Abstract
In 2001, Afghanistan's Ministry of Public Health inherited a devastated health system and some of the worst health statistics in the world. The health system was rebuilt based on the Basic Package of Health Services (BPHS). This paper examines why the BPHS was needed, how it was developed, its content and the changes resulting from the rebuilding. The methods used for assessing change were to review health outcome and health system indicator changes from 2004 to 2011 structured along World Health Organisation's six building blocks of health system strengthening. BPHS implementation contributed to success in improving health status by translating policy and strategy into practical interventions, focusing health services on priority health problems, clearly defining the services to be delivered at different service levels and helped the Ministry to exert its stewardship role. BPHS was expanded nationwide by contracting out its provision of services to non-governmental organisations. As a result, access to and utilisation of primary health care services in rural areas increased dramatically because the number of BPHS facilities more than doubled; access for women to basic health care improved; more deliveries were attended by skilled personnel; supply of essential medicines increased; and the health information system became more functional.
Keywords: Basic Package of Health Services, contracting out, non-governmental organisations, health systems strengthening, Afghanistan
Introduction
After the collapse of the Taliban in 2001, the Ministry of Public Health (MOPH) of the new Afghan Interim Authority faced the challenging task of addressing some of the world's worst health indicators in a country with a devastated health system. Three indicators illustrate the dire health status of the country's population. The maternal mortality ratio, estimated at 1600 per 100,000 live births, was the highest ever recorded (Bartlett et al., 2005). The infant and child mortality rates, 165 and 257 per 1000 live births, respectively, both ranked as the fourth highest in the world in 2002. And access to health services, defined as living within one hour walking of a health facility, in 2001 was limited to less than 10% of the population (Ministry of Public Health, 2008).
The situation of the health system was not unique: ‘health systems in countries emerging from conflict are often characterized by damaged infrastructure, limited human resources, weak stewardship and proliferation of non-government organizations’ (Roberts, Guy, Sondorp, & Lee-Jones, 2008). But the way in which the situation improved in the period 2003–2011 in Afghanistan is exemplary. Several factors contributed to the relative success of rebuilding the health system in Afghanistan, and this paper focuses on one major factor: the development and implementation of the Basic Package of Health Services (BPHS).
Why the BPHS was needed
The public-sector health system was largely dysfunctional, with services delivered by a multitude of national and international non-governmental organisations (NGOs), often focused on their own areas of interest. Clinics, qualified health personnel, and other health resources were insufficient in number and maldistributed (Ministry of Health, 2002). But the desire of the MOPH to prioritise underserved rural areas was not shared in the Cabinet, which expressed more interest in strengthening the curative sector, particularly the national hospitals. International agencies, which had kept vertical initiatives going, were also reluctant to consider other delivery mechanisms.
At the same time, many donors were interested in strengthening the health system and willing to coordinate and provide considerable funding – although not enough to address all health needs. Stakeholders nonetheless recognised the need for policies and strategies to maximise the benefits for the largest number of beneficiaries, including a priority-setting mechanism. The high mortality of women and children needed to be addressed urgently, and both the causes of that mortality and the health interventions to alleviate it had been documented (Bobadilla, Cowley, Musgrove, & Saxenian, 1994).
The concept of using a package of essential health services to tackle the most urgent health problems while rebuilding the health system was not new (Bobadilla et al., 1994); it had been used in other countries like Bosnia and Herzegovina (Hrabaè, Ljubiæ, & Bagariæ, 2000), Cambodia (Hilla & Eangb, 2007), Rwanda (Ministry of Health [Rwanda], National Population Office [Rwanda], & ORC Macro, 2003) and Uganda (Ministry of Health, 2000). The BPHS provided a package adapted to Afghanistan and based on the available evidence promised to become a powerful tool to help to focus all stakeholders on the MOPH's priorities (Belay 2010; Health and Fragile States Network 2009).
How the BPHS was developed
Parameters for development of the BPHS
The World Health Organisation (WHO) led the initial drafting of an essential package of health interventions with limited input from the MOPH and little information about the country. The resulting document contained little indication of priorities or how to implement the recommended services. The major donors – the European Community, US Agency for International Development (USAID) and World Bank – communicated the need for and cited examples of a well-defined and integrated health service package. In response, the MOPH asked a Health Coordination Taskforce to design one. The taskforce faced the challenge of limited availability of national expertise, but could benefit from donor-funded international advisors.
Despite the lack of up-to-date epidemiological information and of baseline data to measure impact, the members of the taskforce knew that women and children were the most vulnerable groups, prone to diseases that are largely preventable and easily treated (Ickx, 2002; Salama, 2003; Waldman & Hanif, 2002). For children, those are the vaccine-preventable diseases, acute respiratory infections and diarrheal diseases. For women, problems related to pregnancy and childbirth take a heavy toll. Chronic malnutrition and micronutrient deficiencies lead to or exacerbate health problems in both groups.
In addition to deciding what health problems to address, the MOPH needed information about the type, location, condition and number of health facilities; health services offered; equipment and drugs available; and number of health workers. To obtain this information, a joint inventory of every health facility, the Afghanistan National Health Resources Assessment (ANHRA), was undertaken. The survey confirmed that about 80% of service delivery was provided by NGOs and identified huge gaps in critical services, and inequity in distribution of services (Ministry of Health, 2002).
In 2002, most MOPH leaders lacked public health experience. This became a major challenge when they evaluated what health services to provide with limited resources, how to address the pressure of the medical establishment to invest in hospital-based curative services and how to deal with offers of donations that would benefit only a small number of people while burdening the Government of Afghanistan with high operating costs. The Ministry developed a framework to guide its decisions about health services and facilities, policies and offers of assistance so that it could plan how to use its resources and those of donors to benefit the most people and be sustainable: the Public-Health Decision Tool.
The Public-Health Decision Tool helped the MOPH achieve four key goals: (1) assisting policy-makers to select health priorities, (2) establishing criteria for making choices about interventions, (3) ensuring that the choices about health services to be delivered were consistent with national health objectives and (4) maintaining MOPH priorities over time (Ministry of Health, 2003; Ministry of Public Health, 2005a). The decision framework consists of four questions:
-
(1)
Effectiveness: does the intervention have proven effectiveness for diseases or conditions that impose a heavy disease burden on Afghanistan?
-
(2)
Scaling up: can the intervention be implemented on a national scale and benefit a large part of the population?
-
(3)
Equity: is the intervention fair in who will have access to and benefit from it?
-
(4)
Sustainability: is the intervention affordable now and for the long term?
Content of the BPHS
The MOPH agreed that the BPHS would be reviewed within two years to adjust the content of the package based on its effectiveness in addressing health needs. The package had seven components: maternal and newborn health, child health and immunisation, nutrition, control of communicable diseases, mental health, disability and provision of essential drugs (Figure 1; Ministry of Health, 2003). Mental health and disability became second tier components, only implemented where financial and human resources permitted.
Figure 1.
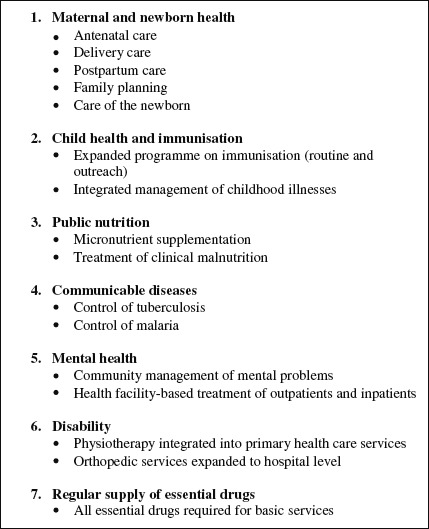
Components of Afghanistan's Basic Package of Health Services 2003.
Source: Ministry of Health (2003): A Basic Package of Health Services for Afghanistan, 2003/1382. Kabul: MOH, Islamic Republic of Afghanistan; 2003.
The BPHS defined each type of health facility in the primary care system – health post, basic health centre, comprehensive health centre and district hospital – and the size of its catchment population. It also clearly linked specific health services to each type of facility and defined the corresponding types and number of staff needed, equipment required and essential drugs necessary for the services provided.
The BPHS and contracting for service delivery
The development of a mechanism whereby the MOPH would contract with NGOs to provide the BPHS services paralleled – even drove – the development of the BPHS. In the government, some felt that health service delivery was a function of the state and distrusted the private sector. NGOs providing health services had concerns about being entangled with the government and losing their independence. Donors wanted to support the MOPH's autonomy but recognised its very limited capacity for direct service delivery and provided examples of public–private partnerships from abroad, which convinced the MOPH to consider using NGOs for provision of BPHS services.
The agreed-on approach was that the MOPH would contract with well- established NGOs to deliver the BPHS in a defined geographic area, such as a province or group of districts. The Ministry was involved in selecting the NGOs through a competitive bid process, managing the contracts and monitoring and evaluating performance. The contracts ranged from 12 to 36 months. NGOs were paid according to budgets that they submitted as part of their bids; full payment depended on achievement of agreed-on goals. There were differences among the three major donors in how NGOs were contracted (Loevinsohn & Sayed 2008; Palmer, Strong, Wali, & Sondorp, 2006; Waldman, Strong, & Wali, 2006) and one donor experimented with ‘contracting in’ three provincial health directorates. The donors' varied internal audit requirements prevented taking a single approach to contracting. The institutionalisation of a Grants and Contracts Management Unit within the MOPH, which included recruitment of knowledgeable former NGO staff, allowed the Ministry to lead the planning and implementation of primary health services.
A complementary important development for BPHS was the commitment of the three major health donors to fund the BPHS in a set number of provinces so that all provinces of the country were covered. These three donors agreed to fund the BPHS based on initial estimates that it could be provided for US$4.55 per capita (Newbrander, Yoder, & Bilby, 2007). Recent experience showed the per capita costs of provision of BPHS ranged from $4.30 to $5.12 (Newbrander et al., 2007). Thus the cost of providing the BPHS compares similarly with experiences of other low-income countries (Loevinsohn & Harding, 2005).
Strategies that bolstered the BPHS
Focusing on community-based health care, through health posts served by community health workers (CHWs), was a major strategy to increase access to services. This community component was essential for targeting underserved areas in a country where over 80% of the population lived in rural areas in 2001. Even non-literate CHWs, male and female, in remote communities can treat childhood health problems and communicable diseases such as malaria. They provide basic reproductive health services for women, including counselling pregnant women to seek trained birth attendants.
Donors and the MOPH agreed on the importance of monitoring and evaluating the delivery of the BPHS. The health management information system (HMIS) was revised to provide routine service statistics. A separately contracted third party annually evaluated 29 key performance indicators, in a Balanced Scorecard (BSC), to assess progress in BPHS implementation (Edward et al., 2011). The Ministry used the information to plan, manage and monitor the health system and determine when corrective action was needed.
The ANHRA identified the dearth of qualified female staff in health facilities in 2002. Several NGOs had started community-midwife training, where communities were encouraged to select community midwives, who were deployed in clinics in their villages, making delivery care by a skilled birth attendant available outside hospitals throughout the country. Although encouraging the initiative, it took the MOPH until 2005 to get official endorsement of the National Midwife Education and Accreditation, thus allowing the expansion of this training into a nationwide programme (Ministry of Public Health, 2005a).
Evolution of the BPHS
Three significant changes have taken place since the BPHS was introduced. In 2005, the MOPH revised the package by eliminating the two tiers: mental health services (Ventevogel et al., 2012) and services for those with disabilities were elevated to be equal with the other five elements of the BPHS. The Ministry also added HIV control and incorporated two principles from its health financing strategy: everyone who needs care must receive it, regardless of ability to pay, and the quality of care provided must be the same for paying and non-paying patients.
A second major change also occurred in 2005: the development of the MOPH's Essential Package of Hospital Services (EPHS; Ministry of Public Health, 2005b). The EPHS complemented the BPHS by specifying the in-patient clinical and ancillary services and defining staffing, equipment and drugs for the three types of hospitals: district, provincial and national. The link between the BPHS and EPHS health services is the district hospital, which serves as the first referral-level hospital for primary care facilities. With the two packages, the MOPH specified all the services, staffing and equipment expected at every level of the Afghan health system.
In 2010, the MOPH undertook a third, more significant revision of the BPHS, which expanded services at each level of health facility and formulated more detailed recommendations about how to implement priority interventions at different levels. Some people were concerned that the amended BPHS might become a comprehensive package of services, rather than a basic package, without regard for the burden of disease. Other critics called for a cost–benefit analysis for each new service recommended. In the end, the MOPH added services on a trial basis, in areas where sufficient funding was available. The Ministry also required reporting about the efficiency of implementation strategies, to guide future decisions about national implementation.
Methods
This paper does not attempt to establish a causal relationship between the introduction of the BPHS and changes in the health status of the population. Instead, it examines changes in health outcomes after introduction of the BPHS in each of six building blocks of health system strengthening established by WHO (Unpublished World Health Organization, 2007). Widely accepted as a comprehensive description of the health system, they offer a good structure for systematically reviewing the changes made. The six building blocks are:
-
(1)
service delivery
-
(2)
health workforce
-
(3)
information
-
(4)
medical products, vaccines, and technologies
-
(5)
financing
-
(6)
leadership and governance
In addition to health outcomes, health system indicators can also reflect how easy it is to obtain services and how gender-sensitive they are. The areas we measured and the rationale for including them are explained below.
Service delivery
Assessing the availability of services is a function of the number and types of health facilities, on one hand, and actual utilisation, on the other. Hence we used the following indicators:
number of active health facilities (health sub-centres, basic health centres, comprehensive health centres and district hospitals)
number of active health posts (community-level care)
total patient visits per month (health facilities and health posts)
average number of people receiving health services daily through clinics and direct outreach workers per health facility.
We selected the following measures of priority interventions to reduce maternal and child mortality and morbidity:
maternal mortality ratio
total deliveries at health facilities
women of childbearing age receiving a second dose of tetanus toxoid (TT2)
under-five mortality rate
infant mortality rate
children under one year of age receiving a third dose of diptheria, pertussis and tetanus (DPT) or Pentavalent vaccine (Penta3).
The best available information on communicable diseases is the number of health facilities that can diagnose and treat people with tuberculosis (TB). The indicator is: health facilities providing Directly Observed Treatment, Short Course (DOTS) services.
Health workforce
Cultural factors prevent women from being seen by a male health worker in several areas of Afghanistan. Hence, the number of female health workers is critical to make health services accessible to women. We used the following data to examine this aspect of the health workforce:
number of active female CHWs
female CHWs as a percentage of total CHWs
percentage of BPHS and EPHS facilities with at least one female health worker.
Since a major means of reducing maternal mortality is to increase the number of births attended by skilled birth attendants, we also measured midwives per 10,000 population.
Information
Availability of key health management information is crucial to a well-functioning health system. One aspect of a good HMIS is the percentage of service delivery points regularly submitting information. The indicator we used is: percentage of BPHS facilities reporting information.
Medical products, vaccines and technologies
Even with increased access to health services, essential medicines and supplies must be available when patients are seen. The data we examined are:
percentage of BPHS facilities with at least one essential drug stock-out
annual expenditure for drugs and contraceptives in 13 provinces.
Financing
Sufficient and regular financing is necessary for a health system to perform well. The extent to which a country commits its own resources to health reflects the priority of health, so we looked at the proportion of the total development resources expended by the Afghan Government for health. Using the national health accounts assessment conducted in 2010 (Ministry of Public Health, 2011), we examined:
health expenditure as a percentage of the gross domestic product
the national development budget devoted to health
contributions of donors to the health sector compared to the government's annual expenditure on health.
Leadership and governance
Governance is the ability of the health system to respond to the needs of different population groups at various levels of the health system. We measured leadership and governance with several proxy measures:
Central: coordination mechanisms for the MOPH and its partners
Provincial: submission rate for minutes of meetings of Provincial Health Coordinating Committees
Community: number of Family Health Action Groups established and number of health shura meetings held. At the community level, community shuras (committees) provide leadership and support to all health-related activities in the community. The shuras select, support and supervise the CHWs in the community; encourage families to use preventive health services; and provide leadership in promoting new behaviours, such as use of contraception. The emergence of Family Health Action Groups, collaborating with the CHWs, has also been important in shaping health actions and interventions at the local level in Afghanistan.
Data sources
The data for this review come from a variety of sources. Since the HMIS is a regular, national reporting system and was initiated early in the rebuilding of the health system, it is the preferred source when data are available. Data from the BSC were used to complement HMIS data in several instances. Both sources have data, which were obtained over a period of time, so it is possible to analyse trends. We also used additional data from surveys and special studies.
Mortality figures came from the 2002 reproductive-age mortality studies (RAMOS I; Bartlett et al., 2005) for maternal mortality, and from the 2006 Afghan Household Survey (AHS; Ministry of Public Health, Johns Hopkins University, & Indian Institute of Health Management Research, 2006) the 2010 Afghan Mortality Survey (AMS; Afghan Public Health Institute Ministry of Public Health, Central Statistics Organization, ICF Macro, Indian Institute of Health Management Research, & WHO Regional Office for the Eastern Mediterranean, 2011) for infant and child mortality. All three surveys indicate limits to their representativeness. We have taken into account, when comparing the mortality ratios and rates in the three surveys, that they used different methodologies, had different sample sizes and covered different portions of the country. Nonetheless, they provided the national data for policy and planning decisions.
For instance, the RAMOS I in 2002 covered only four districts in four provinces, representing only 4% of the population (Bartlett et al., 2005). Since no other data were available at that time, the oft-cited national 2002 estimates for maternal mortality were derived from this small sample. The 2010 AMS is the first comprehensive national mortality survey in Afghanistan and the first to provide direct estimates (Afghan Public Health Institute Ministry of Public Health et al., 2011). The survey covered all 34 provinces and represented 87% of the population. RAMOS I and AMS also use a different definition for pregnancy-related deaths, further inspiring caution when comparing maternal mortality rates.
While the 2006 AHS (Ministry of Public Health et al., 2006), which served as the basis for infant mortality and child mortality rate estimates cited by the MOPH, had a larger sample (8278 households) than the RAMOS I, the number of households surveyed was only one-third of the number surveyed by the AMS in 2010 (22,897), and AHS surveyed only rural areas. Furthermore, due to security issues, the 2006 survey excluded five provinces, so it represented only 72% of the rural population of Afghanistan.
Results
The data show significant gains in the rebuilt and strengthened Afghan health system, when we examine all its components.
Service delivery
The total number of active BPHS facilities increased from 1075 in 2004 to 1829 in 2011 – a 70% increase. The BPHS facilities regularly reporting increased more than fourfold, from 392 to 1689. The average number of rural population per active BPHS facility decreased from 15,175 to 10,849. The number of reported active health posts increased from 631 to 12,213 in the same period; part of which is due to the increase in number of reporting facilities, but after correction this would still indicate a more than fourfold increase in health posts. Table 1 shows the trends by year. All numbers suggest increased access of the population to the services provided by BPHS facilities and health posts.
Table 1.
Access: Active health facilities and health posts and rural and total population per BPHS facility, 2004–2011.
| 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | Change factor 2004–2011 from 2004 baseline | |
|---|---|---|---|---|---|---|---|---|---|
| Active BPHS health facilities registereda | 1075 | 1178 | 1132 | 1200 | 1493 | 1687 | 1837 | 1829 | 1.70 |
| Per cent change year-to-year | 10 | −4 | 6 | 24 | 13 | 9 | 0 | ||
| Active BPHS health facilities reportinga (percentage of registered facilities reporting) | 392 (36) | 828 (70) | 986 (87) | 1079 (90) | 1326 (89) | 1511 (90) | 1671 (91) | 1689 (92) | 4.31 |
| Per cent change year-to-year health facilities reporting | 111 | 19 | 9 | 23 | 14 | 11 | 1 | ||
| Active health posts reporting | 631 | 4818 | 7116 | 9702 | 10,922 | 11,147 | 11,426 | 12,213 | 18.35 |
| Per cent change year-to-year | 664 | 48 | 36 | 13 | 2 | 3 | 7 | ||
| Rural population per BPHS facility | 15,175 | 14,247 | 15,245 | 14,789 | 12,223 | 11,124 | 10,505 | 10,849 | 0.71 |
| Total population per BPHS facility | 19,157 | 17,985 | 19,254 | 18,677 | 15,437 | 14,049 | 13,267 | 13,702 | 0.72 |
| Total population | 20,593,695 | 21,186,183 | 21,795,718 | 22,412,820 | 23,047,394 | 23,699,935 | 24,370,952 | 25,060,917 | 1.22 |
Source: MOPH, various HMIS reports, 2004–2011.
Health facilities include health sub-centres, basic health centres, comprehensive health centres and district hospitals.
Increased access does not automatically translate into increased utilisation, however. Yet the absolute number of patient visits in the BPHS system increased from 2.0 million to 44.8 million per year, more than one would expect based on the increase in population and service delivery points only. The increase in the average number of new patient visits per month from 435 to 2209 per facility suggests strongly increased use of services. This trend is confirmed by BSC results showing that the percentage of BPHS facilities seeing more than 750 new patients a month increased from 22% in 2004 to 85% in 2008 (Edward et al., 2011; Table 2).
Table 2.
Utilisation: Patient visits and services at health posts and health facilities, 2004–2011.
| 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | Change factor 2004–2011 from 2004 baseline | |
|---|---|---|---|---|---|---|---|---|---|
| Total patient visits to health posts and health facilities | 2,046,038 | 9,310,085 | 16,446,547 | 21,355,120 | 29,670,418 | 36,972,745 | 40,365,444 | 44,773,537 | 21.88 |
| Average number of patients receiving health services daily at clinics and outreach services | 6537 | 29,745 | 52,545 | 68,227 | 94,794 | 118,124 | 128,963 | 143,046 | 21.88 |
| Per cent change year-to-year | 355 | 77 | 30 | 39 | 25 | 9 | 11 | ||
| Average number of patient visits per health facility per month | 435 | 937 | 1390 | 1649 | 1865 | 2039 | 2013 | 2209 | 5.08 |
| Per cent change year-to-year | 115 | 48 | 19 | 13 | 9 | −1 | 10 |
Source: MOPH, various HMIS reports, 2004–2011.
In the priority area of maternal-child health, Table 3 shows that the number of attended births increased over 4000% in seven years and that the number of deliveries per BPHS facility per month increased by a factor higher than the average increase in patient visits, while the number of women receiving two doses of tetanus toxoid increased similar to the number of patient visits. Table 4 shows that the number of children under age one who receive the third dose of Pentavalent vaccine (Penta3) also increased over these years, but by a smaller factor.
Table 3.
Maternal mortality, 2002 and 2010, and utilisation of maternal health services, 2004–2011.
| 2002 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | Change factor 2004–2011 from 2004 baseline | |
|---|---|---|---|---|---|---|---|---|---|---|
| Maternal mortality ratio, national (maternal deaths per 100,000 live births) | 1600 | 327 | ||||||||
| Total deliveries at health facilities | 10,580 | 44,576 | 100,661 | 193,967 | 294,288 | 330,137 | 369,710 | 441,683 | 41.75 | |
| Per cent change year-to-year | 321 | 126 | 93 | 52 | 12 | 12 | 20 | |||
| Women of childbearing age receiving TT2 | 58,341 | 326,300 | 601,882 | 747,096 | 863,723 | 908,578 | 1,015,073 | 1,460,728 | 25.04 | |
| Per cent change year-to-year | 459 | 85 | 24 | 16 | 5 | 12 | 44 |
Source: MOPH, various HMIS reports, 2004–11; Bartlett et al., 2005; Afghan Public Health Institute Ministry of Public Health et al., 2011.
Table 4.
Infant and child mortality, 2002, 2006 and 2010, and utilisation of child health services, 2004–2011.
| 2002 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | Change factor 2004–2011 from 2004 baseline | |
|---|---|---|---|---|---|---|---|---|---|---|
| Infant mortality rate, national (deaths per 1000 live births) | 165 | 129 | 77 | |||||||
| Under-five mortality rate, national (deaths per 1000 live births) | 257 | 191 | 97 | |||||||
| Children <1 year of age receiving Penta3 vaccine | 77,366 | 415,251 | 631,944 | 726,855 | 898,861 | 870,123 | 927,711 | 1,041,671 | 13.46 | |
| Per cent change year-to-year | 437 | 52 | 15 | 24 | −3 | 7 | 12 |
Sources: MOPH, various HMIS reports, 2004–2011; 2002 and 2006 mortality figures: Ministry of Public Health, 2008; 2010 mortality figures: Afghan Public Health Institute Ministry of Public Health et al., 2011.
Table 5 demonstrates that the proportion of BPHS facilities offering DOTS increased from 11% in 2004 to 66% in 2011, reflecting increased TB control capacity of the system.
Table 5.
Access: Service delivery for communicable disease tuberculosis, 2004–2011.
| 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | Change factor 2004–2011 from 2004 baseline | |
|---|---|---|---|---|---|---|---|---|---|
| Health facilities with DOTS services | 45 | 200 | 545 | 776 | 882 | 1114 | 1071 | 1111 | 24.78 |
| Per cent change year-to-year | 344 | 173 | 42 | 14 | 26 | −3 | 4 |
Source: MOPH, various HMIS reports, 2004–2011.
Health workforce
The number of active CHWs, the percentage of CHWs who are women, and the number of facilities with at least one female health worker have all increased since 2004 (see Table 6). Table 6 also shows that increased insecurity, especially in the areas where the Taliban are more active, has caused some female health workers and CHWs to drop out of the health workforce due to fears of reprisals and recriminations. Another earlier study showed that degradation of security in Afghanistan has adversely affected the presence of female health workers at clinics (Ameli & Newbrander, 2008). The increased number of midwives trained since 2004 has also increased the opportunity for skilled birth attendance, as shown in Table 6 (Currie, Azfar, & Fowler, 2007).
Table 6.
Health workforce: Females as a proportion of the health workforce, facilities with female health worker, and midwives per 10,000 population, 2004–11.
| 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | Change factor 2004–2011 from 2004 baseline | |
|---|---|---|---|---|---|---|---|---|---|
| Active female CHWs | 729 | 3995 | 5964 | 9185 | 10,147 | 10,576 | 10,300 | 10,980 | 15.06 |
| Per cent change year-to-year | 448 | 49 | 54 | 11 | 4 | −3 | 7 | ||
| Female CHWs as per cent of total CHWs | 44 | 47 | 50 | 50 | 50 | 49 | 48 | 48 | 1.09 |
| Per cent change year-to-year | 7 | 5 | 0 | 0 | −1 | −2 | 0 | ||
| Per cent of BPHS and EPHS facilities with at least one female health worker | 54 | 57 | 77 | 79 | 77 | 79 | 74 | 74 | 1.37 |
| Per cent change year-to-year | 6 | 34 | 3 | −2 | 2 | −5 | −1 | ||
| Midwives per 10,000 population | 0.08 | 0.27 | 0.52 | 0.64 | 0.70 | 0.80 | 0.79 | 0.82 | 10.25 |
| Per cent change year-to-year | 235 | 93 | 23 | 10 | 14 | −2 | 3 |
Source: MOPH, various HMIS reports, 2004–2011.
Information
The HMIS has grown in its effectiveness: from only a third of facilities regularly reporting their data to the HMIS to 90% in 2011. Likewise, routine statistics from 75% of the active health posts are available. Aspects of the HMIS that contributed to its successful implementation were limited computerisation – only up to the level that could be sustained locally, decentralised data collection and entry and full access to all public data for all partners contributing data to the system (Ickx, 2010).
Medical products, vaccines and technologies
Table 7 demonstrates that percentage of facilities with stock-outs of one essential medicine has decreased over time. This measure is taken by monitors visiting BPHS health facilities, so it does not mean that the stock-out is constant. Rather it is a measure at one point in time for a particular health facility.
Table 7.
Supply of medicines: Stock-outs and expenditure for drugs and contraceptives for health facilities, 2004–2011.
| 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | Change factor 2004–2011 from 2004 baseline | |
|---|---|---|---|---|---|---|---|---|---|
| Per cent of BPHS and EPHS facilities with at least one essential drug stock-out | 80.3 | 70.4 | 78.9 | 76.3 | 70.0 | 66.8 | 66.8 | 61.0 | 0.76 |
| Per cent change year-to-year | −12 | 12 | −3 | −8 | −5 | 0 | −9 | ||
| Annual expenditure for drugs and contraceptives (US$) for 13 USAID-funded provinces | 1,036,983 | 3,027,657 | 3,729,524 | 3,301,793 | 3,062,378 | 5,309,348 | 4,804,968 | 5,058,723 | 4.88 |
| Per cent change year-to-year | 192 | 23 | −11 | −7 | 73 | −9 | 5 |
Source: MOPH, various HMIS reports, 2004–2011; Management Sciences for Health, procurement records.
Financing
As of 2009, Afghanistan spent 10% of its gross domestic product on health (Ministry of Public Health, 2011). Contributions of donors, NGOs and MOPH partners represented more than three times the government's annual expenditure for health. Relatively high and steady funding from donors for the health system enabled much of the development and progress noted.
A regular supply of pharmaceuticals has also been critical to provision of services. Table 7 demonstrates this support: the value of drugs purchased for BPHS and EPHS services in the 13 USAID-funded provinces had increased to US$5.3 million by 2009 from $1.0 million in 2004 as utilisation went up (Newbrander, Bishop, Roshan, & Ickx, 2012). While the financing of health has been strong, the challenge will be to maintain earlier levels of financing in the future as donors decrease their participation in the Afghan health sector in the coming years (Belay, 2010).
Leadership and governance
Leadership and governance occur at different levels of the health system and are difficult to quantify. The MOPH early on actively pursued the government's Priority Reform and Reconstruction policy, contributing to selecting an appropriate and motivated workforce at central and provincial level. Provincial officials have mentioned a real increase in the productivity of health professionals as early as 2006 (World Health Organization, 2006). At the central level, the MOPH manifested its readiness to collaborate with all donors and agencies that accepted the national priorities by establishing coordination mechanisms that:
demonstrated to stakeholders the willingness of the MOPH to lead the health sector;
enhanced sector-wide health development by involving all stakeholders, whether public, private non-profit, private-for-profit or international agencies;
fostered discussion about the effective and efficient use of limited resources;
promoted working towards sustainability of the health system and the Ministry.
At the central level, the MOPH established taskforces, consisting of key technical advisors, to provide input on specific topics, such as nutrition and reproductive health. These groups assist directorates and departments to develop policies, intervention strategies, implementation guidelines and programme recommendations. The National Technical Coordination Committee, which represents all agencies involved in health, serves as an information-sharing forum.
At the provincial level, the MOPH formed Provincial Health Coordination Committees (PHCCs) in each province in 2003 to coordinate the activities of all provincial stakeholders. While it is difficult to determine how effective the PHCCs have been, we used the percentage of provinces regularly submitting minutes of the PHCC meetings to the MOPH Provincial Liaison Office as a proxy for the degree to which they have been active. The data are incomplete, but discussions with office staff indicate that an increasing number of provincial PHCCs were submitting these reports regularly in 2010.
The number of health shura meetings held in all provinces increased from 972 in 2004 to 12,452 in 2011 (Table 8), nearly a 13-fold increase during that time. The BSC reported that 95% of health facilities had records of meetings with the health shura (Edward et al., 2011). The number of active Family Health Action Groups established by 2011 was 3165.
Table 8.
Governance: Number of health shura (committee) meetings, 2004–2011.
| 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | Change factor 2004–2011 from 2004 baseline | |
|---|---|---|---|---|---|---|---|---|---|
| Number of meetings with health shura (committee) | 972 | 5101 | 7613 | 10,566 | 11,422 | 12,387 | 11,442 | 12,452 | 12.81 |
| Per cent change year-to-year | 425 | 49 | 39 | 8 | 8 | −8 | 9 |
Source: MOPH, HMIS reports 2004–2011.
Discussion
The results of the countrywide introduction and sustained implementation of the BPHS in 2003 are significant, both for improved health indicators and for development of a new health system that continue to focus on priority community-based services for this rural country. The data show large gains when we examine the components of the rebuilt and strengthened health system.
Nationwide implementation of a well-defined BPHS enabled increased health service delivery in Afghanistan through:
increased access, reflected in increased numbers of service delivery points and BPHS facilities;
increased utilisation, reflected in the average number of patient visits of 2209 per month in 2011, compared with estimated averages of 450 per month in 1973 (O'Connor, 1980) and 520 per month in 1991 (O'Connor, 1994);
better access for women, since 80% of facilities have female health staff and the number of midwives has increased;
increased utilisation of services for deliveries, reflected in the increases in facility-based deliveries.
The MOPH's focus on women and children in the BPHS has had significant effects on the health of those groups, as documented in the reductions in infant, child and maternal mortality in the 2010 Afghan Morality Survey. Despite tremendous progress, however, Afghanistan still compares poorly to countries in the same region – India, Bangladesh, Pakistan and Nepal – in measures of child mortality, maternal mortality and contraceptive use, although the gap has been significantly reduced.
We cannot attribute this progress to only one factor or determine the proportionate contribution of several concurrent factors to that progress. Comparing results from other fragile states that used the Afghan BPHS as a model, such as Liberia, South Sudan and Somalia, with the results achieved in Afghanistan is not possible, because they have not yet evaluated the changes since introduction of their basic packages to the same extent.
We think, however, that the experience in Afghanistan is a good example of the design and implementation of a basic health service policy and package that contributed to overall health system strengthening. Improved service delivery, in turn, is generally accepted as a stabilising factor in a post-conflict situation (Health and Fragile States Network, 2009; Vaux & Visman, 2005). The lesson for other fragile states faced with restructuring their health systems is that, with good information and the political commitment required to address urgent health needs, focused technical interventions can achieve positive results. Further, the MOPH's preoccupation with equity and making the underserved a priority from the very start, as demonstrated as a key component of their Public Health Decision Framework, was probably one of the factors that lead to success. This is different than what happened in Cambodia and Uganda, where inequity in service delivery of the new system is cited as a reason for failure (Vaux & Visman, 2005). So the Afghan BPHS experiment represents important lessons in health system reconstruction and strengthening efforts for other countries.
We considered issues that arise in maximising the capacity of service delivery in conflict or post-conflict situations in order to understand possible reasons for the success of the BPHS in Afghanistan (Newbrander, Waldman, & Shepherd-Banigan, 2011). The BPHS was developed as the key tool for implementing the draft health policy and strategy of the nascent post-Taliban MOPH. The BPHS not only indicated what interventions and service were needed, but also clearly indicated what preventive and curative care needed to be provided at the different service levels. It reduced a myriad of health facility types that NGOs had developed to a common and limited set of health facility types (Ministry of Health, 2002; Ministry of Health, 2003; health sub-centres, basic health centres, comprehensive health centres and district hospitals), each with recommended staffing, medicines, supplies and equipment matching the services to be provided. This provided a clear road map for the MOPH, donors and the different health service providers to start rebuilding the health system, along with the possibility of projecting the costs of implementing the package.
One pitfall the BPHS helped to avoid was restoration of a previous largely inefficient and inequitable health service delivery system, which was one factor that undermined the successful implementation of a similar package in Uganda (Vaux & Visman, 2005). While some were nostalgic about the ‘golden years’ of the 1970s, there is evidence that the highly centralised public health system was inefficient in delivery of health services in the rural areas then (O'Connor, 1980). The BPHS allowed all actors in the health sector to take advantage of the small window of opportunity when rapid change can be implemented with minimal barriers. One has to credit the MOPH of the Transitional Authority in 2002 for grasping the opportunity.
While in many countries the post-conflict period brings ample donor funding for health, few nations make optimal use of the funding. Maybe inspired by less successful examples in East Timor, Cambodia and Mozambique (Vaux & Visman, 2005), the primary donors in the health sector in Afghanistan agreed on priorities with the MOPH in 2002, and the BPHS helped to steer donor efforts towards common objectives. The establishment by the MOPH of coordination mechanisms for policy and strategy development, as well as implementation of service delivery, contributed to ensuring sustained support for BPHS implementation, in spite of changing leadership in the MOPH.
Several post-conflict countries have relied on non-governmental entities for service delivery, which allows rapid expansion of services but may neglect government capacity building and sometimes bypass the public-sector system. While we do not know what will happen in the long term, the contracting out of BPHS services in Afghanistan seems promising for sustainability because:
the MOPH is involved in contracting through a specific unit in the Ministry;
the Ministry monitors performance and links continued support for service delivery to achievement of results;
donors are exploring with the MOPH continuation of the contracting schemes through the normal government budgeting process.
There are advantages and disadvantages to our methodology of using the WHO six building blocks of health system strengthening to assess BPHS (Alva, Kleinau, Pomeroy, & Rowan, 2009). First, it is a complex integrated approach. Applying the building blocks allowed us to focus the assessment and discussion on what WHO and other agencies see as the prerequisites for solid health system strengthening or in the case of Afghanistan, health system rebuilding. Second, by systematically applying the building blocks respects the interdependence of the many BPHS interventions and prevents us from singling out a single intervention and overestimating its contribution to the progress made. The disadvantage of our approach is that different agencies often use different indicators for measuring progress or measure the same indicator differently. The choice of indicators in a particular situation is often determined by what data are readily available. This was our approach, we took what data were available that allowed linking back to the building blocks. All indicators used in the paper are also recommended by others, but we are well aware that they may not capture all aspects of the BPHS. With time, a more solid set of globally accepted indicators may emerge to assist us in such assessments. The BPHS addressed aspects of all six health system building blocks. But to what precise degree it contributed to the successes noted in Afghanistan merits a more detailed and formal study.
Conclusion
As donor resources begin to decrease in the years ahead, the MOPH must focus on sustaining the hard-won gains of the greatly expanded health system. In addition, to reach the remaining 20–30% of the population for whom access to health care is most difficult, Afghanistan will need to renew its emphasis on expanding community-based initiatives rather than increasing the number of health facilities. Afghanistan has achieved significant progress in the development of its health system since 2001, but the next challenge is to consolidate these gains and find innovative means for maintaining them while expanding access to and continuing to improve the quality of BPHS care.
BPHS implementation contributed to success in improving health status by:
translating policy and strategy into practical interventions;
focusing on priority interventions;
clearly defining the services to be delivered at different service levels;
addressing the continuum of care from community to facility, including referral.
Design and implementation of the BPHS was not done in a vacuum but was promoted by:
close coordination with donors and their flexibility in exploring funding mechanisms;
willingness of the MOPH to explore reformation instead of restoration;
optimal use of civil society organisations through performance-based contracting;
timely development of routine HMIS and independent evaluations of BPHS implementation.
We recommend similar studies of other packages of services recently developed in post-conflict countries.
References
- Afghan Public Health Institute Ministry of Public Health, Central Statistics Organization, ICF Macro, Indian Institute of Health Management Research, & WHO Regional Office for the Eastern Mediterranean. Afghanistan mortality survey 2010. 2011. Retrieved February 10, 2013, from http://moph.gov.af/Content/Media/Documents/AMS2010FinalFullReport14122011142624269553325325.pdf.
- Alva S., Kleinau E., Pomeroy A., Rowan K. Measuring the impact of health systems strengthening: A review of the literature. 2009. Retrieved January 30, 2013, from http://transition.usaid.gov/our_work/global_health/hs/publications/impact_hss.pdf.
- Ameli O., Newbrander W. Contracting for health services: Effects of utilization and quality on the costs of the Basic Package of Health Services. Bulletin of the World Health Organization. 2008;86:12–20. doi: 10.2471/BLT.08.053108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartlett L., Mawji S., Whitehead S., Crouse C., Dalil S., Ionete D. the Afghan Maternal Mortality Study Team. Where giving birth is a forecast of death: Maternal mortality in four districts in Afghanistan, 1999–2002. Lancet. 2005;365:864–870. doi: 10.1016/S0140-6736(05)71044-8. [DOI] [PubMed] [Google Scholar]
- Belay T., editor. Building on early gains in Afghanistan's health, nutrition, and population sector: Challenges and options. Washington, DC: World Bank; 2010. [Google Scholar]
- Bobadilla J., Cowley P., Musgrove P., Saxenian H. Design, content and financing of an essential national package of health services. Bulletin of the World Health Organization. 1994;72:653–662. [PMC free article] [PubMed] [Google Scholar]
- Currie S., Azfar P., Fowler R. C. A bold new beginning for midwifery in Afghanistan. Midwifery. 2007;23:226–234. doi: 10.1016/j.midw.2007.07.003. [DOI] [PubMed] [Google Scholar]
- Edward A., Kunar B., Kakar F., Salehi A., Burnham G., Peters D. Configuring Balanced Scorecards for measuring health system performance: Evidence from 5 years' evaluation in Afghanistan. PLoS Medicine. 2011;8(7):e1001066. doi: 10.1371/journal.pmed.1001066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health and Fragile States Network. Health systems strengthening in fragile contexts: A report on good practices and new approaches. 2009. Retrieved from http://www.healthandfragilestates.org/index2.php?option=com_docman&task=doc_view&gid=54&Itemid=38.
- Hilla S., Eangb M. Resistance and renewal: Health sector reform and Cambodia's national tuberculosis programme. Bulletin of the World Health Organization. 2007;85:631–636. doi: 10.2471/BLT.06.036822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hrabaè B., Ljubiæ B., Bagariæ I. Basic package of health entitlements and solidarity in the Federation of Bosnia and Herzegovina. Croatian Medical Journal. 2000;1:287–293. [PubMed] [Google Scholar]
- Ickx P. Health intelligence in emergencies: Which information and why? Health in emergencies. Geneva: World Health Organization; 2002. Retrieved October 4, 2012, from http://www.who.int/hac/about/8632.pdf. [Google Scholar]
- Ickx P. Development of the HMIS in Afghanistan. 2010. Presentation prepared for 2010 American Public Health Association Annual Meeting. Unpublished.
- Loevinsohn B., Harding A. Buying results? Contracting for health service delivery in developing countries. Lancet. 2005;366:676–681. doi: 10.1016/S0140-6736(05)67140-1. [DOI] [PubMed] [Google Scholar]
- Loevinsohn B., Sayed G. Lessons from the health sector in Afghanistan: How progress can be made in challenging circumstances. Journal of the American Medical Association. 2008;300:724–726. doi: 10.1001/jama.300.6.724. [DOI] [PubMed] [Google Scholar]
- Ministry of Health. Afghanistan national health resources assessment. Vol. 2002. Kabul: MOH, Transitional Islamic Government of Afghanistan; 2002. Retrieved October 4, 2012, from http://www.msh.org/afghanistan/ANHRA_2002_LITE.pdf. [Google Scholar]
- Ministry of Health. A Basic Package of Health Services for Afghanistan 2003/1382. Kabul: Transitional Islamic Government of Afghanistan; 2003. Retrieved October 4, 2012, from http://unpan1.un.org/intradoc/groups/public/documents/apcity/unpan018852.pdf. [Google Scholar]
- Ministry of Health [Rwanda], National population Office [Rwanda], & ORC Macro. Rwanda service provision assessment survey 2001. Calverton, MD: Author; 2003. [Google Scholar]
- Ministry of Health [Uganda] Health sector strategic plan 2000/1–2004/5. Kampala: MOH; 2000. [Google Scholar]
- Ministry of Public Health. A Basic Package of Health Services for Afghanistan 2005/1384. Kabul: Transitional Islamic Government of Afghanistan; 2005a. Retrieved October 4, 2012, from http://www.msh.org/afghanistan/pdf/Afghanistan_BPHS_2005_1384.pdf. [Google Scholar]
- Ministry of Public Health. The essential package of hospital services for Afghanistan 2005/1384. Kabul: Islamic Republic of Afghanistan; 2005b. Retrieved January 31, 2013, from http://moph.gov.af/Content/Media/Documents/EPHS-2005-FINAL29122010164126629.pdf. [Google Scholar]
- Ministry of Public Health. Afghanistan health indicators: Fact sheet. Kabul: MOPH; 2008. Retrieved February 10, 2012, from http://moph.gov.af/Content/Media/Documents/Afg-Health-Indicators-Factsheet-August20082812201014152812.pdf. [Google Scholar]
- Ministry of Public Health. National health accounts Afghanistan 2008–2009: Preliminary findings. Kabul: Afghanistan Ministry of Public Health; 2011. Retrieved January 25, 2012, from: http://www.who.int/nha/country/afg/afg-nha_2008-2009.pdf. [Google Scholar]
- Ministry of Public Health, Johns Hopkins University, & Indian Institute of Health Management Research. Afghanistan health survey 2006: Estimates of priority health indicators for rural Afghanistan. 2006. Retrieved October 4, 2012, from http://www.independentadvocate.org/downloads/afghanistan-health-survey-2006.pdf.
- Newbrander W., Bishop C., Roshan A., Ickx P. Health system strengthening 2002–2011: Improvements in the health system of Afghanistan. Cambridge, MA: Management Sciences for Health; 2012S. Unpublished paper prepared for Tech-Serve Project. [Google Scholar]
- Newbrander W., Waldman R., Shepherd-Banigan M. Rebuilding and strengthening health systems and providing basic health services in fragile states. Disasters. 2011;35:639–660. doi: 10.1111/j.1467-7717.2011.01235.x. [DOI] [PubMed] [Google Scholar]
- Newbrander W., Yoder R., Bilby A. Rebuilding health systems in post-conflict countries: Estimating the costs of basic services. The International Journal of Health Planning and Management. 2007;22(4):1–18. doi: 10.1002/hpm.878. [DOI] [PubMed] [Google Scholar]
- O'Connor R. W., editor. Managing health systems in developing areas: Experiences from Afghanistan. Lexington, MA: Lexington Books; 1980. [Google Scholar]
- O'Connor R. W., editor. Health care in Muslim Asia: Development and disorder in wartime Afghanistan. Langham, MD: University Press of America; 1994. [Google Scholar]
- Palmer N., Strong L., Wali A., Sondorp E. Contracting out health services in fragile states. British Medical Journal. 2006;332:718–721. doi: 10.1136/bmj.332.7543.718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts B., Guy S., Sondorp E., Lee-Jones L. A Basic Package of Health Services for post-conflict countries: Implications for sexual and reproductive health services. Reproductive Health Matters. 2008;16(31):57–64. doi: 10.1016/S0968-8080(08)31347-0. [DOI] [PubMed] [Google Scholar]
- Salama P. Status of the health and nutrition sector in Afghanistan: Progress and challenges 2001–2003. Kabul: UNICEF; 2003. Unpublished presentation by the Chief Health and Nutrition Officer of UNICEF. [Google Scholar]
- Vaux T., Visman E. Service delivery in countries emerging from conflict: Final report. Bradford: Department of Peace Studies, Centre for International Co-operation and Security, University of Bradford; 2005. [Google Scholar]
- Ventevogel P., van de Put W., Faiz H., van Mierlo B., Siddiqi M., Komproe I. H. Improving access to mental health care and psychosocial support within a fragile context: A case study from Afghanistan. PLoS Medicine. 2012;9(5):e1001225. doi: 10.1371/journal.pmed.1001225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waldman R., Hanif H. The public health system in Afghanistan: Current issues. Kabul: Afghanistan Research and Evaluation Unit; 2002. Retrieved October 4, 2012, from http://amec.glp.net/c/document_library/get_file?p_l_id=844072&folderId=1038976&name=DLFE-20312.pdf. [Google Scholar]
- Waldman R., Strong L., Wali A. Afghanistan's health system since 2001: Condition improved, prognosis cautiously optimistic. Kabul: Afghanistan Research and Evaluation Unit; 2006. Briefing Paper Series. Retrieved October 4, 2012, from http://reliefweb.int/sites/reliefweb.int/files/resources/29CDF62E3C6F8E23492572C6001A8420-Full_Report.pdf. [Google Scholar]
- World Health Organization. Report of the health system review mission to Afghanistan 9 to 18 July 2006: Challenges and the way forward. Alexandria, Egypt: WHO Eastern Mediterranean Regional Office; 2006. [Google Scholar]
- Unpublished World Health Organization. Everybody's business: Strengthening health systems to improve health outcomes: WHO's framework for action. Geneva: Author; 2007. [Google Scholar]


