Abstract
Background
Indoor tanning has been found to be addictive. However, the most commonly-used tanning dependence measures have not been well-validated.
Objective
The study’s purpose was to explore the psychometric characteristics of and compare the mCAGE (modified Cut-down, Annoyed, Guilty, Eye-opener Scale), mDSM-IV-TR (modified Diagnostic and Statistical Manual of Mental Disorders – Fourth Edition - Text Revised), and TAPS (Tanning Pathology Scale) measures of tanning dependence and provide recommendations for research and practice.
Methods
This study was a cross-sectional online survey with 18–25 year old female university students. The main outcome variable was tanning dependence measured by the mCAGE, mDSM-IV-TR, and TAPS.
Results
Internal consistency of the TAPS subscales was good but was poor for the mCAGE and mDSM-IV-TR, except when their items were combined. Agreement between the mCAGE and mDSM-IV-TR was fair. Factor analysis of the TAPS confirmed the current four-factor structure. All of the tanning dependence scales were significantly correlated with one another. Likewise, most of the tanning dependence scales were significantly correlated with other measures of tanning attitudes and behaviors. However, the tolerance to tanning TAPS subscale was not significantly correlated with any measure of tanning attitudes or behaviors and had the lowest subscale internal reliability and eigenvalues.
Conclusion
Based on the data and existing literature, we make recommendations for the continued use of tanning dependence measures. Intervention may be needed for the approximately 5% of college women who tend to be classified as tanning dependent across measures. Monitoring of individuals reporting tanning dependence symptoms is warranted.
Introduction
Ultraviolet (UV) radiation exposure is associated with skin cancers, including deadly melanomas.1–4 Some individuals, especially young adults and adolescents, obtain large amounts of UV exposure from tanning intentionally in the sun and in tanning salons.5,6 Throughout this manuscript, we refer to indoor tanning, sunbathing, as well as tanning in general. The primary reason individuals intentionally tan their skin is to enhance their appearance.7–14 However, a minority of individuals become psychologically and physically dependent on (addicted to) such UV exposure. Although tanning dependence is not an official disorder listed in the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders,15 it has been defined based on traditional substance dependence measures and criteria (i.e., tolerance, withdrawal, difficulty controlling the behavior). The prevalence of tanning dependence varies by population and measurement strategy, with rates of 22 to 45% among college indoor tanners, 18% among college sunbathers, and 5 to 27% among general college student samples in the US.16–21 Tanning dependence is likely to have biologic underpinnings, primarily related to the opioid system (see 22,23 for a review). Tanning dependent individuals may tan frequently and put themselves at even greater risk of skin cancer than other tanners. Frequent tanners and tanning dependent individuals tend to have more psychiatric and substance disorder symptoms than others. 19,20,24–28
Psychometric properties of existing tanning dependence measures have not been well-established, since tanning dependence research is still nascent. Tanning dependence has been assessed primarily using two scales developed by Warthan and colleagues,29 who modified the standard substance dependence criteria from the DSM-IV-TR15 for tanning as well as those of the four-item CAGE scale,30 which has traditionally been used in screening for problematic alcohol use. CAGE is an acronym that refers to its four items: attempts to Cut down on drinking (in this case, tanning), feeling Annoyed when told to not do a behavior, feeling Guilty when doing the behavior too much, and wanting to engage in the behavior first thing in the morning (Eye-opener). The modified 7-item DSM-IV-TR criteria pertain to tolerance, withdrawal, and engaging in the behavior (i.e., tanning) despite negative consequences, which are key criteria of all substance dependence disorders. Prior research has found good reliability, sensitivity, specificity, and validity of the CAGE for alcohol disorders31–33 and measures used to assess DSM-IV substance dependence criteria.34 However, the only two studies that reported internal consistency data for the mCAGE and mDSM-IV-TR measures of tanning dependence found low Cronbach’s alpha levels of 0.57–0.58 for the mCAGE and 0.56 for the mDSM-IV-TR.17,19,20
A third measure of tanning dependence which has been less frequently used is the 16-item Tanning Pathology Scale (TAPS).35 The TAPS assesses multidimensional pathological tanning motives. Though the TAPS is not framed as a measure of tanning dependence, constructs assessed include key addictive symptoms that predict tanning intentions and behavior such as tolerance and out of control behavior despite awareness of negative consequences.35 Subscales are perceiving tanning as a problem, opiate-like reactions to tanning, tolerance to tanning, and dissatisfaction with skin tone. Cronbach’s alphas for the four subscales range from 0.62 to 0.90.35 TAPS scores are correlated with tanning intentions scores.35 More recently, a self-administered clinical interview for tanning abuse and dependence was developed (SITAD)16 but was not assessed in the current study.
Despite the existence of several measures to assess tanning dependence, there seems to be scant agreement regarding an operational definition. The purpose of the study was to assess optimal and valid measurement of tanning dependence. The aims were as follows: 1) to examine internal consistency of the mCAGE, mDSM-IV-TR, and TAPS among young adult women, including a factor analysis to further examine the structure of the TAPS and 2) to compare measure agreement and assess convergent validity. Study results can help to provide recommendations for future research and practice related to the assessment of tanning dependence.
Materials and Methods
Participants
All female psychology students at a northeastern university across six academic terms from 2009–2011 were invited to participate in the study by email. Eligibility criteria included female sex and age between 18 and 25 years (M = 19.9, SD = 1.6). Three hundred and six women completed the questionnaires. Racial distribution was as follows: 68.2% White, 15.1% Asian, 11.8% Other/Mixed, and 4.9% Black. Four percent of the sample identified themselves as Hispanic/Latina.
Measures
Tanning dependence
As described above, tanning dependence was assessed using the mCAGE and mDSM-IV-TR adapted by Warthan and colleagues29 and the TAPS developed by Hillhouse and colleagues.29,35
The CAGE items are: “Do you try to CUT down on the time you spend tanning but find yourself still tanning?”, “Do you ever get ANNOYED when people tell you not to tan?”, “Do you ever feel GUILTY that you are tanning too much?”, and “When you wake up in the morning, do you want to tan?” [EYE-OPENER]. Sample mDSM-IV-TR items are: “Do you think you need to spend more and more time tanning to maintain your color?” and “Do your beliefs about skin cancer keep you from spending time in the sun or going to tanning beds?”
TAPS response options utilize a 5-point Likert-type scale of agreement (1 = strongly disagree, 5 = strongly agree). Item responses are summed for each subscale. Sample TAPS items are: “Sometimes I think my tanning is out of control”, “I feel tranquil after a tanning session”, “Tanning doesn’t relieve my stress as well as it did when I started”, and “I wish I had been born with a darker shade of skin”.
Endorsing two out of the four mCAGE items meets criteria for tanning dependence, endorsing three of the mDSM-IV-TR items meets criteria for tanning dependence, whereas the TAPS provides continuous scores on each of its subscales.
Tanning attitudes and behaviors
In order to assess convergent validity of the tanning dependence measures, additional measures of tanning attitudes and behaviors were included. Participants were asked to indicate how many times they indoor tanned in the past month and past year. Given the skewed nature of the responses, scores were dichotomized into having indoor tanned in the past month and past year versus not having indoor tanned, similar to dichotomization procedures used in related studies.36,37 Ever indoor tanners were asked about their current pattern of tanning bed use, with options being “once in a while for special occasions,” “mainly during a specific season,” “all year round,” and “don’t use anymore.” Given the small number of responses for “all year round,” this group was categorized together with “mainly during a specific season.” Those who have never indoor tanned were grouped with “don’t use anymore.” This categorization was adapted from the indoor tanning patterns scheme used by Hillhouse and colleagues.16
Perceived benefits of tanning were assessed using three items from Johnson38, with an example of an item being “Having a tan improves the way I look.” Items were scores on a 5-point Likert-type scale of agreement. These items showed acceptable internal consistency in our sample, with Cronbach’s alpha of 0.78. Intentions to avoid tanning were assessed using two items from Jackson and Aiken39, with participants being asked to indicate their intentions to “avoid tanning” and “avoid intentionally sunbathing.” Items were scored on a 7-point Likert-type scale of agreement. Attitudes and beliefs such as perceived benefits and intentions are common constructs from well-validated health behavior theories such as the Health Belief Model and the Theory of Planned Behavior.40,41
Procedures
Participants were recruited via e-mail and web through a psychology department research subject pool. After consenting via an online consent form, students completed the online questionnaire at their convenience. Participants were given research participation extra credit for an academic course and a $20 PayPal voucher as compensation. This study was approved by the university’s and a cancer center’s Institutional Review Boards.
Data Analysis
Statistical analyses were done using SPSS software, version 19.0. Correlations between the tanning dependence measures and internal consistency of the three tanning dependence measures in our sample were assessed. Agreement on meeting tanning dependence criteria according to the mCAGE and mDSM-IV-TR measures was determined. Both exploratory and confirmatory factor analyses were done for the TAPS. A cut-point was proposed for the TAPS based on the frequency distribution and cut-off rates for the mCAGE and mDSM-IV-TR. Finally, convergent validity was assessed by examining associations with indoor tanning in the past month, indoor tanning in the past year, current tanning bed use pattern (year-round/seasonal, for special events, no longer uses or never used), perceived benefits of tanning, and intention to avoid tanning. Pearson’s correlations, independent sample t-tests, and one-way analysis of variance (ANOVA) were used. Scheffé post hoc tests were used when ANOVA results were significant.
Results
Correlations among the measures
See Table 1 for correlations between tanning dependence measures (mCAGE, mDSM-IV-TR, TAPS). All correlations were significant at the 0.01 level and ranged from 0.15 to 0.64.
Table 1.
Correlations, Means, and Standard Deviations of Study Variables (N = 306) a
| Variables b | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|
| 1. mCAGE | -- | 0.52*** | 0.49*** | 0.39*** | 0.33*** | 0.31*** |
| 2. mDSM-IV-TR | -- | 0.29*** | 0.55*** | 0.53*** | 0.15** | |
| TAPS Subscales | ||||||
| 3. Perceiving tanning as problem | -- | 0.51*** | 0.38*** | 0.64*** | ||
| 4. Opiate-like effects of tanning | -- | 0.50*** | 0.39*** | |||
| 5. Dissatisfaction with skin tone | -- | 0.31*** | ||||
| 6. Tolerance of tanning | -- | |||||
| M | 0.4 | 2.3 | 11.1 | 8.3 | 6.7 | 4.5 |
| SD | 0.8 | 2.2 | 5.6 | 4.7 | 3.5 | 2.3 |
p < .05,
p < .01,
p < .001;
Correlations are based on tanning dependence scores, not whether criteria for tanning dependence has been met;
Range of possible scores: mCAGE (0–4), mDSM-IV-TR (0–10), Perceiving tanning as a problem (8–40), Opiate-like effects (4–20), Dissatisfaction with skin tone (4–20), Tolerance of tanning (3–15)
Characteristics of the mCAGE and mDSM-IV-TR
Internal consistency of the mCAGE and mDSM-IV-TR was poor,42 with Kuder-Richardson 20 scores of 0.64 and 0.59, respectively. Seventy-six percent were not tanning dependent based on either measurement. Nine percent of the sample was tanning dependent based on mCAGE criteria. Twenty-one percent of the sample was tanning dependent based on mDSM-IV-TR criteria. Fifteen percent were tanning dependent based on mDSM-IV-TR criteria only, while four percent were tanning dependent based on mCAGE criteria only. Five percent were tanning dependent based on both measurements. The Kappa value between the two measures was 0.26, indicating only fair agreement.43 We assessed internal consistency when the items from the mCAGE and mDSM-IV-TR were combined into one scale since they have mostly been used simultaneously in studies. In this case, internal consistency met the standard of acceptability, with a Kuder-Richardson 20 score of 0.70.42 We also conducted a latent class analysis, which did not reveal any subscales or problematic items when the two scales were combined (data not shown).
Characteristics of the TAPS
All TAPS subscales showed strong internal consistency in our sample (alphas = 0.92, 0.91, 0.85, and 0.81, for perceiving tanning as a problem, opiate-like effects of tanning, dissatisfaction with skin tone, and tolerance of tanning, respectively). A confirmatory factor analysis using the proposed structure from Hillhouse and colleagues29,35 with maximum-likelihood estimation procedures was conducted,35 with the variance of the latent factors (i.e., tanning is a perceived problem, opiate-like effects from tanning, dissatisfaction with skin tone, and tolerance of tanning) set to 1. The chi-square statistic was significant, indicating that the model might be a poor fit, χ2 = 485.90, df = 129, p < .001. However, the chi-square value may have been affected by the relatively large sample size and considerable correlations between items.44 The values of the Comparative Fit Index (CFI = 0.91) and the root mean square error of approximation (RMSEA = .098, CI=.089, .107) together indicate a fair model fit.45 All latent variables (i.e., TAPS subscales) were significantly correlated with each other, and all items were significantly associated with their assigned subscales. An exploratory principal components factor analysis (EFA) was also done to determine optimal model structure using the TAPS items. The EFA confirmed four factors based on the scree plot with all factors having eigenvalues greater than 1.00 (8.36, 2.57, 1.39, and 1.07 for perceiving tanning as a problem, opiate-like effects from tanning, dissatisfaction with skin tone, and tolerance of tanning, respectively). The unrotated factors accounted for 74.3% of the total variance of the items. All factor loadings were greater than 0.50.
Comparison of the Measures
It is problematic to calculate an ideal “cut-point” for tanning dependence on the TAPS, based on the mCAGE or mDSM-IV-TR criteria, given the lack of agreement between these measures. However, 5% of our sample scored 54 or higher on the TAPS, consistent with 5% of the sample meeting criteria for tanning dependence based on BOTH the mCAGE and mDSM-IV-TR measures (see Figure 1). Sensitivity and specificity values for this cut-point cannot be determined due to the lack of a gold standard measure. This proposed cutpoint showed fair agreement with meeting criteria for tanning dependence based on the mCAGE (Kappa value of 0.27), but little agreement with meeting criteria based on the mDSM-IV-TR measure (Kappa value of 0.13).
Figure 1.
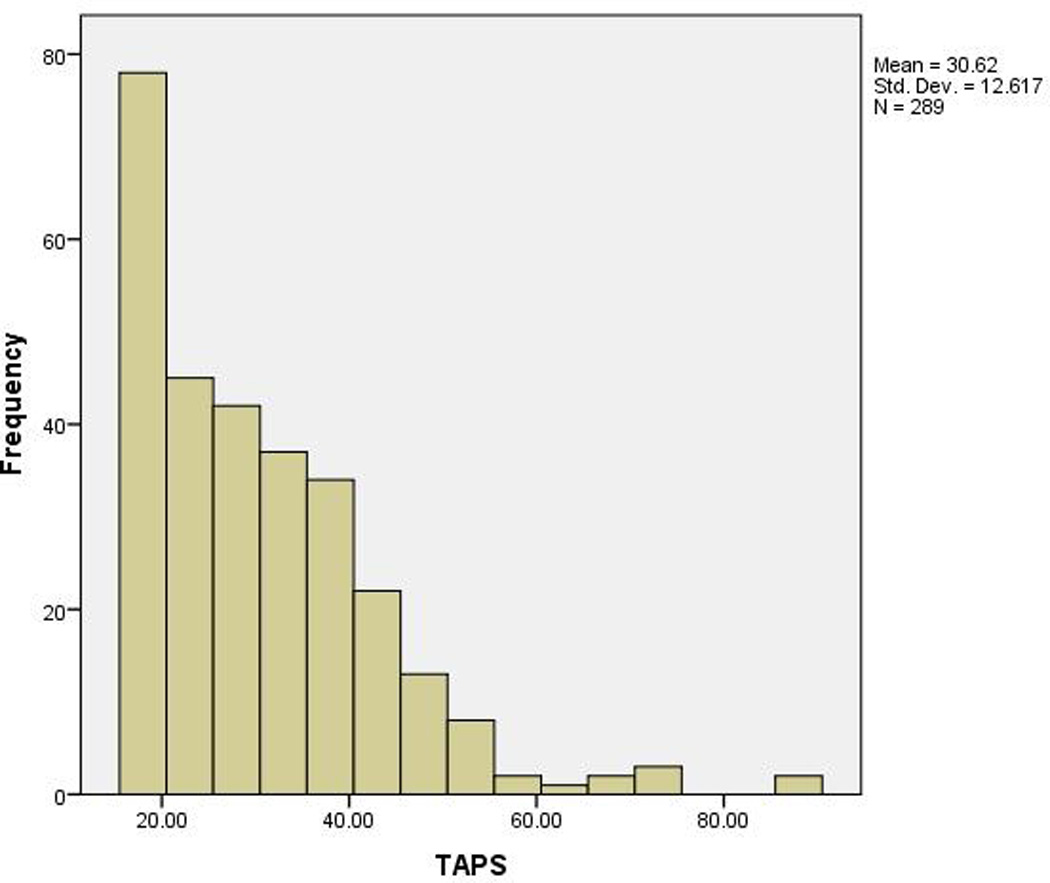
Frequencies of TAPS scores
Regarding convergent validity, most measures of tanning dependence were significantly correlated with tanning attitudes and behaviors. However, tolerance to tanning was not significantly correlated with the tanning attitudes or behavioral measures (see Table 2).
Table 2.
Correlations between Tanning Dependence and Tanning Attitudes: Convergent Validity (N = 306) a
| Variables | Benefits of Tanning | Intentions to Avoid Tanning |
|---|---|---|
| mCAGE | 0.29*** | −0.35*** |
| mDSM-IV-TR | 0.55*** | −0.67*** |
| TAPS Subscales | ||
| Perceiving tanning as problem | 0.08 | −0.23*** |
| Opiate-like effects of tanning | 0.43*** | −0.53*** |
| Dissatisfaction with skin tone | 0.54*** | −0.46*** |
| Tolerance to tanning | −0.02 | −0.05 |
p < .05,
p < .01,
p < .001;
Correlations are based on tanning dependence scores, not whether criteria for tanning dependence has been met.
Those who indoor tanned in the past year had higher scores on the mCAGE, t(95) = −5.54, p < .001, and mDSM-IV-TR measures, t(112) = −9.89, p < .001, as well as significantly higher scores for all TAPS subscales except for tolerance to tanning [t(105) = −2.81, p < .01, t(303) = −7.96, p < .001, and t(299) = −7.12, p < .001, for perceiving tanning as a problem, opiate-like effects of tanning, and dissatisfaction with skin tone, respectively], relative to those who have not indoor tanned in the past year. The same trends were found between those who indoor tanned in the past month versus those who did not, with those who indoor tanned in the past month having higher scores on the mCAGE, t(41) = −4.68, p < .001, and mDSM-IV-TR measures, t(45) = −8.41, p < .001, as well as higher scores for all TAPS subscales except for tolerance [t(43) = −3.41, p < .01, t(303) = −6.15, p < .001, and t(299) = −4.74, p < .001, for perceiving tanning as a problem, opiate-like effects of tanning, and dissatisfaction with skin tone, respectively] (see Table 3).
Table 3.
Correlations between Tanning Dependence and Tanning Behaviors: Convergent Validity (N = 306) a
| Variables | Tanned in Past Year | Tanned in Past Month | Seasonal/Year- Round |
Event Tanning | Don’t Tan | ||
|---|---|---|---|---|---|---|---|
| Yes (n = 79) | No (n = 227) | Yes (n = 39) | No (n = 267) | (n = 36) | (n = 46) | (n = 224) | |
| mCAGE | 0.9 (1.1)*** | 0.2 (0.6) | 1.3 (1.3)*** | 0.3 (0.7) | 1.2 (1.2)*** | 0.8 (1.1) | 0.2 (0.6) |
| mDSM-IV-TR | 4.3 (2.2)*** | 1.6 (1.7) | 5.2 (2.3)*** | 1.9 (1.8) | 5.4 (2.1)*** | 3.5 (2.2) | 1.6 (1.6) |
| TAPS Subscales | |||||||
| Perceiving tanning as problem | 13.0 (6.8)** | 10.6 (5.2) | 15.1 (8.1)** | 10.6 (5.0) | 14.1 (6.8) | 12.9 (7.5) | 10.3 (4.8)*** |
| Opiate-like effects of tanning | 11.7 (4.7)*** | 7.2 (4.2) | 12.5 (4.4)*** | 7.8 (4.5) | 13.9 (3.7)*** | 10.0 (4.4) | 7.2 (4.2) |
| Dissatisfaction with skin tone | 8.9 (3.4)*** | 5.9 (3.2) | 9.1 (3.4)*** | 6.3 (3.4) | 9.9 (2.9) | 8.2 (3.3) | 5.9 (3.2)*** |
| Tolerance to tanning | 4.7 (2.3) | 4.5 (2.3) | 5.0 (2.7) | 4.5 (2.2) | 4.6 (2.1) | 5.1 (2.6) | 4.4 (2.2) |
p < .05,
p < .01,
p < .001;
Means and standard deviations are reported.
ANOVA results showed significant group differences for current tanning bed use patterns (i.e., seasonal/year-round, event, and no tanning) for all tanning dependence measures except for tanning tolerance (see Table 3). Those who indoor tan seasonally or year-round reported significantly greater scores on both the mCAGE and mDSM-IV-TR measures than those who tan for specific events, who had significantly greater scores than those who no longer or have never indoor tanned, F(2, 303) = 31.91, p < .001, and F(2, 303) = 81.25, p < .001, respectively. The same trends were shown for opiate-like effects of tanning, F(2, 302) = 44.85, p < .001. Those who no longer or never used a tanning bed reported lower scores for perceiving tanning as a problem and dissatisfaction with skin tone relative to regular and event tanners, F(2, 295) = 9.47, p < .001, and F(2, 298) = 30.27, p < .001, respectively.
Discussion
This is the first study to compare three measures of tanning dependence. We believe that when used as recommended below (e.g., the mCAGE and mDSM-IV-TR in combination), all three measures can be useful in assessing tanning dependence. Internal consistency of the TAPS subscales was good but was poor for the mCAGE and mDSM-IV-TR unless used in combination. Agreement between the mCAGE, mDSM-IV-TR, and TAPS was also only fair, suggesting that they are assessing somewhat different constructs. Factor analysis of the TAPS suggests that the current four-factor structure is probably still best, at least for college women. We found that all of the tanning dependence scales were significantly correlated with one another, and most of the scales were significantly correlated with other relevant measures of tanning attitudes and behaviors as expected. However, tolerance to tanning was not significantly correlated with any measure of tanning attitudes or behaviors and had the lowest of the TAPS subscale internal reliability and eigenvalues. Perhaps a sample with a higher proportion of dependent tanners would demonstrate significant associations with the tolerance to tanning subscale.
More recently, a self-administered clinical interview for tanning abuse and dependence was developed. The Structured Interview for Tanning Abuse and Dependence (SITAD) was developed by Hillhouse and colleagues16 based on the Structured Clinical Interview (SCID) for DSM-IV-TR opiate abuse and dependence modules. The SITAD was developed through consultation with addiction experts, focus groups with tanners, and pretesting including cognitive interviewing. Among a sample of college students, 10.8% met SITAD criteria for tanning abuse, and 5.4% met criteria for tanning dependence.16 These rates are similar to past-year prevalence rates for other substance abuse and dependence disorders reported in national surveys (e.g., 5.8% for alcohol dependence and 7.7% for alcohol or drug dependence in young adults) and lower than previously reported rates using the mCAGE and mDSM-IV-TR.16 Three-week test-retest reliability was good for tanning dependence, with 97% agreement (phi coefficient = 0.84).16 Although agreement for tanning abuse was high (84%), the reliability estimate was relatively low (phi coefficient = 0.43).16 The SITAD has demonstrated evidence of validity in that tanning-dependent participants reported regular indoor tanning, higher indoor tanning frequency, and higher scores on the opiate-like reactions to tanning subscale of the TAPS than non tanning-dependent individuals.
Based on our data and the literature, it appears that the use of the mCAGE and mDSM-IV-TR cut-points in combination, or a cut-point on the TAPS of 54, or the SITAD tanning dependence cut-point, would likely all result in a similar approximately 5% of college students being classified as tanning dependent. The use of the measures in this way would likely produce very reliable and valid results that healthcare professionals and researchers could use to assess problematic tanning behavior. The SITAD also has the advantage of assessing tanning abuse in addition to dependence. When selecting measures, length is often a deciding factor. The combined mCAGE and mDSM-IV-TR consists of 11 items, the TAPS consists of 16 items, and the SITAD consists of 17 items. Thus, the difference in length is relatively minimal. The mDSM-IV-TR and the combination mDSM-IV-TR with mCAGE are somewhat more complicated to score than the other measures alone, but computerized scoring would minimize this issue.
Strengths of the current study include the psychometric comparison of three measures of tanning dependence using a multi-method approach. Limitations include the use of a convenience sample of female undergraduates from one university. However, because tanning and tanning dependence symptoms are common among this group, this was an appropriate study population. Other limitations include the cross-sectional design and use of self-reported data. However, survey data is found to be quite valid, as has been found for self-reported UV exposure46.
In conclusion, this study is informative in confirming the potential need to intervene with the 5% of college women who are putting themselves at high risk for skin cancer and potential psychiatric and addictive problems that have been shown to be associated with frequent tanning and tanning dependence. 19,20,24,25–28 Dermatologists may want to screen patients who are frequent tanners, and to inform them regarding their behaviors and the impact on skin cancer risk. Individuals who report symptoms on these measures without meeting diagnostic criteria could also be monitored by dermatologists, and intervention should be conducted to prevent increases in tanning behavior or related symptomatology to the level of tanning dependence. Screening of high risk populations such as young adult female indoor tanners using the aforementioned measures could be conducted at regular intervals, and referrals to health behavior specialists could be made. Interventions to reduce indoor tanning that have been found to be efficacious, at least in the research setting, have been published, 47,48 but have yet to be assessed in clinical settings. A prospective longitudinal study assessing changes in tanning behavior and dependence across time would also be informative.
Acknowledgments
We are indebted to Ms. Sara Filseth, BA and Ms. Elizabeth Culnan, BA for their assistance with recruitment and data collection and Ms. Jeanne Pomenti, BS for her administrative assistance with this study and the preparation of this manuscript.
Funding/Support: This study was supported in part by R03CA1504202 (CH), T32CA009035 (SD), and P30CA006927 (Cancer Center Grant).
Contributor Information
C.J. Heckman, Email: carolyn.heckman@fccc.edu.
S. Darlow, Email: susan.darlow@fccc.edu.
J.D. Kloss, Email: jdk29@drexel.edu.
J. Cohen-Filipic, Email: jcohenfilipic@ithaca.edu.
S.L. Manne, Email: mannesl@umdnj.edu.
T. Munshi, Email: teja.munshi@fccc.edu.
A.L. Yaroch, Email: ayaroch@centerfornutrition.org.
C. Perlis, Email: clifford.perlis@fccc.edu.
References
- 1.Ferrucci LM, Cartmel B, Molinaro AM, Leffell DJ, Bale AE, Mayne ST. Indoor tanning and risk of early-onset basal cell carcinoma. J Am Acad Dermatol. 2011;67(4):552–562. doi: 10.1016/j.jaad.2011.11.940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Herzog C, Pappo AS, Bondy ML, Bleyer A, Kirkwood J. Chapter 5: Malignant melanoma. In: Bleyer A, O'Leary M, Ries LAG, editors. Cancer epidemiology in older adolescents and young adults 15 to 29 years of age. Bethesda, MD: US Department of Health and Human Services; 2007. pp. 53–63. [Google Scholar]
- 3.Reed KB, Brewer JD, Lohse CM, Bringe KE, Pruitt CN, Gibson LE. Increasing incidence of melanoma among young adults:An epidemiological study in Olmsted County, Minnesota. Mayo Clin Proc. 2012;87(4):328–334. doi: 10.1016/j.mayocp.2012.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhang M, Qureshi AA, Geller AC, Frazier L, Hunter DJ, Han J. Use of tanning beds and incidence of skin cancer. J Clin Oncol. 2012;30(14):1588–1593. doi: 10.1200/JCO.2011.39.3652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Clarke VA, Williams T, Arthey S. Skin type and optimistic bias in relation to the sun protection and suntanning behaviors of young adults. J Behav Med. 1997;20(2):207–222. doi: 10.1023/a:1025586829179. [DOI] [PubMed] [Google Scholar]
- 6.Hillhouse J, Turrisi R, Shields AL. Patterns of indoor tanning use: Implications for clinical interventions. Arch Dermatol. 2007;143(12):1530–1535. doi: 10.1001/archderm.143.12.1530. [DOI] [PubMed] [Google Scholar]
- 7.Young JC, Walker R. Understanding students' indoor tanning practices and beliefs to reduce skin cancer risks. Am J Health Stud. 1998;14:120–126. [Google Scholar]
- 8.Rhainds M, De Guire L, Claveau J. A population-based survey on the use of artificial tanning devices in the province of Quebec, Canada. J Am Acad Dermatol. 1999;40(4):572–576. doi: 10.1016/s0190-9622(99)70439-1. [DOI] [PubMed] [Google Scholar]
- 9.Brandberg Y, Ullen H, Sjoberg L, Holm LE. Sunbathing and sunbed use related to self-image in a randomized sample of Swedish adolescents. Eur J Cancer Prev. 1998;7(4):321–329. doi: 10.1097/00008469-199808000-00008. [DOI] [PubMed] [Google Scholar]
- 10.Beasley TM, Kittel BS. Factors that influence health risk behaviors among tanning salon patrons. Eval Health Prof. 1997;20(4):371–388. doi: 10.1177/016327879702000401. [DOI] [PubMed] [Google Scholar]
- 11.Amir Z, Wright A, Kernohan EE, Hart G. Attitudes, beliefs and behaviour regarding the use of sunbeds amongst healthcare workers in Bradford. Eur J Cancer Care. 2000;9(2):76–79. doi: 10.1046/j.1365-2354.2000.00195.x. [DOI] [PubMed] [Google Scholar]
- 12.Boldeman C, Jansson B, Nilsson B, Ullen H. Sunbed use in Swedish urban adolescents related to behavioral characteristics. Prev Med. 1997;26(1):114–119. doi: 10.1006/pmed.1996.9986. [DOI] [PubMed] [Google Scholar]
- 13.Cafri G, Thompson JK, Roehrig M, et al. Appearance motives to tan and not tan: Evidence for validity and reliability of a new scale. Ann Behav Med. 2008;35(2):209–220. doi: 10.1007/s12160-008-9022-2. [DOI] [PubMed] [Google Scholar]
- 14.Sjöberg L, Holm LE, Ullen H, Brandberg Y. Tanning and risk perception in adolescents. Health Risk Soc. 2004;6(1):81–94. [Google Scholar]
- 15.American Psychiatric Association. Task Force on DSM-IV. Diagnostic and statistical manual of mental disorders: DSM-IV-TR. Washington, DC: 2000. [Google Scholar]
- 16.Hillhouse JJ, Baker MK, Turrisi R, et al. Evaluating a measure of tanning abuse and dependence. Arch Dermatol. 2012;148(7):815–819. doi: 10.1001/archdermatol.2011.2929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Heckman CJ, Egleston BL, Wilson DB, Ingersoll KS. A preliminary investigation of the predictors of tanning dependence. Am J Health Behav. 2008;32(5):451–464. doi: 10.5555/ajhb.2008.32.5.451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Harrington CR, Beswick TC, Leitenberger J, Minhajuddin A, Jacobe HT, Adinoff B. Addictive-like behaviours to ultraviolet light among frequent indoor tanners. Clin Exp Dermatol. 2011;36(1):33–38. doi: 10.1111/j.1365-2230.2010.03882.x. [DOI] [PubMed] [Google Scholar]
- 19.Mosher CE, Danoff-Burg S. Addiction to indoor tanning: Relation to anxiety, depression, and substance use. Arch Dermatol. 2010a;146(4):412–417. doi: 10.1001/archdermatol.2009.385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mosher CE, Danoff-Burg S. Indoor tanning, mental health, and substance use among college students: The significance of gender. J Health Psychol. 2010b;15(6):819–827. doi: 10.1177/1359105309357091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Poorsattar SP, Hornung RL. UV light abuse and high-risk tanning behavior among undergraduate college students. J Am Acad Dermatol. 2007;56(3):375–379. doi: 10.1016/j.jaad.2006.08.064. [DOI] [PubMed] [Google Scholar]
- 22.Heckman CJ. Indoor tanning: Tanning dependence and other health risks. Household and Personal Care Today-Skin Care:Ethnic, whitening & tanning. 2011:120–122. [Google Scholar]
- 23.Heckman CJ. Indoor tanning: Tanning dependence and other health risks. Household and Personal Care Today – Sun Care. 2011:37–10. [Google Scholar]
- 24.Lostritto K, Ferrucci LM, Cartmel B, et al. Lifetime history of indoor tanning in young people: A retrospective assessment of initiation, persistence, and correlates. BMC Public Health. 2012;12:118. doi: 10.1186/1471-2458-12-118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Phillips KA, Conroy M, Dufresne RG, et al. Tanning in body dysmorphic disorder. Psychiatr Q. 2006;77(2):129–138. doi: 10.1007/s11126-006-9002-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Phillips KA, Dufresne RG, Jr., Wilkel CS, Vittorio CC. Rate of body dysmorphic disorder in dermatology patients. J Am Acad Dermatol. 2000;42(3):436–441. doi: 10.1016/s0190-9622(00)90215-9. [DOI] [PubMed] [Google Scholar]
- 27.Hillhouse J, Stapleton J, Turrisi R. Association of frequent indoor UV tanning with seasonal affective disorder. Arch Dermatol. 2005;141(11):1465. doi: 10.1001/archderm.141.11.1465. [DOI] [PubMed] [Google Scholar]
- 28.Leary MR, Saltzman JL, Georgeson JC. Appearance motivation, obsessive-compulsive tendencies and excessive suntanning in a community sample. J Health Psychol. 1997;2(4):493–499. doi: 10.1177/135910539700200406. [DOI] [PubMed] [Google Scholar]
- 29.Warthan MM, Uchida T, Wagner RF., Jr. UV light tanning as a type of substance-related disorder. Arch Dermatol. 2005;141(8):963–966. doi: 10.1001/archderm.141.8.963. [DOI] [PubMed] [Google Scholar]
- 30.Mayfield D, McLeod G, Hall P. The CAGE questionnaire: Validation of a new alcoholism screening instrument. Am J Psychiatry. 1974;131(10):1121–1123. doi: 10.1176/ajp.131.10.1121. [DOI] [PubMed] [Google Scholar]
- 31.Bisson J, Nadeau L, Demers A. The validity of the CAGE scale to screen for heavy drinking and drinking problems in a general population survey. Addiction. 1999;94(5):715–722. doi: 10.1046/j.1360-0443.1999.9457159.x. [DOI] [PubMed] [Google Scholar]
- 32.Liskow B, Campbell J, Nickel EJ, Powell BJ. Validity of the CAGE questionnaire in screening for alcohol dependence in a walk-in (triage) clinic. J Stud Alcohol. 1995;56(3):277–281. doi: 10.15288/jsa.1995.56.277. [DOI] [PubMed] [Google Scholar]
- 33.Malet L, Schwan R, Boussiron D, Aublet-Cuvelier B, Llorca PM. Validity of the CAGE questionnaire in hospital. Eur Psychiatry. 2005;20(7):484–489. doi: 10.1016/j.eurpsy.2004.06.027. [DOI] [PubMed] [Google Scholar]
- 34.Andrews G, Peters L. The psychometric properties of the composite international diagnostic interview. Social Psychiatry Psychiatr Epidemiol. 1998;33(2):80–88. doi: 10.1007/s001270050026. [DOI] [PubMed] [Google Scholar]
- 35.Hillhouse J, Turrisi R, Stapleton J, Robinson J. Effect of seasonal affective disorder and pathological tanning motives on efficacy of an appearance-focused intervention to prevent skin cancer. Arch Dermatol. 2010;146(5):485–491. doi: 10.1001/archdermatol.2010.85. [DOI] [PubMed] [Google Scholar]
- 36.Heckman CJ, Coups EJ, Manne SL. Prevalence and correlates of indoor tanning among US adults. J Am Acad Dermatol. 2008;58(5):769–780. doi: 10.1016/j.jaad.2008.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.O'Riordan DL, Field AE, Geller AC, et al. Frequent tanning bed use, weight concerns, and other health risk behaviors in adolescent females (United States) Cancer Causes Control. 2006;17(5):679–686. doi: 10.1007/s10552-005-0453-9. [DOI] [PubMed] [Google Scholar]
- 38.Johnson JL. Integrating the transtheoretical model: A quantitative analysis in the area of sun exposure. Diss Abstr Int: Section B: The Sciences and Engineering. 2002;62(9-B):4267. [Google Scholar]
- 39.Jackson KM, Aiken LS. Evaluation of a multicomponent appearance-based sun-protective intervention for young women: Uncovering the mechanisms of program efficacy. Health Psychol. 2006;25(1):34–46. doi: 10.1037/0278-6133.25.1.34. [DOI] [PubMed] [Google Scholar]
- 40.Ajzen I. A theory of planned behavior. In: Kuhl J, Beckman J, editors. Action-control: From cognition to behavior. Heidelberg: Springer; 1985. pp. 11–39. [Google Scholar]
- 41.Becker MH. The health belief model and personal health behavior. San Francisco, CA: Society for Public Health Education; 1974. [Google Scholar]
- 42.Nunnally JC. Psychometric theory. 2nd ed. New York: McGraw-Hill; 1978. [Google Scholar]
- 43.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–174. [PubMed] [Google Scholar]
- 44.Kenny DA. [[cited 2012 October 1]];Structural equation modeling. 2012 Available from: http://davidakenny.net/cm/causalm.htm.
- 45.Hu L, Bentler PM. Cutoff criteria for fit indices in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equ Modeling. 1999:61–55. [Google Scholar]
- 46.Daniel LC, Heckman CJ, Kloss JD, Manne SL. Comparing alternative methods of measuring skin color and damage. Cancer Causes Control. 2009;20(3):313–321. doi: 10.1007/s10552-008-9245-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gibbons FX, Gerrard M, Lane DJ, Mahler HI, Kulik JA. Using UV photography to reduce use of tanning booths: A test of cognitive mediation. Health Psychol. 2005;24(4):358–363. doi: 10.1037/0278-6133.24.4.358. [DOI] [PubMed] [Google Scholar]
- 48.Hillhouse JJ, Turrisi R. Examination of the efficacy of an appearance-focused intervention to reduce UV exposure. J Behav Med. 2002;25(4):395–409. doi: 10.1023/a:1015870516460. [DOI] [PubMed] [Google Scholar]


