Abstract
Background
Early repolarization (ER), a common electrocardiographic phenotype, has been associated with increased mortality risk in middle-aged adults. Data are sparse on long-term follow-up and outcomes associated with ER in younger adults.
Methods and Results
We prospectively examined 5,039 participants (mean age 25 years at baseline, 40% black) from the CARDIA cohort over 23 years. Twelve-lead electrocardiograms were recorded and analyzed at Years 0, 7 and 20 and coded as definite or probable ER using a standardized algorithm. Cox regression was used, and models were adjusted for important baseline and clinical covariates. Kaplan-Meier curves were created for presence of ER and total mortality and cardiovascular (CV) mortality. Participants with ER were more likely to be black, male, smoke, have higher systolic blood pressure, lower heart rate, and BMI, and also higher exercise duration, and longer PR, QRS and QT intervals. ER was associated with total mortality (HR1.77, 1.38–2.28, p<0.01), and CV mortality (HR 1.59, 1.01–2.50, p=0.04) in unadjusted analyses, but adjustment for age, sex, and race attenuated associations almost completely. Sex-race stratified analyses showed no significant associations between ER and outcome for any of the subgroups except blacks.
Conclusions
The presence of ER at any time point over 23 years of follow-up was not associated with adverse outcomes. Black race and male sex confound the unadjusted association of ER and outcomes, with no race-sex interactions noted. Further studies are necessary to understand the factors associated with heightened risk of death in those who maintain ER into and beyond middle age.
Keywords: ECG, ECG criteria, outcome, mortality, early repolarization
Introduction
Data regarding the prognostic significance of the classic ER phenotype in young adults, in whom early repolarization (ER) is much more common (prevalence of 15–30%), are sparse.1–6 Reports to date have focused on middle-aged (and not young) subjects, single (rather than serial) ECG assessments, limited race/ethnicity groups and abbreviated follow-up.7–10 It is, therefore, important to provide prospective evaluation of the prognosis of the classical definition of ER using a young, contemporary cohort balanced on sex and race. When encountering ER on a standard 12-lead ECG, the everyday practicing clinician seeks guidance as to the prognostic significance of this more prevalent ER phenotype.
Given the low prevalence of the more ominous ER phenotype, and the limitations of prior studies using the more classic definition of ER, our goal was to explore whether the classic ER phenotype was associated with adverse outcomes. Our evaluation includes several strengths: 1) cohort balanced on sex and race; 2) serial ECG assessment over 20 years; 3) contemporary risk factors; and 4) rigorous adjudication of outcomes.
Using the Coronary Artery Disease Risk in Adults (CARDIA) study, we analyzed high-quality 12-lead ECGs for the presence of ER starting at a young age (age 25 years at baseline) to middle age (mean age 45 years) and assessed whether the presence of ER was associated with adverse outcomes, specifically total mortality and cardiovascular mortality. Such knowledge will expand understanding of the mechanisms and natural history of this important ECG phenotype and may help elucidate and refine which phenotypes may be associated with an increased risk of mortality and sudden cardiac death.
Methods
Study Sample
The CARDIA cohort was initiated to investigate the development of heart disease risk factors beginning in young adulthood. Details of the study design and procedures have previously been published.11 Briefly, 5115 men and women aged 18 to 30 years with approximate balance in distribution of sex, race (black and white), and education were enrolled in 1985 and 1986 from 4 field centers: Birmingham, AL (University of Alabama at Birmingham); Chicago, IL (Northwestern University); Minneapolis, MN (University of Minnesota); and Oakland, CA (Kaiser Permanente Northern California). Participants were examined at baseline (Y0) and at follow-up examinations in year 2 (Y2), Y5, Y7, Y10, Y15, Y20 and Y25. The CARDIA study has had a high retention rate, with 72% completing the in-person examination at Y20. With the addition of telephone contact with participants who did not attend exams, follow-up has been maintained on 91% of all baseline participants. For the present analysis, we used data from participants attending the Y0, Y7, and Y20 exam dates from whom resting 12-lead ECGs were obtained. Outcomes were adjudicated through Y23. Of the initial 5115 participants, there were 34 participants with missing baseline ECG’s and 12 with ECG abnormalities that preclude diagnosis of ER. Therefore, the total number of participants included in the present analysis is 5039 for Y0. Using hierarchical exclusion procedures for participants with missing ECG’s (N=1393 for Y7, N=2546 for Y20), ECGs with abnormalities precluding the diagnosis of ER, such as paced rhythms, WPW, QRS duration > 120 msec (N=2 for Y7, N=10 for Y20) or medications affecting ST segment, such as antiarrhythmic drugs (N=5 for Y7, N=8 for Y20), there were 3676 participants available for the Y7 analysis, and 2523 for Y20. All participants signed informed consent at each examination, and the institutional review boards at each site approved study protocols.
Clinical Characteristics
Demographic, anthropometric, physiologic, and laboratory measurements for each participant were obtained according to previously published standardized protocols.11 Briefly, clinical covariates from Years 0 and 20, selected a priori because of their known association with cardiovascular diseases, included age, sex, race, measures of blood pressure, height and weight, body-mass index (BMI), smoking history, and total and HDL-cholesterol. Race and sex were reported by the study participants. Weight was measured with the use of a standard balance-beam scale, with the participant wearing light clothing without shoes. The body-mass index was calculated as the weight in kilograms divided by the square of the height in meters. Diabetes was considered to be present if the person was taking medication for diabetes. Total cholesterol and high-density lipoprotein (HDL) cholesterol were measured from fasting samples.
Echocardiographic Imaging
As part of the examination at Y5, CARDIA participants underwent two-dimensional and M-mode echocardiography performed on an Acuson cardiac ultrasound (Siemens) machine. Measurements were performed using standard echocardiogram definitions.
ECG Analysis
Resting ECGs were obtained in conjunction with the CARDIA Fitness Study, an ancillary study of the main CARDIA cohort during examinations at Y0, Y7, and Y20.4 ECGs were recorded immediately prior to the exercise portion of exam visits Y0, Y7, and Y20. For resting electrocardiography, all participants had standard limb and precordial ECG leads placed, with use of the Heartsquare device12 to determine appropriate placement of the precordial leads (V1–V6). Identical electrocardiographs (at Y20, GE MAC1200 Marquette Electronics, Milwaukee, WI) were used in all clinical centers. For the Year 0 and 7 ECGs, hard copies of the tracings were sent to the Central ECG Laboratory (EPICARE Center, Wake Forest University, Winston-Salem, North Carolina) and visually read for the ECG definitions of ER used specifically for this study. At Y20, ECG recordings were transmitted via modem to the EPICARE Center for reading using Marquette 12SL (GE Marquette, Milwaukee, Wisconsin). All ECGs received were inspected visually to detect technical errors, missing leads, and inadequate quality, and such records were rejected from electrocardiographic data files.
Definition and Coding of ER
ER was diagnosed using a definition developed by the Epidemiological Cardiology Research Center (EPICARE, Winston-Salem, NC), which is based on application of strict criteria selected from previous publications as follows: a) Definite ER: STJ elevation > 1mm in ≥ 50% of beats, T wave amplitude ≥ 5 mm, prominent J point, upward concavity of the ST, and a distinct notch or slur on the downstroke of the R wave in any of V3–V6; or STJ elevation > 2mm in ≥ 50% of beats, T wave amplitude ≥ 5 mm, prominent J point and upward concavity of the ST segment in any of V3–V6. For the STJ elevation, there had to be > 1 mm in ≥ 50% of beats, where there is at least > 1 mm elevation at the J joint that maintains at least 1 mm elevation until the end of the ST segment. b) Probable ER: STJ elevation > 1mm in ≥ 50% of beats, prominent J point, and upward concavity of the ST segment in any of V3–V6 and T wave amplitude ≥ 8 mm in any of the chest leads. For the STJ elevation, there had to be > 1 mm in ≥ 50% of beats, where there is at least > 1mm elevation at the J point that maintains at least 1 mm elevation until the end of the ST segment. and c) Possible ER: presence of Minnesota code 9–2 [ST segment elevation > 1.0mm in any of leads I, II, III, aVL, aVF, V5 and V6 OR ST segment elevation > 2.0 mm in any of leads V1–V4] or Minnesota code 9–5 [T-wave amplitude > 12 mm in any of leads I,II,III,aVL,aVF,V1,V2,V3,V4, V5, V6]13 (See Figure 1). Possible ER and no ER are combined as one group in the analysis. All ECGs were read for ER characteristics by a single reader. Details of the reproducibility and repeatability of this coding algorithm has been previously reported.14
Figure 1.
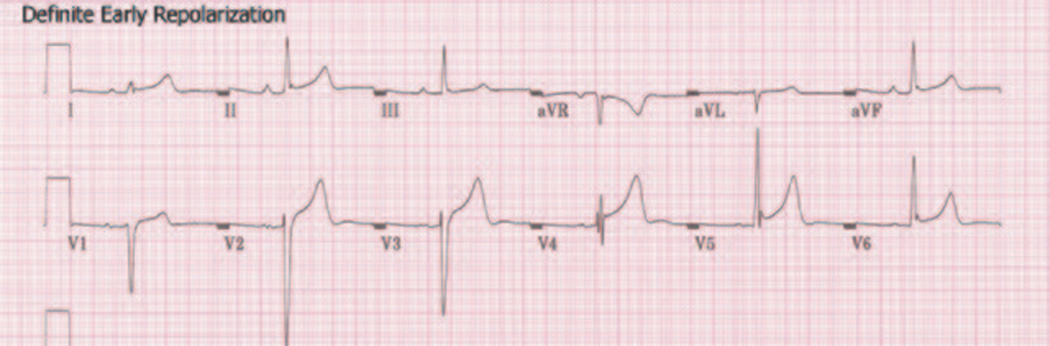
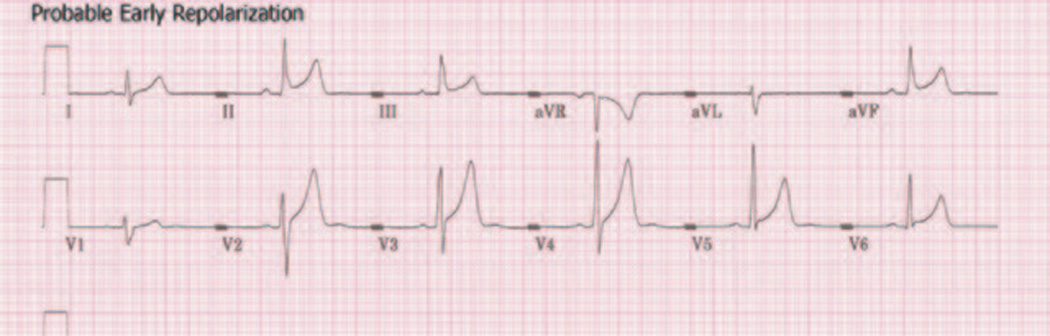
A: Example of “definite” early repolarization using EPICARE definition. B: Example of “probable” early repolarization using EPICARE definition. “Definite” and “probable” patterns of early repolarization - Definite ER is defined as presence of STJ elevation > 1mm in ≥50% of beats, T wave amplitude ≥5 mm, prominent J point, upward concavity of the ST, and a distinct notch or slur on the downstroke of the R wave in any of V3–V6; or STJ elevation > 2mm in ≥50% of beats, T wave amplitude ≥5 mm, prominent J point and upward concavity of the ST segment in any of V3–V6. Probable ER is defined a STJ elevation > 1mm in ≥ 50% of beats, prominent J point, and upward concavity of the ST segment in any of V3–V6 and T wave amplitude ≥8 mm in any of the chest leads
Similar to all Minnesota codes, Definite and Probable are in hierarchical order, where the most serious/most confirmed overrides the less serious/less confirmed. Therefore, Definite is defined first (i.e. the denominator is all participants), then among the remaining participants who are not classified as “Definite,” “Probable” is then explored (i.e. the denominator is everyone that is not classified as Definite). Using this hierarchical methodology, categories of ER were created as defined above.
Outcomes Adjudication
Participants were followed for the development of incident cardiovascular events up to 23 years from their baseline examinations. Trained personnel abstracted any medical records suggesting possible cardiovascular events. Physicians from the CARDIA study events committee, blinded to CARDIA study data and ECG results, independently reviewed all medical records for end point classification using pre-specified criteria. Event classification was determined by reviewers and adjudication was performed as necessary. Reviewers classified myocardial infarction (MI) as definite, probable, or absent, based on pre-specified criteria, including symptoms (e.g., chest pain), ECG abnormalities, and cardiac biomarker levels. These criteria have been previously described.15 Total mortality was death from any cause. Cardiovascular death was death from any cardiovascular cause. We also included a separate analysis incorporating the addition of myocardial infarction. In categories where MI was included in the outcome measure, such as “total death + MI” or “CV death + MI,” we counted the first event of an MI (fatal or non-fatal) or a death from any cause or the first event of an MI (fatal or non-fatal) or a death due to some other cardiovascular cause.
Statistical Analysis
All analyses were performed using SAS version 9.1 (SAS institute, Cary, NC). Participant were classified into ER presence (ER+: definite/probable ER) versus no ER presence (ER−). Baseline characteristics were compared by ER status using generalized linear models for continuous variables and chi-square tests for categorical variables, as appropriate. We classified outcomes as total mortality alone, total mortality or myocardial infarction, and cardiovascular mortality, CV mortality or MI. Kaplan-Meier curves were constructed to illustrate the cumulative incidence of event outcomes by ER status. We tested the association of ER and outcomes using Cox proportional hazards regression analysis. All the models were fitted initially unadjusted; adjusted for age alone; sex alone; race alone; age, sex, and race; and a model adjusted for age, sex, race, and clinical covariates. The covariates included factors known to be associated with cardiovascular risk, including systolic blood pressure, BMI, total cholesterol/HDL ratio, current smoker, blood pressure treatment, baseline heart rate, and fitness level. Fitness was defined by exercise duration on a graded exercise treadmill test. For purposes of this analysis, we performed secondary analyses a priori, stratifying participants into “low” and “high” fitness based on the median value. No statistically significant interactions were present. Proportional hazards assumptions were checked and found to be appropriate.
We also performed secondary analyses for the following: 1) total mortality alone with definite ER alone; 2) definite ER and total mortality or cardiovascular mortality separately; 3) “maintainers” of ER (from Y0 to Y7) and total mortality or cardiovascular mortality. A p value < 0.05 (two-tailed) was considered statistically significant.
Results
Study Sample
Baseline characteristics of the study sample, categorized by status of ER (Y0, Y7, Y20) are shown in Table 1. The study sample consisted of 5039 participants at Y0, of whom 941 (18.7%) had definite ER, 314 (6.2%) had probable ER, and 265 (5.2%) had possible ER. Compared with participants without ER at baseline (Y0), participants with definite/probable ER were more likely to be black, male, smoke, have higher SBP, lower heart rate and BMI, total cholesterol, and HDL, and higher physical activity and fitness levels, and longer PR, QRS and QT intervals (all statistically significant). Year 5 echocardiographic LV mass, LVEDD, and LVPWT were also higher in those with baseline ER. The prevalence of definite/probable ER diminishes over time: Y0 (24.8%), Y7 (14.7%), and Y20 (6.6%). Characteristics of participants with and without ER at Y7 and Y20 generally followed similar patterns of association, although risk factor levels and prevalence were higher, as expected. Two exceptions of note include increasing prevalence of black participants in those with ER at Y7 and Y20 and increasing LV mass metrics over time in those without ER versus stable levels of LV mass in those with ER.
Table 1.
Baseline characteristics of the study population by status of early repolarization*
| ER Y0 | ERY7 | ERY20 | ||||
|---|---|---|---|---|---|---|
| Characteristic | No (n=3790) |
Yes (n=1249) |
No (n=3115) |
Yes (n=538) |
No (n=2326) |
Yes (n=165) |
| Age (yrs) | 24.9±3.7 | 24.5±3.6 | 32.1±3.6 | 31.5±3.5 | 45.3±3.6 | 44.9±3.4 |
| Female, % | 69.5 | 8.8 | 62.3 | 7.3 | 59.8 | 13.9 |
| Black, % | 50.0 | 56.5 | 46.0 | 55.8 | 42.9 | 66.7 |
| SBP (mmHg) | 109.2±10.9 | 113.8±10.3 | 108.1±12.2 | 111.8±10.7 | 114.8±14.2 | 118.3±13.9 |
| DBP (mmHg) | 68.3±9.5 | 69.6±9.8 | 69±10 | 70±9.3 | 71.5±11 | 71.7±9.7 |
| Anti-HTN Rx | 2.4 | 1.8 | 1.8 | 0.9 | 16.3 | 12.1 |
| BMI (kg/m2) | 24.7±5.4 | 23.7±3.3 | 27.1±6.3 | 24.8±3.6 | 29.3±7 | 25.9±4.3 |
| Current smoker, % | 28.6 | 35.5 | 25.2 | 34.1 | 16.5 | 25.3 |
| TC (mg/dL) | 177.8±33.5 | 173.5±33.1 | 177.0±33.8 | 175.0±35.11 | 186.9±34 | 178.1±34 |
| HDL (mg/dL) | 53.5±13.3 | 52.1±12.9 | 51.0±114.1 | 51.2±13.7 | 54.7±17 | 55.1±16.4 |
| LDL (mg/dL) | 109.7±31.3 | 106.8±30.9 | 107.9±31.2 | 106.1±33.6 | 110.7±31.7 | 104.8±30.4 |
| †Diabetes (%) | 1.2 | 0.8 | 4.7 | 1.1 | 9.3 | 2.4 |
| FBG | 82.1±16 | 84.1±16.1 | 91.8±18.6 | 92.1±10.4 | 99±25 | 94.5±10.5 |
| Insulin | 11.4±8.4 | 9.4± 6.3 | 14.6±18.1 | 12.2±8 | 16.1±10.5 | 12.5±5.9 |
| Exercise duration (minute) | 9.0± 3.0 | 11.5±2.7 | 8.7±2.9 | 10.9±2.8 | 7.0±2.6 | 8.9±2.6 |
| Physical activity score (Exercise units) | 388.1±285.9 | 516.9±321.9 | 321.8±267.5 | 445.7±277.9 | 341.7±274.6 | 430.4±318.5 |
| HR (bpm) | 64.5±10.6 | 57.7± 9.0 | 65.1±10.7 | 59.2±9.3 | 66±10.1 | 62.2±9.2 |
| PR (msec) | 146.8±22.1 | 152.2±23.6 | 150.1±21.8 | 155.3±25.3 | 158±22.4 | 162.2±23.3 |
| QRS (msec) | 81±7.3 | 86.1± 8.8 | 82.7±7.4 | 87.3±8.7 | 89.2±9.7 | 91.5±8.2 |
| QT (msec) | 385±26.3 | 393.6±26.8 | 385.0±25.4 | 392.3±26.8 | 397.5±30.6 | 399±32 |
| ‡QTindex | 96.2±4.6 | 94.4±4.4 | 96.6±4.3 | 94.9±4.2 | 100.2±4.0 | 98.2±4.1 |
| §Cornell product LVH | 1184±397 | 1165±551 | 1223.4±410 | 1100.3±535 | 1441±505 | 1054±583 |
| ECG LV Mass Index | 32.2±5.5 | 33.4±5 | 34.2±6.0 | 33.6±4.8 | 36.9±9.7 | 33.5±4.7 |
| YR 5 Echo LVEDD (cm) | 4.9±0.48 | 5.1±0.45 | 4.93±0.49 | 5.11±0.46 | -- | -- |
| Yr 5 Echo LVPWT (cm) | 0.83±0.14 | 0.89±0.13 | 0.84±0.14 | 0.88±0.13 | -- | -- |
ER defined as definite or probable by uniform criteria
Abbreviations: SBP = Systolic blood pressure, DBP = diastolic blood pressure, HDL = High density lipoprotein, LDL = Low density lipoprotein, LVH = left ventricular hypertrophy, LVMI = Left ventricular mass index (see below for definition), LVDD = Left ventricular diastolic diameter, FBG = fasting blood glucose, HR = heart rate, BMI = body mass index, HTN Rx = hypertension treatment
Means ± standard deviation unless otherwise indicated
Defined as self-reported “yes” or fasting glucose ≥126 mg/dL
qtdur1* (hr + 100)/656
Cornell voltage (CV) > 2200µV for women; > 2800µV for men
At Y20, characteristics more likely to be associated with definite/probable ER include: male sex, black race, higher SBP less likely to be taking anti-hypertensive treatment, lower BMI, higher HDL, longer exercise duration and higher physical activity score. Higher LV mass was more prevalent in those without than with definite/probable ER at Y20.
Event Rates
The Kaplan-Meier curves for ER+ (definite and probable) and ER− with total mortality and CV mortality are shown in Figures 2a–b. Among 5039 participants eligible for analysis with baseline ECGs, of whom 1249 had Y0 ECG ER+, crude event rates are shown in Table 2. Event rates in 1000 person-years are as follows for the outcomes of interest: 2.59 per 1000 person years for total mortality; 2.91 per 1000 person years for total mortality + MI; 0.83 per 1000 person years for CV mortality; and 1.18 per 1000 person years for CV mortality + MI.
Figure 2.
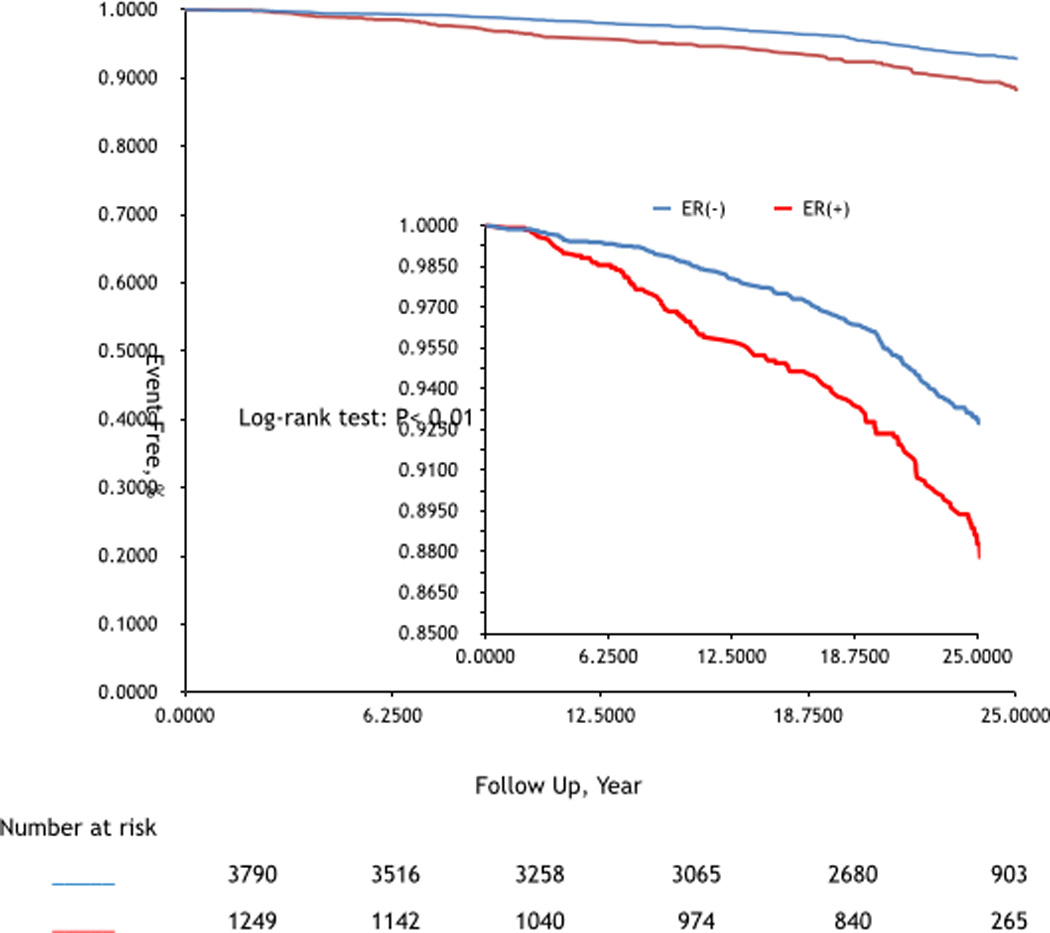
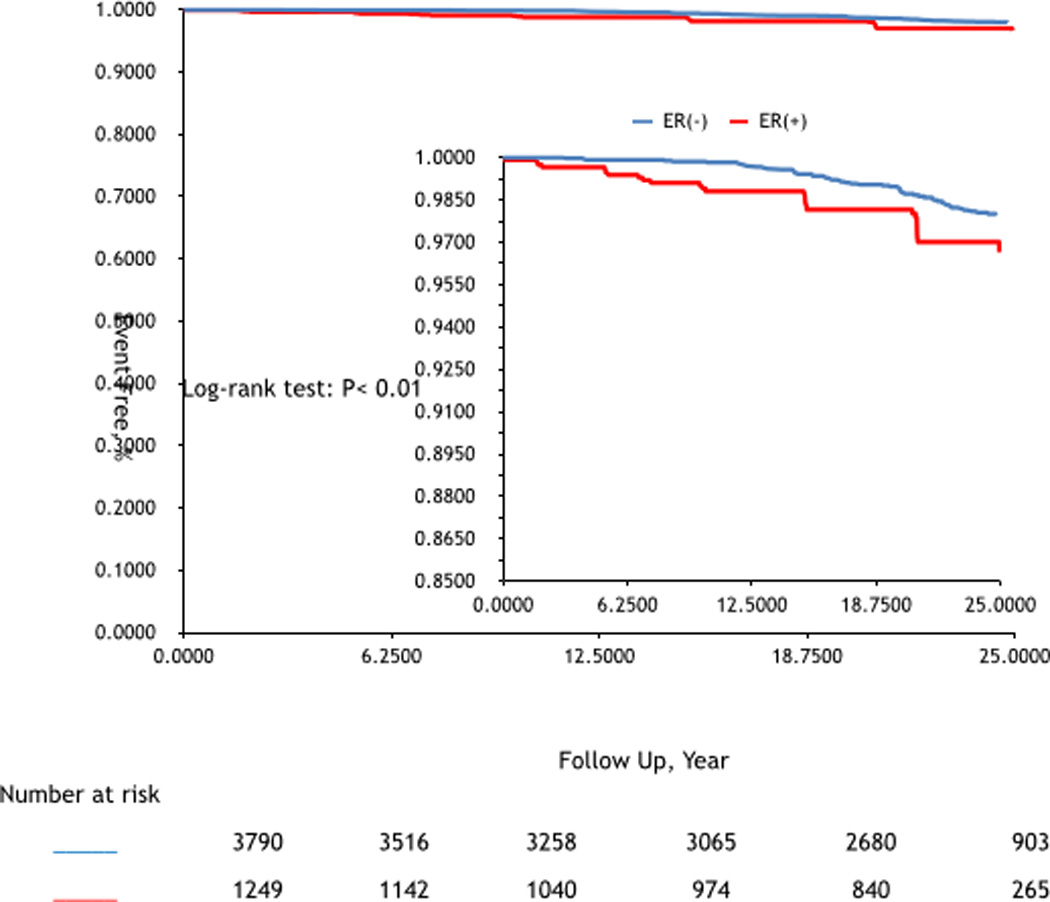
A: Kaplan-Meier estimates of total mortality comparing participants by Y0 ER status. B: Kaplan-Meier estimates of cardiovascular (CV) mortality comparing participants by Y0 ER status.
Table 2.
Association of Definite/Probable †Early Repolarization at Baseline Y0 and Outcome at Year 23, in Unadjusted and Adjusted Models
| Total Death N=262 (event rate 5.2%) |
CV Death N=84 (event rate 1.7%) |
|||
|---|---|---|---|---|
| Models | HR (95% CI) | P | HR (95% CI) | P |
| Unadjusted | 1.77 (1.38–2.28) | <0.01 | 1.59 (1.01–2.50) | 0.04 |
| Low fit# | 2.77 (1.83–4.20) | <0.01 | 2.25 (1.04–4.88) | 0.04 |
| High fit | 1.58 (1.12–2.24) | 0.009 | 1.59 (0.85–2.97) | 0.15 |
| Age adjusted | 1.80 (1.40–2.32) | <0.01 | 1.63 (1.03–2.56) | 0.04 |
| Low fit | 2.80 (1.85–4.24) | <0.01 | 2.27 (1.05–4.92) | 0.04 |
| High fit | 1.61 (1.13–2.28) | 0.008 | 1.64 (0.88–3.09) | 0.12 |
| Sex adjusted | 1.13 (0.85–1.50) | 0.42 | 0.97 (0.59–1.61) | 0.91 |
| Low fit | 1.27 (0.79–2.05) | 0.33 | 0.94 (0.39–2.23) | 0.88 |
| High hit | 1.13 (0.79–1.63) | 0.50 | 1.09 (0.57–2.09) | 0.79 |
| Race adjusted | 1.72 (1.33–2.21) | <0.01 | 1.51 (0.96–2.38) | 0.07 |
| Low fit | 2.65 (1.75–4.04) | <0.01 | 1.87 (0.86–4.06) | 0.11 |
| High fit | 1.32 (0.93–1.88) | 0.12 | 1.29 (0.68–2.45) | 0.43 |
| Age/sex/race adjusted | 1.07 (0.81–1.42) | 0.63 | 0.90 (0.55–1.45) | 0.69 |
| Low fit | 1.22 (0.76–1.98) | 0.41 | 0.79 (0.33–1.87) | 0.58 |
| High fit | 1.07 (0.74–1.53) | 0.73 | 1.04 (0.54–1.99) | 0.91 |
| Full Model | 1.16 (0.85–1.57) | 0.35 | 0.96 (0.56–1.65) | 0.88 |
| Low fit | 1.30 (0.78–2.17) | 0.32 | 0.70 (0.27–1.85) | 0.47 |
| High fit | 1.05 (0.72–1.53) | 0.79 | 1.10 (0.56–2.17) | 0.78 |
ER represents definite or probable early repolarization using uniform criteria
Fitness: low (<50% vs. high >=50%)
Full model adjusted for systolic BP, BMI, TC/HDL ratio, smoker, blood pressure treatment, heart rate at baseline, exercise fitness (low vs. high – see text)
Total Mortality Association with ER
Our models exploring outcomes associated with ER are shown in Table 2. The total death rate (per 1,000 follow-up year) is 3.83 for definite ER, 3.91 for probable ER, 5.3 for possible ER, and 1.9 for no ER. ER was associated with total death, in unadjusted analysis (HR 1.77, 1.38–2.28, p<0.01). When adjusting for age or race alone, the findings remained significant (age: HR 1.80, 1.40–2.32; p<0.01; sex: race: HR 1.72, 1.33–2.21; p<0.01). When adjusting for sex alone, the association between ER and outcome was not statistically significant. However, when adjusting for age, sex, and race, the association between ER and total mortality attenuated substantially to nonsignificance (HR 1.07, 0.81–1.42; p=0.63). Further multivariable adjustment for traditional cardiovascular risk factors yielded similar results for the association between baseline ER and Event 1 (HR 1.16, 0.85–1.57; p=0.35). When we analyzed the outcome of total death or MI with ER, we found a similar pattern of results. Unadjusted HRs for all outcomes were higher for those with lower fitness than those with higher fitness, but adjustment for sex and race attenuated associations of ER with outcomes to nonsignificance in both fitness strata.
CV Mortality Association with ER
ER also was associated with CV death in unadjusted analysis (HR 1.59, 1.01–2.50; p=0.04), as well as after adjustment for age alone (HR 1.63, 1.03–2.56; p=0.04), while adjustment for race (HR 1.51, 0.96–2.38; p=0.07) and sex alone (HR 0.97, 0.59–1.61; p=0.91) yielded no statistically significant association. When further adjustment for age, sex and race was performed, in addition to multivariable adjustment for clinical covariates, findings were sharply attenuated to nonsignificance (Table 2). When we analyzed the outcome of CV mortality or MI with ER, we found a similar pattern of results, but findings remained statistically significant when performing age and race adjustments separately. Unadjusted HRs for all outcomes were higher for those with lower fitness than those with higher fitness, but adjustment for sex and race attenuated associations of ER with outcomes to nonsignificance in both fitness strata.
Outcomes Stratified by Fitness Levels
“Low” fitness levels uniformly were associated with higher hazard ratios across all of our models. ER also was associated with total mortality in unadjusted analysis, stratified by “low” and “high” fitness levels (unadjusted “low”: HR 2.77, 1.83–4.20; p<0.01), compared with “high” fitness levels (unadjusted “high”: HR 1.58, 1.12–2.24; p=0.009). After age, sex, and race adjustment, findings were attenuated to nonsignificance. Our findings were similar when analyzing ER with CV mortality.
Patterns of Association by Sex-Race Groups
We performed sex-race stratified analyses, specifically examining the outcome of Event 1. The association of ER and Event 1 was not significant for any of the subgroups explored except in blacks, although tests for interactions were not significant. Twenty-three year event rates were as follows for ER− vs. ER+: white men: 6.8% vs. 5.8%; white women: 2.8% vs. 0%; black men: 9.8% vs. 11.7%; black women: 4.3% vs. 4.8%. As expected, event rates were higher for men compared with women and for black compared with white participants in our younger adult cohort.
Exploratory Analyses
None of our sensitivity analyses demonstrated a statistically significant association between ER and outcome. We examined associations by ER pattern over time (ER maintainers, losers, gainers, never, from Y0 to Y20) with outcomes. Event rates by ER pattern, respectively, were: 3.1%, 1.4%, 0%, and 1.4% for total mortality, and 1.0%, 0.8%, 0%, and 0.8% for cardiovascular mortality. Event rates were too small by category of ER pattern over time to identify robust associations. We currently do not have the power to answer the question whether ER which is detected at age 25 and persists into middle age is associated with elevated risk.
Discussion
In this large, biracial cohort followed prospectively from young age through middle age, we observed that ER is associated with total and CV mortality in unadjusted analyses. However, after multivariable adjustment, the association of ER and total mortality and cardiovascular mortality was not statistically significant. The associations between ER and our primary outcome measures were largely confounded by sex and race, but no sex-race interactions were noted. Young adult men and blacks had higher prevalence of ER at baseline and over follow-up, and these groups also had higher event rates of our primary outcome measures. However, the presence of ER was not independently associated with adverse outcomes once we adjusted for sex and race. In addition, when we explored outcomes with the pattern of ER over time (e.g., maintenance, loss, gain, or never presence of ER), there were no statistically robust associations.
The vast majority of ER in our study sample regressed by Y20. In the 4.7% of whom “definite ER” remained prevalent at Y20, characteristics associated with predicting maintenance of ER from Y0 to Y20 were black race (OR 2.62, 95% CI 1.61,4.25), BMI (0.62 per 1 standard deviation (SD), (0.40,0.94)), serum triglycerides (0.66 per 1 SD, (0.45,0.98)) and QRS duration (1.68 per 1 SD, (1.37,2.06)) at baseline.4 Importantly, even among this sample of participants who maintained ER over 20 years, the majority of whom were black, there was no increased risk of total mortality or cardiovascular mortality.
Our findings support the hypothesis that the pattern of “definite/probable” ER from young adulthood to middle age is largely a benign phenotype. The observation that black race predominantly attenuates the association between ER and outcomes suggests that this ER phenotype in younger adults and blacks may represent a different phenotype – a more “benign” electrophysiologic entity than that reported by other investigators in those of European descent in middle age.5–6 Furthermore, we found no statistically significant associations between ER and adverse outcomes in those who maintain ER or in those whose ER phenotype regresses, or emerges over time in this cohort.
Perhaps the risk of mortality and sudden death becomes more heightened in those in whom ER persists into middle age, but not for the vast majority of those in whom it is present in young adulthood. Prospective studies exploring the more “ominous” phenotype in young adults appear warranted. Whether it is ER alone, or the presence of ER and subsequent accrual of risk factors or triggers (such as myocardial infarction or structural heart disease) that elevates this risk in middle age requires further study. Recent studies have implicated ER and a trigger (e.g., STEMI) or a fixed substrate (e.g., myocardial scar) as factors that increase the risk of ventricular arrhythmias16–18 in middle-aged and older patients.
Our study is consistent with previous reports on a number of levels. First, prior reports6 have suggested ER may, in fact, be more common in blacks. Second, ER appears to be more common in those with greater exercise duration/fitness.19 Third, certain characteristics appear to be more commonly associated with ER, including lower heart rate, less BMI, and longer PR, QRS and QT intervals. Whether these are characteristics that are noted with cardiovascular fitness and/or greater vagal tone is not well understood, but suggests that certain environmental factors may increase the prevalence of ER. The observation that there is an inverse relationship between advancing age, and ER regression suggests, perhaps, that regression of ER may be related to poor or loss of cardiovascular fitness (as our findings suggest) and, therefore, maintenance of ER over time may imply a heritable component, as described by Noseworthy and colleagues.20
Our findings extend prior observations that young adults, both blacks and whites, followed prospectively from young adulthood into middle age, have a low risk of total and cardiovascular mortality associated with ER. There are several plausible hypotheses for this observation at this time. First, differences in ethnicities or genetic background may explain differences in total and cardiovascular risk in our study compared to those demonstrating a higher risk. Studies in those of European and Asian ancestry have reported heightened risk, while reports in blacks have not. Moreover, several studies7–8 implicating elevated risk of the ER phenotype investigated participants with clinical manifestations which may be consistent with a risk marker of arrhythmia (e.g., syncope, aborted sudden death). Second, ER may be an underlying electrophysiologic substrate, which may require a trigger (e.g., myocardial infarction)16–18 to heighten sudden death risk. As participants live longer and become exposed to greater cardiovascular risk factors, the presence of ER into middle-age, for example, may increase risk of death, as has been reported in several middle-aged population studies. One study21 using J point elevation alone, not early repolarization as defined in our study, suggested that whites were more likely to experience sudden cardiac death. Whether blacks, who typically have a greater burden of cardiovascular risk factors with advancing age, are more likely to experience adverse outcomes in middle age and beyond, bears further investigation in older, multi-racial/ethnic cohorts.
Clinical Implications
While previous studies have suggested that the early repolarization phenotype is benign, recent data suggest that there may be substantial risk with certain ER phenotypes. Therefore, the clinician is faced with uncertainty about the consequences of this phenotype in young age. Using a visually confirmed definition of early repolarization commonly employed in clinical practice, our study found that the vast majority of participants in the CARDIA study do not have a heightened risk of adverse outcomes, whether the participant maintains or loses the phenotype, to middle age. We acknowledge that it is possible that we have not yet followed our study population long enough to manifest a heightened risk. At this time, while it is unreasonable to expect clinical practice to change, those who “maintain” the ER phenotype into middle and older age years may benefit from ECG monitoring until further studies explore the associations of ER and adverse outcomes in these middle age and older patient groups.
Strengths and Limitations
Strengths of our study include its prospective nature, uniform definition of ER, phenotypic characterization, biracial study population, and a high retention rate for outcomes ascertainment. This is the largest prospective study to date of a young biracial cohort with early repolarization and outcomes that uses serial ECG assessment. Given that early repolarization may “disappear,” “emerge,” or be “maintained” over time allows us an opportunity to analyze outcomes associated with the natural history of ER in this unique cohort.
Limitations of our study include the different definition used by EPICARE compared with prior published reports. One such difference is the absence of inferior lead characterization of early repolarization for “definite” or “probable” ER, which has been reported to be an important regional risk marker of ER, particularly in those who suffer SCD. However, the prevalence of inferior lead ER pattern has been reported to be low in middle age (3.8%) and younger (2.5%) study populations; therefore, its prognostic significance for this study population overall is likely limited but unknown. In addition, the purpose of our study was not to apply the more uncommon phenotype of ER to the CARDIA cohort, but to utilize the more common ER phenotype seen in clinical practice to understand prospective risk. Because we cannot specify risk based specifically on regionality of ECG lead placement in our study, it is unknown whether even a small prevalence of ER in the inferior leads may have altered our findings. Our differing definition from that reported by Haissaguerre, Tikkanen and Rosso may explain differences in outcomes noted between studies and may limit the external validity of our sample to the SCD population of interest. A limitation of our paper may be that we have preselected an ER phenotype that may represent a benign phenotype. What is not known, however, is whether this phenotype increases the risk of death in middle-age subjects who are exposed to a potential trigger (e.g., MI). Further studies are needed to better define these prospective associations. Nonetheless, our analysis remains clinically important and generalizable to the everyday clinician, as the proposed definition in this manuscript is the commonly accepted electrocardiographic syndrome of ER.
Supplementary Material
Acknowledgments
Funding Sources: Work on this manuscript was supported (or partially supported) by contracts: University of Alabama at Birmingham, Coordinating Center, N01-HC-95095; University of Alabama at Birmingham, Field Center, N01-HC-48047; University of Minnesota, Field Center and Diet Reading Center (Year 20 Exam), N01-HC-48048; Northwestern University, Field Center, N01-HC-48049; and Kaiser Foundation Research Institute, N01-HC-48050; from the National Heart, Lung and Blood Institute. Also supported by RO1 HL086792-01; Donald M. Lloyd-Jones, MD, ScM.
Footnotes
Conflict of Interest Disclosures: None.
References
- 1.Sutherland SE, Gazes PC, Keil JE, Gilbert GE, Knapp RG. Electrocardiographic abnormalities and 30-year mortality among white and black men of the Charleston Heart Study. Circulation. 1993;88:2685–2692. doi: 10.1161/01.cir.88.6.2685. [DOI] [PubMed] [Google Scholar]
- 2.Machado DB, Crow RS, Boland LL, Hannan PJ, Taylor HA, Jr, Folsom AR. Electrocardiographic findings and incident coronary heart disease among participants in the Atherosclerosis Risk in Communities (ARIC) study. Am J Cardiol. 2006;97:1176–1181. doi: 10.1016/j.amjcard.2005.11.036. [DOI] [PubMed] [Google Scholar]
- 3.Klatsky AL, Oehm R, Cooper RA, Udaltsova N, Armstrong MA. The early repolarization normal variant electrocardiogram: correlates and consequences. Am J Med. 2003;115:171–177. doi: 10.1016/s0002-9343(03)00355-3. [DOI] [PubMed] [Google Scholar]
- 4.Walsh JA, Ilkhanoff L, Soliman EZ, Prineas R, Liu K, Ning H, Lloyd-Jones DM. Natural history of early repolarization syndrome: Coronary Artery Risk Development in Young Adults (CARDIA) study. J Am Coll Cardiol. 2013;61:863–869. doi: 10.1016/j.jacc.2012.11.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Uberoi A, Jain NA, Perez M, Weinkopff A, Ashley E, Hadley D, Turakhia MP, Froelicher V. Early repolarization in an ambulatory clinical population. Circulation. 2011;124:2208–2214. doi: 10.1161/CIRCULATIONAHA.111.047191. [DOI] [PubMed] [Google Scholar]
- 6.Perez MV, Uberoi A, Jain NA, Ashley E, Turakhia MP, Froelicher V. The prognostic value of early repolarization with ST-segment elevation in African Americans. Heart Rhythm. 2012;9:558–565. doi: 10.1016/j.hrthm.2011.11.020. [DOI] [PubMed] [Google Scholar]
- 7.Haissaguerre M, Derval N, Sacher F, Jesel L, Deisenhofer I, de Roy L, Pasquie JL, Nogami A, Babuty D, Yli-Mayry S, De Chillou C, Scanu P, Mabo P, Matsuo S, Probst V, Le Scouarnec S, Defaye P, Schlaepfer J, Rostock T, Lacroix D, Lamaison D, Lavergne T, Aizawa Y, Englund A, Anselme F, O'Neill M, Hocini M, Lim KT, Knecht S, Veenhuyzen GD, Bordachar P, Chauvin M, Jais P, Coureau G, Chene G, Klein GJ, Clementy J. Sudden cardiac arrest associated with early repolarization. N Engl J Med. 2008;358:2016–2023. doi: 10.1056/NEJMoa071968. [DOI] [PubMed] [Google Scholar]
- 8.Rosso R, Kogan E, Belhassen B, Rozovski U, Scheinman MM, Zeltser D, Halkin A, Steinvil A, Heller K, Glikson M, Katz A, Viskin S. J-Point Elevation in Survivors of Primary Ventricular Fibrillation and Matched Control Subjects: Incidence and Clinical Significance. J Am Coll Cardiol. 2008;52:1231–1238. doi: 10.1016/j.jacc.2008.07.010. [DOI] [PubMed] [Google Scholar]
- 9.Tikkanen JT, Anttonen O, Junttila MJ, Aro AL, Kerola T, Rissanen HA, Reunanen A, Huikuri HV. Long-term outcome associated with early repolarization on electrocardiography. N Engl J Med. 2009;361:2529–2537. doi: 10.1056/NEJMoa0907589. [DOI] [PubMed] [Google Scholar]
- 10.Haruta K, Matsuo K, Tsuneto A, Ichimaru S, Hida S, Sera N, Imaizumi M, Nakashima E, Maemura K, Akahoshi M. Incidence and prognostic value of early repolarization pattern in the 12-lead electrocardiogram. Circulation. 2011;123:2931–2937. doi: 10.1161/CIRCULATIONAHA.110.006460. [DOI] [PubMed] [Google Scholar]
- 11.Friedman GD, Cutter GR, Donahue RP, Hughes GH, Hulley SB, Jacobs DRJ, Liu K, Savage PJ. CARDIA: study design, recruitment, and some characteristics of the examined subjects. J Clin Epidemiol. 1988;41:1105–1116. doi: 10.1016/0895-4356(88)90080-7. [DOI] [PubMed] [Google Scholar]
- 12.Rautaharju P, Wolf HK, Eifler WJ, Blackburn H. A simple procedure for positioning precordial ECG and VCG electrodes using an electrode locator. J Electrocardiol. 1976;9:35–40. doi: 10.1016/s0022-0736(76)80007-6. [DOI] [PubMed] [Google Scholar]
- 13.Prineas RJ, Crow RS, Blackburn H. The Minnesota Code Manual of Electrocardiographic Findings: Standards and Procedures for Measurement and Classification. Boston, MA: John Wright - PSG, Inc.; 1982. [Google Scholar]
- 14.Soliman EZ, Elsalam MA, Li Y. Early repolarization and markers of ventricular arrhythmogenesis in patients referred to ambulatory 24-hour ECG recording. Int J Cardiol. 2012;160:175–180. doi: 10.1016/j.ijcard.2011.04.005. [DOI] [PubMed] [Google Scholar]
- 15.Bibbins-Domingo K, Pletcher MJ, Lin F, Vittinghoff E, Gardin JM, Arynchyn A, Lewis CE, Williams OD, Hulley SB. Racial differences in incident heart failure among young adults. N Engl J Med. 2009;360:1179–1190. doi: 10.1056/NEJMoa0807265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Patel RB, Ng J, Reddy V, Chokshi M, Parikh K, Subacius H, Alsheikh-Ali AA, Nguyen T, Link MS, Goldberger JJ, Ilkhanoff L, Kadish AH. Early repolarization associated with ventricular arrhythmias in patients with chronic coronary artery disease. Circ Arrhythm Electrophysiol. 2010;3:489–495. doi: 10.1161/CIRCEP.109.921130. [DOI] [PubMed] [Google Scholar]
- 17.Naruse Y, Tada H, Harimura Y, Hayashi M, Noguchi Y, Sato A, Yoshida K, Sekiguchi Y, Aonuma K. Early repolarization is an independent predictor of occurrences of ventricular fibrillation in the very early phase of acute myocardial infarction. Circ Arrhythm Electrophysiol. 2012;5:506–513. doi: 10.1161/CIRCEP.111.966952. [DOI] [PubMed] [Google Scholar]
- 18.Patel RB, Ilkhanoff L, Ng J, Chokshi M, Mouchli A, Chacko SJ, Subacius H, Bhojraj S, Goldberger JJ, Kadish AH. Clinical characteristics and prevalence of early repolarization associated with ventricular arrhythmias following acute ST-elevation myocardial infarction. Am J Cardiol. 2012;110:615–620. doi: 10.1016/j.amjcard.2012.04.042. [DOI] [PubMed] [Google Scholar]
- 19.Noseworthy PA, Weiner R, Kim J, Keelara V, Wang F, Berkstresser B, Wood MJ, Wang TJ, Picard MH, Hutter AM, Jr, Newton-Cheh C, Baggish AL. Early repolarization pattern in competitive athletes: clinical correlates and the effects of exercise training. Circ Arrhythm Electrophysiol. 2011;4:432–440. doi: 10.1161/CIRCEP.111.962852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Noseworthy PA, Tikkanen JT, Porthan K, Oikarinen L, Pietila A, Harald K, Peloso GM, Merchant FM, Jula A, Vaananen H, Hwang SJ, O’Donnell CJ, Salomaa V, Newton-Cheh C, Huikuri HV. The early repolarization pattern in the general population: clinical correlates and heritability. J Am Coll Cardiol. 2011;57:2284–2289. doi: 10.1016/j.jacc.2011.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Olson KA, Viera AJ, Soliman EZ, Crow RS, Rosamond WD. Long-term prognosis associated with J-point elevation in a large middle-aged biracial cohort: the ARIC study. Eur Heart J. 2011;32:3098–3106. doi: 10.1093/eurheartj/ehr264. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


