Abstract
Vanishing white matter disease (VWM) is a genetic leukoencephalopathy linked to mutations in the eukaryotic translation initiation factor 2B (eIF2B). It is a disease of infants, children and adults, who experience a slowly progressive neurological deterioration with episodes of rapid clinical worsening triggered by stress and eventually leading to death. Characteristic neuropathological findings include cystic degeneration of the white matter with scarce reactive gliosis, dysmorphic astrocytes, and paucity of myelin despite an increase in oligodendrocytic density. To assess whether a defective maturation of macroglia may be responsible for the feeble gliosis and lack of myelin, we investigated the maturation status of astrocytes and oligodendrocytes in the brains of 8 VWM patients, 4 patients with other white matter disorders and 6 age-matched controls with a combination of immunocytochemistry, histochemistry, scratch-wound assays, Western blot and quantitative PCR. We observed increased proliferation and a defect in the maturation of VWM astrocytes. They show an anomalous composition of their intermediate filament network with predominance of the δ-isoform of the glial fibrillary acidic protein and an increase in the heat shock protein αB-crystallin, supporting the possibility that a deficiency in astrocyte function may contribute to the loss of white matter in VWM. We also demonstrated a significant increase in numbers of pre-myelinating oligodendrocyte progenitors in VWM, which may explain the co-existence of oligodendrocytosis and myelin paucity in the patients’ white matter.
Keywords: Astrocytes, GFAPδ, Glia maturation, Olig2 cytoplasmic translocation, Oligodendrocyte progenitor cells, Vanishing white matter
INTRODUCTION
Leukoencephalopathy with vanishing white matter (VWM; OMIM number 603896) (1), also referred to as childhood ataxia with diffuse central nervous system hypomyelination (2) and myelinopathia centralis diffusa (3), is one of the most prevalent inherited childhood white matter disorders (4). VWM is caused by mutations in any of 5 genes that encode the eukaryotic translation initiation factor 2B (eIF2B) (5, 6), a ubiquitously expressed heteropentamer involved in the regulation of protein synthesis. Clinically, VWM is characterized by progressive cerebellar ataxia with spasticity and cognitive decline. VWM is typified by episodes of major neurological deterioration triggered by mild stresses as fever and minor trauma, which may lead to unexplained coma and death (4).
The radiographic and pathologic findings in VWM are distinctive (7). The loss of white matter documented on MRI correlates with increasing rarefaction and cystic degeneration of the tissue, which is eventually replaced by fluid. Macroglia are selectively involved. In and around areas of cavitation the degree of reactive gliosis is disproportionately low relative to the extent of white matter damage, whereas those reactive astrocytes that are found exhibit overtly aberrant morphology (4, 7, 8). In less involved areas of relative preservation, lack of myelin is accompanied by increased density of oligodendrocytes identified by their morphological and immunohistochemical properties (8, 9).
This study was designed to investigate the nature of glial pathology in VWM, in particular the role of astrocytes in the cystic degeneration of the white matter. In addition, we sought to understand the paradox of lack of myelin in the face of increased oligodendrocytic density. In addressing both issues we asked whether defective glial maturation might represent a critical causal determinant of VWM.
MATERIALS AND METHODS
Patients
Brain tissue from 8 genetically proven VWM patients was collected at the VU University Medical Center in Amsterdam, the Netherlands, or obtained from the Brain and Tissue Bank for Developmental Disorders at the University of Maryland, Baltimore, MD. The non-neurological controls included 5 subjects without significant or confounding neuropathological findings at autopsy. Additional control tissue was obtained from an adult who underwent therapeutic surgical resection for refractory epilepsy. In addition, 4 disease controls were used: 1 patient with juvenile-onset X-linked adrenoleukodystrophy (X-ALD); 1 child with infantile Krabbe disease (globoid cell leukodystrophy, GLD); 1 patient with adolescent-onset Alexander disease (AXD); and an adult with multiple sclerosis (MS) (Table 1). The study was approved by the Institutional Review Board. Informed consent was obtained in all cases. Tissue from patients VWM295 and VWM80 has been used in previous studies (10–12).
Table 1.
Demographic Data and Usage of Patient Material
| Subject | Age | Clinical diagnosis | Usage |
|---|---|---|---|
| VWM295 | 4.5 mo | Severe VWM; β, Gly200Val/Pro291Ser* | IHC, WB, qPCR |
| VWM251 | 4 y | Severe VWM; ε, Thr91Ala/Val437Met* | Primary astrocytic culture, ICC |
| VWM576 | 6 y | Severe VWM; ε, Thr91Ala/Val437Met* | Primary oligodendrocytic and astrocytic culture, ICC |
| VWM367 | 10 y | Classic VWM; ε, Arg113His/Ala403Val* | IHC, qPCR |
| VWM80 | 12 y | Classic VWM; ε, Thr91Ala/Trp628Arg* | IHC, WB, qPCR |
| VWM99 | 16 y | Classic VWM; ε, Thr91Ala/Trp628Arg* | IHC |
| VWM3 | 29 y | Mild VWM; ε, Thr91Ala/Thr91Ala* | IHC, WB, qPCR, primary astrocytic culture, ICC |
| VWM44 | 36 y | Mild VWM; ε, Arg113His/Arg133His* | IHC, primary astrocytic culture |
| Control 1 | 29 w GA | Non-neurological control (intrauterine sepsis) | Primary astrocytic culture, ICC |
| Control 2 | 4.5 mo | Non-neurological control (multiple traumatic injuries) | IHC, WB, qPCR |
| Control 3 | 13 y | Non-neurological control (multiple traumatic injuries) | IHC, WB, qPCR |
| Control 4 | 21 y | Non-neurological control (brachio-oto-renal syndrome) | Primary astrocytic culture, ICC, qPCR |
| Control 5 | 47 y | Non-neurological control (refractory epilepsy, surgical specimen) | Primary astrocytic culture, ICC |
| Control 6 | 63 y | Non-neurological control (breast carcinoma) | IHC, qPCR |
| Control 7 | 1 y | Krabbe disease | IHC |
| Control 8 | 12 y | X-linked adrenoleukodystrophy | IHC |
| Control 9 | 29 y | Alexander disease | IHC |
| Control 10 | 66 y | Multiple sclerosis | IHC |
The mutant eIF2B subunit and amino acid changes are indicated. IHC, immunohistochemistry; WB, Western blot analysis; qPCR, quantitative PCR analysis; ICC, immunocytochemistry; GA, gestational age; VWM, vanishing white matter disease.
The study focused on frontal lobe white matter and brain specimens were selected from relatively preserved subcortical areas adjacent to cavitary foci. Corresponding areas were selected from controls. Because of the different stages of disease that influenced the amount of white matter obtainable and different abundance of control tissue, not all VWM patients and controls could be used for each experiment (Table 1).
Immunohistochemical staining
Tissue from 5 VWM patients, 3 non-neurological controls and 4 neurological controls was snap-frozen and conserved at −80°C. Twenty-µm-thick sections were mounted on glass slides, fixed in 1% or 4% paraformaldehyde, and subsequently permeabilized with 0.1% saponin, blocked in 5% normal donkey serum and incubated with primary antibodies for 24 to 72 hours at 4°C. In addition, tissue from patient VWM367 was formalin-fixed and paraffin-embedded, and sections were deparaffinized and stained according to standard protocols. Immunohistochemistry was performed using the antibodies listed in Table 2. Negative controls, by omitting the primary antibody, were included in each experiment. After staining with secondary antibodies (Alexa 488-, 568-, and 594-tagged anti-mouse, anti-rabbit, and anti-chicken IgG, and anti-mouse IgM; 1:400; Molecular Probes; Invitrogen, Breda, The Netherlands), sections were counterstained with DAPI (10 ng/ml; Molecular Probes; Invitrogen) and photographed using a Leica DM6000B microscope or an Olympus FluoView 300 confocal microscope. Immunopositivity on paraffin-embedded material was detected with 3.3’ diaminobenzidine as chromogen.
Table 2.
Antibodies and q-PCR Primers
| Antibody | Marker | Dilution | Vendor | Catalog no. |
|---|---|---|---|---|
| Ki67 (Mib-1) | Cell proliferation | 1:400 | Neomarkers | clone SP6, RM-9106-S1 |
| GFAP | Astrocytes | 1:1000 | Millipore | AB5541 |
| S100β | Astrocytes | 1:200 | Sigma | S2532 |
| Vimentin | Astrocytes | 1:2000 | clone V9 (a) | |
| Nestin | Astrocytes | 1:200 | Millipore | MAB5623 |
| GFAPδ | Astrocytes | 1:500 | (b) | |
| αB-crystallin | Astrocytes | 1:1000 | Novocastra | ABCRYS-512-U |
| CD44 (Hermes3) | Astrocyte progenitors | 1:1000 | (c) | |
| Olig2 | OPC/Oligodendrocytes | 1:400 | Abcam | ab33427 |
| PDGFRα (CD140a) | OPC | 1:100 | BD Pharmigen | 556001 |
| NG2 | OPC | 1:100 | Millipore | MAB2029 (clone 9.2.27) |
| GalC (O1) | Oligodendrocytes | 1:30 | Millipore | AB142 |
| GalC (O1) | Oligodendrocytes | 1:50 | Sigma-Aldrich | O7014 |
| GAPDH | Constitutively expressed | 1:500 | Abcam | Ab9485 |
| q-PCR primer (5’-3’) | Sequence | |||
| GFAPδ, forward | CCTACAGGAAGCTGCTAGAG | |||
| GFAPδ, reverse | GCGTTCCATTTACAATCTGGT | |||
| Total GFAP, forward | AGAAGCTCCAGGATGAAACC | |||
| Total GFAP, reverse | TTCATCTGCTTCCTGTCTATAGG | |||
| GFAPα, forward | AGAGGTCATTAAGGAGTCCA | |||
| GFAPα, reverse | CAACTATCCTGCTTCTGCTC | |||
| GAPDH, forward | CTCTCTGCTCCTCCTGTTCGAC | |||
| GAPDH, reverse | TGAGCGATGTGGCTCGGCT | |||
| HPRT, forward | ATGGGAGGCCATCACATTGT | |||
| HPRT, reverse | ATGTAATCCAGCAGGTCAGCAA | |||
| RPLP0, forward | GTGATGTGCAGCTGATCAAGACT | |||
| RPLP0, reverse | GATGACCAGCCCAAAGGAGA | |||
| CypB, forward | AAGGACTTCATGATCCAGGG | |||
| CypB, reverse | TGAAGTTCTCATCGGGGAAG | |||
Antibody manufactured at the Department of Pathology, VU University Medical Center, Amsterdam, the Netherlands.
Antibody manufactured at the Netherlands Institute for Neurosciences, Amsterdam, the Netherlands (ref. 17).
Antibody kind gift of E. Aronica, University of Amsterdam, the Netherlands.
Quantification and Statistical Analysis
The total numbers of labeled and unlabeled cells were counted in at least 10 standardized fields using a 10× objective lens. For each stained section, immunopositive cells were counted individually and expressed as a percentage of the total number of DAPI-positive cells to avoid bias due to different cell density. The results of these counts were expressed as means ± standard deviations and compared using an unpaired Student t-test. The Prism4 software (Graph Pad Software, Inc., San Diego, CA) was used for these analyses.
SDS-PAGE and Western Blotting
Cell lysates of white and gray brain matter from 3 VWM patients and 2 controls were obtained, as previously described (10). In brief, approximately 1 mg of material was homogenized in NP40-lysis-buffer containing a protease inhibitor cocktail (Roche, Indianapolis, IN) with 1 mM dithiothreitol. The supernatants were run on 4% to 12% SDS-polyacrylamide Precast gels (Invitrogen) and transferred onto PVDF membranes (Immobilon P; Millipore, Billerica, MA). The blots were incubated with antibodies against glial fibrillary acidic proteinγδ (GFAPδ) and the endogenous protein glyceraldehyde-3-phosphate dehydrogenase (GAPDH) to control equal loading. Proteins were visualized using alkaline phosphatase-coupled secondary antibodies and ECF Western blot detection reagent (Amersham, Piscataway, NJ).
RNA isolation, Reverse Transcription, and Real-Time Quantitative-PCR
White matter samples from 4 VWM patients and 4 non-neurological controls were used for real-time quantitative-PCR (q-PCR) analysis of GFAP isoforms. RNA was extracted from frozen tissue with Trizol (Invitrogen, La Jolla, CA) and purified using RNeasy (Qiagen, Chatsworth, CA) according to manufacturers’ specifications. Subsequent reverse transcription to cDNA was performed with SuperScript III reverse transcriptase (Invitrogen) and q-PCR by using a LightCycler 480 II (Roche, Woerden, The Netherlands). Transcript-specific primers were generated with Primer Express software (Applied Biosystems, Foster City, CA) and designed to overlap exon-exon boundaries to prevent genomic DNA amplification (Table 2). The PCR reaction was carried out using a volume of 10 µl containing SYBR green PCR mix, 3.0 µM primers, and 0.03 µg cDNA. The relative abundance of transcript expression was calculated using the cycle of threshold value and normalized to the endogenous controls GAPDH, hypoxanthine-guanine phosphoribosyl transferase, cyclophilin B and ribosomal protein, large, P0.
Primary astrocyte cultures and scratch-wound assay
Primary astrocytes from 4 VWM patients and 3 non-neurological controls were grown in DMEM/F12 + Glutamax (Invitrogen) + 10% FCS (Hyclone, ThermoScientific, Etten-leur, The Netherlands) + 1 mM sodium pyruvate (Invitrogen) + 1× G5 supplement (Invitrogen) to a maximum of 6 passages. Cells were then plated on poly-l-lysine (P4707, Sigma-Aldrich, Zwijndrecht, The Netherlands) coated 12-well plates with clear bottoms (Corning Costar 3712, VWR, Amsterdam, The Netherlands) at a density of 1 × 106 cells/well in a volume of 1 ml, and incubated overnight (37°C, 5% CO2).
Scratching was performed 24 hours later using a custom made sterile aluminium scratch mould (cross with leg length 10 mm, gap diameter of 1 mm) and a sterile p10 filter tip to ensure standardized scratches. With the device in the well, the pipette tip was placed in the top-corner and pulled toward the user. Plates were fixed with 4% paraformaldehyde immediately or after a 24-, 48- or 72-hour incubation. After nuclear counterstain with DAPI (0.1 µg/ml, D9542, Sigma-Aldrich), images were acquired in an automated fashion using a Cellomics ArrayScan VTI HCS Reader (Cellomics, Inc., Pittsburgh, PA). Cell locations were determined using the accompanying software based on their nuclear staining. The resulting 49 images per well (and corresponding datasets of cell locations) were subsequently integrated using an in-house developed tool to determine the numbers of cells inside or outside the scratch area. The same scratch area definition was used for all wells.
Magnetic sorting of oligodendrocyte progenitor cells
Frontal white matter from patient VWM367 was separated from the gray matter, collected in HBSS with magnesium and calcium (Invitrogen), and then dissected and dissociated to a single-cell suspension using papain as described (13). The cells were suspended at 4 × 106 cells/ml in DMEM/F12/N1 + Glutamax (Invitrogen) with bFGF (20 ng/ml; Invitrogen) in 100-mm TC-treated culture dishes (Corning Costar) and incubated overnight (37°C, 5% CO2).
The day after dissociation, the cells were washed twice in HBSS without magnesium and calcium (Invitrogen), incubated with magnetically labelled anti-A2B5 beads (Milteny Biotec, Utrecht, The Netherlands), and sorted using positive selection columns according to the manufacturer’s protocol. To differentiate A2B5-positive glia progenitors into oligodendrocytes, cells were plated at 50,000 cells/well in double coated poly-l-lysine (P4707, Sigma-Aldrich) + laminin (10 µg/ml; L6274, Sigma-Aldrich) 8-well Labtek chamber slides (NUNC, VWR), in 400 µl DMEM/F12/N1 + Glutamax (Invitrogen) with neurotrophin-3 (2 ng/ml; N1905, Sigma-Aldrich), and thyroid hormone T3 (2 ng/ml; T5516, Sigma-Aldrich) for 72 hours. Cells were then fixed with 4% paraformaldehyde prior to immunocytochemistry (Table 2).
RESULTS
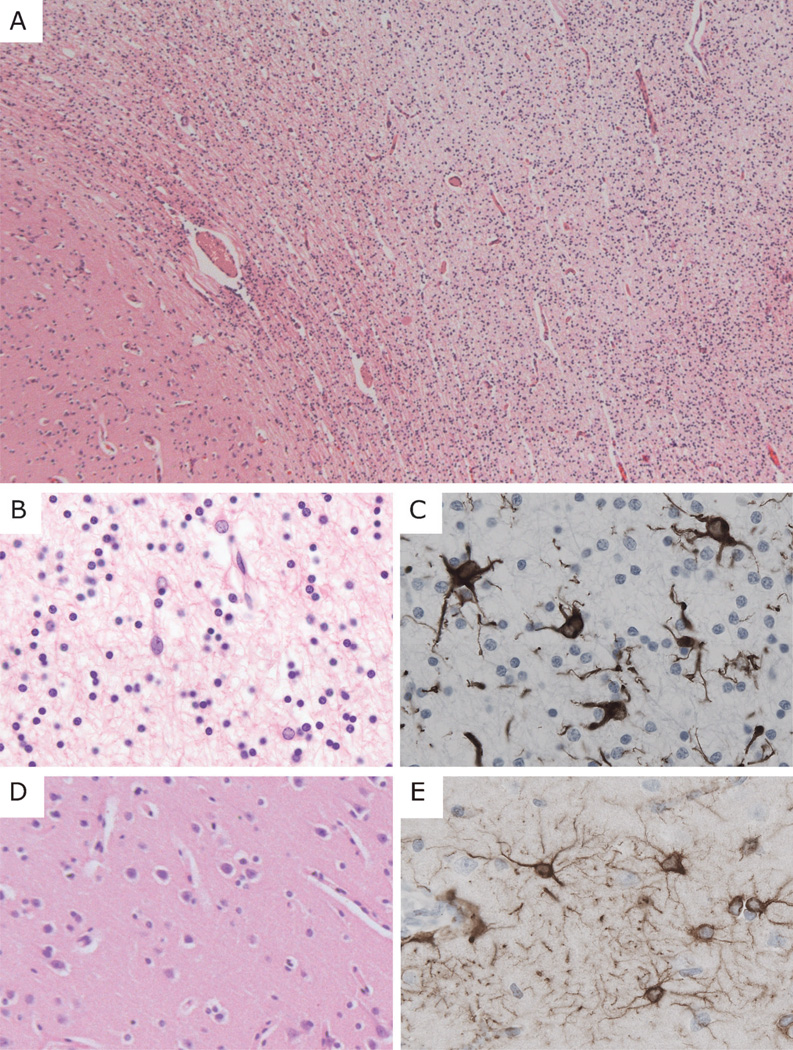
Hematoxylin and eosin-stained tissue sections of the VWM patients showed white matter rarefaction with myelin paucity and increased cellular density. The U-fibers were relatively preserved (Fig. 1A). Many cells in the VWM white matter exhibited oligodendroglial morphologies. Around areas of white matter vacuolation, astrocytes with coarse, blunt processes were also identified (Fig. 1B, C). Remarkably, despite the overtly aberrant appearance of white matter astroglia, their counterparts in adjacent gray matter regions appeared normal (Fig. 1D, E). Histopathology of the 4 neurological controls was consistent with their respective diagnoses (14). No significant abnormalities were found in the non-neurological controls.
Figure 1.
General neuropathological features of vanishing white matter disease. (A) Low-power magnification hematoxylin and eosin staining of the white matter (right side of field) from the frontal lobe of patient VWM367 shows tissue rarefaction and increased cellular density. The U-fibers appear relatively preserved; the overlying cortex is normal. (B, C) At higher magnification, white matter astrocytes display abnormal morphology with coarse blunt processes. (D, E) The cortical architecture and morphology of cortical astrocytes are normal. (A, B, D) Hematoxylin and eosin; (C, E) immunohistochemistry for glial fibrillary acidic protein. Original magnifications: A, 25×; B–E, 200×.
Astrocyte Pathology in Vanishing White Matter
Astrocytes proliferate in VWM in vivo and in vitro
To investigate the meager reactive gliosis in VWM we first determined whether astrocytes actively proliferate in VWM lesions. Compared to controls there was a significantly increased proportion of GFAP-positive astrocytes in the tissue from VWM patients that stained positively for the proliferation marker MIB-1/Ki-67 (Fig 2A). Some of these Ki-67-positive/GFAP-positive cells displayed incomplete nuclear separation or frank karyokinesis without cytokinesis (Fig. 2B).
Figure 2.
Vanishing white matter disease (VWM) astrocytes proliferate actively but do not reach full maturity. (A) There are significantly higher numbers of Ki-67-positive astrocytes in the white matter of VWM patients than in controls (n = 5 patients, 3 controls; p < 0.0001; bars = SD). (B) Double stain for glial fibrillary acidic protein (GFAP) and Ki-67 shows cells with incomplete separation of the nucleus and abnormal morphology with blunt processes (patient VWM3). (C) Scratch-wound assays of control 5 (left panel) and patient VWM44 (right panel) show increased proliferation of primary cultured astrocytes in the scratch 48 hours after administration of a mechanical stress. Nuclei of the proliferating cells inside the scratch area are blue. Nuclei of the unstressed cells outside this area are red; their net number is not changed vs. controls. (D) The slope of proliferation in the scratch area; the individual net values are indicated as dots (n = 4 patients, 3 controls; p = 0.06; the lack of significance is due to the large variance of cell growth among the different VWM patients vs. controls). (E, F) GFAP-positive astrocytes from VWM patients express the intermediate filament nestin (patient VWM99) (E), and are S100β-negative (F) patient VWM3), suggesting that they are immature. (G) Astrocytes from controls show normal morphology with fine arborizations and both nuclear and cytoplasmic S100β-immunoreactivity (control 2; single S100β staining in inset). Nuclei are stained with DAPI (blue) in all panels. Original magnifications: (B, F) bars indicate 2 µm and 10 µm, respectively; original magnifications: E, G, 400×.
Consistent with these observations, scratch-wound assays performed on primary astrocyte cultures from 4 VWM patients and 3 non-neurological controls showed that the slope of the cell growth inside the scratch area was markedly steeper in the cultures from the VWM patients, indicating a faster cell growth rate (Fig. 2C, D).
Astrocytes in VWM remain immature and express galactocerebroside and olig2
There was consistent and robust co-expression of vimentin and nestin in GFAP-positive cells from the VWM patients, suggesting immaturity (Fig. 2E). Consistent with this, no nuclear S100β immunolabeling was detected (Fig. 2F). By contrast, virtually all astrocytes in non-neurological disease control samples were nestin-negative and S100β-positive (Fig. 2G).
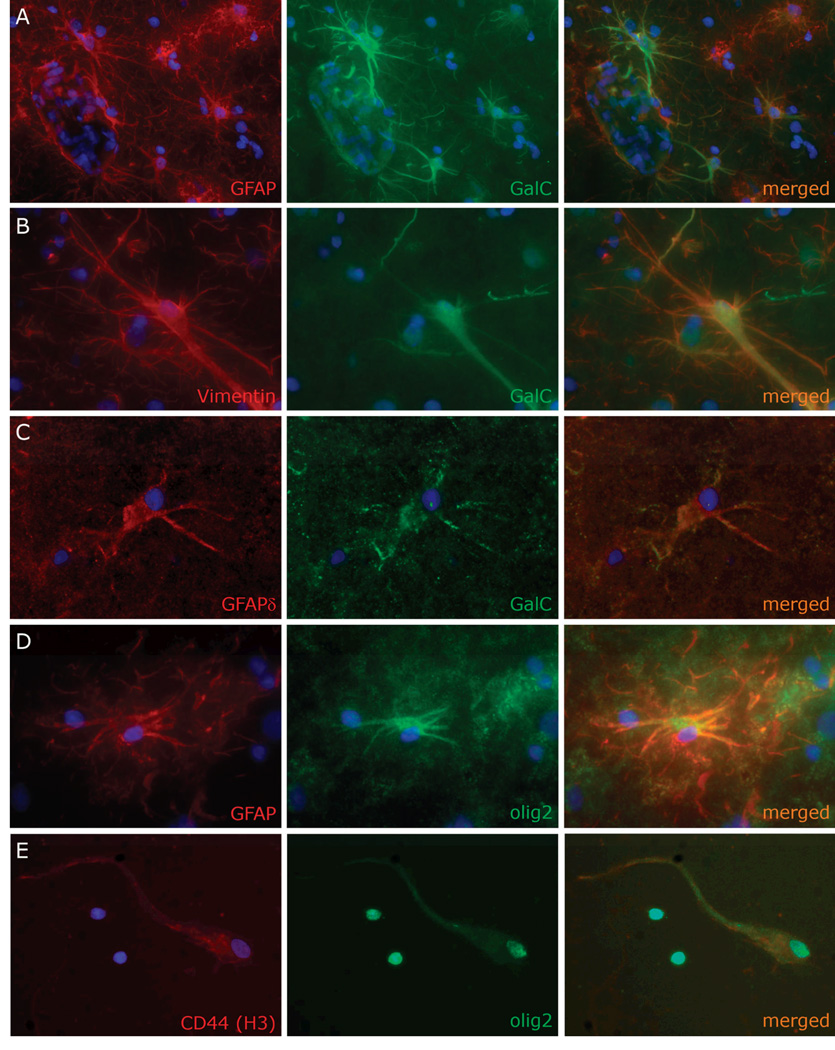
Aberrant co-expression of GFAP together with the oligodendrocyte-specific marker galactocerebroside (GalC) was previously described in vitro (11). This was interpreted as indicating a mixed lineage or immature cell type. GalC immunostaining on white matter sections from all VWM and controls samples and 2 anti-GalC antibodies from different manufacturers yielded identical results. Apparent astrocytes in the VWM patient white matter expressed GalC in a diffuse fashion in the cytoplasm of the cell body and processes (Fig. 3A–C). Similar, though less intense GalC expression was found in the white matter of the GLD patient, both in GFAP-positive astrocytes and in giant multinucleated GFAP-negative globoid cells. Rare and faintly GalC-positive astrocytes were found in the MS plaque and within an active demyelinating area in the X-ALD case. However, in both latter conditions, GalC-labeled astrocytes displayed punctate rather than diffuse immunoreactivity. No GalC expression was found in the AXD astrocytes or in non-neurological disease controls.
Figure 3.
Vanishing white matter disease (VWM) astrocytes express oligodendrocytic lineage-specific proteins. (A, B) Double stain for glial fibrillary acidic protein (GFAP) (A, patient VWM3) or vimentin (B, patient VWM99) and galactocerebroside (GalC) show dysmorphic astrocytes with homogeneous cytoplasmic GalC immunoreactivity extending far into the processes. (C) In astrocytes from VWM patients, GalC colocalizes with other astrocytic lineage specific-markers, including GFAPδ (patient VWM44). (D) GFAP-positive cells with astrocyte morphology also express olig2 with a cytoplasmic immunoreactivity pattern (patient VWM80). E: Primary culture of sorted glial progenitors shows a cell with both nuclear and cytoplasmically translocated olig2 and morphology and CD44-immunoreactivity, consistent with an astrocyte progenitor; 2 oligodendrocyte lineage-committed cells only express nuclear olig2 (patient VWM576). In all panels, the nuclei are stained with DAPI (blue). Original magnifications: A, E, 200×; B–D, 400×.
Some VWM astrocytes also co-expressed the oligodendrocyte transcription factor olig2. In these cells, olig2-immunoreactivity was in the astrocyte cytoplasm (Fig. 3D). In contrast, no olig2-positive astrocytes were found in sections from the neurological and non-neurological disease controls. This finding was also documented in glia progenitor cells sorted from the white matter of patient VWM576. When cultured in a medium specific for oligodendrocytes, cells expressed olig2 in the nuclei, consistent with their oligodendrocytic differentiation. However, cells were also found with both nuclear and cytoplasmic olig2 immunoreactivity and bipolar morphology, suggesting that there was a transition from oligodendrocyte-committed progenitor cells to astrocyte progenitor cells. Consistent with this, these cells expressed GFAP (data not shown) and the astrocyte progenitor marker CD44 (Fig. 3E).
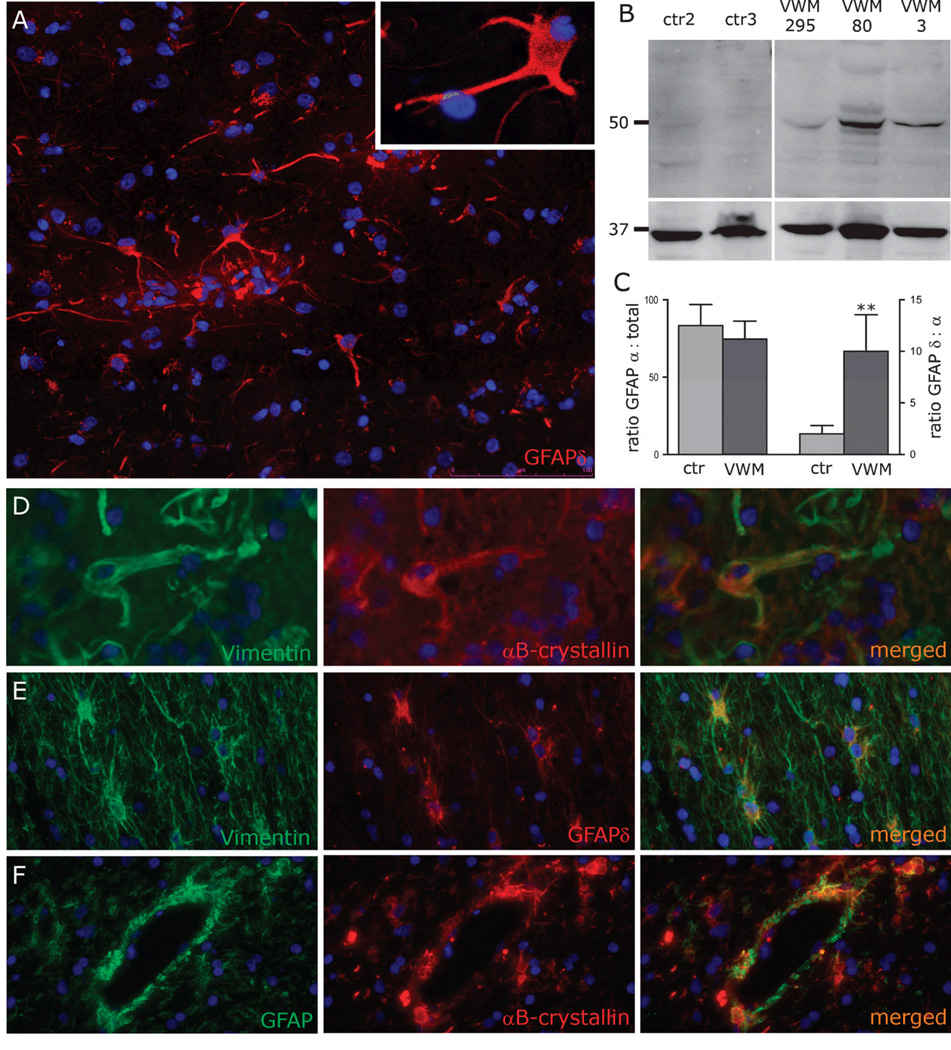
Dysmorphic astrocytes in VWM overexpress both GFAPδ and αB-crystallin
To gain insight into the morphology of VWM astrocytes, tissue sections were immunostained for GFAPδ, a protein isoform of GFAP. Astrocytes throughout VWM white matter were uniformly GFAPδ-positive, showing intense immunoreactivity in the cytoplasm that extended far into the processes (Fig. 4A). No GFAPδ-positive astrocytes were detected in the white matter from normal controls. Western blotting of cell extracts of white matter from 3 VWM patients and 2 age-matched controls confirmed the immunohistochemical data, i.e. GFAPδ was clearly detectable in the white matter of the VWM patients but not in the controls (Fig. 4B). To investigate GFAPδ upregulation at the mRNA level, q-PCR was performed on corresponding white matter areas from 4 VWM patients and 4 non-neurological disease controls. Although GFAPδ transcripts were weakly expressed in the control tissues (even in the absence of readily detectable protein), these GFAPδ transcripts were on average 5 times higher in VWM (Fig. 4C). Importantly, we found no significant difference between VWM and controls with respect to the message levels of the predominant isoform GFAPα (Fig. 4C). To assess the specificity of this finding, immunostaining was extended to the 4 neurological controls. White matter astrocytes in AXD were diffusely GFAPδ-positive (Fig. 4E). Small numbers of faintly GFAPδ-positive cells were detected within an MS plaque and in the X-ALD white matter, which were confined to areas of active demyelination and colocalized with reactive astrocytes (data not shown). No GFAPδ-positive astrocytes were found in the GLD case (data not shown).
Figure 4.
Vanishing white matter disease (VWM) astrocytes over-express glial fibrillary acidic protein δ (GFAPδ) and αB-crystallin. (A) Dysmorphic astrocytes in the white matter of a VWM patient (VWM3) are strongly GFAPδ-positive. Immunoreactivity extends far into the processes (inset). (B) Higher amounts of GFAPδ are detected by Western blot of white matter lysates from 3 VWM patients vs. age-matched non-neurological disease controls. The upper blot shows GFAPδ (49 kDa) and the lower blot, the loading control glyceraldehyde-3-phosphate dehydrogenase (GAPDH) (37 kDa). (C) q-PCR of the same patients and controls confirms that GFAPδ expression is significantly increased at the mRNA level (p = 0.005, error bars = SDs). The abundance of the mRNA transcripts of the predominant isoform GFAPα is comparable (p = 0.4). (D) Dysmorphic VWM astrocytes also over-express αB-crystallin, shown colocalizing with the astrocytic marker vimentin (patient VWM3). (E, F) Similar GFAPδ (E) and αB-crystallin (F) expression is found in the white matter of the Alexander disease (AXD) patient, with strong perivascular αB-crystallin-immunoreactivity consistent with Rosenthal fibers (F). Note the normal morphology of AXD astrocytes (E). In all pictures nuclei are stained with DAPI (blue). Original magnifications: A, E, F, 200×; (A, inset) 630×; D, 400×.
To explore the possible role of GFAPδ overexpression in the morphology of VWM astrocytes, brain sections were probed for the heat shock protein αB-crystallin. Astrocytes in the VWM patient samples showed robust immunoreactivity for αB-crystallin; its distribution overlapped with that of GFAP and vimentin (Fig. 4D). GFAPδ and αB-crystallin co-expressing astrocytes were detected also in AXD (Fig 4F). No αB-crystallin-positive astrocytes were found in the other neurological and non-neurological controls.
Oligodendrocytes in Vanishing White matter
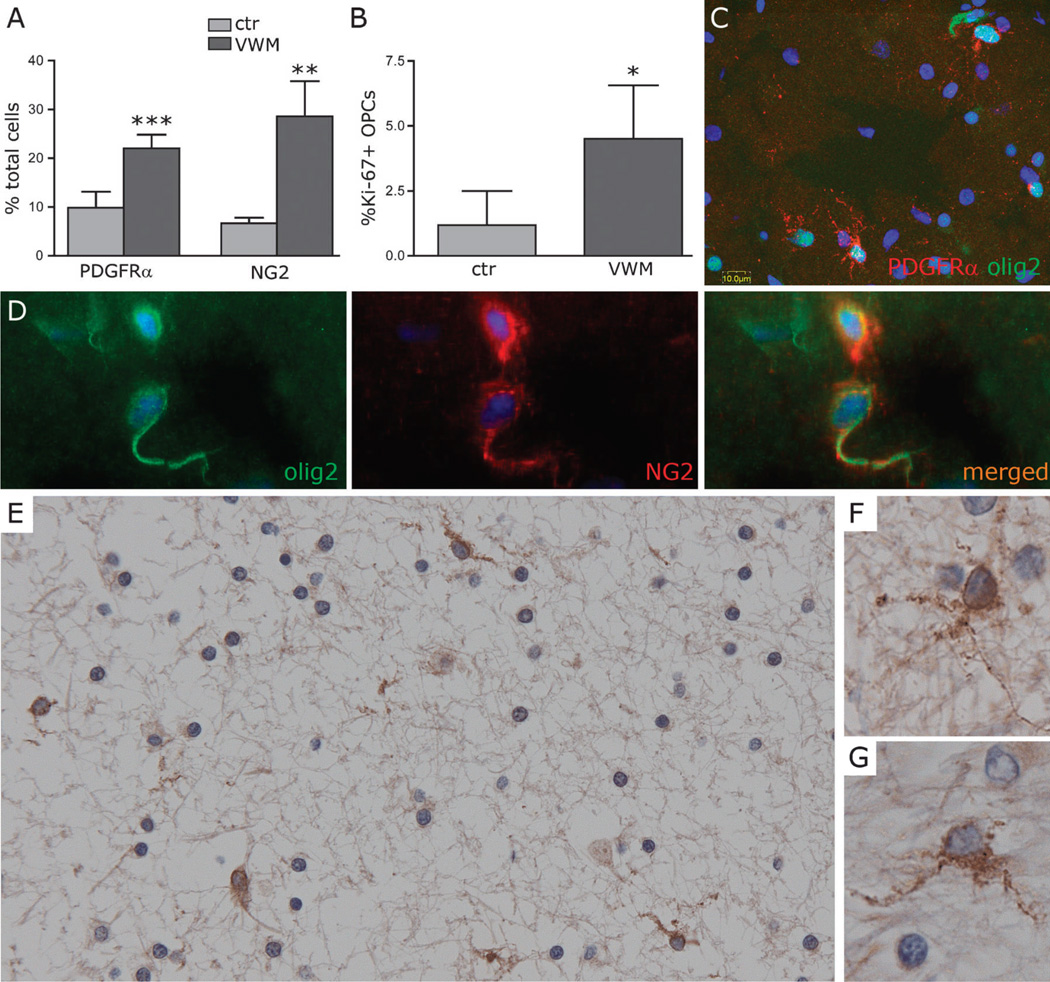
Increased density of oligodendrocyte progenitor cells in VWM
To investigate whether the maturation status of oligodendroglia is perturbed in VWM we identified cells in the oligodendrocyte lineage by their nuclear expression of olig2 and assessed the proportion of early oligodendrocyte-competent progenitor cells (OPCs) by their co-expression of the α-subunit of the receptor for platelet-derived growth factor (PDGFRα). PDGFRα-labeling index varied inversely with age in controls, being highest in the white matter from the 4.5-month-old infant. However, in VWM white matter the numbers of PDGFRα-positive cells were constant, irrespective of patient age and were significantly increased (2.2-fold) vs. controls (Fig. 5A). PDGFRα positivity identified cells with small cell bodies that give rise to multiple branched fine radial processes (Fig. 5C, E–G), consistent with the morphology of OPCs in the white matter. Double staining for PDGFRα and Ki-67 showed that these immature oligodendrocyte lineage cells were continuing to proliferate in the VWM patient white matter at a higher rate than in controls (Fig. 5B).
Figure 5.
Increased density of oligodendrocyte progenitor cells (OPCs) in the white matter of Vanishing white matter (VWM) patients. (A) There are higher numbers of OPCs in the white matter of VWM patients vs. controls as revealed by both platelet-derived growth factor α (PDGFRα) (p < 0.0001) and NG2 immunoreactivity (p = 0.001) (n = 5 patients, 3 controls; bars = SD). (B) Cell counts of Ki-67-positive OPCs show increased proliferation in VWM patients vs. non-neurological controls (p = 0.01) (n = 5 patients, 3 controls; bars = SD). (C–G) Both PDGFRα and NG2 antibodies identify cells with nuclear olig2-positivity (C, patient VWM295; D, patient VWM99) and little cytoplasm with multiple short branches (E–G, patient VWM367; PDGFRα). The olig2 antibody also labels cells with cytoplasmic immunoreactivity (uppermost cell in C; lower cell in D). These cells are presumably immature astrocytes. Nuclei in (C) and (D) are stained with DAPI (blue). Original magnifications: C, see bar; E, 200×; D, F, G, 400×.
Because PDGFRα alone did not stain a proportion of cells in the VWM white matter, tissue sections were additionally probed against another nominal OPC marker, chondroitin sulphate proteoglycan (NG2). There was also a significantly increased density (4.2-fold) of NG2-positive OPCs in the VWM vs. control white matter (Fig. 5A). The anti-NG2 antibody also labeled other cell types, i.e. pericytes lining blood vessels; therefore, NG2-positive OPCs were identified by both NG2 positivity and morphology. As for PDGFRα, NG2-positvie OPCs had small round cell bodies with thin processes (Fig. 5D), whereas pericytes along the blood vessels are elongated cells without processes.
DISCUSSION
Astrocytic immaturity: a clue for meager gliosis and failing scar formation in VWM
Reactive gliosis is limited in the white matter of VWM patients, which appears to be disproportionate to the often dramatic extent of local tissue loss. This relative lack of proportionate gliosis may contribute to the development of the cavitating lesions typical of the disease.
To investigate the mechanistic basis for this observation, we first evaluated the proliferation index of VWM astrocytes. Several lines of evidence suggest that mature astrocytes can re-enter the cell cycle. Thus, parenchymal astrocytes, like persistent glial progenitor cells, may be a source of new glia following CNS injury (15). We found that a significant proportion of astrocytes are proliferating in VWM, suggesting that the local generation of new astrocytes is not impaired in vivo. The same result was observed in vitro after mechanical stress. A previous study using cultured cells derived from VWM brain had reported that the generation of new astrocytes in vitro might be severely compromised (11). The discordance between these prior observations in culture and our in vitro results may derive from unique aspects of the response of VWM cells to the culture environment in basal conditions and after stress.
To evaluate whether the deficient reactive gliosis in VWM might be related to a failure in the maturation of newly generated astrocytes (16), we assessed the expression patterns of their intermediate filaments. Astrocytes express a predictable, sequential pattern of intermediate filaments during differentiation, which is recapitulated in response to injury. The human GFAP promoter drives GFAP expression at very early stages of astrocyte development. Immature astrocytes also express nestin and vimentin, whereas only vimentin is co-expressed with GFAP in mature cells (17, 18). As such, the concurrent induction of nestin and upregulation of GFAP and vimentin are hallmarks of reactive astrocytosis, both experimentally and in disease (19). In this, the induction of nestin expression has been regarded as indicative of astrocytic de-differentiation (20). We also assessed the expression of the Ca2+- and Zn2+-binding protein S100β. Expression of this protein in the adult brain defines a developmental stage, in which astrocytes lose their stem cell potential and reduce migratory behavior to acquire a terminally differentiated phenotype (21, 22). We found that VWM astrocytes, like reactive astrocytes, robustly express nestin, vimentin and GFAP but express little immuno-detectable S100β, all suggesting an immature phenotype. The relative ratios and net abundance of total GFAP and GFAPα mRNA transcripts were unchanged. Together, these data suggest that VWM astrocytes are blocked from developmental maturation, thereby impairing reactive gliosis. The failure of VWM astrocytes to upregulate the predominant GFAP isoform GFAPα may have significant functional consequences for their cytoskeletal architecture, ability to scar cavitated tissue, and interlaminar signaling.
VWM astrocytes express oligodendrocyte-specific markers
In their in vitro study of astrocytic dysfunction in cultures derived from a VWM patient, Dietrich et al reported that after exposure to bone morphogenic protein 4, which typically induces astrocytic phenotype from phenotypically unrestricted progenitor cells, 30–50% of the GFAP-positive cells showed an aberrant mixed-lineage phenotype by also expressing the oligodendrocyte-specific galactolipid GalC (11). The same observation was made after RNA-interference targeting of EIF2B5 in normal human glial progenitor cells (11). These data were interpreted as further confirmation of major astrocyte abnormalities in VWM. We demonstrate here that VWM astrocytes are also strongly GalC-positive in situ, showing a diffuse immunoreactivity in the cytoplasm of the cell body and processes. No vesicular distribution of GalC was observed in VWM, as would be expected for astrocytes that have ingested myelin fragments from surrounding degenerating oligodendrocytes. This was probably the case in the few GalC-positive astrocytes we detected in the demyelinating lesions of the MS and X-ALD patients. Conversely, the diffuse GalC distribution in VWM astrocytes is compatible with endogenous synthesis of GalC. Supporting this possibility is the previous finding of an increased specific activity of UDP-galactose:ceramide galactosyltransferase, the enzyme responsible for the final step in GalC synthesis, in the cerebellar white matter of a VWM patient despite a severe paucity of myelin (8). Similarly, the co-expression of GFAP and GalC by many astrocytes in GLD (which is caused by deficient activity of the GalC catabolic enzyme galactocerebroside-β-galactosidase) may also be consistent with our interpretation (A. Suzuki, unpublished observation).
GalC-expressing astrocytes are not unique to VWM. Glial cells expressing GFAP and a variety of oligodendrocytic markers, including GalC, have been described in normal and disease environments both in vitro and in vivo. Interestingly, many of the pathological conditions in which this phenomenon has been noted are disorders of myelin. For example, GFAP/GalC co-expressing cells were detected in glial cultures from shiverer mice, which have a partial deletion of the myelin basic protein gene (MBP) (23), as well as in the cat optic nerve after experimental demyelination (24). GalC-positive astrocytes were also reported in tissue sections from patients with the pigmentary type of orthochromatic leukodystrophy (25). GFAP-positive cells expressing other oligodendrocyte or myelin markers, including sulfatide/O4, myelin basic protein, and myelin/oligodendrocyte specific protein, have been detected in sections of normal adult rat brain (26), hypomyelinated brains of shiverer, quaking and phenylketonuria mice (23), and in the spinal cord of mice with viral-induced demyelination (27). These cells have been variably interpreted as either GFAP-expressing oligodendrocytes (23) or as myelin gene-expressing astrocytes (24, 26, 27). Based on their promiscuous antigenicity and broad distribution, cells with this phenotype have been postulated to represent glial or astrocyte progenitors (26), or to identify a subpopulation of aberrant mature glia that have initiated the concurrent synthesis of both astrocytic and oligodendrocytic determinants (24, 27).
The finding of defective astrocytic maturation in the white matter of VWM patients is further supported by the presence in vivo and in vitro of cells co-expressing nominally mature astrocytic markers with the transcription factor olig2, and with the latter’s translocation to the cytoplasm. Olig2 in glial cells inhibits astrocyte differentiation, thereby allowing the cells to maintain an undifferentiated state or to develop into myelinating oligodendrocytes (28). The loss of olig2 in rodent glial precursor cells is typically a necessary step preceding astrocytic differentiation, both developmentally (29, 30) and after injury (31, 32). This activity of olig2 is regulated by its movement between the nucleus and the cytoplasm. Cytoplasmic translocation functionally inactivates olig2 by sequestering it from its nuclear targets. Our finding of cytoplasmic translocation of olig2 suggests that in humans, as in rodents, the removal of olig2 from the nuclear compartment might also be a necessary condition for astrocytic differentiation after damage. Together, these observations suggest also a dual origin of new astrocytes in VWM, which may arise from both resident astrocytes resuming proliferation in response to injury, and from adult glial progenitor cells, which commit to astrocytic fate following the cytoplasmic translocation of their nuclear olig2.
Dysmorphic astrocytes in VWM display abnormal intermediate filaments properties
The abnormal morphology of VWM astrocytes has been invoked to explain the extensive white matter cavitation and limited gliosis of VWM tissue (11). In the affected white matter, astrocytes have coarse blunt processes instead of the fine arborizations seen in controls (4). We found that VWM white matter astrocytes over-express both GFAPδ and αB-crystallin, features that may explain their abnormal morphology and dysfunctional status.
GFAPδ results from alternative splicing of the GFAP gene, which replaces the 2 final exons of the predominant isoform GFAPα with an alternative terminal exon (33, 34). It is specifically expressed by a subpopulation of astrocytes located in the subpial zone along the brain surface and by the astrocytes lining the ependymal layer around the ventricles, including the neurogenic astrocytes in the subventricular zone of the developing and adult brain (17, 35, 36). In normal adult gray and white matter parenchyma, GFAPδ represents only a small fraction of total GFAP (35, 37). However, in reactive astrocytes both GFAPα and GFAPδ are upregulated, although the ratio of the 2 transcripts remains unchanged (35). It is only under these conditions that GFAPδ becomes detectable with immunohistochemical methods. This is consistent with the finding of only few weakly GFAPδ-positive cells in diseases with reactive gliosis, including Alzheimer disease (35), MS plaques (35, current study), and actively demyelinating areas in X-ALD (current study). In contrast, VWM white matter astrocytes manifest significant overexpression of both GFAPδ protein and mRNA, whereas the corresponding levels of GFAPα are not increased. Diffuse astrocytic GFAPδ-immunolabeling is also found in AXD (37, current study), a leukoencephalopathy caused by GFAP gene mutations (38), in which the inability to form proper astrocytic GFAP networks coexists with incomplete maturation of astrocytes and insufficient myelin formation (39). In vitro assays show that the overexpression of GFAPδ, as well as the expression of the AXD-causing GFAP mutation R416W, both result in the accumulation of assembly incompetent intermediate filament proteins that collapse the endogenous GFAP network and increase the levels of the protein chaperone αB-crystallin (35, 37). VWM astrocytes, like AXD astrocytes (39, current study), are strongly αB-crystallin-immunopositive, suggesting that the disturbed GFAPδ:GFAPα ratio may perturb filament-filament interactions in VWM astrocytes as well, thereby contributing to their aberrant morphology. Moreover, as postulated for AXD (39), the resulting cytoskeletal defects could lead to astrocytic functional impairment, thus leading to widespread effects on other CNS cell types. Because the presence of normal astrocytes is required for endogenous glia progenitor cells to mature into oligodendrocytes and initiate myelination (40), astrocytic dysfunction in VWM might impede myelin formation, maintenance, or both.
Increased density of OPCs: a hint to hypomyelination in VWM
VWM pathology is characterized by a substantial increase in the numbers of oligodendrocytes, both around cavitating lesions and in less affected white matter (4, 8, 9, 41). This oligodendrocytosis is associated with paucity of myelin. To investigate whether this may reflect an oligodendrocytic maturational arrest leading to an increase in immature pre-myelinating cells, we assessed the maturation status of these cells by means of PDGFRα- and NG2-expression. PDGFRα is a receptor for PDGF, a potent mitogen, survival, and differentiation factor for oligodendrocytes (42), currently considered to be the most reliable OPC marker in the adult brain in vivo (42, 43). NG2 is a chondroitin sulphate proteoglycan on the membrane of OPCs; its expression begins slightly later than that of PDGFRα (44). Both markers colocalize in OPCs in vitro (44–46) and in vivo (47, 48). We found that VWM disease white matter contains significantly increased numbers of OPCs, disproportionate to the numbers of mature myelinating oligodendrocytes.
Oligodendrocytes are the cell population in the CNS with the most significant turnover and, as such, all stages of precursor cells exist through adult life (44, 49). In the healthy rodent, the great majority of adult-born oligodendrocytes differentiate from local OPCs (50), consistent with the observation that adult OPCs divide but their numbers do not increase (45). In response to injury, OPCs form a reactive glial population that undergoes hypertrophy and mitosis (51, 52). Adult OPCs can efficiently generate new mature oligodendrocytes in early MS lesions (44, 53), as well as following acute experimental demyelination (54, 55). However, OPC proliferation also occurs chronically in white matter of mice with genetic myelination defects as shiverer (56) and jimpy (57), despite elevated cell density. This has been shown to be closely associated with lack of intact myelin (51). A similar mechanism may operate in VWM, in which both lack of myelin and myelin vacuolation with focal areas of uncompacted myelin close to the axonal membrane are observed (8).
The increase in OPC numbers detected in VWM white matter by NG2 labeling was higher than by PDGFRα labeling. PDGFRα-positive cells exhibit numbers consistent with NG2-positive cells at early developmental stages (47), but are considerably less abundant than the NG2-positive population at older ages (47, 48). In this respect our results are in agreement with earlier reports showing that the distribution of PDGFRα-positive cells within the adult human normal and MS white matter is similar to that of NG2-positive cells, but in numbers that are at least 50% lower (48).
As the ratio of adult OPCs to oligodendrocytes in the normal white matter is approximately 1:4 (52) and our finding of a 2- to over 4-fold increase is consistent with estimates of the number of new oligodendrocytes that are required for repair (51). However, despite increased OPC numbers, no remyelination is observed in VWM. We could not directly investigate whether proliferating OPCs can differentiate into myelin-forming cells in VWM autopsy tissue. Downregulation of NG2 and PDGFRα antigens prior to terminal differentiation of OPCs into mature oligodendrocytes (43, 44, 46) precludes such verification by double immunohistochemical labeling. However, the finding of significantly reduced amounts of myelin structural proteins and lipids previously detected by immunohistochemistry and direct quantification (2, 8, 41, 58) suggests that only few OPCs can differentiate into myelinating oligodendrocytes in the affected white matter of VWM patients.
Conclusion
Our data suggest that a combination of astrocytic immaturity and cytoskeletal dysfunction with increased numbers of maturation-deficient glial progenitor cells may explain the striking concurrence of compensatory oligodendrocytosis, myelin paucity and diminished reactive gliosis that characterize the neuropathological findings in VWM.
ACKNOWLEDGMENTS
Financial support was provided by the Nuts-Ohra Foundation (grant SNO-T-08-32), the Dutch Organization for Scientific Research (ZonMw, TOP grants 903-42-097 and 9120.6002), the “Princes Beatrix Fonds” (grant MAR01-0201), Dr. W.M. Phelps Foundation (grants 03.030 and 2008.029), Stichting Onderzoek Stofwisselingsziekten, the Optimix Foundation for Scientific Research, and in Rochester by grants from the Adelson Medical Research Foundation, National Multiple Sclerosis Society, New York Stem Cell Program, and NINDS R01NS 39559.
We are grateful to all patients who participated in this study and to their families. We thank the Brain and Tissue Bank for Developmental Disorders at the University of Maryland, Baltimore, MD, for providing some of the patient tissue used in this study. We acknowledge also Dr. E. Aronica (University of Amsterdam Academic Medical Center, Amsterdam, the Netherlands) and the Netherlands Brain Bank (Amsterdam) for providing us with brain tissue of the X-ALD and MS patients, respectively. J. Cornelis (Dep. of Molecular and Cellular Neurobiology, Center for Neurogenomics and Cognitive Research FALV, VU University, Amsterdam, the Netherlands), E. Kooi (Dep. of Pathology, VU University Medical Center, Amsterdam, the Netherlands) and G. Lu (Dep. of Neurology, Center for Translational Neuromedicine, University of Rochester Medical Center, Rochester, NY) are acknowledged for their technical assistance with the use of the Cellomics, immunohistochemistry and RNA isolation, respectively.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.van der Knaap MS, Barth PG, Gabreels FJM, et al. A new leukoencephalopathy with vanishing white matter. Neurology. 1997;48:845–855. doi: 10.1212/wnl.48.4.845. [DOI] [PubMed] [Google Scholar]
- 2.Schiffmann R, Moller JR, Trapp BD, et al. Childhood ataxia with diffuse central nervous system hypomyelination. Ann Neurol. 1994;35:331–340. doi: 10.1002/ana.410350314. [DOI] [PubMed] [Google Scholar]
- 3.Brück W, Herms J, Brockmann K, et al. Myelinopathia centralis diffusa (vanishing white matter disease): evidence of apoptotic oligodendrocyte degeneration in early lesion development. Ann Neurol. 2001;50:532–536. doi: 10.1002/ana.1227. [DOI] [PubMed] [Google Scholar]
- 4.van der Knaap MS, Pronk JC, Scheper GC. Vanishing white matter disease. Lancet Neurol. 2006;5:413–423. doi: 10.1016/S1474-4422(06)70440-9. [DOI] [PubMed] [Google Scholar]
- 5.Leegwater PA, Vermeulen G, Könst AA, et al. Subunits of the translation initiation factor eIF2B are mutant in leukoencephalopathy with vanishing white matter. Nat Genet. 2001;29:383–388. doi: 10.1038/ng764. [DOI] [PubMed] [Google Scholar]
- 6.van der Knaap MS, Leegwater PA, Könst AA, et al. Mutations in each of the five subunits of translation initiation factor eIF2B can cause leukoencephalopathy with vanishing white matter. Ann Neurol. 2002;51:264–270. doi: 10.1002/ana.10112. [DOI] [PubMed] [Google Scholar]
- 7.Bugiani M, Boor I, Powers JM, et al. Leukoencephalopathy with vanishing white matter: a review. J Neuropathol Exp Neurol. 2010;69:987–996. doi: 10.1097/NEN.0b013e3181f2eafa. [DOI] [PubMed] [Google Scholar]
- 8.Rodriguez D, Gelot A, della Gaspera B, et al. Increased density of oligodendrocytes in childhood ataxia with diffuse central hypomyelination (CACH) syndrome: neuropathological and biochemical study of two cases. Acta Neuropathol. 1999;97:469–480. doi: 10.1007/s004010051016. [DOI] [PubMed] [Google Scholar]
- 9.van Haren KP, van der Voorn JP, van der Knaap MS, et al. The life and death of oligodendrocytes in vanishing white matter disease. J Neuropathol Exp Neurol. 2004;63:618–630. doi: 10.1093/jnen/63.6.618. [DOI] [PubMed] [Google Scholar]
- 10.van der Voorn JP, van Kollenburg B, Bertrand G, et al. The unfolded protein response in vanishing white matter. J Neuropathol Exp Neurol. 2005;64:770–775. doi: 10.1097/01.jnen.0000178446.41595.3a. [DOI] [PubMed] [Google Scholar]
- 11.Dietrich J, Lacagnina M, Gass D, et al. EIF2B5 mutations compromise GFAP+ astrocyte generation in vanishing white matter leukodystrophy. Nature Medicine. 2005;11:277–283. doi: 10.1038/nm1195. [DOI] [PubMed] [Google Scholar]
- 12.van Kollenburg B, van Dijk J, Garbern J, et al. Glia-specific activation of all pathways of the unfolded protein response in vanishing white matter disease. J Neuropathol Exp Neurol. 2006;65:707–715. doi: 10.1097/01.jnen.0000228201.27539.50. [DOI] [PubMed] [Google Scholar]
- 13.Roy NS, Wang S, Harrison-Restelli C, et al. Identification, isolation, and promoter-defined separation of mitotic oligodendrocyte progenitor cells from the adult human subcortical white matter. J Neurosci. 1999 Nov 15;19(22):9986–9995. doi: 10.1523/JNEUROSCI.19-22-09986.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Powers JM. The leukodystrophies: overview and classification. In: Lazzarini RA, editor. Myelin Disorders and Biology. Vol. 2. San Diego, CA: Elsevier Academic Press; 2004. pp. 663–690. [Google Scholar]
- 15.Carmen J, Magnus T, Cassiani-Ingoni R, et al. Revisiting the astrocyte-oligodendrocyte relationship in the adult CNS. Progress in Neurobiology. 2007;82:151–162. doi: 10.1016/j.pneurobio.2007.03.001. [DOI] [PubMed] [Google Scholar]
- 16.Buffo A, Rite A, Tripathi P, et al. Origin and progeny of reactive gliosis: a source of multipotent cells in the injured brain. Proc Natl Acad Sci USA. 2008;105:3581–3586. doi: 10.1073/pnas.0709002105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Middeldorp J, Boer K, Sluijs JA, et al. GFAPδ in radial glia and subventricular zone progenitors in the developing human cortex. Development. 2010;137:313–321. doi: 10.1242/dev.041632. [DOI] [PubMed] [Google Scholar]
- 18.Eliasson C, Sahlgren C, Berthold CH, et al. Intermediate filament protein partnership in astrocytes. J Biol Chem. 1999;274:23996–24006. doi: 10.1074/jbc.274.34.23996. [DOI] [PubMed] [Google Scholar]
- 19.Pekny M, Pekna M. Astrocyte intermediate filaments in CNS pathologies and regeneration. J Pathol. 2004;204:428–437. doi: 10.1002/path.1645. [DOI] [PubMed] [Google Scholar]
- 20.Shibuya S, Miyamoto O, Auer RN, et al. Embryonic intermediate filament, nestin, expression following traumatic spinal cord injury in adult rats. Neuroscience. 2002;4:905–916. doi: 10.1016/s0306-4522(02)00323-8. [DOI] [PubMed] [Google Scholar]
- 21.Raponi E, Agnes F, Delphin C, et al. S100B expression defines a state in which GFAP-expressing cells lose their neural stem potential and acquire a more mature developmental stage. Glia. 2007;55:165–177. doi: 10.1002/glia.20445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Donato R, Sorci G, Riuzzi F, et al. S100B’s double life: intracellular regulator and extracellular signal. Biochim Biophys Acta. 2009;1793:1008–1022. doi: 10.1016/j.bbamcr.2008.11.009. [DOI] [PubMed] [Google Scholar]
- 23.Dyer CA, Kendler A, Jean-Guillaume D, et al. GFAP-positive and myelin marker-positive glia in normal and pathological environments. J Neurosci Res. 2000;60:412–426. doi: 10.1002/(SICI)1097-4547(20000501)60:3<412::AID-JNR16>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 24.Carroll WM, Jennings AR, Mastaglia FL. Reactive glial cells in CNS demyelination contain both GC and GFAP. Brain Res. 1987;411:364–369. doi: 10.1016/0006-8993(87)91088-2. [DOI] [PubMed] [Google Scholar]
- 25.Möller JC, Sünkeler IH, Oertel WH, Mennel HD. Die pigmentierte form der orthochromatischen leukodystrophie. Nervenarz. 2003;74:1127–1133. doi: 10.1007/s00115-003-1585-3. [DOI] [PubMed] [Google Scholar]
- 26.Pernber Z, Molander-Melin M, Berthold C-H, et al. Expression of the myelin and oligodendrocyte progenitor marker sulfatide in neurons and astrocytes of adult rat brain. J Neurosci Res. 2002;69:86–93. doi: 10.1002/jnr.10264. [DOI] [PubMed] [Google Scholar]
- 27.Godfraind C, Friedrich VL, Holmes KV, et al. In vivo analysis of glial cell phenotypes during a viral demyelinating disease in mice. J Cell Biol. 1989;109:2405–2416. doi: 10.1083/jcb.109.5.2405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhou Q, Anderson DJ. The bHLH transcription factors OLIG2 and OLIG1 couple neuronal and glial subtype specification. Cell. 2002;109:61–73. doi: 10.1016/s0092-8674(02)00677-3. [DOI] [PubMed] [Google Scholar]
- 29.Marshall CA, Novitch BG, Goldman JE. Olig2 directs astrocyte and oligodendrocyte formation in postnatal subventricular zone cells. J Neurosci. 2005;25:7289–7298. doi: 10.1523/JNEUROSCI.1924-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cai J, Chen Y, Cai W-H, Hurlock EC, et al. A crucial role for Olig2 in white matter astrocyte development. Development. 2007;134:1887–1889. doi: 10.1242/dev.02847. [DOI] [PubMed] [Google Scholar]
- 31.Cassiani-Ingoni R, Coksaygan T, Xue H, et al. Cytoplasmic translocation of Olig2 in adult glial progenitors marks the generation of reactive astrocytes following autoimmune inflammation. Exp Neurol. 2006;201:349–358. doi: 10.1016/j.expneurol.2006.04.030. [DOI] [PubMed] [Google Scholar]
- 32.Magnus T, Coksaygan T, Korn T, et al. Evidence that nucleocytoplasmic Olig2 translocation mediates brain-injury-induced differentiation of glial precursors to astrocytes. J Neurosci Res. 2007;85:2126–2137. doi: 10.1002/jnr.21368. [DOI] [PubMed] [Google Scholar]
- 33.Condorelli DF, Nicoletti VG, Barresi V, et al. Structural features of the rat GFAP gene and identification of a novel alternative transcript. J Neurosci Res. 1999;56:219–228. doi: 10.1002/(SICI)1097-4547(19990501)56:3<219::AID-JNR1>3.0.CO;2-2. [DOI] [PubMed] [Google Scholar]
- 34.Nielsen AL, Holm IE, Johansen M, et al. A new splice variant of glial fibrillary acidic protein, GFAP epsilon, interacts with the presenilin proteins. J Biol Chem. 2002;277:29983–29991. doi: 10.1074/jbc.M112121200. [DOI] [PubMed] [Google Scholar]
- 35.Roelofs RF, Fischer DF, Houtman SH, et al. Adult human subventricular, subgranular, and subpial zones contain astrocytes with a specialized intermediate filament cytoskeleton. Glia. 2005;52:289–300. doi: 10.1002/glia.20243. [DOI] [PubMed] [Google Scholar]
- 36.van den Berge SA, Middeldorp J, Zhang CE, et al. Longterm quiescent cells in the aged human subventricular neurogenic system specifically express GFAP-δ. Aging Cell. 2010;9:313–326. doi: 10.1111/j.1474-9726.2010.00556.x. [DOI] [PubMed] [Google Scholar]
- 37.Perng M-D, Wen S-F, Gibbon T, et al. Glial fibrillary acidic protein filaments can tolerate incorporation of assembly-compromised GFAP-δ, but with consequences for filament organization and αB-crystallin association. Mol Biol Cell. 2008;19:4521–4533. doi: 10.1091/mbc.E08-03-0284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Brenner M, Johnson AB, Boespflug-Tanguy O, et al. Mutations in GFAP, encoding glial fibrillary acidic protein, are associated with Alexander disease. Nat Genet. 2001;27:117–120. doi: 10.1038/83679. [DOI] [PubMed] [Google Scholar]
- 39.Mignot C, Boespflug-Tanguy O, Gelot A, et al. Alexander disease: putative mechanisms of an astrocytic encephalopathy. Cell Mol Life Sci. 2004;61:369–385. doi: 10.1007/s00018-003-3143-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Talbott JF, Loy DN, Liu Y, et al. Endogenous Nkx2.2+/Olig2+ oligodendrocyte precursor cells fail to remyelinate the demyelinated adult rat spinal cord in the absence of astrocytes. Exp Neurol. 2005;192:11–24. doi: 10.1016/j.expneurol.2004.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Francalanci P, Eymard-Pierre E, Dionisi-Vici C, et al. Fatal infantile leukodystrophy: a severe variant of CACH/VWM syndrome, allelic to chromosome 3q27. Neurology. 2001;15:265–270. doi: 10.1212/wnl.57.2.265. [DOI] [PubMed] [Google Scholar]
- 42.Grinspan J. Cells and signaling in oligodendrocyte development. J Neuropathol Exp Neurol. 2002;61:297–306. doi: 10.1093/jnen/61.4.297. [DOI] [PubMed] [Google Scholar]
- 43.Zhang S-C, Ge B, Duncan ID. Tracing human oligodendroglial development in vitro. J Neurosci Res. 2000;59:421–429. doi: 10.1002/(SICI)1097-4547(20000201)59:3<421::AID-JNR17>3.0.CO;2-C. [DOI] [PubMed] [Google Scholar]
- 44.Nishiyama A, Komitova M, Suzuki R, et al. Polydendrocytes (NG2 cells): multifunctional cells with lineage plasticity. Nat Rev Neurosci. 2009;10:9–22. doi: 10.1038/nrn2495. [DOI] [PubMed] [Google Scholar]
- 45.Rivers LE, Young KM, Rizzi M, et al. PDGFRA/NG2 glia generate myelinating oligodendrocytes and piriform projection neurons. Nature Neurosci. 2008;11:1392–1401. doi: 10.1038/nn.2220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zhu X, Bergles DE, Nishiyma A. NG2 cells generate both oligodendrocytes and gray matter astrocytes. Development. 2008;135:145–157. doi: 10.1242/dev.004895. [DOI] [PubMed] [Google Scholar]
- 47.He Y, Cai W, Wang L, et al. A developmental study on the expression of PDGFαR immunoreactive cells in the brain of postnatal rats. Neurosci Res. 2009;65:272–279. doi: 10.1016/j.neures.2009.07.011. [DOI] [PubMed] [Google Scholar]
- 48.Wilson HC, Scolding NJ, Raine CS. Co-expression of PDGF alpha receptor and NG2 by oligodendrocyte precursors in human CNS and multiple sclerosis lesions. J Immunol. 2006;176:162–173. doi: 10.1016/j.jneuroim.2006.04.014. [DOI] [PubMed] [Google Scholar]
- 49.Dawson MR, Polito A, Levine JM, et al. NG2-expressing glial progenitor cells: an abundant and widespread population of cycling cells in the adult rat CNS. Mol Cell Neurosci. 2003;24:476–488. doi: 10.1016/s1044-7431(03)00210-0. [DOI] [PubMed] [Google Scholar]
- 50.Dimou L, Simon C, Kirchhoff F, et al. Progeny of Olig2-expressing progenitors in the gray and white matter of the adult mouse cerebral cortex. J Neurosci. 2008;28:10434–10442. doi: 10.1523/JNEUROSCI.2831-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.di Bello CI, Dawson MR, Levine JM, et al. Generation of oligodendroglial progenitors in acute inflammatory demyelinating lesions of the rat brain stem is associated with demyelination rather than inflammation. J Neurocytol. 1999;28:365–381. doi: 10.1023/a:1007069815302. [DOI] [PubMed] [Google Scholar]
- 52.Levine JM, Reynolds R, Fawcett JW. The oligodendrocyte precursor cell in health and disease. Trends Neurosci. 2001;24:39–47. doi: 10.1016/s0166-2236(00)01691-x. [DOI] [PubMed] [Google Scholar]
- 53.Raine CS, Wu E. Multiple sclerosis: remyelination in acute lesions. J Neuropathol Exp Neurol. 1993;52:199–204. [PubMed] [Google Scholar]
- 54.Gensert JM, Goldman JE. Endogenous progenitors remyelinate demyelinated axons in the adult CNS. Neuron. 1997;19:197–203. doi: 10.1016/s0896-6273(00)80359-1. [DOI] [PubMed] [Google Scholar]
- 55.Watanabe M, Toyama Y, Nishiyama A. Differentiation of proliferated NG2-positive glial progenitor cells in a remyelinating lesion. J Neurosci Res. 2002;69:826–836. doi: 10.1002/jnr.10338. [DOI] [PubMed] [Google Scholar]
- 56.Bu J, Banki A, Wu Q, et al. Increased NG2(+) glial cell proliferation and oligodendrocyte generation in the hypomyelinating mutant shiverer. Glia. 2004;48:51–63. doi: 10.1002/glia.20055. [DOI] [PubMed] [Google Scholar]
- 57.Wu Q, Miller RH, Ransohoff RM, et al. Elevated levels of the chemokine GRO-1 correlate with elevated oligodendrocyte progenitor proliferation in the Jimpy mutant. J Neurosci. 2000;20:2609–2617. doi: 10.1523/JNEUROSCI.20-07-02609.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Tedeschi G, Shiffmann R, Barton NW, et al. Proton magnetic resonance spectroscopic imaging in childhood ataxia with diffuse central nervous system hypomyelination. Neurology. 1995;45:1526–1532. doi: 10.1212/wnl.45.8.1526. [DOI] [PubMed] [Google Scholar]