Abstract
Worldwide, nontuberculous mycobacteria (NTM) have become emergent pathogens of pulmonary infections in cystic fibrosis (CF) patients, with an estimated prevalence ranging from 5 to 20%. This work investigated the presence of NTM in sputum samples of 129 CF patients (2 to 18 years old) submitted to longitudinal clinical supervision at a regional reference center in Rio de Janeiro, Brazil. From June 2009 to March 2012, 36 NTM isolates recovered from 10 (7.75%) out of 129 children were obtained. Molecular identification of NTM was performed by using PCR restriction analysis targeting the hsp65 gene (PRA-hsp65) and sequencing of the rpoB gene, and susceptibility tests were performed that followed Clinical and Laboratory Standards Institute recommendations. For evaluating the genotypic diversity, pulsed-field gel electrophoresis (PFGE) and/or enterobacterial repetitive intergenic consensus sequence PCR (ERIC-PCR) was performed. The species identified were Mycobacterium abscessus subsp. bolletii (n = 24), M. abscessus subsp. abscessus (n = 6), Mycobacterium fortuitum (n = 3), Mycobacterium marseillense (n = 2), and Mycobacterium timonense (n = 1). Most of the isolates presented resistance to five or more of the antimicrobials tested. Typing profiles were mainly patient specific. The PFGE profiles indicated the presence of two clonal groups for M. abscessus subsp. abscessus and five clonal groups for M. abscesssus subsp. bolletii, with just one clone detected in two patients. Given the observed multidrug resistance patterns and the possibility of transmission between patients, we suggest the implementation of continuous and routine investigation of NTM infection or colonization in CF patients, including countries with a high burden of tuberculosis disease.
INTRODUCTION
The survival rate for cystic fibrosis (CF) patients has increased in recent years, mainly due to early diagnosis, nutritional therapies, and the discovery of new antimicrobial agents. Acute or chronic pulmonary infections caused by bacteria are the major causes of morbidity and mortality in CF patients (1). For the last 20 to 25 years, nontuberculous mycobacteria (NTM) have emerged as newly detected pathogens in CF patients. Several centers around the world have reported the isolation of NTM in the respiratory tracts of CF patients. Nowadays, this prevalence varies between 5 and 20% (2, 3, 4, 5, 6, 7), with most of those cases (>90%) caused by species of the Mycobacterium avium complex (MAC) and the Mycobacterium abscessus group (5, 8, 9).
NTM have been found and described in diverse environments and clinical scenarios, due to their adaptive biological properties and opportunistic potentials. It is considered that selective pressure in hospital environments, predominantly caused by excessive antibiotic use, has contributed to NTM resistance to a large number of antibiotics and disinfection processes, such as antituberculosis agents (i.e., isoniazid and pyrazinamide), glutaraldehyde, and organomercury compounds (10). However, NTM usually present as susceptible to aminoglycosides and macrolides (11, 12, 13). Cefoxitin, quinolone, and tetracyclines are other options for drug treatment, specifically for rapidly growing mycobacteria (RGM) infections. However, similar to other bacteria commonly associated with CF infections, NTM resistant strains have been reported. Broda et al. (14) reported clarithromycin susceptibility rates of 57% in Mycobacterium abscessus isolates. Binder et al. (13) suggested that all CF patients undertake evaluation for NTM disease, due to continual exposure to macrolides for other bacterial infections.
In Brazil, microbiological studies involving CF patients are rare, with most focused on infections caused by Burkholderia cenocepacia and/or Pseudomonas aeruginosa (2). The Instituto Fernandes Figueira (IFF) is a large unit that belongs to the Oswaldo Cruz Foundation (FIOCRUZ) and is the major clinical research center for CF children in Rio de Janeiro state and in the country of Brazil. Microbiological surveillance of these patients is common; however, investigation of NTM disease has only been performed since June 2009. Given the lack of epidemiological information on NTM in Brazilian CF children and the emergence of NTM as pathogens in this population worldwide, the significance of developing research on NTM and the association with CF is definitely warranted. Epidemiological studies in European cohorts have demonstrated a high prevalence of NTM infections in CF patients, but these countries have lower disease burdens of tuberculosis (TB). Brazil is one of the main high-TB-burden countries, and large epidemics of NTM infections have been described in recent literature (10). Therefore, it is necessary to undergo studies looking at the prevalence of NTM in CF patients to better understand the magnitude of this emergence in different countries globally.
This is the first complete study providing genotypic identification, antimicrobial susceptibility profiles, and strain diversity of nontuberculous mycobacteria isolates recovered from CF patients in Brazil.
MATERIALS AND METHODS
Mycobacterial isolates.
From June 2009 to March 2012, spontaneous sputum samples from CF patients monitored at a local reference center (IFF-FIOCRUZ, Rio de Janeiro, Brazil) were sent monthly to the Bacteriology and Mycobacteriology laboratories at Hospital Universitário Pedro Ernesto, Rio de Janeiro, Brazil, for routine microbiological investigation. Sputum samples were processed with NALC-NaOH and 5% oxalic acid decontamination as recommended by the National Guideline for TB and NTM Laboratory Surveillance (15). A total of 36 NTM isolates were recovered from sputum samples obtained from 10 of 129 children (7.75%; 2 to 18 years old).
Species identification.
A loopful of bacterial growth from Löwenstein-Jensen medium was mixed in 100 μl of TE (Tris-HCl at 10 mM, EDTA at 1 mM; pH 8.0). The suspensions were boiled at 100°C for 10 min and immediately incubated at 20°C for 12 h. Genotypic identification of the 36 isolates was performed by using PCR restriction analysis targeting the hsp65 gene (PRA-hsp65) with the primers TB11, 5′-ACCAACGATGGTGTGTCCAT-3′, and TB12, 5′-CTTGTCGAACCGCATACCCT-3′ (16). A denaturation step of 95°C for 5 min was followed by 45 cycles of 94°C for 1 min, 60°C for 1 min, and 72°C for 1 min and by a final extension of 72°C for 7 min. Amplicons were submitted to individual digestions with the restriction enzymes BstEII and HaeIII (Promega Corporation, Madison, WI) for 3 h at 60°C and 37°C, respectively. The digestion products were analyzed after 4% agarose gel electrophoresis at 3 V/cm using 25- and 50-bp DNA ladders (Invitrogen). The PRA-hsp65 profiles were analyzed using the algorithm available at the PRA site (http://app.chuv.ch/prasite/index.html).
All the results were confirmed by partial sequencing of the rpoB gene by using the primers Myco F (5′-GCAAGGTCACCCCGAAGGG-3′) and Myco R (5′-AGCGGCTGCTGGGTGATCATC-3′), according to the methodology described by Adekambi, Colson, and Drancourt (17). Region V rpoB gene sequences were submitted for BLAST similarity analysis (Basic Local Alignment Tool; http://www.ncbi.nlm.nih.gov/BLAST) and comparison to the sequences from M. abscessusT ATCC 19977 (JF346872), “M. massilienseT” CIP 108297 (EU254721.1), “M. bolletiiT” CCUG 50184 (DQ987717.1), the M. abscessus subsp. bolletii epidemic strain INCQS 594 (EU117207.1), M. fortuitum ATCC 6841 (JF346874.1), M. marseillense strain 62863 (EF584444.1), and M. timonense strain 3256799 (EF584435.1).
Antimicrobial susceptibility testing.
The RGM isolates were tested against dilutions of amikacin (128 to 1 μg/ml), cefoxitin (256 to 2 μg/ml), ciprofloxacin (16 to 0.125 μg/ml), clarithromycin (64 to 0.5 μg/ml), doxycycline (32 to 0.25 μg/ml), moxifloxacin (16 to 0.125 μg/ml), and sulfamethoxazole-trimethoprim (16/304 to 0.5/9.5 μg/ml). Slowly growing mycobacteria (SGM) were tested against amikacin (128 to 1 μg/ml), clarithromycin (64 to 0.5 μg/ml), streptomycin (16 to 0.125 μg/ml), ethambutol (16 to 0.125 μg/ml), moxifloxacin (16 to 0.125 μg/ml), and rifampin (16 to 0.125 μg/ml). MICS were measured using the microdilution broth method proposed by the Clinical Laboratory and Standards Institute (CLSI) (18). Only noninducible clarithromycin patterns (reading at 3 to 5 days) were evaluated in this study for M. abscessus.
The breakpoints proposed by Siddiqii and collaborators (19) were used to determine the resistance profiles of amikacin, streptomycin, ethambutol, and rifampin for SGM.
ERIC-PCR.
Enterobacterial repetitive intergenic consensus PCR (ERIC-PCR) was performed for the pulsed-field gel electrophoresis (PFGE)-nontypeable isolates in order to verify the genotypic diversity among them. The primers ERIC1R (5′-ATGTAAGCTCCTGGGGATTCAC-3′) and ERIC2 (5′-AAGTAAGTGACTGGGGTGAGCG-3′) were applied (20). The mixture was heated at 95°C for 4 min, followed by 35 cycles of 95°C for 45 s, 52°C for 1 min, and 70°C for 10 min and a last step of 70°C for 20 min. PCR products were analyzed after 2% gel electrophoresis (5 V/cm) and stained with ethidium bromide and using a 100-bp DNA ladder (Invitrogen). The profiles obtained by electrophoresis were analyzed and compared using the Bionumerics version 6.6 software platform (Applied Maths, Belgium). Dice's coefficient was applied, and a dendrogram based on percentages of similarity was generated by the using the unweighted-pair group with arithmetic mean (UPGMA) method. The genotypic grouping was done by automated and visual analyses of the gels, using a cutoff value of 85% similarity and a tolerance index of 1.5%.
PFGE.
PFGE was performed when multiple RGM isolates of the same species were obtained, in order to verify the genotypic diversity. The M. abscessus subsp. bolletii strain CRM 0019, which belongs to the BRA100 clone (10), and CCUG 48898 were used as control strains. The cells were grown in Mueller-Hinton agar (Becton, Dickinson and Company, Brazil) at 35 to 37°C for 7 days. Then, 3 isolated colonies were transferred to a flask containing 40 ml of Mueller-Hinton broth (Becton, Dickinson and Company, Brazil) with 0.1% Tween 80 (Sigma-Aldrich, Brazil) and incubated at 37°C. Flasks were shaken at 300 × g for at least 4 days until the optical density at 650 nm (OD650) reached 0.7. The cells from the liquid culture were harvested by centrifugation at 18,000 × g at 4°C for 25 min (Eppendorf 5810 R centrifuge). The pellet was frozen at −20°C for 2 h and then resuspended in STE-Tween 80 buffer (100 mM NaCl, 10 mM Tris [pH 8.0], 50 mM EDTA [pH 8.0], and 0.1% Tween 80) and mixed volume/volume with 2% low-melting-point agarose (Sigma-Aldrich, Brazil). The plugs were incubated at 4°C for 20 min. Each plug was individually treated with the solution containing STE plus 10 mg/ml lysozyme and incubated at 35 to 37°C for 16 h, followed by a new incubation at 4°C for 1 h. The lysis solution was replaced by a solution containing 0.5M EDTA and 1% Sarkosyl and incubated at 4°C for 1 h. It was then replaced by 0.5M EDTA, 1% Sarkosyl, and 50 mg/ml proteinase K (Invitrogen Life Technologies) for each sample. The plugs were incubated at 55°C for 24 h and at 4°C for 1 h. Each plug was washed with 1× TE and incubated for 30 min at 4°C. After this step, a new incubation at 55°C for 1 h with 1× TE and 0.12 mg/ml of phenylmethylsulfonyl fluoride (PMSF) was done. Each plug was washed three times with 1× TE, with incubation for 30 min at room temperature. The plugs were stored in 0.5M EDTA (Sigma-Aldrich) at 4°C. For the restriction enzyme digestion, a 3-mm piece was cut and washed twice with 1× TE at 4°C for 30 min, washed in 0.1% Triton at 4°C for 2 h, and then digested with 30 U DraI (Promega). Plugs were incubated for 16 h at 37°C and washed with 0.05M at 4°C for 15 min. The plugs were melted at 70°C, and the samples were loaded on a 1% agarose gel (Sigma-Aldrich) in 5× TE for the PFGE. The Lambda ladder PFG marker (Uniscience) was used as a molecular weight marker. The PFGE was performed on a CHEF DR III apparatu, using the following settings: initial time of 1.6 s, final time of 21.3 s, running time of 24 h, 6 V/cm, and 120° included angle. Gels were stained and photographed, and PFGE patterns obtained were analyzed by using Bionumerics version 6.6 software (Applied Maths, Belgium). Dice's coefficient was applied, and the dendrogram based on similarity percentages was generated by using the UPGMA method. The genotypic grouping was done by automated and visual analyses of the gels, using a tolerance index of 1.5%.
Statistical analysis.
Evaluation of discriminatory power was performed for M. abscessus subsp. bolletii isolate PFGE patterns by using the numerical index of discrimination (D), based on Simpson's index of diversity as described by Hunter and Gaston (21).
Ethics.
This study was approved by the Brazilian Ethics Committee and Regional committee (213/08-CEP HUCFF UFRJ, Caracterização Epidemiológica e Laboratorial das Micobacterioses do Trato Respiratório Inferior no Estado do Rio de Janeiro). Consent terms were obtained for all patients included in this study.
RESULTS
M. tuberculosis was not detected among any CF sputum samples. Considering NTM, 36 isolates were recovered from 10 patients, and multiple isolations of the same RGM species were observed. Although we considered the RGM isolated to be associated with respiratory infections, as recommended by the American Thoracic Society (ATS) (22), these organisms were not related to clinical syndromes. A letter identified each patient that had a positive isolate for NTM. The numbers in parentheses correspond to how many positive NTM isolates were found in each patient: A (3), B (3), C (2), D (3), E (2), F (2), G (1), H (15), I (4), J (1).
The analysis of the PRA-hsp65 results showed 22 M. abscessus type II (BstE II 235/210-HaeIII 200/70/60) restriction profiles, 8 M. abscessus type I (BstE II 235/210-HaeIII 145/70/60), 2 M. chimerae/M. intracellulare (BstE II 235/120/100-HaeIII 145/130/60), and 4 M. fortuitum type II (BstE II 235/120/85-HaeIII 140/120/60). The partial sequencing of the rpoB gene identified all isolates, indicating 98 to 100% similarity among 24 M. abscessus subsp. bolletii isolates and reference strains in the BLAST database, 98% similarity for 6 M. abscessus subsp. abscessus isolates, 99% similarity for 3 M. fortuitum isolates, 100% similarity for 2 M. marseillense isolates, and 100% similarity for 1 M. timonense isolate. However, these results were different from the PRA-hsp65 results for 2 isolates (CRM 694 and CRM 696), from patients G and C and identified as M. chimerae/M. intracellulare. These isolates showed 100% similarity to M. marseillense and, for CRM 747 (from patient C), 98% similarity to M. abscessus subsp. bolletii. Table 1 shows the results of the comparison between the techniques.
TABLE 1.
Comparison of PRA-hsp65 and rpoB sequencing results for identification of NTM strains isolated from sputum samples of 10 CF patients in Rio de Janeiro, Brazil
| Patient | Isolate | Isolation date (day/mo/yr) | Molecular identification based on: |
|
|---|---|---|---|---|
| PRA-hsp65 | rpoB sequence | |||
| A | CRM 511 | 17/06/2009 | M. abscessus type 1 | M. abscessus subsp. abscessus |
| CRM 718 | 24/02/2010 | M. abscessus type 1 | M. abscessus subsp. abscessus | |
| CRM 740 | 23/06/2010 | M. abscessus type 1 | M. abscessus subsp. abscessus | |
| B | CRM 641 | 21/10/2009 | M. abscessus type 1 | M. abscessus subsp. abscessus |
| CRM 697 | 11/01/2010 | M. abscessus type 1 | M. abscessus subsp. abscessus | |
| CRM 720 | 16/04/2011 | M. abscessus type 1 | M. abscessus subsp. abscessus | |
| C | CRM 696 | 03/12/2009 | M. chimerae/M. intracellulare | M. marseillense |
| CRM 747 | 12/07/2010 | M. abscessus type 1 | M. abscessus subsp. bolletii | |
| D | CRM 512 | 22/06/2009 | M. abscessus type 2/M. bolletii type 1 | M. abscessus subsp. bolletii |
| CRM 640 | 19/12/2009 | M. abscessus type 2/M. bolletii type 1 | M. abscessus subsp. bolletii | |
| CRM 920 | 20/06/2011 | M. abscessus type 2/M. bolletii type 1 | M. abscessus subsp. bolletii | |
| E | CRM 473 | 03/06/2009 | M. abscessus type 2/M. bolletii type 1 | M. abscessus subsp. bolletii |
| CRM 639 | 02/09/2009 | M. abscessus type 2/M. bolletii type 1 | M. abscessus subsp. bolletii | |
| F | CRM 836 | 19/01/2011 | M. abscessus type 2/M. bolletii type 1 | M. abscessus subsp. bolletii |
| CRM 901 | 21/03/2011 | M. abscessus type 2/M. bolletii type 1 | M. abscessus subsp. bolletii | |
| G | CRM 694 | 02/09/2009 | M. chimerae/M. intracellulare | M. marseillense |
| H | CRM 569 | 06/07/2009 | M. abscessus type 2/M. bolletii type 1 | M. abscessus subsp. bolletii |
| CRM 642 | 21/10/2009 | M. abscessus type 2/M. bolletii type 1 | M. abscessus subsp. bolletii | |
| CRM 719 | 31/03/2010 | M. abscessus type 2/M. bolletii type 1 | M. abscessus subsp. bolletii | |
| CRM 723 | 24/04/2010 | M. abscessus type 2/M. bolletii type 1 | M. abscessus subsp. bolletii | |
| CRM 732 | 02/06/2010 | M. abscessus type 2/M. bolletii type 1 | M. abscessus subsp. bolletii | |
| CRM 835 | 13/01/2011 | M. abscessus type 2/M. bolletii type 1 | M. abscessus subsp. bolletii | |
| CRM 915 | 14/04/2011 | M. abscessus type 2/M. bolletii type 1 | M. abscessus subsp. bolletii | |
| CRM 916 | 14/04/2011 | M. abscessus type 2/M. bolletii type 1 | M. abscessus subsp. bolletii | |
| CRM 917 | 14/04/2011 | M. abscessus type 2/M. bolletii type 1 | M. abscessus subsp. bolletii | |
| CRM 927 | 14/07/2011 | M. abscessus type 2/M. bolletii type 1 | M. abscessus subsp. bolletii | |
| CRM 928 | 04/08/2011 | M. abscessus type 2/M. bolletii type 1 | M. abscessus subsp. bolletii | |
| CRM 949 | 02/06/2010 | M. abscessus type 2/M. bolletii type 1 | M. abscessus subsp. bolletii | |
| CRM 950 | 08/11/2011 | M. abscessus type 2/M. bolletii type 1 | M. abscessus subsp. bolletii | |
| CRM 1009 | 12/03/2012 | M. abscessus type 2/M. bolletii type 1 | M. abscessus subsp. bolletii | |
| CRM 1010 | 12/03/2012 | M. abscessus type 2/M. bolletii type 1 | M. abscessus subsp. bolletii | |
| I | CRM 695 | 03/12/2009 | M. fortuitum type 2 | M. timonense |
| CRM 724a | 17/06/2009 | M. fortuitum type 2 | M. fortuitum | |
| CRM 725 | 17/06/2009 | M. fortuitum type 2 | M. fortuitum | |
| CRM 726 | 15/07/2009 | M. fortuitum type 2 | M. fortuitum | |
| J | CRM 803 | 30/08/2010 | M. abscessus type 1 | M. abscessus subsp. bolletii |
CRM 724 and CRM 725 were distinct colonies isolated from the same sputum sample.
Table 2 shows the MICs against the antimicrobials tested against RGM. Considering the three MAC isolates, all of them presented full resistance to streptomycin (MIC, 5 μg/ml), and they also showed intermediate resistance to ethambutol (MIC, 2.5 to 5 μg/ml), moxifloxacin (MIC, 2 μg/ml), and rifampin (MIC, 1 to 4 μg/ml). The M. marseillense isolates (CRM 694 and CRM 696) were highly resistant to amikacin (MIC, 8 μg/ml), and isolate CRM 695 showed intermediate levels of resistance to this drug (MIC, 4 μg/ml). All isolates were susceptible to clarithromycin (MIC, 1 to 2 μg/ml).
TABLE 2.
Antimicrobial susceptibilities of the NTM isolates recovered from sputum samples of CF patients in Rio de Janeiro, Brazil
| Patient | Isolate | Organism | MICa (μg/ml) |
||||||
|---|---|---|---|---|---|---|---|---|---|
| AMI | CEF | CIP | CLA | DOX | MOX | T/S | |||
| A | CRM 511 | M. abscessus subsp. abscessus | 8 (S) | 64 (I) | 8 (R) | 8 (R) | >32 (R) | 8 (R) | > 04/76 (R) |
| A | CRM 718 | M. abscessus subsp. abscessus | 32 (I) | 32 (I) | >16 (R) | 1 (S) | >32 (R) | 16 (R) | >08/152 (R) |
| A | CRM 740 | M. abscessus subsp. abscessus | 32 (I) | 128 (R) | >16 (R) | 32 (R) | >32 (R) | 16 (R) | > 04/76 (R) |
| B | CRM 641 | M. abscessus subsp. abscessus | 8 (S) | 256 (R) | 4 (R) | 4 (I) | >32 (R) | 16 (R) | >16/304 (R) |
| B | CRM 697 | M. abscessus subsp. abscessus | 16 (S) | 32 (I) | 16 (R) | 16 (R) | >32 (R) | 16 (R) | >16/304 (R) |
| B | CRM 720 | M. abscessus subsp. abscessus | 64 (R) | 64 (I) | >16 (R) | 16 (R) | >32 (R) | 64 (R) | >16/304 (R) |
| C | CRM 747 | M. abscessus subsp. bolletii | >128 (R) | 256 (R) | >16 (R) | 32 (R) | >32 (R) | 16 (R) | > 04/76 (R) |
| D | CRM 512 | M. abscessus subsp. bolletii | 8 (S) | 64 (I) | 8 (R) | 2 (S) | >32 (R) | 16 (R) | >16/304 (R) |
| D | CRM 640 | M. abscessus subsp. bolletii | 8 (S) | 64 (I) | 2 (I) | <0.5 (S) | >32 (R) | 32 (R) | >16/304 (R) |
| D | CRM 920 | M. abscessus subsp. bolletii | 8 (S) | 256 (R) | >16 (R) | <0.5 (S) | >32 (R) | 4 (R) | >16/304 (R) |
| E | CRM 473 | M. abscessus subsp. bolletii | 8 (S) | 64 (I) | 8 (R) | <0.5 (S) | >32 (R) | 16 (R) | >16/304 (R) |
| E | CRM 639 | M. abscessus subsp. bolletii | 8 (S) | 256 (R) | 16 (R) | <0.5 (S) | >32 (R) | 32 (R) | >16/304 (R) |
| F | CRM 836 | M. abscessus subsp. bolletii | 8 (S) | 32 (I) | >16 (R) | <0.5 (S) | >32 (R) | 32 (R) | > 04/76 (R) |
| F | CRM 901 | M. abscessus subsp. bolletii | 8 (S) | 64 (I) | >16 (R) | <0.5 (S) | >32 (R) | 32 (R) | > 04/76 (R) |
| H | CRM 569 | M. abscessus subsp. bolletii | 16 (S) | 128 (R) | 16 (R) | 64 (R) | >32 (R) | 32 (R) | > 04/76 (R) |
| H | CRM 642 | M. abscessus subsp. bolletii | 8 (S) | 128 (R) | 16 (R) | >64(R) | >32 (R) | 32(R) | > 04/76 (R) |
| H | CRM 719 | M. abscessus subsp. bolletii | >128 (R) | 64 (I) | >16 (R) | 32 (R) | >32 (R) | 128(R) | >16/304 (R) |
| H | CRM 723 | M. abscessus subsp. bolletii | >128 (R) | 128 (R) | >16 (R) | 32 (R) | >32(R) | 32(R) | >16/304 (R) |
| H | CRM 732 | M. abscessus subsp. bolletii | >128 (R) | 256 (R) | >16 (R) | 32 (R) | >32 (R) | 128 (R) | >16/304 (R) |
| H | CRM 835 | M. abscessus subsp. bolletii | >128 (R) | 64 (I) | >16 (R) | >64 (R) | >32 (R) | 32 (R) | >16/304 (R) |
| H | CRM 915 | M. abscessus subsp. bolletii | >128 (R) | 256 (R) | >16 (R) | >64 (R) | >32 (R) | 16 (R) | >16/304 (R) |
| H | CRM 916 | M. abscessus subsp. bolletii | >128 (R) | 64 (I) | >16 (R) | >64 (R) | >32 (R) | 32 (R) | >16/304 (R) |
| H | CRM 917 | M. abscessus subsp. bolletii | >128 (R) | 64 (I) | >16 (R) | >64 (R) | >32 (R) | 32 (R) | >16/304 (R) |
| H | CRM 927 | M. abscessus subsp. bolletii | >128 (R) | 64 (I) | >16 (R) | >64 (R) | >32 (R) | 16 (R) | >16/304 (R) |
| H | CRM 928 | M. abscessus subsp. bolletii | >128 (R) | 64 (I) | >16 (R) | >64(R) | >32 (R) | 256 (R) | >16/304 (R) |
| H | CRM 949 | M. abscessus subsp. bolletii | >128 (R) | 64 (I) | >8 (R) | >16 (R) | >32 (R) | >2 (I) | >16/304 (R) |
| H | CRM 950 | M. abscessus subsp. bolletii | >128 (R) | 64 (I) | >16 (R) | >16 (R) | >32 (R) | >2 (I) | >16/304 (R) |
| H | CRM 1009 | M. abscessus subsp. bolletii | >128 (R) | 64 (I) | >8 (R) | >16 (R) | >32 (R) | >2 (I) | >16/304 (R) |
| H | CRM 1010 | M. abscessus subsp. bolletii | >128 (R) | 64 (I) | >8 (R) | >16 (R) | >32 (R) | >2 (I) | >16/304 (R) |
| I | CRM 724 | M. fortuitum | 8 (S) | >256 (R) | 8 (R) | 16 (R) | >32 (R) | <2 (S) | > 04/76 (R) |
| I | CRM 725 | M. fortuitum | 8 (S) | >256 (R) | 8 (R) | 4 (I) | >32 (R) | <2 (S) | > 04/76 (R) |
| I | CRM 726 | M. fortuitum | <1 (S) | >256 (R) | 0.5 (S) | 16 (R) | 32 (R) | <2 (S) | > 04/76 (R) |
| J | CRM 803 | M. abscessus subsp. bolletii | <1 (S) | 64 (I) | 1 (S) | 32 (R) | <0.25 (S) | 16 (R) | > 04/76 (R) |
AMI, amikacin; CEF, cefoxitin; CIP, ciprofloxacin; CLA, clarithromycin; DOX, doxycycline; MOX, moxifloxacin; T/S, trimethoprim-sulfamethoxazole; R, resistant; S, susceptible; I, intermediate.
The M. abscessus subsp. bolletii isolate CRM 803 from patient J showed susceptibility to amikacin, ciprofloxacin, and doxycycline. Isolates from patient A initially presented susceptibility to one of the 7 drugs tested and evolved to complete nonsusceptibility over a period of 4 months. Isolates from patient B presented similar characteristics over a period of 15 months. For patient H, only the first 2 isolates were susceptible to one of the tested drugs, followed by 13 complete nonsusceptible isolates during the period of study.
A predominant genotype was found among the isolates of M. fortuitum, with 2 isolates (CRM 725 and CRM 726) sharing an identical profile and another isolate (CRM 724) with 95% similarity to the others. All isolates were obtained from the same patient, found nontypeable by PFGE, and analyzed by ERIC-PCR (Fig. 1).
FIG 1.
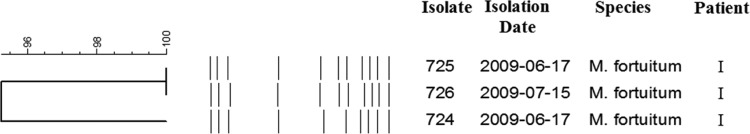
Dendrogram obtained from the automated analysis of the ERIC-PCR profiles of the M. fortuitum isolates, showing the similarity coefficients (as percentages). Dice's coefficient was used as the algorithm for the construction of the dendrogram.
Thirty M. abscessus spp. isolates were analyzed by PFGE, only and CRM 473, CRM 512, CRM 915, and CRM 949 were classified as nontypeable due to DNA degradation when we used PFGE or ERIC-PCR.
Based on PFGE analysis, two distinct genotypes were obtained among the six isolates of M. abscessus subsp. abscessus (Fig. 2). The isolates CRM 641 and CRM 697 presented an identical profile and were considered clones. Even though isolate CRM 720 was isolated from the same patient (B), it did not belong to the same clone, and it was classified within the same genotype, MAA 1. The isolates CRM 511, CRM 718, and CRM 740, obtained from the same patient (A), were identical and were classified as genotype MAA 2.
FIG 2.

Dendrogram obtained from the automated analysis of the PFGE profiles of the M. abscessus subsp. abscessus isolates, showing the similarity coefficients (as percentages). Dice's coefficient was used as the algorithm for the construction of the dendrogram.
Among 20 isolates of M. abscessus subsp. bolletii that were studied, five different genotypes were obtained (Fig. 3) among seven related different profiles. The isolates CRM 569, CRM 639, CRM 642, CRM 719, CRM 723, CRM 732, CRM 747, CRM 835, CRM 916, CRM 917, CRM 927, CRM 928, CRM 950, CRM 1009, and CRM 1010 were classified as genotype MAB 1. With the exception of isolate CRM 639, the genotype MAB 1 presented with identical profiles for all isolates. CRM 639 and CRM 747 were the only ones not isolated from the same patient. Genotype MAB 2 presented two distinctly related profiles. The isolates CRM 836 and CRM 901 were identical and were obtained from the same patient. Isolate CRM 803 and the reference strain CCUG 48898 presented unique genotypes, MAB 3 and MAB 4, respectively. We observed that genotype MAB 5 comprised CRM 640 and CRM 920, following the patient-specific profile. None of the CF clinical isolates presented a profile that was similar to the control strains. The D values for PFGE typing of MAA and MAB were 1.00 (nonapproximated 95% confidence interval [CNIA], 0.456 to 1.000) and 0.952 (95% CINA, 0.761 to 1.000), respectively.
FIG 3.
Dendrogram obtained from the automated analysis of the PFGE profiles of the M. abscessus subsp. bolletii isolates, showing the similarity coefficients (as percentages). Dice's coefficient was used as the algorithm for the construction of the dendrogram.
DISCUSSION
Several studies worldwide have reported the prevalence of NTM in CF patients. In France, a prevalence of 6.6% for NTM among 1,582 CF patients was reported (6). In Toronto, Canada, the prevalence of NTM among 98 CF patients between 6 and 18 years old was 6.1% (5). In Spain, the prevalence of NTM among 220 CF patients was 7.72%; however, the patient ages ranged between 6 and 74 years old (3). A study developed in Israel that reported a prevalence of 22.6% for NTM among 186 CF patients reported results that differed considerably from those of several other studies around the world (4). In our country of Brazil, we found only one study, which showed a prevalence of 11% for NTM among 54 CF adult patients (2). Our study here showed a prevalence of 7.75% for CF patients colonized/infected with NTM.
The PRA-hsp65 had a concordance of 86.11% with the results obtained from the partial sequencing of rpoB. The isolates CRM 720, CRM 747, and CRM 803 were identified by PRA-hsp65 as M. abscessus type I, whereas by rpoB sequencing they were identified as M. abscessus subsp. bolletii. The isolates identified as M. chimerae/M. intracellulare by PRA-hsp65 were identified as M. marseillense by rpoB sequencing. The isolate CRM 695 identified as M. fortuitum by PRA-hsp65 was the one that presented the largest discordance with the rpoB sequencing results, even after several repetitions. However, the PRA-hsp65 database does not contain a profile for M. timonense, which may have caused this difference in identification between the methods used.
The M. abscessus group was the predominant NTM in our study (eight patients), followed by MAC (three patients) and M. fortuitum (one patient). With the exception of patients C (M. marseillense and M. abscessus subsp. boletii) and patient I (M. fortuitum and M. timonense), who presented isolates of two different species, the remaining patients presented isolates of only one species, allowing a better investigation of clonality. These results were similar to those of previous studies in which the main species belonged to the M. abscessus group (7, 23, 24). However, our results differed from those of other studies in which most of the isolated species were MAC (3, 5). In addition, characterization of the microbiological profile of CF patients as developed by Paschoal et al. (2) does not identify NTM to the species level. Currently, CF NTM colonization/infection may be related to distinct NTM species prevalent in distinct countries, reinforcing the importance of species identification in therapeutic decision making.
Brown-Elliott et al. (25) reported that most of the strains of the M. abscessus group show resistance to doxycycline, ciprofloxacin, and moxifloxacin. Only one isolate of M. abscessus subsp. boletii, obtained from patient J, was susceptible to doxycycline (MIC, ≤ 0.25 μg/ml) and ciprofloxacin (MIC, 1 μg/ml). It is expected that the isolates belonging to M. abscessus obtained from CF patients may show resistance to amikacin and other aminoglycosides, as these drugs are commonly used for treatment of bacterial infections, although amikacin resistance is rare among M. abscessus isolates recovered from different sources worldwide.
Although multidrug-resistant NTM have been reported in studies involving CF patients (6, 7, 26), the present work shows the highest rates compared to other studies in the scientific literature. Nevertheless, even considering infections using the ATS criteria, only patient H presented with development of pulmonary disease without resolution to date. The majority of the isolates from our study (97.2%) were resistant to five or more antimicrobials, with the exception of isolate CRM 803, obtained from patient J. Fourteen M. abscessus subsp. bolletii isolates (13 from patient H and 1 from patient B) had amikacin MICs higher than 128 μg/ml, one M. abscessus subsp. abscessus isolate had a MIC of 64 μg/ml (patient C), and two isolates had MICs of 32 μg/ml (patient A). The first isolate from patient A showed susceptibility to amikacin; however, the two following isolates, obtained afterwards, showed intermediate resistance. The same was observed for patients C and H. The mechanisms for the acquisition of NTM resistance to amikacin are unknown. Nevertheless, mutations in specific regions of the rrs and rpsL genes may confer aminoglycoside resistance in mycobacteria (26, 27, 28).
We recovered only three MAC isolates, two M. marseillense (CRM 694 and CRM 696) and one M. timonense (CRM 695), and all of them were susceptible to clarithromycin. According to the CLSI 2011 guidelines, clarithromycin is the chosen drug for the treatment of MAC infections, followed by moxifloxacin. The drug resistance of MAC in CF patients is rare, which facilitates longer antimicrobial treatments (25). Other drugs, such as ethambutol and rifampin, are used in association with clarithromycin therapy. In some cases, amikacin is used together with clarithromycin. However, due to the long duration of the treatment, which may last longer than 6 months, and the nephrotoxic and ototoxic side effects caused by amikacin, this therapy has been abandoned (25, 28, 29). Furthermore, the present results, based on the breakpoints described by Siddiqi et al. (19), indicate that the therapy with amikacin, ethambutol, moxifloxacin, rifampin, or streptomycin may be ineffective due to the high amikacin MIC for isolates CRM 694 and CRM 696 (8 μg/ml) and the intermediate resistance found for other drugs.
According to the review published by Pitombo et al. (30), most M. fortuitum strains are susceptible to amikacin, cefoxitin, ciprofloxacin, imipenem, linezolid, and sulfamethoxazole-trimethoprim; however, M. fortuitum isolates from CF patients in the present study were resistant to cefoxitin, ciprofloxacin, doxycycline, and sulfamethoxazole-trimethoprim. Isolates CRM 724 and CRM 725 also showed resistance to clarithromycin. According to Brown-Elliott et al. (25), the M. fortuitum group presents sulfonamide susceptibility of 100%; however, all M. fortuitum isolates from CF patients in our study were resistant to sulfamethoxazole-trimethoprim, with MICs higher than 8/152 μg/ml.
ERIC-PCR is a simple molecular tool and can be used for genotyping mycobacteria. A study by Sampaio et al. (31) compared different genotyping techniques for 17 isolates of M. fortuitum from an outbreak of infection postmammoplasty, and in this comparison ERIC-PCR indicated clonal profiles that were identical to the gold standard technique (PFGE). ERIC-PCR is considered a fast and economic alternative to PFGE. In a study with 40 Ugandan children and teenagers with pulmonary infection caused by M. fortuitum, ERIC-PCR revealed the presence of a clonal group of three isolates, another group comprised of two isolates, and also 35 distinct profiles (32).
A clonal group of M. fortuitum was recovered from patient I and had over 95% similarity. It is interesting that even though they had the same genotypic restriction pattern, CRM 725 and CRM 726 showed different susceptibility profiles. Isolate CRM 724 showed the same susceptibility profile as CRM 725, as both were isolated from the same clinical sample. In conclusion, a single sputum sample presented two different types of colonies with slightly different genotypic profiles; the small colony named CRM 724 and the larger one named CRM 725. The isolation of CRM 726 occurred 30 days after the isolation of the cited isolates (CRM 724 and CRM 725) and had a profile identical to CRM 725. The susceptibility profile and the genotypic profile results from isolates obtained from this clinical case suggest multiclonal NTM colonization with the same species, which may represent recent genomic mutations in mycobacterial populations.
The PFGE results for the M. abscessus subsp. abscessus isolates revealed two distinct genotypes: MAA 1 and MAA 2. The MAA 1 PFGE pattern comprised three isolates from patient B and showed two identical strains (CRM 641 and CRM 697) and one other (CRM 720) with a similarity of 88%. The MIC data for these isolates suggest that the most recent isolated strain (CRM 720) has resistance to amikacin and has different PFGE patterns from the others. A recent study described a patient infected with M. abscessus subsp. bolletii that had acquired resistance to amikacin during therapy with the same drug (26). The genotype MAA 2 comprised 3 clonal isolates from patient A. However, the resistance profile was different among the three isolates. These aspects may indicate that the molecular basis involved in the alteration of susceptibility to drugs may not be related to the M. abscessus subsp. abscessus genotypic profile obtained from PFGE. Further studies are required for better understanding of this.
The PFGE results for isolates identified as M. abscessus subsp. bolletii were classified into five different genotypes (MAB 1 to 5). Among those five genotypes, MAB 1 represented most of the M. abscessus subsp. bolletii isolates (15). All the isolates from patient H had this genotype, as did isolate CRM 747 from patient C and CRM 639 obtained from patient E. CRM 639 had a profile that differed from the other isolates by only one band. After review of medical records, we verified that no other isolation of mycobacteria occurred from patients C and E up to the date we finished this study, suggesting that these bacteria may have represented the most transient microbiota of these patients. It was also very startling that the MAB 1 genotype was circulating among three patients and that this same clone remains, causing severe disease in patient H up to the present day (data not shown).
The genotype MAB 2 was comprised of isolates CRM 836 and CRM 901 isolated from patient D, with identical molecular and susceptibility profiles, which confirmed a patient-specific pattern. Similarly, the genotype MAB 5 was found for two clones isolated from the same patient (D), one isolated 18 months after the first isolation.
PFGE for MAA and MAB 2 were evaluated by using a discriminatory index, which presented values higher than 0.90. These results confirmed the elevated discriminatory power of this method for diversity studies of these species, as shown in previous studies (33, 34).
The data obtained in this work will contribute to a better comprehension of NTM colonization/infection of CF patients. The observed NTM characteristics are alarming, since most of the isolates circulating among the patients showed resistance to multiple drugs. Isolation of highly resistant strains from CF patients must be considered a significant threat to public health, mainly due to the paucity of alternative therapy or potentially untreatable disease. Based on these findings, it is highly recommended that CF patients be monitored for NTM infections.
These findings, which are unprecedented in a country with a high incidence of TB, reinforce the importance of systematic and routine research for the identification of mycobacteria to the species level and susceptibility evaluations of antimicrobials. Studies on monitoring of NTM transmission through respiratory equipment among CF patients may also be useful, to better understand rates of colonization and prevalence of these organisms in these settings.
ACKNOWLEDGMENTS
The Plataform DNA sequencing program (PDTIS/FIOCRUZ), Rio de Janeiro, Brazil, is acknowledged for performance of the rpoB sequencing procedures. We appreciate the collaboration with Alcon Laboratórios do Brasil Ltd. for the moxifloxacin donation.
This study was supported in part by the Fundação de Amparo à Pesquisa do Estado do Rio de Janeiro (FAPERJ; projects 103.225/2011, 103.287/2011, 110.272/2010, 110.761/2010, and 111.497/2008), the Conselho Nacional de Desenvolvimento Científico e Tecnológico (MCT/CNPq; projects 476536/2012-0, 473444/2010-0, and 567037/2008-8), and PDTIS-FIOCRUZ.
Footnotes
Published ahead of print 11 June 2014
REFERENCES
- 1.Marques E. 2011. Perfil microbiológico na fibrose cística. Rev. Hosp. Univ. Pedro Ernesto 10(4):23–35 http://revista.hupe.uerj.br/detalhe_artigo.asp?id=69 [Google Scholar]
- 2.Paschoal IA, de Oliveira Villalba W, Bertuzzo CS, Cerqueira EM, Pereira MC. 2007. Cystic fibrosis in adults. Lung 185:81–87. 10.1007/s00408-006-2597-0 [DOI] [PubMed] [Google Scholar]
- 3.Girón RM, Máiz L, Barrio I, Martínez MT, Salcedo A, Prados C. 2008. Nontuberculous mycobacterial infection in patients with cystic fibrosis: a multicenter prevalence study. Arch. Bronconeumol. 44:679–684 (In Spanish.) 10.1016/S1579-2129(09)60006-9 [DOI] [PubMed] [Google Scholar]
- 4.Levy I, Grisaru-Soen G, Lerner-Geva L, Kerem E, Blau H, Bentur L, Aviram M, Rivlin J, Picard E, Lavy A, Yahav Y, Rahav G. 2008. Multicenter cross-sectional study of nontuberculous mycobacterial infections among cystic fibrosis patients, Israel. Emerg. Infect. Dis. 14:378–384. 10.3201/eid1403.061405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Radhakrishnan DK, Yau Y, Corey M, Richardson S, Chedore P, Jamieson F, Dell SD. 2009. Non-tuberculous mycobacteria in children with cystic fibrosis: isolation, prevalence, and predictors. Pediatr. Pulmonol. 44:1100–1106. 10.1002/ppul.21106 [DOI] [PubMed] [Google Scholar]
- 6.Roux AL, Catherinot E, Ripoll F, Soismier N, Macheras E, Ravilly S, Bellis G, Vibet MA, Le Roux E, Lemonnier L, Gutierrez C, Vincent V, Fauroux B, Rottman M, Guillemot D, Gaillard JL, Hermann J-L, OMA Group 2009. Multicenter study of prevalence of nontuberculous mycobacteria in patients with cystic fibrosis in France. J. Clin. Microbiol. 47:4124–4128. 10.1128/JCM.01257-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Seddon P, Fidler K, Raman S, Wyatt H, Ruiz G, Elston C, Perrin F, Gyi K, Bilton D, Drobniewski F, Newport M. 2013. Prevalence of nontuberculous mycobacteria in cystic fibrosis clinics, United Kingdom, 2009. Emerg. Infect. Dis. 19:1128–1130. 10.3201/eid/1907.120615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Olivier KN, Weber DJ, Wallace RJ, Faiz AR, Lee JH, Zhang Y, Brown-Elliot BA, Handler A, Wilson RW, Schechter MS, Edwards LJ, Chakraborti S, Knowles MR, Nontuberculous Mycobacteria in Cystic Fibrosis Study Group 2003. Nontuberculous mycobacteria. I: multicenter prevalence study in cystic fibrosis. Am. J. Respir. Crit. Care Med. 167:828–834. 10.1164/rccm.200207-678OC [DOI] [PubMed] [Google Scholar]
- 9.Esther CR, Henry MM, Molina PL, Leigh MW. 2005. Nontuberculous mycobacterial infection in young children with cystic fibrosis. Pediatr. Pulmonol. 40:39–44. 10.1002/ppul.20222 [DOI] [PubMed] [Google Scholar]
- 10.Duarte RS, Lourenço MC, Fonseca LeS, Leão SC, Amorim ED, Rocha IL, Coelho FS, Viana-Niero C, Gomes KM, da Silva MG, Lorena NS, Pitombo MB, Ferreira RM, Garcia MH, de Oliveira GP, Lupi O, Vilaça BR, Serradas LR, Chebabo A, Marques EA, Teixeira LM, Dalcolmo M, Senna SG, Sampaio JL. 2009. Epidemic of postsurgical infections caused by Mycobacterium massiliense. J. Clin. Microbiol. 47:2149–2155. 10.1128/JCM.00027-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Huang TS, Lee SS, Hsueh PR, Tsai HC, Chen YS, Wann SR, Leu HS, Ko WC, Yan JJ, Yuan SZ, Chang FY, Lu JJ, Wang JH, Wang HK, Liu YC. 2008. Antimicrobial resistance of rapidly growing mycobacteria in western Taiwan: SMART program 2002. J. Formos. Med. Assoc. 107:281–287. 10.1016/S0929-6646(08)60088-1 [DOI] [PubMed] [Google Scholar]
- 12.Brown BA, Wallace RJ, Onyi GO, De Rosas V. 1992. Activities of four macrolides, including clarithromycin, against Mycobacterium fortuitum, Mycobacterium chelonae, and M. chelonae-like organisms. Antimicrob. Agents Chemother. 36:180–184. 10.1128/AAC.36.1.180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Binder AM, Adjemian J, Olivier KN, Prevots DR. 2013. Epidemiology of nontuberculous mycobacterial infections and associated chronic macrolide use among persons with cystic fibrosis. Am. J. Respir. Crit. Care Med. 188:807–812. 10.1164/rccm.201307-1200OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Broda A, Jebbari H, Beaton K, Mitchell S, Drobniewski F. 2013. Comparative drug resistance of Mycobacterium abscessus and M. chelonae isolates from patients with and without cystic fibrosis in the United Kingdom. J. Clin. Microbiol. 51:217–223. 10.1128/JCM.02260-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ministério da Saúde. 2008. Identificação de micobactérias, p 436 In de Sáude M. (ed), Manual Nacional de Vigilância Laboratorial da Tuberculose e outras Micobactérias, 1st ed. Ministério da Saúde, Brasilia, Brazil [Google Scholar]
- 16.Telenti A, Marchesi F, Balz M, Bally F, Böttger EC, Bodmer T. 1993. Rapid identification of mycobacteria to the species level by polymerase chain reaction and restriction enzyme analysis. J. Clin. Microbiol. 31:175–178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Adékambi T, Colson P, Drancourt M. 2003. rpoB-based identification of nonpigmented and late-pigmenting rapidly growing mycobacteria. J. Clin. Microbiol. 41:5699–5708. 10.1128/JCM.41.12.5699-5708.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Clinical and Laboratory Standard Institute. 2011. Susceptibility testing of Mycobacteria, Nocardiae, and other aerobic actinomycetes. Approved standard, 2nd ed., document M24–A2 CLSI, Wayne, PA: [PubMed] [Google Scholar]
- 19.Siddiqi SH, Heifets LB, Cynamon MH, Hooper NM, Laszlo A, Libonati JP, Lindholm-Levy PJ, Pearson N. 1993. Rapid broth macrodilution method for determination of MICs for Mycobacterium avium isolates. J. Clin. Microbiol. 31:2332–2338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Versalovic J, Koeuth T, Lupski JR. 1991. Distribution of repetitive DNA sequences in eubacteria and application to fingerprinting of bacterial genomes. Nucleic Acids Res. 19:6823–6831. 10.1093/nar/19.24.6823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hunter PR, Gaston MA. 1988. Numerical index of the discriminatory ability of typing systems: an application of Simpson's index of diversity. J. Clin. Microbiol. 26:2465–2466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Griffith DE, Aksamit T, Brown-Elliott BA, Catanzaro A, Daley C, Gordin F, Holland SM, Horsburgh R, Huitt G, Iademarco MF, Iseman M, Olivier K, Ruoss S, von Reyn CF, Wallace RJ, Winthrop K, ATS Mycobacterial Diseases Subcommittee, American Thoracic Society, Infectious Diseases Society of America 2007. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am. J. Respir. Crit. Care Med. 175:367–416. 10.1164/rccm.200604-571ST [DOI] [PubMed] [Google Scholar]
- 23.Sermet-Gaudelus I, Le Bourgeois M, Pierre-Audigier C, Offredo C, Guillemot D, Halley S, Akoua-Koffi C, Vincent V, Sivadon-Tardy V, Ferroni A, Berche P, Scheinmann P, Lenoir G, Gaillard JL. 2003. Mycobacterium abscessus and children with cystic fibrosis. Emerg. Infect. Dis. 9:1587–1591. 10.3201/eid0912.020774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Valenza G, Tappe D, Turnwald D, Frosch M, König C, Hebestreit H, Abele-Horn M. 2008. Prevalence and antimicrobial susceptibility of microorganisms isolated from sputa of patients with cystic fibrosis. J. Cyst. Fibros. 7:123–127. 10.1016/j.jcf.2007.06.006 [DOI] [PubMed] [Google Scholar]
- 25.Brown-Elliott BA, Nash KA, Wallace RJ. 2012. Antimicrobial susceptibility testing, drug resistance mechanisms, and therapy of infections with nontuberculous mycobacteria. Clin. Microbiol. Rev. 25:545–582. 10.1128/CMR.05030-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bryant JM, Grogono DM, Greaves D, Foweraker J, Roddick I, Inns T, Reacher M, Haworth CS, Curran MD, Harris SR, Peacock SJ, Parkhill J, Floto RA. 2013. Whole-genome sequencing to identify transmission of Mycobacterium abscessus between patients with cystic fibrosis: a retrospective cohort study. Lancet 381:1551–1560. 10.1016/S0140-6736(13)60632-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jnawali HN, Yoo H, Ryoo S, Lee KJ, Kim BJ, Koh WJ, Kim CK, Kim HJ, Park YK. 2013. Molecular genetics of Mycobacterium tuberculosis resistant to aminoglycosides and cyclic peptide capreomycin antibiotics in Korea. World J. Microbiol. Biotechnol. 29:975–982. 10.1007/s11274-013-1256-x [DOI] [PubMed] [Google Scholar]
- 28.Du Q, Dai G, Long Q, Yu X, Dong L, Huang H, Xie J. 2013. Mycobacterium tuberculosis rrs A1401G mutation correlates with high-level resistance to kanamycin, amikacin, and capreomycin in clinical isolates from mainland China. Diagn. Microbiol. Infect. Dis. 77:138–142. 10.1016/j.diagmicrobio.2013.06.031 [DOI] [PubMed] [Google Scholar]
- 29.Kasperbauer SH, Daley CL. 2008. Diagnosis and treatment of infections due to Mycobacterium avium complex. Semin. Respir. Crit. Care Med. 29:569–576. 10.1055/s-0028-1085708 [DOI] [PubMed] [Google Scholar]
- 30.Pitombo MB, Lupi O, Duarte RS. 2009. Infections by rapidly growing mycobacteria resistant to disinfectants: a national matter? Rev. Bras. Ginecol. Obstet. 31:529–533 (In Portugese.) 10.1590/S0100-72032009001100001 [DOI] [PubMed] [Google Scholar]
- 31.Sampaio JL, Viana-Niero C, de Freitas D, Höfling-Lima AL, Leão SC. 2006. Enterobacterial repetitive intergenic consensus PCR is a useful tool for typing Mycobacterium chelonae and Mycobacterium abscessus isolates. Diagn. Microbiol. Infect. Dis. 55:107–118. 10.1016/j.diagmicrobio.2006.01.006 [DOI] [PubMed] [Google Scholar]
- 32.Asiimwe BB, Bagyenzi GB, Ssengooba W, Mumbowa F, Mboowa G, Wajja A, Mayanja-Kiiza H, Musoke PM, Wobudeya E, Kallenius G, Joloba ML. 2013. Species and genotypic diversity of non-tuberculous mycobacteria isolated from children investigated for pulmonary tuberculosis in rural Uganda. BMC Infect. Dis. 13:88. 10.1186/1471-2334-13-88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Machado G, Matsumoto C, Chimara E, Duarte R, Freitas D, Palaci M, Hadad D, Lima K, Lopes ML, Ramos R, Campos C, Caldas P, Heym B, Leao SC. 4 June 2014. Comparison of a multilocus sequence typing scheme versus pulsed-field gel electrophoresis for typing Mycobacterium abscessus isolates. J. Clin. Microbiol. 10.1128/JCM.00688-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Matsumoto CK, Chimara E, Bombarda S, Duarte RS, Leão SC. 2011. Diversity of pulsed-field gel electrophoresis patterns of Mycobacterium abscessus type 2 clinical isolates. J. Clin. Microbiol. 49:62–68. 10.1128/JCM.01665-10 [DOI] [PMC free article] [PubMed] [Google Scholar]



