lap: 50 m) was measured. A questionnaire was performed to investigate QOL, including physical and mental conditions and anxiety in daily living activities, using the World Health Organization QOL Assessment 26 (WHO/QOL26)9). The WHO/QOL26 is a scale in which an increase in value represents improvement. It consists of 26 questions in 5 domains: physical and psychological areas, social relationship, environment, and overall, and the average QOL is calculated by dividing the total score by the number of questions. It was adopted because the patients complete it by themselves, and so it is appropriate for surveys in outpatient clinics. The same evaluation was performed after 3 months.
For 2-group comparison of the background and rates of change in the physical therapy evaluation items, the Mann-Whitney U-test was used, regarding p<0.05 as significant. Statistical analysis was performed using SPSS 17.0 J for Windows.
RESULTS
Table 1 shows a comparison of the patient background between the 2 groups. The mean age was 67.2±6.5 years in the M1 group and 65.2±4.5 years in the W1 group. The GOLD stages were I, II, III, and IV in 0, 6, 3, and 9 patients in the M1 group, respectively, and 4, 2, 10, and 2 patients in the W1 group, respectively. No significant difference was noted in any item between the M1 and W1 groups.
Table 1. Background of the subjects.
| M1 group | W1 group | |
|---|---|---|
| Number | 18 | 18 |
| Age | 67.2±6.5 | 65.2±4.5 |
| Height (m) | 1.65±0.06 | 1.65±0.05 |
| Weight (kg) | 58.3±6.9 | 63.4±4.4 |
| BMI | 21.2±2.5 | 23.1±1.2 |
| GOLD class | I: 0, II: 6, III: 3, IV: 9 | I: 4, II: 2, III: 10, IV: 2 |
| VC (L) | 3.2±0.7 | 3.3±0.6 |
| %VC (%) | 98.6±18 | 97.4±18 |
| FEV1.0 (L) | 1.44±0.6 | 1.2±0.5 |
| %FEV1.0 (%) | 49.5±20 | 40.2±17 |
| FEV1.0% (%) | 44.6±14 | 36.3±14 |
Mean±SD. BMI: body mass index, GOLD class: from the international guideline COPD, VC: vital capacity, %VC: % predicted VC, FEV1.0: forced expiratory volume in 1 second, %FEV1.0: % predicted FEV1.0, FEV1.0%: forced expiratory volume in 1 second percent
Table 2 shows the pre- and post-intervention results of examinations for the 3-month (12-week) outpatient pulmonary rehabilitation program in the M1 and W1 groups. Table 3 shows a comparison of the rates of change. Significant improvements of QMVC, 6MWD, environment, and the average QOL were noted in the W1 group compared with the M1 group.
Table2. Pre- and post-intervention results for the pulmonary rehabilitation items.
| Rate of change | M1 group | W1 group | |||
|---|---|---|---|---|---|
| Pre | Post | Pre | Post | ||
| VC | 3.21±0.7 | 3.35±0.8 | 3.3±0.6 | 3.41±0.7 | |
| %VC | 98.6±18 | 102.4±22 | 97.4±18 | 100.7±17 | |
| FEV1.0 | 1.44±0.6 | 1.58±0.6 | 1.2±0.5 | 1.55±0.8 | |
| %FEV1.0 | 49.5±20 | 57.9±17 | 40.2±17 | 55.3±24 | |
| FEV1.0% | 44.6±14 | 46.9±12 | 36.3±14 | 44.2±19 | |
| QMVC | 4.9±1.6 | 5.4±1.5 | 4.28±1.8 | 5.15±1.7 | |
| WHO/QOL26 | |||||
| Physical | 20.7±2.3 | 22.8±1.4 | 21.7±1.5 | 24.3±2.8 | |
| Psychology | 19.5±2.8 | 20.3±2.4 | 18.6±3.1 | 20.5±2.0 | |
| Society | 10.2±1.8 | 10.0±0.8 | 9.67±1.9 | 9.83±1.5 | |
| Environment | 25.4±1.6 | 25.5±3.0 | 21.3±2.5 | 27.8±1.7 | |
| Overall | 6.22±0.9 | 6.22±1.0 | 6.17±0.4 | 6.5±0.9 | |
| AverageQOL | 3.16±0.3 | 3.26±0.3 | 2.98±0.3 | 3.42±0.1 | |
| 6MWD | 410±66 | 437±99 | 399±101 | 468±107 | |
Mean±SD, QMVC: quadriceps maximal voluntary contraction force, WHO/QOL26: The World Health Organization QOL Assessment 26, 6MWD: six-minute walking distance
Table 3. Comparison of the rate of change in pulmonary rehabilitation items due to differences in the frequency of intervention.
| Rate of change | M1 group | W1 group | |
|---|---|---|---|
| VC | 4.3±12.5 | 5.5±19.4 | |
| %VC | 3.9±11.3 | 4.9±16.6 | |
| FEV1.0 | 14.0±32.1 | 32.5±52.3 | |
| %FEV1.0 | 25.3±35.4 | 42.4±50.9 | |
| FEV1.0% | 8.3±20.3 | 21.3±26.1 | |
| QMVC | 10.7±14.5 | 24.6±16** | |
| WHO/QOL26 | |||
| Physical | 11.4±10.5 | 12.6±14.8 | |
| Psychological | −0.16±20.3 | −4.9±14.3 | |
| Social | 1.94±25.9 | 6.4±29.2 | |
| Environment | 0.7±12.9 | 31.4±9.0** | |
| Overall | 2.41±25.5 | 5.95±18.4 | |
| Average QOL | 4.4±13.8 | 15.6±10.3* | |
| 6MWD | 6.05±15.3 | 18.6±7.9** | |
Mean±SD, * p<0.05; ** p<0.01
DISCUSSION
No significant differences were noted in the rate of change in any item for respiratory function (VC, %VC, FEV1.0, %FEV1.0, and FEV1.0%) after the intervention between the M1 and W1 groups. Improvement of respiratory function was not considered in many reports on respiration10), and no difference in the rate of change associated with the difference in the intervention frequency was noted in our study.
For pulmonary rehabilitation, it is important to increase the exercise capacity by increasing the peripheral muscle strength and cardiorespiratory endurance. Among the evaluation items for exercise capacity, the 6MWD is frequently used to evaluate COPD patients, and an increase in the value markedly influences ADL and the QOL3). The distance increased by 27 and 81 m on average in the M1 and W1 groups, respectively. For interpretation of the results of the 6MWD, Redelmeier et al.11) proposed that an increase of 70 m or more is a significant improvement as a result of an intervention in patients with stable COPD. Thus, the W1 group achieved a significant improvement.
On comparison of the rates of intervention-induced change in QMVC and 6MWD, the rates were significantly greater in the W1 group than in the M1 group. The W1 group was frequently instructed in Home ex, which may have maintained their motivation for pulmonary rehabilitation and led to the favorable outcomes.
On comparison of the rate of change in WHO/QOL26, the rates for “environment” and “average QOL” were significantly greater in the W1 group than in the M1 group. Since the “environment” domain contained a question asking about the quality of the follow-up for the disease at the hospital, this may have been involved in the high rate of change in the W1 group because of the high frequency of intervention. The rates of change in the other items were also greater in the W1 group, which may have influenced the difference in the rate of change in “average QOL”. Regarding the WHO/QOL26, the standard average QOL is 3.29 in healthy subjects and 3.34 in those aged 60–79 years, the age of the patients in our study9). The average QOL before intervention was 3.16 in the M1 group and 2.98 in the W1 group, and the values after intervention were 3.26 and 3.42, respectively. QOL improved to a favorable level after intervention in the W1 group, suggesting that a higher intervention frequency is more effective in improving QOL.
The M1 and W1 groups underwent 12 weeks of outpatient pulmonary rehabilitation centering on Home ex guidance. The rehabilitation aimed at improving lower limb muscle strength, exercise tolerance, and QOL was more effective in the once-a-week intervention group in which Home ex guidance was performed more frequently.
REFERENCES
- 1.National Heart, Lung and Blood institute, World Health Organization: Global initiative for chronic obstructive lung disease (GOLD): global strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary. Disease.Am J Respir Care Med, 2001, 163: 1256–1276 [DOI] [PubMed] [Google Scholar]
- 2.Ries AL: Position paper of the American Association of Cardiovascular and Pulmonary Rehabilitation. Scientific basis of pulmonary rehabilitation. J Cardiopulm Rehabil, 1990, 10: 418–441 [Google Scholar]
- 3.Ries AL, Bauldoff GS, Carlin BW, et al. : Pulmonary rehabilitation: joint ACCP/AACVPR evidence-based clinical practice guidelines. Chest, 2007, 131: 4S–42S [DOI] [PubMed] [Google Scholar]
- 4.Ando M, Mori A, Esaki H, et al. : [A study of the long-term effectiveness of an outpatient pulmonary rehabilitation program]. Nihon Kokyuki Gakkai Zasshi, 1999, 37: 680–687 [PubMed] [Google Scholar]
- 5.Ando M, Mori A, Esaki H, et al. : [The effects of pulmonary rehabilitation in elderly patients]. Nihon Kokyuki Gakkai Zasshi, 2003, 41: 81–88 [PubMed] [Google Scholar]
- 6.Minoguchi H, Shibuya M, Miyagawa T, et al. : Cross-over comparison between respiratory muscle stretch gymnastics and inspiratory muscle training. Intern Med, 2002, 41: 805–812 [DOI] [PubMed] [Google Scholar]
- 7.Swallow EB, Reyes D, Hopkinson NS, et al. : Quadriceps strength predicts mortality in patients with moderate to severe chronic obstructive pulmonary disease. Thorax, 2007, 62: 115–120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Man WD, Hopkinson NS, Harraf F, et al. : Abdominal muscle and quadriceps strength in chronic obstructive pulmonary disease. Thorax, 2005, 60: 718–722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nakane Y, Tasaki M, Miyaoka E: WHOQOL-BREF survey of general population. Iryo To Shakai, 1999, 9: 123–131 [Google Scholar]
- 10.Ries AL, Moser KM: Comparison of isocapnic hyperventilation and walking exercise training at home in pulmonary rehabilitation. Chest, 1986, 90: 285–289 [DOI] [PubMed] [Google Scholar]
- 11.Redelmeier DA, Bayoumi AM, Goldstein RS, et al. : Interpreting small differences in functional status: the six minute walk test in chronic lung disease patients. Am J Respir Crit Care Med, 1997, 155: 1278–1282 [DOI] [PubMed] [Google Scholar]