Abstract
The antiphagocytic capsule of Bacillus anthracis is a major virulence factor. We hypothesized that it may also mediate virulence through inhibition of the host's immune responses. During an infection, the capsule exists attached to the bacterial surface but also free in the host tissues. We sought to examine the impact of free capsule by assessing its effects on human monocytes and immature dendritic cells (iDCs). Human monocytes were differentiated into iDCs by interleukin-4 (IL-4) and granulocyte-macrophage colony-stimulating factor (GM-CSF) over 7 days in the presence of capsule derived from wild-type encapsulated B. anthracis Ames (WT) or a control preparation from an isogenic B. anthracis Ames strain that produces only 2% of the capsule of the WT (capA mutant). WT capsule consistently induced release of IL-8 and IL-6 while the capA mutant control preparation elicited either no response or only a minimal release of IL-8. iDCs that were differentiated in the presence of WT capsule had increased side scatter (SSC), a measure of cellular complexity, when assessed by flow cytometry. iDCs differentiated in the presence of WT capsule also matured less well in response to subsequent B. anthracis peptidoglycan (Ba PGN) exposure, with reduced upregulation of the chemokine receptor CCR7, reduced CCR7-dependent chemotaxis, and reduced release of certain cytokines. Exposure of naive differentiated control iDCs to WT capsule did not alter cell surface marker expression but did elicit IL-8. These results indicate that free capsule may contribute to the pathogenesis of anthrax by suppressing the responses of immune cells and interfering with the maturation of iDCs.
INTRODUCTION
Bacillus anthracis is the causative agent of anthrax and an important biothreat agent. The virulence of B. anthracis derives primarily from the products of two plasmids, pX01, which carries the genes for lethal toxin and edema toxin (1), and pX02, which carries the genes required for synthesizing capsule (2, 3). B. anthracis capsule covers the outer surface of the bacilli and protects them from phagocytosis by immune cells (4–6). While most bacterial capsules are polysaccharides, B. anthracis capsule is a homopolymer composed entirely of d-glutamic acid residues connected by γ linkages (7). These unusual attributes make B. anthracis capsule both relatively resistant to degradation by mammalian proteases and a poorly immunogenic thymus-independent type 2 antigen (8, 9).
In in vitro broth culture and during infection, B. anthracis bacilli release capsule fragments. These free capsule fragments can accumulate to significant concentrations in the blood of moribund animals (7). Serum concentrations of B. anthracis capsule greater than 500 μg/ml have been reported in mice (10), and concentrations greater than 1 mg/ml have been reported in rhesus macaques (11). Concentrations in local lesions could potentially be as high or even higher. Capsule free from the bacillus has been demonstrated to accumulate in animal tissues (12, 13). Early experiments with capsule recovered from the plasma and exudates of moribund guinea pigs showed that purified capsule could enhance the virulence of spores when coinjected with them (14). More recently, coinjection of purified capsule with an attenuated mutant of B. anthracis restored its virulence (15). We have also observed that free capsule can inhibit the antimicrobial activity of human defensins (D. K. O'Brien and A. M. Friedlander, unpublished data). Given this evidence that free capsule as well as bacillus-bound capsule contributes to virulence, we hypothesized that the shed capsule might contribute to pathogenesis by interfering with innate immune responses as has been observed with the anthrax toxins (16). Therefore, we sought to examine the effect of free capsule on human monocytes and immature dendritic cells (iDCs). Capsule released by B. anthracis into the medium during in vitro growth was harvested from broth culture supernatants of wild-type encapsulated B. anthracis Ames (WT). Human monocytes were differentiated into iDCs in the presence of the purified free capsule over the course of 7 days. Cytokine levels were measured on days 3 and 7 to assess the nature of the response over time. We found that WT capsule consistently elicited interleukin-8 (IL-8) and IL-6 on days 3 and 7. The resulting iDCs had an altered phenotype showing increased side scatter (SSC) when they were assessed by flow cytometry. Furthermore, maturation of these iDCs in response to B. anthracis peptidoglycan (Ba PGN) was impaired as indicated by reduced CCR7 expression, reduced chemotaxis toward the CCR7 ligands CCL19 and CCL21, and reduced cytokine secretion. These results indicate that capsule shed from B. anthracis acts on cells of the human innate immune system, inhibiting the function of DCs, and thus may play a role in the pathogenesis of anthrax.
MATERIALS AND METHODS
B. anthracis strains.
B. anthracis Ames was from the USAMRIID collection. An isogenic capsule-reduced strain with inactivated capA (capA mutant) was derived from B. anthracis Ames as follows. A 1.24-kb DNA fragment containing the capA gene was amplified from the B. anthracis Ames genome. The capA gene was inactivated by the insertion of the nonpolar kanamycin fragment (17) into the BamHI site located 700 bp downstream of the ATG site and cloned into the Escherichia coli/Bacillus subtilis shuttle vector pEO-3 (18, 19). The resulting plasmid, designated pKLM2, was passaged through the dam dcm strain of E. coli GM2683. To construct the isogenic capA mutant strain of B. anthracis, pKLM2 was first transformed into B. anthracis Ames by electroporation and selected by growth in the presence of erythromycin at 30°C. Next, the plasmid containing the insertionally inactivated capA gene was integrated into pXO2 by selection and growth at 42°C in the presence of kanamycin (18). To resolve the plasmid from pX02, mutants were selected as previously described (20) and confirmed by PCR analysis.
Capsule preparation.
Capsule was harvested from broth culture supernatants of the WT and capA mutant B. anthracis strains as follows. A single colony was used to inoculate brain heart infusion (BHI) broth. After overnight growth on a shaker at 37°C, the culture was diluted 1:1,000 in BHI broth containing 0.8% (wt/vol) sodium bicarbonate in a flask with a filter cap. Broth cultures were incubated at 37°C for 20 to 24 h in a shaker incubator with an atmosphere containing 20% carbon dioxide, and then the bacterial cells were pelleted at 3,000 × g for 30 min. Supernatants were filtered (0.2 μm), brought to a final concentration of 1 mM magnesium chloride and 2.5 U/ml Benzonase (EMD Chemicals, Gibbstown, NJ), and incubated overnight at 4°C. Trichloroacetic acid was then added to 10% (vol/vol). After 1 h on ice, mixtures were centrifuged as before, and the supernatant was neutralized with 10% (wt/vol) sodium acetate powder. Three volumes of 95% ethanol was added to precipitate the capsule overnight at −20°C. After centrifugation as before, the capsule-containing pellets were washed three times with 70% ethanol. The pellets from WT and capA mutant cultures were dried overnight and then dissolved in equivalent volumes of endotoxin-free 100 mM sodium phosphate buffer. Equivalent cultures of WT and capA mutant B. anthracis were grown and harvested in parallel. The preparation from the capsule-reduced capA mutant strain was used as a control for any material that copurified during the purification process. The capsule preparations were shown to be free of DNA after being run on agarose gels and stained with ethidium bromide and to be free of protein after being run on SDS-PAGE gels and stained with Coomassie blue. All capsule preparations were tested for endotoxin contamination using a Limulus amebocyte lysate (LAL) endpoint chromogenic assay (Lonza, Walkersville, MD) before use in cell culture.
Capsule quantitation was based upon the WT preparation. The preparation from the capA mutant strain, which was cultured and purified in parallel, was resuspended in an equivalent volume. The capA mutant strain produces 2% of the amount of capsule produced by the WT strain as determined by amino acid analysis (data not shown). The relative amounts of capsule in the two strains were also analyzed by agarose gel electrophoresis as previously described (21).
Peptidoglycan testing.
The WT and capA mutant capsule preparations were tested for peptidoglycan by Immunetics, Inc. (Boston, MA), using the BacTx assay.
Ba PGN.
Ba PGN was purified similarly to the method of Candela and Fouet (22). B. anthracis Ames was grown overnight on Trypticase soy agar at 37°C. A single colony was used to inoculate BHI broth for overnight growth in a 37°C shaker incubator. Ten microliters was inoculated into 100 ml nutrient broth with yeast extract (8 g nutrient broth, 3 g yeast extract per liter) without added bicarbonate or carbon dioxide. After overnight growth in a 37°C shaker incubator, bacteria were centrifuged at 2,500 × g for 30 min. The pellet was resuspended in 20 ml of TNS (50 mM Tris, pH 7.4, 150 mM NaCl, 1% SDS) and put in a 100°C water bath for 10 min. The boiled bacteria were pelleted, resuspended, and boiled a second time. After the second round of boiling, the bacteria were pelleted and then resuspended in 50 mM Tris, pH 7.4. The suspension was sonicated, frozen overnight at −70°C, and ultracentrifuged at 40,000 × g for 20 min. The pellet was resuspended in TNS, boiled, and ultracentrifuged again. The resulting pellet was resuspended in 10 ml 50 mM Tris, pH 7.4, with 200 μg proteinase K and incubated overnight at 4°C. One milliliter of 10% SDS was added, and the sample was boiled and washed four times with sterile water for injection. The sample was then dried in a hood and resuspended in sterile water. Amino acid analysis results for Ba PGN (Alphalyse Inc., Palo Alto, CA) were very similar to those reported by Langer et al. (23). PGN purified from B. anthracis Ames did not have more glutamic acid than did PGN purified from B. anthracis ΔANR (pX01− pX02−), which lacks the capsule, indicating that there is no significant amount of capsule associated with the purified Ba PGN (data not shown). All Ba PGN preparations were tested for endotoxin contamination using an LAL endpoint chromogenic assay as described above before use in cell culture.
Monocyte-DC cultures.
Human monocytes were purified by Percoll density gradient centrifugation from leukopacks obtained from the Department of Transfusion Medicine (Clinical Center, National Institutes of Health, Bethesda, MD). Purified monocytes were washed three times with sterile Dulbecco's phosphate-buffered saline (Gibco, Grand Island, NY) and differentiated into iDCs by cultivation at 37°C in 5% CO2 in the following medium for 7 days: RPMI 1640 (Mediatech, Manassas, VA) supplemented with 2 mM glutamine (Gibco), 25 mM HEPES (Gibco), 10% fetal bovine serum (FBS) (HyClone, Logan, UT), 50 μM β-mercaptoethanol, 50 ng/ml IL-4 (Peprotech, Rocky Hill, NJ), and 50 ng/ml granulocyte-macrophage colony-stimulating factor (GM-CSF) (Peprotech). Experimental cultures included up to 1,000 μg/ml of B. anthracis WT capsule in 100 mM sodium phosphate buffer. Control cells were cultured without capsule in the presence of an equivalent volume of 100 mM sodium phosphate buffer or in differentiation medium alone. Ten nanograms of lipopolysaccharide per milliliter (from E. coli 055:B5; Sigma, St. Louis, MO) diluted in 100 mM sodium phosphate buffer was used as a positive control in the 7-day differentiation experiments. On days 3 and 5, 50% of the medium was replaced with fresh differentiation medium supplemented with the same concentration of test material in order to maintain the same conditions throughout the experiment. On day 7 when the monocytes had differentiated into iDCs, either the experiment was concluded or 50% of the medium was replaced with fresh medium plus 1 μg/ml Ba PGN or 100 ng/ml LPS to induce maturation of the iDCs to mature DCs (mDCs). For experiments with naive differentiated iDCs, cells were cultured in differentiation medium alone for 7 days with feeds on days 3 and 5, stimulation on day 7, and harvest of medium samples on day 9.
Cytokine measurement.
Duplicate wells of medium samples were assayed for human IL-1β, IL-6, IL-8, IL-10, IL-12p70, IL-2, gamma interferon (IFN-γ), GM-CSF, and tumor necrosis factor alpha (TNF-α) using human proinflammatory 9-plex platform ultrasensitive plates (Meso Scale Discovery, Gaithersburg, MD). The plates were analyzed using a Sector Imager 2400 (Meso Scale Discovery) according to the manufacturer's protocol. Data are shown as the mean pg/ml ± standard error of the mean (SEM) or as fold increases in cytokines in cells exposed to capsule compared to untreated control cells. IL-23 was measured using the human IL-23 enzyme-linked immunosorbent assay (ELISA) Ready SET Go! kit (eBioscience, San Diego, CA) as mean pg/ml ± SEM according to the manufacturer's protocol. Statistical significance of the data presented as mean pg/ml ± SEM was determined by two-tailed t tests comparing the means for the treated samples to those of the untreated control (GraphPad Software, La Jolla, CA). A P value of <0.05 was considered significant.
Flow cytometry.
After differentiation of monocytes to iDCs or maturation of iDCs to mDCs, the cells were stained with antibodies specific for human major histocompatibility complex class I (MHC I), MHC II, CD83, or CCR7 or with isotype control antibodies purchased from BD Pharmingen (San Jose, CA). Flow cytometry experiments were run in a FACSCalibur cytometer (BD Biosciences, Billerica, MA), and the data were analyzed using Cell Quest Pro software (BD Biosciences). Statistical significance of the data was determined by two-tailed t tests comparing average mean fluorescence intensities (MFIs) for the capsule-treated samples to those for the controls (GraphPad Software). Statistical significance of differences in SSC between capsule-treated cells and controls was similarly determined by two-tailed t tests. A P value of <0.05 was considered significant.
Chemotactic activity assay.
After maturation of iDCs to mDCs, cells were pelleted and resuspended in binding medium (RPMI 1640 supplemented with 1% bovine serum albumin) at 5 × 105 live cells/ml. Cells were added to the inner chambers of transwells with 5-μm-pore polycarbonate membranes (Corning, Corning, NY). Binding medium alone or supplemented with 10 ng/ml recombinant human CCL19 or recombinant human CCL21 (Peprotech, Rocky Hill, NJ) was added to the outer chamber. Cells were incubated in the transwells for 4.5 h at 37°C and 5% CO2. The transwells were then aspirated and transferred to fresh wells containing cell detachment solution (Cell Biolabs, Inc., San Diego, CA) and incubated for 30 min at 37°C and 5% CO2. The transwells were then discarded. Duplicate samples of the combined medium and cell detachment solution containing the migrated cells for each cell treatment were transferred to a black-walled 96-well plate (Corning) and lysed with lysis buffer (Cell Biolabs, Inc.) supplemented with CyQuant GR dye (Life Technologies, Eugene, OR). After 20 min of incubation at room temperature, fluorescence was read at 480 nm/520 nm in a SpectraMax M5 fluorescence plate reader (Molecular Devices, Sunnyvale, CA). Chemotactic index was calculated by dividing fluorescence units observed in the presence of the ligands by fluorescence units observed in the absence of ligand. P values were determined by comparing the means of the chemotactic indices for the mDCs of all four donors matured with or without WT capsule in a two-tailed t test. A P value of <0.05 was considered significant.
RESULTS
B. anthracis capsule elicits a distinct cytokine response from human monocytes over the course of differentiation into iDCs.
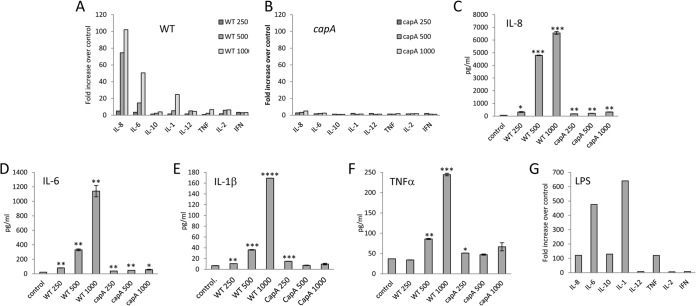
We first sought to determine whether or not B. anthracis capsule could elicit a cytokine response from differentiating human monocytes. Human monocytes were cultured in medium supplemented with human IL-4 and GM-CSF to promote their differentiation into iDCs over the course of 7 days. Capsule prepared from the WT strain of B. anthracis at concentrations of 250 to 1,000 μg/ml or equivalent amounts of the preparation from the capA mutant strain were included in the differentiation medium. The capA mutant strain produced only 2% of the amount of capsule of the WT strain as determined by amino acid analysis (data not shown), and the relative amounts of capsule in the two preparations are shown in Fig. 1. Cells cultured with equivalent volumes of the sodium phosphate control buffer or 10 ng/ml LPS served as negative and positive controls, respectively. Medium samples collected on days 3 and 7 were assayed for human IL-8, IL-6, IL-10, IL-1β, IL-12p70, TNF-α, IL-2, and IFN-γ to assess responses of the cells to the capsule over time. The results for a representative donor are shown in Fig. 2. The WT capsule consistently elicited statistically significant IL-8 and IL-6 responses on day 3 (Fig. 2A, C, and D) in all six donors tested at 500 μg/ml (P range, <0.01 to <0.0001 for IL-8 and for IL-6). In contrast, an equivalent amount of the capA mutant preparation, which contained all the potential copurifying material derived from the broth culture and harvest process, elicited only very low levels of IL-8 (Fig. 2B and C) from the six donors tested at 500 μg/ml (P range, <0.05 to <0.0001). The capA mutant preparation also elicited very low levels of IL-6 (Fig. 2B and D) from five out of six donors tested at 500 μg/ml (P range, <0.05 to <0.001), including the one shown in Fig. 2. Three out of six donors, including the one shown in Fig. 2, also exhibited significant release of IL-1β in response to 500 μg/ml WT capsule on day 3 (Fig. 2A and E, P range, <0.01 to <0.001), but only one treated with an equivalent amount of the capA mutant preparation did (P < 0.05). Four out of six donors exhibited significant release of TNF-α in response to 500 μg/ml WT capsule on day 3 (Fig. 2A and F; P range, <0.01 to <0.001), while only three of six treated with an equivalent amount of the capA mutant preparation did (Fig. 2B and F; P range, <0.05 to <0.01). The cytokine release elicited by WT capsule was in all cases dramatically greater than that observed with the capA mutant preparation as illustrated by the donor shown in Fig. 2 (A versus B). Similar cytokine profiles were observed on day 7 (data not shown). The WT capsule elicited a dose-dependent cytokine response pattern that was distinctly different from that elicited by LPS, which typically elicited a combination of IL-1β, IL-10, and TNF-α in addition to IL-8 and IL-6 (Fig. 2G). Furthermore, LPS elicited larger amounts of IL-6 than IL-8, while the reverse was observed with WT capsule. WT capsule, even at the highest dose of 1,000 μg/ml, elicited fewer cytokines and in smaller amounts than did LPS at 10 ng/ml (compare Fig. 2A and G).
FIG 1.

Capsule expression is greatly reduced in the capA mutant B. anthracis strain. Capsule was purified from broth culture supernatants as described in Materials and Methods. Fifty micrograms of capsule from WT (lane 1) and capA mutant (lane 2) per lane was electrophoresed on a 1% agarose gel, and the gel was stained with methylene blue.
FIG 2.
B. anthracis capsule induces cytokine responses from differentiating human monocytes. (A to F) Differentiating human monocytes were exposed to 250 to 1,000 μg/ml of WT capsule (A, C, D, E, and F) or an equivalent amount of capA mutant preparation (B, C, D, E, and F) for 7 days. Medium samples collected on day 3 were analyzed for cytokines as described in Materials and Methods. (A and B) Data are presented as the fold increase over the basal cytokine levels released by unstimulated control cells cultured in parallel. Data for IL-8 (C), IL-6 (D), IL-1β (E), and TNF-α (F) from day 3 are also presented as mean pg/ml ± SEM (n = 2). Statistical significance of the IL-8, IL-6, IL-1β, and TNF-α responses compared to the unstimulated control was determined by t test (*, P < 0.05; **, P < 0.01; ***, P < 0.001; ****, P < 0.0001). (G) The comparable fold increase in cytokine response of differentiating human monocytes exposed to 10 ng/ml LPS is shown after 3 days of culture. Data from a representative donor are shown.
The cytokine responses to the WT capsule are not due to any broth culture or harvest-derived components or contaminants such as endotoxin because the capA mutant preparation, which was subjected to the same culture and purification conditions in parallel, did not elicit comparable cytokine responses and both preparations have similarly low levels of endotoxin (<0.25 endotoxin units [EU]/ml). In addition, the cytokine pattern observed with LPS is distinctly different from that seen with WT capsule as noted above. Because capsule is covalently attached to the PGN layer of the bacillus (22, 24), and because PGN has been reported in the literature to be a potent inducer of cytokine release (23, 25–28), PGN in the capsule preparation was also a possible stimulator of the cytokine responses. However, the WT capsule and capA mutant preparations were found to contain only 0.05% and 0.11% PGN, respectively. Thus, the cytokine release induced by the WT capsule is not due to PGN, as it contained half the amount of PGN present in the relatively inactive capA mutant preparation.
Exposure to B. anthracis capsule during differentiation yields iDCs with a slightly altered phenotype.
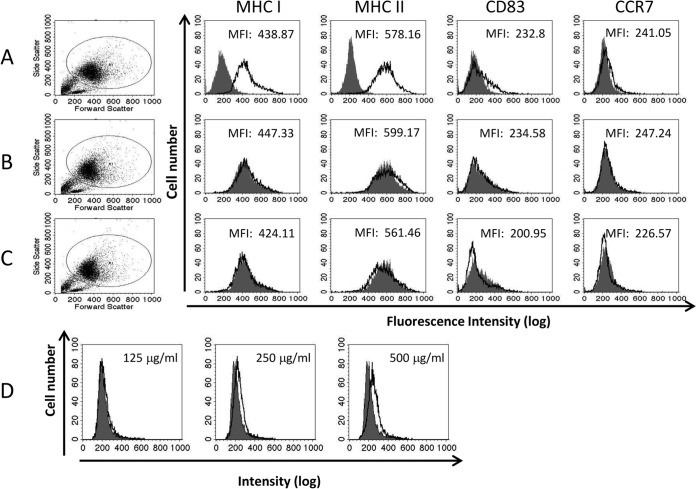
We hypothesized that since continuous exposure to capsule during differentiation elicited cytokine responses from the monocytes, it might affect the phenotype of the resulting iDCs. Capsule prepared from the WT strain of B. anthracis at concentrations of 125 to 500 μg/ml or equivalent amounts of the preparation from the capA mutant strain were included in the differentiation medium. On day 7, the phenotype of the differentiated iDCs was analyzed by flow cytometry. Naive control iDCs differentiated in the absence of capsule expressed high levels of MHC I and II but very little CD83 or CCR7 as shown with the donor in Fig. 3. Cells differentiated in the presence of 500 μg/ml WT capsule did not show any significant changes in cell surface marker expression compared to the naive control cells (P > 0.05 for all markers, n = 6 donors, Fig. 3B), nor did the cells differentiated in the presence of an equivalent amount of the capA mutant preparation (P > 0.05 for all markers, n = 6 donors, Fig. 3C). However, there was a dose-dependent increase in SSC in the cells exposed to WT capsule (Fig. 3D). This effect was observed in five out of six donors (P < 0.01 for 500 μg/ml) including the one shown. The capA mutant preparation also increased the SSC over that of the untreated control (P < 0.05 for the 500-μg/ml equivalent), but without the dose dependence observed with WT capsule (data not shown).
FIG 3.
Exposure of monocytes to B. anthracis capsule during differentiation alters the phenotype of the resulting iDCs. Differentiating human monocytes were exposed to 125 to 500 μg/ml WT capsule or equivalent amounts of capA mutant preparation for 7 days. On day 7, the cells were assessed for MHC I, MHC II, CD83, CCR7, and SSC by flow cytometry. (A) The filled histograms represent the isotype control staining, and the black-outlined histograms represent the marker staining for the naive control iDCs. (B and C) The filled histograms represent the marker staining for the naive control iDCs. The black-outlined histograms represent the marker staining for the cells differentiated in the presence of 500 μg/ml WT capsule (B) or capA mutant preparation (C). P values were determined by comparing the means of the MFIs for the WT capsule- and capA mutant-treated cells for all donors tested to the mean MFI for the naive control iDCs (P > 0.05 for all markers, n = 6 donors). (D) The filled histograms represent the SSC for the naive control iDCs. The black-outlined histograms represent the SSC for the cells differentiated in the presence of WT capsule. Statistical significance of changes in SSC compared to the naive control was determined by t test (P < 0.01, for 5 of 6 donors). Data from a single donor are shown.
Differentiation in the presence of capsule results in DCs with reduced CCR7 expression and reduced CCR7-dependent chemotaxis upon maturation with Ba PGN.
Since iDCs differentiated in the presence of WT capsule did not have an entirely normal phenotype as evidenced by the increase in SSC, we hypothesized that they might not convert to an mDC phenotype in response to PGN as do normal iDCs when stimulated with a maturation factor (29). To test this, monocytes differentiated into iDCs in the presence or absence of WT capsule (500 μg/ml) or an equivalent amount of the capA mutant preparation were subsequently stimulated with a maturing dose of Ba PGN (1 μg/ml) on day 7. Control naive iDCs were maintained in differentiation medium alone without Ba PGN in order to retain the immature phenotype (Fig. 4A). On day 9, medium samples were collected for cytokine analysis (see below) and the cells were stained with fluorescently labeled antibodies specific for human MHC I and II, plus CD83 and CCR7, cell surface markers that are associated with mDCs (29, 30), and analyzed by flow cytometry. Day 9 naive control iDCs express high levels of MHC I and II and low levels of CD83 and CCR7 (Fig. 4A). Ba PGN induced maturation of naive control iDCs that were not exposed to capsule preparations, as indicated by the increased cell surface expression of MHC I, MHC II, CD83, and CCR7 (Fig. 4B). Increased expression of these cell surface markers was still noted in cells that had been differentiated in the presence of the WT capsule, but CCR7 upregulation was inhibited (Fig. 4C). This occurred in all five donors tested with WT capsule (P < 0.05, n = 5 donors), including the one shown in Fig. 4, while the capA mutant preparation showed no statistically significant inhibition of CCR7 in the same group of donors (Fig. 4D, P > 0.05, n = 5 donors). When a similar experiment was conducted using LPS to induce maturation instead of Ba PGN, increased expression of MHC I, MHC II, CD83, and CCR7 was similarly observed while CCR7 upregulation was also significantly inhibited in cells exposed to WT capsule during differentiation (P < 0.05, n = 5 donors; see Fig. S1C in the supplemental material), but not in cells exposed to an equivalent amount of the capA mutant preparation (P > 0.05, n = 5 donors; see Fig. S1D).
FIG 4.

Differentiation in the presence of B. anthracis capsule results in DCs with reduced CCR7 expression and reduced CCR7-dependent chemotaxis upon maturation with Ba PGN. Human monocytes were differentiated into iDCs in the presence of 500 μg/ml WT capsule or an equivalent amount of capA mutant preparation for 7 days. Control cells were differentiated in parallel in the absence of capsule. On day 7, the cells were stimulated with 1 μg/ml Ba PGN to induce the mDC phenotype. Additional control cells were maintained in differentiation medium alone to preserve the iDC phenotype. On day 9, half of the cells were assessed for MHC I, MHC II, CD83, and CCR7 expression by flow cytometry (A, B, C, and D). (A) The filled histograms represent the isotype control staining, and the black-outlined histograms represent the marker staining for the naive control iDCs. (B) The filled histograms represent the unstimulated naive control iDCs. The black-outlined histograms represent control iDCs after stimulation with 1 μg/ml Ba PGN to induce the mDC phenotype. (C and D) The filled histograms represent the mDC control. The black-outlined histograms represent Ba PGN-stimulated cells that were exposed to 500 μg/ml WT capsule (C) or to capA mutant preparation (D). P values were determined by comparing the means of the MFI for the WT capsule- and capA mutant-treated cells for all donors tested to the mean MFI for the Ba PGN-matured controls (P < 0.05 only for CCR7 for WT capsule, n = 5 donors). Histograms and MFIs shown are from a single donor. (E and F) The other half of the cells was subjected to a migration assay using CCL19 (E) or CCL21 (F) as the chemoattractive ligand, and the chemotactic index was calculated as described in Materials and Methods. Data shown are the means of the chemotactic indices for all the donors tested (n = 4). Statistical significance was determined by t test (*, P < 0.05, n = 4 donors).
CCR7 expression by mDCs allows them both to migrate to and to enter lymph nodes (31). Since CCR7 expression was reduced in cells exposed to WT capsule that were matured with Ba PGN, we sought to determine whether or not CCR7-dependent chemotaxis was also reduced by testing the cells in a chemotactic activity assay using the CCR7 ligands CCL19 and CCL21 (31) as chemoattractants. Human monocytes were differentiated into iDCs in the presence of 500 μg/ml capsule or an equivalent amount of the capA mutant preparation. Control cells were differentiated in the absence of capsule. One microgram of Ba PGN per ml was added on day 7 to capsule-differentiated, capA mutant-differentiated, and naive control cells to induce maturation. Additional control cells were maintained unstimulated to preserve the iDC phenotype. On day 9, the cells were assessed for CCR7-dependent chemotaxis in a chemotactic activity assay using CCL19 or CCL21 as the chemoattractive ligand. Control iDCs matured with Ba PGN demonstrated significant chemotaxis toward both CCL19 and CCL21 compared to the unstimulated control cells (P < 0.001, n = 4 donors, Fig. 4E and F). Capsule-differentiated, Ba PGN-matured cells showed a significant decrease in chemotaxis toward both CCL19 and CCL21 compared to that of Ba PGN-matured control cells (P < 0.05, n = 4 donors, Fig. 4E and F), while the capA mutant-differentiated, Ba PGN-matured cells did not (P > 0.05, n = 4 donors, Fig. 4E and F), consistent with the lack of statistically significant CCR7 expression inhibition in these cells (Fig. 4D). These data indicate that not only is CCR7 expression decreased in monocytes differentiated in capsule prior to maturation induction by Ba PGN but CCR7-dependent chemotaxis toward CCL19 and CCL21 is decreased as well.
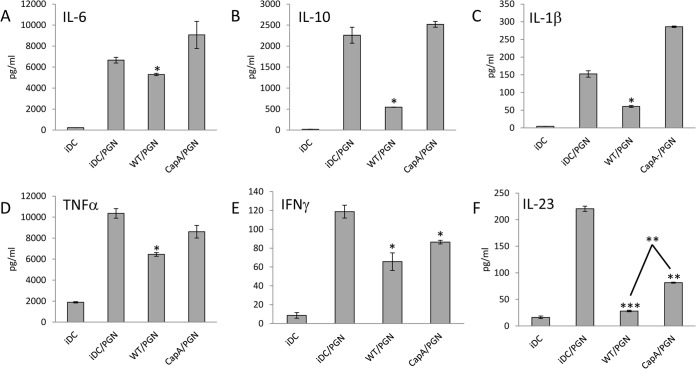
Differentiation in the presence of capsule results in DCs with reduced cytokine release upon maturation with Ba PGN.
In addition to inducing increased cell surface marker expression by iDCs, Ba PGN also induces cytokine release. Thus, we next determined if differentiation in the presence of capsule would alter this response of iDCs to Ba PGN. Monocytes differentiated into iDCs in the presence or absence of WT capsule (500 μg/ml) or an equivalent amount of the capA mutant preparation were subsequently stimulated with a maturing dose of Ba PGN (1 μg/ml) on day 7 and medium was collected on day 9 as described above. Ba PGN stimulated the release of all of the cytokines tested except for IL-2. Exposure to WT capsule during differentiation resulted in decreased release of IL-6 (Fig. 5A), IL-10 (Fig. 5B), IL-1β (Fig. 5C), TNF-α (Fig. 5D), IFN-γ (Fig. 5E), and IL-23 (Fig. 5F) upon stimulation with Ba PGN. IL-6 release was inhibited by WT capsule only (P < 0.05) in three out of five donors, including the one shown in Fig. 5. IL-10 was inhibited by WT capsule (P < 0.05) in four out of five donors, with the capA mutant preparation having a similar effect in one donor. IL-1β release was inhibited by WT capsule in three out of five donors while the capA mutant preparation inhibited IL-1β release in only one donor. TNF-α release was inhibited by WT capsule (P < 0.05) in four out of five donors, with the capA mutant preparation having a similar effect in only one donor. IFN-γ release was inhibited (P < 0.05) in all five donors receiving WT capsule, with the capA mutant preparation having a similar effect in four donors, including the one shown. IL-23 was significantly inhibited in cells exposed to the capsule in three out of four donors (P < 0.001, Fig. 5F). IL-23 was also significantly inhibited in cells exposed to the capA mutant preparation in three out of four donors (P < 0.01). The inhibition of IL-23 was greater in cells exposed to the WT capsule in two out of three donors, including the one shown in Fig. 5.
FIG 5.
Exposure of monocytes to B. anthracis capsule during differentiation alters the resulting iDCs' cytokine response to Ba PGN. Human monocytes were differentiated into iDCs in the presence of 500 μg/ml capsule or capA mutant preparation for 7 days. Control cells were differentiated in parallel in the absence of capsule. On day 7, the treated and naive control cells were stimulated with 1 μg/ml Ba PGN. Additional control cells were maintained unstimulated. On day 9, the media were analyzed for cytokines. Several donors exhibited decreased release of IL-6 (A), IL-10 (B), IL-1β (C), TNF-α (D), IFN-γ (E), and IL-23 (F) upon stimulation with Ba PGN (*, P < 0.05; **, P < 0.01; ***, P < 0.001; n = 2). P values for the responses to the two preparations (WT and capA mutant) were determined by comparing the mean pg/ml of each cytokine detected for the treated cells to the mean pg/ml of each cytokine detected for the control cells for each of four or five donors in a two-tailed t test. Data shown are from a representative donor.
In a similar experiment, we also determined if differentiation in the presence of capsule would alter the cytokine response of iDCs to maturation with LPS. Human monocytes differentiated into iDCs in the presence or absence of WT capsule (500 μg/ml) or an equivalent amount of the capA mutant preparation were subsequently stimulated with a maturing dose of LPS (100 ng/ml) on day 7, and medium was analyzed for cytokines on day 9. IL-10 release was significantly inhibited (P < 0.05) in WT capsule-differentiated cells compared to the naive differentiated control in five out of five donors tested, compared to four out of five donors for the capA mutant preparation. In three of the five donors, the inhibition was greater for the WT capsule (P < 0.05), while in one donor it was greater for the capA mutant preparation (data not shown). IL-12p70 release was significantly inhibited (P < 0.05) compared to the naive control in three out of five donors by both the WT capsule and the capA mutant preparations but was only significantly greater with WT in one donor (data not shown). There was no significant inhibition by WT capsule of LPS-stimulated release of any other cytokines in the majority of donors.
Thus, while there were differences among the donors, the WT capsule significantly inhibited upregulation of CCR7 in response to Ba PGN or LPS while the capA mutant preparation had no significant effect on CCR7. Effects on the cytokine release in response to a maturing dose of Ba PGN were more variable, with WT capsule showing more significant inhibition for most cytokines tested. However, the similarities between WT capsule and the capA mutant preparation with respect to IFN-γ release in response to Ba PGN and IL-10 and IL-12p70 release in response to LPS suggest that these particular inhibitory effects may be due not to capsule but to other undefined components of the preparations that remain to be identified.
Simultaneous exposure to B. anthracis capsule and Ba PGN does not inhibit the responses of naive iDCs.
The decreased responsiveness to Ba PGN by the iDCs that had been differentiated in the presence of capsule could be mediated by capsule interfering directly with Ba PGN or by a change in the cells that occurred over time. In order to test whether or not capsule could interfere with the response to Ba PGN directly, naive iDCs differentiated in the absence of capsule were exposed to capsule plus a maturing dose of Ba PGN (1 μg/ml) simultaneously. Human monocytes were differentiated into iDCs over the course of 7 days. On day 7, the naive iDCs were exposed to capsule from the WT (500 μg/ml) or an equivalent amount of the capA mutant preparation plus 1 μg/ml Ba PGN simultaneously. Control iDCs were exposed to 1 μg/ml Ba PGN alone or were maintained in differentiation medium alone to retain the immature phenotype. On day 9, medium samples were collected and the cells were analyzed for surface expression of MHC I, MHC II, CD83, and CCR7 as described above. Ba PGN induced upregulation of MHC I, MHC II, CD83, and CCR7 when introduced alone or with WT capsule (data not shown). Indeed, upregulation of these cell surface markers was almost entirely unaffected in cells from four of four donors exposed to capsule plus Ba PGN. This is in direct contrast to the cells exposed to WT capsule during differentiation (Fig. 4) and suggests that capsule does not directly inhibit the interaction of Ba PGN with cells and that more prolonged preexposure to capsule mediates changes in the cells that make them less responsive. Consistent with the absence of changes in cell surface marker expression after simultaneous exposure to Ba PGN and WT capsule, there were no significant changes in the cytokine response profile to Ba PGN given together with WT capsule compared to Ba PGN alone (data not shown). Similar results were obtained when LPS was used to mature the cells instead of Ba PGN (data not shown).
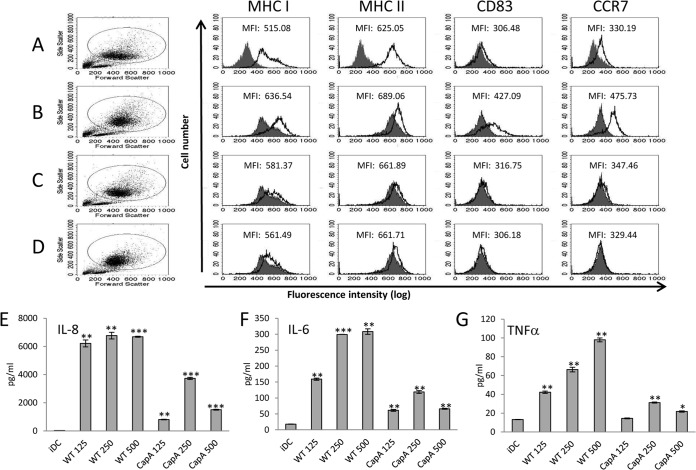
B. anthracis capsule is not a maturation factor for human iDCs.
Since capsule reproducibly elicits a cytokine response from differentiating human monocytes, we next determined whether it would also elicit a cytokine response from naive differentiated human iDCs and possibly alter expression of cell surface markers as well. Human monocytes were differentiated over 7 days into iDCs, after which they were exposed to capsule derived from WT (125 to 500 μg/ml) or an equivalent amount of the capA mutant preparation. Control cells either were maintained in differentiation medium in order to retain their immature phenotype or were stimulated with 100 ng/ml LPS to induce maturation. On day 9, medium samples were collected and the cells were analyzed for surface expression of human MHC I, MHC II, CD83, and CCR7 by flow cytometry. Naive control iDCs expressed high levels of MHCs and very low levels of CD83 and CCR7 (Fig. 6A). Exposure to 100 ng/ml LPS induced upregulation of MHC I, MHC II, CD83, and CCR7 as expected (Fig. 6B), while exposure to up to 500 μg/ml of the WT capsule did not significantly affect cell surface expression of MHC I, MHC II, CD83, and CCR7 (P > 0.05, n = 3 donors, Fig. 6C). Similarly, no significant effect on cell surface markers was observed with the capA mutant preparation (P > 0.05, n = 3 donors, Fig. 6D). Despite the lack of changes in cell surface marker expression, there were cytokine responses to the WT capsule and capA mutant preparations. Results from a representative donor are shown in Fig. 6E to G. As with the differentiating monocytes, 500 μg/ml WT capsule induced significant release of IL-8 in all donors tested (P range, <0.01 to <0.0001; n = 3). In contrast to the differentiating monocytes, WT capsule induced significant (P < 0.01) release of IL-6 in two out of three donors tested (including the one shown in Fig. 6), rather than in all donors. Also in contrast to the differentiating monocytes, low-level, but statistically significant (P range, <0.05 to <0.001), TNF-α release was observed with WT capsule in all donors tested. Similar to the differentiating monocytes, the capA mutant preparation elicited statistically significant (P < 0.01) IL-8 only from all donors. The magnitude of the IL-8 response to WT capsule was significantly greater than that to the equivalent amount of capA mutant preparation (P < 0.01). Low, but statistically significant, IL-6 and TNF-α release in response to the equivalent amount of capA mutant preparation (P < 0.01 for IL-6 and <0.05 for TNF-α) was observed in two out of three donors, including the one shown in Fig. 6. However, these responses were much smaller than those to WT capsule (P < 0.05 for IL-6, P < 0.01 for TNF-α). Thus, the cytokine response of the iDCs to anthrax capsule was similar, though not identical, to the response of the differentiating monocytes.
FIG 6.
Exposure of naive iDCs to B. anthracis capsule does not induce an mDC phenotype but does elicit cytokines. Human monocytes were differentiated into iDCs over the course of 7 days. On day 7, the iDCs were exposed to 500 μg/ml WT capsule or an equivalent amount of capA mutant preparation. On day 9, the cells were assessed for MHC I, MHC II, CD83, and CCR7 expression by flow cytometry (A, B, C, and D) and the media were analyzed for cytokines (E, F, and G). (A) The filled histograms represent the isotype control staining, and the black-outlined histograms represent the marker staining for the untreated naive control iDCs. (B) The filled histograms represent the unstimulated naive control iDCs, and the black-outlined histograms represent control iDCs that were stimulated with 100 ng/ml LPS to induce the mDC phenotype. (C and D) The filled histograms represent the unstimulated naive control iDCs. The black-outlined histograms represent cells that were exposed to 500 μg/ml WT capsule (C) or to capA mutant preparation (D). P values were determined by comparing the means of the MFI for the WT capsule and capA mutant-treated cells for all donors tested to the mean MFI for the unstimulated naive control iDCs (P > 0.05 for all markers, n = 3 donors). (E, F, and G) Data are presented as mean pg/ml ± SEM (n = 2) for IL-8 (E), IL-6 (F), and TNF-α (G). Statistical significance of the IL-8, IL-6, and TNF-α responses compared to the unstimulated iDC control was determined by t test (*, P < 0.05; **, P < 0.01; ***, P < 0.001). Data from a single donor are shown.
DISCUSSION
Capsule is one of the chief virulence factors for B. anthracis. The mechanism by which capsule enhances virulence is presumed to be mainly by the prevention of ingestion and killing of the bacteria by phagocytic cells. However, vegetative bacilli shed large amounts of capsule during their growth, and previous studies have indicated that the free capsule may also contribute to virulence (14, 15). We hypothesized that free capsule might contribute to pathogenesis by interfering with innate immune responses. Therefore, in this study we examined the effects of free capsule on cells of the human innate immune system. We purified capsule shed naturally by vegetative bacilli during broth culture to acquire free capsule that would be similar to the free capsule present in the infected host. To control for possible contaminants or components arising from the broth culture and purification procedure, we prepared capsule material from a fully virulent WT B. anthracis strain and from an isogenic capsule-reduced capA mutant strain that produces only 2% of the capsule of the WT. When these two preparations were applied to differentiating human monocytes, the WT capsule preparation consistently elicited both IL-8 and IL-6 from all donors, while the capA mutant preparation elicited only very low levels of IL-8 from all donors and very low levels of IL-6 from some donors. Cytokine responses to WT capsule were consistently significantly greater and showed better dose dependence than did cytokine responses to the capA mutant preparation. Although B. anthracis capsule consistently elicited IL-8 and IL-6, it is a weak inducer of cytokines in differentiating monocytes and iDCs compared to LPS. We could detect a cytokine response at capsule concentrations as low as 125 μg/ml, but 500 μg/ml or more was required for robust responses. Even at concentrations of 1,000 μg/ml, the cytokines released were only a fraction of those released in response to 10 ng/ml of LPS. Although the concentrations of capsule used in this study were high, they were not so high as to be physiologically irrelevant, considering that serum concentrations greater than 500 μg/ml have been reported in mice (10) and concentrations greater than 1 mg/ml have been reported in rhesus macaques (11) with anthrax.
Various controls suggested that the cytokine responses were in fact due to the capsule in the WT preparation. The capA mutant preparation, which is greatly reduced in capsule and prepared in parallel in a manner identical to that of the WT capsule, produced nearly no cytokine release from the differentiating monocytes. Both preparations were practically free of LPS (<0.25 EU/ml), and furthermore, the pattern of cytokines induced by capsule was distinctly different from that seen with LPS. PGN, a relatively potent cytokine inducer (22, 24–27), has been shown to be released by vegetative B. anthracis bacilli during culture (25). While very low levels of PGN were found in the preparations, this was not likely to be the source of cytokine release since the inactive capA mutant preparation contained twice as much PGN as did the active WT capsule. The trace amounts of capsule, PGN, and possibly other B. anthracis cell wall components in the capA mutant preparation may be responsible for the very low IL-8 and IL-6 responses observed.
These results are in contrast to those in a recent report describing release of IL-1β by human monocyte-derived dendritic cells in response to 100 μg/ml B. anthracis capsule (32). In that report, Cho et al. did not see the increase in IL-6 that we observed, and they did not test for IL-8. The capsule purification protocol that they used differs substantially from ours. Furthermore, they do not mention testing for contamination by LPS. Also, they do not indicate the amount of PGN present in their capsule preparation. Unlike B. anthracis capsule, Ba PGN, as noted above, induces a robust cytokine response and, in our study, maturation of human iDCs. Either LPS contamination or PGN might account for the IL-1β observed by Cho et al.
The consistency and specificity of the cytokine responses to WT capsule suggest that it may bind to a pattern recognition receptor. This idea is supported by a recent report suggesting that B. anthracis capsule mediates TNF-α release through TLR2, based on the differential response of macrophages from strains of hamsters with or without functional TLR2 (33). It is possible that human TLR2 also functions as a receptor for B. anthracis capsule. Experiments are under way to explore this hypothesis.
Examination of the iDCs differentiated in the presence of B. anthracis capsule by flow cytometry revealed a subtle change in the phenotype. SSC increased in response to WT capsule in a dose-dependent manner. This change could reflect the presence of vacuoles filled with undegraded capsule, or an increase in dendrites, or a combination of the two. Increases in SSC were observed with the capA mutant preparation as well, but these were small by comparison and did not show dose dependence. No significant changes in MHC I, MHC II, CD83, or CCR7 expression compared to the naive control were observed in the capsule-differentiated iDCs. The combination of the cytokine response and the increase in SSC indicated that the presence of B. anthracis capsule during differentiation altered the resulting iDCs. The relevance of these changes was demonstrated by the impaired responses of the capsule-differentiated iDCs to maturation induced by Ba PGN, as indicated by consistently smaller increases in cell surface expression of CCR7 and by the concomitant reduction in CCR7-dependent chemotaxis toward CCL19 and CCL21. It is possible that this effect was due to the IL-6 released by the differentiating monocytes in response to the capsule. Human monocytes differentiated into iDCs in the presence of as little as 5 ng/ml IL-6 have also been shown to be impaired in upregulation of CCR7 in response to a maturing dose of LPS (34). In addition to inhibition of CCR7 upregulation, release of IL-6, IL-10, IL-1β, TNF-α, IFN-γ, and IL-23 upon maturation with Ba PGN was inhibited in the majority of donors whose cells were exposed to capsule. Surprisingly, release of IFN-γ upon maturation with Ba PGN was also inhibited in the majority of donors whose cells were exposed to the capA mutant preparation. We also noted that the capA mutant preparation as well as the capsule inhibited LPS induction of IL-10 release. This indicates that the effect on Ba PGN-stimulated IFN-γ release and LPS-stimulated IL-10 release is likely due to another unidentified component present in both of the preparations. This other component was not as effective as capsule in suppressing DC responses, as it did not mediate statistically significant inhibition of CCR7 expression and function like the capsule did. Its primary effect in Ba PGN-matured cells was inhibition of IFN-γ release. One donor treated with the capA mutant preparation showed inhibition of IL-10, IL-1β, and TNF-α in response to Ba PGN as well. While that one individual was remarkably sensitive to the unidentified component, the majority of donors were affected more by the capsule.
Not only was upregulation of CCR7 expression upon maturation with Ba PGN significantly impaired in the capsule-differentiated DCs, but chemotaxis toward the CCR7 ligands CCL19 and CCL21 was also significantly impaired. The impairment of CCR7 that we observed could have an impact on the development of an adaptive immune response. CCR7 expression by mature DCs allows them both to migrate to and to enter lymph nodes (31). Furthermore, signaling through CCR7 inhibits apoptosis of mature DCs, thereby extending their life span and increasing the probability of T cell activation (35, 36). Therefore, impaired CCR7 expression and the consequently impaired CCR7-dependent migration due to capsule exposure could contribute to pathogenesis by potentially reducing activation of T cells and impairing the development of an adaptive immune response. This could have consequences for pathogenesis, as the successful induction of a Th1 immune response has been shown to be protective in mice against a nontoxigenic, encapsulated strain of B. anthracis (37).
Less consistent than the reduction in CCR7 expression and CCR7-dependent chemotaxis, but still significant, there were also reductions in the release of IL-10 and TNF-α in four out of five donors, IL-6 and IL-1β in three out of five donors, and IL-23 in three out of four donors. Inhibition of IL-23 was also noted with both capsule and the capA mutant preparation but was greater with capsule in two of three subjects. Although inhibition of IFN-γ release cannot be ascribed solely to capsule, inhibition was more consistently observed with capsule than with the capA mutant preparation. These inhibitory effects were due to changes that occurred in the cells over time rather than to direct interference of capsule with the Ba PGN, since capsule added together with Ba PGN to naive differentiated iDCs had no effect. Impaired release of these cytokines could have consequences in the context of anthrax. Although IL-10 usually acts as an anti-inflammatory cytokine, it has also been shown to be a potent stimulator of NK cells (38, 39) that can increase their killing capacity and release of perforin and granzyme B (37). NK cells have recently been shown to contribute to suppressing bacteremia during B. anthracis infection in mice (40, 41). IL-6 can support survival of the naive T cell pool (42) and can drive differentiation of Th17 cells (43). TNF-α and IL-1β also drive differentiation of Th17 cells from naive CD4+ T cells (44), while IL-23 supports Th17 survival and activity (45). The Th17 lineage contributes to immunity against both extracellular and intracellular bacterial infection as well as fungal pathogens by inducing production of antimicrobial peptides by epithelial cells and by recruiting and activating phagocytes (44, 46). Simultaneous inhibition of IL-6, IL-1β, TNF-α, and IL-23 could thus blunt the development of a Th17 response that could contribute to impaired resistance to infection.
Statistically significant reductions in the expression of CCR7 upon maturation, in chemotaxis toward the CCR7 ligands CCL19 and CCL21, and inhibition of some cytokines as indicated above were observed only in cells exposed to capsule, indicating that these effects are mediated by the capsule. Inhibition of the Th1-promoting and macrophage-activating (36) cytokine IFN-γ in response to Ba PGN was almost as effectively mediated by the capA mutant control preparation, indicating that there is likely another active component present in both preparations. However, this other component lacked the breadth of effect that capsule had. Between the impairment of CCR7 expression and CCR7-dependent chemotaxis and the inhibition of the release of Th17-promoting cytokines by capsule, there may be interference with adaptive immune responses and thus resistance to anthrax.
WT capsule elicited a distinct cytokine response from differentiating human monocytes, including IL-8, IL-6, and TNF-α, while the capA mutant preparation had a much lesser effect, eliciting only minimal amounts of IL-8 and IL-6 consistently. No remarkable changes in cell surface markers were noted when naive iDCs were exposed to the capsule preparations. Similarly, the monocytes differentiated in the presence of capsule showed only subtle phenotypic changes until they were subsequently exposed to Ba PGN or LPS. The naive iDCs that were exposed to capsule for 48 h retained the naive phenotype but were not subsequently challenged with a maturation stimulus such as Ba PGN or LPS. Perhaps, this shorter exposure to capsule might also have impaired the subsequent responses of the DCs to Ba PGN. The minimum amount of time that capsule needs to be present to impair the cells' sensitivity to inflammatory stimuli will require further study.
Capsule is known to enhance the virulence of B. anthracis by protecting the vegetative bacilli from phagocytosis by immune cells (4–6). This poorly immunogenic outermost layer may also shield more reactogenic bacterial factors on intact bacilli, such as PGN, from being sensed by pattern recognition receptors on host cells. In support of this hypothesis, it has been shown that human primary myeloid DCs and human monocyte-derived DCs release less IL-12p40, IL-6, and TNF-α when they are cocultured with an encapsulated strain of B. anthracis than when they are cocultured with an unencapsulated strain (47). Our results indicate that the capsule may not need to be bound to the bacilli in order to protect them from the immune system. In this study, we demonstrate the ability of shed capsule to induce only a very modest cytokine response from differentiating monocytes compared to more robust stimuli like LPS and PGN and to inhibit the responsiveness and maturation of iDCs differentiated in capsule to a subsequent inflammatory stimulus. These findings might result in impairment of DC function in vivo. It is thus possible that while bacillus-bound capsule protects vegetative bacilli from phagocytosis, the shed capsule also contributes to the virulence of B. anthracis by blunting the responses of innate and adaptive immune cells to more inflammatory stimuli from the spore or bacillus, such as PGN, thus allowing the infection to become established.
Supplementary Material
ACKNOWLEDGMENTS
We thank Neil X. Krueger of Immunetics, Inc., for conducting the PGN analysis. We also thank Anna Trivett for purifying the monocytes.
The opinions, interpretations, conclusions, and recommendations are those of the authors and not necessarily endorsed by the US Army.
The work was supported by the Defense Threat Reduction Agency grant CBM.VAXBT.03.10.RD.015.
Footnotes
Published ahead of print 2 June 2014
Supplemental material for this article may be found at http://dx.doi.org/10.1128/IAI.01857-14.
REFERENCES
- 1.Mikesell P, Ivins BE, Ristroph JD, Dreier TM. 1983. Evidence for plasmid-mediated toxin production in Bacillus anthracis. Infect. Immun. 39:371–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Green BD, Battisti L, Koehler TM, Thorne CB, Ivins BE. 1985. Demonstration of a capsule plasmid in Bacillus anthracis. Infect. Immun. 49:291–297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Uchida I, Sekizaki T, Hashimoto K, Terakado N. 1985. Association of the encapsulation of Bacillus anthracis with a 60 megadalton plasmid. J. Gen. Microbiol. 131:363–367. [DOI] [PubMed] [Google Scholar]
- 4.Makino S, Uchida I, Terakado N, Sasakawa C, Yoshikawa M. 1989. Molecular characterization and protein analysis of the cap region, which is essential for encapsulation in Bacillus anthracis. J. Bacteriol. 171:722–730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Scorpio A, Chabot DJ, Day WA, O'Brien DK, Vietri NJ, Itoh Y, Mohamadzadeh M, Friedlander AM. 2007. Poly-γ-glutamate capsule-degrading enzyme treatment enhances phagocytosis and killing of encapsulated Bacillus anthracis. Antimicrob. Agents Chemother. 51:215–222. 10.1128/AAC.00706-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Keppie J, Harris-Smith PW, Smith H. 1963. The chemical basis of the virulence of Bacillus anthracis. IX. Its aggressins and their mode of action. Br. J. Exp. Pathol. 44:446–453. [PMC free article] [PubMed] [Google Scholar]
- 7.Zwartouw HT, Smith H. 1956. Polyglutamic acid from Bacillus anthracis grown in vivo: structure and aggressin activity. Biochem. J. 63:437–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Goodman JW, Nitecki DE. 1967. Studies on the relation of a prior immune response to immunogenicity. Immunology 16:577–583. [PMC free article] [PubMed] [Google Scholar]
- 9.Wang TT, Lucas AH. 2004. The capsule of Bacillus anthracis behaves as a thymus-independent type 2 antigen. Infect. Immun. 72:5460–5463. 10.1128/IAI.72.9.5460-5463.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kozel TR, Murphy WJ, Brandt S, Blazar BR, Lovchik JA, Thorkildson P, Percival A, Lyons CR. 2004. mAbs to Bacillus anthracis capsular antigen for immunoprotection in anthrax and detection of antigenemia. Proc. Natl. Acad. Sci. U. S. A. 101:5042–5047. 10.1073/pnas.0401351101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Boyer AE, Quinn CP, Hoffmaster AR, Kozel TR, Saile E, Marston CK, Percival A, Plikaytis BD, Woolfitt AR, Gallegos M, Sabourin P, McWilliams LG, Pirkle JL, Barr JR. 2009. Kinetics of lethal factor and poly-d-glutamic acid antigenemia during inhalation anthrax in rhesus macaques. Infect. Immun. 77:3432–3441. 10.1128/IAI.00346-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sutherland MD, Thorkildson P, Parks SD, Kozel TR. 2008. In vivo fate and distribution of poly-γ-d-glutamic acid, the capsular antigen from Bacillus anthracis. Infect. Immun. 76:899–906. 10.1128/IAI.01176-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Roelants GE, Whitten LF, Hobson A, Goodman JW. 1969. Immunochemical studies on the poly-γ-d-glutamyl capsule of Bacillus anthracis. J. Immunol. 103:937–943. [PubMed] [Google Scholar]
- 14.Smith H, Gallop RC. 1956. The chemical basis of the virulence of Bacillus anthracis. VI: an extracellular immunising aggressin isolated from exudates of infected guinea-pigs. Br. J. Exp. Pathol. 37:144–155. [PMC free article] [PubMed] [Google Scholar]
- 15.Makino S, Watarai M, Cheun H, Shirahata T, Uchida I. 2002. Effect of the lower molecular capsule released from the cell surface of Bacillus anthracis on the pathogenesis of anthrax. J. Infect. Dis. 186:227–233. 10.1086/341299. [DOI] [PubMed] [Google Scholar]
- 16.Tournier J, Paccani SR, Quesnel-Hellman A, Baldari CT. 2009. Anthrax toxins: a weapon to systematically dismantle the host immune defenses. Mol. Aspects Med. 30:456–466. 10.1016/j.mam.2009.06.002. [DOI] [PubMed] [Google Scholar]
- 17.Menard R, Sansonetti PJ, Parsot C. 1993. Nonpolar mutagenesis of the ipa genes defines IpaB, IpaC, and IpaD as effectors of Shigella flexneri entry into epithelial cells. J. Bacteriol. 175:5899–5906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bozue JA, Parthasarathy N, Phillips LR, Cote CK, Fellows PF, Mendelson I, Shafferman A, Friedlander AM. 2005. Construction of a rhamnose mutation in Bacillus anthracis affects adherence to macrophages but not virulence in guinea pigs. Microb. Pathog. 38:1–12. 10.1016/j.micpath.2004.10.001. [DOI] [PubMed] [Google Scholar]
- 19.Mendelson I, Tobery S, Scorpio A, Bozue J, Shafferman A, Friedlander AM. 2004. The NheA component of the non-hemolytic enterotoxin of Bacillus cereus is produced by Bacillus anthracis but is not required for virulence. Microb. Pathog. 37:149–154. 10.1016/j.micpath.2004.06.008. [DOI] [PubMed] [Google Scholar]
- 20.Cote CK, Bozue J, Moody KL, DiMezzo TL, Chapman CE, Welkos SL. 2008. Analysis of a novel spore antigen in Bacillus anthracis that contributes to spore opsonization. Microbiology 154:619–632. 10.1099/mic.0.2007/008292-0. [DOI] [PubMed] [Google Scholar]
- 21.Scorpio A, Chabot DJ, Day WA, Hoover TA, Friedlander AM. 2010. Capsule depolymerase overexpression reduces Bacillus anthracis virulence. Microbiology 156:1459–1467. 10.1099/mic.0.035857-0. [DOI] [PubMed] [Google Scholar]
- 22.Candela T, Fouet A. 2005. Bacillus anthracis CapD, belonging to the γ-glutamyltranspeptidase family, is required for the covalent anchoring of capsule to peptidoglycan. Mol. Microbiol. 57:717–726. 10.1111/j.1365-2958.2005.04718.x. [DOI] [PubMed] [Google Scholar]
- 23.Langer M, Malykhin A, Maeda K, Chakrabarty K, Williamson KS, Feasley CL, West CM, Metcalf JP, Coggeshall KM. 2008. Bacillus anthracis peptidoglycan stimulates an inflammatory response in monocytes through the p38 mitogen-activated protein kinase pathway. PLoS One 3:e3706. 10.1371/journal.pone.0003706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Richter S, Anderson VJ, Garufi G, Lu L, Budzik JM, Joachimiak A, He C, Schneewind O, Missiakas D. 2009. Capsule anchoring in Bacillus anthracis occurs by a transpeptidation reaction that is inhibited by capsidin. Mol. Microbiol. 71:404–420. 10.1111/j.1365-2958.2008.06533.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Iyer JK, Khurana T, Langer M, West CM, Ballard JD, Metcalf JP, Merkel TJ, Coggeshall KM. 2010. Inflammatory cytokine response to Bacillus anthracis peptidoglycan requires phagocytosis and lysosomal trafficking. Infect. Immun. 78:2418–2428. 10.1128/IAI.00170-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Barua S, Iyer JK, Larabee JL, Raisley B, Hughes MA, Coggeshall KM, Ballard JD. 2013. Toxin inhibition of antimicrobial factors induced by Bacillus anthracis peptidoglycan in human blood. Infect. Immun. 81:3693–3702. 10.1128/IAI.00709-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mattsson E, Verhage L, Rollof J, Fleer A, Verhoef J, Van Dijk H. 1993. Peptidoglycan and teichoic acid from Staphylococcus epidermidis stimulate human monocytes to release tumour necrosis factor-α, interleukin-1 β, and interleukin-6. FEMS Immunol. Med. Microbiol. 7:281–287. 10.1111/j.1574-695X.1993.tb00409.x. [DOI] [PubMed] [Google Scholar]
- 28.Wang JE, Dahle MK, McDonald M, Foster SJ, Aasen AO, Thiemermann C. 2003. Peptidoglycan and lipoteichoic acid in gram-positive bacterial sepsis: receptors, signal transduction, biological effects, and synergism. Shock 20:402–414. 10.1097/01.shk.0000092268.01859.0d. [DOI] [PubMed] [Google Scholar]
- 29.Banchereau J, Steinman RM. 1998. Dendritic cells and the control of immunity. Nature 392:245–252. 10.1038/32588. [DOI] [PubMed] [Google Scholar]
- 30.Yanagihara S, Komura E, Nagafune J, Watarai H, Yamaguchi Y. 1998. EB11/CCR7 is a new member of dendritic cell chemokine receptor that is up-regulated upon maturation. J. Immunol. 161:3096–3102. [PubMed] [Google Scholar]
- 31.Müller G, Lipp M. 2003. Shaping up adaptive immunity: the impact of CCR7 and CXCR5 on lymphocyte trafficking. Microcirculation 10:325–334. 10.1080/mic.10.3-4.325.334. [DOI] [PubMed] [Google Scholar]
- 32.Cho M, Ahn H, Ha H, Park J, Chun J, Kim B, Oh H, Rhie G. 2010. Bacillus anthracis capsule activates caspase-1 and induces interleukin-1β release from differentiated THP-1 and human monocyte-derived dendritic cells. Infect. Immun. 78:387–392. 10.1128/IAI.00956-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Weiss S, Levy H, Fisher M, Kobiler D, Altboum Z. 2009. Involvement of TLR2 in innnate response to Bacillus anthracis infection. Innate Immun. 15:43–51. 10.1177/1753425908100379. [DOI] [PubMed] [Google Scholar]
- 34.Hegde S, Pahne J, Smola-Hess S. 2004. Novel immunosuppressive properties of interleukin-6 in dendritic cells: inhibition of NF-κB binding activity and CCR7 expression. FASEB J. 18:1439–1441. 10.1096/fj.03-0969fje. [DOI] [PubMed] [Google Scholar]
- 35.Sanchez-Sanchez N, Riol-Blanco L, de la Rosa G, Puig-Kroger A, Garcia-Bordas J, Martin D, Longo N, Cuadrado A, Cabanas C, Corbi AL, Sanchez-Mateos P, Rodriguez-Fernandez JL. 2004. Chemokine receptor CCR7 induces intracellular signaling that inhibits apoptosis of mature dendritic cells. Blood 104:619–625. 10.1182/blood-2003-11-3943. [DOI] [PubMed] [Google Scholar]
- 36.Escribano C, Delgado-Martin C, Rodriguez-Fernandez JL. 2009. CCR7-dependent stimulation of survival in dendritic cells involves inhibition of GSK3β. J. Immunol. 183:6282–6295. 10.4049/jimmunol.0804093. [DOI] [PubMed] [Google Scholar]
- 37.Glomski IJ, Corre J, Mock M, Goossens PL. 2007. Cutting edge: IFN-γ-producing CD4 T lymphocytes mediate spore-induced immunity to capsulated Bacillus anthracis. J. Immunol. 178:2646–2650. 10.4049/jimmunol.178.5.2646. [DOI] [PubMed] [Google Scholar]
- 38.Mocellin S, Panelli MC, Wang E, Nagorsen D, Marincola FM. 2003. The dual role of IL-10. Trends Immunol. 24:36–43. 10.1016/S1471-4906(02)00009-1. [DOI] [PubMed] [Google Scholar]
- 39.Schulz U, Kreutz M, Multhoff G, Stoelcker B, Kohler M, Andreesen R, Holler E. 2010. Interleukin-10 promotes NK cell killing of autologous macrophages by stimulating expression of NKG2D ligands. Scand. J. Immunol. 72:319–331. 10.1111/j.1365-3083.2010.02435.x. [DOI] [PubMed] [Google Scholar]
- 40.Gonzales CM, Williams CB, Calderon VE, Huante MB, Moen ST, Popov VL, Baze WB, Peterson JW, Endsley JJ. 2012. Antibacterial role for natural killer cells in host defense to Bacillus anthracis. Infect. Immun. 80:234–242. 10.1128/IAI.05439-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Klezovich-Benard M, Corre J, Jusforgues-Saklani H, Fiole D, Burjek N, Tournier J, Goossens PL. 2012. Mechanisms of NK cell-macrophage Bacillus anthracis crosstalk: a balance between stimulation by spores and differential disruption by toxins. PLoS Pathog. 8:e1002481. 10.1371/journal.ppat.1002481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hong C, Nam AS, Keller HR, Ligons DL, Park J, Yoon H, Park JJ, Luckey MA, Park J. 2013. Interleukin-6 expands homeostatic space for peripheral T cells. Cytokine 64:532–540. 10.1016/j.cyto.2013.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhu J, Yamane H, Paul WE. 2010. Differentiation of effector CD4 T cell populations. Annu. Rev. Immunol. 28:445–489. 10.1146/annurev-immunol-030409-101212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.McGeachy MJ, McSorley SJ. 2012. Microbial-induced Th17: superhero or supervillain? J. Immunol. 189:3285–3291. 10.4049/jimmunol.1201834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gaffen SL. 2011. Recent advances in the IL-17 cytokine family. Curr. Opin. Immunol. 23:613–619. 10.1016/j.coi.2011.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Curtis MM, Way SS. 2009. Interleukin-17 in host defence against bacterial, mycobacterial and fungal pathogens. Immunology 126:177–185. 10.1111/j.1365-2567.2008.03017.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hahn AC, Lyons CR, Lipscomb MF. 2008. Effect of Bacillus anthracis virulence factors on human dendritic cell activation. Hum. Immunol. 69:552–561. 10.1016/j.humimm.2008.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.