Abstract
In Afghanistan, malnutrition in children less than 60 months of age remains high despite nutritional services being offered in health facilities since 2003. Afghanistan's Ministry of Public Health solicited extensive community consultation to develop pictorial community-based growth monitoring and promotion (cGMP) tools to help illiterate community health workers (CHWs) provide nutritional assessment and counselling. The planned evaluation in the five districts where cGMP was implemented demonstrated that a mean weight-for-age (WFA) Z-score of 414 participant children was 0.3 Z-scores higher than that of matched non-participants who lived outside of cGMP programme catchment areas. The mean change in WFA Z-scores at evaluation was 0.3 (95% CI 0.3, 0.4) Z-scores higher than at entry into the programme. The most influential factor on WFA Z-score changes in participants was initial WFA Z-score. Those with an initial WFA Z-score of less than −2 experienced a mean increase of 0.33 (95% CI 0.29, 0.38) WFA Z-scores per session attended, while those with a baseline WFA Z-score of greater than zero showed a decrease of 0.19 (95% CI 0.22, 0.15) WFA Z-scores per session attended. These results are encouraging since they demonstrate that the cGMP programme in Afghanistan for illiterate women has some potential to contribute to improving nutrition, specifically in underweight children of either sex who enter the programme at less than nine months of age and attend 50% or more sessions.
Keywords: Afghanistan, nutrition, growth monitoring, child health, health promotion, community-based health services
Introduction
Afghanistan has one of the highest childhood mortality rates in the world; 1 in 10 Afghan children die before reaching five years of age (Afghan Public Health Institute, Central Statistics Office, ICF Macro, IIHMR, & WHO/EMRO, 2011; Central Statistics Office and UNICEF, 2012). Most childhood deaths in developing countries are associated with malnutrition, and the vast majority of these deaths is related to mild or moderate malnutrition (Pelletier, 1994). Chronic undernutrition in the form of stunting affects 55% of under-five-year-old children in Afghanistan, and 31% of Afghan children under five years of age are moderately or severely underweight (Central Statistics Office and UNICEF, 2012). The consequences of chronic undernutrition on cognitive development and ensuing adult productivity are preventable if early interventions are implemented (Grantham-McGregor et al., 2007; Victoria et al., 2008; Walker et al., 2007). Therefore, tackling the high prevalence of undernutrition in Afghanistan by implementing nutrition programmes that effectively prevent malnutrition, cannot be overstated as essential to improving the health of Afghans (World Bank, 2006).
In 2002, Afghanistan's health system, destroyed after 25 years of conflict, began the slow process of rebuilding. Trained health-care workers returned to the country and new trainees graduated. Many health facilities were built and the Ministry of Public Health (MOPH) developed policies and facility-based programmes that focused on the health needs of sick women and children (Afghan Ministry of Public Health, 2005). The reestablishment of the Public Nutrition Department in the MOPH resulted in a strong nutritional policy framework and a network of Provincial Nutrition Officers. Despite these efforts, preventing malnutrition has been challenging because healthy Afghan children do not regularly attend health facilities and because of the complexity of providing health and preventive services to all Afghans, especially in rural areas (Afghan Ministry of Public Health, 2005).
In Afghanistan, service provision has been complicated by several factors: 77% of Afghans live in sparsely inhabited areas with poor transportation, few trained health professionals and only 8% of women were literate in 2003 (The United Nations Children's Fund [UNICEF], 2005). Thus while the Afghan health system matures, community health workers (CHWs) play an important role in service delivery. By 2012, 22,300 CHWs, of whom 49% were female, had been trained and were providing basic preventative and limited curative services in rural areas. Challenges faced by CHWs include their low literacy levels, lack of job aids to address malnutrition, lack of security and cultural norms that require women to be accompanied by a male relative when circulating in public. Enabling CHWs to provide nutritional services involved developing a community-based programme that was easy for women to attend, acceptable to family decision-makers and provided by trained women in the community using locally relevant, easily understood and pictorial tools.
Community-based growth monitoring and promotion (cGMP) programmes have been implemented in developing countries of Asia, Africa and the Americas (World Bank, 2006). Although programmes vary, their aims are consistent: the promotion of regular growth-monitoring sessions for children under the age of five and the provision of nutritional counselling based on the weight gained and the child's age (BASICS II, 2004; Rifkin, Hewitt, & Draper, 2007; Schaetzel, Griffiths, Del Rosso, & Plowman, 2008). A fundamental component included in most programmes is community-based social change that identifies community-level solutions to prevent malnutrition (Ashworth, Shrimpton, & Jamil, 2008; Schaetzel et al., 2008; World Bank, 2006).
Although most cGMP programmes have not been adequately evaluated, cGMP programmes in Madagascar, Honduras and Uganda have shown success in nutritional parameters, and other programmes have resulted in improved caretaker knowledge (Alderman, 2007; Galasso & Umapathi, 2007; Schaetzel, et al., 2008). Several reports describe the importance of targeting children less than two years of age, training female CHW in nutrition, including a community platform to encourage behaviour change, using simplified assessment and counselling cards that do not require plotting of Z-scores and facilitating referral of malnourished children to health facilities (Anderson, Chintu, & Kapulula, 2009; Ashworth et al., 2008; Gartner, Maire, Kameli, Traissac, & Delpeuch, 2006; Schaetzel et al., 2008; Tontisirin, Attig, & Winichagoon, 1995; World Bank, 2006). Conducting an early evaluation of the cGMP programme has been emphasised, with the intent of making timely modifications to the programme (Engle et al., 2007; Galasso & Umapathi, 2007; Afghan Ministry of Public Health and Centers for Disease Control, 2009; Schaetzel et al., 2008; Walker et al., 2011; World Bank, 2006).
The Afghan Ministry of Public Health (MOPH) used these key programme elements and its extensive experience in creating community-oriented programmes to design a cGMP programme with three components: (1) to monitor the weights of children from birth to two years to identify those who had not gained adequate weight, (2) to give the caretakers of these children tools to aid the children in ‘catch-up’ growth and promote optimal feeding practices and (3) to create social change by mobilising caretakers to regularly weigh children under the age of two and discuss appropriate food and feeding techniques with other female caretakers and CHWs (BASICS II, 2003, 2004; Contreras et al., 2004; Fiedler, 2000; Rifkin et al., 2007; UNICEF, 2008). In Afghanistan, Family Health Action Groups (FHAGs) have been adopted as ‘community platforms’ by the MOPH (Figure 1). They offer an activity, such as weighing of children under age five, that functions as a catalyst to bring together young children and their female caretakers, with consequent social change and improvements in child health (Future Generations, 2006; Levitt, UNICEF, & Afghan Ministry of Public Health, 2005; UNICEF, 2003).
Figure 1.
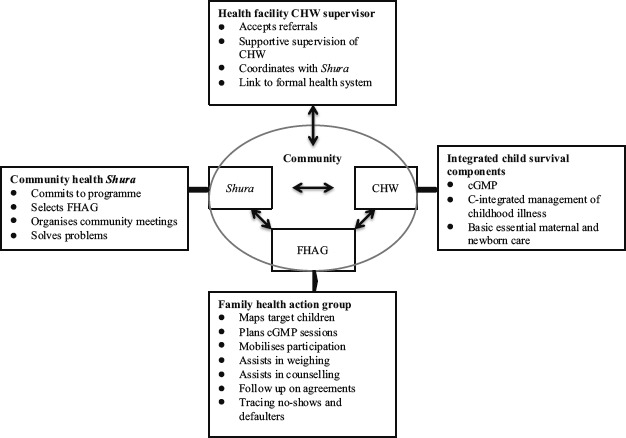
Afghan community platform for integrated child survival programme, including nutrition.
Developing pictorial tools to assess children's weight gain and provide nutritional counselling to caretakers involved extensive community consultation. During the first step in this process, the concept of the programme was described to village mullahs and elders to obtain feedback on counselling, assessment and recording tools previously developed in Afghanistan and in other countries (Afghan Ministries of Agriculture & Public Health, 2008; Schaetzel et al., 2008). After incorporating this feedback in seven consultative discussions with female CHWs and FHAG members, all symbols, colours and drawings used in the counselling, assessment and recording tools, including the weighing scale, the gradations on the scale and the weight symbols were discussed and modified until consensus on the tools was achieved (Figure 2). In 2008, after the tools had been finalised, the Public Nutrition Department field tested them and concluded that the tools could be used by CHWs and FHAG members to assess children's weight gain and provide advice to caregivers.
Figure 2.
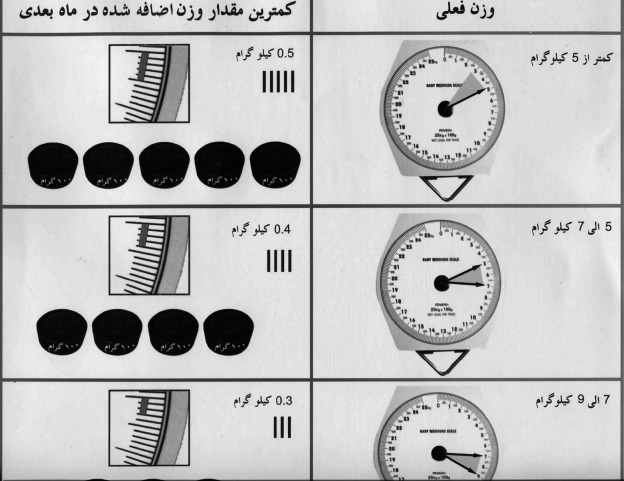
Pictorial assessment tool used by CHWs to assess appropriate weight gain.
The cGMP programme in Afghanistan became one of three components of an Integrated Child Survival Package developed as a demonstration project that began in May 2009 in five rural districts of five provinces in Afghanistan: Shahfoladi (Bamyan Province), Ghorian (Herat Province), Qarqin (Jawzjan Province), Farza (Kabul Province) and Farkhar (Takhar Province; Figure 3). These districts, where the Basic Package of Health Services was being implemented by five different non-governmental organisations (NGOs), represented different ethnic, language and religious groups of Afghanistan and varied in distance to the closest urban centre. Other components of the Integrated Child Survival Package included community-based integrated management of childhood illnesses (C-IMCI), which emphasised appropriate care and health-care seeking for sick children, and basic essential maternal and newborn care, which emphasised improving neonatal care, birth spacing and improving knowledge of when to seek care for pregnant women and young infants. Participation in all programmes was entirely self-selected on the part of caretakers.
Figure 3.
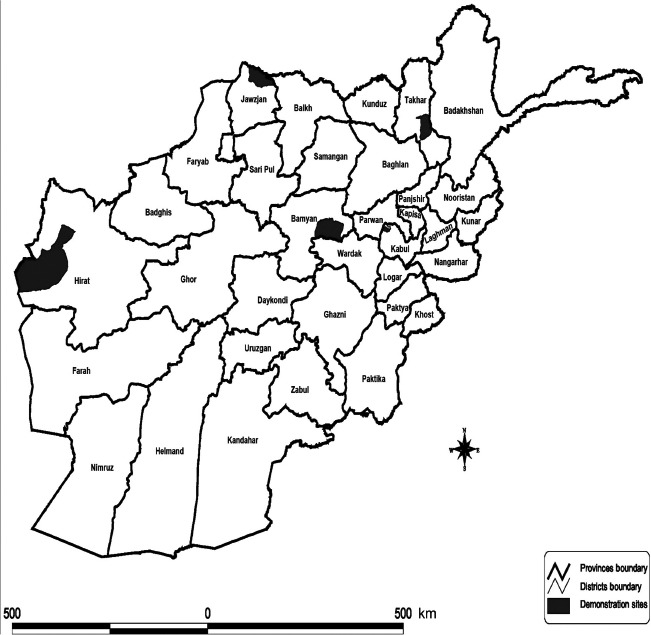
Map of five demonstration districts for cGMP programme.
NGO employees, previously trained in cGMP, taught the CHWs for five days in 2009. Both female and male CHWs were trained in all five districts but only in Bamyan Province did male CHWs systematically attend the weighing sessions. Skills taught to the CHWs included how to (1) zero the Salter scale and weigh the child, (2) use the pictorial tools to record weights, (3) determine if weight gains were adequate, (4) identify whom to counsel and (5) counsel on feeding. CHWs were regularly supervised and monitored by the NGOs. The CHWs used colour-coded pictorial charts to illustrate acceptable weight gains for particular ages so they could assess which children had not gained sufficient weight (Figure 2). The target weights in the charts were based on weight-for-age (WFA) Z-scores (Ashworth et al., 2008; de Onis & Blössner, 1997). WFA, rather than weight-for-height measurements, were used because of the relatively short time frame for the evaluation, the extra training and equipment required to measure height and because WFA is an easily understood, commonly used parameter in cGMP programmes (Levitt et al., 2005). In the five districts where cGMP had been implemented, the programme was considered by the MOPH to be acceptable to Afghan communities based on high levels of participation in preparatory community meetings and the findings in NGO reports (July 2010) that an average of 53% of the targeted children were participating in the programme.
Objectives
The purpose of this evaluation was to assess the cGMP programme's impact on the nutritional status of young, Afghan children. This evaluation was designed to determine:
If children less than 18 months old who had participated in the cGMP programme had WFA Z-scores closer to the reference than non-participants of the same age and sex who lived nearby.
If the WFA Z-scores of participants in the cGMP programme improved during the period of their involvement, based on comparing, for each participant, WFA Z-scores at the evaluation and the last cGMP visit to initial visit Z-scores.
Methods
We used a cross-sectional comparison of mean WFA Z-scores between participant and non-participant groups matched for age, sex and geographic area, and a retrospective comparison between initial, final and survey WFA Z-scores in a cohort of cGMP participants who met the inclusion criteria for the evaluation.
The evaluation took place in 78 of the 99 existing health posts in five districts of the demonstration project areas. Health posts were included if at least two children in cGMP programmes met the inclusion criteria. Of 5550 children who had been registered in the cGMP programme, 548 potential participants were selected by systematically identifying the following five criteria from a retrospective chart review:
-
(1)
Age at the time of the evaluation 6–18 months
-
(2)
Age at registration in the cGMP programme of 9 months or less
-
(3)
Registered after 31 December 2009, when full implementation of the cGMP demonstration projects was established
-
(4)
Registered a minimum of three months in the cGMP programme
-
(5)
Attended a minimum of 50% of planned sessions
Non-participants were selected based on agreement by any caretaker to be included in the evaluation if their child satisfied four inclusion criteria:
-
(1)
Had the same age (±1 month) as the matched participant
-
(2)
Had the same sex as the matched participant
-
(3)
Had never participated in any cGMP programme
-
(4)
Lived in similar areas to participants but outside of the catchment area of the cGMP programme.
Non-participant caretakers received counselling and a referral to a health facility if the nutritional status of the child warranted treatment.
Standard MOPH procedures for consent and anonymity were followed. These were identical to those used in the annual household surveys of the MOPH's USAID-funded Partnership Contracts for Health Services. Participants and non-participants who met the inclusion criteria were asked to be involved in the evaluation by teams of CHWs and evaluators. Non-participants were assured that participation in the assessment had no influence on their future participation in the cGMP programme.
Pairs of male physicians with previous experience in CHW training and supervision collected data for both the retrospective and the matched comparison between June and August 2011. The physicians received training in (1) acquiring data from the cGMP pictorial cards, (2) verifying ages of the children from vaccination cards, (3) calibrating and using Salter scales to obtain children's weights and (4) appropriately administering the questionnaire. Protocols were refined and finalised during a trial round when technical training officers verified the data collectors' skills.
The physician teams verified inclusion criteria when collecting data from the cGMP pictorial cards. Age of the child was obtained from the vaccination card, the cGMP card or, as a last recourse, by asking the caretaker. In the cGMP cards, the recorded weights of children included clothing because undressing the child for weighing was not acceptable to caretakers. For the evaluation visit, calibrated Salter scales were used to weigh the clothed children and similar clothing separately so that cultural preferences were respected. This allowed comparing clothed weight of the child to the initial cGMP weights and unclothed weights to those of matched non-participants. Physicians supervised the weighing of the participants by CHWs and weighed all non-participants.
For the matched comparison, a structured questionnaire was used and included questions regarding age, literacy and schooling of the mother, size of the family and birth order of the measured child. Resource and time constraints limited more in-depth questions. The selection of non-participants in geographic proximity to participants yet outside of cGMP programme catchment areas was designed to control, as much as possible, for potential confounding influences not elucidated in the evaluation.
Data were entered into pre-formatted spreadsheets and sent electronically to technical officers in Kabul, who verified surveys for completeness and cross-checked paper copies with digital entries. WFA Z-scores for all weights and ages were calculated using the Nutritional Survey function in WHO Anthro software for personal computers. STATA version 11 (StataCorp LP, College Station, TX) was used for the analysis. Statistical significance was set at 0.05. The Student's t test and analysis of variance (ANOVA) were used to test statistical significance to compare means, and the Chi-square statistic was used to compare proportions.
Comparison of mean WFA Z-scores between participants and non-participants
In this comparison, the mean WFA Z-scores of participants were compared with that of non-participants to identify if the cGMP programme was associated with improved nutrition over and above environmental effects. Mean WFA Z-scores of 414 participants and 414 non-participants were calculated using unclothed child weights. Proportions of participants and non-participants with specific caretakers' and children's characteristics as well as reasons for either attending or not attending a cGMP programme were compared. Results were verified by repeating analyses using observations for which age had been identified only from vaccination cards and a second analysis that included only WFA Z-scores between 4 and −4. To ascertain evaluator bias, mean and variance in Z-scores were compared across physician teams.
Retrospective comparison of WFA Z-scores changes amongst participants
In this analysis, the mean change in 411 participants' WFA Z-scores between the first and the last cGMP visits (measured by the CHW) was compared with the mean change in WFA Z-scores between the first cGMP visit and the evaluation visit (supervised weighing by the CHW). The comparison estimated whether participation in the cGMP programme was associated with an increase in WFA Z-scores and provided some degree of concordance of measurements by the CHWs and the physicians. A per unit impact of the programme was estimated by calculating rates of change in WFA Z-scores per session attended for the last cGMP visit and the evaluation visit. Three observations were excluded from this analysis – two because of erroneous initial WFA Z-scores and one because no weight was recorded during the last cGMP visit.
Controlled and uncontrolled linear regression analyses identified associations of independent variables with changes in WFA Z-scores. Two separate outcome variables were used: (1) the difference in WFA Z-scores between the evaluation visit and the first cGMP visit and (2) the difference in WFA Z-scores between the last and the first cGMP visits. To minimise the effect of potential CHW measurement error in the initial WFA Z-scores, only observations within three standard deviations of the WFA Z-score mean of non-participants were included (assumed to be similar to participants' mean initial WFA Z-scores), that is, WFA Z-scores from −4.2 to 2.2.
In each linear regression model, independent variables from the literature that were considered to be significant predictors of nutritional status were included: caretaker literacy, size of family, proportion of planned sessions attended, age of child upon entry to cGMP, sex of child and initial Z-score upon entry to cGMP programme. Continuous independent variables included proportion of planned visits attended and age of the child. Family size was calculated according to the number of children sleeping in the same house and eating at the same hearth. Categorical variables included the province where the cGMP programme had been implemented, sex of the child, WFA Z-score at registration and caretaker's literacy. Caretaker's literacy was categorised into literate (self-perception of ability to count, read and write), illiterate (unable to count, read or write) and ‘did not answer’. The cut-offs for WFA Z-score categories were determined so that similar numbers of observations existed in each category.
Results
Demographic characteristics of participants and non-participants
Mean age of the caretakers was 27.5 years in participants and 27.6 years in non-participants who lived nearby the health post-catchment areas or districts (Table 1). Literacy was slightly higher, but statistically insignificant, in the participants' caretakers (8.3%) compared to non-participants' caretakers (5.7%). A higher but statistically insignificant proportion of caretakers did not answer this question in participants' caretakers (9.9% (95% CI 7.0, 12.8)) compared to the non-participants' caretakers [6.3% (95% CI 3.9, 8.6)]. In each group, the mean age of children was 11.2 months and 45% were females. Caregivers of participants and non-participants reported similar current health status of children, and there was no statistically significant difference in mean family size.
Table 1.
Characteristics of caretakers and children and WFA Z-scores in participants and non-participants.
| Characteristic | Non-participants | Participants | P value* |
|---|---|---|---|
| N | 414 | 414 | |
| Provincea | N (%) | N (%) | |
| Kabul | 83 (20.0%) | 83 (20.0%) | na |
| Bamyan | 103 (24.9%) | 103 (24.9%) | na |
| Herat | 105 (25.4%) | 105 (25.4%) | na |
| Jawzjan | 50 (12.1%) | 50 (12.1%) | na |
| Takhar | 73 (17.6%) | 73 (17.6%) | na |
| Caretaker characteristics | (95% CI) | (95% CI) | |
| Mean age in years | 27.6 (27.1, 28.2) | 27.5 (27.0, 28.1) | 0.9 |
| Literacy | 0.06 | ||
| Illiterate (not able to read, write or count) | 88.4% (85.3, 91.5) | 82.6% (78.9, 86.3) | |
| Literacy (percentage able to read, write and count) | 5.7% (3.3, 7.8) | 8.3% (5.5,11.1) | |
| Refused to answer | 6.3% (3.9, 8.6) | 9.9% (7.0, 12.8) | |
| Able to count | 100% | 99.9% (99.6, 100) | 0.3 |
| Mean no. years schooling | 0.4 (0.2, 0.6) | 0.4 (0.2, 0.5) | 0.9 |
| Child characteristics | (95% CI) | (95% CI) | |
| Child age in months at evaluation | 11.2 (10.9, 11.6) | 11.2 (10.9,11.6) | 1.0 |
| Sex | |||
| Male | 55% | 55% | na |
| Female | 45% | 45% | na |
| Mean birth order of child | 3.7 (3.5, 3.9) | 3.8 (3.6, 4.0) | 0.5 |
| Mean no. of children | 3.7 (3.5, 3.9) | 3.8 (3.6, 4.0) | 0.5 |
| Health of child | N (%) | N (%) | |
| Sick | 74 (18%) | 75 (18%) | 1.0 |
| Somewhat healthy | 168 (41%) | 155 (37%) | 0.2 |
| Healthy | 154 (37%) | 167 (40%) | 0.4 |
| No answer | 18 (4%) | 17 (4%) | 1.0 |
| cGMP programme attendance | (95% CI) | (95% CI) | |
| Percentage of planned sessions attended | na | 87.0% (85.6,88.4) | na |
| Number of sessions attended | 7.1 (6.8, 7.3) | na | |
| N (%) | N (%) | ||
| Reasons for | Non-attendance | Attendance | |
| Sick child | 2 (0.5%) | 31 (8%) | <0.001 |
| Healthy child | 11 (3%) | – | |
| Knowledge or beliefs | 149 (36%) | 354 (86%) | <0.001 |
| Child accompanied siblings | na | 10 (2%) | |
| Child received care elsewhere | 34 (8%) | na | |
| No local resources | 217 (52%) | na | |
| Child required food | 8 (2%) | ||
| Do not know | 11 (3%) | ||
| Mean weight for age Z-scores | Mean (95% CI) | Mean (95% CI) | |
| Using unclothed child weights | |||
| Evaluation visit | −1.2 (−1.3, −1.1) | −0.9 (−1.0, −0.8) | <0.01 |
| Evaluation visit (age from vaccination card only n = 775) | −1.1 (−1.2, −1.0) | −0.9 (−1.0, −0.8) | <0.01 |
| Using clothed child weights | |||
| Evaluation visit | −0.8 (−0.9, −0.7) | 0.9 | |
| Last cGMP visit | −0.8 (−0.9, −0.7) | 0.9 | |
| Difference in WFA Z-scores | Mean (95% CI) | ||
| N | 411 | ||
| Last cGMP visit | 0.3 (0.2, 0.5) | <0.001 | |
| Last cGMP visit (age from vaccination card only n = 376) | 0.4 (0.2, 0.5) | <0.001 | |
| Evaluation visit | 0.3 (0.2, 0.5) | <0.001 | |
| Evaluation visit (age from vaccination card only n = 376) | 0.4 (0.2, 0.6) | <0.001 | |
| Difference in WFA Z-scores per session attended | Mean (95% CI) | ||
| Last cGMP visit | 0.04 (0.02, 0.06) | ||
| By initial WFA Z-score | <0.001 | ||
| Less than −2 | 0.24 (0.20, 0.29) | ||
| −2 to less than 0 | 0.02 (0.00, 0.04) | ||
| 0 or higher | −0.15 (−0.19, −0.11) | ||
| Evaluation visit | 0.05 (0.02, 0.08) | ||
| By initial WFA Z-score | <0.001 | ||
| Less than −2 | 0.33 (0.29, 0.38) | ||
| −2 to less than 0 | 0.01 (0.01, 0.04) | ||
| 0 or higher | −0.19 (−0.22, −0.15) |
Statistical significance set to 0.05.
Although male and female CHWs were trained, only female CHWs were used for the cGMP programmes with the exception of Bamyan, where it was culturally acceptable to have male CHWs provide this service for female caretakers.
Eighty-five per cent of participants' caretakers described bringing the child to the cGMP programme because of knowledge or belief that the programme would be helpful to the child. In the non-participants' caretaker group, the second most common reason for not attending cGMP programme was a belief that the cGMP programme would not be helpful (36%). The most common reason in the non-participant group for not attending a cGMP programme was the absence of a nearby programme (52%).
WFA Z-scores
Table 1 demonstrates that participants had a statistically significantly higher mean WFA Z-score, −0.9 (95% CI −1.0, −0.8), than non-participants, −1.2 (95% CI −1.3, −1.1). For participants, the mean change in WFA Z-scores was the same for both the last cGMP visit and the evaluation visit, a statistically significant increase of 0.3 (95% CI 0.2, 0.5) WFA Z-scores. Overall, the rate of change of WFA Z-score per session attended was 0.05 (95% CI 0.02, 0.08) Z-scores for the evaluation visit and 0.04 (95% CI 0.02, 0.06) Z-scores for the last cGMP visit. These rates of change per session attended were higher in those with initial WFA Z-scores of less than −2 (0.33 (95% CI 0.29,0.38) WFA Z-scores), compared to children with initial WFA Z-scores between −2 and 0 (0.01 (95% CI −0.01, 0.04) WFA Z-scores), and to those with initial WFA Z-scores above 0 (−0.19 (95% CI −0.22, −0.15) WFA Z-scores). Similar rates of change were noted for the last cGMP visit.
Factors associated with changes in WFA Z-scores in participants
Initial WFA Z-score
A child's initial WFA Z-score was the most influential factor associated with changes in WFA Z-scores during enrolment in the cGMP programme (Table 2; Figure 4). In the uncontrolled analysis, an initial WFA Z-score of less than −2 was associated with a 2.97 (95% CI 2.67, 3.27) increase in WFA Z-scores for the evaluation visit compared to those whose starting Z-scores were 0 or above. The magnitude of this association was smaller for those whose initial WFA Z-score was between −2 and 0. When the association was controlled for other factors, the change in WFA Z-scores remained similar in value and statistical significance. Figures 5 and 6 demonstrate a reverse linear relationship between initial WFA Z-score and change in WFA Z-score for both the evaluation visit and the last cGMP visit. This association when controlled for other factors represented an increase of 0.79 (95% CI 0.73, 0.86) WFA Z-scores per unit decrease in initial WFA Z-score for the evaluation visit. Similar, but somewhat smaller, associations were apparent for the last cGMP visit.
Table 2.
Determinants of changes in WFA Z-scores amongst participants of cGMP programme.
| WFA Z-score difference (evaluation and first visits) |
Z-score difference (last and first visits) |
|||||||
|---|---|---|---|---|---|---|---|---|
| Outcome variable |
Uncontrolled model |
Controlled model |
Uncontrolled model |
Controlled model |
||||
| Independent variable (95% CI) | Regression coefficient | P value | Regression coefficient | P value | Regression coefficient | P value | Regression coefficient | P value |
| N | 388 | 388 | 382 | 382 | ||||
| Caretaker literacy | ||||||||
| Not literate | Reference | Reference | Reference | Reference | ||||
| Literate | −0.08 (−0.63, 0.46) | 0.8 | 0.21 (−0.20, 0.62) | 0.6 | −0.19 (−0.66, 0.29) | 0.4 | 0.16 (−0.22, 0.55) | 0.4 |
| No answer | −1.01 (−1.50, −0.52) | <0.001 | −0.06 (−0.44, 0.33) | 0.8 | −0.40 (−0.82, 0.01) | 0.06 | 0.36 (−0.01, 0.72) | 0.06 |
| Size of family | −0.04 (−0.11, 0.03) | 0.4 | −0.02 (−0.08, 0.03) | 0.4 | 0.01 (−0.08, 0.05) | 0.7 | 0.00 (−0.05, 0.05) | 0.98 |
| Sex of child | ||||||||
| Female | Reference | Reference | Reference | Reference | ||||
| Male | −0.18 (−0.48, 0.12) | 0.2 | −0.22 (−0.43, −0.01) | 0.04 | −0.19 (−0.44, 0.06) | 0.1 | −0.21 (−0.41, −0.01) | 0.04 |
| Age of first contact | −0.03 (−0.10, 0.04) | 0.4 | 0.00 (−0.05, 0.05) | 0.9 | 0.03 (−0.03, 0.09) | 0.4 | 0.05 (0.00, 0.09) | 0.04 |
| WFA Z-score at first visita | ||||||||
| Z-score ≥0 | Reference | Reference | Reference | Reference | ||||
| −2< Z-score <0 | 1.12 (0.87, 1.38) | <0.001 | 1.09 (0.84, 1.34) | <0.001 | 0.96 (0.72, 1.20) | <0.001 | 0.92 (0.68, 1.16) | <0.001 |
| Z-score < −2 | 2.97 (2.67, 3.27) | <0.001 | 2.84 (2.54, 3.14) | <0.001 | 2.21 (1.93, 2.49) | <0.001 | 2.17 (1.88, 2.45) | <0.001 |
| Percentage of sessions attended | 1.43 (0.41, 2.45) | 0.01 | 1.01 (0.20, 1.82) | 0.02 | 0.57 (−0.30, 1.43) | 0.2 | 0.43 (−0.34, 1.20) | 0.3 |
| Provinceb | ||||||||
| Kabul | Reference | Reference | − | Reference | Reference | – | ||
| Bamyan | 0.81 (0.39, 1.24) | <0.001 | 0.42 (0.09, 0.76) | <0.01 | 0.42 (0.06, 0.79) | <0.02 | 0.31 (−0.01, 0.63) | 0.06 |
| Herat | 0.31 (−0.12, 0.73) | 0.2 | 0.31 (−0.02, 0.64) | 0.07 | 0.21 (−0.15, 0.57) | 0.3 | 0.35 (0.03, 0.67) | 0.03 |
| Jawzjan | 0.76 (0.26, 1.27) | <0.01 | 0.50 (0.09, 0.91) | 0.02 | 0.62 (0.19, 1.05) | <0.01 | 0.53 (0.14, 0.92) | <0.01 |
| Takhar | 1.22 (0.76, 1.69) | <0.001 | 0.61 (0.25, 0.97) | 0.001 | 0.96 (0.57, 1.35) | <0.001 | 0.65 (0.31, 0.99) | <0.001 |
| Constant | −2.03 (−2.89, −1.18) | <0.001 | −1.57 (−2.38, −0.75) | <0.001 | ||||
| R2 | 0.55 | 0.43 | ||||||
| Adjusted R2 | 0.53 | 0.41 | ||||||
| Probability > F | <0.001 | <0.001 | ||||||
Note: Bold values indicate statistical significance based on p < 0.05 and non-overlapping confidence intervals.
In the controlled regression models in which the initial WFA Z-score variable was changed from categorical to continuous, a 0.79 (95% CI 0.73, 0.86) increase in WFA Z-score per unit decrease in initial WFA Z-score for the evaluation visit and a 0.61 (95% CI 0.55, 0.68) increase in WFA Z-score per unit decrease in initial WFA Z-score for the last cGMP visit were demonstrated.
Although male and female CHWs were trained, only female CHWs were used for the cGMP programmes with the exception of Bamyan, where it was culturally acceptable to have male CHWs provide this service for female caretakers.
Figure 4.
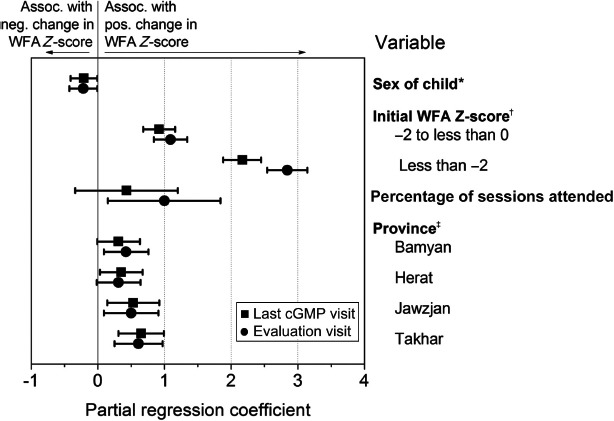
Determinants of WFA Z-score changes in the last cGMP visit and evaluation visit. Notes: Coefficients of variation were controlled for family size, child sex, and age of child at first cGMP visit. *Reference category was illiterate caretaker. †Reference category was initial WFA Z-score zero or above. ‡Reference category was Kabul Province.
Figure 5.
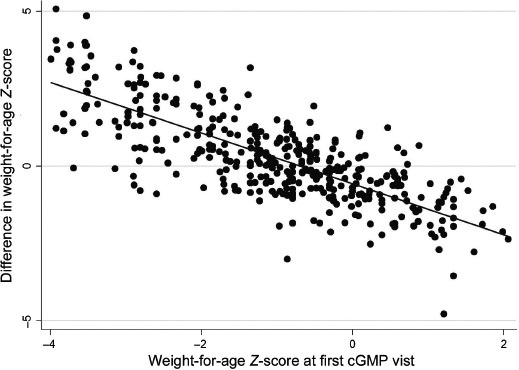
WFA Z-score differences: Last cGMP visit compared to initial visit.
Figure 6.
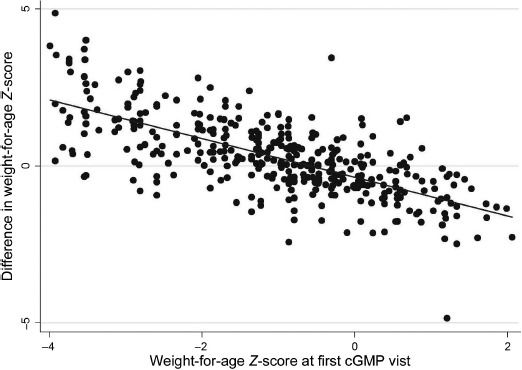
WFA Z-score differences: Evaluation visit compared to initial cGMP visit.
Province
Compared with Kabul, Herat had statistically similar strengths of associations in three of the four analyses and a statistically significant greater association in the controlled analysis for the last cGMP visit. In the uncontrolled analysis for the evaluation visit, when compared to Kabul, Takhar demonstrated a 1.22 (95% CI 0.76, 1.69) increase in WFA Z-score. Likewise for Bamyan, there was a 0.81 (95% CI 0.39, 1.24) increase in WFA Z-score, and Jawzjan showed a 0.76 (95% CI 0.26, 1.27) increase in WFA Z-score. Controlled analyses for the evaluation visit demonstrated similar associations for these provinces. Slightly reduced positive relationships were found in the controlled and uncontrolled analyses for the last cGMP visit.
Attendance
In this evaluation, the mean number of sessions attended by participants was 7.1 (95% CI 6.8, 7.3), representing a mean of 87% (95% CI 85.6, 88.4) of planned cGMP sessions. Although only participants who had attended 50% or more of planned sessions were included in the evaluation, there was a statistically significant positive association between a unit change in the percentage of planned sessions attended and increases in WFA Z-scores for both the evaluation visit and the last cGMP visit. In the uncontrolled analysis, there was an increase of 1.42 (95% CI 0.41, 2.45) WFA Z-scores per unit change in the percentage of sessions attended for the evaluation visit. This association remained significant when controlled for other factors. In the controlled and uncontrolled analyses for the last cGMP visit, these associations were weaker and not statistically significant.
Caretaker literacy
In the uncontrolled analyses, caretaker literacy was associated with a statistically insignificant decrease in WFA Z-scores for both outcome variables. In the controlled analyses, the associations were slightly positive but remained statistically insignificant. Refusal to answer this question was associated with decreased WFA Z-scores in both comparisons. In neither controlled analysis was the association statistically significant.
Sex of the child
Although not statistically significant in uncontrolled analyses, male sex, in controlled analyses, was associated with a statistically significant reduction in WFA Z-score: −0.22 (95% CI −0.43, −0.01) for the evaluation visit and −0.21 (95% CI −0.41, −0.01) for the last visit.
Age of first contact with cGMP programme
The mean age of entry into the cGMP programme for this evaluation was 3.4 months, a minimum of less than one month and a maximum of nine. Age at entry into the programme demonstrated a statistically significant relationship with changes in WFA Z-scores in the controlled analysis for the last cGMP visit but not in any other regression analysis.
Discussion
cGMP programme and nutritional status
We found evidence that the cGMP programme, designed in Afghanistan to be provided by illiterate CHWs in tandem with female FHAG members, was associated with improved nutritional status in children who had attended 50% or more sessions and entered the programme before nine months of age in the five districts where the evaluation was conducted. These children had significantly higher average WFA Z-scores than those who were not enrolled in the programme but lived in neighbouring health post-catchment areas or neighbouring districts, a more positive association than those observed in Honduras and Malawi (Anderson et al., 2009; Schaetzel et al., 2008). In the absence of a supplementary feeding programme, the nutritional status of participant children significantly improved during attendance in this programme, similar to findings in Uganda, Madagascar and China (Alderman, 2007; Galasso & Umapathi, 2007; Li et al., 2007) These results suggest that cGMP delivered by illiterate CHWs could contribute to improved nutritional status in Afghan children.
CHW implementation
During this evaluation, CHWs demonstrated to the evaluators their skills in obtaining appropriate weights and correctly categorising children's weight gain, using simple pictorial tools. The mean WFA Z-scores obtained during the evaluation were similar to those from the last cGMP visit, even though the evaluation visit, 40% of the time, was one month later than the last entry in the cGMP card. The retrospective design of this evaluation did not allow for evaluation of the accuracy of the CHWs initial WFA measurements when they were less experienced and as a consequence, it is possible that measurement error may have inflated or deflated the change in WFA Z-scores during the cGMP programme. In this programme, monthly monitoring reports illustrated that 67% of caretakers of children who had not gained weight were counselled, and a smaller proportion than that was found in Honduras but higher than in other countries (Anderson et al., 2009; Schaetzel et al., 2008; World Bank, 2006). With maturation of the programme, counselling could improve and result in even higher nutritional gains.
Acceptability of cGMP programme by communities
The programme was designed to enable illiterate CHWs to provide services to illiterate caretakers in village settings or homes, and as such, this programme could conceivably facilitate access to this promotional activity by the majority of women in Afghanistan. We believe that this programme was accepted by communities because of the extensive community consultation and the high levels of participation amongst targeted children early in the programme. Most of the non-participants had not participated because of the absence of a nearby programme. Although 36% of the non-participants indicated a lack of belief in the helpfulness of the cGMP programmes, they had never been exposed to one.
Factors associated with improved nutrition
The finding that low baseline WFA Z-score was the most influential factor associated with WFA Z-score improvements could suggest that catch-up growth in this programme is possible even in the absence of supplementary feeding. The finding that higher baseline WFA Z-scores were associated with fall behind growth or no change in growth suggests that initial WFA Z-score may be interpreted as controlling for ‘regression to the mean’. Quantifying the change in WFA Z-scores beyond ‘regression to the mean’ – the change that could be attributed to the cGMP programme – would require having obtained baseline WFA Z-scores for controls and comparison, between participants and controls, of changes in WFA Z-scores as a function of baseline nutritional status. This study design would have been ethically challenging in the absence of offering treatment to controls with low baseline values. It is also possible that these associations were affected by measurement error early in the programme; an effect that, with experience, later diminished. The important question of whether the demonstrated growth is sustained would require a long-term evaluation.
The lack of associations between nutritional outcomes and caretaker literacy and the slightly positive relationship with female sex of the child were encouraging findings suggesting that the cGMP programme was designed for equitable access. The association with female children relative to males likely stems from the female-centred efforts that have been ongoing in Afghanistan for over a decade. Caretaker illiteracy appeared to be unrelated to whether the child's nutritional status improved or not, contrary to findings in Madagascar and in a previous study in Kabul, where literacy was an important predictor of improved nutrition (Galasso & Umapathi, 2007; Mashal et al., 2008). The vast majority of the caretakers were illiterate, suggesting that access and, consequently, any improvement in their children's nutritional status, was dependent on other factors.
The Afghan cGMP programme, because it occurs in villages and in homes, facilitates regular attendance. This evaluation suggested that incremental attendance above 50% of planned visits appeared to be associated with improved nutritional status. Since 70% of 5550 children registered in the cGMP programmes had attended 50% or more of planned sessions at an early stage of programme development, the potential impact of this programme could be significant. The improvement in nutritional status per attended session further supports the importance of regular attendance, also demonstrated in Central America and Africa (Alderman, 2007; Galasso & Umapathi, 2007; Schaetzel et al., 2008).
The provinces most associated with improved WFA Z-scores, even when controlled for caretaker and child characteristics, were Takhar, and Jawzjan, two of the three most rural provinces with difficult transportation infrastructure. Programmatic factors that could lead to poorer nutritional outcomes did not appear to explain the observation. Turnover in the implementing NGO and staff occurred in all districts. Although sex ratios of trained CHWs differed across provinces, only female CHWs were involved in the weighing sessions of the cGMP programme, with the exception of Bamyan. Implementation of additional nutritional programmes, such as community IMCI with an improved nutrition module, a kitchen gardening programme, a positive deviance hearth, did occur in 2010 in Herat, Bamyan, and Jawzjan; however, these were small scale and did not occur in Kabul or Jawzjan.
Limitations
This evaluation had no established standard to continuously verify the work done by CHWs, and it is possible that the initial weights recorded by the CHWs resulted in some measurement error. This may have magnified or reduced the association between low initial WFA Z-scores and Z-score improvements. The similarity in mean WFA Z-scores at evaluation visits and those at the last cGMP visit suggests that experienced CHWs were able to adequately perform their duties. Another potential error could have resulted from the CHWs' weighing of clothed children. Since light clothing was worn in the summer when the evaluation occurred and diapers are uncommon in rural Afghanistan, this effect is likely to be small.
Due to time and financial constraints, selection of control areas in close geographic proximity was used for matching instead of exploring caretakers' experiences with food security, wealth, transportation and security. We believe that the selection of controls was suitable given the circumstances. Potential differences between participants and matched comparisons living near neighbouring health posts or in nearby districts may have introduced some bias, the effect of which is unknown. The nutritional changes in WFA Z-scores in participants lend some support to the assumption of similar characteristics in these two groups.
Evaluating the potential effect of a small number of sporadic additional nutritional programmes that may have confounded these results by providing knowledge, resources and skills to the CHWs and caretakers is beyond the scope of this assessment.
Conclusions
This evaluation suggests that the cGMP programme in Afghanistan for illiterate women has the potential to contribute to improving nutrition, specifically in underweight children of either sex who enter the programme at less than nine months of age and attend 50% or more sessions. Given the potential benefits in child nutrition and the expected cost savings of cGMP over facility-based nutrition efforts, expansion of the programme appears warranted.
Our findings suggest that a long-term evaluation of this programme should be conducted to assess sustained growth in matched pairs of children up to five years of age and include a more extensive inquiry into food security, wealth and other potentially confounding factors. In the future, given the successful implementation thus far, stunting may become feasible to assess by measuring participants' height. Although this programme demonstrated substantial participation by illiterate women in their villages, research to define the critical distance and other social issues that prevent women from participating in a health promotional programme such as cGMP would be of practical value.
Acknowledgements
We would like to acknowledge the contributions of Dr Said Alishah Alawi, MOPH, and Dr Najibullah and Dr Farooq, USAID/BASICS. Dr Barbara Timmons of MSH provided final editing of the paper. We extend special thanks to the Afghan children, their mothers and other caretakers who so willingly participated in the programme and evaluation.
Funding
The US Agency for International Development (USAID) funded the survey under the Basic Support for Institutionalizing Child Survival (BASICS) Project, contract number [GHA-I-00-04-00002-00], in collaboration with the MOPH's Child and Adolescent Health Department. The fieldwork was undertaken by the NGOs that implement the BASIC package of health services: Agency for assistance and development of Afghanistan in Bamyan, Care of Afghan Families in Takhar, Coordination of Humanitarian Assistance in Herat, MOVE Welfare Organisation in Jawzjan and STEP Health and Development Organisation in Kabul. Dr Abdul Ahmad Roshan and Mr Hafizullah Mahmudi of the Tech-Serve Project were funded by USAID and managed by MSH-provided assistance in developing the database and analysis routines.
References
- Afghan Ministries of Agriculture & Public Health. Healthy food, happy baby, lively family—improved feeding practices and recipes for Afghan children and mothers. Kabul: United Nations Food & Agriculture Organization; 2008. [Google Scholar]
- Afghan Ministry of Public Health. Basic package of health services. Kabul: Author; 2005. [Google Scholar]
- Afghan Ministry of Public Health and Centers for Disease Control. Afghanistan national nutrition survey: 2004. Atlanta, GA: CDC; 2009. [Google Scholar]
- Afghan Public Health Institute, Central Statistics Office, ICF Macro, IIHMR, & WHO/EMRO. Afghanistan mortality survey 2010. Calverton, MA: Author; 2011. [Google Scholar]
- Alderman H. Improving nutrition through community growth promotion: Longitudinal study of the nutrition and early child development program in Uganda. World Development. 2007;35:1376–1389. doi: 10.1016/j.worlddev.2007.04.003. [DOI] [Google Scholar]
- Anderson M. A., Chintu M., Kapulula P. Assessment of USAID/BASICS’ community essential nutrition actions program in Malawi. Arlington, VA: Basic Support for Institutionalizing Child Survival (USAID/BASICS) for the United States Agency for International Development (USAID); 2009. [Google Scholar]
- Ashworth A., Shrimpton R., Jamil K. Growth monitoring and promotion: Review of evidence of impact. Maternal and Child Nutrition. 2008;4:86–117. doi: 10.1111/j.1740-8709.2007.00125.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BASICS II. Tools for operationalizing essential nutrition actions. Arlington, VA: USAID; 2003. [Google Scholar]
- BASICS II. Using essential nutrition actions to accelerate coverage with nutrition interventions in high mortality settings. Arlington, VA: USAID; 2004. [Google Scholar]
- Central Statistics Office and UNICEF. Afghanistan multiple indicator cluster survey 20100–2011: Final report. Kabul: Author; 2012. [Google Scholar]
- Contreras A., Drabo Y., Shimp L., de Quinteros P., Linares M. A., Mbaye M., Alvarado V. Operationalizing key family practices for child health and nutrition at scale: The role of behaviour change. Arlington, VA: BASICS/USAID; 2004. [Google Scholar]
- de Onis M., Blössner M. WHO global database on child growth and malnutrition. Geneva: Program of Nutrition World Health Organization; 1997. [DOI] [PubMed] [Google Scholar]
- Engle P., Black M., Behrman J., Cabral de Mello M., Gertler P., Kapiriri L., Eming Young M. Strategies to avoid the loss of developmental potential in more than 200 million children in the developing world. Lancet. 2007;369:229–242. doi: 10.1016/S0140-6736(07)60112-3. [DOI] [PubMed] [Google Scholar]
- Fiedler J. L. The Nepal national vitamin a program: Prototype to emulate or donor enclave? Health Policy & Planning. 2000;15:145–156. doi: 10.1093/heapol/15.2.145. [DOI] [PubMed] [Google Scholar]
- Future Generations. Afghan women improving health. 2006. Unpublished report.
- Galasso E., Umapathi N. Impact evaluation series; no. IE 19; Policy Research working paper, No. WPS 4424. Washington, DC: World Bank; 2007. Improving nutritional status through behavioral change: Lessons from Madagascar. [Google Scholar]
- Gartner A., Maire B., Kameli Y., Traissac P., Delpeuch F. Process evaluation of the senegal-community nutrition project: An adequacy assessment of a large scale urban project. Tropical Medicine and International Health. 2006;11:955–966. doi: 10.1111/j.1365-3156.2006.01644.x. [DOI] [PubMed] [Google Scholar]
- Grantham-McGregor S., Bun Cheung Y., Cueto S., Glewwe P., Richeter L., Strupp B. Developmental potential in the first 5 years for children in developing countries. Lancet. 2007;369:60–70. doi: 10.1016/S0140-6736(07)60032-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levitt E. UNICEF, & Afghan Ministry of Public Health. Growth monitoring & promotion in Afghanistan: A review of current policy and practice. Kabul: Ministry of Public Health; 2005. [Google Scholar]
- Li Y., Hotta M., Shi A., Yin J., Guo G., Kawata K., Ushijima H. Malnutrition improvement for infants under 18 months old of Dai minority in Luxi, China. Pediatrics International. 2007;49:273–279. doi: 10.1111/j.1442-200X.2007.02349.x. [DOI] [PubMed] [Google Scholar]
- Mashal T., Takano1 T., Nakamura K., Kizuki M., Hemat S., Watanabe M., Seino K. Factors associated with the health and nutritional status of children under 5 years of age in Afghanistan: Family behaviour related to women and past experience of war-related hardships. BMC Public Health, 2008;8:301–314. doi: 10.1186/1471-2458-8-301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pelletier D. The relationship between child anthropometry and mortality in developing countries: Implications for policy, programs and future research. Journal of Nutrition. 1994;124:2047S–2081S. doi: 10.1093/jn/124.suppl_10.2047S. [DOI] [PubMed] [Google Scholar]
- Rifkin S., Hewitt G., Draper A. Community participation in nutrition programs for child survival and anemia. London: University of Westminster; 2007. [Google Scholar]
- Schaetzel T., Griffiths M., Del Rosso J. M., Plowman B. Evaluation of the AIN-C program in Honduras. Arlington, VA: Basic Support for Institutionalizing Child Survival, USAID; 2008. [Google Scholar]
- Tontisirin K., Attig G. A., Winichagoon P. An eightstage process for national nutrition development. Food and Nutrition Bulletin. 1995;16(1):8–16. [Google Scholar]
- UNICEF. Getting to the roots—mobilizing community volunteers to combat Vitamin A deficiency disorders in Nepal. Kathmandu: UNICEF Regional Office for South Asia; 2003. [Google Scholar]
- UNICEF. Best estimates of social indicators for children in Afghanistan. New York, NY: Author; 2005. [Google Scholar]
- UNICEF; UNICEF. Recommendations from a technical consultation. New York, NY: Author; 2008. Experts' consultation on growth monitoring and promotion strategies: Program guidance for a way forward; pp. 1–8. [Google Scholar]
- Victoria C., Adair L., Fall C., Hallal P., Martorelli R., Richter L. Maternal and Child Undernutrition Study Group. Maternal and child undernutrition: Consequences for adult health and human capital. Lancet. 2008;371:340–357. doi: 10.1016/S0140-6736(07)61692-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker S. P., Wachs T. D., Gardner J., Lozoff B., Wasserman G., Pollitt E. International Child Development Working Group. Child development: Risk factors for adverse outcomes in developing countries. Lancet. 2007;369:145–157. doi: 10.1016/S0140-6736(07)60076-2. [DOI] [PubMed] [Google Scholar]
- Walker S. P., Wachs T. D., Grantham-McGregor S., Black M. M., Nelson C. A., Huffman S. L., Richter L. Inequality in early childhood: Risk and protective factors for early child development. Lancet. 2011;378:1325–1338. doi: 10.1016/S0140-6736(11)60555-2. [DOI] [PubMed] [Google Scholar]
- World Bank. Repositioning nutrition as central to development: A strategy for large-scale action. Washington, DC: Author; 2006. [Google Scholar]


