ABSTRACT
H9N2 avian influenza virus has been prevalent in poultry in many parts of the world since the 1990s and occasionally crosses the host barrier, transmitting to mammals, including humans. In recent years, these viruses have contributed genes to H5N1 and H7N9 influenza viruses, threatening public health. To explore the molecular mechanism for the airborne transmission of H9N2 virus, we compared two genetically close strains isolated from chickens in 2001, A/chicken/Shanghai/7/2001(SH7) and A/chicken/Shanghai/14/2001 (SH14). SH7 is airborne transmissible between chickens, whereas SH14 is not. We used reverse genetics and gene swapping to derive recombinant SH7 (rSH7), rSH14, and a panel of reassortant viruses. Among the reassortant viruses, we identified segments HA and PA as governing the airborne transmission among chickens. In addition, the NP and NS genes also contributed to a lesser extent. Furthermore, the mutational analyses showed the transmissibility phenotype predominantly mapped to the HA and PA genes, with HA-K363 and PA-L672 being important for airborne transmissibility among chickens. In addition, the viral infectivity and acid stability are related to the airborne transmissibility. Importantly, airborne transmission studies of 18 arbitrarily chosen H9N2 viruses from our collections confirmed the importance of both 363K in HA and 672L in PA in determining their levels of transmissibility. Our finding elucidates the genetic contributions to H9N2 transmissibility in chickens and highlights the importance of their prevalence in poultry.
IMPORTANCE Our study investigates the airborne transmissibility of H9N2 viruses in chickens and the subsequent epidemic. H9N2 virus is the donor for several prevalent reassortant influenza viruses, such as H7N9/2013 and the H5N1 viruses. Poultry as the reservoir hosts of influenza virus is closely associated with human society. Airborne transmission is an efficient pathway for influenza virus transmission among flocks and individuals. Exploring the mechanism of the airborne transmission of the H9N2 virus in chickens could provide essential data regarding prevention and control of influenza endemics and pandemics.
INTRODUCTION
H9N2 avian influenza virus in poultry has been endemic to many parts of the world (1) and also transmits to mammalian species, such as swine and canines (2, 3). Since the late 1990s, multiple human cases of H9N2 infection have been reported in Asia (4–7). In recent years, the reassortant viruses that originated from H9N2 and other subtype influenza viruses may extend the host range or increase the virulence of the original virus, thereby threatening both the poultry industry and public health (8–10). It is reported that H9N2 viruses contribute to the genetic and geographic diversity of H5N1 viruses (1, 11). The emerging novel H7N9/2013 viruses share 6 internal genes with the H9N2 virus that is currently circulating in China (12). Some H7N9 viruses potentially transmit among human beings via respiratory droplets (13, 14). Whether the internal genes of H9N2 origin play an important role in the transmission is not clear.
Aerosols, droplets, and direct contact are three transmission routes for influenza A viruses. Among poultry, the fecal/oral route is common for the transmission of avian influenza virus. The airborne route, including aerosols and droplet particles, would cause the efficient transmission of influenza viruses among poultry, and even people, in intensive farms. Airborne transmission would increase the likelihood of interspecies transmission. The transmissibility methods of different subtypes of influenza A viruses in different species are various, and the mechanism underlying airborne transmission of influenza virus is multifactorial. Reverse genetics and serial passage in vivo are applied to study the relationship between viral characteristics and airborne transmissibility (15–18). It is reported that aerosol transmissibility is associated with some viral genes and key amino acids. The amino acids in the receptor binding site (RBD) in hemagglutinin (HA), which contribute to the interaction between viruses and hosts (19), play a pivotal role in cross-species transmission due to sialic acid (SA) receptor differences in hosts (20). Avian influenza viruses preferentially bind α-2,3-linked SA (21), whereas human influenza viruses more readily bind to α-2,6 linked SA (22, 23). Additionally, the amino acid residue at position 226 (H3 numbering), which is in the receptor binding site of HA, is vital for transmissibility (16, 24). Some artificially modified viruses showed that other amino acid positions in HA, PB2, and other genes may be involved in airborne transmission (15, 16, 18, 25), such as the amino acids in N-glycosylation sites of HA and the amino acid residue at position 627 in PB2. The NA and M genes also may contribute to airborne transmissibility to some extent (26–28).
Although reports on H9N2 viruses and their infections are highly documented, studies related to the transmission route and underlining mechanism are scarce. As H9N2 subtype influenza viruses have become prevalent in poultry in many countries in recent years, clarifying the mechanism of transmission would improve our understanding of their biological characteristics of rapid spreading and would help eventually formulate better prevention and control of H9N2 virus. In the current study, we chose two of our previously characterized H9N2 viruses (29), which are genetically close to each other but differ in transmissibility, to explore the mechanism for the airborne transmission of H9N2 viruses in chickens. We further used 18 wild-type H9N2 strains to confirm the effect of 363K in HA and 672L PA for viral airborne transmissibility.
MATERIALS AND METHODS
Ethics statement.
All animal experiments were approved by the Jiangsu Administrative Committee for Laboratory Animals (permission number SYXK-SU-2007-0005) and complied with the Jiangsu Laboratory Animal Welfare and Ethics guidelines of the Jiangsu Administrative Committee of Laboratory Animals.
Viruses.
A/chicken/Shanghai/2/1999 (SH2), A/chicken/Shanghai/3/2000 (SH3), A/chicken/Shanghai/7/2000 (SH7), A/chicken/Shanghai/14/2000 (SH14), A/chicken/Shanghai/1/2001 (SH101), A/chicken/Shanghai/1/2002 (SH1), and A/chicken/Shanghai/3/2002 (SH302), which were isolated from vaccinated flocks in a broiler chicken farm in eastern China, are genetically close to each other. Previous data showed that SH7 and SH1 are airborne transmissible, whereas SH2, SH3, and SH14 are not (29). Other wild-type H9N2 viruses (see Fig. 6) were isolated from chickens in a live bird market and a chicken farm in recent years (29).
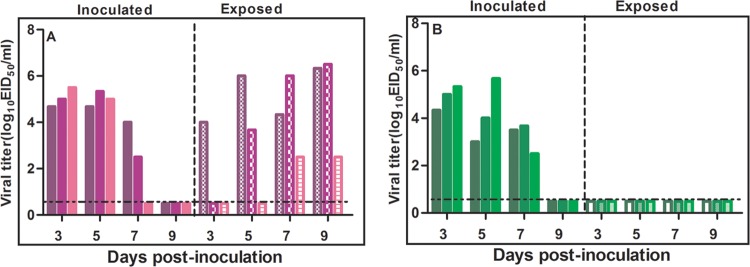
FIG 6.
Key amino acid differences in the HA and PA genes of 15 arbitrarily chosen prevalent H9N2 viruses used for the airborne transmission study. Differences in the amino acid residues in PA and HA of the isolates are shown as single-letter amino acid codes with their positions at the top of the diagram. The amino acid positions of HA are based on the numbering for mature H9 HA.
Reverse genetics and site-directed mutagenesis.
The gene segments of SH7 and SH14 were amplified and cloned into the pHW2000 plasmid as previously described (30, 31). A site-directed mutagenesis kit (Trans Gene, Inc.) was used to create specific mutations in the HA and PA genes, and the primers are available upon request. Virus rescue of a panel of reassortant viruses with either SH7 or SH14 as the backbone virus was performed as previously described (32, 33).
Transmission study.
Six-week-old specific-pathogen-free (SPF) chickens were divided into infected and exposed groups (three chickens per group). On the first day postinoculation (dpi), naive chickens of the exposed group were placed in a cage directly adjacent to an infected group for airborne transmission, with a distance of 50 cm between cages. The infected group was inoculated intranasally and via the conjunctiva with 106 50% egg infective doses (EID50) of viruses. Oropharyngeal swabs were collected every 2 days from both infected and exposed groups beginning 3 dpi, and the virus was titrated in 10-day-old embryonated SPF chicken eggs for EID50/ml counts (34). Sera were collected from all chickens at 21 dpi for the hemagglutinin inhibition (HI) test as outlined in the OIE Manual of Diagnostic Tests and Vaccines for Terrestrial Animals (http://www.oie.int/manual-of-diagnostic-tests-and-vaccines-for-terrestrial-animals/).
Median infective dose for chickens.
To determine the median (50%) infective dose for chickens (CID50), groups of four 6-week-old SPF chickens were inoculated intranasally and via the conjunctiva with dilutions of viruses, and oropharyngeal and cloacal swabs were collected over 11 days. To measure viral shedding, 10-day-old SPF chickens eggs were inoculated with the swabs. The viral CID50 was calculated using the method of Reed and Muench (34).
Acid stability studies.
To determine viral acid stability, viral infectivity was measured as 50% tissue culture infective doses (TCID50). First, viruses were diluted 10-fold in phosphate-buffered saline (PBS). The pH of the diluted viruses was lowered by careful, dropwise addition of 0.1 M citric acid until the desired pH was reached. Different pH buffers were used, ranging from pH 4.4 to 7.2. The viruses then were incubated at 37°C for 1 h. The titers of acid-treated viruses were determined by TCID50 assay in MDCK cells.
Stochastic general airborne transmission probability of prevalent H9N2 virus.
To investigate the airborne transmission potential of prevalent H9N2 viruses, we found the complete sequences of the effective genes of H9N2 viruses in GenBank and analyzed the frequencies of the polymorphisms in their coding effective amino acid residues. We used all of the complete coding sequences from 1996 to 2013.
Nucleotide sequence accession numbers.
The nucleotide sequence data obtained in this study are available from GenBank under the accession numbers KF835981 to KF835986, JQ356873, JQ356882, KJ000697 to KJ000710, and EU753303 to EU753326.
RESULTS
Distinct airborne transmission ability between SH7 and SH14.
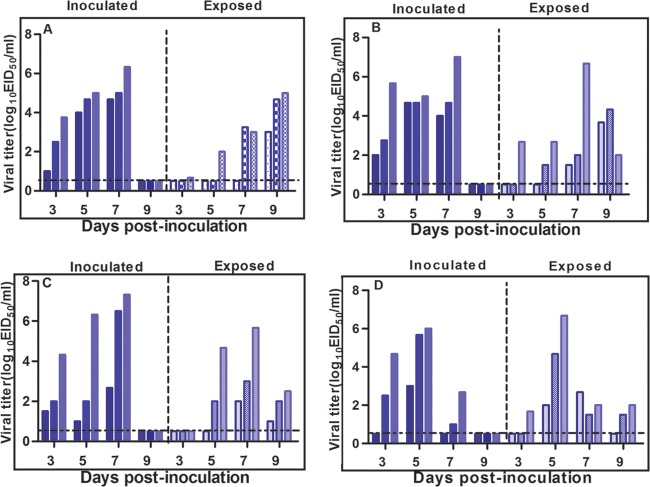
The transmissibility-divergent SH7 and SH14 viruses (29) were used to rescue recombinant SH7 (rSH7) and rSH14 by reverse genetics. Airborne transmission experiments with rSH7 and rSH14 were conducted together with their wild-type counterparts SH7 and SH14 in chickens. The exposed chickens in the rSH7 and SH7 groups shed viruses at 3, 5, 7, and 9 dpi, whereas rSH14 and SH14 groups did not shed viruses (Table 1). The peak titer of viruses in the oropharyngeal swabs of rSH7-exposed chickens reached 106.5 EID50/ml (Fig. 1A), and the HI titers were 320 to 640 on 21 dpi (Table 1). In contrast, the rSH14-exposed chickens did not shed virus (Fig. 1B), and seroconversion was not detected (Table 1). The results showed that rSH7 and rSH14, like their wild-type counterparts SH7 and SH14, had distinct airborne transmission abilities.
TABLE 1.
Airborne transmission study of wild-type and rescued SH7 and SH14 viruses
| Virus and group | Virus shedding on daya: |
Seroconversionb (HI titer) | |||
|---|---|---|---|---|---|
| 3 | 5 | 7 | 9 | ||
| SH7 | |||||
| Inoculated | 3/3 | 3/3 | 2/3 | 0/3 | 3/3 (1,280, 1,280, 1,280) |
| Exposed | 1/3 | 3/3 | 3/3 | 3/3 | 3/3 (640, 640, 1,280) |
| SH14 | |||||
| Inoculated | 3/3 | 3/3 | 2/3 | 0/3 | 3/3 (1,280, 1,280, 1,280) |
| Exposed | 0/3 | 0/3 | 0/3 | 0/3 | 0/3 (<10, <10, <10) |
| rSH7 | |||||
| Inoculated | 3/3b | 3/3 | 2/3 | 0/3 | 3/3 (1,280, 1,280, 1,280) |
| Exposed | 1/3 | 3/3 | 3/3 | 3/3 | 3/3 (320, 320, 640) |
| rSH14 | |||||
| Inoculated | 3/3 | 3/3 | 2/3 | 0/3 | 3/3 (1,280, 1,280, 1,280) |
| Exposed | 0/3 | 0/3 | 0/3 | 0/3 | 0/3 (<10, <10, <10) |
The number of days after chickens were inoculated/exposed. Data are numbers of chickens shedding virus/total number of chickens.
HI antibody titers of chickens on day 21 postinoculation/postexposure.
FIG 1.
Transmission of the rescued wild-type viruses in chickens. We inoculated groups of chickens intranasally and via the conjunctiva with 106 EID50 of rSH7 (A) and rSH14 (B). After 24 h of inoculation, three naive SPF chickens of the exposed group were placed in an adjacent cage as described in the text. Oropharyngeal swabs were collected 3, 5, 7, and 9 dpi. Viral titers of oropharyngeal swabs were determined by endpoint titration in SPF embryonated eggs. Each pattern bar represents the viral titers from an individual chicken. The dashed horizontal line indicates the lower limit of detection.
PA and HA genes of SH7 play a dominant role in airborne transmission.
To determine the critical genes for the airborne transmission of rSH7, we generated 8 reassortant viruses with the backbone of SH7, i.e., 7-14PB2, 7-14PB1, 7-14PA, 7-14HA, 7-14NP, 7-14NA, 7-14M, and 7-14NS, each containing a single gene segment from the SH14 virus. The airborne transmission studies showed that the exposed chickens in both the 7-14PA and 7-14HA groups did not shed viruses or exhibit seroconversion (Table 2). The other six reassortant viruses were able to transmit to exposed chickens via an airborne route (Table 2), indicating the critical role of HA and PA in airborne transmissibility of the SH7 virus. In addition, only two of three exposed chickens in the 7-14NP and 7-14NS groups shed viruses at 7 dpi (Table 2). The HI titers of the exposed chickens in the two groups were only 80 (Table 2), which were much lower than those of the parental rSH7, indicating that NP and NS genes, to a lesser extent, also contribute to the airborne transmission ability.
TABLE 2.
Airborne transmission study of reassortant viruses with the SH7 backbone and one gene from SH14
| Virus and group | Virus shedding on daya: |
Seroconversionb (HI titer) | |||
|---|---|---|---|---|---|
| 3 | 5 | 7 | 9 | ||
| 7-14PB2 | |||||
| Inoculated | 2/3 | 3/3 | 2/3 | 0/3 | 3/3 (1,280, 1,280, 1,280) |
| Exposed | 1/3 | 2/3 | 3/3 | 3/3 | 3/3 (320, 320, 640) |
| 7-14PB1 | |||||
| Inoculated | 2/3 | 3/3 | 3/3 | 0/3 | 3/3 (320, 640, 1,280) |
| Exposed | 1/3 | 3/3 | 3/3 | 2/3 | 3/3 (80, 160, 160) |
| 7-14PA | |||||
| Inoculated | 2/3 | 3/3 | 3/3 | 0/3 | 3/3 (320, 640, 640) |
| Exposed | 0/3 | 0/3 | 0/3 | 0/3 | 0/3 (<10, <10, <10) |
| 7-14HA | |||||
| Inoculated | 1/3 | 3/3 | 2/3 | 0/3 | 3/3 (1,280, 1,280, 1,280) |
| Exposed | 0/3 | 0/3 | 0/3 | 0/3 | 0/3 (<10, <10, <10) |
| 7-14NP | |||||
| Inoculated | 3/3 | 3/3 | 2/3 | 0/3 | 3/3 (320, 320, 320) |
| Exposed | 0/3 | 1/3 | 2/3 | 0/3 | 2/3 (<10, 40, 80) |
| 7-14NA | |||||
| Inoculated | 3/3 | 3/3 | 2/3 | 0/3 | 3/3 (1,280, 1,280, 1,280) |
| Exposed | 0/3 | 1/3 | 3/3 | 1/3 | 3/3 (80, 80, 160) |
| 7-14M | |||||
| Inoculated | 3/3 | 2/3 | 3/3 | 0/3 | 3/3 (640, 1,280, 1,280) |
| Exposed | 2/3 | 2/3 | 3/3 | 2/3 | 3/3 (160, 320, 320) |
| 7-14NS | |||||
| Inoculated | 3/3 | 3/3 | 2/3 | 0/3 | 3/3 (640, 640, 1,280) |
| Exposed | 0/3 | 0/3 | 2/3 | 1/3 | 3/3 (20, 40, 80) |
The number of days after chickens were inoculated/exposed. Data are numbers of chickens shedding virus/total number of chickens.
HI antibody titers of chickens on day 21 postinoculation/postexposure.
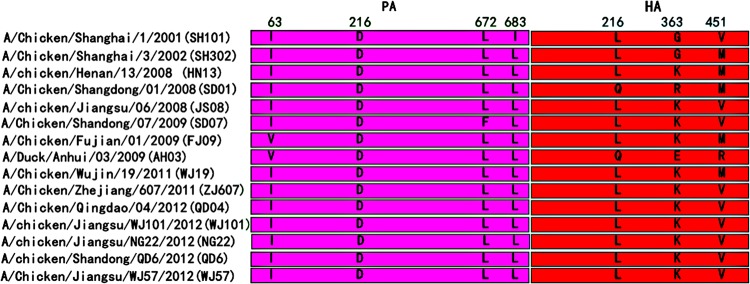
To further determine the genes and the cooperation of these genes required for airborne transmission ability, we subsequently used SH14 as a backbone to rescue reassortant viruses with PA, HA, NP, and NS genes from SH7, generating 14-7HA, 14-7PA, 14-7(PA+HA), 14-7(PA+HA+NP), 14-7(PA+HA+NS), and 14-7(PA+HA+NP+NS). Neither virus shedding nor seroconversion was detected in any of the chickens exposed to 14-7HA and 14-7PA (Table 3), whereas virus shedding and seroconversion were detectable in the exposed chickens with the remaining four reassortant viruses bearing both the HA and PA genes from rSH7 (Table 3). These results suggested that both PA and HA are critical for viral airborne transmissibility. In the 14-7(PA+HA) virus-infected group, only one of three exposed chickens at 3 dpi shed viruses, and the viral titer was just 100.67 EID50/ml (Fig. 2A). All three exposed chickens shed viruses until 9 dpi, and the HI titer of seroconversion was relatively low (Table 3). On the other hand, upon introducing the NP or NS gene, or both, from SH7 to SH14, the exposed chickens were infected by the airborne route. In groups 14-7(PA+HA+NP) and 14-7(PA+HA+NS), the exposed chickens shed viruses at 7 dpi and also had higher HI titers of seroconversion than those in group 14-7(PA+HA) (Fig. 2B and C and Table 3). In group 14-7(PA+HA+NP+NS), all of the exposed chickens shed viruses at 5 dpi, with the highest viral titer and the highest HI titer of seroconversion being 1,280 (Fig. 2D and Table 3). Our findings suggest that both PA and HA of SH7 are essential for its airborne transmission among chickens, and NP and NS may contribute to a lesser extent in this regard.
TABLE 3.
Airborne transmission study of reassortant viruses with the SH14 backbone and genes from SH7
| Virus and group | Virus shedding on daya: |
Seroconversionb (HI titer) | |||
|---|---|---|---|---|---|
| 3 | 5 | 7 | 9 | ||
| 14-7HA | |||||
| Inoculated | 1/3 | 2/3 | 3/3 | 0/3 | 3/3 (640, 640, 1,280) |
| Exposed | 0/3 | 0/3 | 0/3 | 0/3 | 0/3 (<10, <10, <10) |
| 14-7PA | |||||
| Inoculated | 1/3 | 2/3 | 3/3 | 0/3 | 3/3 (640, 640, 1,280) |
| Exposed | 0/3 | 0/3 | 0/3 | 0/3 | 0/3 (<10, <10, <10) |
| 14-7(PA+HA) | |||||
| Inoculated | 3/3 | 3/3 | 3/3 | 0/3 | 3/3 (320, 640, 1,280) |
| Exposed | 0/3 | 1/3 | 2/3 | 3/3 | 3/3 (20, 40, 40) |
| 14-7(PA+HA+NP) | |||||
| Inoculated | 3/3 | 3/3 | 3/3 | 0/3 | 3/3 (640, 1,280, 1,280) |
| Exposed | 1/3 | 2/3 | 3/3 | 3/3 | 3/3 (40, 80, 160) |
| 14-7(PA+HA+NS) | |||||
| Inoculated | 1/3 | 3/3 | 3/3 | 0/3 | 3/3 (160, 320, 1,280) |
| Exposed | 0/3 | 2/3 | 3/3 | 3/3 | 3/3 (20, 80, 80) |
| 14-7(PA+HA+NP+NS) | |||||
| Inoculated | 1/3 | 3/3 | 2/3 | 0/3 | 3/3 (640, 640, 1,280) |
| Exposed | 1/3 | 3/3 | 3/3 | 2/3 | 3/3 (160, 320, 1,280) |
The number of days after chickens were inoculated/exposed. Data are numbers of chickens shedding virus/total number of chickens.
HI antibody titers of chickens on day 21 postinoculation/exposure.
FIG 2.
Transmission of reassortant viruses with the SH14 backbone. We inoculated groups of chickens intranasally and via the conjunctiva with 106 EID50 14-7(PA+HA) (A), 14-7(PA+HA+NP) (B), 14-7(PA+HA+NS) (C), or 14-7(PA+HA+NP+NS) (D). After 24 h of inoculation, three naive SPF chickens of the exposed group were placed in an adjacent cage as described in the text. Oropharyngeal swabs were collected 3, 5, 7, and 9 dpi. Viral titers of oropharyngeal swabs were determined by endpoint titration in SPF embryonated eggs. Each pattern bar represents the virus titers from an individual chicken. The dashed horizontal line indicates the lower limit of detection.
Amino acid at position 363K in HA and 672L in PA are vital for airborne transmission of SH7.
For SH7, together with the other three reported viruses of SH1, SH2, and SH3, 7 amino acids in PA and HA commonly were different between the airborne transmissible viruses and those that did not have airborne transmissibility (29) (Fig. 3). To pinpoint the effective amino acid residues in HA and PA involved in airborne transmissibility, we generated a series of mutants which were independently modified. Seven different amino acids in the seven mutant strains were different from those in SH14 and were named 7HAL216Q, 7HAK363R, 7HAV451M, 7PAI63V, 7PAD216N, 7PAL672F, and 7PAI683L, and we tested their transmissibility in chickens (Table 4). Even the Q216L mutation would be likely to influence the receptor binding preference (23). The exposed chickens in the 7HAL216Q group were infected (Table 4). These results indicated that leucine (L) at position 216 (226 in H3 numbering) in HA does not affect the airborne transmission of SH7 in chickens. Two of three exposed chickens in the 7HAv451M group shed viruses at 7 dpi, and their serum HI titers at 21 dpi were no more than 40 (Table 4). However, the mutation of position 363 in HA of SH7 resulted in no virus shedding by the exposed chicken and no seroconversion (Table 4). In the groups of viruses containing a mutation in PA, all of the exposed chickens in 7PAI63V and 7PAD216N groups shed viruses and also seroconverted (Table 4). However, viral shedding and seroconversion were detected in only one exposed chicken of the 7PAI683L group, and the HI titer was only 40 by 21 dpi (Table 4). No virus was detected in the exposed chickens of the 7PAL672F group, and seroconversion was less than 10 (Table 4). Taken together, the data indicated that lysine (K) at position 363 in HA and L at position 672 in PA have a significant role in airborne transmission in chickens, whereas others, such as 451V in HA and 683I in PA, play a minor role.
FIG 3.
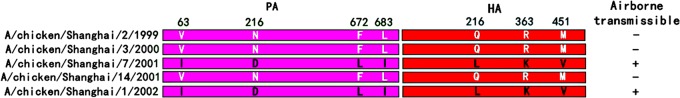
Schematic diagram of commonly divergent amino acids of the HA and PA genes between airborne-transmissible viruses and viruses that are not airborne transmissible. Differences in the amino acid residues in PA and HA between airborne-transmissible viruses and viruses that are not airborne transmissible are shown as single-letter amino acid codes with their positions at the top of the diagram. The white and black letters indicate the amino acid regions originating from transmissible viruses and nontransmissible viruses, respectively. The amino acid positions of HA are based on the numbering of mature H9 HA.
TABLE 4.
Airborne transmission of reassortant SH7 viruses with site-directed mutations in HA or PA gene
| Virus and group | Virus shedding on daya: |
Seroconversionb (HI titer) | |||
|---|---|---|---|---|---|
| 3 | 5 | 7 | 9 | ||
| 7HAL226Qc | |||||
| Inoculated | 1/3 | 3/3 | 3/3 | 0/3 | 3/3 (1,280, 1,280, 1,280) |
| Exposed | 0/3 | 3/3 | 3/3 | 1/3 | 3/3 (320, 320, 640) |
| 7HAK363R | |||||
| Inoculated | 2/3 | 3/3 | 3/3 | 0/3 | 3/3 (1,280, 1,280, 1,280) |
| Exposed | 0/3 | 0/3 | 1/3 | 0/3 | 0/3 (<10, <10, <10) |
| 7HAV451M | |||||
| Inoculated | 2/3 | 3/3 | 3/3 | 0/3 | 3/3 (1,280, 1,280, 1,280) |
| Exposed | 0/3 | 0/3 | 2/3 | 0/3 | 2/3 (<10, 20, 40) |
| 7PAI63V | |||||
| Inoculated | 3/3 | 3/3 | 2/3 | 0/3 | 3/3(320, 640, 1,280) |
| Exposed | 1/3 | 2/3 | 3/3 | 2/3 | 3/3 (80, 160, 640) |
| 7PAD216N | |||||
| Inoculated | 3/3 | 3/3 | 2/3 | 0/3 | 3/3 (320, 640, 640) |
| Exposed | 0/3 | 2/3 | 3/3 | 2/3 | 3/3 (40, 160, 160) |
| 7PAL672F | |||||
| Inoculated | 1/3 | 3/3 | 3/3 | 0/3 | 3/3 (320, 640, 1,280) |
| Exposed | 0/3 | 0/3 | 0/3 | 0/3 | 0/3 (<10, <10, <10) |
| 7PAI683L | |||||
| Inoculated | 1/3 | 3/3 | 3/3 | 0/3 | 3/3 (640, 640, 1,280) |
| Exposed | 0/3 | 0/3 | 1/3 | 1/3 | 2/3 (<10, 20, 40) |
The number of days after chickens were inoculated/exposed. Data are numbers of chickens shedding virus/total number of chickens.
HI antibody titers of chickens on day 21 postinoculation/postexposure.
The amino acids are represented by individual letter abbreviations. L, leucine; Q, glutamine; K, lysine; R, arginine; V, valine; M, methionine; I, isoleucine; D, aspartic acid, N, asparaginate; F, phenylalanine.
PA-L672F and HA-K363R decrease viral infectivity.
To explore why the site mutations in PA and HA abolished airborne transmissibility, we compared the viral shedding kinetics and infectivities of SH7, SH14, 7PAL672F, and 7HAK363R. The titers of virus shed from the oropharynx were higher than those from the cloaca for all four viruses (Fig. 4). The results revealed that the tissue tropisms of 7PAL672F and 7HAK363R were similar to those of SH7 and SH14, which favor the respiratory tract. At 5 dpi, the viral titers of chickens of group SH7 were higher than those of group SH14 (Fig. 4). The chickens that were inoculated with 7PAL672F and 7HAK363R shed lower levels of virus than chickens in the SH14 group (Fig. 4). We further used CID50 titers to evaluate the infectivities of the four viruses. The CID50 of SH7 is 102.0 EID50, and that of SH14 is 102.33 EID50 (Table 5), indicating that the infectivity of chickens by SH7 is more than twice as likely as that by SH14. The site mutation viruses of 7PAL672F and 7HAK363R, which were not transmissible by an airborne pathway, showed higher CID50 titers than the parental SH7 (Table 5). These results suggested that the site mutations at position 672 in PA and position 363 in HA decreased the viral infectivities. If equivalent titers of SH7, SH14, 7PAL672F, and 7HAK363R were used to inoculate chickens, the SH7 virions would be most successful at infecting chickens.
FIG 4.
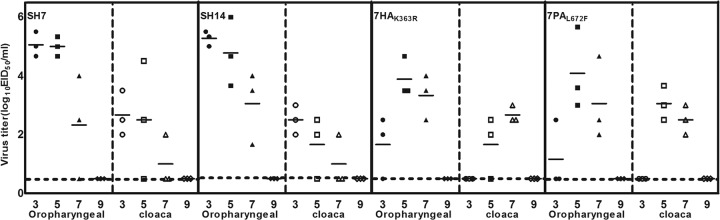
Virus-shedding titers of SPF chickens inoculated with SH7, SH14, and mutated viruses. The SPF chickens were inoculated with 106 EID50 SH7, SH14, 7HAK363R, and 7PAL672F. Oropharyngeal swabs and cloacal swabs were collected 3, 5, 7, and 9 dpi. Viral titers of swabs were determined by endpoint titration in SPF embryonated eggs. Each pattern bar represents the viral titers from an individual chicken. The dashed horizontal line indicates the lower limit of detection.
TABLE 5.
Viral infectivity and airborne transmissibility
| Virus | CID50 (EID50) | Airborne transmission |
|---|---|---|
| SH7 | 102.0 | + |
| SH14 | 102.33 | − |
| 7PAL672F | 103.67 | − |
| 7HAK363R | 102.33 | − |
HA-K363R decreases viral acid stability.
Amino acid position 363 is positioned at the N terminus of the HA2 subunit of hemagglutinin, which is thought to be the acid active site for fusion activity (35). To determine the relationship between viral acid stability and airborne transmissibility, we incubated aliquots of SH7, SH14, and 7HAK363R individually in pH-adjusted buffers ranging from pH 7.2 to pH 4.4 for 1 h, after which we measured the titers of the viruses (Fig. 5). The infectivity of the 7HAK363R virus was reduced by 5-fold after exposure to the pH 6.2 buffer, reduced by >100-fold after exposure to the pH 6.0 buffer, and completely eliminated by the pH 4.8 buffer. Wild-type SH7 was more resistant to acid inactivation than 7HAK363R was, as SH7 lost <1 log10 infectivity in the pH 6.0 buffer, lost <2 log10 infectivity in the pH 5.2 buffer, and became completely inactivated by the pH 4.8 buffer. Similar to 7HAK363R, SH14 was sensitive to acid. It lost >2 log10 infectivity at pH 6.2 and continuously lost infectivity in the lower pH buffer. After incubation at pH 5.0, SH14 lost all infectivity.
FIG 5.
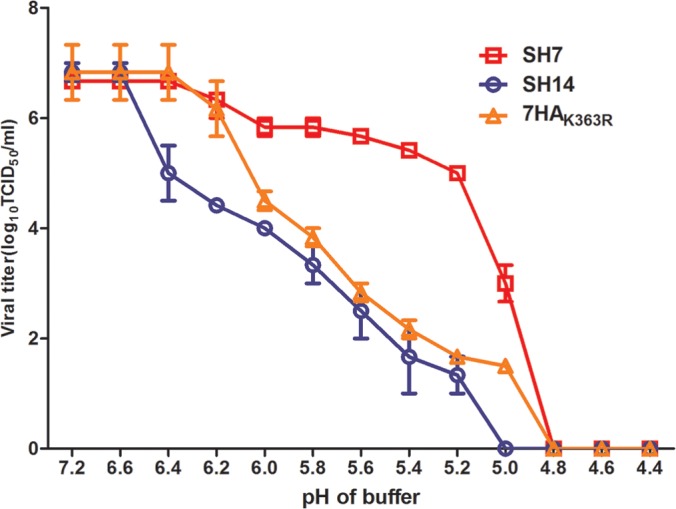
Acid stability of the H9N2 influenza viruses. Prestandardized virus stock was diluted in PBS buffer adjusted to the indicated pH and incubated for 1 h at 37°C. The remaining infectious virus titer was quantified by performing TCID50 assays with MDCK cells.
Residue 363K in HA and 672L in PA are critical for airborne transmission in other prevalent H9N2 viruses.
Our study of SH7/SH14 showed that residue 363K of HA and 672L of PA are critical for airborne transmission. To test this finding more broadly, we arbitrarily chose 18 prevalent H9N2 isolates from our collections to examine their airborne transmissibility in chickens. We also analyzed the 7 divergent amino acids of the 18 H9N2 viruses (Fig. 6). Exposed chickens in groups SH2, SH3, SH101, SH302, SD01, SD07, and AH03 did not shed viruses or seroconvert (Table 6), indicating that the 7 viruses were incapable of airborne transmission. Residue 672 in PA was 672F in SD07, and the other six viruses did not contain the 363K residue in HA (Fig. 6). Virus-shedding viruses and seroconversion of the exposed chickens in the groups of the other 11 viruses were detectable. This finding suggested that the exposed chickens in each of the 11 groups were infected by the airborne route (Table 6). All 11 of the viruses that bear both 363K in HA and 672L in PA simultaneously were readily airborne transmissible, even though the number of virus-shedding chickens and the HI titers of exposed chickens varied (Table 6). The results add more data supporting the importance of position 363 in HA and 672 in PA for the airborne transmissibility of the H9N2 virus. Three of four exposed chickens in the FJ09 and QD4 groups, and only two in the HN13 and SD01 groups, shed viruses and seroconverted (Table 6), which revealed different airborne transmission efficiencies of these viruses. Although the four viruses both contained the 363K residue in HA and the 672L residue in PA, the amino acid at position 451 in HA or at position 683 in PA were the same as those of SH14 (Fig. 6), suggesting the minor function of these two positions.
TABLE 6.
Airborne transmission of 18 arbitrarily chosen prevalent H9N2 viruses
| Virus and group | Virus shedding on daya: |
Seroconversionb (HI titer) | Airborne transmissibility | |||
|---|---|---|---|---|---|---|
| 3 | 5 | 7 | 9 | |||
| SH2 | ||||||
| Inoculated | 3/4 | 4/4 | 2/4 | 0/4 | 4/4 (40, 160, 160, 320) | − |
| Exposed | 0/4 | 0/4 | 0/4 | 0/4 | 0/4 (<10, <10, <10, <10) | |
| SH3 | ||||||
| Inoculated | 4/4 | 3/4 | 2/4 | 0/4 | 4/4 (80, 320, 320, 640) | − |
| Exposed | 0/4 | 0/4 | 0/4 | 0/4 | 0/4 (<10, <10, <10, <10) | |
| SH101 | ||||||
| Inoculated | 2/4 | 4/4 | 4/4 | 0/4 | 4/4 (160, 320, 640, 640) | − |
| Exposed | 0/4 | 0/4 | 0/4 | 0/4 | 0/4 (<10, <10, <10, <10) | |
| SH1 | ||||||
| Inoculated | 4/4 | 4/4 | 1/4 | 0/4 | 4/4 (1,280, 1,280, 1,280, 1,280) | + |
| Exposed | 4/4 | 4/4 | 3/4 | 1/4 | 4/4 (160, 320, 640, 640) | |
| SH302 | ||||||
| Inoculated | 3/4 | 4/4 | 4/4 | 1/4 | 4/4 (320, 640, 640, 640) | − |
| Exposed | 0/4 | 0/4 | 0/4 | 0/4 | 0/4 (<10, <10, <10, <10) | |
| HN13 | ||||||
| Inoculated | 3/4 | 4/4 | 4/4 | 0/4 | 4/4 (320, 320, 640, 640) | + |
| Exposed | 0/4 | 0/4 | 2/4 | 1/4 | 2/4 (<10, <10, 20, 80) | |
| SD01 | ||||||
| Inoculated | 4/4 | 4/4 | 3/4 | 0/4 | 4/4 (640, 640, 640, 1,280) | − |
| Exposed | 0/4 | 0/4 | 0/4 | 0/4 | 0/4 (<10, <10, <10, <10) | |
| JS08 | ||||||
| Inoculated | 4/4 | 3/4 | 4/4 | 4/4 | 4/4 (320, 640, 640, 1,280) | + |
| Exposed | 1/4 | 4/4 | 4/4 | 4/4 | 4/4 (80, 160, 320, 320) | |
| SD07 | ||||||
| Inoculated | 3/4 | 4/4 | 1/4 | 0/4 | 4/4 (40, 160, 320, 640) | − |
| Exposed | 0/4 | 0/4 | 0/4 | 0/4 | 0/4 (<10, <10, <10, <10) | |
| FJ09 | ||||||
| Inoculated | 4/4 | 4/4 | 4/4 | 3/4 | 4/4 (320, 320, 640, 640) | + |
| Exposed | 0/4 | 0/4 | 3/4 | 1/4 | 3/4 (<10, 40, 80, 80) | |
| AH03 | ||||||
| Inoculated | 2/4 | 3/4 | 4/4 | 1/4 | 4/4 (160, 320, 640, 1,280) | − |
| Exposed | 0/4 | 0/4 | 0/4 | 0/4 | 0/4 (<10, <10, <10) | |
| WJ19 | ||||||
| Inoculated | 4/4 | 4/4 | 4/4 | 0/4 | 4/4 (640, 640, 1,280, 1,280) | + |
| Exposed | 0/4 | 4/4 | 4/4 | 4/4 | 4/4 (20, 80, 160, 320) | |
| ZJ607 | ||||||
| Inoculated | 4/4 | 4/4 | 2/4 | 0/4 | 4/4 (640, 640, 1,280, 1,280) | + |
| Exposed | 0/4 | 2/4 | 4/4 | 4/4 | 4/4 (160, 320, 320, 1,280) | |
| QD4 | ||||||
| Inoculated | 4/4 | 4/4 | 4/4 | 1/4 | 4/4 (320, 320, 640, 640) | + |
| Exposed | 3/4 | 0/4 | 0/4 | 1/4 | 3/4 (<10, 20, 160, 160) | |
| WJ101 | ||||||
| Inoculated | 3/4 | 0/4 | 3/4 | 1/4 | 3/4 (80, 160, 320, 640) | + |
| Exposed | 0/4 | 4/4 | 1/4 | 1/4 | 2/4 (<10, <10, 40, 80) | |
| NG22 | ||||||
| Inoculated | 4/4 | 4/4 | 4/4 | 4/4 | 4/4 (160, 320, 320, 640) | + |
| Exposed | 1/4 | 1/4 | 2/4 | 4/4 | 4/4 (80, 320, 320, 640) | |
| QD6 | ||||||
| Inoculated | 4/4 | 4/4 | 4/4 | 3/4 | 4/4 (320, 640, 640, 1,280) | + |
| Exposed | 4/4 | 4/4 | 3/4 | 1/4 | 4/4 (320, 320, 640, 640, 1,280) | |
| WJ57 | ||||||
| Inoculated | 4/4 | 4/4 | 3/4 | 3/4 | 4/4 (160, 640, 1,280, 1,280) | + |
| Exposed | 3/4 | 4/4 | 2/4 | 2/4 | 4/4 (80, 80, 320, 320) | |
The number of days after chickens were inoculated/exposed. Data are numbers of chickens shedding virus/total number of chickens.
HI antibody titers of chickens on day 21 postinoculation/postexposure.
Potentially airborne-transmissible H9N2 viruses were prevalent in recent years.
We found 739 distinct complete coding PA sequences and 1,975 distinct complete coding HA sequences from 1996 to 2013. We found 611 H9N2 strains with complete PA and HA complete sequences in GenBank, including 403 PA sequences, 1,504 HA sequences, and 352 H9N2 strains with both PA and HA sequences from China. Among these sequences, the amino acid residue at position 672 of PA is L, P, or F, and the amino acid residue at position 363 of HA is K, R, T, E, V, or N. We analyzed the proportion of sequences with PA 672L and/or HA 363K by year. Some strains with PA 672F were isolated even in 1996 and 1997, whereas most H9N2 viruses had PA 672L (Fig. 7A). The proportion of 363K in HA increased gradually (Fig. 7A). Among the 130 HA sequences obtained in 2009, 38 sequences with 363T, which were genetically close to each other and were all isolated from South Korea, lowered the proportion of HA 363K in 2009 (36). In 1998, H9N2 influenza virus was endemic to China, and the proportion of strains with both PA 672L and HA 363K PA reached its first peak as well (Fig. 7B). The trend of the proportions of H9N2 strains with both PA 672L and HA 363K was stable and then rose sharply rose in 2003 (Fig. 7A). In the past 4 years, the proportions of HA 363K alone and both PA 672L and HA 363K have been stable and are present in more than 80% of H9N2 strains worldwide and in China (Fig. 7A and B). These findings indicate the prevalence of airborne-transmissible H9N2 viruses.
FIG 7.
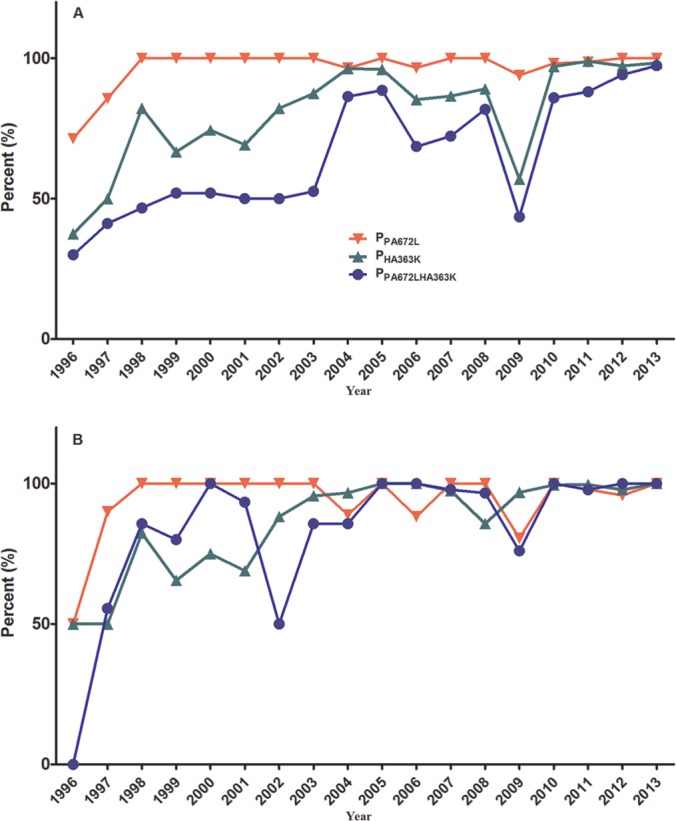
Proportions of H9N2 viruses with PA 672L and HA 363K in GenBank from 1996 to 2013. There were 739 distinct complete PA sequences, 1,975 HA sequences, and 611 H9N2 strains with both PA and HA sequences (A), and there were 403 PA sequences, 1,504 HA sequences, and 352 H9N2 strains from China (B). PPA672L is the proportion of PA sequences with 672L in 739 PA complete coding sequences in 1 year. PHA363K is the proportion of HA sequences with 363K in 1,976 HA complete coding sequences in 1 year. PPA672LHA363K is the proportion of H9N2 viruses with both PA 672L and HA 363K in 611 H9N2 strains in 1 year.
DISCUSSION
Previous studies on influenza viruses of mammalian origin have shown that airborne transmission is associated with the biological properties of the virus and other factors (37–39). To ascertain the underlying mechanism of the airborne transmission of the prevalent H9N2 avian influenza virus (40), we generated a panel of reassortant viruses derived from two H9N2 viruses, SH7 and SH14. We assessed airborne transmissibility by determining viral shedding in oropharyngeal swabs and seroconversion in this study. The viral shedding and seroconversion titers were not significantly different between chickens in the SH7 and SH14 infection groups (Fig. 1 and 4). Airborne transmission was not obviously associated with viral shedding in inoculated chickens under the experimental conditions of this study. The viruses possessing both the PA and HA genes of SH7 were able to infect neighboring chickens through the airborne route (Tables 2 and 3). In addition, the presence of the NP and NS genes of SH7 enhanced the efficiency of airborne transmission for recombined SH14 (Fig. 2B, C, and D).
We further identified the effective amino acids of position 363 in HA and position 672 in PA for airborne transmission (Table 4). The two amino acids influenced the viral shedding and infectivity for chickens (Fig. 4 and Table 5). The viral shedding of SH7 and SH14 were not significantly different; however, the infectivity of SH7 was superior. In addition, the levels of infectivity and viral shedding of SH7 were higher than those of 7HAK363R, which did not have airborne transmissibility. The substitution of E363K in HA significantly altered the airborne transmission capability of SH7 (Table 4) and also reduced its acid stability (Fig. 5). The infectivity of SH7 was found to be stable in a wide range of different pH buffers (pH 7.2 to 5.2). However, 7HA K363R and SH14 not only were unable to transmit by the airborne pathway but also were sensitive to acid inactivation. The sustained and efficient airborne transmission of virus requires a certain level of stability of the HA protein in an acidic environment due to the varied pHs of different hosts' respiratory tracts (16). Amino acid position 363 (position 43 in HA2) is located at the secondary structure α-helix in the HA2 stalk (41) and participates in the conformational change of the fusion peptide projected toward the target membrane (42, 43). The mutations of α-helix residues can alter the pH of activation of the HA protein (44–47). In addition, the pH of activation of the HA protein is associated with viral replication, virulence, and transmissibility (15, 16, 41, 48, 49). In this study, the acid stability of SH7 would allow it to maintain infectivity in the chickens' respiratory tracts for a long time. Amino acid position 672 of PA also was related to the airborne transmission of SH7 (Table 4). Like the alteration K363R in HA, L672F in PA decreased infectivity and viral shedding for chickens nearly 50-fold, but it did not change the tissue tropism. PA is implicated in viral RNA replication, transcription, host proteolytic activity, and viral pathogenicity (50–53). When the influenza A virus PA C-terminal region (residues 257 to 716) exists in the RNP complex with the PB1 N terminus, it has a fold resembling a dragon's head of the RNP complex. Position 672 is positioned in the PB1 binding region (54) and is responsible for a temperature-sensitive phenotype (55). Position 672 in PA would affect the viral stability in the environment, leading to diverse abilities for airborne transmissibility. Thus, even though the chickens inoculated with H9N2 viruses shed similar doses of virus, the stability and fitness of the viruses in airborne particles and in the hosts' respiratory tracts were varied, resulting in different levels of transmissibility.
Among the tested wild-type H9N2 viruses, both 363K in HA and 672L in PA were critical for airborne transmissibility, but the transmission efficiencies of the viruses were different (viral shedding and seroconversion) (Table 6). The results indicated that other factors influence airborne transmission, such as position 451 in HA and 683 in PA (Tables 3 and 6). In addition, amino acid position 216 (226 according to H3 numbering) of HA is responsible for receptor binding specificity (56) and is associated with airborne transmission in mammals (15, 37, 57). An L residue at position 216 in HA is responsible for human virus-like receptor specificity (56). In this study, the amino acid residue at position 216 is an L in the airborne-transmissible strain SH7, which contributes to the airborne transmissibility of other influenza A virus subtypes in mammals (15, 37, 57). However, the L216Q substitution in HA did not alter airborne transmissibility of SH7 in chickens (Table 4).
The genes of SH7 and SH14 clustered together with A/chicken/Shanghai/F/98, which belongs to the BJ/94 lineage (29, 58). H9N2 viruses circulating in recent years in China are mainly descendants of BJ/94-like and G1-like genotypes (58–61). The representative strain of the BJ/94-like genotype is A/chicken/Beijing/1/94, and the representative strain of the G1-like genotype is A/quail/Hong Kong/G1/97. Both of the strains contain residue 672L in PA and 363K in HA. The first isolated H9N2 virus, A/turkey/Wisconsin/1/1966, and the widely used reference strain A/duck/Hong Kong/Y280/97 did not contain 672L in PA or 363K in HA. In a previous study, wild-type A/duck/Hong Kong/702/79 (H9N2) (HK702), which cannot transmit by the airborne route in chickens, was adapted in quails and chickens through 23 serial passages. The adapted HK702 strain, which is airborne transmissible in chickens, bears an E363K substitution in HA as well (18). From 1966 to 1995, the availability of the complete sequences of PA and HA was limited. Owing to the epidemic of H9N2 subtype influenza virus in several countries and the development of sequencing techniques, more complete H9N2 coding sequences have been submitted to GenBank since 1996. The proportion of strains with both PA 672L and HA 363K increased in 1998, which coincided with the epidemic of H9N2 viruses (29). In recent years, H9N2 viruses with both 672L in PA and 363K in HA are preponderant (Fig. 7A and B), indicating the prevalence of airborne-transmission H9N2 strains.
Recently, H9N2 viruses have been known to donate internal genes of other influenza A virus subtypes, such as H5N1, H5N2, and H7N9, in humans and poultry (2, 11, 40, 62). We hypothesized that the HA, PA, NP, and NS genes associated with airborne transmission as demonstrated here are transferred to other influenza viruses. Our results highlight that both 672L in PA and 363K in HA are critical residues for airborne-transmissible H9N2 virus and elucidated the current status of H9N2 avian influenza virus.
ACKNOWLEDGMENTS
This study was supported by the National Natural Science Foundation of China (31101827), Chinese National High-Tech R&D Program (863 Program; 2011AA10A200), and the Research and Innovation Project of College Students in Jiangsu Province (no. CXZZ13-0912).
Footnotes
Published ahead of print 11 June 2014
REFERENCES
- 1.Dong G, Luo J, Zhang H, Wang C, Duan M, Deliberto TJ, Nolte DL, Ji G, He H. 2011. Phylogenetic diversity and genotypical complexity of H9N2 influenza A viruses revealed by genomic sequence analysis. PLoS One 6:e17212. 10.1371/journal.pone.0017212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yu H, Zhou YJ, Li GX, Ma JH, Yan LP, Wang B, Yang FR, Huang M, Tong GZ. 2011. Genetic diversity of H9N2 influenza viruses from pigs in China: a potential threat to human health? Vet. Microbiol. 149:254–261. 10.1016/j.vetmic.2010.11.008 [DOI] [PubMed] [Google Scholar]
- 3.Zhang K, Zhang Z, Yu Z, Li L, Cheng K, Wang T, Huang G, Yang S, Zhao Y, Feng N, Fu J, Qin C, Gao Y, Xia X. 2013. Domestic cats and dogs are susceptible to H9N2 avian influenza virus. Virus Res. 175:52–57. 10.1016/j.virusres.2013.04.004 [DOI] [PubMed] [Google Scholar]
- 4.Blair PJ, Putnam SD, Krueger WS, Chum C, Wierzba TF, Heil GL, Yasuda CY, Williams M, Kasper MR, Friary JA, Capuano AW, Saphonn V, Peiris M, Shao H, Perez DR, Gray GC. 2013. Evidence for avian H9N2 influenza virus infections among rural villagers in Cambodia. J. Infect. Public Health 6:69–79. 10.1016/j.jiph.2012.11.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Butt KM, Smith GJ, Chen H, Zhang LJ, Leung YH, Xu KM, Lim W, Webster RG, Yuen KY, Peiris JS, Guan Y. 2005. Human infection with an avian H9N2 influenza A virus in Hong Kong in 2003. J. Clin. Microbiol. 43:5760–5767. 10.1128/JCM.43.11.5760-5767.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen Y, Zheng Q, Yang K, Zeng F, Lau SY, Wu WL, Huang S, Zhang J, Chen H, Xia N. 2011. Serological survey of antibodies to influenza A viruses in a group of people without a history of influenza vaccination. Clin. Microbiol. Infect. 17:1347–1349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Peiris M, Yuen KY, Leung CW, Chan KH, Ip PL, Lai RW, Orr WK, Shortridge KF. 1999. Human infection with influenza H9N2. Lancet 354:916–917. 10.1016/S0140-6736(99)03311-5 [DOI] [PubMed] [Google Scholar]
- 8.Zhao G, Gu X, Lu X, Pan J, Duan Z, Zhao K, Gu M, Liu Q, He L, Chen J, Ge S, Wang Y, Chen S, Wang X, Peng D, Wan H, Liu X. 2012. Novel reassortant highly pathogenic H5N2 avian influenza viruses in poultry in China. PLoS One 7:e46183. 10.1371/journal.pone.0046183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhao S, Suo L, Jin M. 2012. Genetic characterization of a novel recombinant H5N2 avian influenza virus isolated from chickens in Tibet. J. Virol. 86:13836–13837. 10.1128/JVI.02595-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhang Y, Wang N, Cao J, Chen H, Jin M, Zhou H. 2013. Genetic characterization of H1N2 swine influenza virus isolated in China and its pathogenesis and inflammatory responses in mice. Arch. Virol. 158:1965–1972. 10.1007/s00705-013-1685-8 [DOI] [PubMed] [Google Scholar]
- 11.Zhang P, Tang Y, Liu X, Liu W, Zhang X, Liu H, Peng D, Gao S, Wu Y, Zhang L, Lu S. 2009. A novel genotype H9N2 influenza virus possessing human H5N1 internal genomes has been circulating in poultry in eastern China since 1998. J. Virol. 83:8428–8438. 10.1128/JVI.00659-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gao R, Cao B, Hu Y, Feng Z, Wang D, Hu W, Chen J, Jie Z, Qiu H, Xu K, Xu X, Lu H, Zhu W, Gao Z, Xiang N, Shen Y, He Z, Gu Y, Zhang Z, Yang Y, Zhao X, Zhou L, Li X, Zou S, Zhang Y, Yang L, Guo J, Dong J, Li Q, Dong L, Zhu Y, Bai T, Wang S, Hao P, Yang W, Han J, Yu H, Li D, Gao GF, Wu G, Wang Y, Yuan Z, Shu Y. 2013. Human infection with a novel avian-origin influenza A (H7N9) virus. N. Engl. J. Med. 368:1888–1897. 10.1056/NEJMoa1304459 [DOI] [PubMed] [Google Scholar]
- 13.Watanabe T, Kiso M, Fukuyama S, Nakajima N, Imai M, Yamada S, Murakami S, Yamayoshi S, Iwatsuki-Horimoto K, Sakoda Y, Takashita E, McBride R, Noda T, Hatta M, Imai H, Zhao D, Kishida N, Shirakura M, de Vries RP, Shichinohe S, Okamatsu M, Tamura T, Tomita Y, Fujimoto N, Goto K, Katsura H, Kawakami E, Ishikawa I, Watanabe S, Ito M, Sakai-Tagawa Y, Sugita Y, Uraki R, Yamaji R, Eisfeld AJ, Zhong G, Fan S, Ping J, Maher EA, Hanson A, Uchida Y, Saito T, Ozawa M, Neumann G, Kida H, Odagiri T, Paulson JC, Hasegawa H, Tashiro M, Kawaoka Y. 2013. Characterization of H7N9 influenza A viruses isolated from humans. Nature 501:551–555. 10.1038/nature12392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhang Q, Shi J, Deng G, Guo J, Zeng X, He X, Kong H, Gu C, Li X, Liu J, Wang G, Chen Y, Liu L, Liang L, Li Y, Fan J, Wang J, Li W, Guan L, Li Q, Yang H, Chen P, Jiang L, Guan Y, Xin X, Jiang Y, Tian G, Wang X, Qiao C, Li C, Bu Z, Chen H. 2013. H7N9 influenza viruses are transmissible in ferrets by respiratory droplet. Science 341:410–414. 10.1126/science.1240532 [DOI] [PubMed] [Google Scholar]
- 15.Herfst S, Schrauwen EJ, Linster M, Chutinimitkul S, de Wit E, Munster VJ, Sorrell EM, Bestebroer TM, Burke DF, Smith DJ, Rimmelzwaan GF, Osterhaus AD, Fouchier RA. 2012. Airborne transmission of influenza A/H5N1 virus between ferrets. Science 336:1534–1541. 10.1126/science.1213362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Imai M, Watanabe T, Hatta M, Das SC, Ozawa M, Shinya K, Zhong G, Hanson A, Katsura H, Watanabe S, Li C, Kawakami E, Yamada S, Kiso M, Suzuki Y, Maher EA, Neumann G, Kawaoka Y. 2012. Experimental adaptation of an influenza H5 HA confers respiratory droplet transmission to a reassortant H5 HA/H1N1 virus in ferrets. Nature 486:420–428. 10.1038/nature10831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhang Y, Zhang Q, Kong H, Jiang Y, Gao Y, Deng G, Shi J, Tian G, Liu L, Liu J, Guan Y, Bu Z, Chen H. 2013. H5N1 hybrid viruses bearing 2009/H1N1 virus genes transmit in guinea pigs by respiratory droplet. Science 340:1459–1463. 10.1126/science.1229455 [DOI] [PubMed] [Google Scholar]
- 18.Hossain MJ, Hickman D, Perez DR. 2008. Evidence of expanded host range and mammalian-associated genetic changes in a duck H9N2 influenza virus following adaptation in quail and chickens. PLoS One 3:e3170. 10.1371/journal.pone.0003170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Childs RA, Palma AS, Wharton S, Matrosovich T, Liu Y, Chai W, Campanero-Rhodes MA, Zhang Y, Eickmann M, Kiso M, Hay A, Matrosovich M, Feizi T. 2009. Receptor-binding specificity of pandemic influenza A (H1N1) 2009 virus determined by carbohydrate microarray. Nat. Biotechnol. 27:797–799. 10.1038/nbt0909-797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wan H, Perez DR. 2007. Amino acid 226 in the hemagglutinin of H9N2 influenza viruses determines cell tropism and replication in human airway epithelial cells. J. Virol. 81:5181–5191. 10.1128/JVI.02827-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vines A, Wells K, Matrosovich M, Castrucci MR, Ito T, Kawaoka Y. 1998. The role of influenza A virus hemagglutinin residues 226 and 228 in receptor specificity and host range restriction. J. Virol. 72:7626–7631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Matrosovich M, Tuzikov A, Bovin N, Gambaryan A, Klimov A, Castrucci MR, Donatelli I, Kawaoka Y. 2000. Early alterations of the receptor-binding properties of H1, H2, and H3 avian influenza virus hemagglutinins after their introduction into mammals. J. Virol. 74:8502–8512. 10.1128/JVI.74.18.8502-8512.2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Connor RJ, Kawaoka Y, Webster RG, Paulson JC. 1994. Receptor specificity in human, avian, and equine H2 and H3 influenza virus isolates. Virology 205:17–23. 10.1006/viro.1994.1615 [DOI] [PubMed] [Google Scholar]
- 24.Pearce MB, Jayaraman A, Pappas C, Belser JA, Zeng H, Gustin KM, Maines TR, Sun X, Raman R, Cox NJ, Sasisekharan R, Katz JM, Tumpey TM. 2012. Pathogenesis and transmission of swine origin A(H3N2)v influenza viruses in ferrets. Proc. Natl. Acad. Sci. U. S. A. 109:3944–3949. 10.1073/pnas.1119945109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kaminski MM, Ohnemus A, Staeheli P, Rubbenstroth D. 2013. Pandemic 2009 H1N1 influenza A virus carrying a Q136K mutation in the neuraminidase gene is resistant to zanamivir but exhibits reduced fitness in the guinea pig transmission model. J. Virol. 87:1912–1915. 10.1128/JVI.02507-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shi H, Ashraf S, Gao S, Lu J, Liu X. 2010. Evaluation of transmission route and replication efficiency of H9N2 avian influenza virus. Avian Dis. 54:22–27. 10.1637/8937-052809-Reg.1 [DOI] [PubMed] [Google Scholar]
- 27.Angel M, Kimble JB, Pena L, Wan H, Perez DR. 2013. In vivo selection of H1N2 influenza virus reassortants in the ferret model. J. Virol. 87:3277–3283. 10.1128/JVI.02591-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chou YY, Albrecht RA, Pica N, Lowen AC, Richt JA, Garcia-Sastre A, Palese P, Hai R. 2011. The M segment of the 2009 new pandemic H1N1 influenza virus is critical for its high transmission efficiency in the guinea pig model. J. Virol. 85:11235–11241. 10.1128/JVI.05794-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhang P, Tang Y, Liu X, Peng D, Liu W, Liu H, Lu S. 2008. Characterization of H9N2 influenza viruses isolated from vaccinated flocks in an integrated broiler chicken operation in eastern China during a 5 year period (1998-2002). J. Gen. Virol. 89:3102–3112. 10.1099/vir.0.2008/005652-0 [DOI] [PubMed] [Google Scholar]
- 30.Hoffmann E, Neumann G, Hobom G, Webster RG, Kawaoka Y. 2000. “Ambisense” approach for the generation of influenza A virus: vRNA and mRNA synthesis from one template. Virology 267:310–317. 10.1006/viro.1999.0140 [DOI] [PubMed] [Google Scholar]
- 31.Hoffmann E, Stech J, Guan Y, Webster RG, Perez DR. 2001. Universal primer set for the full-length amplification of all influenza A viruses. Arch. Virol. 146:2275–2289. 10.1007/s007050170002 [DOI] [PubMed] [Google Scholar]
- 32.Hoffmann E, Neumann G, Kawaoka Y, Hobom G, Webster RG. 2000. A DNA transfection system for generation of influenza A virus from eight plasmids. Proc. Natl. Acad. Sci. U. S. A. 97:6108–6113. 10.1073/pnas.100133697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sun Y, Qin K, Wang J, Pu J, Tang Q, Hu Y, Bi Y, Zhao X, Yang H, Shu Y, Liu J. 2011. High genetic compatibility and increased pathogenicity of reassortants derived from avian H9N2 and pandemic H1N1/2009 influenza viruses. Proc. Natl. Acad. Sci. U. S. A. 108:4164–4169. 10.1073/pnas.1019109108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Reed LJ, Muench H. 1938. A simple method of estimating fifty percent endpoints. Am. J. Hyg. 27:493–497 [Google Scholar]
- 35.Ohuchi M, Ohuchi R. 1997. Active site for fusion activity of influenza virus hemagglutinin. Nihon Rinsho 55:2648–2653 [PubMed] [Google Scholar]
- 36.Park KJ, Kwon HI, Song MS, Pascua PN, Baek YH, Lee JH, Jang HL, Lim JY, Mo IP, Moon HJ, Kim CJ, Choi YK. 2011. Rapid evolution of low-pathogenic H9N2 avian influenza viruses following poultry vaccination programmes. J. Gen. Virol. 92:36–50. 10.1099/vir.0.024992-0 [DOI] [PubMed] [Google Scholar]
- 37.Imai M, Herfst S, Sorrell EM, Schrauwen EJ, Linster M, De Graaf M, Fouchier RA, Kawaoka Y. 2013. Transmission of influenza A/H5N1 viruses in mammals. Virus Res. 178:15–20. 10.1016/j.virusres.2013.07.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tellier R. 2009. Aerosol transmission of influenza A virus: a review of new studies. J. R. Soc. Interface 6(Suppl 6):S783–S790. 10.1098/rsif.2009.0302.focus [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yang W, Marr LC. 2011. Dynamics of airborne influenza A viruses indoors and dependence on humidity. PLoS One 6:e21481. 10.1371/journal.pone.0021481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kageyama T, Fujisaki S, Takashita E, Xu H, Yamada S, Uchida Y, Neumann G, Saito T, Kawaoka Y, Tashiro M. 2013. Genetic analysis of novel avian A(H7N9) influenza viruses isolated from patients in China, February to April 2013. Euro Surveill. 18:20453 http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=20453 [PMC free article] [PubMed] [Google Scholar]
- 41.DuBois RM, Zaraket H, Reddivari M, Heath RJ, White SW, Russell CJ. 2011. Acid stability of the hemagglutinin protein regulates H5N1 influenza virus pathogenicity. PLoS Pathog. 7:e1002398. 10.1371/journal.ppat.1002398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Floyd DL, Ragains JR, Skehel JJ, Harrison SC, van Oijen AM. 2008. Single-particle kinetics of influenza virus membrane fusion. Proc. Natl. Acad. Sci. U. S. A. 105:15382–15387. 10.1073/pnas.0807771105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bullough PA, Hughson FM, Skehel JJ, Wiley DC. 1994. Structure of influenza haemagglutinin at the pH of membrane fusion. Nature 371:37–43. 10.1038/371037a0 [DOI] [PubMed] [Google Scholar]
- 44.Daniels RS, Downie JC, Hay AJ, Knossow M, Skehel JJ, Wang ML, Wiley DC. 1985. Fusion mutants of the influenza virus hemagglutinin glycoprotein. Cell 40:431–439. 10.1016/0092-8674(85)90157-6 [DOI] [PubMed] [Google Scholar]
- 45.Thoennes S, Li ZN, Lee BJ, Langley WA, Skehel JJ, Russell RJ, Steinhauer DA. 2008. Analysis of residues near the fusion peptide in the influenza hemagglutinin structure for roles in triggering membrane fusion. Virology 370:403–414. 10.1016/j.virol.2007.08.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Steinhauer DA, Martin J, Lin YP, Wharton SA, Oldstone MB, Skehel JJ, Wiley DC. 1996. Studies using double mutants of the conformational transitions in influenza hemagglutinin required for its membrane fusion activity. Proc. Natl. Acad. Sci. U. S. A. 93:12873–12878. 10.1073/pnas.93.23.12873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cotter CR, Jin H, Chen Z. 2014. A single amino acid in the stalk region of the H1N1pdm influenza virus HA protein affects viral fusion, stability and infectivity. PLoS Pathog. 10:e1003831. 10.1371/journal.ppat.1003831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zaraket H, Bridges OA, Duan S, Baranovich T, Yoon SW, Reed ML, Salomon R, Webby RJ, Webster RG, Russell CJ. 2013. Increased acid stability of the hemagglutinin protein enhances H5N1 influenza virus growth in the upper respiratory tract but is insufficient for transmission in ferrets. J. Virol. 87:9911–9922. 10.1128/JVI.01175-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hulse DJ, Webster RG, Russell RJ, Perez DR. 2004. Molecular determinants within the surface proteins involved in the pathogenicity of H5N1 influenza viruses in chickens. J. Virol. 78:9954–9964. 10.1128/JVI.78.18.9954-9964.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hu J, Hu Z, Song Q, Gu M, Liu X, Wang X, Hu S, Chen C, Liu H, Liu W, Chen S, Peng D. 2012. The PA-gene-mediated lethal dissemination and excessive innate immune response contribute to the high virulence of H5N1 avian influenza virus in mice. J. Virol. 87:2660–2672. 10.1128/JVI.02891-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Liu Y, Lou Z, Bartlam M, Rao Z. 2009. Structure-function studies of the influenza virus RNA polymerase PA subunit. Sci. China C Life Sci. 52:450–458. 10.1007/s11427-009-0060-1 [DOI] [PubMed] [Google Scholar]
- 52.Hara K, Nakazono Y, Kashiwagi T, Hamada N, Watanabe H. 2013. Co-incorporation of the PB2 and PA polymerase subunits from human H3N2 influenza virus is a critical determinant of the replication of reassortant ribonucleoprotein complexes. J. Gen. Virol. 94:2406–2416. 10.1099/vir.0.053959-0 [DOI] [PubMed] [Google Scholar]
- 53.Yamayoshi S, Yamada S, Fukuyama S, Murakami S, Zhao D, Uraki R, Watanabe T, Tomita Y, Macken C, Neumann G, Kawaoka Y. 2013. Virulence-affecting amino acid changes in the PA protein of H7N9 influenza A viruses. J. Virol. 88:3127–3134. 10.1128/JVI.03155-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ping J, Keleta L, Forbes NE, Dankar S, Stecho W, Tyler S, Zhou Y, Babiuk L, Weingartl H, Halpin RA, Boyne A, Bera J, Hostetler J, Fedorova NB, Proudfoot K, Katzel DA, Stockwell TB, Ghedin E, Spiro DJ, Brown EG. 2011. Genomic and protein structural maps of adaptive evolution of human influenza A virus to increased virulence in the mouse. PLoS One 6:e21740. 10.1371/journal.pone.0021740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zurcher T, de la Luna S, Sanz-Ezquerro JJ, Nieto A, Ortin J. 1996. Mutational analysis of the influenza virus A/Victoria/3/75 PA protein: studies of interaction with PB1 protein and identification of a dominant negative mutant. J. Gen. Virol. 77(Part 8):1745–1749. 10.1099/0022-1317-77-8-1745 [DOI] [PubMed] [Google Scholar]
- 56.Wan H, Sorrell EM, Song H, Hossain MJ, Ramirez-Nieto G, Monne I, Stevens J, Cattoli G, Capua I, Chen LM, Donis RO, Busch J, Paulson JC, Brockwell C, Webby R, Blanco J, Al-Natour MQ, Perez DR. 2008. Replication and transmission of H9N2 influenza viruses in ferrets: evaluation of pandemic potential. PLoS One 3:e2923. 10.1371/journal.pone.0002923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Tumpey TM, Maines TR, Van Hoeven N, Glaser L, Solorzano A, Pappas C, Cox NJ, Swayne DE, Palese P, Katz JM, Garcia-Sastre A. 2007. A two-amino acid change in the hemagglutinin of the 1918 influenza virus abolishes transmission. Science 315:655–659. 10.1126/science.1136212 [DOI] [PubMed] [Google Scholar]
- 58.Sun Y, Pu J, Jiang Z, Guan T, Xia Y, Xu Q, Liu L, Ma B, Tian F, Brown EG, Liu J. 2010. Genotypic evolution and antigenic drift of H9N2 influenza viruses in China from 1994 to 2008. Vet. Microbiol. 146:215–225. 10.1016/j.vetmic.2010.05.010 [DOI] [PubMed] [Google Scholar]
- 59.Zhang Y, Yin Y, Bi Y, Wang S, Xu S, Wang J, Zhou S, Sun T, Yoon KJ. 2012. Molecular and antigenic characterization of H9N2 avian influenza virus isolates from chicken flocks between 1998 and 2007 in China. Vet. Microbiol. 156:285–293. 10.1016/j.vetmic.2011.11.014 [DOI] [PubMed] [Google Scholar]
- 60.Bi J, Deng G, Dong J, Kong F, Li X, Xu Q, Zhang M, Zhao L, Qiao J. 2010. Phylogenetic and molecular characterization of H9N2 influenza isolates from chickens in Northern China from 2007–2009. PLoS One 5:e13063. 10.1371/journal.pone.0013063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Xu KM, Smith GJ, Bahl J, Duan L, Tai H, Vijaykrishna D, Wang J, Zhang JX, Li KS, Fan XH, Webster RG, Chen H, Peiris JS, Guan Y. 2007. The genesis and evolution of H9N2 influenza viruses in poultry from southern China, 2000 to 2005. J. Virol. 81:10389–10401. 10.1128/JVI.00979-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wu A, Su C, Wang D, Peng Y, Liu M, Hua S, Li T, Gao GF, Tang H, Chen J, Liu X, Shu Y, Peng D, Jiang T. 2013. Sequential reassortments underlie diverse influenza H7N9 genotypes in China. Cell Host Microbe 14:446–452. 10.1016/j.chom.2013.09.001 [DOI] [PubMed] [Google Scholar]