Abstract
Objective
The best combination of questions to define asthma in epidemiological asthma studies is not known. We summarized the operational definitions of asthma used in prevalence studies and empirically assess how asthma prevalence estimates vary depending on the definition used.
Methods
We searched the Thomson Reuters ISI Web of knowledge and included (1) cross-sectional studies (2) on asthma prevalence (3) conducted in the general population and (4) containing an explicit definition of asthma. The search was limited to the 100 most-cited papers or published since January 2010. For each paper, we recorded the asthma definition used and other variables. Then we applied the definitions to the data of the Portuguese National Asthma survey (INAsma) and of the 2005–2006 National Health and Nutrition Examination Survey (NHANES) computing asthma prevalence estimates for the different definitions.
Results
Of 1738 papers retrieved, 117 were included for analysis. Lifetime asthma, diagnosed asthma and current asthma were defined in 8, 12 and 29 different ways, respectively. By applying definitions of current asthma on INAsma and NHANES data, the prevalence ranged between 5.3%-24.4% and 1.1%-17.2%, respectively.
Conclusions
There is considerable heterogeneity in the definitions of asthma used in epidemiological studies leading to highly variable estimates of asthma prevalence. Studies to inform a standardized operational definition are needed. Meanwhile, we propose a set of questions to be reported when defining asthma in epidemiological studies.
Keywords: Asthma, Definition, Epidemiology, Prevalence, Review
Introduction
The World Health Organization recommends assessing population needs concerning chronic respiratory diseases to better define adequate health policies [1]. Epidemiological studies at a population level, and prevalence studies in particular, are essential for this purpose.
The main multinational studies on asthma prevalence are the European Community Respiratory Health Survey (ECRHS) in adults [2], and the International Study of Asthma and Allergies in Childhood (ISAAC) in children and adolescents [3]. The European Union–funded Global Allergy and Asthma European Network (GA2LEN) recently conducted a large survey on the prevalence of airway and allergic diseases, built mainly on the questions and definitions used in the ECRHS [4].
Although the definitions used to diagnose asthma has a great impact on prevalence estimates [5], a standardized operational definition of asthma is still lacking. Asthma should ideally be defined by a combination of symptoms, clinical diagnosis, pulmonary function tests and studies of either bronchial hyperresponsiveness (BHR) or reversibility of airflow obstruction [6-8]. However, this is rarely feasible. In fact, in the context of population studies, only a few have combined the use of an initial symptoms questionnaire followed by clinical assessment including lung function tests in subsamples of symptomatic and asymptomatic individuals [2,3].
The aim of this paper is 1) to provide an overview of the operational definitions of asthma used in recent prevalence studies and 2) to empirically assess the impact of the definition used on the prevalence of asthma estimates using data from the first Portuguese National Asthma survey, Inquérito Nacional sobre Asma (INAsma) [9] and National Health and Nutrition Examination Survey (NHANES) 2005–2006 [10]. Based on this approach we propose a set of questions to be used when defining asthma in epidemiological studies, until a standardized operational definition based on prospective data can be established.
Methods
Literature search strategy and inclusion criteria
We performed a systematic literature search of the Thomson Reuters ISI Web of Knowledge. The initial search targeted papers with the terms “asthma” and “prevalence” in the title and the final selection included (i) cross-sectional studies (ii) on asthma prevalence (iii) conducted in the general population.To have a comprehensive overview of the definitions of asthma, with both the most recent definitions and most cited ones, we had two criteria in the papers selection: 1) The search was limited to the studies published between January 2010 and October 2013 and 2) the 100 most-cited papers on the topic were included in the initial search (Figure 1).
Figure 1.
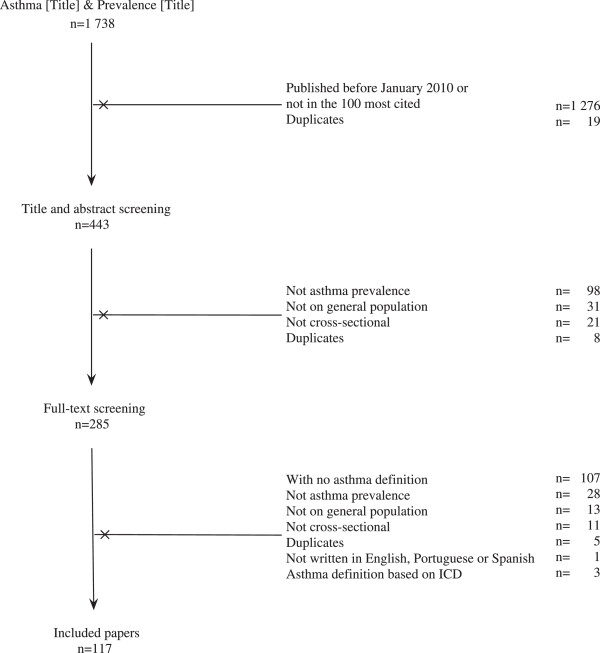
Study selection. From the 1 738 papers retrieved from the Web of Knowledge using the terms asthma and prevalence in the title; 117 were finally included in the study.
Papers written in languages other than English, Portuguese, Spanish or French were excluded, as were those without an explicit definition of asthma or with definitions of asthma based on the International Classification of Diseases (ICD).
Data extraction from published studies
Papers were screened by a single author (AS-S) in two phases (title and abstract and full-text screening) to exclude duplicates and articles that did not meet the eligibility criteria. Papers satisfying the inclusion criteria were examined and data on country, number and age of participants, site of screening, questionnaire used, prevalence value and 95% confidence interval (CI) and definition of asthma were recorded on a purpose-designed form. Doubts regarding the inclusion of papers and data extraction were clarified in agreement with a second investigator.
Epidemiologic studies datasets
The Inquérito Nacional sobre Asma (INAsma) was conducted in 2010 under the auspices of the Portuguese Health Directorate and estimated a prevalence of current asthma (defined as affirmative to the question “Have you ever had asthma?” and at least one of 3 symptoms in the last 12 months: wheezing, waking with breathlessness or having an asthma attack) of 6.8% for the Portuguese population [9]. The INAsma survey comprised two phases: estimation of the prevalence of current asthma and estimation of the proportion of asthmatic patients with controlled disease. The INAsma survey and current study were reported in accordance with the STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) statement guidelines [11].
The National Health and Nutrition Examination Survey (NHANES) 2005–2006 assessed the health and nutritional status of the United States population. And estimated a prevalence of asthma (defined as affirmative to the following questions: 1) Has a doctor or other health professional ever told you that you have asthma? 2) Do you still have asthma?) of 8.8% for the U.S. population [12].
Further details on databases can be found in Additional file 1.
Data analysis
For each asthma definition recorded, we presented the corresponding prevalence value and 95% CI (if available) and computed the proportion of individuals with asthma using data from the INAsma survey and NHANES 2005–2006.
The definitions found were reproduced as they appeared in each paper and were grouped into 3 general subgroups: (i) current asthma (if the definition included current asthma features such as symptoms, current use of medication or the “still have asthma” expression); (ii) diagnosed asthma (if the definition included an asthma diagnosis by a health care professional or ever use of medication for asthma, but not any current asthma feature) and (iii) lifetime asthma (if the definition included having ever had asthma, but not any current asthma feature or asthma diagnosis).
Statistical analyses were performed using IBM SPSS Statistics v21 (2012 SPSS Inc., IBM Company, Chicago, US). The two phases of INAsma comprises data from 6 257 participants, both males and females from 0 to 98 years old. NHANES 2005–06 comprises data from 10 348 participants both males and females from 0 to 150 years old. Using the two phases of INAsma and NHANES 2005–2006 data, we estimated the proportion of individuals with 95% CI with asthma for each of the definitions in all applicable cases and when the necessary data were available.The elements used in each paper to define current asthma were plotted in a diagram (Figure 2). The size of the circles is proportional to the number of definitions in which the element is used. Different colors were attributed to definition elements depending if they were related to symptoms in the last 12 months, lung function tests or to physician diagnosis. Definitions elements were connected in the sequence established by the definition in each study. The number of times each connection was used is also indicated.
Figure 2.
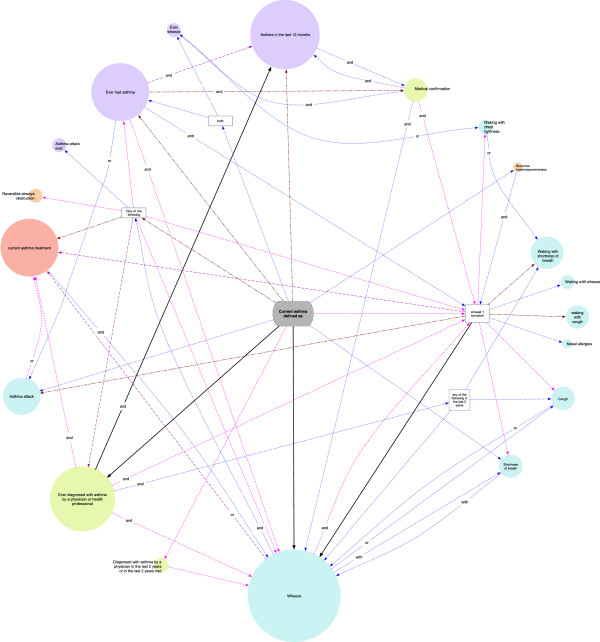
Elements of the definitions of “Current asthma” connected in the order established by each studies. Symptoms in the last 12 months are represented in blue, lung function tests in orange and physician diagnosis in green. The size of each element is proportional to the number of definitions using the element. The color of the lines indicates the number of times each connection was used: once (blue), twice (pink), three times (purple), four to eight times (red) and more than ten times (black). To simplify the diagram, breathlessness and dyspnea were considered the same.
Results
Of the 1738 papers retrieved from the Web of Knowledge database, 117 were included for analysis (Figure 1). The characteristics of the studies included are summarized in Additional file 2 and 3. They described prevalence studies conducted all over the world, on children (27.4%), on adolescents (10.3%), on children and adolescents (25.6%), on adults (25.6%), on elders (1.7%) and on all population(8.5%). Several questionnaires were applied, but the most common one was the ISAAC questionnaire, used in 45.5% of studies.
Lifetime asthma was defined in 34 papers, diagnosed asthma in 54 and current asthma in 61 (see Additional file 4). The 3 subgroups were defined in 8, 12 and 29 different ways, respectively (Tables 1 and 2).The definition of current asthma in each paper was based on a combination of elements. The most common elements were “wheeze in the last 12 months” (in 30 definitions) and “ever diagnosed with asthma by a physician or health professional” (in 21 definitions) (Figure 2). “Current asthma treatment” was used in 12 definitions. Other common symptoms were “shortness of breath at rest” (n = 8), “asthma attack” (n = 7), “shortness of breath/dyspnea” (n = 4), “nocturnal cough” (n = 4) and “cough” (n = 3) in the last 12 months. Only 3 papers used “bronchial hyperresponsiveness” or “reversibility of airflow obstruction” in their definition of asthma. The most common combination used to define current asthma was “Ever diagnosed with asthma by a health professional” together with “still have asthma” (n = 13).
Table 1.
Definitions of “current asthma” and prevalence estimates computed using data from INAsma survey (n = 6257) and from NHANES 2009 (n = 10348)
|
Current asthma definition |
INAsma |
NHANES 05/06 |
|---|---|---|
| % [95%CI] | % [95%CI] | |
| Ever had asthma and wheeze in the last 12 months [13] |
9.3 [8.8-10.0] |
n.a. |
| Ever had asthma and this was confirmed by a physician and at least one in the last 12 months: wheeze, waking with tightness in the chest, waking with breathlessness, waking with cough [14] |
8.5 [7.7-9.3]* |
n.a. |
| Ever had asthma and at least one of 3 symptoms in the last 12 months: wheezing, waking with breathlessness or having an asthma attack [9] |
10.3 [9.5-11.0] |
n.a. |
| Ever had asthma and still have asthma [15,16] |
n.a. |
n.a. |
| Ever had asthma and was this confirmed by a physician and wheeze and/or taking medication(s) for asthma or wheezing in the past 12 months [17] |
n.a. |
n.a. |
| At least one of the following: 1) Ever had asthma and was confirmed by a doctor and still have asthma or 2) significant bronchodilator response according to reversibility [18] |
n.a. |
n.a. |
| Ever had asthma and still have asthma and was confirmed by a physician [19] |
n.a. |
n.a. |
| At least one of the following: 1) Ever had asthma and wheezing in the last 12 months or 2) wheezing 4 times or more during the last 12 months or 3) physician diagnosis and wheezing in the last 12 months or 4) current use of inhalation steroids [20] |
n.a. |
n.a. |
| Diagnosed with asthma by a physician and wheeze in the last 12 months [21] |
7.6 [6.9-8.3]* |
1.7 [1.5-1.9] |
| Diagnosed with asthma by a physician and currently taking asthma medication [22] |
7.4 [6.7-8.1]* |
1.1 [0.9-1.3] |
| Diagnosed with asthma by a physician and use of asthma medication in the last 12 months and cough or wheeze in the last 12 months [23] |
5.3 [4.7-5.9]† |
n.a. |
| Diagnosed with asthma by a physician and at least one: currently taking asthma medication, attacks of shortness of breath or recurrent wheeze in the last 12 months [24] |
6.3 [5.6-6.0]*,‡ |
n.a. |
| Diagnosed with asthma by a physician and still have asthma [25-37] |
n.a. |
8.4 [7.9-8.4] |
| Diagnosed with asthma by a physician and any of the following in the previous 2 years: wheezing following a common cold, dyspneal feeling at night or early in the morning, cough or wheeze during exercise [38] |
n.a. |
n.a. |
| Physician stated that (you) had asthma in the last 2 years or on 2 or more separate occasions had wheezing in the last 2 years [39,40] |
n.a. |
n.a. |
| At least one of the following: 1) Diagnosed with asthma by a physician and at least 1 symptom in the last 12 months: wheeze, wheezes with attacks of shortness of breath, nocturnal attacks of shortness of breath, use of asthma medication or 2) reversible airways obstruction [41] |
n.a. |
n.a. |
| Wheeze in the last 12 months [42-54] |
22.9 [21.9-23.9] |
12.9 [12.2-13.5] |
| Wheeze in the last 12 months or currently taking asthma medication [55] |
24.4 [23.3-25.5] |
12.9 [12.2-13.5] |
| Current wheeze and 1 of the following: 1) ever had an asthma attack or 2) ever had asthma or 3) taking medication(s) for asthma or wheeze [56] |
9.3 [8.6-10.0]** |
n.a. |
| Asthma attack or currently taking asthma medication [2] |
9.0 [8.3-9.7] |
n.a. |
| At least one in the last 12 months: Waking at night by shortness of breath, had an asthma attack or currently taking any medicines (including inhalers, aerosols or tablets) for asthma [57] |
14.5 [13.6-15.4] |
n.a. |
| At least one of the following symptoms: wheeze in the last 12 months, coughing constantly for more than 3 weeks in any time in your life, attack of asthma in the last 12 months, or nasal allergies including hay fever in the last 12 months [58] |
n.a. |
17.2 [16.5-17.9]‡‡ |
| Wheeze in the last 12 months and at least 1 of the following in the last 12 months: any lifetime episode of asthma; wheezing during physical exercise; four or more episodes of wheezing in the previous year; or waking at night at least once a week due to wheezing [59] |
n.a. |
8.8 [8.3-9.3]†† |
| Asthma in the last 12 months [60-66] |
n.a. |
n.a. |
| Had a condition which causes difficulty in breathing, with wheezing noises in the chest in the last 12 months [67] |
n.a. |
n.a. |
| At least one of the following: 1) any symptom in the last 12 months: wheezing, shortness of breath, coughing bouts or dyspnea or 2) previous physician-based diagnosis of asthma or 3) use of medication for asthma [68] |
n.a. |
n.a. |
| Both: 1) Ever whistling sound from chest or chest tightness or breathlessness in the morning, and 2) having suffered from asthma or having an attack of asthma in the past 12 months or using bronchodilators [69] |
n.a. |
n.a. |
| Bronchial hyperresponsiveness and asthma symptoms (wheeze, night cough, or shortness of breath at rest) within the previous 12 months [70] |
n.a. |
n.a. |
| At least one of the following: 1) Recent symptoms (wheeze or nocturnal cough) or 2) asthma medication use [71] | 39.5 [38.2-40.7] | n.a. |
*Questions related to this variable were only asked in the second phase of INAsma; therefore the total number of participants was corrected for non-response in phase II (total n = 4949). n.a. – not available – Questions related to this variable were not asked in the INAsma survey. †“Cough” was interpreted as “waking with cough” for estimation purposes. ‡The variable was considered as “diagnosed with asthma by a physician and currently taking asthma medication and attacks of asthma or wheeze in the last 12 months” for estimation purposes. ††The variable was considered without the symptom “any lifetime episode of asthma” for estimation purposes. ‡‡The variable was considered without the symptom “attack of asthma in the last 12 months” for estimation purposes. **“ever had an asthma attack” was considered as “ever had an asthma attack in the last 12 months” for estimation purposes.
Table 2.
Definitions of “Lifetime asthma” and “Diagnosed asthma” and prevalence estimates computed using data from INAsma survey (n = 6257) and from NHANES 2009 (n = 10348)
|
Definition |
INAsma |
NHANES 05/06 |
|---|---|---|
| % [95%CI] | % [95%CI] | |
|
Lifetime asthma |
|
|
| Ever had asthma [3,9,14,16,17,24,51,54,66,72-89] |
14.5 [13.6-15.4] |
n.a. |
| Wheeze in the last 12 months or ever had asthma [90] |
28.1 [27.0-29.2] |
n.a. |
| Had a condition which causes difficulty in breathing, with wheezing noises in the chest [67] |
n.a. |
n.a. |
| Self-report of dyspnea and nocturnal dyspnea associated with wheezing, or attacks of dyspnea with wheezing, or physician-diagnosed asthma [91] |
n.a. |
n.a. |
| Ever had wheeze [92] |
n.a. |
n.a. |
| Report of simultaneous dyspnea and wheezing in the absence of upper respiratory infections [93] |
9.5 [8.8-10.2] |
n.a. |
| Ever had wheeze and cough more than other (children) and breathlessness at rest or exercise [94] |
n.a. |
n.a. |
| Ever had asthma and/or one of the following: wheeze, cough or acute shortness of breath due to external factors [95] |
n.a. |
n.a. |
|
Diagnosed asthma |
|
|
| Ever diagnosed with asthma by a physician or health professional [21,23,24,26,28,29,52,66,85-88,91,92,94,96-118] |
9.3 [8.5-10.2]* |
13.4 [12.7-14.1] |
| Diagnosed with asthma by a physician or wheezing in the last 12 months, apart from cold or the flu [119] |
20.1 [19.0-21.2]* |
24.5 [23.6-25.3]† |
| Diagnosed with asthma by a physician in the last 12 months [120,121] |
n.a. |
n.a. |
| Ever had asthma and medical confirmation [14,17,38,122] |
9.3 [8.5-10.1]* |
n.a. |
| Ever had asthma and use of medication for asthma [9] |
8.2 [7.5-8.9] |
n.a. |
| Ever diagnosed with asthma by a physician or health professional and Ever stayed over night in the hospital for wheezing [123] |
2.5 [2.1-2.9]* |
n.a. |
| Ever diagnosed with asthma by a physician or health professional and use of medication for asthma [47] |
7.4 [6.7-8.1]* |
1.1 [0.9-1.3] |
| History of asthma and physical examination and skin-prick tests and peak flow measurements [53] |
n.a. |
n.a. |
| History of asthma and physical signs of asthma (rhonchi or chest deformity) [124] |
n.a. |
n.a. |
| Diagnosed with asthma by a physician or symptoms (presence of wheezing, history of dry cough, recurrent wheeze, dyspnea/ recurrent difficulty in breathing or recurrent chest tightness) with clinical assessment [125] |
n.a. |
n.a. |
| Recurrent wheezing episodes, clinically confirmed by a physician, exactly a pediatrician or a pediatric pulmonologist [126] |
n.a. |
n.a. |
| Physician stated that (you) had asthma in the last 2 years, on 2 or more separate occasions had wheezing in the last 2 years, or had asthma prior to 2 years ago or on 2 or more separate occasions had wheezing prior to 2 years ago [39,40] | n.a. | n.a. |
*Questions related to this variable were only asked in the second phase of INAsma; therefore the total number of participants was corrected for non-response in phase II (total n = 4949). n.a. – not available – Questions related to this variable were not asked in the INAsma survey. †“apart from cold or the flu” was not considered for estimation purposes.
Most of the papers using “wheeze in the last 12 months” as an element to define current asthma described the prevalence of asthma in children, adolescents or both (n = 21,70% - data not shown).
The prevalence of asthma estimates based on the applicable definitions of current asthma ranged between 5.3% and 39.5% in the Portuguese population for the 13 (45%) applicable definitions and between 1.1% and 17.2% in U.S. population for the 7(24%) applicable definitions (Table 1).
The definitions varied even in papers that used the same questionnaire. For instance, eight different definitions were used in 18 studies of the ISAAC questionnaire (see Additional file 5 and Figure 3). Using the eight variants of the definition of current asthma based on the ISAAC questionnaire, the proportion of children and adolescents with asthma estimated from the INAsma data varied between 9.0% and 20.5% (Figure 3).
Figure 3.
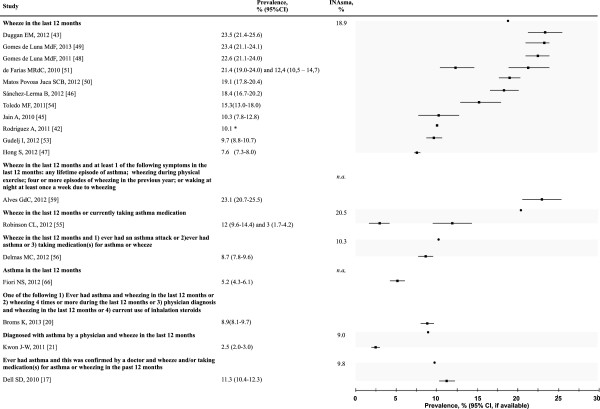
Prevalence of asthma according to several definitions of the “Current asthma” based on ISAAC questionnaire. Prevalence estimates for Portuguese children aged 6, 7, 13 and 14 years old were computed using data from the INAsma survey (also see Additional file 5). *95% CI not available. n.a. – not available. Proportion of people with asthma using the INAsma data are represented by •; prevalence stated in other studies are represented by ■. Lines represent the CI (when available). Shades gather the values for the same definition.
Concerning definitions of lifetime asthma, three definitions could be used with data from INAsma with prevalence estimates ranging between 9.5% and 28.1%; none of the definitions were applicable to NHANES data (Table 2).
Discussion
The operational definitions of asthma varied extensively among studies and do not allow to compare estimates between studies, even if similar data collection methods were used. Additionally, when we applied the definitions of current asthma to two datasets from population studies, we found that the prevalence of asthma ranged from 5.3% to 39.5% in Portuguese population and from 1.1% to 17.2% in U.S. population depending on the definition used. Current asthma was most frequently defined by the combination of “ever diagnosed with asthma by a health professional” with “still having asthma”. Wheeze was the most frequently used current symptom, especially in children.
The Web of Knowledge was the only database used for the search. While this may be seen as a limitation of the present study, this approach allowed the inclusion of the most-cited papers on asthma prevalence conducted in both children and adults.
The wide variability of the estimates computed for different definitions is in accordance with the results of a study in children [5]. The variety of definitions identified in the present study illustrates both the difficulty of identifying people with asthma by questionnaire and the difficulty of establishing an internationally accepted definition, even when the same questionnaire is used.
The few published studies that have validated asthma questionnaires, used BHR tests or a physician’s diagnosis as gold-standard [8,127,128]. These reports concluded that questions on wheeze are the most sensitive and questions such as “Have you ever had asthma?” or questions on “waking with attacks of shortness of breath” and “morning tightness” have high specificity for asthma [8,127,128]. In our review, wheeze was the most commonly used symptom, especially in children. However, it should be noted that a diagnosis of asthma based on wheeze is only accurate during some stages of childhood [129,130] and the use of a comprehensive description of asthma symptoms might reduce the risk of misclassification of asthma in children. Pekkanen and coworkers also suggested that definitions using a combination of asthma symptoms increase specificity against self-report of ever having asthma and BHR and that the use of a continuous asthma score based on asthma symptoms increases both the specificity and power for predicting asthma [7].
The present study shows that prior asthma diagnosis by a health professional was commonly used to define asthma. However, in some countries and cultural contexts, the use of prior diagnosis may lead to an under- or overestimation of asthma prevalence [131]. Attention to this potential problem is especially important in multinational studies and, in fact, ISAAC [3] and ECRHS [2] do not consider a prior diagnosis definitive for asthma.
Standardized definitions are necessary for prevalence comparisons worldwide. This should be achieved by the validation of self-reported features, against objective measure, such as (i) variability of airflow obstruction, reversibility and BHR, (ii) physician classification including current therapy and (iii) persistence of diagnosis at clinical long-term follow-up. By reporting the sensitivity and specificity of different approaches, these validation studies would inform the decision on a standardized operational definition of asthma for epidemiological purposes.Based on the data presented, we propose an initial comprehensive set of questions (Figure 4) that can be used in validation studies while allowing comparisons with previous prevalence studies of asthma. As this is an early step to achieve a standardized definition of asthma, we suggest that at this time, the data items proposed in Figure 4 should be reported separately to increase the inter-study comparability.
Figure 4.
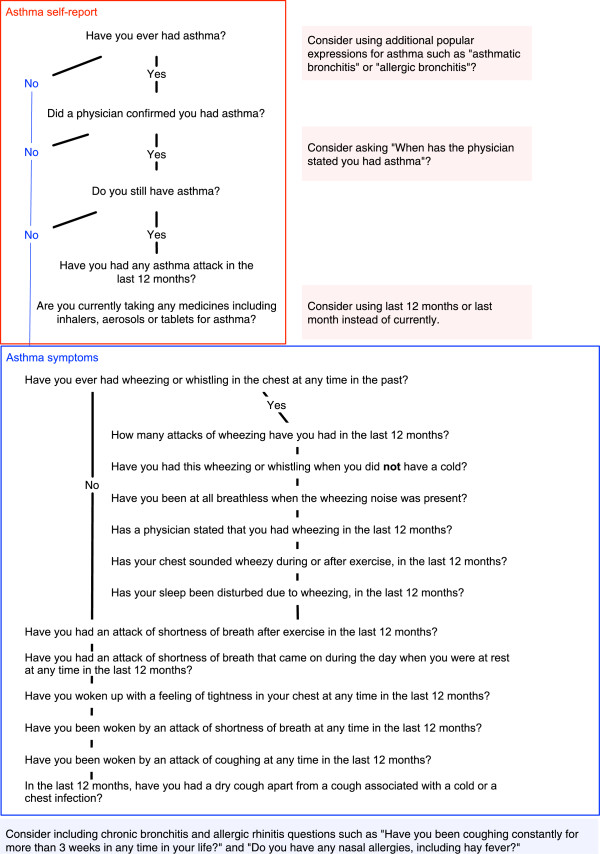
Questions to be asked and independently reported.
Conclusions
The operational definition of asthma has an important effect on estimates of asthma prevalence in epidemiologic studies. There is a need for an accurate standardized operational definition of asthma. To inform this definition it is important to estimate the sensibility and specificity of a set of questions (Figure 4) against reversibility/variability of the airflow obstruction, BHR and clinical assessment.
Abbreviations
BHR: Bronchial hyperresponsiveness; CI: Confidence Interval; ECRHS: European Community Respiratory Health Survey; GA2LEN: Global Allergy and Asthma European Network; ICD-9: International Classification of Diseases; INAsma: Inquérito Nacional sobre Asma (Portugal); ISAAC: International Study of Asthma and Allergies in Childhood; NHANES: National Health and Nutrition Examination Survey (USA).
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
AS-S participated in data collection, analysis and wrote the manuscript draft, LFA participated in study design and reviewed the manuscript, TJ, CRC, MMA and ABA reviewed the manuscript and JB provided critical review during the project and reviewed the manuscript, JAF is responsible for the INAsma project and participated in all stages and tasks of the present study. All authors have read and approved the final manuscript.
Supplementary Material
Databases details.
Summary of the included studies.
Definitions in the ten most cited and the ten most recent papers from the 117 included by Average citations per year at the end of 2013.
Studies presenting three different subgroups of the definition of asthma. Of the 117 papers included, 34 provided a definition for lifetime asthma, 54 for diagnosed asthma and 61 for current asthma; 5 papers defined the three types of asthma.
Summary of studies with Current asthma definitions that used the International Study of Asthma and Allergies in Childhood (ISAAC) questionnaire (n = 18).
Contributor Information
Ana Sá-Sousa, Email: anasasousa@gmail.com.
Tiago Jacinto, Email: tiagoaqjacinto@gmail.com.
Luís Filipe Azevedo, Email: lazevedo@med.up.pt.
Mário Morais-Almeida, Email: mmoraisalmeida@netcabo.pt.
Carlos Robalo-Cordeiro, Email: carlos.crobalo@gmail.com.
António Bugalho-Almeida, Email: bugalho.almeida@netcabo.pt.
Jean Bousquet, Email: jean.bousquet@orange.fr.
João Almeida Fonseca, Email: jfonseca@med.up.pt.
Acknowledgment
This work had financial support of the Sociedade Portuguesa de Alergologia e Imunologia Clínica; Sociedade Portuguesa de Pneumologia and Fundação Ciência e Tecnologia (PTDC/SAU-SAP/119192/2010).
References
- Bousquet J, Khaltaev, Cruz AA. Global surveillance, prevention and control of Chronic Respiratory Diseases: A comprehensive approach. Switzerland: World Health Organization; 2007. [Google Scholar]
- Burney P Chinn C Luczynska C Jarvis D Vermeire P Bousquet J Nowak D Prichard J Marco de R Rijcken B Anto J Alves J Boman G Kesteloot H Nielsen N Paoletti P Variations in the prevalence of respiratory symptoms, selfreported asthma attacks, and use of asthma medication in the European Community Respiratory Health Survey (ECRHS) Eur Respir J 19969687–695.8726932 [Google Scholar]
- Asher MI, Anderson HR, Stewart AW, Crane J, Ait-Khaled N, Anabwani G, Anderson HR, Beasley R, Bjorksten B, Burr ML, Clayton TO, Ellwood P, Keil U, Lai CKW, Mallol J, Martinez FD, Mitchell EA, Montefort S, Pearce N, Robertson CF, Shah JR, Sibbald B, Strachan DP, von Mutius E, Weiland SK, Williams HC, Comm IS. Worldwide variations in the prevalence of asthma symptoms: the International Study of Asthma and Allergies in Childhood (ISAAC) Eur Respir J. 1998;12:315–335. doi: 10.1183/09031936.98.12020315. [DOI] [PubMed] [Google Scholar]
- Bousquet J, Burney PG, Zuberbier T, Cauwenberge PV, Akdis CA, Bindslev-Jensen C, Bonini S, Fokkens WJ, Kauffmann F, Kowalski ML, Lodrup-Carlsen K, Mullol J, Nizankowska-Mogilnicka E, Papadopoulos N, Toskala E, Wickman M, Anto J, Auvergne N, Bachert C, Bousquet PJ, Brunekreef B, Canonica GW, Carlsen KH, Gjomarkaj M, Haahtela T, Howarth P, Lenzen G, Lotvall J, Radon K, Ring J. et al. GA2LEN (Global Allergy and Asthma European Network) addresses the allergy and asthma 'epidemic’. Allergy. 2009;64:969–977. doi: 10.1111/j.1398-9995.2009.02059.x. [DOI] [PubMed] [Google Scholar]
- Van Wonderen KE, Van Der Mark LB, Mohrs J, Bindels PJ, Van Aalderen WM, Ter Riet G. Different definitions in childhood asthma: how dependable is the dependent variable? Eur Respir J. 2010;36:48–56. doi: 10.1183/09031936.00154409. [DOI] [PubMed] [Google Scholar]
- Pekkanen J, Pearce N. Defining asthma in epidemiological studies. Eur Respir J. 1999;14:951–957. doi: 10.1034/j.1399-3003.1999.14d37.x. [DOI] [PubMed] [Google Scholar]
- Pekkanen J, Sunyer J, Anto JM, Burney P. Operational definitions of asthma in studies on its aetiology. Eur Respir J. 2005;26:28–35. doi: 10.1183/09031936.05.00120104. [DOI] [PubMed] [Google Scholar]
- Toren K, Brisman J, Jarvholm B. Asthma and asthma-like symptoms in adults assessed by questionnaires. A literature review Chest. 1993;104:600–608. doi: 10.1378/chest.104.2.600. [DOI] [PubMed] [Google Scholar]
- Sa-Sousa A, Morais-Almeida M, Azevedo LF, Carvalho R, Jacinto T, Todo-Bom A, Loureiro C, Bugalho-Almeida A, Bousquet J, Fonseca JA. Prevalence of asthma in Portugal - The Portuguese National Asthma Survey. Clin Transl Allergy. 2012;2:15–15. doi: 10.1186/2045-7022-2-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Health and Nutrition Examination Survey 2005–2006. [ http://www.cdc.gov/nchs/nhanes/nhanes2005-2006/nhanes05_06.htm]
- von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61:344–349. doi: 10.1016/j.jclinepi.2007.11.008. [DOI] [PubMed] [Google Scholar]
- Gergen PJ, Arbes SJ, Calatroni A, Mitchell HE, Zeldin DC. Total IgE and Asthma Prevalence in the U.S. Population: Results from the National Health and Nutrition Examination Survey (NHANES) 2005–2006. J Allergy Clin Immunol. 2009;124:447–453. doi: 10.1016/j.jaci.2009.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burr ML, Butland BK, King S, Vaughan-Williams E. Changes in asthma prevalence: two surveys 15 years apart. Arch Dis Child. 1989;64:1452–1456. doi: 10.1136/adc.64.10.1452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fukutomi Y, Nakamura H, Kobayashi F, Taniguchi M, Konno S, Nishimura M, Kawagishi Y, Watanabe J, Komase Y, Akamatsu Y, Okada C, Tanimoto Y, Takahashi K, Kimura T, Eboshida A, Hirota R, Ikei J, Odajima H, Nakagawa T, Akasawa A, Akiyama K. Nationwide Cross-Sectional Population-Based Study on the Prevalences of Asthma and Asthma Symptoms among Japanese Adults. Int Arch Allergy Immunol. 2010;153:280–287. doi: 10.1159/000314369. [DOI] [PubMed] [Google Scholar]
- Weitzman M, Gortmaker SL, Sobol AM, Perrin JM. Recent trends in the prevalence and severity of childhood asthma. JAMA. 1992;268:2673–2677. [PubMed] [Google Scholar]
- Crain EF, Weiss KB, Bijur PE, Hersh M, Westbrook L, Stein REK. An estimate of the prevalence of asthma and wheezing among inner-city children. Pediatrics. 1994;94:356–362. [PubMed] [Google Scholar]
- Dell SD, Foty RG, Gilbert NL, Jerret M, To T, Walter SD, Stieb DM. Asthma and allergic disease prevalence in a diverse sample of Toronto school children: results from the Toronto Child Health Evaluation Questionnaire (T-CHEQ) Study. Can Respir J. 2010;17:e1–6. doi: 10.1155/2010/913123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chittleborough CR, Taylor AW, Dal Grande E, Gill TK, Grant JF, Adams RJ, Wilson DH, Ruffin RE. Team NWAHS. Gender differences in asthma prevalence: Variations with socioeconomic disadvantage. Respirology. 2010;15:107–114. doi: 10.1111/j.1440-1843.2009.01638.x. [DOI] [PubMed] [Google Scholar]
- Ekici A, Ekici M, Kocyigit P, Karlidag A. Prevalence of Self-Reported Asthma in Urban and Rural Areas of Turkey. J Asthma. 2012;49:522–526. doi: 10.3109/02770903.2012.677893. [DOI] [PubMed] [Google Scholar]
- Broms K, Norback D, Eriksson M, Sundelin C, Svardsudd K. Prevalence and co-occurrence of parentally reported possible asthma and allergic manifestations in pre-school children. BMC Public Health. 2013;13:764. doi: 10.1186/1471-2458-13-764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwon J-W, Kim B-J, Song Y, Seo J-H, Kim T-H, Yu J, Kim HB, Lee SY, Kim W-K, Kim K-W, Ji H-M, Kim K-E, Kim H, Hong S-J. Changes in the Prevalence of Childhood Asthma in Seoul from 1995 to 2008 and Its Risk Factors. Allergy Asthma Immunol Res. 2011;3:27–33. doi: 10.4168/aair.2011.3.1.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clifford RD, Radford M, Howell JB, Holgate ST. Prevalence of respiratory symptoms among 7-year-old and 11-year-old schoolchildren and association with asthma. Arch Dis Child. 1989;64:1118–1125. doi: 10.1136/adc.64.8.1118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haby MM, Peat JK, Marks GB, Woolcock AJ, Leeder SR. Asthma in preschool children: prevalence and risk factors. Thorax. 2001;56:589–595. doi: 10.1136/thorax.56.8.589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ekerljung L, Andersson A, Sundblad BM, Ronmark E, Larsson K, Ahlstedt S, Dahlen SE, Lundback B. Has the increase in the prevalence of asthma and respiratory symptoms reached a plateau in Stockholm, Sweden? Int J Tuberc Lung Dis. 2010;14:764–771. [PubMed] [Google Scholar]
- Arif AA, Delclos GL, Lee ES, Tortolero SR, Whitehead LW. Prevalence and risk factors of asthma and wheezing among US adults: an analysis of the NHANES III data. Eur Respir J. 2003;21:827–833. doi: 10.1183/09031936.03.00054103a. [DOI] [PubMed] [Google Scholar]
- Barry AC, Mannino DM, Hopenhayn C, Bush H. Exposure to Indoor Biomass Fuel Pollutants and Asthma Prevalence in Southeastern Kentucky: Results From the Burden of Lung Disease (BOLD) Study. J Asthma. 2010;47:735–741. doi: 10.3109/02770903.2010.485661. [DOI] [PubMed] [Google Scholar]
- Oraka E, King ME, Callahan DB. Asthma and Serious Psychological Distress Prevalence and Risk Factors Among US Adults, 2001–2007. Chest. 2010;137:609–616. doi: 10.1378/chest.09-1777. [DOI] [PubMed] [Google Scholar]
- Oraka E, Elizabeth HJ, King ME, Callahan DB. Asthma Prevalence among US Elderly by Age Groups: Age Still Matters. J Asthma. 2012;49:593–599. doi: 10.3109/02770903.2012.684252. [DOI] [PubMed] [Google Scholar]
- Rodriguez MA, Winkleby MA, Ahn D, Sundquist J, Kraemer HC. Identification of population subgroups of children and adolescents with high asthma prevalence - Findings from the Third National Health and Nutrition Examination Survey. Arch Pediatr Adolesc Med. 2002;156:269–275. doi: 10.1001/archpedi.156.3.269. [DOI] [PubMed] [Google Scholar]
- Ma J, Xiao L, Knowles SB. Obesity, insulin resistance and the prevalence of atopy and asthma in US adults. Allergy. 2010;65:1455–1463. doi: 10.1111/j.1398-9995.2010.02402.x. [DOI] [PubMed] [Google Scholar]
- Akinbami LJ, Lynch CD, Parker JD, Woodruff TJ. The association between childhood asthma prevalence and monitored air pollutants in metropolitan areas, United States, 2001–2004. Environ Res. 2010;110:294–301. doi: 10.1016/j.envres.2010.01.001. [DOI] [PubMed] [Google Scholar]
- Akinbami LJ, Moorman JE, Liu X. Asthma prevalence, health care use, and mortality: United States. Natl Health Stat Report. 2005–2009;2011:1–14. [PubMed] [Google Scholar]
- Akinbami LJ, Moorman JE, Bailey C, Zahran HS, King M, Johnson CA, Liu X. Trends in asthma prevalence, health care use, and mortality in the United States. NCHS data brief. 2001–2010;2012:1–8. [PubMed] [Google Scholar]
- Zahran HS, Bailey C, Garbe P. Vital Signs: Asthma Prevalence, Disease Characteristics, and Self-Management Education-United States, 2001–2009 (Reprinted from MMWR, vol 60, pg 547–552, 2011) JAMA. 2011;305:2514–2516. [PubMed] [Google Scholar]
- Moorman JE, Zahran H, Truman BI, Molla MT. Centers for Disease C, Prevention. Current asthma prevalence - United States, 2006–2008. Morbidity and mortality weekly report Surveillance summaries (Washington, DC: 2002) 2011;60((Suppl)):84–86. [Google Scholar]
- Frazier JC, Loveland KM, Zimmerman HJ, Helgerson SD, Harwell TS. Prevalence of Asthma Among Adults in Metropolitan Versus Nonmetropolitan Areas in Montana, 2008. Prev Chronic Dis. 2012;9:E09. [PMC free article] [PubMed] [Google Scholar]
- Coker TR, Kaplan RM, Chung PJ. The Association of Health Insurance and Disease Impairment with Reported Asthma Prevalence in U.S. Children. Health Serv Res. 2012;47:431–445. doi: 10.1111/j.1475-6773.2011.01339.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fukutomi Y, Taniguchi M, Watanabe J, Nakamura H, Komase Y, Ohta K, Akasawa A, Nakagawa T, Miyamoto T, Akiyama K. Time trend in the prevalence of adult asthma in Japan: findings from population-based surveys in Fujieda City in 1985, 1999, and 2006. Allergol Int. 2011;60:443–448. doi: 10.2332/allergolint.10-OA-0282. [DOI] [PubMed] [Google Scholar]
- Anthracopoulos MB, Pandiora A, Fouzas S, Panagiotopoulou E, Liolios E, Priftis KN. Sex-specific trends in prevalence of childhood asthma over 30 years in Patras, Greece. Acta Paediatr. 2011;100:1000–1005. doi: 10.1111/j.1651-2227.2011.02255.x. [DOI] [PubMed] [Google Scholar]
- Anthracopoulos MB, Fouzas S, Pandiora A, Panagiotopoulou E, Liolios E, Priftis KN. Prevalence trends of rhinoconjunctivitis, eczema, and atopic asthma in Greek schoolchildren: four surveys during 1991–2008. Allergy Asthma Proc. 2011;32:56–62. doi: 10.2500/aap.2011.32.3504. [DOI] [PubMed] [Google Scholar]
- Musafiri S, van Meerbeeck J, Musango L, Brusselle G, Joos G, Seminega B, Rutayisire C. Prevalence of atopy, asthma and COPD in an urban and a rural area of an African country. Respir Med. 2011;105:1596–1605. doi: 10.1016/j.rmed.2011.06.013. [DOI] [PubMed] [Google Scholar]
- Rodriguez A, Vaca M, Oviedo G, Erazo S, Chico ME, Teles C, Barreto ML, Rodrigues LC, Cooper PJ. Urbanisation is associated with prevalence of childhood asthma in diverse, small rural communities in Ecuador. Thorax. 2011;66:1043–1050. doi: 10.1136/thoraxjnl-2011-200225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duggan EM, Sturley J, Fitzgerald AP, Perry IJ, Hourihane JOB. The 2002–2007 trends of prevalence of asthma, allergic rhinitis and eczema in Irish schoolchildren. Pediatr Allergy Immunol. 2012;23:464–471. doi: 10.1111/j.1399-3038.2012.01291.x. [DOI] [PubMed] [Google Scholar]
- Anderson HR, Butland BK, Strachan DP. Trends in prevalence and severity of childhood asthma. Br Med J. 1994;308:1600–1604. doi: 10.1136/bmj.308.6944.1600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jain A, Bhat HV, Acharya D. Prevalence of Bronchial Asthma in Rural Indian Children: A Cross Sectional Study from South India. Indian J Pediatr. 2010;77:31–35. doi: 10.1007/s12098-009-0308-6. [DOI] [PubMed] [Google Scholar]
- Sanchez-Lerma B. High Prevalence of Asthma and Allergic Diseases in Children Aged 6 and 7 Years From the Canary Islands: The International Study of Asthma and Allergies in Childhood (vol 19, pg 383, 2009) J Investig Allergol Clin Immunol. 2012;22:79–79. [PubMed] [Google Scholar]
- Hong S, Son DK, Lim WR, Kim SH, Kim H, Yum HY, Kwon H. The prevalence of atopic dermatitis, asthma, and allergic rhinitis and the comorbidity of allergic diseases in children. Environ Health Toxicol. 2012;27:e2012006–e2012006. doi: 10.5620/eht.2012.27.e2012006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luna MFG, Almeida PC, Silva MGC. Asthma and rhinitis prevalence and co-morbidity in 13-14-year-old schoolchildren in the city of Fortaleza, Ceara State, Brazil. Cad Saude Publica. 2011;27:103–112. doi: 10.1590/s0102-311x2011000100011. [DOI] [PubMed] [Google Scholar]
- de Luna MFG, Fischer GB, de Luna JRG, da Silva MGC, de Almeida PC, Chiesa D. Prevalences of asthma and rhinitis among adolescents in the city of Fortaleza, Brazil: temporal changes. J Bras Pneumol. 2013;39:128–137. doi: 10.1590/S1806-37132013000200003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matos Povoas Juca SCB, Takano OA, Lacerda Moraes LS, Guimaraes LV. Asthma prevalence and risk factors in adolescents 13 to 14 years of age in Cuiaba, Mato Grosso State. Brazil Cad Saude Publica. 2012;28:689–697. doi: 10.1590/s0102-311x2012000400008. [DOI] [PubMed] [Google Scholar]
- de Farias MRC, Rosa AM, Hacon SS, de Castro HA, Ignotti E. Prevalence of asthma in schoolchildren in Alta Floresta- a municipality in the southeast of the Brazilian Amazon. Rev Bras Epidemiol. 2010;13:49–57. doi: 10.1590/s1415-790x2010000100005. [DOI] [PubMed] [Google Scholar]
- Bennoor KS, Hassan MR, Hossain MA, Mahmud AM, Ahmad MM, Habib GM. Trends of asthma in Bangladesh: findings of the national asthma prevalence study -1999 and 2010. Respirology. 2011;16:212–212. [Google Scholar]
- Gudelj I, Mrkic Kobal I, Munivrana Skvorc H, Mise K, Vrbica Z, Plavec D, Tudoric N. Intraregional differences in asthma prevalence and risk factors for asthma among adolescents in Split-Dalmatia County, Croatia. Med Sci Monit. 2012;18:PH43–50. doi: 10.12659/MSM.882609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toledo MF, Rozov T, Leone C. Prevalence of asthma and allergies in 13-to 14-year-old adolescents and the frequency of risk factors in carriers of current asthma in Taubate, Sao Paulo, Brazil. Allergol Immunopathol (Madr) 2011;39:284–290. doi: 10.1016/j.aller.2010.09.004. [DOI] [PubMed] [Google Scholar]
- Robinson CL, Baumann LM, Gilman RH, Romero K, Manuel Combe J, Cabrera L, Hansel NN, Barnes K, Gonzalvez G, Wise RA, Breysse PN, Checkley W. The Peru Urban versus Rural Asthma (PURA) Study: methods and baseline quality control data from a cross-sectional investigation into the prevalence, severity, genetics, immunology and environmental factors affecting asthma in adolescence in Peru. Bmj Open. 2012;2:e000421. doi: 10.1136/bmjopen-2011-000421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delmas MC, Guignon N, Leynaert B, Annesi-Maesano I, Com-Ruelle L, Gonzalez L, Fuhrman C. Prevalence and control of asthma in young children in France. Rev Mal Respir. 2012;29:688–696. doi: 10.1016/j.rmr.2011.11.016. [DOI] [PubMed] [Google Scholar]
- Julia-Serda G, Cabrera-Navarro P, Acosta-Fernandez O, Martin-Perez P, Losada-Cabrera P, Garcia-Bello MA, Carrillo-Diaz T, Anto-Boque J. High prevalence of asthma and atopy in the Canary Islands, Spain. Int J Tuberc Lung Dis. 2011;15:536–541. doi: 10.5588/ijtld.10.0303. [DOI] [PubMed] [Google Scholar]
- Mahboub BH, Al-Hammadi S, Rafique M, Sulaiman N, Pawankar R, Al Redha AI, Mehta AC. Population prevalence of asthma and its determinants based on European Community Respiratory Health Survey in the United Arab Emirates. BMC Pulm Med. 2012;12:4. doi: 10.1186/1471-2466-12-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alves GC, Santos DN, Feitosa CA, Barreto ML. Community violence and childhood asthma prevalence in peripheral neighborhoods in Salvador, Bahia State. Brazil Cad Saude Publica. 2012;28:86–94. doi: 10.1590/s0102-311x2012000100009. [DOI] [PubMed] [Google Scholar]
- Akinbami LJ, Schoendorf KC. Trends in childhood asthma: Prevalence, health care utilization, and mortality. Pediatrics. 2002;110:315–322. doi: 10.1542/peds.110.2.315. [DOI] [PubMed] [Google Scholar]
- Agrawal S. Effect of Indoor Air Pollution from Biomass and Solid Fuel Combustion on Prevalence of Self-Reported Asthma among Adult Men and Women in India: Findings from a Nationwide Large-Scale Cross-Sectional Survey. J Asthma. 2012;49:355–365. doi: 10.3109/02770903.2012.663030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agrawal S, Pearce N, Ebrahim S. Prevalence and risk factors for self-reported asthma in an adult Indian population: a cross-sectional survey. Int J Tuberc Lung Dis. 2013;17:275–282. doi: 10.5588/ijtld.12.0438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burney PGJ, Chinn S, Rona RJ. Has the prevalence of asthma increased in children - evidence from the national study of health and growth 1973–86. Br Med J. 1990;300:1306–1310. doi: 10.1136/bmj.300.6735.1306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krstic G. Asthma Prevalence Associated with Geographical Latitude and Regional Insolation in the United States of America and Australia. PloS One. 2011;6:e18492. doi: 10.1371/journal.pone.0018492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sousa CA, Cesar CLG, Barros MBA, Carandina L, Goldbaum M, Pereira JCR. Prevalence of asthma and risk factors associated: population based study in Sao Paulo, Southeastern Brazil, 2008–2009. Rev Saude Publica. 2012;46:825–833. doi: 10.1590/s0034-89102012000500009. [DOI] [PubMed] [Google Scholar]
- Fiori NS, Goncalves H, Dumith SC, Dropa Chrestani Cesar MA, Menezes AMB, Cardozo Macedo SE. Ten-year trends in prevalence of asthma in adults in southern Brazil: comparison of two population-based studies. Cad Saude Publica. 2012;28:135–144. doi: 10.1590/s0102-311x2012000100014. [DOI] [PubMed] [Google Scholar]
- Mak H, Johnston P, Abbey H, Talamo RC. Prevalence of athma and health-service utilization of asthmatic-children in an inner-city. J Allergy Clin Immunol. 1982;70:367–372. doi: 10.1016/0091-6749(82)90026-4. [DOI] [PubMed] [Google Scholar]
- Moreira SM, Ribeiro ACG, Fonseca M, Lourenco O, Taborda-Barata L. Comparative study of the prevalence, clinical features, sensitisation profiles and risk factors for Bronchial Asthma between elderly and young adults in Cova da Beira Portugal. Eur J Med Res. 2010;15:216–216. [Google Scholar]
- Parasuramalu BG, Huliraj N, Rudraprasad BM, Prashanth Kumar SP, Ramesh Masthi NR, Gangaboraiah. Prevalence of bronchial asthma and its association with smoking habits among adult population in rural area. Indian J Public Health. 2010;54:165–168. doi: 10.4103/0019-557X.75742. [DOI] [PubMed] [Google Scholar]
- Woolcock AJ, Peat JK, Salome CM, Yan K, Anderson SD, Schoeffel RE, McCowage G, Killalea T. Prevalence of bronchial hyperresponsiveness and asthma in a rural adult-population. Thorax. 1987;42:361–368. doi: 10.1136/thx.42.5.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornell AG, Mellins RB, Acosta LM, Rundle AG, Miller RL, Kinney PL, Yan B, Perera FP, Jacobson JS, Goldstein IF, Chillrud SN, Perzanowski MS. Exhaled No Is Elevated With Exposure To Black Carbon And Dust Mite Allergen Among 7 And 8-Year-Old Children Living In High And Low Asthma Prevalence Neighborhoods In New York City. Am J Respir Crit Care Med. 2011;183:A4473. [Google Scholar]
- Studnicka M, Hackl E, Pischinger J, Fangmeyer C, Haschke N, Kuhr J, Urbanek R, Neumann M, Frischer T. Traffic-related NO2 and the prevalence of asthma and respiratory symptoms in seven year olds. Eur Respir J. 1997;10:2275–2278. doi: 10.1183/09031936.97.10102275. [DOI] [PubMed] [Google Scholar]
- Mortz CG, Lauritsen JM, Bindslev-Jensen C, Andersen KE. Prevalence of atopic dermatitis, asthma, allergic rhinitis, and hand and contact dermatitis in adolescents. The Odense Adolescence Cohort Study on Atopic Diseases and Dermatitis. Br J Dermatol. 2001;144:523–532. doi: 10.1046/j.1365-2133.2001.04078.x. [DOI] [PubMed] [Google Scholar]
- Kolokotroni O, Middleton N, Nicolaou N, Pipis S, Priftis KN, Milton DK, Yiallouros PK. Temporal changes in the prevalence of childhood asthma and allergies in urban and rural areas of Cyprus: results from two cross sectional studies. BMC Public Health. 2011;11:858. doi: 10.1186/1471-2458-11-858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearce N, Aiet-Khaled N, Beasley R, Mallol J, Keil U, Mitchell E, Robertson C, Grp IPTS. Worldwide trends in the prevalence of asthma symptoms: phase III of the International Study of Asthma and Allergies in Childhood (ISAAC) Thorax. 2007;62:758–766. doi: 10.1136/thx.2006.070169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Upton MN, McConnachie A, McSharry C, Hart CL, Smith GD, Gillis CR, Watt GCM. Intergenerational 20 year trends in the prevalence of asthma and hay fever in adults: the Midspan family study surveys of parents and offspring. Br Med J. 2000;321:88–92. doi: 10.1136/bmj.321.7253.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bjorksten B, Dumitrascu D, Foucard T, Khetsuriani N, Khaitov R, Leja M, Lis G, Pekkanen J, Priftanji A, Riikjarv MA. Prevalence of childhood asthma, rhinitis and eczema in Scandinavia and Eastern Europe. Eur Respir J. 1998;12:432–437. doi: 10.1183/09031936.98.12020432. [DOI] [PubMed] [Google Scholar]
- Galassi C, De Sario M, Biggeri A, Bisanti L, Chellini E, Ciccone G, Petronio MG, Piffer S, Sestini P, Rusconi F, Viegi G, Forastiere F. Changes in prevalence of asthma and allergies among children and adolescents in Italy: 1994–2002. Pediatrics. 2006;117:34–42. doi: 10.1542/peds.2004-2709. [DOI] [PubMed] [Google Scholar]
- Leung R, Wong G, Lau J, Ho A, Chan JKW, Choy D, Douglass C, Lai CKW. Prevalence of asthma and allergy in Hong Kong schoolchildren: An ISAAC study. Eur Respir J. 1997;10:354–360. doi: 10.1183/09031936.97.10020354. [DOI] [PubMed] [Google Scholar]
- Robertson CF, Heycock E, Bishop J, Nolan T, Olinsky A, Phelan PD. Prevalence of asthma in melbourne schoolchildren - changes over 26 years. Br Med J. 1991;302:1116–1118. doi: 10.1136/bmj.302.6785.1116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pegas PN, Alves CA, Scotto MG, Evtyugina MG, Pio CA, Freitas MC. Risk factors and prevalence of asthma and rhinitis among primary school children in Lisbon. Rev Port Pneumol. 2011;17:109–116. doi: 10.1016/j.rppneu.2011.01.004. [DOI] [PubMed] [Google Scholar]
- Lopez-Silvarrey-Varela A, Pertega-Diaz S, Rueda-Esteban S, Manuel Sanchez-Lastres J, Angel San-Jose-Gonzalez M, Sampedro-Campos M, Perez-Castro T, Garnelo-Suarez L, Bamonde-Rodriguez L, Lopez-Silvarrey-Varela J, Gonzalez-Barcala J. Prevalence and Geographic Variations in Asthma Symptoms in Children and Adolescents in Galicia (Spain) Arch Bronconeumol. 2011;47:274–282. doi: 10.1016/j.arbres.2011.01.009. [DOI] [PubMed] [Google Scholar]
- Pearce N, Sunyer J, Cheng S, Chinn S, Bjorksten B, Burr M, Keil U, Anderson HR, Burney P, Com ISCE. Comparison of asthma prevalence in the ISAAC and the ECRHS. Eur Respir J. 2000;16:420–426. doi: 10.1183/9031936.00.16337700. [DOI] [PubMed] [Google Scholar]
- Kaur B, Anderson HR, Austin J, Burr M, Harkins LS, Strachan DP, Warner JO. Prevalence of asthma symptoms, diagnosis, and treatment in 12–14 year old children across Great Britain (international study of asthma and allergies in childhood, ISAAC UK) Br Med J. 1998;316:118–124. doi: 10.1136/bmj.316.7125.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ekerljung L, Sundblad B-M, Ronmark E, Larsson K, Lundback B. Incidence and prevalence of adult asthma is associated with low socio-economic status. Clin Respir J. 2010;4:147–156. doi: 10.1111/j.1752-699X.2009.00164.x. [DOI] [PubMed] [Google Scholar]
- Lam HT, Ronmark E, Tu'o'ng NV, Ekerljung L, Chuc NTK, Lundback B. Increase in asthma and a high prevalence of bronchitis: results from a population study among adults in urban and rural Vietnam. Respir Med. 2011;105:177–185. doi: 10.1016/j.rmed.2010.10.001. [DOI] [PubMed] [Google Scholar]
- James AL, Knuiman MW, Divitini ML, Hui J, Hunter M, Palmer LJ, Maier G, Musk AW. Changes in the prevalence of asthma in adults since 1966: the Busseltion health study. Eur Respir J. 2010;35:273–278. doi: 10.1183/09031936.00194308. [DOI] [PubMed] [Google Scholar]
- Wennergren G, Ekerljung L, Alm B, Eriksson J, Lotvall J, Lundback B. Asthma in late adolescence - farm childhood is protective and the prevalence increase has levelled off. Pediatr Allergy Immunol. 2010;21:806–813. doi: 10.1111/j.1399-3038.2010.01057.x. [DOI] [PubMed] [Google Scholar]
- Arnedo-Pena A, Garcia-Marcos L, Fuertes Fernandez-Espinar J, Bercedo-Sanz A, Aguinaga-Ontoso I, Gonzalez-Diaz C, Carvajal-Uruena I, Busquet-Monge R, Morales Suarez-Varela M, Garcia de Andoin N, Batlles-Garrido J, Blanco-Quiros A, Lopez-Silvarrey Varela A, Garcia-Hernandez G. Sunny hours and variations in the prevalence of asthma in schoolchildren according to the International Study of Asthma and Allergies (ISAAC) Phase III in Spain. Int J Biometeorol. 2011;55:423–434. doi: 10.1007/s00484-010-0353-x. [DOI] [PubMed] [Google Scholar]
- Alsowaidi S, Abdulle A, Bernsen R. Prevalence and Risk Factors of Asthma among Adolescents and Their Parents in Al-Ain (United Arab Emirates) Respiration. 2010;79:105–111. doi: 10.1159/000219248. [DOI] [PubMed] [Google Scholar]
- Guo YLL, Lin YC, Sung FC, Huang SL, Ko YC, Lai JS, Su HJ, Shaw CK, Lin RS, Dockery DW. Climate, traffic-related air pollutants, and asthma prevalence in middle-school children in Taiwan. Environ Health Perspect. 1999;107:1001–1006. doi: 10.1289/ehp.991071001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwang G-S, Choi J-W, Yoo Y, Choung J-T, Yoon C-S. Residential Environmental Risk Factors for Childhood Asthma Prevalence in Metropolitan and Semirural Cities in Korea. Asia Pac J Public Health. 2012;24:58–67. doi: 10.1177/1010539510373139. [DOI] [PubMed] [Google Scholar]
- Sousa SIV, Ferraz C, Alvim-Ferraz MCM, Martins FG, Vaz LG, Pereira MC. Spirometric tests to assess the prevalence of childhood asthma at Portuguese rural areas: Influence of exposure to high ozone levels. Environ Int. 2011;37:474–478. doi: 10.1016/j.envint.2010.11.014. [DOI] [PubMed] [Google Scholar]
- Koshy G, Delpisheh A, Brabin BJ. Trends in prevalence of childhood and parental asthma in Merseyside, 1991–2006. J Public Health. 2010;32:488–495. doi: 10.1093/pubmed/fdq027. [DOI] [PubMed] [Google Scholar]
- Hansen TE, Evjenth B, Holt J. Increasing prevalence of asthma, allergic rhinoconjunctivitis and eczema among schoolchildren: three surveys during the period 1985–2008. Acta Paediatr. 2013;102:47–52. doi: 10.1111/apa.12030. [DOI] [PubMed] [Google Scholar]
- Zollner IK, Weiland SK, Piechotowski I, Gabrio T, von Mutius E, Link B, Pfaff G, Kouros B, Wuthe J. No increase in the prevalence of asthma, allergies, and atopic sensitisation among children in Germany: 1992–2001. Thorax. 2005;60:545–548. doi: 10.1136/thx.2004.029561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim SY, Jung JY, Park MS, Kang YA, Kim EY, Kim SK, Chang J, Kim YS. Increased Prevalence of Self-Reported Asthma Among Korean Adults: An Analysis of KNHANES I and IV Data. Lung. 2013;191:281–288. doi: 10.1007/s00408-013-9453-9. [DOI] [PubMed] [Google Scholar]
- Bjerg A, Sandstrom T, Lundback B, Ronmark E. Time trends in asthma and wheeze in Swedish children 1996–2006: prevalence and risk factors by sex. Allergy. 2010;65:48–55. doi: 10.1111/j.1398-9995.2009.02105.x. [DOI] [PubMed] [Google Scholar]
- Bai J, Zhao J, Shen K-L, Xiang L, Chen A-H, Huang S, Huang Y, Wang J-S, Ye R-W. Current Trends of the Prevalence of Childhood Asthma in Three Chinese Cities : A Multicenter Epidemiological Survey. Biomed Environ Sci. 2010;23:453–457. doi: 10.1016/S0895-3988(11)60007-X. [DOI] [PubMed] [Google Scholar]
- Peat JK, Haby M, Spijker J, Berry G, Woolcock AJ. Prevalence of asthma in adults in Busselton, Western-Australia. Br Med J. 1992;305:1326–1329. doi: 10.1136/bmj.305.6865.1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kainu A, Pallasaho P, Piirila P, Lindqvist A, Sovijarvi A, Pietinalho A. Increase in prevalence of physician-diagnosed asthma in Helsinki during the Finnish Asthma Programme: improved recognition of asthma in primary care? A cross-sectional cohort study. Prim Care Respir J. 2013;22:64–71. doi: 10.4104/pcrj.2013.00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al Ghobain MO, Al-Hajjaj MS, Al Moamary MS. Asthma prevalence among 16-to 18-year-old adolescents in Saudi Arabia using the ISAAC questionnaire. BMC Public Health. 2012;12:239. doi: 10.1186/1471-2458-12-239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- To T, Stanojevic S, Moores G, Gershon AS, Bateman ED, Cruz AA, Boulet LP. Global asthma prevalence in adults: findings from the cross-sectional world health survey. BMC Public Health. 2012;12:204. doi: 10.1186/1471-2458-12-204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wehrmeister FC, de Anselmo Peres KG. Regional inequalities in the prevalence of asthma diagnosis in children: an analysis of the Brazilian National Household Sample Survey, 2003. Cad Saude Publica. 2010;26:1839–1852. doi: 10.1590/s0102-311x2010000900017. [DOI] [PubMed] [Google Scholar]
- Strachan DP, Anderson HR, Limb ES, Oneill A, Wells N. A national survey of asthma prevalence, severity, and treatment in Great-Britain. Arch Dis Child. 1994;70:174–178. doi: 10.1136/adc.70.3.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrea Rodriguez L, Jose Rey J, Berena Herrera A, Castro H, Niederbacher J, Maria Vera L, Libia Cala L, Bolivar F. Respiratory symptoms associated with asthma prevalence and air pollution in preschool children. Biomedica. 2010;30:15–22. [PubMed] [Google Scholar]
- Goh DYT, Chew FT, Quek SC, Lee BW. Prevalence and severity of asthma, rhinitis, and eczema in Singapore schoolchildren. Arch Dis Child. 1996;74:131–135. doi: 10.1136/adc.74.2.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shakurnia AH, Assar S, Afra M, Latifi M. Prevalence of asthma among schoolchildren in Ahvaz, Islamic Republic of Iran. East Mediterr Health J. 2010;16:651–656. [PubMed] [Google Scholar]
- Fedortsiv O, Brozek GM, Luchyshyn N, Kubey I, Lawson JA, Rennie DC, Zejda JE. Prevalence of childhood asthma, rhinitis, and eczema in the Ternopil region of Ukraine - results of BUPAS study. Adv Med Sci. 2012;57:282–289. doi: 10.2478/v10039-012-0034-6. [DOI] [PubMed] [Google Scholar]
- Vonmutius E, Fritzsch C, Weiland SK, Roll G, Magnussen H. Prevalence of asthma and allergic disorders among children in United Germany - a descriptive comparison. Br Med J. 1992;305:1395–1399. doi: 10.1136/bmj.305.6866.1395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Litonjua AA, Carey VJ, Weiss ST, Gold DR. Race, socioeconomic factors, and area of residence are associated with asthma prevalence. Pediatr Pulmonol. 1999;28:394–401. doi: 10.1002/(sici)1099-0496(199912)28:6<394::aid-ppul2>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- Nriagu J, Martin J, Smith P, Socier D. Residential hazards, high asthma prevalence and multimorbidity among children in Saginaw, Michigan. Sci Total Environ. 2012;416:53–61. doi: 10.1016/j.scitotenv.2011.10.040. [DOI] [PubMed] [Google Scholar]
- Downs SH, Marks GB, Sporik R, Belosouva EG, Car NG, Peat JK. Continued increase in the prevalence of asthma and atopy. Arch Dis Child. 2001;84:20–23. doi: 10.1136/adc.84.1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lukrafka JL, Fuchs SC, Moreira LB, Picon RV, Fischer GB, Fuchs FD. Performance of the ISAAC Questionnaire to Establish the Prevalence of Asthma in Adolescents: A Population-Based Study. J Asthma. 2010;47:166–169. doi: 10.3109/02770900903483766. [DOI] [PubMed] [Google Scholar]
- Miller JE. The effects of race/ethnicity and income on early childhood asthma prevalence and health care use. Am J Public Health. 2000;90:428–430. doi: 10.2105/ajph.90.3.428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zobeiri M. Prevalence, risk factors and severity of asthma symptoms in children of Kermanshah, IRAN: ISAAC phase I, II. Acta Med Iran. 2011;49:184–188. [PubMed] [Google Scholar]
- Yeh K-W, Ou L-S, Yao T-C, Chen L-C, Lee W-I, Huang J-L, Grp PS. Prevalence and risk factors for early presentation of asthma among preschool children in Taiwan. Asian Pac J Allergy Immunol. 2011;29:120–126. [PubMed] [Google Scholar]
- Joseph CLM, Foxman B, Leickly FE, Peterson E, Ownby D. Prevalence of possible undiagnosed asthma and associated morbidity among urban schoolchildren. J Pediatr. 1996;129:735–742. doi: 10.1016/s0022-3476(96)70158-0. [DOI] [PubMed] [Google Scholar]
- Gergen PJ, Mullally DI, Evans R. National survey of prevalence of asthma among children in United-States, 1976 to 1980. Pediatrics. 1988;81:1–7. [PubMed] [Google Scholar]
- Jie Y, Isa ZM, Jie X, Ismail NH. Asthma and Asthma-Related Symptoms among Adults of an Acid Rain-Plagued City in Southwest China: Prevalence and Risk Factors. Pol J Environ Stud. 2013;22:717–726. [Google Scholar]
- Rerksuppaphol S, Rerksuppaphol L. Carotenoid intake and asthma prevalence in Thai children. Pediatr Rep. 2012;4:e12–e12. doi: 10.4081/pr.2012.e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Marco R, Pesce G, Marcon A, Accordini S, Antonicelli L, Bugiani M, Casali L, Ferrari M, Nicolini G, Panico MG, Pirina P, Zanolin ME, Cerveri I, Verlato G. The Coexistence of Asthma and Chronic Obstructive Pulmonary Disease (COPD): Prevalence and Risk Factors in Young. Middle-aged and Elderly People from the General Population. PloS One. 2013;8:e62985. doi: 10.1371/journal.pone.0062985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryant-Stephens T, West C, Dirl C, Banks T, Briggs V, Rosenthal M. Asthma Prevalence in Philadelphia: Description of Two Community-Based Methodologies to Assess Asthma Prevalence in an Inner-City Population. J Asthma. 2012;49:581–585. doi: 10.3109/02770903.2012.690476. [DOI] [PubMed] [Google Scholar]
- Waite DA, Eyles EF, Tonkin SL, Odonnell TV. Asthma prevalence in Tokelauan children in 2 environments. Clin Allergy. 1980;10:71–75. doi: 10.1111/j.1365-2222.1980.tb02082.x. [DOI] [PubMed] [Google Scholar]
- de Sousa JC, Santo ME, Colaco T, Almada-Lobo F, Yaphe J. Asthma in an Urban Population in Portugal: A prevalence study. BMC Public Health. 2011;11:347. doi: 10.1186/1471-2458-11-347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zivkovic Z, Vukasinovic Z, Cerovic S, Radulovic S, Zivanovic S. Prevalence of childhood asthma and allergies in Serbia and Montenegro. World J Pediatr. 2010;6:331–336. doi: 10.1007/s12519-010-0207-y. [DOI] [PubMed] [Google Scholar]
- Burney PG, Laitinen LA, Perdrizet S, Huckauf H, Tattersfield AE, Chinn S, Poisson N, Heeren A, Britton JR, Jones T. Validity and repeatability of the IUATLD (1984) Bronchial Symptoms Questionnaire: an international comparison. Eur Respir J. 1989;2:940–945. [PubMed] [Google Scholar]
- de Marco R, Cerveri I, Bugiani M, Ferrari M, Verlato G. An undetected burden of asthma in Italy: the relationship between clinical and epidemiological diagnosis of asthma. Eur Respir J. 1998;11:599–605. [PubMed] [Google Scholar]
- Skytt N, Bønnelykke K, Bisgaard H. “To wheeze or not to wheeze”: That is not the question. J Allergy Clin Immunol. 2012;130:403–407. doi: 10.1016/j.jaci.2012.04.043. [DOI] [PubMed] [Google Scholar]
- Wright AL. Epidemiology of asthma and recurrent wheeze in childhood. Clin Rev Allergy Immunol. 2002;22:33–44. doi: 10.1007/s12016-002-0004-z. [DOI] [PubMed] [Google Scholar]
- Discussion document of symptom outcomes. [ http://www.ecrhs.org/Publications/symptomoutcomes.pdf]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Databases details.
Summary of the included studies.
Definitions in the ten most cited and the ten most recent papers from the 117 included by Average citations per year at the end of 2013.
Studies presenting three different subgroups of the definition of asthma. Of the 117 papers included, 34 provided a definition for lifetime asthma, 54 for diagnosed asthma and 61 for current asthma; 5 papers defined the three types of asthma.
Summary of studies with Current asthma definitions that used the International Study of Asthma and Allergies in Childhood (ISAAC) questionnaire (n = 18).


