Abstract
Whole-genome sequencing was used to compare longitudinal isolates of Staphylococcus aureus that developed resistance to oxacillin (MIC up to 16 μg/ml). The mecA gene was absent. A novel 5-bp TATCC frameshift insertion in a gene encoding an ABC transporter similar to that of the teichoic acid translocation ATP-binding protein TagH and a 3-bp GCT nonframeshift insertion in the pdhA pyruvate dehydrogenase gene were detected in the oxacillin-resistant isolates.
CASE REPORT
An 81-year-old man with an automated implantable cardioverter defibrillator (AICD) and pacemaker (PM) presented with 1 day of fever and chills without localizing symptoms. His past medical history was significant for diabetes mellitus, deep vein thrombosis, coronary atherosclerotic disease with remote bypass grafting, and ischemic cardiomyopathy (ICM) with a third-degree atrial flutter and an atrioventricular block requiring AICD/PM. His initial PM had been implanted 12 years previously in the left chest wall. The PM generator (and not the PM leads) had been extracted 4 years previously due to malfunction and replaced with an AICD/PM in his right chest wall.
Two months before the current admission, he received a 4-week course of intravenous nafcillin at an outside facility for methicillin-susceptible Staphylococcus aureus (MSSA) bacteremia resulting from cellulitis of his left toe (see Table 1 for details). A transthoracic echo (TTE) and tagged nuclear scan of the toe were negative for endocarditis and osteomyelitis, respectively. Within 4 days of treatment, he had defervesced and demonstrated clinical improvement, and blood cultures were negative for MSSA. Two days after stopping the treatment, however, the fever resumed and he was noted to have recurrent MSSA bacteremia identified by the BD Phoenix automated microbiology system (BD Biosciences, Franklin Lakes NJ). Transesophageal echocardiography (TEE) failed to demonstrate vegetations on the AICD/PM leads or valves. He was prescribed 2 weeks of oral linezolid treatment followed by 2 weeks of cephalexin. His blood cultures again cleared rapidly within 3 days of antibiotic initiation, and he clinically improved. The patient completed the linezolid course, but he self-discontinued the cephalexin (Keflex) after 5 days. He was readmitted to the outside hospital, having had fever over the preceding 24 h but no pain over his spine, joints, or cardiac device site. Physical exam findings were normal, with the exception of a temperature of 102.0°F, a pulse of 100 beats per minute, and an audible 3/6 systolic murmur at the left sternal border. Bilateral AICD/PM pocket sites were without erythema, tenderness, or swelling, and no peripheral stigmata of endocarditis were noted. Blood cultures again grew MSSA, with an oxacillin MIC of 2 μg/ml and cefazolin MIC of <2 μg/ml, and intravenous nafcillin was resumed. A TEE was repeated and demonstrated vegetations on the two right atrial wires. The patient was transferred to our institution for extraction of the cardiac device.
TABLE 1.
Culture results and treatment time course of our patienta
| Day(s) | Culture | Treatment | Additional note(s) |
|---|---|---|---|
| 1, 3 | Blood cultures grew MSSA | i.v. nafcillin for 4 wk | Presenting complaint was fever and cellulitis; the source of the bacteremia was left toe cellulitis |
| 5 | Blood cultures showed no growth | By TTE, the EF was 25%; there were no vegetations; a nuclear scan of left foot revealed no osteomyelitis | |
| 36 | Blood cultures grew MSSA (isolate 1) | p.o. linezolid for 2 wk followed by p.o. cephalexin for 5 days (prescribed for 2 wk but self-discontinued by patient) | Presenting complaint was fever; by TEE, the EF was 25%; there were no vegetations |
| 39 | Blood cultures exhibited no growth | ||
| 62, 63 | Blood cultures grew MSSA (isolate 2) | i.v. vancomycin plus i.v. piperacillin-tazobactam for 2 days, followed by i.v. cefazolin for 5 days | Presenting complaint was fever; by TEE, the EF was 55%; there was right atrial vegetation on 2 pacer wires and possibly on the wire extending to the right ventricle |
| 70 | Blood cultures exhibited no growth | i.v. vancomycin for 45 days | |
| 72 | PM/AICD lead culture grew MRSA; the right generator pocket culture grew MRSA (isolate 3) | All AICD/PM leads and the generator were extracted; a temporary AICD/PM was implanted; on day 85, a permanent PM/AICD was reimplanted; at the 6-wk follow-up, the patient was clinically well and afebrile and exhibited no recurrence of bacteremia; at the 4-mo follow-up, the patient was clinically well and afebrile, and there was no recurrence of bacteremia |
i.v., intravenous; TTE, transthoracic echocardiogram; TEE, transesophageal echocardiogram; EF, ejection fraction; p.o., per os.
On transfer, repeat blood cultures were negative for bacterial growth. The patient underwent extraction of the AICD/PM and all device leads, with placement of a temporary dual-chamber AICD/PM in the right subclavian vein since the patient was PM dependent. On extraction, cultures from the AICD/PM generator pocket site and device leads were positive for methicillin-resistant S. aureus (MRSA), as detected by the MicroScan WalkAway plus (Siemens, Hoffman Estates, IL) automated susceptibility system using the Pos Combo 33 breakpoint panel. The treatment regimen was changed to intravenous vancomycin. After 2 weeks, the AICD/PM was reimplanted and the generator placed in a new, right-sided, subpectoral pocket, and he was discharged with 6 weeks of intravenous vancomycin treatment. At the 6-week follow-up, he denied fever and was clinically well, so the antibiotics were discontinued. At a 4-month reevaluation, he continued to feel well and had no recurrences of fever and no documented bacteremia.
Because the development of oxacillin resistance was noted by the Infectious Disease team caring for the patient, the two MSSA isolates (isolate 1 and isolate 2) from the most recent episodes of bacteremia were available and were obtained from the outside hospital. The MRSA isolate from the pacemaker pocket (isolate 3) was recovered in the clinical microbiology laboratory at our institution. Breakpoint testing for susceptibility to oxacillin and other antibiotics for each of the three isolates was repeated using the Pos Combo 33 Gram-positive identification/susceptibility panels and the MicroScan WalkAway plus instrument using both the Prompt inoculum preparation system and the turbidity standard technique for preparation of inocula. MICs were also determined by testing with fresh subcultures on two separate days using Sensititre GPALL1F standard susceptibility MIC plates (Trek Diagnostic Systems, Inc., Cleveland, OH), with manual inoculation and reading of results. Reference broth microdilution was performed in the laboratory of David Lonsway at the Centers for Disease Control and Prevention (CDC) in Atlanta, GA, according to CLSI guidelines. The results of susceptibility testing for these isolates are shown in Table 2. No differences were seen in the MICs obtained by MicroScan whether the Prompt or the turbidity inoculation system was used. We identified a progressive increase in the MICs of oxacillin, ampicillin, penicillin, and cefoxitin for the three isolates. The oxacillin MIC for isolate 3 at 16 μg/ml was 32 times higher than that for pretreatment isolate 1 (0.5 μg/ml indicates susceptibility) and was above the susceptibility breakpoint (≥4 μg/ml indicates resistance). The oxacillin MIC for isolate 2 was variable and tested resistant by MicroScan and the broth microdilution Sensititre panel but susceptible by reference broth microdilution and by the BD Phoenix system at the outside hospital.
TABLE 2.
Susceptibility testing results for β-lactam antibioticsa
| Isolate | Testb | Oxacillin MIC (μg/ml) | Interpretation | Ampicillin MIC (μg/ml) | Interpretation | Penicillin MIC (μg/ml) | Interpretation | Cefoxitin MIC (μg/ml) | Disk zone (mm) | Interpretation |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | MicroScan | ≤0.5 | S | |||||||
| Broth microdilution (Sensititre) | 0.5 | S | 1 | R | 1 | R | ||||
| Reference broth microdilution | 0.5 | S | 2 | R | 4 | 25 | S | |||
| 2 | MicroScan | >2 | R | |||||||
| Broth microdilution (Sensititre) | 4 | R | 2 | R | 4 | R | ||||
| Reference broth microdilution | 0.25 | S | 1 | 4 | 28 | S | ||||
| 3 | MicroScan | >2 | R | |||||||
| Broth microdilution (Sensititre) | >4 | R | 4 | R | 4 | R | ||||
| Reference broth microdilution | 16 | R | >2 | R | 8 | 19 | R |
R, resistant; S, susceptible.
In the MicroScan, MICs were the same regardless of inoculation method (Prompt inoculum versus turbidity technique). In the Sensititre assay, testing was done in replicate, with no difference in results.
Isolate 1 tested resistant to penicillin, with an MIC of 1 to 2 μg/ml, and the MIC was increased approximately 2-fold for isolate 3, with an MIC of 4 μg/ml. Isolate 2 was also resistant to penicillin, but the MIC was variable and tested at 4 μg/ml using the Sensititre panel and at 1 μg/ml by reference broth microdilution. Similarly, all isolates were resistant to ampicillin, but the MIC of ampicillin increased from 1 μg/ml for isolate 1 to 2 μg/ml for isolate 2 and to 4 μg/ml for isolate 3. The cefoxitin MIC was susceptible at 4 μg/ml for isolates 1 and 2 but resistant at 8 μg/ml for isolate 3. Cefoxitin results were confirmed by disk diffusion testing. All three isolates remained susceptible, with no increases in MICs, to all other antibiotics tested (chloramphenicol, daptomycin, gentamicin, linezolid, rifampin, trimethoprim sulfamethoxazole, quinupristin-dalfopristin, tetracycline, erythromycin, vancomycin, ciprofloxacin, levofloxacin, moxifloxacin, tigecycline, and clindamycin).
All three isolates tested negative in the Oxoid PBP2′ latex agglutination test (Remel Inc., Lenexa, KS) and did not contain the mecA gene, as determined by a laboratory-developed PCR assay (1).
Oxacillin and cefoxitin induction studies were done at the CDC to determine whether prior exposure to these antibiotics could significantly increase the oxacillin or cefoxitin MICs. Suspensions (0.5 McFarland standard) of each isolate were prepared from the edge of the growth around the oxacillin and cefoxitin disk zones. Corresponding suspensions were inoculated onto Mueller-Hinton agar plates with a 1-μg oxacillin disk or a 30-μg cefoxitin disk and incubated at 35°C for 24 h. The resulting zone diameters were measured, and this process was repeated for four consecutive days. A significant change was defined as a change from the CLSI susceptibility category to the intermediate or resistance category. Isolate 1 showed no significant changes in oxacillin zone diameter or MIC after 4 days of induction and remained susceptible throughout the induction period. Isolate 2 produced colonies with a progressively smaller zone diameter, which corresponded to an interpretation of intermediate after two rounds of induction and resistant after four rounds.
To determine if the three isolates represented the same strain or different strains, they were submitted to ARUP Laboratories (Salt Lake City, UT) for genomic analysis by restriction digestion using SmaI, followed by pulsed-field gel electrophoresis. All three S. aureus isolates were determined to have indistinguishable DNA fingerprints.
Whole-genome sequencing was used to compare the three isolates. Genomic DNA from each isolate was prepared using the Wizard genomic DNA purification kit (Promega, Madison, WI) with modifications in steps 3 to 5, as follows: cell pellets were resuspended in 300 μl of Tris-EDTA (TE) buffer, 50 μg/ml lysostaphin was used as the lytic enzyme, and samples were incubated at 37°C for 45 min. Sequencing of the paired-end genomic libraries was performed on an Illumina HiSeq 2000 platform using standard chemistry and a standard protocol (Illumina Inc., San Diego, CA). Multilocus sequence typing (MLST) of the isolates using their whole-genome sequence data identified all three isolates as MLST sequence type 5 (ST5), with identical DNA sequences at all seven loci (2). Low-quality sequences (average Phred quality score, <20) were discarded using a stand-alone version of PRINSEQ v0.20.4 (3), and the remaining reads were mapped against an ST5 reference genome, S. aureus N315 (NCBI GenBank accession number NC_002745) using the Burrows-Wheeler short-read aligner (4). Single nucleotide polymorphisms (SNPs) and insertion deletions (indels) were called using the Genome Analysis Toolkit (GATK) pipeline (5). An SNP or indel was considered true if that position contained at least 10 high-quality reads and more than 90% of them supported an alternate allele different from the reference base. The nucleotide regions corresponding to S. aureus pathogenicity islands SaPIn1, SaPIn2, and SaPIn3 (from S. aureus strain N315) and prophage ϕN315, which were missing from the sequenced strains, and the positions within the repetitive regions (any repeated unit of a copy number equal to or greater than 5 bp) were excluded from calling SNPs.
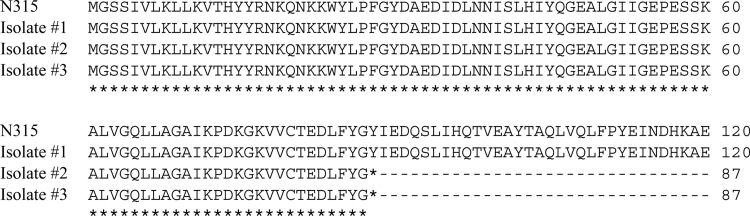
Comparative analysis of the whole-genome sequences revealed that isolates 2 and 3 differed from their parent strain (isolate 1) by a 5-bp TATCC frameshift insertion mutation in the putative gene encoding an ABC transporter similar to the teichoic acid translocation ATP-binding protein TagH (SA1688 locus in the N315 genome). This led to the production of a truncated protein that was only 87 amino acids long instead of the 505-amino-acid-long wild-type protein (Fig. 1). Isolate 3 had an additional nonframeshift insertion mutation of 3 bp, GCT, at codon 324 in the pyruvate dehydrogenase E1 component alpha subunit gene pdhA (SA0943-1 locus in the N315 genome). In addition to having the strain-specific changes mentioned above, all three isolates differed from the reference N315 genome by a common set of 163 SNPs (117 in the coding region and 46 in the intergenic region) and 11 indels (2 in the coding region and 9 in the intergenic region). All three isolates harbored blaZ genes, suggesting that they were capable of producing a β-lactamase enzyme. Whole-genome sequence results also confirmed that none of the isolates contained the mecA gene.
FIG 1.
Partial protein sequence alignment showing truncated ABC transporter sequence in isolates 2 and 3. The wild-type sequence, as in the N315 reference sequence, and the isolate 1 sequence is 505 amino acids long, whereas in oxacillin-resistant isolates 2 and 3, it is truncated at amino acid position 87 due to a frameshift insertion mutation.
Resistance to oxacillin in S. aureus is typically caused by the acquisition of a mobile genetic element, the staphylococcal cassette chromosome mec (SCCmec), which encodes a penicillin-binding protein, PBP2a, that has low binding affinity for methicillin and other β-lactam antibiotics (6, 7). Oxacillin resistance in S. aureus isolates lacking a mecA gene is infrequently reported. Known mechanisms of non-mecA-mediated oxacillin resistance include hyperproduction of blaZ-encoded β-lactamase (8), overexpression or modification of normal constitutive PBP genes (9–11), the presence of a methicillinase (12), or the expression of the divergent mecA homologue mecC (13).
The large census population numbers of bacteria in infections with S. aureus allow them to develop spontaneous mutations during the course of treatment (14). Conditions that support generation of a persistent population of bacteria, such as incubation in the presence of subinhibitory concentrations of an antibiotic at the site of infection, complex or chronic infections requiring a long duration of treatment, or repeated administration of antibiotics because of relapse or reinfection, are particularly conducive to the development of antibiotic-resistant mutants (15, 16).
Identification of the same ABC transporter gene mutation in the two breakthrough isolates supports its involvement in β-lactam MIC increases. Although the interactions are complex and not completely defined, there is evidence that the teichoic acid and peptidoglycan biosynthetic pathways in S. aureus are connected, and there are reports of an as-yet poorly defined functional interaction between teichoic acids and β-lactam antibiotics (17, 18). That oxacillin resistance was detected in some clinical susceptibility assays and undetected in others in the first breakthrough isolate may be related to the ability of the resistance to be induced after several rounds of replication in the presence of antibiotic. The additional mutation detected in the pdhA gene in the second breakthrough isolate was associated with stable oxacillin resistance. We do not have a ready explanation for how this mutation may function to enhance oxacillin resistance. The comparative genomics analysis between resistant S. aureus isolates and the susceptible parent strain described here provides leads for future functional genomics studies to uncover the specific mechanisms underlying the observed emergence of antibiotic resistance.
Nucleotide sequence accession number.
The raw sequence reads from the project have been deposited in the National Center for Biotechnology Information (NCBI) Sequence Read Archive (SRA) database under accession number SRP042337.
Footnotes
Published ahead of print 21 May 2014
REFERENCES
- 1.Limbago B, Fosheim GE, Schoonover V, Crane CE, Nadle J, Petit S, Heltzel D, Ray SM, Harrison LH, Lynfield R, Dumyati G, Townes JM, Schaffner W, Mu Y, Fridkin SK. 2009. Characterization of methicillin-resistant Staphylococcus aureus isolates collected in 2005 and 2006 from patients with invasive disease: a population-based analysis. J. Clin. Microbiol. 47:1344–1351. 10.1128/JCM.02264-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Inouye M, Conway TC, Zobel J, Holt KE. 2012. Short read sequence typing (SRST): multi-locus sequence types from short reads. BMC Genomics 13:338–338. 10.1186/1471-2164-13-338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schmieder R, Edwards R. 2011. Quality control and preprocessing of metagenomic datasets. Bioinformatics 27:863–864. 10.1093/bioinformatics/btr026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Li H, Durbin R. 2010. Fast and accurate long-read alignment with Burrows-Wheeler transform. Bioinformatics 26:589–595. 10.1093/bioinformatics/btp698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McKenna A, Hanna M, Banks E, Sivachenko A, Cibulskis K, Kernytsky A, Garimella K, Altshuler D, Gabriel S, Daly M, DePristo MA. 2010. The Genome Analysis Toolkit: a MapReduce framework for analyzing next-generation DNA sequencing data. Genome Res. 20:1297–1303. 10.1101/gr.107524.110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Malachowa N, DeLeo FR. 2010. Mobile genetic elements of Staphylococcus aureus. Cell Mol. Life Sci. 67:3057–3071. 10.1007/s00018-010-0389-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Deurenberg RH, Vink C, Kalenic S, Friedrich AW, Bruggeman CA, Stobberingh EE. 2007. The molecular evolution of methicillin-resistant Staphylococcus aureus. Clin. Microbiol. Infect. 13:222–235. 10.1111/j.1469-0691.2006.01573.x [DOI] [PubMed] [Google Scholar]
- 8.Barg N, Chambers H, Kernodle D. 1991. Borderline susceptibility to antistaphylococcal penicillins is not conferred exclusively by the hyperproduction of beta-lactamase. Antimicrob. Agents Chemother. 35:1975–1979. 10.1128/AAC.35.10.1975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Georgopapadakou NH, Smith SA, Bonner DP. 1982. Penicillin-binding proteins in a Staphylococcus aureus strain resistant to specific beta-lactam antibiotics. Antimicrob. Agents Chemother. 22:172–175. 10.1128/AAC.22.1.172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tomasz A, Drugeon HB, de Lencastre HM, Jabes D, McDougall L, Bille J. 1989. New mechanism for methicillin resistance in Staphylococcus aureus: clinical isolates that lack the PBP 2a gene and contain normal penicillin-binding proteins with modified penicillin-binding capacity. Antimicrob. Agents Chemother. 33:1869–1874. 10.1128/AAC.33.11.1869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Henze UU, Berger-Bachi B. 1995. Staphylococcus aureus penicillin-binding protein 4 and intrinsic beta-lactam resistance. Antimicrob. Agents Chemother. 39:2415–2422. 10.1128/AAC.39.11.2415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Massidda O, Montanari MP, Varaldo PE. 1992. Evidence for a methicillin-hydrolysing beta-lactamase in Staphylococcus aureus strains with borderline susceptibility to this drug. FEMS Microbiology Lett. 71:223–227 [DOI] [PubMed] [Google Scholar]
- 13.Laurent F, Chardon H, Haenni M, Bes M, Reverdy M-E, Madec J-Y, Lagier E, Vandenesch F, Tristan A. 2012. MRSA harboring mecA variant gene mecC, France. Emerg. Infect. Dis. 18:1465–1467. 10.3201/eid1809.111920 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mwangi MM, Wu SW, Zhou Y, Sieradzki K, de Lencastre H, Richardson P, Bruce D, Rubin E, Myers E, Siggia ED, Tomasz A. 2007. Tracking the in vivo evolution of multidrug resistance in Staphylococcus aureus by whole-genome sequencing. Proc. Natl. Acad. Sci. U. S. A. 104:9451–9456. 10.1073/pnas.0609839104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Maclean RC, Hall AR, Perron GG, Buckling A. 2010. The evolution of antibiotic resistance: insight into the roles of molecular mechanisms of resistance and treatment context. Discov. Med. 10:112–118 [PubMed] [Google Scholar]
- 16.Johnson PJT, Levin BR. 2013. Pharmacodynamics, population dynamics, and the evolution of persistence in Staphylococcus aureus. PLoS Genet. 9:e1003123. 10.1371/journal.pgen.1003123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brown S, Xia G, Luhachack LG, Campbell J, Meredith TC, Chen C, Winstel V, 7 Gekeler C, Irazoqui JE, Peschel A, Walker S. 2012. Methicillin resistance in Staphylococcus aureus requires glycosylated wall teichoic acids. Proc. Natl. Acad. Sci. U. S. A. 109:18909–18914. 10.1073/pnas.1209126109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bernal P, Zloh M, Taylor PW. 2009. Disruption of d-alanyl esterification of Staphylococcus aureus cell wall teichoic acid by the β-lactam resistance modifier (−)-epicatechin gallate. J. Antimicrob. Chemother. 63:1156–1162. 10.1093/jac/dkp094 [DOI] [PMC free article] [PubMed] [Google Scholar]