Abstract
Patients with deficiency in the interferon gamma receptor (IFN-γR) are unable to respond properly to IFN-γ and develop severe infections with nontuberculous mycobacteria (NTM). IFN-γ and IFN-α are known to signal through STAT1 and activate many downstream effector genes in common. Therefore, we added IFN-α for treatment of patients with disseminated mycobacterial disease in an effort to complement their IFN-γ signaling defect.
We treated four patients with IFN-γR deficiency with adjunctive IFN-α therapy in addition to best available antimicrobial therapy, with or without IFN-γ, depending on the defect. During IFN-α treatment, ex vivo induction of IFN target genes was detected. In addition, IFN-α driven gene expression in patients’ cells and mycobacteria induced cytokine response were observed in vitro. Clinical responses varied in these patients. IFN-α therapy was associated with either improvement or stabilization of disease. In no case was disease exacerbated. In patients with profoundly impaired IFN-γ signaling who have refractory infections, IFN-α may have adjunctive anti-mycobacterial effects.
Keywords: IFN-γ receptor deficiency, mycobacterial disease, IFN-α, STAT1, IFN-γ, nontuberculous mycobacteria
INTRODUCTION
Type I (IFN-α/β) and type II interferons (IFN-γ) are important immunomodulatory cytokines classically associated with protection against viruses and intracellular pathogens, respectively. In patients with defects in IFN-γ signaling, M. tuberculosis (MTB), environmental nontuberculous mycobacteria (NTM), Bacillus Calmette-Guérin (BCG), dimorphic yeasts and Salmonella spp can cause infections which are typically extensive and can be fatal [1, 2].
Although the signaling pathways and the immunological functions of type I and type II interferons are thought to be somewhat distinct, they overlap through the common use of Janus kinase (JAK) 2 and Signal Transducer and Activator of Transcription (STAT) 1. Binding of IFN-γ to its specific receptors (IFN-γR1 and IFN R2) activates JAK1 and JAK2, leading to the phosphorylation of STAT1, the formation of active STAT1 homodimers, and the induction of IFN-γ target genes. Similarly, IFN-α/β bind to their shared receptors (IFNAR1 and IFNAR2) leading to activation of JAK1 and tyrosine kinase (Tyk) 2, the phosphorylation of STAT1 and STAT2, and the formation of STAT1 homodimers and STAT1/STAT2 heterodimers which activate both common IFN-γ and IFN-α target genes, respectively [3]. Interferon regulatory factor (IRF) 1 is important in regulating immune responses and is commonly induced by Type I and II interferons. The chemokines CXCL9 (monokine induced by interferon-gamma or MIG), CXCL10 (interferon-inducible protein-10, IP-10) and CXCL11 (interferoninducible T cell alpha-chemoattractant, I-TAC) are structurally and functionally related molecules. CXCL10 and CXCL11 are induced by IFN-α/β as well as IFN-γ, whereas CXCL9 induction is mostly restricted to IFN-γ [4]. These chemokines are best known for their roles in leucocyte trafficking, mainly on activated CD4+ Th1 cells, CD8+ T cells and NK cells. The enzyme indoleamine 2,3-dioxygenase (IDO) catabolizes the essential amino acid tryptophan and is induced by interferons. It plays a role in inhibiting replication of pathogens and also has immunoregulatory functions [5,6]. IFN-γ is approved for prophylaxis in chronic granulomatous disease (CGD), osteopetrosis [7, 8], and has been used in patients with refractory mycobacterial diseases [1]. IFN-α is approved for viral infections such as hepatitis [9], cystic hygroma [10] and chronic myelogenous leukemia [11]. IFNs modulate the production of inflammatory cytokines, such as TNF-α, which has antimicrobial properties. The importance of this pathway is evidenced by anti-TNF therapies, which increase susceptibility to mycobacterial infections, such as MTB, M. abscessus, M. avium, M. leprae and intracellular fungi [12–16]. The IFN pathway also impacts on the IL-1 response [17, 18], and mice deficient in IL-1 succumb to MTB infection [19, 20].
We describe four patients with mutations in the IFN-γ receptor whose disseminated mycobacterial infections were refractory to best available therapy. Adjunctive treatment with IFN-α was associated with variable clinical responses, some of which were extremely beneficial. Moreover, none had major toxicities or increased mycobacterial burdens while on IFN-α. Gene expression in vitro and ex vivo showed activation of both typical IFNa and IFN-γ inducible genes in response to IFN-α, as well as the sustained production of mycobacterium-induced TNF-α and IL-1β in vitro. IFN-α may be able to overcome some aspects of impaired IFN-γ signaling and to confer clinical benefits to a selected group of patients.
MATERIAL AND METHODS
Subjects
All patients (Table 1) were followed and treated at the National Institutes of Health, NIH. Patients or their guardians provided informed consent on approved protocols of the National Institutes of Health. Whole blood was obtained from patients before and after IFN-α administration. Blood from healthy volunteers and elutriated monocytes were obtained under appropriate protocols through the Department of Transfusion Medicine, NIH. Alveolar macrophages (AM) were isolated from bronchoalveolar lavage fluid obtained from normal donors on NIAID IRB approved protocols.
Table 1.
Patient characteristics
| Patient | Age | Sex | Immunodeficiency | Mutation | Country of origin | Age at disease onset | Isolated mycobacterial strains | Disease localization | Interferon treatment |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 22 | female | complete IFNγR1 deficiency | compound heterozygous 373(+1)g→t 202(-1)g→c |
US | 1 yr | MAC M. fortuitum M. kansasii M. abscessus |
bone bone marrow liver lung lymph nodes |
IFNα2b |
| 2 | 19 | Male | complete IFNγR1 deficiency | homozygous 22delC |
Pakistan | 2 yr | MAC M. abscessus |
blood liver lung lymph nodes skin |
IFNα2b → PEG IFN alpha |
| 3 | 5 | Male | partial IFNγR1 deficiency | homozygous I87T |
Chile | 2 mo | M. bovis BCG | bone brain lung lymph nodes pleura skin |
IFNα2b & IFNγ |
| 4 | 52 | female | partial IFNγR1 deficiency | heterozygous 818del4 |
US | 20 yr | MAC M. fortuitum M. avium X-cluster |
Maxillary sinus skin palate lymph nodes |
IFNα2b & IFNγ |
Cell culture and stimulation
Peripheral blood mononuclear cells (PBMCs) obtained from whole blood by gradient density centrifugation (BioWhittaker, Walkersville, MD) and elutriated monocytes were plated in (3×10 6 cells/well) in RPMI 1640 with 5% human AB serum, (Gibco BRL), 2mM L-glutamine, penicillin 100U/ml, 100μg/ml streptomycin, at 37°C. For monocyte differentiation, cells were kept in culture for 6–7 days, and allowed to differentiate into monocyte-derived macrophages (MDM). For AM, bronchoalveolar lavage (BAL) fluid was immediately cooled (4°C) and filtered through a cell strainer to remove particulate debris before centrifugation. Cells were counted and plated for stimulation as above. PBMC were either left unstimulated or stimulated with human IFN-γ 400 IU/ml (R&D System, Minneapolis, MN) or IFN-α2b 1,000 IU/ml (PBL Biomedical Laboratories, Piscataway, NJ). MDM and AM cultured in supplemented media without antibiotics were stimulated with live mycobacteria (M. avium, ATCC 35717) at a multiplicy of infection (MOI) of 5, in the presence or absence of IFN-γ or IFN-α for 3 h (for evaluation of gene expression) or 20 h (for detection of cytokine release). Supernatants were recovered and frozen at −20°C until use. Ex vivo evaluation of gene expression was assayed in cells (PBMC) obtained from patients before and after (14–20 h) IFN-α injection and left unstimulated.
Cytokine determination
Culture supernatants were further analyzed for cytokine levels using a custom bead based cytokine assay for IL-1β, TNF-α and of the chemokine CXCL10/IP-10 (Bio-Plex assay, BioRad, Hercules, CA), processed according to the manufacturer’s specifications.
Real time PCR
Total RNA was extracted from isolated cells with the RNeasy mini kit (QIAGEN). For RT-PCR, 1 μg of total RNA was reverse transcribed (Invitrogen) and the resulting cDNA amplified by PCR using the ABI 7500 Sequencer and Taqman expression assays (Applied Biosystems). GAPDH was used as a control for normalization.
Data were analyzed using the 2−ΔΔCT method and results expressed as mean fold induction.
Statistical analysis
Results are presented as mean ± standard deviation (SD). Statistical comparisons were made using Student’s t-test (GraphPad Prism Software, San Diego, CA). The statistical significance level adopted was p < 0.05.
RESULTS
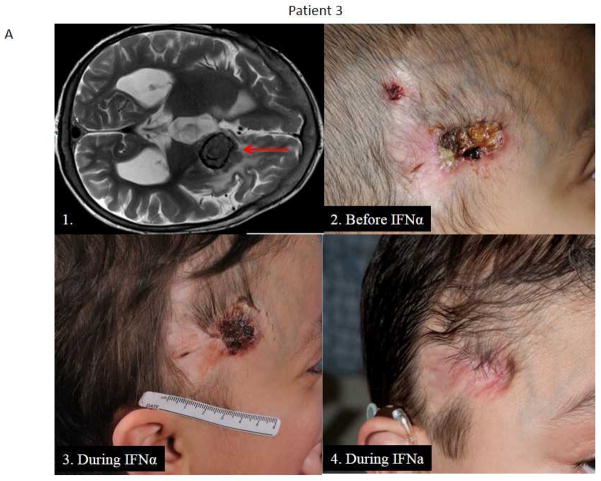
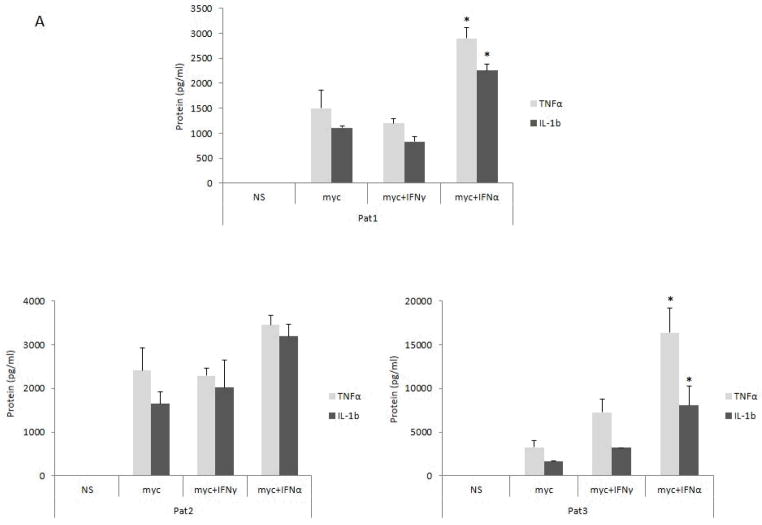
Patient 1 is a 22-year-old Caucasian woman born in the US to unrelated parents. Flow cytometry identified absent expression of IFN-γR1 on monocytes and lack of STAT1 phosphorylation in response to IFN-γ in vitro (not shown). She is compound heterozygous for IFNGR1 mutations: paternal allele, 373 (+1)g→t in intron 3 resulting in complete deletion of exon 3; maternal allele, 201(-1)g→c in intron 2 generating a cryptic splice site in the middle of exon 3 causing an in frame deletion of 34 aa. She presented at 1 year with disseminated Mycobacterium avium complex (MAC) involving bone, bone marrow, lung, lymph nodes and liver. While on antimycobacterial therapy, she had recurrent lymphadenopathy and osteomyelitis growing MAC, M. kansasii and M. fortuitum. At age 17, persistent pulmonary and mediastinal MAC (Fig. 1a) led to referral to the NIH and IFN-α2b, 3 million units three times weekly subcutaneously, was added. After three months on IFN-α, chest CT showed marked reduction of pulmonary disease, she reported increased energy, her temperature normalized, and after one year her lesions had resolved completely (Fig. 1b). Two years later she presented with abdominal pain and increased retroperitoneal lymphadenopathy due to M. abscessus. IFN-α was stopped and antimycobacterial regimen included carbapenems and tigecycline resulting in clinical improvement.
Figure 1.
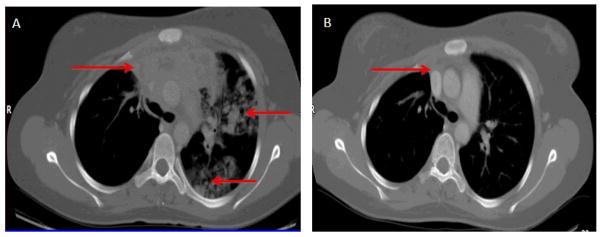
Patient 1 (a) CT chest showing necrotizing mediastinal lymphadenitis and extensive parenchymal disease due to refractory MAC infection; (b) After 1 year of treatment with IFN-α, cervical, mediastinal and parenchymal disease had resolved completely.
Patient 2 was a 19-year-old Pakistani male living in Norway whose cells had absent IFN-γR1 surface expression and lack of responsiveness to IFN-γ in vitro. He had homozygous IFNGR1 22delC leading to a frameshift and premature stop codon. He first presented to NIH at 4 years with a history of disseminated MAC [21]. At 13 years new submandibular and axillary lymphadenopathy grew M. abscessus, which was persistent and disseminated despite antimycobacterial therapy. After two years, with failure to thrive, weight loss and lymphadenopathy, linenezolid was changed to tigecycline and IFN-α2b (3 million units three times weekly subcutaneously) was added. At age 18 he was re-admitted with increasing hepatomegaly and deteriorating liver function tests. Meropenem was introduced and short acting changed to pegylated IFN-α. Blood cultures on pegylated IFN were reduced to <1 colony/ml M. abscessus. Three months later, new liver and lung lesions proved to be B-cell lymphoma; biopsies showed no mycobacteria. He died due to disseminated B-cell lymphoma at 20 years. No autopsy was performed.
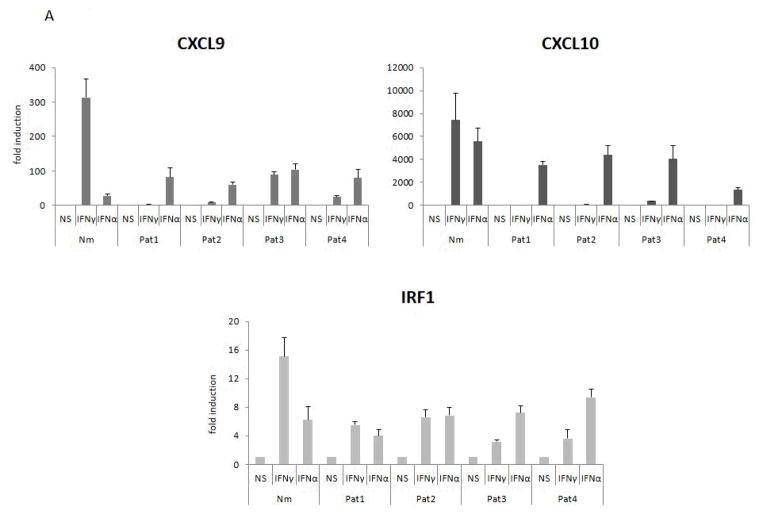
Patient 3 is a 7-year-old Chilean male who received BCG immunization at birth. At age two months he presented with hydrocephalus and cerebral lesions that grew M. bovis BCG with involvement of bone, lung and lymph nodes. At 2 years while on antimycobacterial therapy, partial IFN-γR1 deficiency due to homozygous I87T [22] was diagnosed. Two months of IFN-γ 150μg/m2 subcutaneously daily led to worsening hydrocephalus and fever. He was referred to the NIH at 3 years with severe failure to thrive, persistent hydrocephalus, intra-cerebral lesions (Fig. 2a.1), a draining head wound at the site of brain biopsy (Fig. 2a.2) and a large right pleural mass (Fig. 2b). The pleural mass biopsy grew multidrug resistant M. bovis. IFN-γ was re-started (150μg/m2 subcutaneously) three times weekly. His antimycobacterial regimen was extended to levofloxacin, linezolid, clofazimine, azithromycin and capreomycin. After three months, he remained ill and IFN-α2b, 0.1 million units subcutaneously three times weekly, was alternated with IFN-γ. On this regimen, he started gaining weight, his head wound healed (Fig. 2a.3, after 8 months on IFN-α therapy; Fig. 2a.4, after 21 months), his pleural mass decreased (Fig. 2c) and laboratory parameters slowly improved. He is now well without serious hospitalizations for over three years. His therapy has been reduced to azithromycin and IFN-γ alone.
Figure 2.
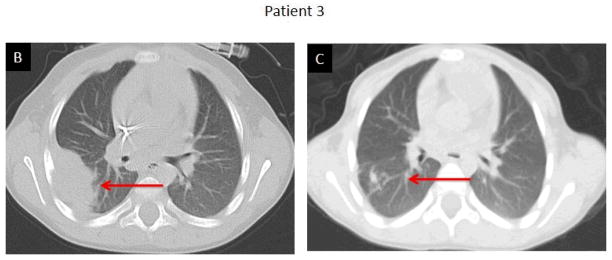
Patient 3 (a) 1. Multidrug resistant disseminated M. bovis BCG infection with intracerebral lesions; 2. A draining head wound; 3 and 4. The lesion progressively healed while on combined IFN-α and IFN-γ therapy; (b) A large right pleural mass before IFN-α which (c) completely resolved on combined IFN-α and IFN-γ treatment; (d) Laboratory paremeters improved following initiation of IFN-α (arrow).
Patient 4 is a 52-year-old Caucasian female with recurrent lymphadenopathy, rashes and hospitalizations since childhood. She has been treated with prolonged antibiotics and intermittent corticosteroids. In her 20s M. fortuitum was isolated from a lymph node. She was diagnosed with partially responsive IFNGR1 818del4 [23] after her son had osteomyelitis secondary to MAC and was found to have IFNGR1 818del4. Another son had died of disseminated MAC infection. At 50 years she presented with cervical and supraclavicular lymphadenopathy and her maxillary sinuses growing M. avium-X cluster. Therapy included doxycycline, clarithromycin, trimethoprim/sulfamethoxazole, rifampin and IFN-γ 100μg/m2 subcutaneously three times weekly. At 52 years new skin lesions and a hard palate fistula arose. In view of persistent and progressive disease, IFN-α2b 3 million units subcutaneously was added three times weekly alternated with IFN-γ. Her lymphadenopathy and skin infiltration improved and her fistula closed. Since that time she has had no new infections. She continues on both interferons and oral antibiotics.
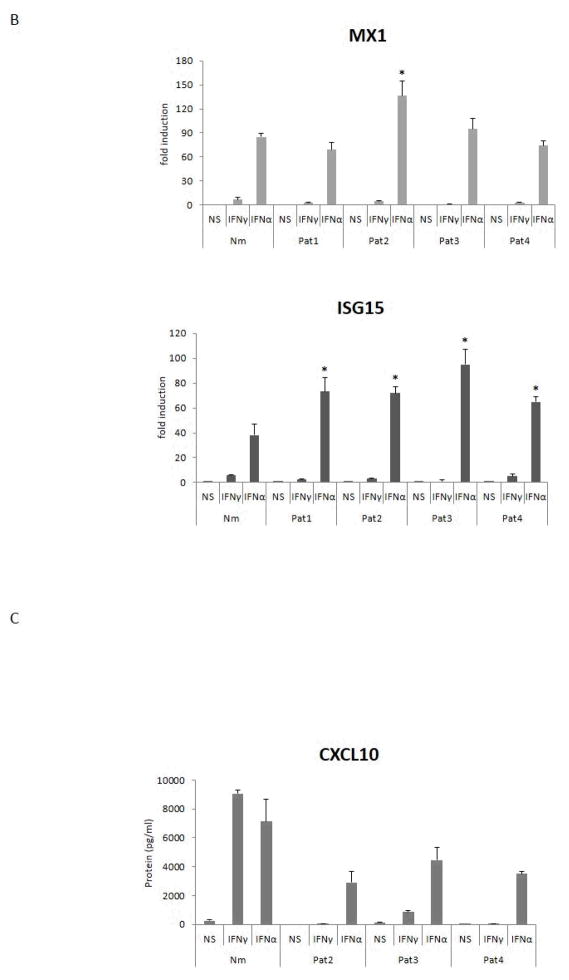
Analysis of gene expression in primary human cells in vitro
Cells from patients with partial or complete IFN-γR deficiency showed reduced or absent responses to stimulation with IFN-γ. Expression of CXCL9 and CXCL10 was strikingly diminished in patients 1, 2, 3, and 4 compared to controls. Induction of IRF1 in response to IFN-γ was about half normal (Fig. 3a). On the other hand, stimulation of the same cells with IFN-α raised the expression of CXCL10 (except patient 4), CXCL9 and IRF1 to levels close to normal (Fig. 3a). Induction of the more IFN-α specific target genes, MX1 and ISG15, was normal to high in patients’ cells (Fig. 3b). CXCL10 protein levels in stimulated culture supernatants correlated with message (Fig. 3c).
Figure 3. Gene expression in vitro.
PBMC from normal donors (Nm) and IFN-γR deficient patients were stimulated with IFN-γ (400 IU/ml) or IFN-α (1,000 IU/ml) for 3 h and assayed for the expression of target genes (a) CXCL9, CXCL10, IRF-1 and (b) MX1, ISG15. *p<0.05 vs. the response observed in healthy controls; (c) Levels of CXCL10 protein were assayed in the 20 h culture supernatants. Results are mean ± SD of five independent experiments.
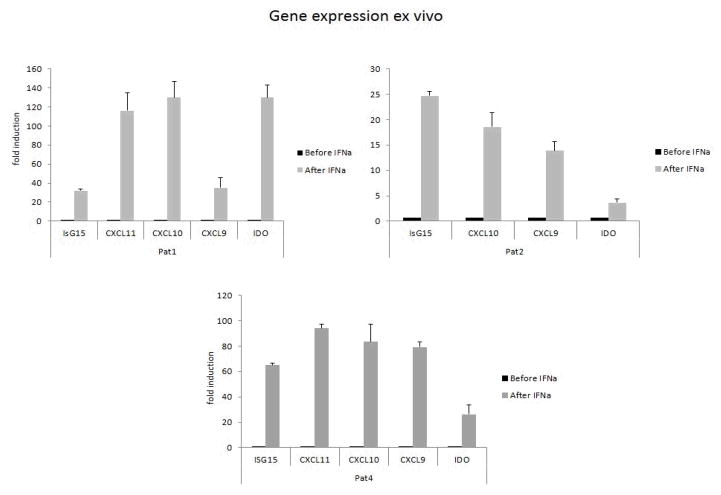
Ex vivo analysis of gene expression in patients’ cells following IFN-α treatment
Ex vivo mRNA expression was assayed in PBMCs from patients 1, 2 and 4 during treatment with IFN-α, looking at expression of ISG15, CXCL9, CXCL10, CXCL11 and IDO before and one day after injection. As expected, transcription of the typical IFN-α regulated gene ISG15 was enhanced after IFN-α injection (Fig. 4). Induction of CXCL9 and CXCL10, which are typically impaired in response to IFN-γ in patients with defective IFN-γ signalling, and of CXCL11 and IDO, genes modulated by both IFN-γ and IFN-α, were robustly up-regulated in patients’ PBMCs 18–20 h following IFN-α injection (Fig. 4).
Figure 4. Gene expression ex vivo.
Gene expression in fresh isolated unstimulated PBMC obtained from IFN-γR deficient patients was assayed before and 20 h after IFN-α injection. Results for each patient represent mean fold induction ± SD of triplicate wells for each condition compared to samples obtained before IFN-α injection.
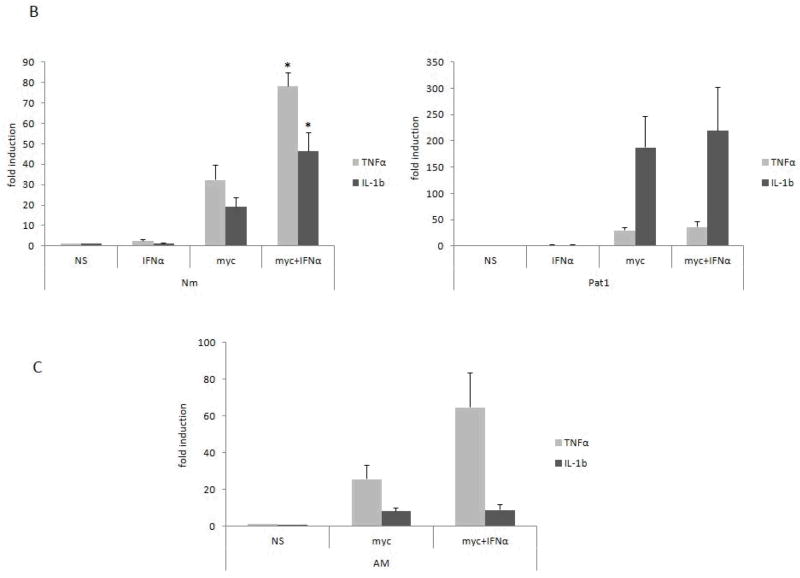
Mycobacteria induced cytokine response in vitro is sustained by IFN-α
Evaluation of the effect of IFN-α on in vitro cytokine production was assayed in MDM obtained from healthy donors and patients following incubation with mycobacteria. M. avium-induced TNF-α and IL-1β secretion were modestly to markedly enhanced following stimulation with IFN-α (Fig. 5a). Similar responses were observed when cells were stimulated with M. abscessus (not shown). In comparison to normals and to the findings on protein expression, Patient 1 cells showed robust induction of IL-1β message in response to mycobacteria, which was not much altered by IFN-α (Fig. 5b). A similar effect of IFN-α on M. avium induced responses was also detected in alveolar macrophages (Fig. 5c), suggesting that the modulatory action of IFN treatment may be active in the lung tissue environment.
Figure 5. Gene expression following mycobacterial stimulation.
(a) MDM obtained from patients were stimulated with mycobacteria (myc = M. avium, MOI 5) and IFN-α (1,000 IU/ml) added simultaneously to the wells. Supernatant levels (pg/ml) of TNF-α and IL-1β were assayed 20 h after culture stimulation; (b) Gene expression was evaluated in MDM 3 h after stimulation; (c) Alveolar macrophages (AM) obtained from normal donors were plated, stimulated and assayed as above. Results are mean ± SD of three independent experiments. *p<0.05 when compared to cells stimulated with mycobacteria alone.
Macrophage differentiation is known to be modulated by many factors, such as GM-CSF/CSF2, and M-CSF/CSF1, which lead to specific response profiles, cell morphologies and phenotypes (M1 and M2 macrophages, respectively) [24, 25]. The induction of CSF2 in MDM cultures (but not CSF1, not shown) triggered by the mycobacteria (M. avium, 342 ± 98.1 fold induction) was remarkable and sustained by IFN-α (M. avium + IFN-α, 756 ± 208).
DISCUSSION
We hypothesized that IFN-α could bypass defective IFN-γ signalling, since both use STAT1 and induce phospho-STAT1 homodimers. Further, low dose IFN-γ followed by IFN-α has been demonstrated to lead to STAT1 dependent up-regulation of typical IFN-γ inducible genes, shifting the IFN-α response to a more pro-inflammatory phenotype [26, 27].
IFN-α therapy seemed to be useful in our patients with IFN-γ signaling defects who had resistant intracellular infections. These four IFN-γR deficient patients suffered from extensive refractory disseminated mycobacterial infections due to compromised IFN-γ response. Although the extent of the clinical effect of IFN-α varied between patients, all showed some degree of clinical response with either improvement or stabilization.
Importantly, in no case did IFN-α therapy exacerbate disease. Signaling through both the IFN-γ and the IFN-α receptors is both specific and promiscuous. In addition to the canonical STATs (STAT1, STAT2), others are activated following the same signals (STAT3, STAT4) [1, 28]. The activation of STAT1 dependent genes is reinforced here since ex vivo mRNA expression after IFN-α injection in patients 1, 2, and 4 clearly showed the induction of both common IFN genes and more classical IFN-γ specific genes, supporting the hypothesis that IFN-α activation, at least at pharmacologic doses and adminstrations, overlaps molecularly to some extent with IFN-γ activation. In vitro expression of IFN-γ and IFN-α induced genes observed in these patients followed IFN-α stimulation were similar to or higher than those levels induced in normals. It remains unclear to what extent IFN-α can replace IFN-γ in the setting of IFN-γR deficiency, but it clearly fails to do so spontaneously.
Patient 1 showed marked clinical and radiological response to IFN-α within two months of treatment, followed by further improvement over the next year. It is unlikely that this effect was caused by the change of azithromycin for clarithromycin in her antimycobacterial regimen. Interestingly, after two years on IFN-α therapy she developed disseminated M. abscessus infection, suggesting that conventional dose IFN-α was able to control MAC but insufficient to prevent M. abscessus infection. Patient 2 had persistent M. abscessus infection in the lung, blood and liver despite conventional IFN-α therapy. The use of pegylated IFN-α with its different pharmacokinetic and pharmacodynamic properties may have been effective in this condition, as it is in hepatitis B and C [29, 30].
Following introduction of pegylated IFN-α, the patient’s liver biopsy and culture showed no mycobacteria and his last set of blood cultures were negative for MAC. Patient 3 had impaired IFN-γ signalling, but had enough residual function that high dose daily IFN-γ led to fever, inflammation and hydrocephalus. We reduced his IFN-γ to every other day, which he tolerated better and then added IFN-α because his extensive multidrug resistant BCG infection persisted despite aggressive antimycobacterial treatment with end organ toxicity. The combination of IFN-α and IFN-γ treatment led to rapid and sustained clinical improvement. Despite persistent infection over many years, patient 4 had significant clinical improvement only following the combination of IFN-α and IFN-γ therapy. Two other patients treated with IFN-α in the setting of IFN-γR deficiency have been previously reported [31–33]. These patients showed mild transient clinical improvement even though IFN-α therapy was introduced late in the course of severe disseminated disease.
Type I interferons are constitutively produced in a broad range of tissues, are critical mediators of the innate and adaptive immune responses and modulate macrophage function [17, 34]. IL-1 has important proinflammatory effects and contributes to host defence. Moreover, macrophage differentiation and release of cytokines, such as TNF-α and GM-CSF, are critical for control and resolution of infection and are induced by mycobacteria. We found that MDM from normals and patients co-stimulated with M. avium and IFN-α (or IFN-γ) showed no downregulation of TNF-α or IL-1 responses.
The clinical impact of IFN-α therapy on these patients and the in vitro data are in sharp contrast to reports of enhanced MTB growth in mice associated with induction of Type I interferons [19, 20, 35]. The use of the potent stimulator of IFN-α production, Poly-IC, led to suppression of IL-1 production in MTB infected mice, arguing against a beneficial effect of IFN-α in mycobacterial control [19, 20]. However, the differences between these studies and our observations include host and pathogen species, as well as the potentially complex nature of the Poly-IC itself. Other studies described enhanced mycobacterial growth with IFN-α administration [36] or enhanced IFN gene signature in patients with active tuberculosis [37, 38]. Some studies have shown increased mycobacterial burden in IFN-α deficient mice [39], decreased mycobacterial burden in mice treated with IFN-β [40], and increased chemotaxis of T cells activated by IFN-α and mycobacterial infection [41]. One recent publication showed that IFN-α was unable to up-regulate LPS-induced TNF-α secretion in human MDM and was not associated with in vitro killing of M. smegmatis [42]. The effects of IFNs on macrophage responses will likely be dependent on cell differentiation and activation state. It is feasible to postulate that patients 1 and 2 reported here had some baseline levels of IFN-γ response in vivo, which allowed some effective clinical responses to IFN-α. The beneficial effects of IFN-α treatment may rely on the priming effects that IFN-γ and IFN-α exert on each other in mutual responses [26]. Recently, Bogunovic et al. [43] described patients with inherited ISG15 deficiency who had associated mycobacterial disease. ISG15 is induced by IFN-α and activates T and NK cells to more effective production of IFN-γ, a mechanism that could also enhance control of mycobacterial disease in our setting. The investigation of mechanisms by which IFN-α helps these patients to control infection need to be extended to investigate the role of other cytokines and microbicidal assays.
Since mycobacterial species can behave differently in their induction of inflammatory responses as well as their responses to treatment, adjunctive IFN-α therapy may drive different effects depending on the type of mycobacteria and on the patient’s clinical condition. Despite the variability of response, IFN-α induces typical IFN-γ responsive genes in vivo and may boost therapeutic anti-mycobacterial effects in patients with NTM infections caused by IFN-γ signaling disorders. The mechanisms, optimal dosing regimen and optimum time to initiate this therapy remain to be determined.
Acknowledgments
We are grateful to M.E. Hanks for technical assistance. The research was supported by the Division of Intramural Research of National Institute of Allergy and Infectious Diseases, National Institutes of Health.
Footnotes
Conflict of Interest: The authors declare that they have no conflicts of interest.
References
- 1.Boisson-Dupuis S, Kong XF, Okada S, Cypowyj S, Puel A, Abel L, Casanova JL. Inborn errors of human STAT1: allelic heterogeneity governs the diversity of immunological and infectious phenotypes. Curr Opin Immunol. 2012;24:364–78. doi: 10.1016/j.coi.2012.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Holland SM. Immunotherapy of mycobacterial infections. Semin Respir Infect. 2001;16:47–59. doi: 10.1053/srin.2001.22728. [DOI] [PubMed] [Google Scholar]
- 3.Stark GR, Darnell JE., Jr The JAK-STAT pathway at twenty. Immunity. 2012;36:503–14. doi: 10.1016/j.immuni.2012.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mantovani A, Sica A, Sozzani S, Allavena P, Vecchi A, Locati M. The chemokine system in diverse forms of macrophage activation and polarization. Trends in Immunol. 2004;25:677–86. doi: 10.1016/j.it.2004.09.015. [DOI] [PubMed] [Google Scholar]
- 5.Heseler K, Spekker K, Schmidt SK, MacKenzie CR, Däubener W. Antimicrobial and immunoregulatory effects mediated by human lung cells: role of IFN-gamma-induced tryptophan degradation. FEMS Immunol Med Microbiol. 2008;52:273–81. doi: 10.1111/j.1574-695X.2007.00374.x. [DOI] [PubMed] [Google Scholar]
- 6.Fallarino F, Grohmann U, Puccetti P. Indoleamine 2,3-dioxygenase: from catalyst to signaling function. Eur J Immunol. 2012;42:1932–7. doi: 10.1002/eji.201242572. [DOI] [PubMed] [Google Scholar]
- 7.Marciano BE, Wesley R, De Carlo ES, Anderson VL, Barnhart LA, Darnell D, et al. Long-term interferongamma therapy for patients with chronic granulomatous disease. Clin Infect Dis. 2004;39:692–9. doi: 10.1086/422993. [DOI] [PubMed] [Google Scholar]
- 8.Key LL, Jr, Rodriguez RM, Willi SM, Wright NM, Hatcher HC, Eyre DR, et al. Long-term treatment of osteopetrosis with recombinant human interferon gamma. N Engl J Med. 1995;332:1594–9. doi: 10.1056/NEJM199506153322402. [DOI] [PubMed] [Google Scholar]
- 9.McHutchison JG, Lawitz EJ, Shiffman ML, Muir AJ, Galler GW, McCone J, et al. Peginterferon alpha-2b or alpha-2a with ribavirin for treatment of hepatitis C infection. N Engl J Med. 2009;361:580–93. doi: 10.1056/NEJMoa0808010. Erratum in: N Engl J Med 2009, 361, 1027. [DOI] [PubMed] [Google Scholar]
- 10.Senoh D, Hanaoka U, Tanaka Y, Tanaka H, Hayashi K, Yanagihara T, Hata T. Antenatal ultrasonographic features of fetal giant hemangiolymphangioma. Ultrasound Obstet Gynecol. 2001;17:252–4. doi: 10.1046/j.1469-0705.2001.00347.x. [DOI] [PubMed] [Google Scholar]
- 11.Simonsson B, Hjorth-Hansen H, Bjerrum OW, Porkka K. Interferon alpha for treatment of chronic myeloid leukemia. Curr Drug Targets. 2011;12:420–8. doi: 10.2174/138945011794815301. [DOI] [PubMed] [Google Scholar]
- 12.Solovic I, Sester M, Gomez-Reino JJ, Rieder HL, Ehlers S, Milburn HJ, et al. The risk of tuberculosis related to tumour necrosis factor antagonist therapies: a TBNET consensus statement. Eur Respir J. 2010;36:1185–206. doi: 10.1183/09031936.00028510. [DOI] [PubMed] [Google Scholar]
- 13.Besada E. Rapid growing mycobacteria and TNF-α blockers: case report of a fatal lung infection with Mycobacterium abscessus in a patient treated with infliximab, and literature review. Clin Exp Rheumatol. 2011;29:705–7. [PubMed] [Google Scholar]
- 14.Winthrop KL, Chang E, Yamashita S, Iademarco MF, LoBue PA. Nontuberculous mycobacteria infections and anti-tumor necrosis factor-a therapy. Emerg Infect Dis. 2009;15:1556–61. doi: 10.3201/eid1510.090310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lluch P, Urruticoechea A, Lluch J, Moll MC, Matos M, Benet JM, et al. Development of leprosy in a patient with rheumatoid arthritis during treatment with etanercept: a case report. Semin Arthritis Rheum. 2012;42:127–30. doi: 10.1016/j.semarthrit.2012.03.003. [DOI] [PubMed] [Google Scholar]
- 16.Smith JA, Kauffman CA. Endemic fungal infections in patients receiving tumour necrosis factor-alpha inhibitor therapy. Drugs. 2009;69:1403–15. doi: 10.2165/00003495-200969110-00002. [DOI] [PubMed] [Google Scholar]
- 17.Trinchieri G. Type I interferon: friend or foe? J Exp Med. 2010;207:2053–63. doi: 10.1084/jem.20101664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Novikov A, Cardone M, Thompson R, Shenderov K, Kirschman KD, Mayer-Barber KD, et al. Mycobacterium tuberculosis triggers host type I IFN signaling to regulate IL-1β production in human macrophages. J Immunol. 2011;187:2540–7. doi: 10.4049/jimmunol.1100926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Antonelli LR, Gigliotti Rothfuchs A, Goncalves R, Roffe E, Cheever AW, et al. Intranasal Poly-IC treatment exacerbates tuberculosis in mice through the pulmonary recruitment of a pathogen-permissive monocyte/macrophage population. J Clin Invest. 2010;120:1674–82. doi: 10.1172/JCI40817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mayer-Barber KD, Andrade BB, Barber DL, Hieny S, Feng CG, Caspar P, et al. Innate and adaptive interferons suppress IL-1α and IL-1β production by distinct pulmonary myeloid subsets during Mycobacterium tuberculosis infection. Immunity. 2011;35:1023–34. doi: 10.1016/j.immuni.2011.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Holland SM, Dorman SE, Kwon A, Pitha-Rowe IF, Frucht DM, Gerstberger SM, et al. Abnormal regulation of interferon-gamma, interleukin-12, and tumor necrosis factor-alpha in human interferongamma receptor 1 deficiency. J Infect Dis. 1998;178:1095–104. doi: 10.1086/515670. [DOI] [PubMed] [Google Scholar]
- 22.Sologuren I, Boisson-Dupuis S, Pestano J, Vincent QB, Fernández-Pérez L, Chapgier A, et al. Partial recessive IFN-γR1 deficiency: genetic, immunological and clinical features of 14 patients from 11 kindreds. Hum Mol Genet. 2011;20:1509–23. doi: 10.1093/hmg/ddr029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dorman SE, Picard C, Lammas D, Heyne K, van Dissel JT, Baretto R, Rosenzweig SD, Newport M, Levin M, Roesler J, Kumararatne D, Casanova JL, Holland SM. Clinical features of dominant and recessive interferon gamma receptor 1 deficiencies. Lancet. 2004;364:2113–21. doi: 10.1016/S0140-6736(04)17552-1. [DOI] [PubMed] [Google Scholar]
- 24.Martinez FO, Gordon S, Locati M, Mantovani A. Transcriptional profiling of the human monocyte-tomacrophage differentiation and polarization: new molecules and patterns of gene expression. J Immunol. 2006;177:7303–11. doi: 10.4049/jimmunol.177.10.7303. [DOI] [PubMed] [Google Scholar]
- 25.Lacey DC, Achuthan A, Fleetwood AJ, Dinh H, Roiniotis J, Scholz GM, Chang MW, Beckman SK, Cook AD, Hamilton JA. Defining GM-CSF- and macrophage-CSF-dependent macrophage responses by in vitro models. J Immunol. 2012;188:5752–65. doi: 10.4049/jimmunol.1103426. [DOI] [PubMed] [Google Scholar]
- 26.Tassiulas I, Hu X, Ho H, Kashyap Y, Paik P, Hu Y, et al. Amplification of IFN-alpha-induced STAT1 activation and inflammatory function by Syk and ITAM-containing adaptors. Nat Immunol. 2004;5:1181–9. doi: 10.1038/ni1126. [DOI] [PubMed] [Google Scholar]
- 27.Hu X, Ivashkiv LB. Cross-regulation of signaling pathways by interferon-gamma: implications for immune responses and autoimmune diseases. Immunity. 2009;31:539–50. doi: 10.1016/j.immuni.2009.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Casanova JL, Holland SM, Notarangelo LD. Inborn errors of human JAKs and STATs. Immunity. 2012;36:515–28. doi: 10.1016/j.immuni.2012.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Aghemo A, Rumi MG, Colombo M. Pegylated IFN-alpha2a and ribavirin in the treatment of hepatitis C. Expert Rev Anti Infect Ther. 2009;7:925–35. doi: 10.1586/eri.09.70. [DOI] [PubMed] [Google Scholar]
- 30.Keating GM. Peginterferon-alpha-2a (40 kD): A review of its use in chronic hepatitis B. Drugs. 2009;69:2633–60. doi: 10.2165/11203660-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 31.Dorman SE, Holland SM. Mutation in the signal-transducing chain of the interferon-gamma receptor and susceptibility to mycobacterial infection. J Clin Invest. 1998;101:2364–9. doi: 10.1172/JCI2901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ward CM, Jyonouchi H, Kotenko SV, Smirnov SV, Patel R, Aguila H, et al. Adjunctive treatment of disseminated Mycobacterium avium complex infection with interferon alpha-2b in a patient with complete interferon-gamma receptor R1 deficiency. Eur J Pediatr. 2007;166:981–5. doi: 10.1007/s00431-006-0339-1. [DOI] [PubMed] [Google Scholar]
- 33.Rapkiewicz AV, Patel SY, Holland SM, Kleiner DE. Hepatoportal venopathy due to disseminated Mycobacterium avium complex infection in a child with IFN-gamma receptor 2 deficiency. Virchows Arch. 2007;451:95–100. doi: 10.1007/s00428-007-0427-2. [DOI] [PubMed] [Google Scholar]
- 34.Yarilina A, Ivashkiv LB. Type I interferon: a new player in TNF signaling. Curr Dir Autoimmun. 2010;11:94–104. doi: 10.1159/000289199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Manca C, Tsenova L, Bergtold A, Freeman S, Tovey M, Musser JM, et al. Virulence of a Mycobacterium tuberculosis clinical isolate in mice is determined by failure to induce Th1 type immunity and is associated with induction of IFN-alpha/beta. Proc Natl Acad Sci USA. 2001;98:5752–7. doi: 10.1073/pnas.091096998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bouchonnet F, Boechat N, Bonay M, Hance AJ. Alpha/beta interferon impairs the ability of human macrophages to control growth of Mycobacterium bovis BCG. Infect Immun. 2002;70:3020–5. doi: 10.1128/IAI.70.6.3020-3025.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Berry MP, Graham CM, McNab FW, Xu Z, Bloch SA, Oni T, et al. An interferon-inducible neutrophildriven blood transcriptional signature in human tuberculosis. Nature. 2010;466:973–7. doi: 10.1038/nature09247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ottenhoff TH, Dass RH, Yang N, Zhang MM, Wong HE, Sahiratmadja E, et al. Genome-wide expression profiling identifies type 1 interferon response pathways in active tuberculosis. PLoS One. 2012;7:e45839. doi: 10.1371/journal.pone.0045839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kuchtey J, Fulton SA, Reba SM, Harding CV, Boom WH. Interferon-alpha/beta mediates partial control of early pulmonary Mycobacterium bovis bacillus Calmette-Guerin infection. Immunology. 2006;118:39–49. doi: 10.1111/j.1365-2567.2006.02337.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Denis M. Recombinant murine beta interferon enhances resistance of mice to systemic Mycobacterium avium infection. Infect Immun. 1991;59:1857–9. doi: 10.1128/iai.59.5.1857-1859.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lande R, Giacomini E, Grassi T, Remoli ME, Iona E, Miettinen M, et al. IFN-alpha/beta released by Mycobacterium tuberculosis-infected human dendritic cells induces the expression of CXCL10: selective recruitment of NK and activated T cells. J Immunol. 2003;170:1174–82. doi: 10.4049/jimmunol.170.3.1174. [DOI] [PubMed] [Google Scholar]
- 42.van de Wetering D, van Wengen A, Savage NDL, van de Vosse E, van Dissel JT. IFN-α cannot substitute lack of IFN-γ responsiveness in cells of an IFN-γR1 deficient patient. Clin Immunol. 2011;138:282–90. doi: 10.1016/j.clim.2010.12.005. [DOI] [PubMed] [Google Scholar]
- 43.Bogunovic D, Byun M, Durfee LA, Abhyankar A, Sanal O, Mansouri D, et al. Mycobacterial disease and impaired IFN-γ immunity in humans with inherited ISG15 deficiency. Science. 2012;337:1684–8. doi: 10.1126/science.1224026. [DOI] [PMC free article] [PubMed] [Google Scholar]