Abstract
Background: Growth failure remains a persistent challenge in many countries, and understanding child growth patterns is critical to the development of appropriate interventions and their evaluation. The interpretation of changes in mean height-for-age z scores (HAZs) over time to define catch-up growth has been a subject of debate. Most studies of child growth have been cross-sectional or have focused on children through age 5 y.
Objective: The aim was to characterize patterns of linear growth among individuals followed from birth into adulthood.
Design: We compared HAZs and difference in height (cm) from the WHO reference median at birth, 12 mo, 24 mo, mid-childhood, and adulthood for 5287 individuals from birth cohorts in Brazil, Guatemala, India, the Philippines, and South Africa.
Results: Mean HAZs were <0 at birth in the 3 cohorts with data and ranged from −0.6 (Brazil) to −2.9 (Guatemala) at age 24 mo. Between 24 mo and mid-childhood, HAZ values increased by 0.3–0.5 in South Africa, Guatemala, and the Philippines and were unchanged in Brazil and India. Between mid-childhood and adulthood, mean HAZs increased in all cohorts but remained <0 in adulthood [mean range: −0.3 (Brazil) to −1.8 (Guatemala and Philippines)]. However, from 24 mo to adulthood, height differences from the reference median became greater.
Conclusions: From age 2 y to adulthood, mean HAZs increased, even though height deficits relative to the reference median also increased. These 2 metrics may result in different interpretations of the potential for and the impact of catch-up growth in height.
INTRODUCTION
Globally, the prevalence of growth stunting in children <5 y of age decreased from 40% in 1990 to 26% in 2011 (1). Much of this improvement can be attributed to major decreases in the prevalence of stunting in several countries in Asia, whereas stunting prevalence has stagnated in much of Africa over the past 2 decades (2). Growth failure still remains a persistent challenge in many low- and middle-income countries, and understanding child growth patterns is critical to the development of appropriate interventions and their evaluation.
However, research on childhood growth patterns has several limitations. Much of the data on child growth come from cross-sectional studies rather than longitudinal cohorts, limiting the inferences that can be made about how children grow over time. In addition, studies tend to focus on children up to 5 y of age, and less is known about growth patterns after this age. Furthermore, the use and interpretation of indicators such as height-for-age z scores (HAZs) for characterizing growth patterns has been the subject of debate (3).
We aimed to address these limitations in the child growth literature by characterizing patterns of linear growth from birth to adulthood among cohorts in 5 middle-income countries and evaluating these data to further understanding of the interpretation of child growth indicators used to define catch-up growth.
SUBJECTS AND METHODS
We used data from the Consortium of Health-orientated Research in Transitioning Societies (COHORTS), which includes birth cohorts in 5 middle-income countries: the 1982 Pelotas Birth Cohort (Brazil), the Institute of Nutrition of Central America and Panama Nutrition Trial Cohort (Guatemala), the New Delhi Birth Cohort (India), the Cebu Longitudinal Health and Nutrition Survey (the Philippines), and the Birth to Twenty Cohort (South Africa) (4). Each study was reviewed and approved by an appropriate ethics committee or institutional review board, and informed consent was provided by the participants or their caretakers.
The present analysis used length and height data collected within each cohort with the use of study-specific, but comparable, methodologies. Some aspects of the length/height data at these time points were previously published (5, 6). With the exception of the Guatemala cohort, in all studies supine length was measured until age 24 mo, and standing height was measured thereafter. In Guatemala, supine length was measured through the age of 7 y, and for the purposes of comparability, supine length was converted to standing height by subtracting 1.0 cm from lengths obtained at ages 24 mo and older (7). Length (in cm) measurements were available at birth in India, within 6 d of birth in the Philippines, and within 15 d of birth in Guatemala. Length at birth was not measured in South Africa and Brazil.
The studies varied in the timing and frequency of length/height measurements (details published previously) (5). For the present analysis, data from common child ages were used, specifically as follows: birth (India, Philippines, Guatemala), 12 mo (all 5 cohorts), 24 mo (all 5 cohorts), mid-childhood (48 mo in Brazil, Guatemala, India, and South Africa and 102 mo in the Philippines), and adulthood (all 5 cohorts). Mean age at the time of the adult height measurement was 23.1 y in Brazil, 31.3 y in Guatemala, 29.4 y in India, 21.2 y in the Philippines, and 18.2 y in South Africa.
Length and height measurements were converted to z scores (HAZs) by using either the 2006 growth standards (0–59 mo) (8), derived from the longitudinal WHO Multicentre Growth Study, a population of exclusively or predominantly breastfed children from 6 countries, or the 2007 WHO reference curves (5–19 y) (9), which are based on national cross-sectional anthropometric data from the US National Center for Health Statistics for 1977. By using these growth standards, for each time point we also computed the difference between the individuals’ length/height (cm) and the age- and sex-specific value of the 50th percentile of the reference population (referred to hereafter as the height difference).
We restricted the analysis to participants who had either a weight or a length measurement at birth, a length measurement at 12 mo, and a height measurement at 24 mo, mid-childhood, and adulthood (n = 5696). We eliminated from the analysis individuals with implausible HAZ values, defined as |HAZ| >5 at any one round (n = 257) or an absolute value of change in HAZ between rounds >4 (n = 152). After these restrictions, the final analytic sample was n = 5287.
We computed means for the height difference and HAZ and the prevalence of stunting (HAZ <−2.0) at each time point, as well as changes in these measures between time points. We determined the incidence of stunting (the proportion of children who were not stunted at an earlier time point but who were stunted at a later time point), as well as the incidence of recovery (the proportion of children who were stunted at an earlier time point but who were not stunted at a later time point). We used the Intercooled STATA 10.0 (StataCorp) statistical program for all data analyses.
RESULTS
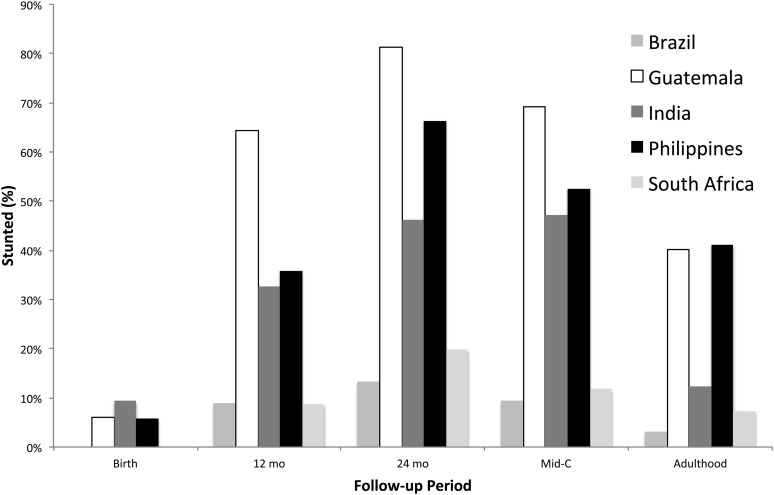
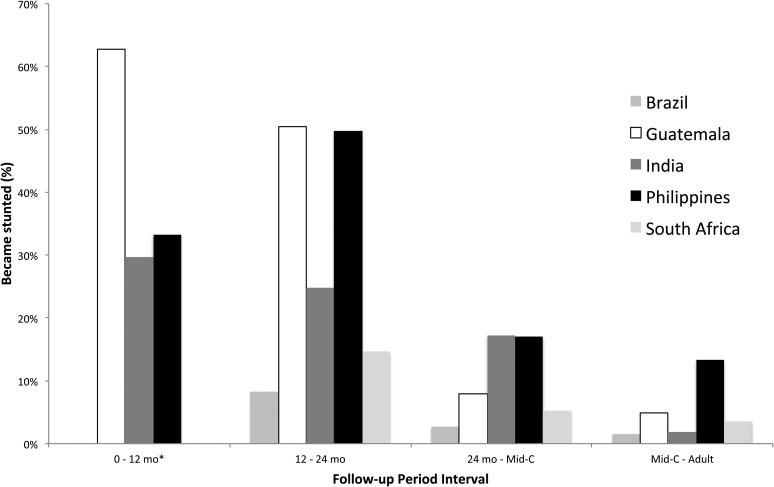
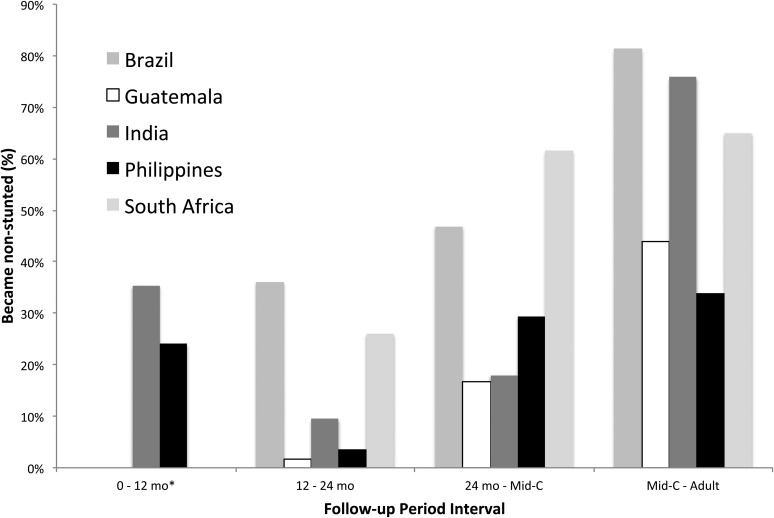
For the 3 cohorts with data, the prevalence of stunting at birth ranged from 5.8% (Philippines) to 9.4% (India) (Figure 1). The prevalence of stunting increased through 24 mo [range of stunting prevalence at 24 mo: 13.2% (Brazil) to 81.2% (Guatemala)]. The prevalence of stunting decreased from 24 mo to adulthood [range at adulthood: 3.2% (Brazil) to 41.1% (Philippines)]. The majority of incident stunting had occurred by age 24 mo (Figure 2); recovery from stunting was highest after age 24 mo (Figure 3).
FIGURE 1.
Prevalence of stunting among children in 5 birth cohorts in middle-income countries: Consortium of Health-orientated Research in Transitioning Societies. Stunting is defined as height-for-age z score <−2.0. Mid-C, mid-childhood.
FIGURE 2.
Incidence of stunting among children in 5 birth cohorts in middle-income countries: Consortium of Health-orientated Research in Transitioning Societies. The incidence of stunting is the proportion of children who were not stunted at an earlier survey round but who were stunted at a later survey round (stunting is defined as height-for-age z score <−2.0). *Height data at birth were not available for Brazil and South Africa. Mid-C, mid-childhood.
FIGURE 3.
Incidence of recovery among children in 5 birth cohorts in middle-income countries: Consortium of Health-orientated Research in Transitioning Societies. The incidence of recovery is the proportion of children who were stunted at an earlier survey round but who were not stunted at a later survey round (stunting is defined as height-for-age z score <−2.0). *Height data at birth were not available for Brazil and South Africa; the incidence of recovery was 0.0% in Guatemala. Mid-C, mid-childhood.
For the 3 cohorts with data, mean HAZs at birth were all <0, and in all 5 cohorts HAZs decreased through age 24 mo (Table 1). Mean HAZ values at 24 mo ranged from −0.6 (Brazil) to −2.9 (Guatemala). Between 24 mo and mid-childhood, mean HAZs increased in South Africa, Guatemala, and the Philippines and were virtually unchanged in Brazil and India. Between mid-childhood and adulthood, mean HAZs increased [range: 0.2 (Philippines) to 0.8 (India)] but remained <0 [adult mean HAZ range: −0.3 (Brazil) to −1.8 (Guatemala and the Philippines)].
TABLE 1.
Measurements of linear growth at selected ages in 5 cohorts from middle-income countries: COHORTS1
| n | Height | Height-for-age z score | Height deficit from reference2 | |
| cm | cm | |||
| Brazil | ||||
| Birth | — | — | — | — |
| 12 mo | 966 | 73.0 ± 3.3 | −0.4 ± 1.2 | −0.3 ± 2.9 |
| 24 mo | 966 | 84.6 ± 3.8 | −0.6 ± 1.2 | −1.5 ± 3.7 |
| Mid-childhood | 966 | 100.0 ± 4.7 | −0.6 ± 1.1 | −2.2 ± 4.5 |
| Adulthood | 966 | 167.5 ± 8.6 | −0.3 ± 0.9 | −2.4 ± 6.1 |
| Guatemala | ||||
| Birth | 197 | 49.3 ± 2.2 | −0.1 ± 1.1 | −0.2 ± 2.1 |
| 12 mo | 266 | 69.1 ± 2.5 | −2.3 ± 0.9 | −5.6 ± 2.4 |
| 24 mo | 266 | 78.1 ± 3.0 | −2.9 ± 0.9 | −8.9 ± 2.9 |
| Mid-childhood | 266 | 93.4 ± 3.7 | −2.4 ± 0.9 | −9.6 ± 3.6 |
| Adulthood | 266 | 157.6 ± 8.2 | −1.8 ± 0.8 | −12.3 ± 5.5 |
| India | ||||
| Birth | 1059 | 48.4 ± 2.1 | −0.6 ± 1.1 | −1.2 ± 2.0 |
| 12 mo | 1070 | 71.3 ± 2.8 | −1.5 ± 1.1 | −3.7 ± 2.7 |
| 24 mo | 1070 | 80.6 ± 3.5 | −1.9 ± 1.1 | −6.6 ± 3.4 |
| Mid-childhood | 1070 | 94.9 ± 4.1 | −1.9 ± 1.0 | −8.1 ± 4.1 |
| Adulthood | 1070 | 163.5 ± 9.2 | −1.1 ± 0.9 | −7.4 ± 5.9 |
| Philippines | ||||
| Birth | 1806 | 49.1 ± 2.0 | −0.2 ± 1.0 | −0.4 ± 2.0 |
| 12 mo | 1806 | 71.0 ± 2.7 | −1.6 ± 1.1 | −3.6 ± 2.6 |
| 24 mo | 1806 | 79.5 ± 3.3 | −2.5 ± 1.0 | −7.4 ± 3.2 |
| Mid-childhood | 1806 | 117.9 ± 5.3 | −2.0 ± 0.9 | −11.7 ± 5.3 |
| Adulthood | 1806 | 157.7 ± 8.2 | −1.8 ± 0.8 | −12.6 ± 5.6 |
| South Africa | ||||
| Birth | — | — | — | — |
| 12 mo | 1179 | 73.4 ± 2.9 | −0.6 ± 1.1 | −1.1 ± 2.8 |
| 24 mo | 1179 | 83.2 ± 3.2 | −1.2 ± 1.0 | −3.8 ± 3.1 |
| Mid-childhood | 1179 | 99.0 ± 4.0 | −0.9 ± 0.9 | −3.6 ± 3.9 |
| Adulthood | 1179 | 165.0 ± 8.7 | −0.6 ± 0.9 | −4.2 ± 6.5 |
Values are means ± SDs unless otherwise indicated. Mid-childhood is defined as 48 mo for all countries except for the Philippines, where it is defined as 102 mo. COHORTS, Consortium of Health-orientated Research in Transitioning Societies.
The reference is the 50th percentile (median) for age- and sex-specific height (cm) based on the WHO growth standards; each individual's height difference from the reference was calculated, and then the mean difference was determined for each country and time point.
As the cohorts aged, the difference between the mean height and the reference medians became greater (Table 1). At 24 mo, the mean difference between the children's heights and the reference ranged from −1.5 cm (Brazil) to −8.9 (Guatemala). Between 24 mo and adulthood there was a further increase in this difference, so that in adulthood the difference ranged from −2.4 cm (Brazil) to −12.6 (Philippines). Thus, from 59% (Philippines) to 90% (South Africa) of the deficit in adult height was established by age 24 mo.
DISCUSSION
By using prospectively followed birth cohorts in 5 middle-income countries, we documented that from age 2 y through adulthood, mean HAZs increased and the prevalence of stunting decreased, even though height deficits relative to the reference median became larger.
Growth is a widely used measure to gauge the quality of a child's environment, because growth failure is related to a wide range of adverse outcomes in later life (10). HAZ values are frequently used to compare children of the same age and sex in different locations and over time. An analysis of cross-sectional data from 54 countries, most of which were low- and middle-income settings, found that mean HAZ was <0 at birth and decreased sharply until age 24 mo, after which it increased slightly until 5 y of age (11). These and many other data support a focus on the first 1000 d of life (conception to 24 mo) for interventions aimed at improving growth. However, several studies, including an earlier article that used COHORTS data (5), showed an increase in HAZ from its nadir at 24 mo. Prentice et al (6) used those data to suggest that there may be periods beyond 24 mo in which substantial catch-up growth occurs, and interventions could improve growth. Lundeen et al (12), Crookston et al (13), Fink and Rockers (14), and Schott et al (15) found similar results for the Young Lives study in Ethiopia, India, Peru, and Vietnam.
The interpretation of within-child changes in mean HAZ over time, particularly in reference to catch-up growth, has been the subject of debate (3, 16). Leroy et al (3) argued that the interpretation of Prentice et al (6) is incorrect and that the increase in mean HAZ after 24 mo does not represent true catch-up growth in terms of height deficits but instead is a result of the method for calculating z scores. Our data support Leroy et al's argument. We showed that increases in HAZ can coexist with further accumulation of deficits in height relative to the reference medians. The arithmetic explanation for this apparent paradox can be found in the calculation of HAZ as the difference between the child's measured length and that of the reference child of the same age and sex, divided by the SD of the age- and sex-specific reference distribution. The SDs of the reference distribution vary by age and are (for males) 1.89 cm at birth, 2.38 at 12 mo, 3.06 at 24 mo, 4.19 at 48 mo, and 7.30 in adulthood (8, 9). A similar pattern holds for females. Thus, for a constant absolute difference in height from the reference, HAZ will attenuate as the SD increases. This same calculation also explains at least part of the decreases in prevalence of stunting, which is defined as HAZ <−2.0. As HAZ increases, the prevalence of stunting will decrease, even without any true recovery of the heights of the individuals being measured.
A limitation of these data is possible sample selection bias resulting from attrition within the cohorts. To be included in the analytic sample, participants had to have a weight or length measurement at birth and length or height measurements at all subsequent time periods. Among the 5 cohorts, Brazil and South Africa had relatively higher attrition of participants. However, an analysis of HAZ patterns in the cross-sectional data showed that they were parallel to the patterns seen among those for whom we have complete longitudinal data, making selection bias unlikely.
Our findings argue for careful interpretation of the metrics used for defining catch-up growth in height in populations in whom growth failure is still the norm. Choosing HAZs or absolute height differences from the median as alternative metrics may result in opposite conclusions about the existence of catch-up growth from birth to adulthood. We suggest that height deficit should always be included in the evaluation, because the mathematical properties of HAZ over time will, by nature, result in a more optimistic assessment of catch-up growth.
In addition, the 2 measurements may differ in their value for evaluating associations between child growth and long-term health and development outcomes. For any given age, HAZ is a linear transformation of the height deficit from the reference median, and thus it is perfectly correlated and equivalent in its predictive value at that time point. However, changes in HAZs and height deficits over time are not necessarily perfectly correlated, and therefore these 2 measurements may differ in their ability to predict long-term outcomes. An important area for future research is determining which metric, changes in HAZ or changes in height deficit over time, is better at predicting different outcomes. We are aware of no such research.
The majority of the deficit in adult height, from 59% in the Philippines to 90% in South Africa, accrues by 24 mo. Taken together with evidence on the importance of early growth for cognitive development in particular and adult human capital in general (17), we strongly endorse a continued focus on the “first 1000 days” as a critical window for interventions to promote human capital over the life course.
Acknowledgments
The COHORTS group members are as follows—Pelotas Birth Cohort (Brazil): Fernando C Barros, Denise Gigante, Pedro C Hallal, Bernardo L Horta, Cesar G Victora (Universidade Federal de Pelotas, Pelotas); INCAP (Instituto de Nutrición de Centra América y Panamá) Nutrition Trial Cohort Study (Guatemala): Reynaldo Martorell, Aryeh D Stein (Emory University, Atlanta, GA); Manual Ramirez-Zea (INCAP, Guatemala); New Delhi Birth Cohort Study (India): Harshpal S Sachdev, Shikha Sinha (Sitaram Bhartia Institute for Science and Research, New Delhi); Lakshmi Ramakrishnan, Nikhil Tandon (All-India Institute of Medical Sciences, New Delhi); Dorairaj Prabhakaran (Centre for the Control of Chronic Diseases, New Delhi); K Srinath Reddy (Public Health Foundation of India, New Delhi); Anita Khalil (The Heart Centre, New Delhi); Poornima Prabhakaran (Initiative for Cardiovascular Health Research in Developing Countries, New Delhi); SK Dey Biswas (Indian Council of Medical Research, New Delhi); Santosh Bhargava, Tarun Gera, KD Gupta, Arti Mishra, Dinesh Mishra, Bhaskar Singh, Rajeshwari Verma (SL Jain Hospital, Delhi); Siddarth Ramji (Maulana Azad Medical College, New Delhi); Caroline HD Fall, Clive Osmond (University of Southampton, Southampton, United Kingdom); Cebu Longitudinal Health and Nutrition Study (Philippines): Linda S Adair (University of North Carolina at Chapel Hill, Chapel Hill, NC); Isabelita Bas, Judith Borja, Nanette Lee (Office of Population Studies, University of San Carlos, Cebu City); Darren L Dahly (University of Leeds, Leeds); Christopher W Kuzawa (Northwestern University, Evanston IL); Birth to Twenty (South Africa): Shane A Norris, Linda Richter (University of the Witwatersrand, Johannesburg), Alan Stein (University of Oxford, Oxford).
The authors’ responsibilities were as follows—EAL and ADS: oversaw the design of the analysis, wrote the manuscript, and had primary responsibility for final content; and EAL: analyzed the data. All of the authors interpreted the data, helped prepare the manuscript, and approved the final version. None of the authors declared a conflict of interest.
REFERENCES
- 1.Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, de Onis M, Ezzati M, Grantham-McGregor S, Katz J, Martorell R, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet 2013;382:427–51. [DOI] [PubMed] [Google Scholar]
- 2.de Onis M, Blossner M, Borghi E. Prevalence and trends of stunting among pre-school children, 1990-2020. Public Health Nutr 2012;15:142–8. [DOI] [PubMed] [Google Scholar]
- 3.Leroy JL, Ruel M, Habicht J-P. Critical windows for nutritional interventions against stunting. Am J Clin Nutr 2013;98:854–8 (letter). [DOI] [PubMed] [Google Scholar]
- 4.Richter LM, Victora CG, Hallal PC, Adair LS, Bhargava SK, Fall CH, Lee N, Martorell R, Norris SA, Sachdev HS, et al. Cohort profile: the Consortium of Health-Orientated Research in Transitioning Societies. Int J Epidemiol 2012;41:621–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stein AD, Wang M, Martorell R, Norris SA, Adair LS, Bas I, Sachdev HS, Bhargava SK, Fall CH, Gigante DP, et al. Growth patterns in early childhood and final attained stature: data from five birth cohorts from low- and middle-income countries. Am J Hum Biol 2010;22:353–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Prentice AM, Ward KA, Goldberg GR, Jarjou LM, Moore SE, Fulford AJ, Prentice A. Critical windows for nutritional interventions against stunting. Am J Clin Nutr 2013;97:911–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Martorell R, Schroeder D, Rivera J, Kaplowitz H. Patterns of linear growth in rural Guatemalan adolescents and children. J Nutr 1995;125:1060S–7S. [DOI] [PubMed] [Google Scholar]
- 8.WHO Multicentre Growth Reference Study Group. WHO child growth standards based on length/height, weight and age. Acta Paediatr Suppl 2006;450:76–85. [DOI] [PubMed] [Google Scholar]
- 9.de Onis M, Onyango A, Borghi E, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ 2007;85:660–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hoddinott J, Behrman JR, Maluccio JA, Melgar P, Quisumbing AR, Ramirez-Zea M, Stein AD, Yount KM, Martorell R. Adult consequences of growth failure in early childhood. Am J Clin Nutr 2013;98:1170–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Victora CG, de Onis M, Hallal PC, Blössner M, Shrimpton R. Worldwide timing of growth faltering: revisiting implications for interventions. Pediatrics 2010;125:e473–80. [DOI] [PubMed] [Google Scholar]
- 12.Lundeen EA, Behrman JR, Crookston BT, Dearden KA, Engle P, Georgiadis A, Penny ME, Stein AD. Growth faltering and recovery in children aged 1–8 years in four low- and middle-income countries: Young Lives. Public Health Nutr (Epub ahead of print 15 November 2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Crookston BT, Schott W, Cueto S, Dearden K, Engle P, Georgiadis A, Lundeen EA, Penny ME, Stein AD, Behrman JR. Postinfancy growth, schooling, and cognitive achievement: Young Lives. Am J Clin Nutr 2013;98:1555–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fink G, Rockers PC. Childhood growth, schooling, and cognitive development: further evidence from the Young Lives Study. Am J Clin Nutr (Epub ahead of print 7 May 2014). [DOI] [PubMed] [Google Scholar]
- 15.Schott WB, Crookston BT, Lundeen EA, Stein AD, Behrman JR. Periods of child growth up to age 8 years in Ethiopia, India, Peru and Vietnam: key distal household and community factors. Soc Sci Med 2013;97:278–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Marshall WA, Tanner JM. Puberty. In: Falkner F, Tanner JM, eds. Human growth: a comprehensive treatise. Volume 1: developmental biology; prenatal growth. New York, NY: Plenum Press, 1986. [Google Scholar]
- 17.Victora CG, Adair L, Fall C, Hallal PC, Martorell R, Richter L, Sachdev HS. Maternal and child undernutrition: consequences for adult health and human capital. Lancet 2008;371:340–57. [DOI] [PMC free article] [PubMed] [Google Scholar]