ABSTRACT
A key characteristic of arenaviruses is their ability to establish persistent infection in their natural host. Different factors like host age, viral dose strain, and route of infection may contribute to the establishment of persistence. However, the molecular mechanisms governing persistence are not fully understood. Here, we describe gain-of-function mutations of lymphocytic choriomeningitis virus (LCMV) expressing Lassa virus (LASV) GP, which can prolong viremia in mice depending on the sequences in the GP-2 cytoplasmic tail. The initial mutant variant (rLCMV/LASV mut GP) carried a point mutation in the cytosolic tail of the LASV glycoprotein GP corresponding to a K461G substitution. Unlike what occurred with the original rLCMV/LASV wild-type (wt) GP, infection of C57BL/6 mice with the mutated recombinant virus led to a detectable viremia of 2 weeks' duration. Further replacement of the entire sequence of the cytosolic tail from LASV to LCMV GP resulted in increased viral titers and delayed clearance of the viruses. Biosynthesis and cell surface localization of LASV wt and mut GPs were comparable.
IMPORTANCE Starting from an emerging virus in a wild-type mouse, we engineered a panel of chimeric Lassa/lymphocytic choriomeningitis viruses. Mutants carrying a viral envelope with the cytosolic tail from the closely related mouse-adapted LCMV were able to achieve a productive viral infection lasting up to 27 days in wild-type mice. Biochemical assays showed a comparable biosynthesis and cell surface localization of LASV wt and mut GPs. These recombinant chimeric viruses could allow the study of immune responses and antivirals targeting the LASV GP.
INTRODUCTION
The prototypic arenavirus lymphocytic choriomeningitis virus (LCMV) represents a powerful experimental model used to study the virus-host interaction of noncytopathic viruses and the role of T cells in clearing viral infections in mouse models (1). Infection with several existing strains results in different outcomes causing either transient, acute infection with virus-specific protective immunity or protracted, chronic infection with persisting viremia and immunosuppression (2). LCMV is an enveloped virus comprising two segments (S and L) of ambisense single-stranded RNA. The S RNA encodes the nucleoprotein (NP) and the envelope glycoprotein precursor (GPC) that is posttranslationally cleaved by signal peptidase and the cellular proprotein convertase SKI-1/S1P into the mature virion glycoprotein complex SSP/GP-1/GP-2 (GPs). The L RNA encodes the RNA-dependent RNA polymerase (L) and a small RING finger protein (Z). The GP mediates cell target attachment and fusion. NP and Z cover several functions, including inhibition of the innate immune response and viral particle budding, respectively. NP and L assemble with the two ambisense segments to form the ribonucleoprotein complexes (RNPs), which serve as the templates for transcription and replication. It has been shown that in LCMV the viral polymerase L and GP-1 of the glycoprotein are important determinants for the outcome of infection; thus, single point mutations are sufficient for the generation of persistent strains (3–5). Further evidence indicates that GP-2 is critical for the assembly and infectivity of arenaviruses, especially the cytoplasmic domain, which plays a key role in the regulation of GP trafficking and interaction with Z and the stable signal peptide (SSP) of GPC (6).
Besides LCMV, one of the most prevalent human pathogens among the arenaviruses is Lassa virus (LASV), classified as a class A select agent by the U.S. National Institutes of Health. Spreading from its natural host, Mastomys natalensis, to humans, LASV causes several hundred thousand infections per year with high mortality in Western Africa. Lassa fever cases are regularly imported into Western industrialized countries (7–11). Considering the number of people affected and the absence of an effective vaccine, the development of novel therapeutics against LASV is urgently needed. LASV shares many biochemical characteristics with the prototypic Old World arenavirus LCMV, particularly in the processing of the GP and for viral budding and matrix function of Z (12, 13). We therefore investigated the properties of a recombinant GP-exchanged LCMV/LASV chimera. Previous studies with recombinant engineered chimeras of New World and Old World arenaviruses expressing genes from either related arenaviruses or rhabdoviruses showed an attenuated viral phenotype associated with immunogenicity (14, 15). Similar observations were made with reassortments of Lassa and Mopeia viruses (16). This resulted in the recommendation of exploiting this strategy for vaccine design (15, 17). Recombinant LCMV viruses expressing the LASV glycoprotein have been used to study virus entry and receptor targeting under biosafety level 2 (BSL2) conditions (18, 19), replication capacity, and T cell response (20). The in vivo behavior of recombinant envelope-exchanged LCMV/LASV GP viruses in adult wild-type (wt) mice has been described, but viremia generally lasted for only 4 days and was controlled by a robust T cell response (20).
In the present study, we identified a novel gain-of-function rLCMV/LASV GP mutant and investigated the effect of changing the LASV GP-2 to LCMV sequences in the viral persistence of recombinant LCMV/LASV GP viruses in vivo.
MATERIALS AND METHODS
Virus sequences.
The following virus strains (GenBank accession numbers) were used: Lassa virus Josiah (NC_004296), LCMV WE (FJ607036), LCMV Pasteur (DQ868485), LCMV Cl13 (DQ361065), LCMV Marseille (DQ286931), LCMV Traub (DQ868487), LCMV Callitrichid (AF325214.1), Lassa virus Bantou 366 (GU830839.1), Lassa virus AV (AF246121.2), Mopeia virus (AY772170.1), Mobala virus (NC_007903.1), and Ippy virus (NC_007905.1).
Virus generation and titration.
Recombinant LCMV (rLCMV) was generated as previously described (21, 22). In brief, after (consensus) cDNAs of the large and small segments of LCMV (ARM strain-derived variant Cl13) were generated, both segments were separately placed under the control of a pol I expression cassette including the 5′ and 3′ untranslated regions (UTRs). The minimal viral trans-acting factors, the polymerase (L) and the nucleoprotein (NP), are expressed by a beta-actin-driven promoter. Seventy-two to 96 h after Lipofectamine plasmid transfection, infectious virus was recovered from the BHK-21 supernatant. Infecting BHK-21 cells at a multiplicity of infection (MOI) of 0.01 after 48 h yielded a working stock (rLCMV/Cl13). By PCR cloning, the GP of LCMV was exchanged to create several LCMV-Lassa virus Josiah GP-2 chimeric viruses. All Lassa virus/LCMV cytosolic domain mutants were generated by circular PCR using the high-fidelity Phusion site-directed mutagenesis kit (New England BioLabs Inc., Ipswitch, MA). Prior to transfection, the cloned plasmids were sequenced to control for desired mutations and to exclude unwanted random mutations. The rLCMV/LCMV-Lassa virus GP-2 chimeric viruses were rescued in the same way as described for rLCMV/Cl13.
The focus-forming assay used to determine viral titers has already been described elsewhere (23). We detected the rLCMV/Jos wt virus with the monoclonal antibody VL-4, which is directed against the nucleoprotein of LCMV and not the GP. LCMV strains Armstrong and variant Cl13 have already been described extensively elsewhere (3).
Growth kinetics.
For in vitro virus growth kinetics, Vero, MC57, and BHK-21 cells, murine peritoneal macrophages, and human peripheral blood mononuclear cells (PBMCs) were used; for all plasmid transfection experiments (i.e., rescue of all described rLCMVs), BHK-21 cells were used. Human PBMCs were donated by human volunteers at the University Medical Centre (Geneva, Switzerland) and were purified using a Ficoll gradient and subsequent wash steps in phosphate-buffered saline (PBS)-EDTA and PBS. Human PBMCs (5 × 105) were seeded in 6-well plates and supplemented with 4 ml of RPMI medium with 10% fetal calf serum (FCS). Supernatant (300 μl) was taken for analysis at specified time points and replaced by medium. Murine peritoneal macrophages were collected from C57BL/6 mice 24 h after intraperitoneal injection of thioglycolate in RPMI medium with 10% FCS. A total of 1 × 106 cells per well were seeded in 6-well plates at day −1. At day 0, cells were infected with an MOI of 0.01 and supplemented with RPMI medium with 10% FCS. Supernatant (1 ml) was taken for analysis at specified time points and replaced by medium.
Animal experiments.
C57BL/6 and HHD mice were bred and maintained in the animal facilities of the University of Geneva and University of Zurich and were housed under specific-pathogen-free (SPF) conditions. Characterization of HHD mice has been carried out previously (24). Animal experiments were approved by the responsible cantonal authorities of Geneva and Zurich and were conducted according to the Swiss law for animal protection.
Infections of approximately 6-week-old mice were performed by the intravenous (i.v.) route with a dose of 102 to 106 focus-forming units (FFU). Virus for infection was grown on BHK-21 cells.
Cell lines, plasmids, and transfection.
Human embryonic kidney (HEK 293T) cells initially obtained from the ATCC were cultivated in Dulbecco's modified Eagle's medium (DMEM; Life Technologies, NY) supplemented with 10% fetal bovine serum (FBS), 100 units/ml penicillin, and 0.1 mg/ml streptomycin. Chinese hamster ovary K1 (CHO K1) cells from the same source were cultivated in DMEM-Ham's F12 at 1:1 (Biochrom AG, Berlin, Germany) supplemented with 10% FBS and penicillin-streptomycin. SKI-1/S1P-deficient CHO K1 cells (SRD12B) were supplemented with 5 μg/ml cholesterol (Sigma-Aldrich, Switzerland), 20 μM sodium oleate (Sigma-Aldrich, Switzerland), and 1 mM sodium mevalonate (Sigma-Aldrich, Switzerland) (25). All cell lines were grown at 37°C in 5% CO2. Transfections of CHO K1 and SRD12B cells were performed with Lipofectamine 2000 (Invitrogen) according to the manufacturer's instructions. Briefly, 2 × 105 cells were seeded 24 h prior to transfection with 0.8 μg of DNA and 2 μl of Lipofectamine 2000 per well. After 4 to 6 h, transfection solutions were replaced with complete medium. Transfection of HEK 293T cell monolayers was performed in poly-d-lysine-coated 10-cm dishes using calcium phosphate. For cell surface expression analysis, cells were transfected with 12 μg of the indicated arenavirus GP-expressing plasmid or enhanced green fluorescent protein (eGFP) expression plasmid as a control. Transfection was evaluated by GFP fluorescence.
Antibodies.
Monoclonal antibody (MAb) 83.6 (anti-LCMV GP) was described previously (26). Mouse anti-α-tubulin MAb was obtained from Sigma-Aldrich, Switzerland. Polyclonal rabbit anti-mouse antibody conjugated to horseradish peroxidase (HRP) (Dako, Glostrup, Denmark) was also used. In flow cytometry analysis, the Alexa Fluor 594-conjugated goat anti-mouse IgG (H+L) (Molecular Probes) was used.
Western blotting.
Cells were washed twice with cold PBS and lysed in CelLytic M mammalian cell lysis/extraction reagent (Sigma-Aldrich, Switzerland) supplemented with the cOmplete Mini protease inhibitor cocktail (Roche, Switzerland). Samples were cleared of cellular debris by centrifugation, mixed in a 1:1 ratio with 2× SDS-PAGE sample buffer (62.5 mM Tris-HCl [pH 6.8], 20% glycerol, 2% SDS, 10% dithiothreitol), boiled for 10 min at 95°C, and centrifuged for 5 min at 13,000 rpm prior to loading. Proteins were separated on polyacrylamide gels and blotted onto a nitrocellulose membrane. Membranes were incubated in blocking solution (PBS, 0.2% [wt/vol] Tween 20, 3% [wt/vol] nonfat milk) and subsequently incubated overnight with primary antibody (MAb 83.3 to LCMV GP-2 at 1:1,000 and MAb to α-tubulin at 1:10,000) at 4°C. Membranes were then washed thoroughly with PBS–0.2% (wt/vol) Tween 20 and incubated for 1 h at room temperature with the HRP-conjugated secondary antibodies (1:3,000). After three washes in PBS–0.2% (wt/vol) Tween 20, membranes were developed with the Amersham ECL Select kit (GE Healthcare Life Sciences, Sweden). For quantification and analysis of Western blotting results, the ImageQuantTL software (GE Healthcare Life Sciences, Sweden) was used.
Flow cytometry analysis.
HEK 293T cells were transfected with the indicated wild-type and mutant GPCs. After 48 h, cells were washed in calcium- and magnesium-free Hanks' balanced salt solution (HBSS; Invitrogen), detached with nonenzymatic cell dissociation solution (Sigma), and resuspended in fluorescence-activated cell sorter (FACS) buffer (1% [vol/vol] fetal bovine serum, 0.1% [wt/vol] sodium azide, PBS). Cell surface staining was performed with MAb 83.6 (1:100) combined with Alexa Fluor 594 secondary antibody (1:200) as previously described (27). Data were acquired with a FACSCalibur flow cytometer and analyzed by using CellQuest software (BD Biosciences, NJ).
Biosafety.
LCMV and all recombinant viruses here were handled under BSL2 conditions. Due notification of all activities involving microorganisms was given to the responsible Swiss authorities (BAFU).
Statistical analyses.
Viral titers were log transformed for statistical analyses. Statistical analyses were performed with PRISM Graph Pad V4.0. One-way analysis of variance (ANOVA) with the Bonferroni posttest was used for the comparison of individual values from multiple groups. Differences in individual values between two groups were analyzed by t tests (unpaired, two-tailed). Statistical significance is defined as P values of <0.05, <0.005, or <0.0005.
RESULTS
Emergence of an rLCMV/LASV GP mutant that can persist in vivo.
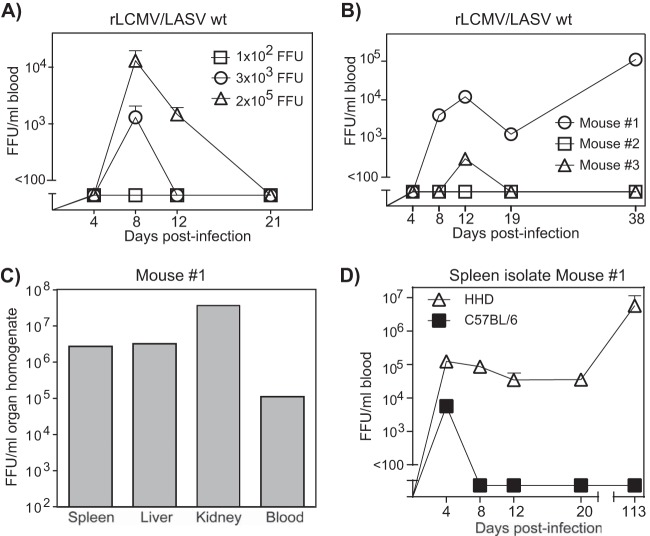
We selected the two mouse strains to have one prototypic strain for LCMV research (C57BL/6) and one with a major histocompatibility complex class I (MHC-I) humanized immune system (HHD). The latter has recently been proposed for use as a mouse model of LASV infection (24). Mice were infected with increasing doses of rLCMV Cl13 (1 × 102 to 2 × 105 FFU) expressing the glycoprotein of the Lassa strain Josiah (LCMV/LASV wt GP). Neither mouse strain showed clinical signs of disease or elevated liver enzymes (data not shown). Several independent experiments could not demonstrate consistent viremia for more than 5 days in C57BL/6 mice (data not shown), similar to previously published data (20). However, infection of HHD mice with high (2 × 105 FFU) and intermediate (3 × 103 FFU) doses of rLCMV/LASV wt GP resulted in a very short, transient viremia with virus clearance within 2 to 3 weeks (Fig. 1A). Surprisingly, in one experiment, a single HHD mouse (mouse 1) infected with 3 × 103 FFU could not eliminate the virus (Fig. 1B). Indeed, after being almost cleared by day 19, the virus rebounded by day 38 and high viremia was detectable not only in the blood but also in spleen, kidney, and liver (Fig. 1C).
FIG 1.
A mutant evolves in an rLCMV/LASV wt GP-infected HHD mouse. (A) HHD mice (n = 3) were infected with rLCMV/LASV wt GP i.v. at different doses (1 × 102, 3 × 103, and 2 × 105 FFU), and virus kinetics were determined. (B) In a repeat experiment, HDD mice (n = 3) were infected i.v. with 3 × 103 FFU of rLCMV/LASV wt GP. Individual mice are shown in the graph. One mouse (mouse #1) showed persistent infection at day 38. (C) Viral titers for different organs and whole blood of mouse 1 from the previous graph are shown. (D) HHD or C57BL/6 mice (n = 3 per group) were infected i.v. with 2 × 105 FFU of rLCMV/LASV mut GP (direct spleen isolate propagated on BHK-21 cells). Viral kinetics were determined.
Since the course of viremia of rLCMV/LASV GP is very short in adult mice (20), we hypothesized that these unexpected findings may result from the emergence of a novel rLCMV/LASV GP variant rather than being dependent on host variability. To verify our hypothesis, a new virus batch was grown on BHK-21 cells from spleen homogenate from mouse 1 (Fig. 1B). Subsequent infection of HHD and C57BL/6 mice with 1 × 106 FFU showed uniformly persistent infection with high viral loads in HHD and detectable viremia in C57BL/6 (Fig. 1D).
Taken together, the data at hand suggested the emergence of a gain-of-function rLCMV/LASV GP variant capable of chronically infecting mice.
In vivo fitness of rLCMV/LASV GP depends on GP-2.
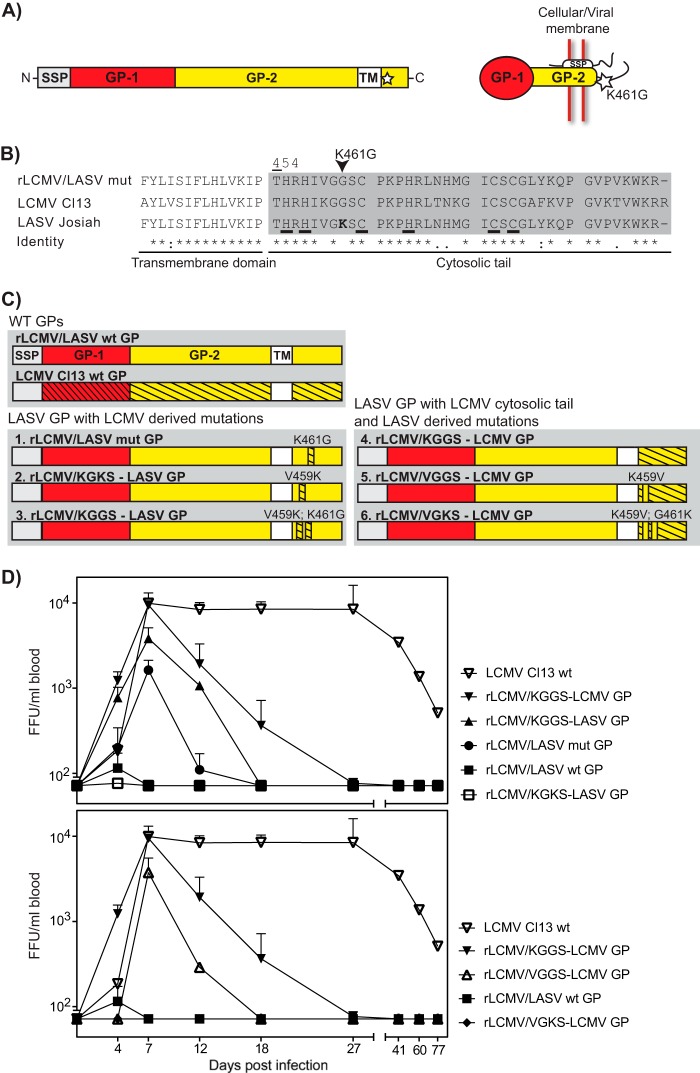
As with many RNA viruses, arenaviruses contain an error-prone RNA polymerase, resulting in the formation of viral quasispecies populations. These quasispecies contain phenotypic variants that underlie the observed high degree of virus adaptability (28). Here, we hypothesized the selection and enrichment of a mutated rLCMV/LASV GP with increased ability to persist in the host. To identify potential mutations, the viral RNA from the spleen of mouse 4 was isolated and the entire viral genome was determined by Sanger sequencing. The chromatograms showed clear peaks and, except for position K461G, did not show heterogeneity. NP, Z, and L sequences were identical to the wt LCMV ones (data not shown). In contrast, analysis of the GPC gene identified a single nonsynonymous mutation, K461G, within the master sequence, still containing the original Lassa virus sequence (Fig. 2A). K461G is located in the GP-2 subunit of the SSP/GP-1/GP-2 complex and is a mutation that requires two changes at the nucleotide level, AAG to GGG (where boldface indicates a substitution).
FIG 2.
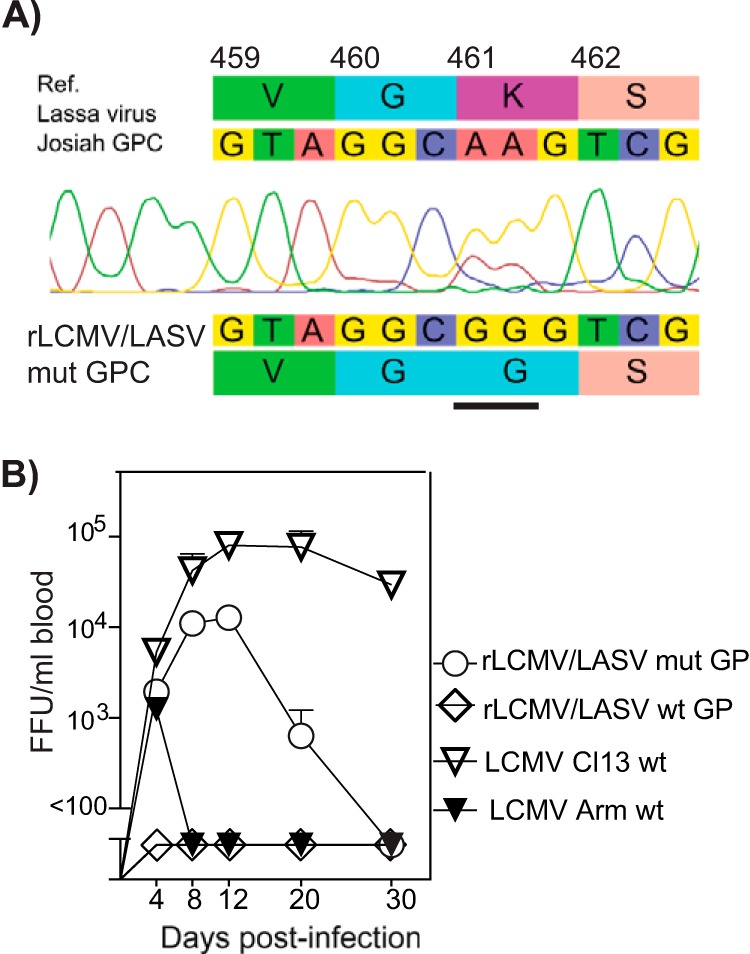
Mutation in the GP-2 cytosolic tail increases fitness of virus. (A) The sequence of the quasispecies with an emerging mutation in GP-2 was determined by classical Sanger sequencing of the complete genome. PCR amplicons generated by one-step RT-PCR from cell culture supernatant were directly sequenced without further subcloning. Mutated nucleotides are underlined. (B) C57BL/6 mice (n = 3 per group) were infected i.v. with 1 × 106 FFU rLCMV/LASV mut GP. Virus kinetics in blood was compared with that of LCMV strains Armstrong and Cl13 up to day 30.
To properly study this new virus isolate and to confirm the importance of the K461G mutation in conferring gain-of-function for the virus, we needed to do so without contamination of a quasispecies population containing the wt sequence. To do this, we recovered an rLCMV expressing the mutated Lassa virus envelope (rLCMV/LASV mut GP) from cDNA by reverse genetics based on plasmid transfection. Importantly, the mutant differed from the originally described live attenuated rLCMV/LASV wt GP only by this particular mutation within the GP-2 (Fig. 2A). The rescued virus did not differ from wild-type virus in virus titer or size of immunofoci. A comparison of the rLCMV/LASV mut GP virus with the prototypic LCMV strains Arm and Cl13 revealed an intermediate phenotype causing transient viremia lasting for >1 week in C57BL/6 mice, which was not observed in rLCMV/LASV wt GP (Fig. 2B). These data supported a direct link between the LASV GP K461G mutation and the ability of the recombinant virus to persist longer in vivo.
The GP-2 cytosolic tail is crucial to confer the in vivo gain-of-function phenotype to the virus.
The K461G mutation is predicted to be located within the cytosolic tail of the envelope GP (Fig. 3A). Interestingly, K461G is not related to any of the known LASV sequences: while every LASV GP described in GenBank carries a K at this position, all strains of the prototypic Old World arenavirus LCMV present a G. This suggests a mutation from an LASV GP toward an LCMV GP (Fig. 3B), which may add to the fitness of the virus. To demonstrate our hypothesis, we created additional viruses with different degrees of changes within the “KGGS” sequence, as we discovered the initial mutation within this region (Fig. 3C, mutants 1 to 3). An additional recombinant chimera having the entire wt cytosolic tail of LCMV GP (rLCMV/KGGS-LCMV GP) was also generated (Fig. 3C, mutant 4). BHK-21 cells were then used for de novo recovery and stock production from cDNA of these novel rLCMV mutants. Viruses were injected into C57BL/6 mice at 1 × 106 FFU, and blood viremia was determined by focus-forming assay over 77 days. As expected, the LCMV Cl13 wt strain (carrying the KGGS sequence) established chronic infection, whereas the rLCMV/LASV wt GP (VGKS) was rapidly cleared. The rLCMV/LASV mut GP (VGGS) showed an intermediate phenotype, in accordance with our previously reported findings (Fig. 2B). Interestingly, changing the LASV GP V549 into K (KGKS) was not sufficient to enable the virus to persist. In contrast, an LASV GP double mutation into the LCMV KGGS sequence improved viral persistence, resulting in titers higher than those of rLCMV/LAS mut GP and delayed clearance. Finally, the rLCMV/KGGS-LCMV GP virus, which carried the entire wt LCMV GP cytosolic tail, was the most persistent among the tested recombinant viruses and was capable of lasting up to 27 days postinfection. Maximum peak viremia of 1 × 104 FFU/ml blood was detected at day 7, which did not differ from LCMV Cl13 virus titers on the same day (Fig. 3D, top panel). However, neither of the rLCMV/LASV chimeric viruses reached the in vivo replicative capacity and ability to persist of wild-type LCMV Cl13.
FIG 3.
In vivo growth kinetics of mutant virus. (A) Schematic view of the glycoprotein protein and presumptive model of the folded protein with indication (star) of the predicted cytosolic location of the observed K461G mutation. (B) LCMV Cl13, LASV Josiah, and LASV mut GP cytosolic tail sequences were aligned, and residue conservation is indicated. The mutated K461G residue is shown, and residues belonging to the zinc finger-like domain are underlined. Numbering refers to the LASV Josiah sequence. (C) Schematic showing the key mutations of the recombinant-engineered LCMV/LASV GP mutants. (D) C57BL/6 wild-type mice were infected with 1 × 106 FFU i.v. of rLCMV/LASV GP, the mutated rLCMV/LASV mut GP, or combinations between VGKS, KGGS, and VGGS with the Lassa virus cytosolic tail (upper panel) or the LCMV cytosolic tail (lower panel). As a control, we injected 1 × 106 FFU i.v. of rLCMV/Cl13. At regular intervals, blood was drawn and virus titers (in FFU/ml) were determined.
Next, we hypothesized that insertion of the LASV “VGKS” sequence into the LCMV GP backbone could negatively affect viral persistence. For this purpose, we generated two additional viral chimeras using the KGGS-LCMV GP as the template. Single (VGGS) or double (VGKS) mutations were then introduced (Fig. 3C, mutants 5 and 6), and GP mutants were used for de novo virus recovery and stock production. Introduction of the VGGS (single mutation toward LASV) sequence into LCMV GP was tolerated but with a cost, resulting in a >1-log titer reduction and a 10-day-shorter infection. A double mutation toward LASV (VGKS) had a dramatic effect on the recombinant virus, which was highly attenuated, similarly to rLCMV/LASV wt GP (Fig. 3D, bottom panel).
Taken together, we showed that viremia and fitness of recombinant rLCMV/LASV GP mutants differ greatly and depend on the mutation from the LASV sequence to the LCMV GP-2 sequence. The strongest fitness is associated with the complete replacement of the cytosolic tail from LCMV (rLCMV/KGGS-LCMV GP). In particular, the KGGS sequence found in the cytosolic tail of LCMV GP-2 is crucial to confer a gain-of-function phenotype to LCMV in vivo. Of note, this was independent from the GP backbone, suggesting a key role of the KGGS sequence on the fitness of the virus. Conversely, introduction of the VGKS sequence found in the cytosolic tail of LASV GP-2 into LCMV GP-2 results in a loss-of-function phenotype of the virus in vivo.
In vitro infection by rLCMV/LASV mut GP mirrors the growth kinetics observed in vivo.
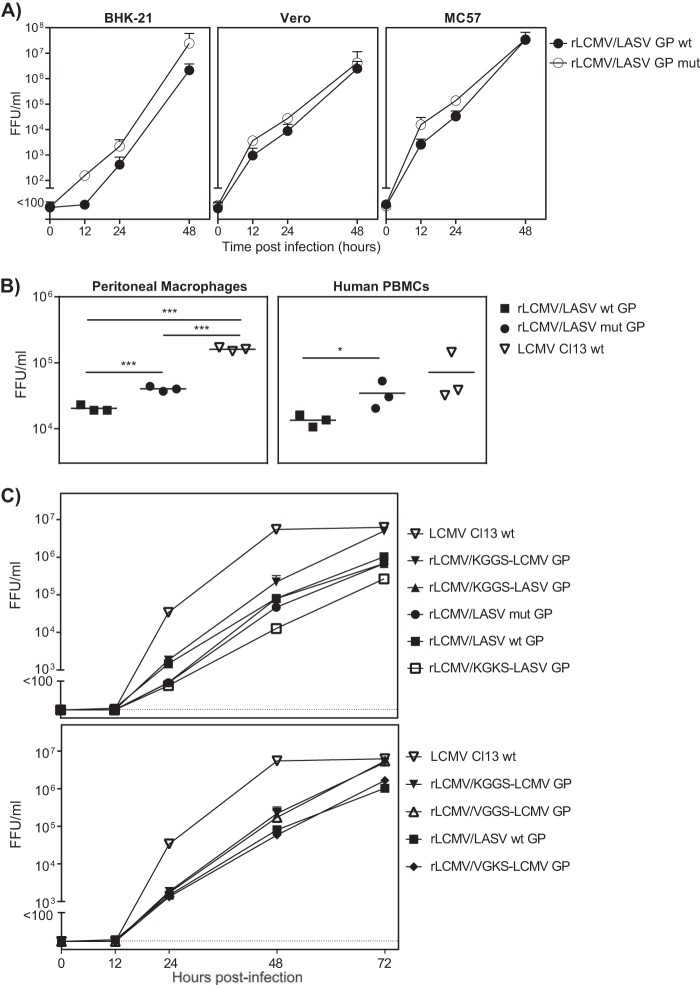
rLCMV/LASV mut GP is a gain-of-function variant. To shed some light on this unexpected in vivo phenotype, we first characterized and compared the virus growth curve kinetics in vitro, using MC57, BHK-21, and Vero cell lines. In addition, we tested primary peritoneal macrophages from mice and human PBMCs. All these experiments, irrespective of the species, suggest a growth advantage of rLCMV/LASV mut GP compared to the original rLCMV/LASV wt GP without being statistically significant (Fig. 4A). Maximal in vitro yields reach equally 1 × 107 FFU/ml for either rLCMV/LASV wt or mut GP virus (Fig. 4A). Comparisons of the mutant and the wild-type GPs with rLCMV Cl13 in primary cells revealed that the mutant is weaker than this particular LCMV strain but stronger than the rLCMV/LASV wt strain (Fig. 4B). While these observations are both significant and in agreement with our in vitro data, they must be interpreted with caution, as the differences are small. When we analyzed the growth kinetics of all virus chimeras, we could see that the fitness of the VGGS sequence from the rLCMV/LASV mut GP could be further improved if the entire cytosolic tail originated from LCMV (Fig. 4C).
FIG 4.
In vitro growth kinetics of mutant virus. (A) MC57, BHK-21, and Vero cells, each in triplicate, were infected at 60 to 70% confluence with either rLCMV/LASV wt GP or the mutated rLCMV/LASV mut GP at an MOI of 0.01. Supernatant was collected at the indicated time points after infection and assessed for FFU/ml. (B) Ex vivo peritoneal macrophages and human PBMCs from healthy volunteers were infected with either rLCMV/LASV GP, the mutated rLCMV/LASV mut GP, or rLCMV/Cl13 as a control. The cells were incubated for 2 or 7 days, respectively, and FFU/ml of the supernatant was determined using a focus-forming assay. Statistically significant differences between groups by ANOVA with the Bonferroni posttest were indicated with a connecting bar and labeled with asterisks (*, P < 0.05; **, P < 0.005; or ***, P < 0.0005) to demonstrate the degree of significance. (C) Subconfluent BHK-21 cells were infected at an MOI of 0.01 with rLCMV/LASV GP, the mutated rLCMV/LASV mut GP, or combinations between VGKS, KGGS, and VGGS with the Lassa cytosolic tail (upper panel) or the LCMV cytosolic tail (lower panel). As a control, wells were infected with rLCMV/Cl13. Virus titers were determined by focus-forming assay. For details of the statistical analysis, see Materials and Methods.
LASV mut and LASV wt GPC: processing and trafficking.
To investigate the impact of the K461G mutation on LASV mut GP biosynthesis and its interactions with other proteins, we performed a more in-depth molecular characterization of the GP variants.
The envelope GP of arenaviruses is synthesized as a precursor that is matured into GP-1, GP-2, and the SSP complex (Fig. 1B) (29, 30). GP-1/GP-2 processing is mediated by the cellular proprotein convertase subtilisin kexin isozyme 1 (SKI-1)/site-1 protease (S1P) and is crucial for infectious virus production. Interfering with GPC maturation greatly affects the envelope glycoprotein incorporation into budding particles (31).
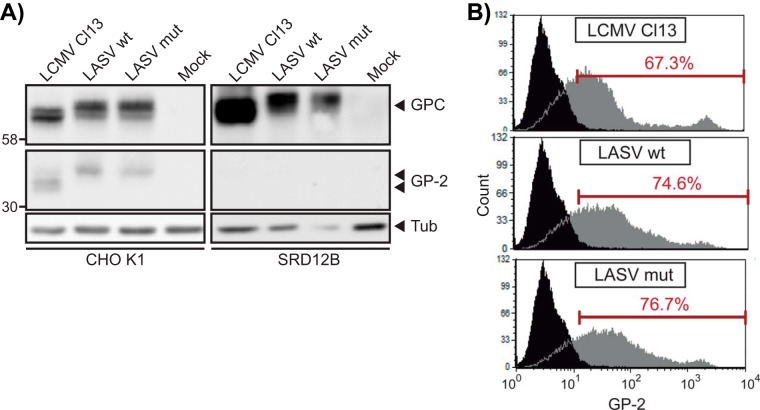
The LASV GPC K461G mutation is located 30 residues away from the C terminus. Alteration of the GP-2 cytosolic tail is known to have drastic effects on GPC maturation (27, 32). To investigate the role of the K461G mutation on LASV mut GPC expression and processing, we transiently transfected the LASV mut GP into either SKI-1/S1P-deficient SRD12B cells or the parental cell line CHO K1. LASV and LCMV GPC wt were used as controls. At 48 h posttransfection, cells were lysed and total proteins separated by SDS-PAGE. Our results (Fig. 5A, left panel) indicate that the expression and maturation of LASV mut GP are similar to expression of the wt GPs. Moreover, since no GP-2 is detectable in the SRD12B lysate, we exclude that the mutation present in the cytosolic tail alters the SKI-1/S1P dependence of GPC processing (Fig. 5A, right panel). Finally, the unprocessed (GPC) and processed (GP-2) glycoproteins showed similar apparent molecular masses in SDS-PAGE, suggesting similar overall glycosylation patterns of mut and wt GPs.
FIG 5.
Characterization of rLCMV/LASV mut GP. (A) The K461G mutation in LASV GPC does not affect the processing by SKI-1/S1P. CHO K1 or SRD12B cells were transfected with the indicated FLAG-tagged LASV GPC. As a mock control, an eGFP-encoding plasmid was used. After 48 h, cells were lysed and subjected to SDS-PAGE, followed by Western blotting. GPC and GP-2 were detected with anti-GP-2 antibody. For normalization of protein amounts, blots were stripped and incubated with an antibody to α-tubulin (Tub). (B) Cell surface expression of mutated LASV GPC is not impaired and is comparable to that of wt GP. HEK 293T cells were transfected with the wt LCMV Cl13 GP, wt LASV GP, or the mutated LASV GP and empty vector (mock) using calcium phosphate. After 48 h, cells were detached and single-cell suspensions prepared. Cell surface GPs were detected with mAb83.6 anti-LCMV GP-2 and an Alexa Fluor 594-conjugated secondary antibody to mouse IgG. Black histogram areas indicate background stained in mock-transfected cells and gray histograms staining in GPC-transfected cells. In histograms, the y axis represents cell numbers and the x axis fluorescence intensity (FL2-H for anti-mouse-Alexa Fluor 594).
Next, we examined the cell surface expression of the LASV wt GP, since productive infection requires virion assembly and budding at the plasma membrane of infected cells (33, 34). HEK 293T cells were transiently transfected with LASV mut GP or with LASV and LCMV wt GP as a control. At 48 h posttransfection, cell surface GP was detected by flow cytometry using an anti-GP-2 specific antibody. Comparable surface expression was detected for all variants (Fig. 5B), indicating that the mutation does not affect GP cellular trafficking and/or stability at the plasma membrane.
DISCUSSION
Former comparisons of different arenaviruses and isolate behavior emphasized the crucial importance of the GP-1 subunit in virus entry and subsequent establishment of a persistent infection (35–37). Despite GP-2 being key for SSP/Z interaction (6) and GPC processing (32), only very recently, a GP-2 mutation was shown to be responsible for the in vivo attenuation of an arenavirus member, namely, the Junin virus vaccine strain Candid1 (38). Here, for the first time we demonstrate the importance of the GP-2 cytosolic tail in the viral fitness of engineered recombinant LCMV viruses expressing the LASV GP.
We observed a dramatic gain of in vivo and in vitro viral replication of recombinant rLCMV/LASV when we changed the sequence of the GP-2 cytosolic tail from LASV to LCMV. Notably, the relative gain of persistence correlated well with the extent of the LASV-to-LCMV sequence mutation. A significant effect was already observed with the single K461G point mutation, which is highly conserved within all known LCMV isolates. We discovered that a point mutation at amino acid 461 of Lassa GP-2 gives rise to the ability to propagate productively in vivo, even in the absence of any mutation in GP-1.
The K461G mutation is located in the cytosolic tail, a segment of the GP that has been shown to be involved in several critical steps of the viral life cycle, including GP maturation, transport, and viral assembly at the plasma membrane (27, 29, 33, 39, 40). We therefore speculated that the present mutation could play a role in one of these steps. Our results indicate that the identified mutation affects neither LASV mut GP posttranslational modifications nor cell surface transport and expression. From these points of view, the two envelope GPs seem indistinguishable. A potential problem with the interpretation of the results from the GP-2 cell surface expression experiment was the GPCs' overexpression. The resulting effect of the mutation could possibly be overridden by this unnaturally high level of expression. This becomes more important when considering that the differences between the growth kinetics of rLCMV/LASV wt GP and rLCMV/LASV mut GP in cultured cells were mild.
The presence of a conserved zinc finger-like domain spanning the original KGGS mutation has been observed for GP-2 of all arenaviruses. This domain was shown to be important for stable SSP and membrane fusion (41). Further studies with recombinant arenaviruses with exchanged NP, Z, L, and SSP would be necessary to determine how the observed mutation affects these interactions.
Our findings help to better understand the molecular biology of the virus in terms of evolution and the impact of gene swapping between closely related arenaviruses. For the rLCMV/LASV GP virus, the GP-2 needs at least one additional mutation to be able to propagate productively in vivo. This knowledge may facilitate the generation of attenuated vaccines by inserting genes of highly pathogenic arenaviruses into an LCMV background. Recent literature suggests that envelope-exchanged Lassa/LCMV can be safely handled in BSL2 labs (20). The recombinant viruses described in this paper may also help to facilitate studies of LASV immunopathology by prolonged viremia in C57BL/6 mice in terms of studying neutralizing antibody responses as well as T cell responses to the Lassa glycoprotein.
This new role of GP-2 may open new avenues in developing vaccines against Lassa virus using a rational hypothesis-driven approach rather than laborious, although highly successful, methods like classical serial passages as in the case of the Argentine hemorrhagic fever vaccine strain (42, 43).
In conclusion, our experiments reveal, for the first time, a critical role for the cytosolic tail of GP in the virulence of rLCMV/LASV. The recombinant viruses described in this paper can be powerful BSL2 tools for investigating LASV immunopathology through prolonged viremia in C57BL/6 mice. This will be key in terms of future studies in neutralizing antibody responses as well as T cell responses to the Lassa glycoprotein.
ACKNOWLEDGMENTS
We thank Daniel Pinschewer for support and advice on this work, which was partly conducted in his laboratory, and Jovan Pavlovic (Institute of Medical Microbiology, University Hospital of Zurich) for access to his facilities. We furthermore thank Gary Nabel from the Vaccine Research Center, NIAID/NIH, who made it possible to conduct part of the work in his laboratory. We are indebted to Rolf Zinkernagel and Hans Hengartner for helpful discussions, for long-term support, and for mentorship. We feel indebted to Dieter Zimmermann (University Hospital of Zurich) for sequencing services, to Edith Horvath for excellent technical assistance, and to Jeffrey Boyington for help with intracellular GP-2 predictions. We thank Stefan Kunz for advice regarding the biochemical assays and for critical reading of the manuscript. We thank Stephan Günther for having provided us with a plasmid encoding the cDNA of Lassa virus Josiah GP. We thank Michael S. Brown and Joseph L. Goldstein (University of Texas Southwestern Medical Center, Dallas, TX) for the S1P-deficient SRD12B cells.
L.F. is supported by Stiftung Propter Homines (Vaduz, Liechtenstein), Fondation Leenaards, and the Mayenfisch Foundation.
Footnotes
Published ahead of print 14 May 2014
REFERENCES
- 1.Zinkernagel RM. 2002. Lymphocytic choriomeningitis virus and immunology. Curr. Top. Microbiol. Immunol. 263:1–5 [DOI] [PubMed] [Google Scholar]
- 2.Ahmed R, Hahn CS, Somasundaram T, Villarete L, Matloubian M, Strauss JH. 1991. Molecular basis of organ-specific selection of viral variants during chronic infection. J. Virol. 65:4242–4247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bergthaler A, Flatz L, Hegazy AN, Johnson S, Horvath E, Lohning M, Pinschewer DD. 2010. Viral replicative capacity is the primary determinant of lymphocytic choriomeningitis virus persistence and immunosuppression. Proc. Natl. Acad. Sci. U. S. A. 107:21641–21646. 10.1073/pnas.1011998107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Oldstone MB, Campbell KP. 2011. Decoding arenavirus pathogenesis: essential roles for alpha-dystroglycan-virus interactions and the immune response. Virology 411:170–179. 10.1016/j.virol.2010.11.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sevilla N, Kunz S, Holz A, Lewicki H, Homann D, Yamada H, Campbell KP, de La Torre JC, Oldstone MB. 2000. Immunosuppression and resultant viral persistence by specific viral targeting of dendritic cells. J. Exp. Med. 192:1249–1260. 10.1084/jem.192.9.1249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Capul AA, Perez M, Burke E, Kunz S, Buchmeier MJ, de la Torre JC. 2007. Arenavirus Z-glycoprotein association requires Z myristoylation but not functional RING or late domains. J. Virol. 81:9451–9460. 10.1128/JVI.00499-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bowen MD, Rollin PE, Ksiazek TG, Hustad HL, Bausch DG, Demby AH, Bajani MD, Peters CJ, Nichol ST. 2000. Genetic diversity among Lassa virus strains. J. Virol. 74:6992–7004. 10.1128/JVI.74.15.6992-7004.2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gunther S, Lenz O. 2004. Lassa virus. Crit. Rev. Clin. Lab Sci. 41:339–390. 10.1080/10408360490497456 [DOI] [PubMed] [Google Scholar]
- 9.Haas WH, Breuer T, Pfaff G, Schmitz H, Kohler P, Asper M, Emmerich P, Drosten C, Golnitz U, Fleischer K, Gunther S. 2003. Imported Lassa fever in Germany: surveillance and management of contact persons. Clin. Infect. Dis. 36:1254–1258. 10.1086/374853 [DOI] [PubMed] [Google Scholar]
- 10.Kitching A, Addiman S, Cathcart S, Bischop L, Krahe D, Nicholas M, Coakley J, Lloyd G, Brooks T, Morgan D, Turbitt D. 2009. A fatal case of Lassa fever in London, January 2009. Euro Surveill. 14(6):pii:19117 http://www.eurosurveillance.org/viewarticle.aspx?ArticleId=19117 [PubMed] [Google Scholar]
- 11.Olschlager S, Flatz L. 2013. Vaccination strategies against highly pathogenic arenaviruses: the next steps toward clinical trials. PLoS Pathog. 9:e1003212. 10.1371/journal.ppat.1003212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Burri DJ, Pasquato A, da Palma JR, Igonet S, Oldstone MB, Kunz S. 2013. The role of proteolytic processing and the stable signal peptide in expression of the Old World arenavirus envelope glycoprotein ectodomain. Virology 436:127–133. 10.1016/j.virol.2012.10.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Capul AA, de la Torre JC, Buchmeier MJ. 2011. Conserved residues in Lassa fever virus Z protein modulate viral infectivity at the level of the ribonucleoprotein. J. Virol. 85:3172–3178. 10.1128/JVI.02081-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Albarino CG, Bird BH, Chakrabarti AK, Dodd KA, White DM, Bergeron E, Shrivastava-Ranjan P, Nichol ST. 2011. Reverse genetics generation of chimeric infectious Junin/Lassa virus is dependent on interaction of homologous glycoprotein stable signal peptide and G2 cytoplasmic domains. J. Virol. 85:112–122. 10.1128/JVI.01837-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bergthaler A, Gerber NU, Merkler D, Horvath E, de la Torre JC, Pinschewer DD. 2006. Envelope exchange for the generation of live-attenuated arenavirus vaccines. PLoS Pathog. 2:e51. 10.1371/journal.ppat.0020051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lukashevich IS, Patterson J, Carrion R, Moshkoff D, Ticer A, Zapata J, Brasky K, Geiger R, Hubbard GB, Bryant J, Salvato MS. 2005. A live attenuated vaccine for Lassa fever made by reassortment of Lassa and Mopeia viruses. J. Virol. 79:13934–13942. 10.1128/JVI.79.22.13934-13942.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pinschewer DD, Perez M, Sanchez AB, de la Torre JC. 2003. Recombinant lymphocytic choriomeningitis virus expressing vesicular stomatitis virus glycoprotein. Proc. Natl. Acad. Sci. U. S. A. 100:7895–7900. 10.1073/pnas.1332709100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pasqual G, Rojek JM, Masin M, Chatton JY, Kunz S. 2011. Old world arenaviruses enter the host cell via the multivesicular body and depend on the endosomal sorting complex required for transport. PLoS Pathog. 7:e1002232. 10.1371/journal.ppat.1002232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rojek JM, Sanchez AB, Nguyen NT, de la Torre JC, Kunz S. 2008. Different mechanisms of cell entry by human-pathogenic Old World and New World arenaviruses. J. Virol. 82:7677–7687. 10.1128/JVI.00560-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lee AM, Cruite J, Welch MJ, Sullivan B, Oldstone MB. 2013. Pathogenesis of Lassa fever virus infection. I. Susceptibility of mice to recombinant Lassa Gp/LCMV chimeric virus. Virology 442:114–121. 10.1016/j.virol.2013.04.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Flatz L, Bergthaler A, de la Torre JC, Pinschewer DD. 2006. Recovery of an arenavirus entirely from RNA polymerase I/II-driven cDNA. Proc. Natl. Acad. Sci. U. S. A. 103:4663–4668. 10.1073/pnas.0600652103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Flatz L, Hegazy AN, Bergthaler A, Verschoor A, Claus C, Fernandez M, Gattinoni L, Johnson S, Kreppel F, Kochanek S, Broek M, Radbruch A, Levy F, Lambert PH, Siegrist CA, Restifo NP, Lohning M, Ochsenbein AF, Nabel GJ, Pinschewer DD. 2010. Development of replication-defective lymphocytic choriomeningitis virus vectors for the induction of potent CD8+ T cell immunity. Nat. Med. 16:339–345. 10.1038/nm.2104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Battegay M, Cooper S, Althage A, Banziger J, Hengartner H, Zinkernagel RM. 1991. Quantification of lymphocytic choriomeningitis virus with an immunological focus assay in 24- or 96-well plates. J. Virol. Methods 33:191–198. 10.1016/0166-0934(91)90018-U [DOI] [PubMed] [Google Scholar]
- 24.Flatz L, Rieger T, Merkler D, Bergthaler A, Regen T, Schedensack M, Bestmann L, Verschoor A, Kreutzfeldt M, Bruck W, Hanisch UK, Gunther S, Pinschewer DD. 2010. T cell-dependence of Lassa fever pathogenesis. PLoS Pathog. 6:e1000836. 10.1371/journal.ppat.1000836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rawson RB, DeBose-Boyd R, Goldstein JL, Brown MS. 1999. Failure to cleave sterol regulatory element-binding proteins (SREBPs) causes cholesterol auxotrophy in Chinese hamster ovary cells with genetic absence of SREBP cleavage-activating protein. J. Biol. Chem. 274:28549–28556. 10.1074/jbc.274.40.28549 [DOI] [PubMed] [Google Scholar]
- 26.Buchmeier MJ, Lewicki HA, Tomori O, Oldstone MB. 1981. Monoclonal antibodies to lymphocytic choriomeningitis and pichinde viruses: generation, characterization, and cross-reactivity with other arenaviruses. Virology 113:73–85. 10.1016/0042-6822(81)90137-9 [DOI] [PubMed] [Google Scholar]
- 27.Kunz S, Edelmann KH, de la Torre JC, Gorney R, Oldstone MB. 2003. Mechanisms for lymphocytic choriomeningitis virus glycoprotein cleavage, transport, and incorporation into virions. Virology 314:168–178. 10.1016/S0042-6822(03)00421-5 [DOI] [PubMed] [Google Scholar]
- 28.Domingo E, Sheldon J, Perales C. 2012. Viral quasispecies evolution. Microbiol. Mol. Biol. Rev. 76:159–216. 10.1128/MMBR.05023-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Eichler R, Lenz O, Strecker T, Eickmann M, Klenk HD, Garten W. 2003. Identification of Lassa virus glycoprotein signal peptide as a trans-acting maturation factor. EMBO Rep. 4:1084–1088. 10.1038/sj.embor.7400002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lenz O, ter Meulen J, Klenk HD, Seidah NG, Garten W. 2001. The Lassa virus glycoprotein precursor GP-C is proteolytically processed by subtilase SKI-1/S1P. Proc. Natl. Acad. Sci. U. S. A. 98:12701–12705. 10.1073/pnas.221447598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rojek JM, Pasqual G, Sanchez AB, Nguyen NT, de la Torre JC, Kunz S. 2010. Targeting the proteolytic processing of the viral glycoprotein precursor is a promising novel antiviral strategy against arenaviruses. J. Virol. 84:573–584. 10.1128/JVI.01697-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schlie K, Strecker T, Garten W. 2010. Maturation cleavage within the ectodomain of Lassa virus glycoprotein relies on stabilization by the cytoplasmic tail. FEBS Lett. 584:4379–4382. 10.1016/j.febslet.2010.09.032 [DOI] [PubMed] [Google Scholar]
- 33.Dalton AJ, Rowe WP, Smith GH, Wilsnack RE, Pugh WE. 1968. Morphological and cytochemical studies on lymphocytic choriomeningitis virus. J. Virol. 2:1465–1478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Murphy FA, Webb PA, Johnson KM, Whitfield SG, Chappell WA. 1970. Arenoviruses in Vero cells: ultrastructural studies. J. Virol. 6:507–518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kunz S, Sevilla N, Rojek JM, Oldstone MB. 2004. Use of alternative receptors different than alpha-dystroglycan by selected isolates of lymphocytic choriomeningitis virus. Virology 325:432–445. 10.1016/j.virol.2004.05.009 [DOI] [PubMed] [Google Scholar]
- 36.Radoshitzky SR, Kuhn JH, Spiropoulou CF, Albarino CG, Nguyen DP, Salazar-Bravo J, Dorfman T, Lee AS, Wang E, Ross SR, Choe H, Farzan M. 2008. Receptor determinants of zoonotic transmission of New World hemorrhagic fever arenaviruses. Proc. Natl. Acad. Sci. U. S. A. 105:2664–2669. 10.1073/pnas.0709254105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Salvato M, Borrow P, Shimomaye E, Oldstone MB. 1991. Molecular basis of viral persistence: a single amino acid change in the glycoprotein of lymphocytic choriomeningitis virus is associated with suppression of the antiviral cytotoxic T-lymphocyte response and establishment of persistence. J. Virol. 65:1863–1869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Albarino CG, Bird BH, Chakrabarti AK, Dodd KA, Flint M, Bergeron E, White DM, Nichol ST. 2011. The major determinant of attenuation in mice of the Candid1 vaccine for Argentine hemorrhagic fever is located in the G2 glycoprotein transmembrane domain. J. Virol. 85:10404–10408. 10.1128/JVI.00856-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Igonet S, Vaney MC, Vonhrein C, Bricogne G, Stura EA, Hengartner H, Eschli B, Rey FA. 2011. X-ray structure of the arenavirus glycoprotein GP2 in its postfusion hairpin conformation. Proc. Natl. Acad. Sci. U. S. A. 108:19967–19972. 10.1073/pnas.1108910108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Klewitz C, Klenk HD, ter Meulen J. 2007. Amino acids from both N-terminal hydrophobic regions of the Lassa virus envelope glycoprotein GP-2 are critical for pH-dependent membrane fusion and infectivity. J. Gen. Virol. 88:2320–2328. 10.1099/vir.0.82950-0 [DOI] [PubMed] [Google Scholar]
- 41.York J, Nunberg JH. 2007. A novel zinc-binding domain is essential for formation of the functional Junin virus envelope glycoprotein complex. J. Virol. 81:13385–13391. 10.1128/JVI.01785-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Albarino CG, Ghiringhelli PD, Posik DM, Lozano ME, Ambrosio AM, Sanchez A, Romanowski V. 1997. Molecular characterization of attenuated Junin virus strains. J. Gen. Virol. 78(Part 7):1605–1610 [DOI] [PubMed] [Google Scholar]
- 43.Maiztegui JI, McKee KT, Jr, Barrera Oro JG, Harrison LH, Gibbs PH, Feuillade MR, Enria DA, Briggiler AM, Levis SC, Ambrosio AM, Halsey NA, Peters CJ. 1998. Protective efficacy of a live attenuated vaccine against Argentine hemorrhagic fever. AHF Study Group. J. Infect. Dis. 177:277–283. 10.1086/514211 [DOI] [PubMed] [Google Scholar]