Abstract
Purpose :
The Direct Anterior Approach (DAA) is well established as a minimal access approach in elective orthopaedic hip surgery. For the growing number of elderly patients with femoral neck fractures treated with Bipolar Hip Hemiarthroplasty (BHH), only a few results do exist. The study shows the clinical and radiological outcome for 180 patients treated by a modified DAA with BHH.
Materials and Methods :
The data of 180 geriatric patients with medial femoral neck fractures were evaluated retrospectively. The general and surgical complications, mobilisation using the Timed Up and Go test (TUG), the social environment pre- and postoperative and the radiological results have been compared with established approaches for geriatric hip surgery.
Results :
After joint replacement, 18 (10%) patients were developed pneumonia, of which 3 (1.7%) died during hospitalisation. In 7 cases (4%), surgical revision had to be carried out: three times (1.7%) because of a seroma, three times (1.7%) because of subcutaneous infection, and one time (0.6%) because the BHH was removed, owing to deep wound infection. One dislocation (0.6%) occurred, as well as one femoral nerve lesion (0.6%) occured. 88.3% of patients were mobilised on walkers or crutches; the Timed Up and Go Test showed a significant improvement during inpatient rehabilitation. 83% were discharged to their usual social environment, 10% were transferred to a short-term care facility and 7% were relocated permanently to a nursing home. 3/4 of patients had a cemented stem alignment in the range between -5° and 5°, while 2/3 of patients had a maximum difference of 1 cm in leg length.
Conclusion :
Using the modified DAA, a high patient satisfaction is achieved after implantation of a BHH. The rate of major complications is just as low as in conventional approaches, and rapid mobilisation is possible.
Keywords: Bipolar hip hemiarthroplasty, femoral neck fracture, geriatrics, minimal invasive surgery.
INTRODUCTION
The number of medial femoral neck fractures has risen in recent decades. Because of the demographic development, this upward trend will continue. In Germany, there will be an increase of more than 70% in the incidence of femoral fractures up until 2020 [1]. In the United States, the estimated number of displaced femoral neck fractures treated annually is currently 250000; this number is expected to reach 500000 by 2040 [2]. Currently, the age of the geriatric population is rising and consequently, so is the rate of comorbidity. A contemporary soft tissue preserving surgical therapy is recommended to achieve a fast mobilisation and to avoid complications associated with immobilisation [3, 4].
The treatment of the geriatric population with cemented bipolar hip hemiarthroplasty (BHH) is a widely accepted method [5-7]. The procedure is standardised and patientsachieve full weight bearing immediately after operation. In recent years, minimal invasive surgery for total hip replacement has become common. Due to minimal invasive procedures, the mobilisation might be faster and the hospital stay shorter [8, 9]. The patients show a lesser blood loss and reduced pain levels [10-15]. These advantages of minimal invasive surgery are essential for geriatric patients, and possibly reduce postoperative mortality. For a minimal invasive approach to the hip, a cadaveric study could show a lower risk of trauma to the abductor and small external rotator muscle for the anterior, in comparison to the posterior approach [16].
The direct anterior approach (DAA) to the hip was first described by Rachbauer [17]. As positive results for total hip arthroplasty (THA) are already published, there is a lack of evidence for the implantation of BHH in elderly patients with osteoporosis after femoral neck fracture [18]. These patients might benefit immensely from a less invasive surgical procedure, with possibly a faster mobilisation and less tissue trauma and blood loss.
The aim of the study was to elaborate clinical and radiological results of 180 geriatric patients with medial femoral neck fractures, treated by BHH with the modified DAA.
MATERIALS AND METHODS
This study represents a retrospective observational study conducted in a level-1 trauma centre (University Hospital Schleswig-Holstein, Campus Luebeck, Department for Trau-matology) during April 2008 and June 2011. 180 consecutive patients were treated for a dislocated medial femoral neck fracture with a cemented BHH. Criterion for exclusion was a pathological or open fracture, or treatment using another method. The approach to the hip was for all patients the modified DAA. The Garden classification was used to classify define the fractures. The observation time period was the length of stay in the trauma hospital and the treatment period at the geriatric rehabilitation hospital.
Description of Modified DAA
The DAA for total hip arthroplasty in patients with symptomatic osteoarthritis is well described by Rachbauer [17]. In our department, the DAA for BHH has been used since 2004. A single-shot antibiosis (Cefuroxim 1.5 g) was given twenty minutes before skin incision. Using the DAA, we found several risk factors for the geriatric population. Therefore, a list of modifications dependent on the soft tissue and bone attributes of geriatric patients was developed in order to reduce these risk factors [19]. A systematic overview of the differences between original DAA and modified DAA are shown in Table 1. All described modifications will help the surgeon to replace a BHH gently, and increase the success rate for BHH in geriatric patients with sensitive soft tissue and poor osteoporotic bone quality.
Table 1.
Overview of the differences between the original DAA and its modification during implantation of the BHH geriatric patients [19].
| Direct Anterior Approach | Modified Direct Anterior Approach | Advantage | |
|---|---|---|---|
| Draping | Both legs are draped flexibly | Only operating leg is draped flexibly | Better hygiene |
| Skin incision | Starts two finger breadths lateral and distal to the ASIS | Starts two finger breadths lateral to the ASIS | Better angle for femoral broaching |
| Retractor position | On ventral rim of acetabulum | Right into femoral head | No risk of breaking in the acetabulum |
| Corkscrew | Inserting in spongiosa bone | Inserting in cortical bone of the head | Easier removal of femoral head |
| Positioning retractor during femoral exposure | Cranial under greater trochanter | Lateral under greater trochanter | Lower risk of fracture of greater trochanter |
| Type of retractor | Sharp and blunt retractors can be used | Only blunt retractors should be used | Lower risk of breaking osteoporotic bone |
| Reduction of head in acetabulum | - | Place head first, attach conus on the stem and reduce afterwards | Lower risk of damage at ventral rim of the acetabulum |
After incision of skin and subcutaneous layer, the fascia of the tensor was incised (Table 1: skin incision). This approach uses an inter-muscular and inter-nerval plane between the gluteus medius, rectus femoris, and tensor fasciae latae muscle. After positioning the retractors around the femoral neck, a T-shaped incision and capsulectomy was performed (Table 1: retractor position). Osteotomy was performed at 45°, ending one finger above the end of the minor trochanter. With a chisel, the dissected neck was mobilised, and a corkscrew removed the head (Table 1: corkscrew). To expose the femur, the opposite leg was hyperabducted first. Next, the femoral elevator was placed 2-4 cm distal to the apex of the greater trochanter in front of the gluteus medius muscle. While placing it from the side and keeping the retractor under gentle power, a fracture to the greater trochanter could be avoided (Table 1: positioning retractor). A gradual but firm anterior pull elevated the femur, simultaneously the assistant adducted and externally rotated the operated leg with the knee straight. Sometimes an additional release of the posterior structures was required to achieve proper femoral exposure. Because of an accumulation of prolonged wound healing in the proximal wound area, a Roux retractor was placed at the site of the cranial wound in order to avoid damage of skin and soft tissue during broaching. To open the femoral canal, an angulated curette was used. Sometimes a rangeur was helpful to extend the opening. Broaching of the femoral canal with special instruments was performed afterwards.
The Minimal Invasive Instruments (MIS) used were from Stryker Orthopaedics (Stryker, Duisburg, Germany). The stem was in all cases a cemented ABG®II, also from Stryker Orthopaedics (Stryker, Duisburg, Germany), cemented with 40 g PMMA-bone cement with Gentamicin (Palacos-RG, Heraeus Medical GmbH, Wehrheim, Germany). The Bipolar Head used was a Stryker UHR® (Universal Head Bipolar System) head.
Postoperative routine during observation was as follows:
- Removal of drainage after 48 hours
- Short mobilisation on operating day, transfer from bed to chair and bathroom on first postoperative day supported, mobilisation with either two crutches or a walker, with full weight bearing on second postoperative day
- DVT prophylaxis with low molecular heparin for 5 weeks.
Demographic Data
For analysis, the age, sex, date of accident and time period until operative treatment were registered. The comorbidity was documented and the American Society of Anesthesiologists (ASA) Score was assigned.
Parameter
During observation, general and surgical complications were noted, including revision surgery for any reason. Also, the 30-day mortality, operating time and number of given red blood cell concentration were evaluated.
The Timed Up and Go test (TUG) is a simple test to assess the mobility and flexibility of the body balance and the consequent risk of fall in particular geriatric patients. The patient sits on a chair with armrests and wears regular footwear. Upon request, the patient gets up without help, walks a distance of 3 m, turns around and sits down again. Medical aids such as crutches are allowed to be used. The TUG, measured in seconds, was collected at the beginning of rehabilitation and at discharge.
Radiology
To evaluate the position of the implanted BHH, a radiograph of the pelvis – in a.p. direction with 10° external rotation in both hips – and a Lauenstein picture were taken on the second postoperative day. With the IMPAX AGFA Health Care software (http://www.agfahealthcare.com), the alignment of the stem was measured as well as the indirect difference of leg length, based on the method of Ranawat et al. [20].
RESULTS
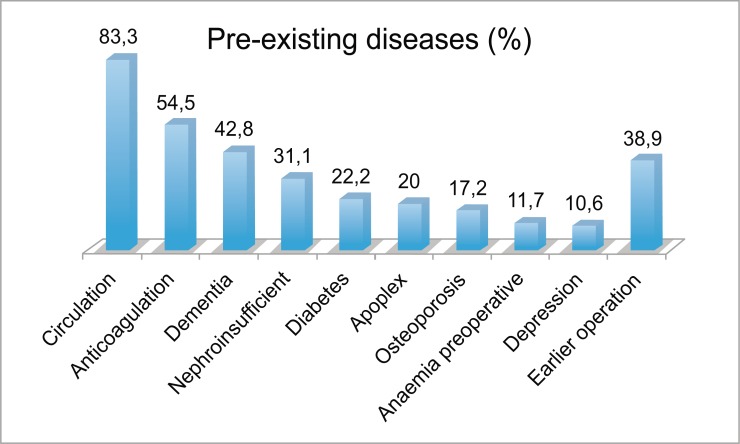
A total of 180 patients were treated for dislocated medial femoral neck fracture. 141 (78.3%) were female and 39 (21.7%) male. The median age was 84.5 ± 7.2 years. 78% were 80 or more years old. ASA classification was in 97% between stages II and III. The comorbidities in Fig. (1) show the typical distribution for the geriatric population (Fig. 1).
Fig. (1).
Typical distribution of the co-morbidity in geriatric patients with a femoral neck fracture.
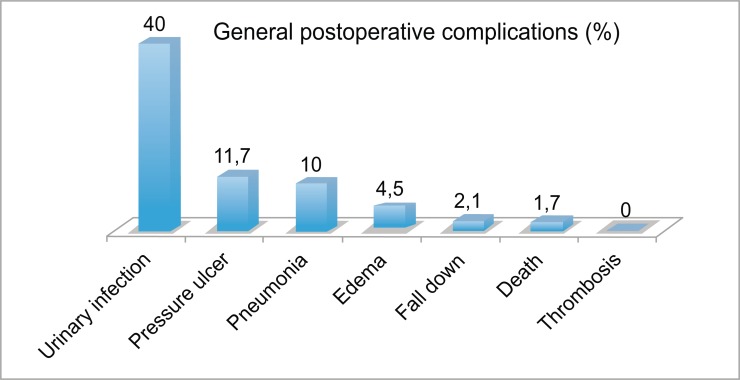
The median stay in hospital was 16 days (4-41 days). 66.2% (119) of patients were treated in the first 48 hours after a fracture was diagnosed. Reasons for delayed operative treatment included current anticoagulation in 16% and bad general state of health in 14% of all patients. The median surgical cut to stitch time was 73 min (39-119 min). In 61% of patients, the operator was an assistant physician, in 49% a senior physician. Nearly 2/3 of patients developed a common postoperative complication (Fig. 2). Infection of the urinary tract had to be treated in 40% of patients. However, it is to be assumed that some patients’ infections were present prior to surgery. In 21 patients (11.7%), a pressure ulcer occurred postoperatively: 17 times in the sacral region (11x stage 1, 6x stage II) and 4 times in the heel (3x stage I, 1x stage II). The postoperative two week mortality was 1.7%. An 89-year-old female had a heart attack with circulation collapse on the fourth day after surgery, while an 85-year-old female had circulation collapse with flat line during cementation of the stem. A 93-year-old woman died because of fulminant pneumonia. Resuscitation was not successful.
Fig. (2).
Urinary tract infection was the most frequent general complication. Pressure ulcers were caused in the sacral region and on the heel, in over 80% of stage 1. Pneumonia was treated successfully in all cases with antibiotic therapy.
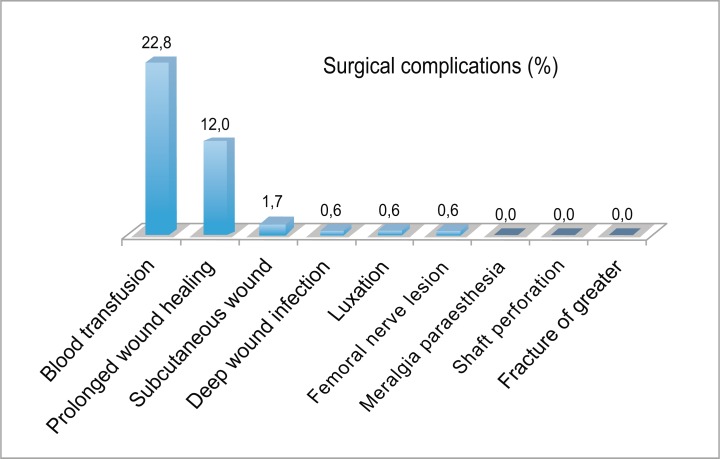
Because of anaemia, 41 patients (22.8%) needed a blood transfusion (Fig. 3). Anaemia was defined as haemoglobin value below 80 mg/L. In 21 patients (12%), a prolonged wound healing was found, which was treated conservatively in all cases, with daily re-dressing of the wound. In three cases (1.7%), an operative revision had to be done because of a seroma, and in three cases (1.7%) because of a subcutaneous infection. In two cases, the pathogen was multisensible Staphylococcus aureus, and in one, a multisensible Proteus mirabilis. In one case (0.6%), a patient developed a deep wound infection with explantation, and revised total hip arthroplasty after a 6-week antibiotic therapy course. The isolated pathogen was a multisensible Enterococcus faecalis. Other major complications were one (0.6%) luxation of the bipolar head because of dysplasia, and one nervus femoralis lesion because of incorrect position of a sharp retractor. No perforation of the shaft, meralgia paraesthetica or fracture of the greater trochanter was seen.
Fig. (3).
12% of patients developed a prolonged wound healing. Severe complication with revision of the wound took place in 4% of cases. One patient had to be revised because of a luxation of the head on the basis of a dysplasia. The BHH was replaced in a total hip arthroplasty over an mDAA. The lesion of the femoral nerve recovered in about 6 months, but the patient remained dependent on a wheelchair for mobility. A DAA typical complication (Meralgia paraesthesia, perforation of the shaft, fracture of the greater trochanter) did not occur in any of the 180 patients.
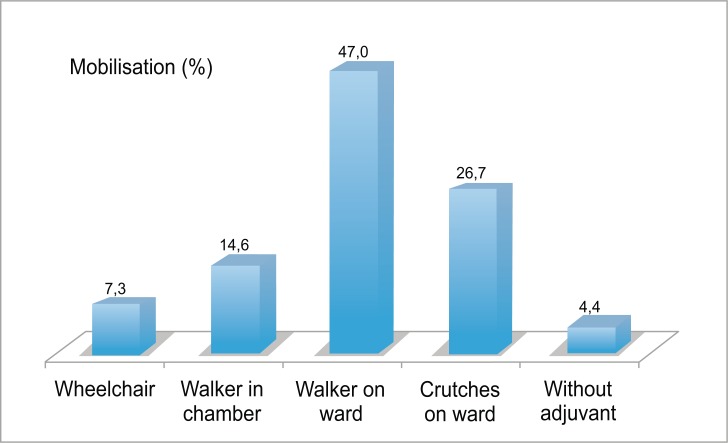
The postoperative mobilisation is shown in Fig. (4). 13 patients (7.3%) were transferred to a wheelchair, while 8 were already wheelchair dependent preoperatively. 111 patients (61.6%) were mobilised with a walker and 48 (26.7%) with crutches. 8 patients (4.4%) were able to move without any sort of medical aids.
Fig. (4).
Graphical representation of the mobilisation of patients, including medical aid before transfer into rehabilitation unit.
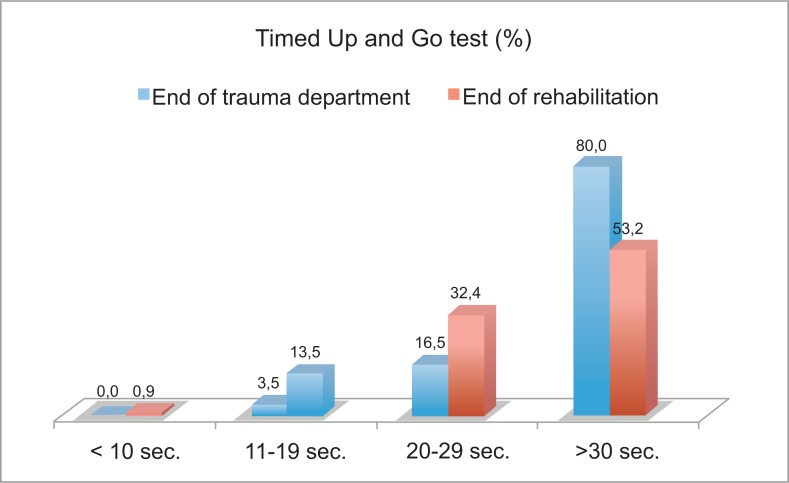
At the end of acute inpatient treatment, the TUG test showed a mean duration of 178.9 ± 134.2 seconds (TUG1), which was reduced at the end of rehabilitation to 119.2 ± 129.6 seconds (TUG2) on average (n = 113). The difference was therefore 59.8 ± 107.1 seconds (p < 0,01) (Fig. 5).
Fig. (5).
During the geriatric rehabilitation, there was a significant improvement in the TUG. 30 patients (26.8%) could be grouped better at the end of the rehabilitation (n = 113).
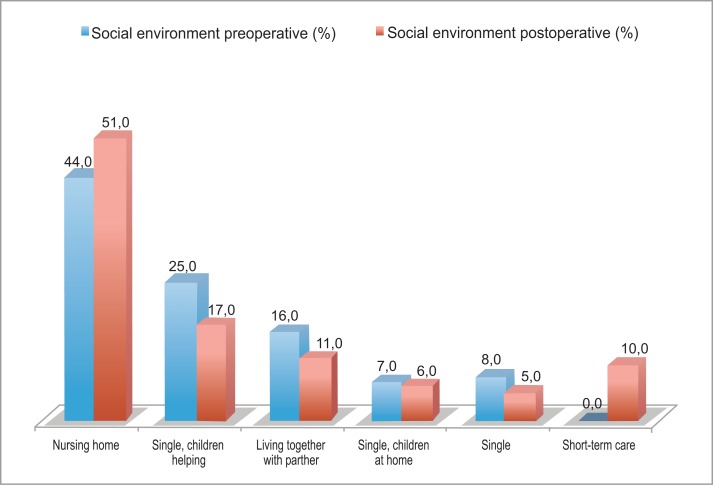
Fig. (6) demonstrates a comparison of the social environment before the fracture (n = 180) and after rehabilitation (n = 167). It shows an increase of 7% in the social environment in nursing homes, and of 10% in the short-term care facilities. Consequently, a decrease in self-social environment is visible. This trend was particularly evident in patients who lived alone before the operation (-8%) or who had the support of their children in everyday life (-3%), as well as in patients who lived with their partners (-5%).
Fig. (6).
Comparison of the social environment preoperative and at the end of rehabilitation.
A correct alignment of the stem (range between -5° to +5°) was seen in 137 patients (76%). 34 patients (19%) had more than 5° valgus direction, while 7 patients (4%) had more than 5° varus direction. Nearly 2/3 of patients had a radiological difference between -0.5 and 0.5 cm in the length of the leg. Because of a previous hip joint close fracture on the opposite leg, only 122 patients were included.
DISCUSSION
Meta-analysis of randomised prospective studies showed a better outcome in patients aged over 65 years with femoral head fractures (Garden III-IV) treated with HEP [7, 21]. Minimal invasive surgical techniques in hip surgery are increasingly being accepted. The new technique aims to reduce perioperative complications and facilitate a faster rehabilitation process. Anterior, antero-lateral and posterior approaches to the hip have been described, as well as the two incision approaches [13, 22-24]. Clinical trials in patients who underwent total hip arthroplasty showed a smaller tissue trauma associated with a reduced morbidity and lower blood loss [25-27]. Using magnetic resonance imaging (MRI) in 25 patients, Ludemann detected no increased damage of the M. gluteus medius postoperative while using the DAA [28]. While many studies regarding minimal invasive approaches for THA in middle-aged patient groups do exist, the growing numbers of the geriatric population are not generally considered in international literature.
We have used the DAA for the hip joint in our trauma department since 2004. Based on several pitfalls, we modified the approach in geriatric patients for the implantation of BHH after femoral neck fracture [19].
In this study, there was a typical distribution with respect to age, sex and co-morbidity in patients with femoral neck fracture. The implantation of a BHH is a training intervention, which was done by an assistant physician in 61% of patients. The medium operating time was 73 minutes, which is similar to other studies treating a femoral neck fracture with cemented BHH, regardless of the surgical approach to the hip joint [29-32]. The number of general postoperative complications also showed the typical pattern of geriatric patients. In 40% of patients, a urinary tract infection was present and treated. Preoperatively, no routine diagnostic was done, so no definite statement can be made to postoperatively-occurring urinary tract infections. Due to our modification of the DAA with respect to the way of draping the legs, we intended to reduce the rate of urinary tract infection. All things considered, though, the different draping had no positive influence on the rate of urinary tract infection. Also, urinary tract infections do not seem to be influenced by the surgical approach to the hip joint [33]. The rate of postoperative pressure ulcers was 11.7%. However, geriatric patients with a medial femoral neck fracture do have a high risk of pressure ulcers. Predisposing factors are hospitalisation for more than 7 days, or transfer from a nursing home [34]. All postoperative pressure ulcers had an early stage (14x stage I, 7x stage II). Interestingly, 83% of the pressure ulcers were present when the patient was operated on later than 48 hours after the accident. This once again underlines the necessity for early operation after trauma. 13 patients (7.3%) were postoperatively mobilised in the wheelchair, and 8 developed a sacral pressure ulcer. As additional risks, almost half of the patients who developed a pressure ulcer had diabetes mellitus, and nearly 1/3 had a body mass index below 20.
The mortality rate during the acute hospital stay was 1.7%, which was low. Schneider et al. reported a 7% mortality rate during hospitalisation for DAA [30]. Yli-Kyyny et al. had a rate of 4.1% in 122 patients with cemented BHH. Fat embolism was the major cause of death during cementing [35]. Even though we used modern cementing techniques, including cement stopper, retrograde application, pressurisation and cement curing consequently over 14 minutes but this also resulted in collective death.
Nearly 25% of patients received postoperative blood transfusions. If the preoperative haemoglobin level was > 100 mg/dL (6 patients), transfusion was administered in only 14.6% of patients. If the haemoglobin level was < 100 mg/dL (35 patients), the number rose to 85.4%. Wick et al. reported in their study that 36% of patients received a blood transfusion after implantation of a cementless BHH [4]. However, it should be noted that several different inter-hospital guidelines for transfusion exist, so a comparison may be difficult.
The overall risk for a major complication in our study was 5.2%. This was almost same when compared to other studies that used different minimally invasive approaches or conventional approaches to the hip joint [29, 36]. In one case (0.6%), a dislocation of the prosthesis occurred. Poignard et al. reported dislocations in about 4.5% of patients after using a posterolateral approach, while Biber et al. reported dislocations in about 3.9% of patients after a posterior approach, and 0.5% after a transgluteal approach [37, 38]. In a meta-analysis of Burgers et al. eight trials with a total of 986 patients were retrieved. The overall dislocation rate was 3%, using lateral, anterolateral, posterolateral or posterior approaches [39]. A total of 7 patients (4%) had to be revised because of a wound infection, and 21 (12%) had a prolonged wound healing. The starting point of impaired wound healing was in all cases the proximal pole of the wound. In this area, the skin is set up under tension because of the proximity to the anterior superior iliac spine while broaching the shaft. The ambition of minimally invasive incisions runs up against limits. The sensitive skin and soft tissue of geriatric patients require a very gentle operative technique; accordingly, we extended the skin incision by 2 cm proximally and used a Roux retractor additionally at the cranial wound area, in order to avoid damage of skin and soft tissue. No prolonged wound healing or wound healing disorder did appear in the last 37 patients of the series. An infection-induced explantation of the BHH was necessary in one case (0.6%). This was low compared to other approaches. Biber et al. described an infection rate of 2.5% after a posterior approach and 3.2% after a transgluteal approach [38]. Rachbauer described meralgia paresthica, shaft perforation and a fracture of the greater trochanter as typical risks for the DAA during THA [17]. In our geriatric collection, none of these complications have occurred. We suspect that this was related to the modifications that we implemented using the DAA [19].
Concerning the mobilisation of patients, so far no suitable specific test exists for the assessment of geriatric patients after implantation of an endoprosthesis. Established tests like the Harris Hip Score as well as the WOMAC are designed mainly for patients who have undergone elective THA. In our results, four weeks postoperative, 159 patients (88.3%) were mobilised either with a walker (61.6%) or with crutches (26.7%). Only 5 patients (3%) who were ambulatory before surgery were confined postoperatively to a wheelchair. Schneider et al. achieved better results for their 3-month follow-up after implantation of BHH with DAA [30]. Only 47 (59%) of 80 patients were dependent on walking aids; the most frequent support was the walker (36%). Concerning the Timed Up and Go test, our results showed a marked improvement in mobilisation after a two-week stay in a geriatric rehabilitation unit, which was statistically significant. The TUG was performed one minute faster on average. Laflamme et al. showed in their study that TUG is an early clinical indicator of future physical function in geriatric patients with femoral neck fracture treated with hemiarthroplasty [40]. At three weeks after the operation, patients who needed longer than 26 seconds to perform the test had a significantly higher probability of using a walker for 2 years after the operation. 77 of our patients (42.7%) required less than 27 seconds to perform the test, so there should be a high probability in this group of being mobile after 2 years, without the need for walking aids. However, it must be taken into account that the mortality rate after 1 year is about 30%, and even more patients are affected by internal or neurological comorbidities. Preoperatively, 101 patients (56.1%) lived in their own homes, but postoperatively the number decreased to 82 (49.1%). 16 patients (10%) were temporarily placed in a short-term care facility. This coincides with the results of Schneppendahl et al. [41]. In his long-term follow-up of patients who underwent BHH because of femoral neck fracture, about 2/3 of patients returned to their original type of accommodation, and the majority reached their original degree of mobility.
A frequently mentioned disadvantage of minimally invasive approaches in arthroplasty is the restricted intraoperative visibility, resulting in difficulty of ensuring the correct positioning of the components [2]. Our postoperative radiological examination showed good results in 76% of patients, in terms of implant position with respect to stem alignment. In 34 patients (19%), the stem was implanted more than 5° valgus. This is due to the difficult entrance level in DAA, despite the use of specially angled broaches. In particular, in patients with obese soft tissue and present osteoporosis, elevation of the greater trochanter for optimal femoral exposure had to be done with powerful levers. This resulted in a significantly increased risk of iatrogenic fracture of the great trochanter. By placing the retractor from the side instead of below the greater trochanter and keeping it under gentle power, a fracture to the greater trochanter was avoided in all 180 patients. The implantation of the stem in a correct alignment still remains difficult when using the mDAA. In our opinion, an increased valgus of more than 5° was acceptable for the geriatric patient population with limited mobility claim; a possible fracture of the great trochanter would worsen the outcome significantly. A correct restoration of the leg length was seen in 2/3 of patients. Schneider et al. and Preininger et al. reported excellent radiological results with respect to stem alignment, restoration of leg length and femoral offset after implantation of a BHH by DAA [30, 42]. Schneider et al. showed that a subsidence of the stem occurred in only 3 cases (3.7%) in a 2.5 year follow-up. No loosening of the stem occurred. Rachbauer and Alecci et al. confirmed in their results a good to very good alignment of the stem after THA when using the DAA [17, 43].
The attending trauma surgeon is often confronted with multi-morbid patients, who have suffered a femoral neck fracture because of a fall. Kinzl et al. provide high demands on the respective treatment concepts [44]. These are: rapid treatment, early mobilisation, full weight bearing, wide applicability, low complication rate and low mortality. All these requirements were satisfied in the present study by implanting a BHH with mDAA. Therefore, in our hospital, mDAA has become the standard approach.
CONCLUSION
Using the mDAA, good results are achieved after operative treatment of femoral neck fractures in geriatric patients. Compared to the established approaches, the postoperative complications are about the same, some less. A minimally invasive incision should not be enforced because of the sensitive skin and soft tissue in geriatric patients. Operation technique must be gentle, otherwise the risk of impaired wound healing is increased. Early postoperative mobilisation is possible for a high percentage of patients, and the majority of patients are discharged after a 4-week hospitalisation in their home environment. The prosthetic stem is implanted correctly, but still keeps difficult part of the operation.
ACKNOWLEDGEMENTS
Declared none.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
REFERENCES
- 1.Frerichmann U, Raschke MJ, Stockle U, Wohrmann S, Lohmann R. Proximal femoral fractures in the elderly. Data from health insurance providers on more than 23 million insured persons. Part 2. Unfallchirurg. 2007;110(7): 610–6. doi: 10.1007/s00113-007-1258-y. [DOI] [PubMed] [Google Scholar]
- 2.Bhandari M, Devereaux PJ, Tornetta P 3rd , et al. Operative management of displaced femoral neck fractures in elderly patients.An international survey. . J Bone Joint Surg Am. 2005;87(9): 2122–30. doi: 10.2106/JBJS.E.00535. [DOI] [PubMed] [Google Scholar]
- 3.Muller CA, Bayer J, Szarzynski E, Sudkamp NP. Implantation of bipolar prosthesis for treatment of medial femoral neck fractures in the elderly. Clinical and radiographic outcome. Zentralbl Chir. 2008;133(6): 590–6. doi: 10.1055/s-0028-1098711. [DOI] [PubMed] [Google Scholar]
- 4.Wick M, Muhr G, Rincon R, Lester D. Surgical treatment of a displaced femoral head fracture with a cement-free dual-headed prosthesis using a minimally invasive approach. Clinical and radiographic outcome. Unfallchirurg. 2005;108(3): 215–21. doi: 10.1007/s00113-004-0868-x. [DOI] [PubMed] [Google Scholar]
- 5.Blomfeldt R, Tornkvist H, Ponzer S, Soderqvist A, Tidermark J. Comparison of internal fixation with total hip replacement for displaced femoral neck fractures.Randoized controlled trial performed at four years. J Bone Joint Surg Am. 2005; 87(8): 1680–8. doi: 10.2106/JBJS.D.02655. [DOI] [PubMed] [Google Scholar]
- 6.Heetveld MJ, Rogmark C, Frihagen F, Keating J. Internal fixation versus arthroplasty for displaced femoral neck fractures.What is the evidence?. J Orthop Trauma. 2009;23(6): 395–402. doi: 10.1097/BOT.0b013e318176147d. [DOI] [PubMed] [Google Scholar]
- 7.Rogmark C, Johnell O. Primary arthroplasty is better than internal fixation of displaced femoral neck fractures.A meta-analysis of 14 randomized studies wth 289 patients. . Acta Orthop. 2006; 77(3): 359–67. doi: 10.1080/17453670610046262. [DOI] [PubMed] [Google Scholar]
- 8.Murphy SB, Tannast M. Conventional vs minimally invasive total hip arthroplasty.A prospective study of rehabilitation and complications. Orthopade. 2006;35(7): 761–4, 6-8. doi: 10.1007/s00132-006-0969-z. [DOI] [PubMed] [Google Scholar]
- 9.DiGioia AM 3rd, Plakseychuk AY, Levison TJ, Jaramaz B. Mini-incision technique for total hip arthroplasty with navigation. J Arthroplasty. 2003;18(2): 123–8. doi: 10.1054/arth.2003.50025. [DOI] [PubMed] [Google Scholar]
- 10.Dorr LD, Maheshwari AV, Long WT, Wan Z, Sirianni LE. Early pain relief and function after posterior minimally invasive and conventional total hip arthroplasty.A prospetive randomized, blinded study. J Bone Joint Surg Am . 2007;89(6): 1153–60. doi: 10.2106/JBJS.F.00940. [DOI] [PubMed] [Google Scholar]
- 11.Vavken P, Kotz R, Dorotka R. Minimally invasive hip replacement.A meta-analysis. Z Orthop Unfall. 2007;145(2): 152–6. doi: 10.1055/s-2007-965170. [DOI] [PubMed] [Google Scholar]
- 12.Howell Jr, Masri BA, Duncan CP. Minimally invasive versus standard incision anterolateral hip replacement.A comparative study. Orthop Clin North Am. 2004;35(2): 153–62. doi: 10.1016/S0030-5898(03)00137-8. [DOI] [PubMed] [Google Scholar]
- 13.Higuchi F, Gotoh M, Yamaguchi N , et al. Minimally invasive uncemented total hip arthroplasty through an anterolateral approach with a shorter skin incision. J Orthop Sci. 2003;8(6): 812–7. doi: 10.1007/s00776-003-0715-x. [DOI] [PubMed] [Google Scholar]
- 14.Cheng T, Feng JG, Liu T, Zhang XL. Minimally invasive total hip arthroplasty.A systematic review. . Int Orthop. 2009;33(6): 1473–81. doi: 10.1007/s00264-009-0743-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Renken F, Renken S, Paech A, Wenzl M, Unger A, Schulz AP. Early functional results after hemiarthroplasty for femoral neck fracture.A randomized comparison between a minimal invasive and a conventional approach. BMC Musculoskelet Disord. 2012;13: 141. doi: 10.1186/1471-2474-13-141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Meneghini RM, Pagnano MW, Trousdale RT, Hozack WJ. Muscle damage during MIS total hip arthroplasty.Smith-Petersen versus posterior approach. Clin Orthop Relat Res. 2006;453: 293–8. doi: 10.1097/01.blo.0000238859.46615.34. [DOI] [PubMed] [Google Scholar]
- 17.Rachbauer F. Minimally invasive total hip arthroplasty.Anterior approach. Orthopade. 2006;35(7): 723–4, 6-9. doi: 10.1007/s00132-006-0964-4. [DOI] [PubMed] [Google Scholar]
- 18.Rachbauer F. Minimally invasive total hip arthroplasty via direct anterior approach. Orthopade. 2005;34(11): 1103–4, 6-8, 10. doi: 10.1007/s00132-005-0854-1. [DOI] [PubMed] [Google Scholar]
- 19.Unger AC, Schulz AP, Paech A, Jurgens C, Renken FG. Modified direct anterior approach in minimally invasive hip hemiarthroplasty in a geriatric population.A feasibility study and description of the technique. Arch Orthop Trauma Surg. 2013;33(11):1509–16. doi: 10.1007/s00402-013-1831-5. [DOI] [PubMed] [Google Scholar]
- 20.Ranawat CS, Dorr LD, Inglis AE. Total hip arthroplasty in protrusio acetabuli of rheumatoid arthritis. J Bone Joint Surg Am. 1980;62(7): 1059–65. [PubMed] [Google Scholar]
- 21.Parker MJ, Gurusamy K. Internal fixation versus arthroplasty for intracapsular proximal femoral fractures in adults. Cochrane Database Syst Rev. 2006;4: CD001708. doi: 10.1002/14651858.CD001708.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Berger RA, Jacobs JJ, Meneghini RM, Della Valle C, Paprosky W, Rosenberg AG. Rapid rehabilitation and recovery with minimally invasive total hip arthroplasty. Clin Orthop Relat Res. 2004;429: 239–47. doi: 10.1097/01.blo.0000150127.80647.80. [DOI] [PubMed] [Google Scholar]
- 23.Berry DJ, Berger RA, Callaghan JJ , et al. Minimally invasive total hip arthroplasty.Develoment early results, and a critical analysis. Presented at the Annual Meeting of the American Orthopaedic Association, Charleston, South Carolina, USA, June 14, 2003,. J Bone Joint Surg Am. 2003; 85-A(11): 2235–46. [PubMed] [Google Scholar]
- 24.Kennon RE, Keggi MJ, Keggi KJ. The minimally invasive anterior approach to hip arthroplasty. Orthopade. 2006;35(7): 731–7. doi: 10.1007/s00132-006-0965-3. [DOI] [PubMed] [Google Scholar]
- 25.Sculco TP, Jordan LC, Walter WL. Minimally invasive total hip arthroplasty.The Hospital for Special Surgery experience. Orthop Clin North Am. 2004;35(2): 137–42. doi: 10.1016/S0030-5898(03)00116-0. [DOI] [PubMed] [Google Scholar]
- 26.Sculco TP. Minimally invasive total hip arthroplasty.In the affirmative. J Arthroplasty. 2004;19(4 ) Suppl 1 : 78–80. doi: 10.1016/j.arth.2004.02.021. [DOI] [PubMed] [Google Scholar]
- 27.Su H, Aharonoff GB, Hiebert R, Zuckerman JD, Koval KJ. In-hospital mortality after femoral neck fracture.Do internal fixation and hemiarthroplasty differ? Am J Orthop (Belle Mead NJ) 2003;32(3): 151–5. [PubMed] [Google Scholar]
- 28.Ludemann M, Kreutner J, Haddad D, Kenn W, Rudert M, Noth U. MRI-based measurement of muscle damage after minimally invasive hip arthroplasty. Orthopade. 2012;41(5): 346–53. doi: 10.1007/s00132-011-1889-0. [DOI] [PubMed] [Google Scholar]
- 29.Tsukada S, Wakui M. Minimally invasive intermuscular approach does not improve outcomes in bipolar hemiarthroplasty for femoral neck fracture. J Orthop Sci. 2010;15(6): 753–7. doi: 10.1007/s00776-010-1541-6. [DOI] [PubMed] [Google Scholar]
- 30.Schneider K, Audige L, Kuehnel SP, Helmy N. The direct anterior approach in hemiarthroplasty for displaced femoral neck fractures. Int Orthop. 2012;36(9): 1773–81. doi: 10.1007/s00264-012-1535-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bjorgul K, Novicoff WM, Saleh KJ. Learning curves in hip fracture surgery. Int Orthop. 2011;35(1): 113–9. doi: 10.1007/s00264-010-0950-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lemos D, Nilssen E, Khatiwada B , et al. Dedicated orthopedic trauma theatres.Effect on morbidity and mortality in a single trauma centre. . Can J Surg. 2009;52(2): 87–91. [PMC free article] [PubMed] [Google Scholar]
- 33.Poh KS, Lingaraj K. Complications and their risk factors following hip fracture surgery. J Orthop Surg (Hong Kong). 2013;21(2): 154–7. doi: 10.1177/230949901302100207. [DOI] [PubMed] [Google Scholar]
- 34.Eberlein-Gonska M, Petzold T, Helass G, Albrecht DM, Schmitt J. The incidence and determinants of decubitus ulcers in hospital care.An analysis of routine quality management data at a university hospital. Dtsch Arztebl Int . 2013;110(33-34): 550–6. doi: 10.3238/arztebl.2013.0550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yli-Kyyny T, Ojanpera J, Venesmaa P , et al. Perioperative complications after cemented or uncemented hemiarthroplasty in hip fracture patients. Scand J Surg. 2013;102(2): 124–8. doi: 10.1177/1457496913482249. [DOI] [PubMed] [Google Scholar]
- 36.Roy L, Laflamme GY, Carrier M, Kim PR, Leduc S. A randomised clinical trial comparing minimally invasive surgery to conventional approach for endoprosthesis in elderly patients with hip fractures. Injury. 2010;41(4): 365–9. doi: 10.1016/j.injury.2009.10.002. [DOI] [PubMed] [Google Scholar]
- 37.Poignard A, Bouhou M, Pidet O, Flouzat-Lachaniette CH, Hernigou P. High dislocation cumulative risk in THA versus hemiarthroplasty for fractures. Clin Orthop Relat Res. 2011;469(11): 3148–53. doi: 10.1007/s11999-011-1987-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Biber R, Brem M, Singler K, Moellers M, Sieber C, Bail HJ. Dorsal versus transgluteal approach for hip hemiarthroplasty.An analysis of early complications in seven hundred and four consecutive cases. Int Orthop. 2012;36(11): 2219–23. doi: 10.1007/s00264-012-1624-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Burgers PT, Van Geene AR, Van den Bekerom MP , et al. Total hip arthroplasty versus hemiarthroplasty for displaced femoral neck fractures in the healthy elderly.A meta-analysis and systematic review of randomized trials. Int Orthop. 2012;36(8): 1549–60. doi: 10.1007/s00264-012-1569-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Laflamme GY, Rouleau DM, Leduc S, Roy L, Beaumont E. The Timed Up and Go test is an early predictor of functional outcome after hemiarthroplasty for femoral neck fracture. J Bone Joint Surg Am. 2012;94(13): 1175–9. doi: 10.2106/JBJS.J.01952. [DOI] [PubMed] [Google Scholar]
- 41.Schneppendahl J, Betsch M, Petrov V , et al. Recovery after hip fractures.Influence of bipolar hemiarthroplasty on physical disability and social dependency in the elderly. Hip Int. 2011;21(6): 751–6. doi: 10.5301/HIP.2011.8824. [DOI] [PubMed] [Google Scholar]
- 42.Preininger B, Jesacher M, Fabsits E, Winkler T. Earlier postoperative mobilization with minimally invasive hip hemiarthroplasty. Unfallchirurg. 2011;114(4): 333–9. doi: 10.1007/s00113-010-1773-0. [DOI] [PubMed] [Google Scholar]
- 43.Alecci V, Valente M, Crucil M, Minerva M, Pellegrino CM, Sabbadini DD. Comparison of primary total hip replacements performed with a direct anterior approach versus the standard lateral approach.Perioperative findings. J Orthop Traumatol. 2011;12(3): 123–9. doi: 10.1007/s10195-011-0144-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kinzl L, Bischoff M, Beck A. Endoprosthesis in medial femoral neck fractures. Chirurg. 2001;72(11): 1266–70. doi: 10.1007/s001040170029. [DOI] [PubMed] [Google Scholar]