Abstract
Purpose
To investigate secular changes in CHD incidence and mortality among adults with and without diabetes and determine the effect of increased lipid-lowering medication use and reductions in low-density lipoprotein cholesterol (LDL-C) levels on these changes.
Methods
We analyzed data on participants aged 45–64 years from the Atherosclerosis Risk in Communities Study in 1987–1996 (early time period) and the Reasons for Geographic and Racial Differences in Stroke Study in 2003–2009 (late time period). Hazard ratios (HR) for the association of diabetes and time period with incident CHD and CHD mortality were obtained after adjustment for socio-demographics, cardiovascular risk factors, lipid-lowering medication use, and LDL-C.
Results
After multivariable adjustment, diabetes was associated with an increased CHD risk during the early (HR=1.99,95% CI=1.59,2.49) and late (HR=2.39,95% CI=1.69,3.35) time periods. CHD incidence and mortality declined between the early and late time periods for individuals with and without diabetes. Increased use of lipid-lowering medication and lower LDL-C explained 33.6% and 27.2% of the decline in CHD incidence and CHD mortality, respectively, for those with diabetes.
Conclusions
Although rates have declined, diabetes remains associated with an increased risk of CHD incidence and mortality, highlighting the need for continuing diabetes prevention and cardiovascular risk factor management.
Keywords: diabetes, CHD, LDL-cholesterol, epidemiology
Substantial declines in CHD incidence, mortality, and case-fatality have occurred in recent decades in the general US population.(1, 2) However, few studies have examined secular changes in CHD morbidity and mortality among people with diabetes; a population with elevated risk for CHD. Some prior studies,(3–6) but not all,(7) reported declines in incident CHD rates for those with diabetes. Moreover, the findings for CHD mortality changes among those with diabetes have been conflicting, with some reports suggesting decreasing rates,(8–13) and others reporting increasing rates(14) as well as differences in rates by sex.(15–17)
Alongside declines in CHD, there has been a significant increase in the use of cardioprotective therapy, particularly lipid-lowering medications.(18, 19) Meta-analyses of randomized clinical trials have demonstrated that treatment to lower low-density lipoprotein cholesterol (LDL-C) is efficacious for reducing the risk of CHD and mortality among individuals with and without diabetes.(20, 21) Additionally, among available medical interventions, prior studies have suggested that the use of lipid-lowering medication and improved cholesterol levels would result in the greatest reduction in CHD risk and mortality.(22, 23) However, the control of LDL-C remains suboptimal,(24, 25) so it is unclear what impact increases in lipid-lowering medication use and associated declines in LDL-C levels may have had on current changes in CHD incidence, mortality, and case-fatality among individuals with and without diabetes.
The objective of this study was to compare CHD incidence, mortality, and case-fatality among middle-aged adults with and without diabetes in two time periods (1987–1996 and 2003– 2009). Additionally, we evaluated the contribution of lipid-lowering medication use and lower LDL-C levels on changes in CHD incidence and mortality over time.
RESEARCH DESIGN AND METHODS
Study populations
Data from 2 prospective cohort studies were included in this analysis—the Atherosclerosis Risk In Communities (ARIC) Study for the early time period (1987–1996) and the REasons for Geographic And Racial Differences in Stroke (REGARDS) Study for the late time period (2003–2009). Details of the design and conduct of each study have been published previously.(26, 27) Briefly, the ARIC study recruited 15,792 participants, age 45–64 years between 1987 and 1989, from 4 communities—Forsyth County, North Carolina; Jackson, Mississippi; suburbs of Minneapolis, Minnesota; and Washington County, Maryland. The REGARDS study recruited 30,239 black and white participants ≥ 45 years of age from the 48 contiguous US states and the District of Columbia between 2003 and 2007. To create comparable populations, only black and white participants from ARIC (n=15,732) and participants age 45 to 64 years at baseline from REGARDS (n=14,992) were eligible for inclusion in this analysis. Participants with a history of CHD at baseline (n=765 in ARIC; n=1,807 in REGARDS) and those missing diabetes status (n=142 in ARIC; n=473 in REGARDS) were excluded resulting in 14,825 ARIC participants for the early time period and 12,712 REGARDS participants for the late time period. Data from the ARIC study were obtained as a limited access dataset from the National Heart, Lung, and Blood Institute. Data from the REGARDS study were obtained from study investigators. The study protocols were approved by the institutional review boards governing research in human subjects at the participating centers and all participants provided written consent. Additionally, the secondary data analysis for this study was approved by the institutional review board at the University of Alabama at Birmingham.
Data collection
Baseline data were collected through interviews and a clinic examination for ARIC participants and through computer-assisted telephone interviews and an in-home examination for REGARDS participants. Age, race, sex, current smoking, and use of antihypertensive and lipid-lowering medications were self-reported during interviews. During the examination for both ARIC and REGARDS, height, weight, and blood pressure were measured and a blood specimen was collected. Both studies used manuals of operations, standardized data collection methods, and quality assurance procedures to ensure data quality. Additionally, each study used central laboratories that participated in the appropriate national laboratory quality programs for specimen analyses. Body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared. Total and high-density lipoprotein cholesterol (HDL-C) and triglycerides were measured enzymatically in ARIC and by colorimetric reflectance spectrophotometry in REGARDS. For participants with serum triglycerides < 4.52 mmol/L (400 mg/dL), LDL-C was calculated by the Friedewald equation.(28) Serum glucose was measured using a hexokinase/glucose-6-phosphate dehydrogenase method in ARIC and colorimetric reflectance spectrophotometry on the Ortho Vitros 950 IRC Clinical Analyzer (Johnson & Johnson Clinical Diagnostics) in REGARDS. Diabetes was defined as self-report of physician-diagnosed diabetes with concurrent use of insulin or oral hypoglycemic medication, serum glucose ≥ 7.0 mmol/L (126 mg/dL) for participants who had fasted for 8 hours, or serum glucose ≥ 11.1 mmol/L (200 mg/dL) for participants who had not fasted for 8 hours prior to blood specimen collection.
Follow-up for incident CHD and CHD mortality
For REGARDS participants, adjudicated CHD outcomes are available through December 31, 2009 for a maximum follow-up period of seven years. To provide comparability across study periods, follow-up of ARIC study participants was truncated at seven years. Incident CHD and CHD mortality events were adjudicated by trained ARIC and REGARDS study investigators, using procedures previously described elsewhere.(29–31) In the ARIC Study, participants were telephoned annually to ascertain hospitalizations and study personnel reviewed local hospital discharge lists. Medical records were obtained and abstracted for adjudication. Additionally, death certificates, interviews with family members, and questionnaires completed by the participant’s physician were used to investigate out-of-hospital deaths.
In the REGARDS study, participants were telephoned biannually to ascertain information on hospitalizations since their last contact for the retrieval of medical records. For participants who died, records of hospitalizations near the time of death were examined. Proxy interviews were conducted to obtain details of the death, including whether the person had a sudden witnessed demise or whether cardiac symptoms were present in the hours preceding death. Additionally, death certificates, autopsy reports, and data from the National Death Index were obtained to adjudicate cause of death. For this study, incident CHD included adjudicated events classified as definite or probable myocardial infarction (MI) or definite or probable CHD death. The 28-day and 365-day case-fatality was defined as the proportion of individuals with a non-fatal CHD event who died within 28 days or 365 days of the event, respectively.
The clinical diagnosis of MI changed over the study period with the introduction of high-sensitivity troponin assays.(32, 33) To reduce the number of CHD cases in 2003–2009 which would not have been diagnosed during 1987–1996, REGARDS participants with a peak in-hospital troponin < 0.5 μg/L were considered non-cases unless they had diagnostic ECG findings consistent with MI. Troponin < 0.5 μg/L was selected as the threshold because it is approximately one order of magnitude above the 99th percentile of normal in most currently available troponin assays.(34)
Statistical analysis
The cumulative incidence of CHD and CHD mortality was calculated using the Kaplan-Meier method for participants with and without diabetes by time period. Within each time period, age, race, and sex-adjusted incidence rates for CHD and CHD mortality were calculated for participants with and without diabetes using Poisson regression models with over-dispersion parameters. Cox proportional hazards models were used to obtain adjusted hazard ratios (HR) for incident CHD and CHD mortality comparing participants with diabetes versus without diabetes in each time period. Initial multivariable adjustment included age, race, and sex. Subsequent models also included adjustment for HDL-C, current smoking, systolic blood pressure, antihypertensive medication use, and BMI. The final models further adjusted for lipid-lowering medication use and LDL-C. For case-fatality, age, race, and sex-adjusted 28-day and 365-day case-fatality rates were calculated and logistic regression used to obtain odds ratios (OR) for case-fatality comparing participants with diabetes versus without diabetes in each time period.
The change in CHD incidence and mortality over time was also evaluated for participants with and without diabetes, separately. For this analysis, HRs for incident CHD and CHD mortality were obtained comparing the late time period to the early time period. To determine the contribution of lipid-lowering medication use and LDL-C levels on changes in CHD incidence and mortality over calendar time, a mediation analysis was conducted using a 1,000 iteration bootstrap.(35) Each iteration included 14,825 and 12,712 observations (i.e., the original sample size) from the original ARIC and REGARDS cohorts respectively, randomly sampled with replacement. The association of time period (late versus early time period) with CHD incidence and mortality was obtained for each iteration using Cox proportional hazards models with and without adjustment for the use of lipid-lowering medication and LDL-C. The percent change in the beta coefficient associated with time period between these two models was calculated. The median difference was used to calculate the percent attenuation with the 2.5th and 97.5th percentiles for the empirical 95% confidence intervals. Missing data for all covariates were imputed using chained equations with 10 data sets.(36) All analyses were conducted using SAS version 9.2 (SAS Institute, Cary NC) and Stata version 12 (Stata Corporation, College Station TX).
RESULTS
Mean age and proportion of men was similar among participants with and without diabetes and across time periods, whereas African-Americans comprised a greater proportion of those with diabetes in the early (1987–1996) and late (2003–2009) time periods (Table 1). Compared with participants in the early time period, those with and without diabetes in the late time period had lower mean LDL-C levels, were more likely to have an LDL-C < 100 mg/dL and to be taking lipid-lowering medications.
Table 1.
Baseline characteristics of individuals with and without diabetes in 1987–1996 and 2003–2009.
| No Diabetes | Diabetes | |||||
| 1987–1996 | 2003–2009 | p-value | 1987–1996 | 2003–2009 | p-value | |
| N | 13,152 | 10,415 | 1,673 | 2,297 | ||
| Age, years | 53.8 (5.7) | 56.9 (5.0) | <0.001 | 55.5 (5.7) | 57.9 (4.6) | <0.001 |
| Men, % | 43.4 | 40.6 | <0.001 | 42.6 | 41.0 | 0.31 |
| African-American, % | 24.5 | 39.1 | <0.001 | 44.9 | 64.3 | <0.001 |
| Current cigarette smoking, % | 26.4 | 18.1 | <0.001 | 23.1 | 17.6 | 0.03 |
| Body mass index, kg/m2 | 27.2 (5.1) | 29.2 (6.2) | <0.001 | 31.1 (6.0) | 33.9 (7.0) | <0.001 |
| Antihypertensive medication use, % | ||||||
| Overall | 21.2 | 38.6 | <0.001 | 48.3 | 72.0 | <0.001 |
| Among hypertensives | 69.4 | 80.8 | <0.001 | 85.2 | 93.2 | <0.001 |
| Systolic blood pressure, mmHg | 120.1 (18.2) | 123.6 (15.5) | <0.001 | 129.9 (20.8) | 130.7 (16.8) | 0.19 |
| HDL cholesterol, mg/dL | 52.9 (17.2) | 53.3 (16.2) | 0.11 | 45.2 (14.7) | 47.5 (13.9) | <0.001 |
| LDL cholesterol, mg/dL | 136.7 (38.9) | 121.1 (33.9) | <0.001 | 141.3 (41.6) | 109.1 (36.0) | <0.001 |
| LDL cholesterol < 100 mg/dL, % | 16.4 | 27.0 | <0.001 | 15.2 | 43.2 | <0.001 |
| Lipid-lowering medication use, % | 2.3 | 21.1 | <0.001 | 4.8 | 42.3 | <0.001 |
| Serum glucose, mg/dL | 98.5 (9.3) | 93.0 (12.8) | <0.001 | 185.5 (82.4) | 150.9 (65.8) | <0.001 |
| Insulin or oral hypoglycemic medication use, % | --- | --- | --- | 49.2 | 86.2 | <0.001 |
HDL: high-density lipoprotein; LDL: low-density lipoprotein
Numbers in tables are mean (standard deviation) or percent
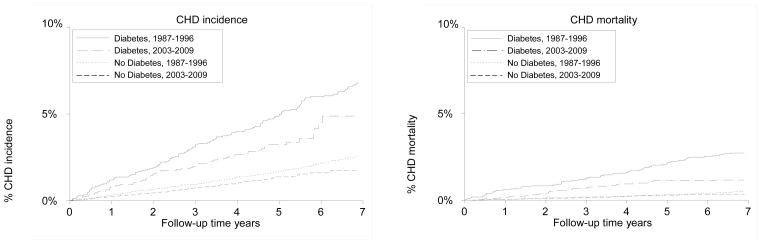
The maximum follow-up time was 7 years for the early and late time periods. In each time period, the CHD cumulative incidence was higher for participants with versus without diabetes (Figure 1). For those with and without diabetes, the incidence of CHD was lower in the late time period. CHD mortality was also lower in the late time period compared with the early time period for those with and without diabetes (Figure 1).
Figure 1.
Kaplan-Meier estimates for incident CHD and CHD mortality, stratified by time period and diabetes status
During the early and late time periods, CHD incidence and mortality rates were higher for those with versus without diabetes (Table 2). After adjustment for demographics and cardiovascular risk factors including lipid-lowering medication use and LDL-C, participants with diabetes had an increased risk of CHD in the early (HR=1.99, 95% CI=1.59, 2.49) and late (HR=2.39, 95% CI=1.69, 3.35) time periods compared with their counterparts without diabetes. Interaction terms for diabetes and time period were not statistically significant (p>0.05) for CHD incidence or mortality.
Table 2.
Coronary heart disease incidence and mortality rates and adjusted hazard ratios (95% CI) for the association of diabetes with CHD incidence and mortality in 1987–1996 and in 2003–2009.
| 1987–1996 | 2003–2009 | p-value interaction | |||
|---|---|---|---|---|---|
| No Diabetes | Diabetes | No Diabetes | Diabetes | ||
| N | 13,152 | 1,673 | 10,415 | 2,297 | |
| CHD incidence | |||||
| Incidence rate* (95% CI) | 3.9 (3.5, 4.4) | 11.1 (9.3, 13.2) | 2.2 (1.8, 2.7) | 5.4 (4.2, 7.0) | --- |
| Model 1† | 1 (ref) | 2.83 (2.29, 3.49) | 1 (ref) | 2.44 (1.78, 3.34) | 0.39 |
| Model 2‡ | 1 (ref) | 1.95 (1.56, 2.43) | 1 (ref) | 2.23 (1.60, 3.13) | 0.33 |
| Model 3§ | 1 (ref) | 1.99 (1.59, 2.49) | 1 (ref) | 2.39 (1.69, 3.35) | 0.95 |
| CHD mortality | |||||
| Mortality rate* (95% CI) | 0.8 (0.7, 1.1) | 4.3 (3.2, 5.7) | 0.4 (0.3, 0.6) | 1.3 (0.9, 1.9) | --- |
| Model 1† | 1 (ref) | 5.21 (3.58, 7.58) | 1 (ref) | 2.90 (1.73, 4.87) | 0.09 |
| Model 2‡ | 1 (ref) | 3.43 (2.30, 5.11) | 1 (ref) | 2.89 (1.66, 5.04) | 0.08 |
| Model 3§ | 1 (ref) | 3.45 (2.31, 5.14) | 1 (ref) | 3.21 (1.81, 5.63) | 0.21 |
CHD: coronary heart disease; CI: confidence interval; p-value for interaction of diabetes status and time period
Rates are per 1,000 person-years and adjusted for age, race, and sex
Model 1: adjusted for age, race, and sex
Model 2: adjusted for age, race, sex, high-density lipoprotein cholesterol, systolic blood pressure, antihypertensive medication use, current smoking, and body mass index
Model 3: adjusted for model 2 variables plus lipid-lowering medication use and low-density lipoprotein cholesterol
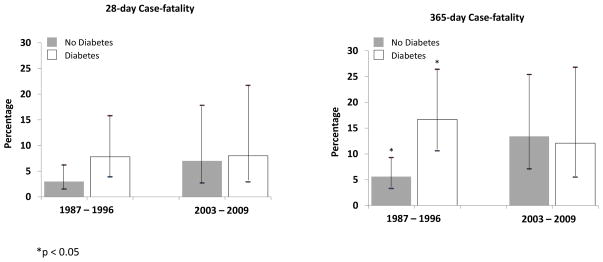
The 28-day and 365-day case-fatality was more than twice as high for those with diabetes, compared to those without, in the early time period, while case-fatality was similar in the late time period (Figure 2). In analyses adjusted for age, race, and sex, diabetes was associated with higher odds of 28-day and 365-day case-fatality in the early time period (28-day OR=2.21, 95% CI=0.97, 5.05; 365-day OR=2.17, 95% CI=1.21, 3.90). However, diabetes was not associated with an increased 28-day (OR=1.11, 95% CI=0.41, 2.98) or 365-day case-fatality (OR=0.96, 95% CI=0.40, 2.27) in the late time period.
Figure 2.
Age, race, and sex-adjusted coronary heart disease case-fatality rates for individuals with and without diabetes in 1987–1996 and 2003–2009
For those with and without diabetes, CHD incidence and mortality rates were lower in the late time period compared with the early time period (Table 3). After multivariable adjustment for demographics and cardiovascular risk factors, not including lipid-lowering medication and LDL-C, participants with and without diabetes in the late time period had a lower risk of CHD and mortality compared with their counterparts in the early time period. These associations were attenuated, but remained statistically significant, after further adjustment for lipid-lowering medication and LDL-C. In mediation analyses for those with diabetes, lipid-lowering medication use and LDL-C accounted for 33.6% (95% CI = 0.4% to 91.9%) and 27.2% (95% CI = −2.9% to 67.6%) of the decline in CHD incidence and mortality, respectively. Among those without diabetes, the attenuation associated with lipid-lowering medication use and LDL-C was 36.1% (95% CI = 15.5% to 81.6%) and 24.2% (95% CI = −1.4% to 104.9%) for CHD incidence and mortality, respectively. Race did not modify the association of time period with CHD incidence and mortality among those with or without diabetes in multivariable-adjusted models. However, there was a suggestion of possible differences by sex for incident CHD among those with diabetes (sex interaction p-value=0.16). Men with diabetes in the late time period had a lower risk of CHD than men with diabetes in the early time period (HR=0.48, 95% CI=0.28, 0.81), whereas for women with diabetes, the risk of CHD was similar in the late versus early time period (HR=1.06, 95% CI=0.61, 1.85). No differences by sex were observed for CHD mortality.
Table 3.
Coronary heart disease incidence and mortality rates and adjusted hazard ratios (95% CI) for the association of time period with CHD incidence and mortality in 1987–1996 and 2003–2009, stratified by diabetes status
| No Diabetes | Diabetes | p-value interaction | |||
|---|---|---|---|---|---|
| 1987–1996 | 2003–2009 | 1987–1996 | 2003–2009 | ||
| N | 13,152 | 10,415 | 1,673 | 2,297 | |
| CHD incidence | |||||
| Incidence rate* (95% CI) | 3.9 (3.5, 4.4) | 2.2 (1.8, 2.7) | 11.1 (9.3, 13.2) | 5.4 (4.2, 7.0) | --- |
| Model 1† | 1 (ref) | 0.60 (0.48, 0.76) | 1 (ref) | 0.53 (0.38, 0.73) | 0.39 |
| Model 2‡ | 1 (ref) | 0.64 (0.50, 0.80) | 1 (ref) | 0.56 (0.40, 0.78) | 0.33 |
| Model 3§ | 1 (ref) | 0.75 (0.59, 0.96) | 1 (ref) | 0.68 (0.46, 0.99) | 0.95 |
| CHD mortality | |||||
| Mortality rate* (95% CI) | 0.8 (0.7, 1.1) | 0.4 (0.3, 0.6) | 4.3 (3.2, 5.7) | 1.3 (0.9, 1.9) | --- |
| Model 1† | 1 (ref) | 0.49 (0.32, 0.76) | 1 (ref) | 0.32 (0.20, 0.52) | 0.09 |
| Model 2‡ | 1 (ref) | 0.55 (0.36, 0.85) | 1 (ref) | 0.34 (0.20, 0.56) | 0.08 |
| Model 3§ | 1 (ref) | 0.64 (0.40, 1.00) | 1 (ref) | 0.45 (0.26, 0.80) | 0.21 |
CHD: coronary heart disease; CI: confidence interval; p-value for interaction of diabetes status and time period
Rates are per 1,000 person-years and adjusted for age, race, and sex
Model 1: adjusted for age, race, and sex
Model 2: adjusted for age, race, sex, high-density lipoprotein cholesterol, systolic blood pressure, antihypertensive medication use, current smoking, and body mass index
Model 3: adjusted for model 2 variables plus lipid-lowering medication use and low-density lipoprotein cholesterol
CONCLUSIONS
In the current analysis, CHD incidence and mortality declined between 1987–1996 and 2003–2009 for individuals both with and without diabetes. Lipid-lowering medication use and improved LDL-C control increased over this time and explained a substantial percentage of the decline in CHD incidence and mortality. However, the approximate 2–3 fold higher risk for both CHD incidence and CHD mortality observed among individuals with diabetes in 1987–1996 remained evident in 2003–2009, even after adjustment for CHD risk factors including use of lipid-lowering therapy and LDL-C levels. In contrast, the higher CHD case-fatality for those with versus without diabetes observed in 1987–1996 was no longer present in 2003–2009.
Our findings are consistent with most prior studies, which have reported declines in CHD incidence among individuals with diabetes. A study in Ontario, Canada reported a 15% decline in MI rates over an 8 year period for those with diabetes after adjustment for age and sex.(3) Similarly, a study in the UK reported declining MI rates between 2004 and 2009 for those with diabetes and noted that diabetes was associated with an increased risk of MI compared with individuals without diabetes.(6) A recent study using data from the US National Hospital Discharge Survey also reported a decline in MI rates for adults with and without diabetes, with the relative risk of MI for those with versus without diabetes declining from 3.8 to 1.8 between 1990–2010.(37) The previous studies used administrative and survey data and did not adjust for cardiovascular risk factors. At least one population-based cohort in the US has examined changes in CHD incidence rates over time among people with and without diabetes after adjusting for cardiovascular risk factors. In the Framingham Heart Study, the CHD incidence rate declined 49.3% from the 1950s to 1990s after adjusting for cardiovascular risk factors. However, diabetes remained associated with an increased risk of CHD at the end of the study period.(5) Our study extends these findings by noting a persistently increased risk for both CHD incidence and mortality associated with diabetes through 2009 after adjustment for cardiovascular risk factors.
Prior studies investigating changes in CHD mortality among individuals with diabetes have reported inconsistent findings. Declines in CHD mortality among individuals with diabetes have been reported in Rochester, MN (1970–1994),(8) Framingham, MA (1950–2001),(9) North Dakota (1997–2002),(10) and Norway (1984–2004).(11) Conversely, an increase in CHD mortality, albeit not statistically significant, was reported among Pima Indians between 1975 and 1989.(14) Additionally, several other studies have reported sex differences in CHD mortality changes among individuals with diabetes. In the NHANES I Epidemiologic Follow-up Study, CHD mortality rates declined from 1971 through 1992 for men with diabetes but increased for women with diabetes.(16) Another study using mortality follow-up data from NHANES I, II, and III reported a decline in CHD mortality over time for men with diabetes but no change for women with diabetes.(15) A recent Swedish study also reported a decline in CHD mortality for men with diabetes but no change for women with diabetes between 1972 and 2004.(17) In contrast, a study using data from the US National Health Interview Survey reported declines in the CVD mortality rate between 1997 and 2006 for individuals with and without diabetes and did not observe any differences by sex.(12) However, the previous study used a broader definition of CVD mortality based on ICD-9 codes 390 to 448 (ICD-10 codes I00 to I78).(12) It is possible that multiple factors, including differences in time periods evaluated, study population characteristics, and methods to assess cause of death, may have contributed to the inconsistent results for CHD mortality. In the current analysis, we used adjudicated CHD mortality events and identified declines in CHD mortality overall for those with and without diabetes and did not observe differences by sex for CHD mortality.
CHD case fatality has declined in community surveillance studies of the general population.(1, 2) In the current analysis, the change in case fatality rates between 1987–1996 and 2003–2009 was small and not statistically significant for those with and without diabetes. Diabetes was not associated with an increased 28-day or 365-day case fatality in the late time period; however, there were few case fatality events so caution should be taken when making inferences based on these findings. Additionally, case fatality includes death from any cause after a participant has had an adjudicated CHD event, so it is possible that clinical advances in the diagnosis of CHD events, particularly in chronically ill patients, may have affected the case fatality rates observed in the late time period in the current analysis.
The use of lipid-lowering medications has increased substantially since the 1990s,(18, 19, 38, 39) with concurrent decreases in mean levels of LDL-C.(39) As expected, a significant increase in lipid-lowering medication use among individuals with and without diabetes as well as a decrease in mean LDL-C between the early and late time periods was observed in the current study. In the Framingham Study, LDL-C control improved between 1970 and 2005 for those without diabetes but was stable for those with diabetes.(24) In contrast, the prevalence of LDL-C < 100 mg/dL increased among those with diabetes in our study, which is in agreement with national data that identified significant increases in LDL-C control among individuals with diabetes between 1999 and 2010.(40) However, it should be recognized that LDL-C associated risk may be underrepresented due to cholesterol-depleted LDL particles that accompany type 2 diabetes.(41)
Several studies have investigated the effect of lipids and lipid-lowering medications on CHD risk among individuals with diabetes.(22, 23, 38, 42) Using the IMPACT model, data from Ontario, Canada showed that statin therapy would lead to the greatest reductions in CHD mortality compared with other pharmacologic therapies.(23) These findings are in agreement with our study, which found that the use of lipid-lowering medication and LDL-C contributed to 33.6% and 27.2% of the observed decline in CHD incidence and mortality, respectively, among those with diabetes.
This study has several potential limitations. Data from 2 community-based cohort studies were included in this analysis. While both studies used standardized protocols, central laboratories, and quality control procedures, there could have been systematic differences in some of the data measures collected and the risk profiles of the participants that could have affected the findings in this study. The clinical diagnosis of MI changed over the study period, which alone could affect CHD changes. To address this issue, we did not classify individuals in the 2003–2009 time period with troponin < 0.5 μg/L as a CHD case unless there was ECG evidence to indicate a MI event. Also, the clinical cut-point for the diagnosis of diabetes changed in 1997 from 140 mg/dL to 126 mg/dL. We defined diabetes using the same glucose cut-point for both the early and late time periods, but it is likely that individuals in the early time period had their diagnosis later based on the criteria used at that time and this may have affected their risk for macrovascular disease. Additionally, other changes occurred in diabetes management during this period that could have also affected risk for vascular outcomes, including the introduction of metformin for diabetes therapy in the US in 1995 and the increased focus on glycemic control as a quality performance measure for diabetes management. Lastly, information on diabetes duration was not available in this study.
In summary, CHD incidence and mortality declined between 1987–1996 and 2003–2009 for middle-aged adults with and without diabetes. Despite the observed declines, individuals with diabetes continue to have a substantially higher risk of CHD incidence and mortality compared with those without diabetes. Increased lipid-lowering medication use and improved LDL-C appear to explain a substantial proportion of the reduction in CHD incidence and mortality over time among those with and without diabetes. These data highlight the need for continued emphasis on diabetes prevention and increased appropriate use of lipid-lowering therapy to achieve LDL-C control for both individuals with and without diabetes.
Acknowledgments
The authors thank the other investigators, the staff, and the participants of the REGARDS study for their valuable contributions. A full list of participating REGARDS investigators and institutions can be found at http://www.regardsstudy.org. The ARIC Study is conducted and supported by the National Heart, Lung, and Blood Institute. This article was prepared using a limited access data set obtained from the National Heart, Lung, and Blood Institute and does not necessarily reflect the opinions or views of the ARIC Study or the National Heart, Lung, and Blood Institute.
Funding Sources
The REGARDS project is supported by a cooperative agreement U01 NS041588 from the National Institute of Neurological Disorders and Stroke and a grant R01 HL 080477 from the National Heart, Lung, and Blood Institute. This analysis, including its design and conduct, was supported by Amgen, Inc. The academic authors conducted all analyses and maintained the rights to publish this manuscript.
List of Abbreviations and Acronyms
- ARIC
Atherosclerosis Risk in Communities Study
- CHD
Coronary Heart Disease
- LDL-C
Low-density lipoprotein cholesterol
- REGARDS
Reasons for Geographic and Racial Differences in Stroke Study
Footnotes
Disclosures
The authors received research support from Amgen, Inc. Dr. Muntner has served as a consultant for Amgen, Inc. Dr. Woolley is an employee of Amgen, Inc.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Rosamond WD, Chambless LE, Folsom AR, Cooper LS, Conwill DE, Clegg L, et al. Trends in the incidence of myocardial infarction and in mortality due to coronary heart disease, 1987 to 1994. N Engl J Med. 1998;339(13):861–7. doi: 10.1056/NEJM199809243391301. [DOI] [PubMed] [Google Scholar]
- 2.Rosamond WD, Chambless LE, Heiss G, Mosley TH, Coresh J, Whitsel E, et al. Twenty-two-year trends in incidence of myocardial infarction, coronary heart disease mortality, and case fatality in 4 US communities, 1987–2008. Circulation. 2012;125(15):1848–57. doi: 10.1161/CIRCULATIONAHA.111.047480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Booth GL, Kapral MK, Fung K, Tu JV. Recent trends in cardiovascular complications among men and women with and without diabetes. Diabetes Care. 2006;29(1):32–7. doi: 10.2337/diacare.29.01.06.dc05-0776. [DOI] [PubMed] [Google Scholar]
- 4.Fox CS, Coady S, Sorlie PD, D’Agostino RB, Sr, Pencina MJ, Vasan RS, et al. Increasing cardiovascular disease burden due to diabetes mellitus: the Framingham Heart Study. Circulation. 2007;115(12):1544–50. doi: 10.1161/CIRCULATIONAHA.106.658948. [DOI] [PubMed] [Google Scholar]
- 5.Fox CS, Coady S, Sorlie PD, Levy D, Meigs JB, D’Agostino RB, Sr, et al. Trends in cardiovascular complications of diabetes. JAMA. 2004;292(20):2495–9. doi: 10.1001/jama.292.20.2495. [DOI] [PubMed] [Google Scholar]
- 6.Vamos EP, Millett C, Parsons C, Aylin P, Majeed A, Bottle A. Nationwide study on trends in hospital admissions for major cardiovascular events and procedures among people with and without diabetes in England, 2004–2009. Diabetes Care. 2012;35(2):265–72. doi: 10.2337/dc11-1682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lopez-de-Andres A, Hernandez-Barrera V, Carrasco-Garrido P, Esteban-Hernandez J, Gil-de-Miguel A, Jimenez-Garcia R. Trends of hospitalizations, fatality rate and costs for acute myocardial infarction among Spanish diabetic adults, 2001–2006. BMC Health Serv Res. 2010;10:59. doi: 10.1186/1472-6963-10-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thomas RJ, Palumbo PJ, Melton LJ, 3rd, Roger VL, Ransom J, O’Brien PC, et al. Trends in the mortality burden associated with diabetes mellitus: a population-based study in Rochester, Minn, 1970–1994. Arch Intern Med. 2003;163(4):445–51. doi: 10.1001/archinte.163.4.445. [DOI] [PubMed] [Google Scholar]
- 9.Preis SR, Hwang SJ, Coady S, Pencina MJ, D’Agostino RB, Sr, Savage PJ, et al. Trends in all-cause and cardiovascular disease mortality among women and men with and without diabetes mellitus in the Framingham Heart Study, 1950 to 2005. Circulation. 2009;119(13):1728–35. doi: 10.1161/CIRCULATIONAHA.108.829176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tierney EF, Cadwell BL, Engelgau MM, Shireley L, Parsons SL, Moum K, et al. Declining mortality rate among people with diabetes in North Dakota, 1997–2002. Diabetes Care. 2004;27(11):2723–5. doi: 10.2337/diacare.27.11.2723. [DOI] [PubMed] [Google Scholar]
- 11.Dale AC, Vatten LJ, Nilsen TI, Midthjell K, Wiseth R. Secular decline in mortality from coronary heart disease in adults with diabetes mellitus: cohort study. BMJ. 2008;337(7661):99–102. doi: 10.1136/bmj.39582.447998.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gregg EW, Cheng YJ, Saydah S, Cowie C, Garfield S, Geiss L, et al. Trends in Death Rates Among U.S. Adults With and Without Diabetes Between 1997 and 2006: Findings from the National Health Interview Survey. Diabetes Care. 2012;35(6):1252–7. doi: 10.2337/dc11-1162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Olafsdottir E, Aspelund T, Sigurdsson G, Benediktsson R, Thorsson B, Harris TB, et al. Similar decline in mortality rate of older persons with and without type 2 diabetes between 1993 and 2004 the Icelandic population-based Reykjavik and AGES-Reykjavik cohort studies. BMC Public Health. 2013;13:36. doi: 10.1186/1471-2458-13-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sievers ML, Nelson RG, Bennett PH. Sequential trends in overall and cause-specific mortality in diabetic and nondiabetic Pima Indians. Diabetes Care. 1996;19(2):107–11. doi: 10.2337/diacare.19.2.107. [DOI] [PubMed] [Google Scholar]
- 15.Gregg EW, Gu Q, Cheng YJ, Narayan KM, Cowie CC. Mortality trends in men and women with diabetes, 1971 to 2000. Ann Intern Med. 2007;147(3):149–55. doi: 10.7326/0003-4819-147-3-200708070-00167. [DOI] [PubMed] [Google Scholar]
- 16.Gu K, Cowie CC, Harris MI. Diabetes and decline in heart disease mortality in US adults. JAMA. 1999;281(14):1291–7. doi: 10.1001/jama.281.14.1291. [DOI] [PubMed] [Google Scholar]
- 17.Jansson SP, Andersson DK, Svardsudd K. Mortality trends in subjects with and without diabetes during 33 years of follow-up. Diabetes Care. 2010;33(3):551–6. doi: 10.2337/dc09-0680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ford ES, Li C, Pearson WS, Zhao G, Mokdad AH. Trends in hypercholesterolemia, treatment and control among United States adults. Int J Cardiol. 2010;140(2):226–35. doi: 10.1016/j.ijcard.2008.11.033. [DOI] [PubMed] [Google Scholar]
- 19.Ford ES, Li C, Sniderman A. Temporal changes in concentrations of lipids and apolipoprotein B among adults with diagnosed and undiagnosed diabetes, prediabetes, and normoglycemia: findings from the National Health and Nutrition Examination Survey 1988–1991 to 2005–2008. Cardiovasc Diabetol. 2013;12:26. doi: 10.1186/1475-2840-12-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Baigent C, Keech A, Kearney PM, Blackwell L, Buck G, Pollicino C, et al. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90 056 participants in 14 randomised trials of statins. Lancet. 2005;366(9493):1267–78. doi: 10.1016/S0140-6736(05)67394-1. [DOI] [PubMed] [Google Scholar]
- 21.Kearney PM, Blackwell L, Collins R, Keech A, Simes J, Peto R, et al. Efficacy of cholesterol-lowering therapy in 18,686 people with diabetes in 14 randomised trials of statins: a meta-analysis. Lancet. 2008;371(9607):117–25. doi: 10.1016/S0140-6736(08)60104-X. [DOI] [PubMed] [Google Scholar]
- 22.Ford ES. Trends in the risk for coronary heart disease among adults with diagnosed diabetes in the U.S.: findings from the National Health and Nutrition Examination Survey, 1999–2008. Diabetes Care. 2011;34(6):1337–43. doi: 10.2337/dc10-2251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wijeysundera HC, Machado M, Farahati F, Wang X, Witteman W, van der Velde G, et al. Association of temporal trends in risk factors and treatment uptake with coronary heart disease mortality, 1994–2005. JAMA. 2010;303(18):1841–7. doi: 10.1001/jama.2010.580. [DOI] [PubMed] [Google Scholar]
- 24.Preis SR, Pencina MJ, Hwang SJ, D’Agostino RB, Sr, Savage PJ, Levy D, et al. Trends in cardiovascular disease risk factors in individuals with and without diabetes mellitus in the Framingham Heart Study. Circulation. 2009;120(3):212–20. doi: 10.1161/CIRCULATIONAHA.108.846519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brown TM, Tanner RM, Carson AP, Yun H, Rosenson RS, Farkouh ME, et al. Awareness, treatment, and control of LDL cholesterol are lower among United States adults with undiagnosed diabetes versus diagnosed diabetes. Diabetes Care. 2013;36(9):2734–40. doi: 10.2337/dc12-2318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.The ARIC Investigators. The Atherosclerosis Risk in Communities (ARIC) Study: design and objectives. Am J Epidemiol. 1989;129(4):687–702. [PubMed] [Google Scholar]
- 27.Howard VJ, Cushman M, Pulley L, Gomez CR, Go RC, Prineas RJ, et al. The Reasons for Geographic and Racial Differences in Stroke Study: objectives and design. Neuroepidemiology. 2005;25(3):135–43. doi: 10.1159/000086678. [DOI] [PubMed] [Google Scholar]
- 28.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18(6):499–502. [PubMed] [Google Scholar]
- 29.White AD, Folsom AR, Chambless LE, Sharret AR, Yang K, Conwill D, et al. Community surveillance of coronary heart disease in the Atherosclerosis Risk in Communities (ARIC) Study: methods and initial two years’ experience. J Clin Epidemiol. 1996;49(2):223–33. doi: 10.1016/0895-4356(95)00041-0. [DOI] [PubMed] [Google Scholar]
- 30.Parmar G, Ghuge P, Halanych JH, Funkhouser E, Safford MM. Cardiovascular outcome ascertainment was similar using blinded and unblinded adjudicators in a national prospective study. J Clin Epidemiol. 2010;63(10):1159–63. doi: 10.1016/j.jclinepi.2009.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Halanych JH, Shuaib F, Parmar G, Tanikella R, Howard VJ, Roth DL, et al. Agreement on cause of death between proxies, death certificates, and clinician adjudicators in the Reasons for Geographic and Racial Differences in Stroke (REGARDS) Study. Am J Epidemiol. 2011;173(11):1319–26. doi: 10.1093/aje/kwr033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Alpert JS, Thygesen K, Antman E, Bassand JP. Myocardial infarction redefined--a consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction. J Am Coll Cardiol. 2000;36(3):959–69. doi: 10.1016/s0735-1097(00)00804-4. [DOI] [PubMed] [Google Scholar]
- 33.Thygesen K, Alpert JS, White HD, Jaffe AS, Apple FS, Galvani M, et al. Universal definition of myocardial infarction. Circulation. 2007;116(22):2634–53. doi: 10.1161/CIRCULATIONAHA.107.187397. [DOI] [PubMed] [Google Scholar]
- 34.Apple FS, Collinson PO. Analytical characteristics of high-sensitivity cardiac troponin assays. Clin Chem. 2012;58(1):54–61. doi: 10.1373/clinchem.2011.165795. [DOI] [PubMed] [Google Scholar]
- 35.Mackinnon DP, Warsi G, Dwyer JH. A simulation study of mediated effect measures. Multivariate Behav Res. 1995;30(1):41. doi: 10.1207/s15327906mbr3001_3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.White IR, Royston P, Wood AM. Multiple imputation using chained equations: Issues and guidance for practice. Stat Med. 2011;30(4):377–99. doi: 10.1002/sim.4067. [DOI] [PubMed] [Google Scholar]
- 37.Gregg EW, Li Y, Wang J, Rios Burrows N, Ali MK, Rolka D, et al. Changes in Diabetes-Related Complications in the United States, 1990–2010. N Engl J Med. 2014;370(16):1514–23. doi: 10.1056/NEJMoa1310799. [DOI] [PubMed] [Google Scholar]
- 38.Charlton J, Latinovic R, Gulliford MC. Explaining the decline in early mortality in men and women with type 2 diabetes: a population-based cohort study. Diabetes Care. 2008;31(9):1761–6. doi: 10.2337/dc08-0137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Carroll MD, Kit BK, Lacher DA, Shero ST, Mussolino ME. Trends in lipids and lipoproteins in US adults, 1988–2010. JAMA. 2012;308(15):1545–54. doi: 10.1001/jama.2012.13260. [DOI] [PubMed] [Google Scholar]
- 40.Ali MK, Bullard KM, Saaddine JB, Cowie CC, Imperatore G, Gregg EW. Achievement of Goals in U.S. Diabetes Care, 1999–2010. N Engl J Med. 2013;368(17):1613–24. doi: 10.1056/NEJMsa1213829. [DOI] [PubMed] [Google Scholar]
- 41.Howard BV. Insulin resistance and lipid metabolism. Am J Cardiol. 1999;84(1, Supplement 1):28–32. doi: 10.1016/s0002-9149(99)00355-0. [DOI] [PubMed] [Google Scholar]
- 42.Olafsdottir E, Aspelund T, Sigurdsson G, Thorsson B, Eiriksdottir G, Harris TB, et al. Effects of statin medication on mortality risk associated with type 2 diabetes in older persons: the population-based AGES-Reykjavik Study. BMJ Open. 2011;1(1):e000132. doi: 10.1136/bmjopen-2011-000132. [DOI] [PMC free article] [PubMed] [Google Scholar]