Abstract
A dilemma in cancer immunology is that, although patients often develop active anti-tumor immune responses, the tumor still outgrows. It has become clear that under the pressure of the host’s immune system, cancer cells have adapted elaborate tactics to reduce their immunogenicity (also known as immunoselection) and/or to actively suppress immune cells and promote immune tolerance (also known as immunosubversion). In this issue of the European Journal of Immunology, Dolen and Esendagli [Eur. J. Immunol. 2013. 43: 747–757] show that acute myeloid leukemia (AML) cells develop an adaptive immune phenotype switching mechanism: In response to attack by activated T cells, the leukemia cells quickly downregulate the T-cell costimulatory ligand B7-H2 and reciprocally upregulate the coinhibitory ligands B7-H1 and B7-DC in order to shut down T-cell activation via the PD-1 pathway. These novel findings and their relevance for cancer immunotherapy, especially potential applications in PD-1 check-point blockade therapy are discussed in this Commentary.
In order to avoid host immune detection and to suppress the host immune response, cancer cells use immunoselection and immunosubversion tactics (reviewed in [1, 2]), often downmodulating MHC and costimulatory molecules, while upregulating co-inhibitory ligands (reviewed in [2]). B7-1 (CD80) and B7-2 (CD86) are the primary costimulatory ligands that promote naïve T-cell priming by engaging CD28 on the surface of T cells [3]. CTLA-4, a CD28 homolog expressed on activated T cells, attenuates T-cell responses upon ligation of B7-1 and/or B7-2 which bind to CTLA-4 with higher affinity than to CD28 [4, 5]. B7-H2 (ICOSL), a B7-1/B7-2 homolog, expressed on antigen-presenting cells as well as on peripheral tissues including vascular endothelial cells [6], also provides a strong costimulatory signal through ICOS, which is expressed on activated T cells and follicular T helper (Tfh) cells [7–10]. Human, but not murine, B7-H2 was recently found to also bind CD28 and CTLA-4 and to stimulate proliferation of human T cells through both the CD28 and ICOS pathways [11]. Interestingly, expression of the strongly-activating, costimulatory molecules B7-2 and B7-H2 has been observed on acute myeloid leukemia (AML) cells [12–14], which was not completely unexpected since myeloid cells naturally express these ligands. It was surprising, however, that the expression of B7-2 and/or B7-H2 on AML cells was associated with poor prognosis by several independent studies [12, 13, 15]. How does a tumor cell utilize and turn these immune stimulatory ligands to its favor and create a suppressive environment? The study by Dolen and Esendagli [16] in this issue of the European Journal of Immunology sheds some lights on the potential scheme deployed by AML cells to trick and suppress the host immune system.
Dolen and Esendagli [16] adopted a conditioned myeloid leukemia cell line, HL-60, as an in vitro model system resembling AML, with the cell line displaying B7-2 and B7-H2 surface expression. PMA-treated HL-60 cells were able to act as costimulators driving CD4+ T-cell proliferation and production of cytokines associated with Th1 and Th17 cells, in the presence of a suboptimal amount of a CD3 antibody mimicking the TCR signal. The costimulation was largely contributed by the B7-2+ HL-60 cells. The expression of costimulatory molecules on leukemia cells thus appears to induce a strong initial T-cell activation and might bring the cancer cells’ own demise. However, continuing the co-culture with activated T cells, the leukemia cell line quickly changed its immune phenotype: it upregulated B7-H1 and B7-DC, downregulated B7-H2, while maintained its B7-2 level. B7-H1 (PD-L1) and B7-DC (PD-L2) are important inhibitory molecules that control the T-cell response by engaging with PD-1 expressed on activated T cells [17–19]. PD-1 is not only expressed on activated T cells but also on activated B and myeloid cells and thus regulates both adaptive and innate immunity [20–22]. The negative regulatory function of the B7-H1/PD-1 pathway has been exploited by tumors as evidenced by the overexpression of B7-H1 on many tumor types, including AML [23–25]. Importantly, the expression of B7-H1 has been correlated with poor prognosis of numerous human malignancies e.g. renal cancer [26]. In addition, the B7-H1/PD-1 pathway has recently been identified to contribute to T-cell exhaustion, a hypo-reactive T-cell condition observed in both cancer and chronic viral infections [27]. Given that B7-H1 is known to be quickly induced in a variety of tissues and cell types upon stimulation by proinflammatory cytokines secreted by activated T cells, including interferons, the upregulation of B7-H1 on the AML cell line is thus likely a result of cytokine stimulation, especially by IFN-γ.
With the observed upregulation of the immune suppressive molecules B7-H1 and B7-DC, and the reciprocal down-modulation of the immune costimulator B7-H2 on the cultured leukemia cell line, Dolen and Esendagli [16] went on further to address whether these adaptive changes by AML cells, upon exposure to activated T cells, provide an immune evasion mechanism for leukemia cells. Indeed, when naive CD4+ T cells were co-cultured with the conditioned leukemia cells, subsequent T-cell activation and cytokine production were dampened. Many of the resulting T cells after incubation with leukemia cells showed a CD25+ CD127−/low Tregcell phenotype. Expression of the PD-1 ligands (i.e. B7-H1 and B7-DC) on the leukemia cells was critical for the cells’ inhibitory activity since inclusion of a PD-1-Ig fusion protein largely abolished the suppression.
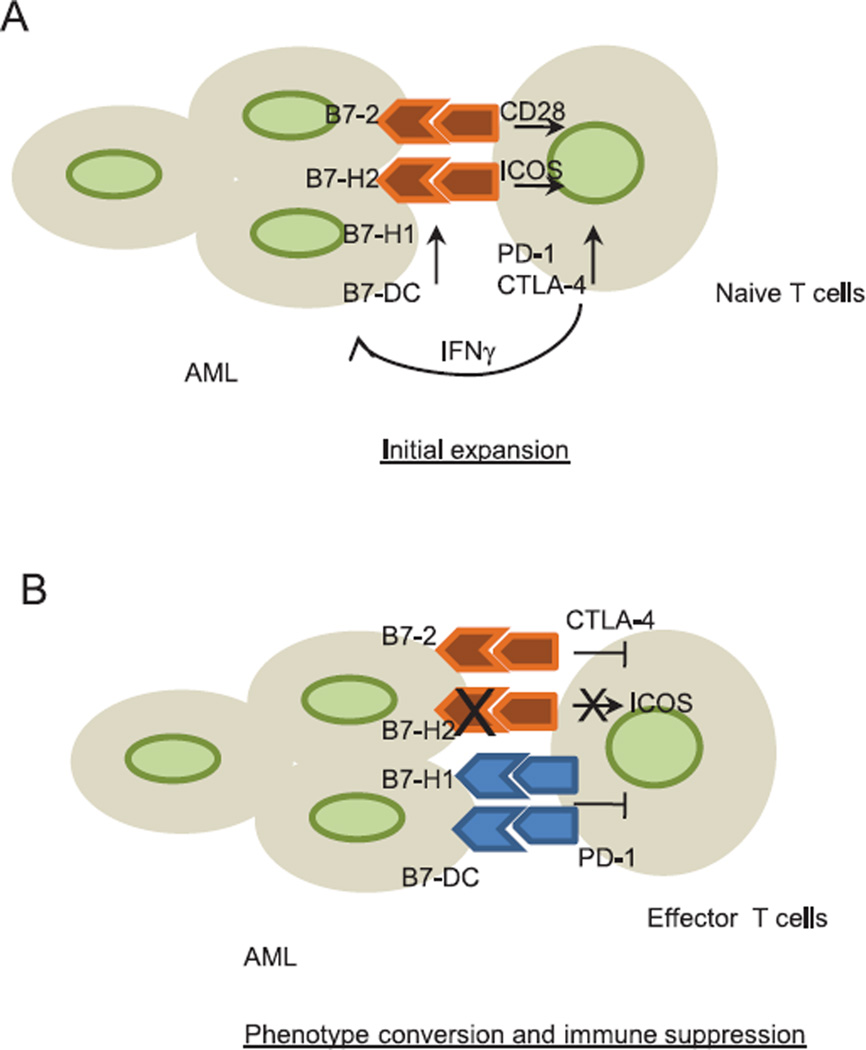
In their article, Dolen and Esendagli [16] describe a very intriguing observation revealing an adaptive resistance mechanism employed by AML cells. Expression of costimulatory ligands such as B7-2 and B7-H2, on AML cells supports initial tumorspecific T-cell expansion and cytokine production (Fig. 1). In response to the proinflammatory cytokines secreted by the activated T cells, AML cells quickly upregulate B7-H1 and B7-DC, and downregulate B7-H2 to shut down subsequent T-cell activation. A recent study in melanoma patients has established a strong association of tumor infiltrating lymphocytes (TILs) with local B7-H1 expression on the tumor [28], indicating that the cancer cell upregulates B7-H1 in response to IFN-γ released by TILs as an adaptive immune-resistance mechanism to suppress local effector T-cell function. PD-1 blockade immunotherapy could thus be especially effective in cases where the B7-H1/PD-1 inhibitory pathway is extensively exploited by the tumor, such as AML cells described by Dolen and Esendagli [16]. A recent exciting anti-PD-1 clinical trial reported objective responses in approximately one third of late-stage melanoma, non-small cell lung carcinoma and renal cell carcinoma patients with a durable response, indicating the formation of long-lasting lymphocyte memory [29]. Expression of tumor-associated B7-H1 prior to treatment seemed to correlate with the favorable clinical response to anti-PD-1 therapy in a small patient cohort [30], suggesting the potential use of tumor B7-H1 expression as a biomarker.
Figure 1.
Adaptive immune resistance of acute myeloid leukemia (AML). (A) AML cells express costimulatory ligands B7-2 and B7-H2 and support an initial tumor specific T cell activation and expansion by engaging CD28 and ICOS on T cells. Activated T cells release an array of proinflammatory cytokines upon activation, including IFN-γ and TNF-α, which in turn upregulate B7-H1 and B7-DC on AML cells. Inhibitory receptors PD-1 and CTLA-4 are also induced upon T cell activation. (B) In response to the immune attack by activated T cell, AML cells quickly switch to an immune suppressive phenotype by downmodulating B7-H2 expression and upregulating PD-1 ligands, B7-H1 and B7-DC. The adaptive phenotypic change triggers T cell coinhibitory signal through PD-1 pathway to shut down T cell response.
Nevertheless, several important issues remain to be addressed in future studies. B7-H2 is known to be upregulated on APCs and peripheral tissues upon stimulation by TLR ligands or proinflammatory cytokines. As a result, the mechanism underlying B7-H2 downregulation on leukemia cells upon co-culture with activated T cells needs to be further elucidated. It also remains to be validated whether similar adaptive immune phenotype changes will occur in vivo in AML cells from different patients, as observed in leukemia cell lines in vitro, or in only a percentage of the cancer patients. Most importantly, the results of the clinical response and phenotypic changes noted in the current ongoing anti-PD-1 trials in leukemia should provide invaluable information about the dynamic interactions of a fluid tumor and host immune system, and help inform the strategy to be used to overcome tumor adaptive evasion.
Acknowledgements
We like to thank Beth Cadugan for editing the manuscript. This work is supported by NIH grant CA142779, CA121974, CA16359 and CA97085.
References
- 1.Zitvogel L, Tesniere A, Kroemer G. Cancer despite immunosurveillance: immunoselection and immunosubversion. Nat Rev Immunol. 2006;6:715–727. doi: 10.1038/nri1936. [DOI] [PubMed] [Google Scholar]
- 2.Chen L. Co-inhibitory molecules of the B7-CD28 family in the control of T-cell immunity. Nat Rev Immunol. 2004;4:336–347. doi: 10.1038/nri1349. [DOI] [PubMed] [Google Scholar]
- 3.Linsley PS, Clark EA, Ledbetter JA. T-cell antigen CD28 mediates adhesion with B cells by interacting with activation antigen B7/BB-1. Proc Natl Acad Sci U S A. 1990;87:5031–5035. doi: 10.1073/pnas.87.13.5031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Krummel MF, Allison JP. CD28 and CTLA-4 have opposing effects on the response of T cells to stimulation. J Exp Med. 1995;182:459–465. doi: 10.1084/jem.182.2.459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Walunas TL, Lenschow DJ, Bakker CY, Linsley PS, Freeman GJ, Green JM, Thompson CB, et al. CTLA-4 can function as a negative regulator of T cell activation. Immunity. 1994;1:405–413. doi: 10.1016/1074-7613(94)90071-x. [DOI] [PubMed] [Google Scholar]
- 6.Khayyamian S, Hutloff A, Buchner K, Grafe M, Henn V, Kroczek RA, Mages HW. ICOS-ligand, expressed on human endothelial cells, costimulates Th1 and Th2 cytokine secretion by memory CD4+ T cells. Proc Natl Acad Sci USA. 2002;99:6198–6203. doi: 10.1073/pnas.092576699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hutloff A, Dittrich AM, Beier KC, Eljaschewitsch B, Kraft R, Anagnostopoulos I, Kroczek RA. ICOS is an inducible T-cell costimulator structurally and functionally related to CD28. Nature. 1999;397:263–266. doi: 10.1038/16717. [DOI] [PubMed] [Google Scholar]
- 8.Yoshinaga SK, Whoriskey JS, Khare SD, Sarmiento U, Guo J, Horan T, Shih G, et al. T-cell co-stimulation through B7RP-1 and ICOS. Nature. 1999;402:827–832. doi: 10.1038/45582. [DOI] [PubMed] [Google Scholar]
- 9.Dong C, Juedes AE, Temann UA, Shresta S, Allison JP, Ruddle NH, Flavell RA. ICOS co-stimulatory receptor is essential for T-cell activation and function. Nature. 2001;409:97–101. doi: 10.1038/35051100. [DOI] [PubMed] [Google Scholar]
- 10.McAdam AJ, Greenwald RJ, Levin MA, Chernova T, Malenkovich N, Ling V, Freeman GJ, et al. ICOS is critical for CD40-mediated antibody class switching. Nature. 2001;409:102–105. doi: 10.1038/35051107. [DOI] [PubMed] [Google Scholar]
- 11.Yao S, Zhu Y, Zhu G, Augustine M, Zheng L, Goode DJ, Broadwater M, et al. B7-h2 is a costimulatory ligand for CD28 in human. Immunity. 2011;34:729–740. doi: 10.1016/j.immuni.2011.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tamura H, Dan K, Tamada K, Nakamura K, Shioi Y, Hyodo H, Wang SD, et al. Expression of functional B7-H2 and B7.2 costimulatory molecules and their prognostic implications in de novo acute myeloid leukemia. Clin Cancer Res. 2005;11:5708–5717. doi: 10.1158/1078-0432.CCR-04-2672. [DOI] [PubMed] [Google Scholar]
- 13.Maeda A, Yamamoto K, Yamashita K, Asagoe K, Nohgawa M, Kita K, Iwasaki H, et al. The expression of co-stimulatory molecules and their relationship to the prognosis of human acute myeloid leukaemia: poor prognosis of B7-2-positive leukaemia. Br J Haematol. 1998;102:1257–1262. doi: 10.1046/j.1365-2141.1998.00901.x. [DOI] [PubMed] [Google Scholar]
- 14.Whiteway A, Corbett T, Anderson R, Macdonald I, Prentice HG. Expression of co-stimulatory molecules on acute myeloid leukaemia blasts may effect duration of first remission. Br J Haematol. 2003;120:442–451. doi: 10.1046/j.1365-2141.2003.04085.x. [DOI] [PubMed] [Google Scholar]
- 15.Graf M, Reif S, Hecht K, Pelka-Fleischer R, Kroell T, Pfister K, Schmetzer H. High expression of costimulatory molecules correlates with low relapse-free survival probability in acute myeloid leukemia (AML) Ann Hematol. 2005;84:287–297. doi: 10.1007/s00277-004-0978-0. [DOI] [PubMed] [Google Scholar]
- 16.Dolen Y, Esendagli G. Myeloid leukemia cells with a B7–2+ subpopulation provoke Th-cell responses and become immunosuppressive through the modulation of B7 ligands. Eur J Immunol. 2013;43:747–757. doi: 10.1002/eji.201242814. [DOI] [PubMed] [Google Scholar]
- 17.Dong H, Zhu G, Tamada K, Chen L. B7-H1, a thirdmember of the B7 family, co-stimulates T-cell proliferation and interleukin-10 secretion. Nat Med. 1999;5:1365–1369. doi: 10.1038/70932. [DOI] [PubMed] [Google Scholar]
- 18.Tseng SY, Otsuji M, Gorski K, Huang X, Slansky JE, Pai SI, Shalabi A, et al. B7-DC, a new dendritic cell molecule with potent costimulatory properties for T cells. J Exp Med. 2001;193:839–846. doi: 10.1084/jem.193.7.839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Freeman GJ, Long AJ, Iwai Y, Bourque K, Chernova T, Nishimura H, Fitz LJ, et al. Engagement of the PD-1 immunoinhibitory receptor by a novel B7 family member leads to negative regulation of lymphocyte activation. J ExpMed. 2000;192:1027–1034. doi: 10.1084/jem.192.7.1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Agata Y, Kawasaki A, Nishimura H, Ishida Y, Tsubata T, Yagita H, Honjo T. Expression of the PD-1 antigen on the surface of stimulated mouse T and B lymphocytes. Int Immunol. 1996;8:765–772. doi: 10.1093/intimm/8.5.765. [DOI] [PubMed] [Google Scholar]
- 21.Yao S, Wang S, Zhu Y, Luo L, Zhu G, Flies S, Xu H, et al. PD-1 on dendritic cells impedes innate immunity against bacterial infection. Blood. 2009;113:5811–5818. doi: 10.1182/blood-2009-02-203141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Said EA, Dupuy FP, Trautmann L, Zhang Y, Shi Y, El-Far M, Hill BJ, et al. Programmed death-1-induced interleukin-10 production by monocytes impairs CD4+ T cell activation during HIV infection. Nat Med. 2010;16:452–459. doi: 10.1038/nm.2106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dong H, Strome SE, Salomao DR, Tamura H, Hirano F, Flies DB, Roche PC, et al. Tumor-associated B7-H1 promotes T-cell apoptosis: a potential mechanism of immune evasion. Nat Med. 2002;8:793–800. doi: 10.1038/nm730. [DOI] [PubMed] [Google Scholar]
- 24.Zou W, Chen L. Inhibitory B7-family molecules in the tumour microenvironment. Nat Rev Immunol. 2008;8:467–477. doi: 10.1038/nri2326. [DOI] [PubMed] [Google Scholar]
- 25.Chen X, Liu S, Wang L, Zhang W, Ji Y, Ma X. Clinical significance of B7-H1 (PD-L1) expression in human acute leukemia. Cancer Biol Ther. 2008;7:622–627. doi: 10.4161/cbt.7.5.5689. [DOI] [PubMed] [Google Scholar]
- 26.Thompson RH, Kuntz SM, Leibovich BC, Dong H, Lohse CM, Webster WS, Sengupta S, et al. Tumor B7-H1 is associated with poor prognosis in renal cell carcinoma patients with long-term follow-up. Cancer Res. 2006;66:3381–3385. doi: 10.1158/0008-5472.CAN-05-4303. [DOI] [PubMed] [Google Scholar]
- 27.Zajac AJ, Blattman JN, Murali-Krishna K, Sourdive DJ, Suresh M, Altman JD, Ahmed R. Viral immune evasion due to persistence of activated T cells without effector function. J Exp Med. 1998;188:2205–2213. doi: 10.1084/jem.188.12.2205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Taube JM, Anders RA, Young GD, Xu H, Sharma R, McMiller TL, Chen S, et al. Colocalization of inflammatory response with B7-h1 expression in human melanocytic lesions supports an adaptive resistance mechanism of immune escape. Sci Transl Med. 2012;4:127–137. doi: 10.1126/scitranslmed.3003689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Topalian SL, Hodi FS, Brahmer JR, Gettinger SN, Smith DC, McDermott DF, Powderly JD, et al. Safety, Activity, and Immune Correlates of Anti-PD-1 Antibody in Cancer. N Engl J Med. 2012;366:2443–2454. doi: 10.1056/NEJMoa1200690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brahmer JR, Drake CG, Wollner I, Powderly JD, Picus J, Sharfman WH, Stankevich E, et al. Phase I study of single-agent anti-programmed death-1 (MDX-1106) in refractory solid tumors: safety, clinical activity, pharmacodynamics, and immunologic correlates. J Clin Oncol. 2010;28:3167–3175. doi: 10.1200/JCO.2009.26.7609. [DOI] [PMC free article] [PubMed] [Google Scholar]